Abstract
Purpose of Review
The aim of this paper is to reflect on leptospirosis studies conducted in Honduras to determine the public health burden of leptospirosis in the country, as well as gain insight into the transmission dynamics of leptospirosis in Honduras.
Recent Findings
Leptospirosis is a global disease affecting many Central American countries including Honduras. In the last two decades, Honduras has had numerous outbreaks of leptospirosis in both animals and humans. Leptospirosis appears to have nationwide endemic tendencies based on epidemiological surveillance and seroprevalence studies.
Summary
In Honduras, based on seroprevalence data and reported cases and outbreaks, leptospirosis appears to be a disease that is endemic, underreported, and at times misidentified. Several high-risk groups of people for leptospirosis have been identified based on occupation, location to potentially infected water sites, and/or those in close proximity to reservoir animals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Leptospirosis is an infectious disease produced by Leptospira spp. of pathogens. Twenty-one known species of Leptospira exist which can be divided into three groups: group I comprises nine pathogenic species; group II is comprised of five intermediate pathogen species and six nonpathogenic species. A final group exists that contains serovar pathogens and nonpathogens. In this group, some 300 Leptospira serovars are identified [1, 2].
Leptospirosis affects animals such as rats, horses, cows, pigs, and others. In some of these animals, the disease can take a drastic turn that can affect reproduction causing abortions and malnourishment. Humans become infected with leptospirosis when they come into contact with infected water, food, or animal remains, at which point leptospirosis is considered a zoonotic disease [3].
Through observation, we see that the prevalence of leptospirosis increases during the rainy season in tropical and subtropical areas. The overall incidence of leptospirosis is unknown, however, according to World Health Organization data. In populations with high-risk factors, during outbreaks, and/or in tropical areas during the rainy season, the incidence can reach more than 100 per 100,000 people [4]. A noteworthy factor in transmission in rural and semi-rural areas in Honduras is the lack of wild animal control. Often, these animals cohabitate in rural and semi-rural areas with people who present as infected.
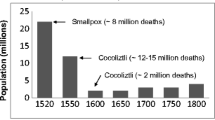
More recent data obtained from Leptospirosis Burden Epidemiology Reference Group’s (LERG) second meeting in 2010 estimates the incidence, excluding outbreaks, of the annual media of human leptospirosis to be 5 cases for every 100,000 inhabitants. Nonetheless, this data may be an underestimate, knowing that in some areas many cases of leptospirosis are diagnosed incorrectly, or not at all, due to the lack of access to laboratory confirmation testing. It is important to note that the greatest annual incidence of leptospirosis occurs in Africa (95.5 per 100,000 people), followed by the Pacific West (66.4), the Americas (12.5), South East Asia (4.8) and Europe (0.5) [5]. This paper provides historical facts as well as a survey of several epidemiological and seroprevalence studies of leptospirosis in Honduras (Fig. 1 and Table 1).
Epidemiological and Seroprevalence Studies of Leptospirosis in Honduras
In Honduras, the first report of leptospirosis occurred in 1964. This outbreak occurred in a stock of pigs coming from the USA [6•, 7]. In 1975, veterinarian Luis A. Espinoza completed a study of leptospirosis prevalence in bovines in the Comayagua Valley of west-central Honduras, in which he found a prevalence rate of 38% [7, 10]. This study also investigated the frequency of serovars, with Bataviae, Pyrogenes, Canicola, Pomona, Grippotyphosa, Sejroe and Autumnalis reported as the most frequently seen. After this discovery, in 1983, the Institute of Veterinarian Medical Investigations from the Secretary of Agriculture and Ranching (Secretaria de Agricultura y Ganadería) (SAG) initiated a system of laboratory surveillance in swine and cattle in 15 of the 18 Honduran departments [6•].
The first cases of leptospirosis in humans in Honduras were reported in 1995 [6•]. These cases occurred in the Department of Choluteca, to the south of the country bordering Nicaragua. Simultaneously, Nicaragua reported an outbreak of 2000 cases of leptospirosis in the community of Achuapa, located to the northeast of the country. Of these cases, 40 were fatal. The five Honduran cases were diagnosed clinically and epidemiologically, of which one was confirmed by the Centers for Disease Control and Prevention (CDC) in Atlanta [8, 10]. An alarming four of the five patients (80%) ended in mortality from pulmonary hemorrhaging [10].
In 1996, leptospirosis was newly introduced in the south of the country, the Departments of Choluteca and Valle reported five cases with clinical and epidemiological symptoms of leptospirosis. While there were no clinical labs for diagnosing leptospirosis at that time, the clinical presentations were similar to the described outbreak in Achuapa, Nicaragua with principal characteristics of massive pulmonary hemorrhaging [9, 11].
In November of 1998, Hurricane Mitch tore through Central America causing extensive flooding [12]. Subsequently, various leptospirosis outbreaks occurred across the country, with a greater number of cases in the Valle de Sula. A total of 237 suspect cases presented, of which 172 were confirmed for leptospirosis, 28% of these cases were confirmed by laboratory testing while the remaining were confirmed clinically and epidemiologically [10, 12]. From that moment on, leptospirosis was considered a public health problem in Honduras, warranting periodical observation for outbreaks. At times, the illness can go unnoticed due to the fact that it is a febrile disease with symptoms similar to dengue, which is endemic in the country. This potential risk of overlooking leptospirosis poses as dangerous, as leptospirosis can be fatal.
In 1998, a study on the seroprevalence of leptospirosis was conducted in the city of Marcovia, Choluteca, Honduras. This study was a collaborative force between SAG and the Secretaria de Salud (Secretary of Health), with financial and technical support from the Pan American Health Organization (PAHO). The study occurred in a population of children greater than 5 years old, utilizing the Microaglutination Technique (MAT) resulting in a seroprevalence of 29% [10, 13]. Following the culmination of recent outbreaks and studies, leptospirosis was established as a required immediate reportable disease in 1999.
During October and November of 2001, another study of leptospirosis seroprevalence was conducted in three communities in Honduras. Two of these communities, Ajuterique and Villa de San Antonio, are located in the Department of Comayugua while the community of Villa de San Francisco is located in the Department of Francisco Morazán. These communities were chosen for the seroprevalence study based on characteristics they possess favoring the proliferation of leptospirosis: tropical climate, rural areas in which humans and reservoir animals interact, and populations that are imminently agricultural. The population studied was distributed by age group, and the group with the largest proportion was comprised of 15 to 44-year-olds. The patient serum samples were analyzed with both enzyme-linked immunosorbent assay (ELISA) and MAT techniques resulting in a seroprevalence of 31%. This study demonstrates that the seroprevalences of the three communities were similar, with a frequency of reactives slightly higher in the Villa de San Antonio community. A direct relationship between seropositivity and the type of labor the population carried out was not observed. The most frequent serovars found were Australis, Sejroe Hardjo and Icterohaemorragiae [14].
Another notable serovprevalence study was carried out in 2002 by a microbiology graduate thesis student at La Universidad Nacional Autónoma de Honduras (UNAH). This study included three populations: sewage workers, slaughterhouse workers and blood donors. The first two groups were chosen as at-risk populations because of their occupational possible contact with contaminated water and animals. The blood donor group was chosen to gain an understanding of the seroprevalence in the general population. The prevalence resulted in 66% of the sewage workers having a major reactivity in the Sejroe Hardjo, Bratislava and Ballum serovars. In the slaughterhouse workers, the prevalence was 26%, with the greatest reactivity to Autumnalis, Pomona and Ballum. In the blood donors, the prevalence was 28% with the top serovar reactors being Ballum, Sejroe Hardjo and Bratislava. Surprisingly, the prevalence in blood donors was somewhat greater than the slaughterhouse workers, possibly due to the fact that the slaughterhouse workers use protective clothing during the slaughtering process, which is believed to be a protective factor when coming in contact with contaminated materials. One should note, however, that sewage workers do not use protective clothing, and had the highest seroprevalence among all three groups [15].
During her field work in 2004, medical student Renske Oegama from The University of Amsterdam completed a sample study of patients from Locomapa, a rural area in the state of Yoro, Honduras. Samples from 22 suspect leptospirosis patients were analyzed with Dri Dot, ELISA IgM and MAT, and none were conclusive with leptospirosis. In this same location, however, another population was studied from which 247 serum samples were analyzed, most of whom were children. Of the samples, 22 were found to be reactive, for a prevalence of 8.9%. The serovars found were related to the domestic and wild animals nearby, none of the domestic animals, conversely, were found to be an important risk factor. The serovars that were most frequent were Australis, Autumnalis, Grippothyphosa, Icterohaemorrhagiae, Javanica, Sejroe and Semaranga [16].
In 2005 and 2006, a very important project was developed with the European Economic Community in conjunction with the Leptospirosis Reference Center, Department of Biomedical Research, Royal Tropical Institute, Amsterdam, The Netherlands. Other leptospirosis collaborating experts were the Leptospirosis laboratory (OIE Reference Laboratory), Bacteriology Department, Department of Veterinary Science, Queen’s University of Belfast, Belfast, United Kingdom and the Virology Department, Collaborating Center for Viral Diseases, “Pedro Kouri” Tropical Medicine Institute, Habana, Cuba. The initial idea of the collaboration was to create a database by way of a multidisciplinary study on hemorrhagic fevers in Central America. The project objective was to develop laboratory tools and a self-supporting international surveillance system for hemorrhagic fevers, initially focusing on leptospirosis and dengue. This project involved four countries in Central America: Costa Rica, Nicaragua, El Salvador and Honduras. Due to political reasons, the only countries remaining in the study were Nicaragua, through support from the Ministerio de Salud (Ministry of Health) (MINSA), and Honduras, through support from researchers at UNAH. Secondary objectives in this project were to establish an analysis system and data exchange; establish tests which are easy and practical to maneuver; optimize the MAT test; introduce quality control techniques; investigate the usefulness of leucocyte counts for differentiation between dengue and leptospirosis; identify frequent leptospirosis serovars in the region; identify reservoirs and clinical patterns related to leptospirosis serovars, known transmission and technological transmission. As a result of several projects continuing like those aforementioned, the majority of the objectives were possible [17] such as development and validation of real-time PCR in leptospirosis diagnosis [18] as well as new serovar isolated in patients in Costa Rica [19].
Several other noteworthy seroprevalence studies have been conducted in Honduras, one of which was conducted in a town named Matasanos in Tamara, near the northeast part of Tegucigalpa (capital city). In this town in 2005, there were two confirmed cases of leptospirosis, both resulting in fatality. The seroprevalence obtained by MAT was 19.73%, and the risk factor more frequently noted was contact with still, dirty water as well as contact with dogs and rodents. The most frequent serovars found were Patoc (nonpathogenic), Cynopteri and Ballum [20]. As a result, another important seroprevalense study was conducted on a population who worked and/or lived near the city’s waste deposit site in Tegucigalpa. The population included 93 adolescents between the ages of 11 and 19 years old. The MAT technique was used and demonstrated 15 positive results with the following serovars: Autumnalis, Canícola, Ballum, Icterohaemorragiae and Celledoni. The overall seroprevalence for the population was 14% [21, 22].
From 2002 through 2006, in order to gain a better understanding of the seroprevalence of leptospirosis in the capital city of Honduras, Tegucigalpa, the Honduran state and medical school and hospital, Hospital Escuela e Instituto Hondureño de Seguridad Social de Tegucigalpa, and Health Region #3 in San Pedro Sula, supported the local hospital by donating the rapid Dri Dot test for sifting through patient samples with symptomatology of leptospirosis. Of these 129 symptomatic patients, samples were analyzed with four different techniques: the rapid Dri Dot test, the rapid Lepto Teck test, the ELISA IgM commercial test from PanBio (Australia) and the MAT technique. The samples were sent to and analyzed in the UNAH laboratories. The positive percentage was 23.2% for the MAT test, 16.3% for the ELISA IgM test and 14.4% for the Dri Dot test. It is possible that the greater number of reactives for the MAT test is due to the fact that in this test, total antibodies are analyzed. Utilizing the MAT techniques, one can conclude that the established frequent serovars in Honduras for the studies realized are Akiyami, Australis, Autumnales, Ballum, Bataviae, Canicola, Grippotyphosa, Hebdomadis, Icterohaemorragiae, Panama, Pomona and Sejroe. Within this group, the most frequent were Australis and Icterohaemorrhagiae [17].
In this same project, 29 samples originated from patients who had clinical dengue symptoms but were negative for dengue serology. In those samples, the presence of IgM was investigated by Leptospira IgM ELISA (PanBio) and using MAT. From these 29 samples, one (3.4%) resulted positive for IgM Leptospira with ELISA and was confirmed by MAT with Leptospira interrogans, serovar Cynopteri titer 1:160, and Icterohaemorrhagiae titer 1:320. The project coordinator, Biomedical Research, Royal Tropical Institute, organized the participants to carry out the proficiency test with the MAT technique in order to guarantee the obtained results [17].
In addition to gaining a greater understanding of leptospirosis confirmation testing, several other community benefits stemmed from this collaborative investigation. First, management of diagnostic leptospirosis techniques was achieved. Secondly, microbiology students from UNAH had the opportunity to craft both laboratory skills as well as field epidemiology techniques. Third, medical interest to determine clinical patterns related to leptospirosis was awakened. More frequent risk factors and the symptomatology of the illness were established by means of an instrument developed as a result of the completed studies. Finally, the coordinators from the Department of Biomedical Research, Royal Tropical Institute, Amsterdam, The Netherlands and the Leptospirosis Laboratory (OIE Reference Laboratory), Bacteriology Department, Department of Veterinary Science, Queen’s University of Belfast, Belfast, UK in the region received molecular technique training on leptospirosis. The results of the studies from this project were presented in regional and international workshops, of which contributed to the surveillance of leptospirosis in Latin America [17].
Conclusion
Based on the survey of these epidemiological and seroprevalence studies, one can conclude that leptospirosis is an important public health concern in Honduras. Five states were identified with consistent reports of leptospirosis human and veterinarian cases. Cases of leptospirosis are currently reported in Honduras in small outbreaks that occur periodically in the southern, central and northern zones of the country, likely as an underreported illness. After analyzing the seroprevalence studies, prevalence of leptospirosis is noteworthy. We also conclude that occupations that bring employees into contact with contaminated animals, animal remains, and/or water may place workers at risk, for which the use of personal protective equipment is suggested. Finally, the crafting of laboratory techniques, which is primarily dependent on serology, in confirming leptospirosis cases in Honduras is important and MAT technique is encouraged.
Abbreviations
- (LERG):
-
Leptospirosis Burden Epidemiology Reference Group
- (SAG):
-
Secretary of Agriculture and Ranching (Secretaria de Agricultura y Ganadería)
- (CDC):
-
Centers for Disease Control and Prevention
- (PAHO):
-
Pan American Health Organization
- (MAT):
-
Microscropic Agglutination Test
- (ELISA):
-
Enzyme-linked immunosorbent assay
- (UNAH):
-
La Universidad Nacional Autónoma de Honduras
- (MINSA):
-
Ministerio de Salud (Ministry of Health)
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Saito M, Villanueva SY, Kawamura Y, Iida KI, Tomida J, Kanemaru T, et al. Leptospiraidonii sp. nov., isolated from environmental water. Int J Syst Evol Microbiol. 2013;63(7):2457–62.
Morey RE, Galloway RL, Bragg SL, Steigerwalt AG, Mayer LW, Levett PN. Species-specific identification of leptospiraceae by 16S rRNA gene sequencing. J Clin Microbiol. 2006;44(10):3510–6.
Rodríguez Alonso B, Gómez de Haz HJ, Pérez Maza B, Cruz de la Paz R. Diagnóstico y tratamiento de la leptospirosis humana. Revista cubana de medicina general integral. 2001;17(1):68–73.
World Health Organization. (2003). Human leptospirosis: guidance for diagnosis, surveillance and control
World Health Organization: Report of the second meeting of the Leptospirosis Burden Epidemiology Reference Group. (2011).
• Velasquez RT, MD. Situacion epidemiologica de la leptospirosis humana, Honduras 2007-2013. Presentation Secretaria de Salud Honduras: Ciudad de Choluteca, Honduras. 2013. An important presentation on the state of leptospirosis in Honduras
Rodezno CE. Pais: Honduras. Presentation at the reunion internacional de paises que estan enfrentando brotes de leptospirosis en las Americas. Managua, Nicaragua: PAHO; 2012.
Ochoa JE, Sánchez A, & Ruiz I. Epidemiología de la leptospirosis en una zona andina de producción pecuaria. 2000.
Agriculture, U. D., & Centers for Disease Control and Prevention, Zaki SR, Shieh WJ. Leptospirosis associated with outbreak of acute febrile illness and pulmonary haemorrhage, Nicaragua, 1995. Lancet. 1996;347(9000):535–6.
La leptospirosis. BVS Honduras. Website: www.bvs.hn/honduras/salud/laleptospirosis.pdf. Retrieved feb 2, 2017.
Secretaría de Salud., & Dirección de vigilancia de la Salud. Manual para el diagnóstico, tratamiento y prevención de la leptospirosis. Tegucigalpa, MDC Honduras, C.A. 2003.
Naranjo M, Suarez M, Fernandez C, et al. Study of leptospirosis outbreak in Honduras following hurricane Mitch and prophylactic protection of the vax-SPIRAL vaccine. MEDICC Rev. 2008;10(3):38–42. Retrieved February 2, 2017.
Solorzano O. Leptospirosis en Honduras, Tegucigalpa. Honduras: Dirección de Vigilancia de la Salud; 2005.
Fernández R. Thesis: Seroprevalencia de leptospirosis en tres comunidades de Honduras. Octubre-Noviembre 2001. UNAH, 2001.
Rosales S. Tesis de Leptospirosis en tres poblaciones en Honduras. UNAH, 2002.
Oegema R. Thesis leptospirosis and dengue in Honduras. Amsterdam: University of Amsterdam; 2004.
Lepto & Dengue Survey. United Kingdom: European Commission. 2006
Ahmed A, Engelberts MFM, Boer KR, Ahmed N, Hartskeerl RA. Development and validation of a real-time PCR for detection of pathogenic Leptospira species in clinical materials. PLoS ONE. 2009;4(9), e7093. doi:10.1371/journal.pone.0007093.
Valverde MA, Goris MGA, Gonzalez V, et al. New serovars of Leptospira isolated from patients in Costa Rica: implications for public health. Journal of Medical Microbiology. (13): 1263-1271. doi: 10.1099/jmm.0.058545-0.
Galo CM, Comunidad Economica Europea, [data file], UNAH, Tegucigalpa, Unpublished dataset, cited with permission. 2004.
Galo CM, Comunidad Economica Europea, [data file], UNAH, Tegucigalpa, Unpublished dataset, cited with permission. 2005.
Faine S. Guidelines for the control of Leptospirosis. World health Organization (WHO Offset Publ. No.67). England: World Health Organization. 1982: 161.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Carmen M. Galo and Kaila A. Fagerstrom declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Leptospirosis in Mesoamerica
Rights and permissions
About this article
Cite this article
Galo, C.M., Fagerstrom, K.A. A Chronological Survey of Leptospirosis in Honduras. Curr Trop Med Rep 4, 47–51 (2017). https://doi.org/10.1007/s40475-017-0103-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40475-017-0103-9