Abstract
Pancreas transplantation offers a functional cure for many patients suffering from diabetes mellitus. Although the outcomes of pancreas transplants were originally plagued with high rates of acute cellular rejection, innovations in immunosuppression regimens over the last two decades have helped steadily improve the graft survival of pancreas transplants. This review surveys the latest trends in immunosuppressive management for pancreas transplant recipients, discussing the controversies and weighing the evidence supporting induction therapy, steroid avoidance/withdrawal, mTOR inhibitors, and new regimens based on costimulatory blockade agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
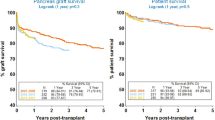
The last decade has posed a frustrating contradiction for the field of pancreas transplantation: despite marked improvements in graft outcome, the volume of pancreas transplants has tapered substantially. In the USA, newly listed active candidates on the pancreas wait list declined from 2153 to 991 since 2003, and the number of pancreas transplants performed in the USA similarly dropped over 30 % during the same time period [1••]. In contrast, 1 year graft function for pancreas transplants alone increased from 51.5 % in 1987–1993 up to 77.8 % in the 2006–2010 cohort [2]. Pancreatic graft outcomes for simultaneous pancreas-kidney (SPK) transplants were better, approaching 85 % at 1 year in the modern era [3]. While technical innovations likely account for some of the improved outcomes, recent innovations in pancreas transplant post-operative management and immunosuppression play a significant role. This critical review will examine the latest evidence surrounding pancreas transplantation immunosuppression.
Induction Therapies
One important innovation in pancreas transplant immunosuppression is the widespread adoption of induction therapy. According to the Scientific Registry of Transplant Recipients (SRTR), the percentage of adult transplant recipients receiving some form of induction therapy at the time of transplant has risen from 64 % to over 90 % over the last 15 years [3]. This high-dose intravenous immunosuppression given at the time of transplant serves to suppress early acute allograft rejection, enables lower doses of maintenance immunosuppression to be given, and may even promote the expansion of regulatory immune cells that suppress alloreactivity [4]. In theory, induction therapy would be desirable for pancreas allograft recipients given the higher rate of rejection compared to recipients of renal or liver allografts, as well as the greater difficulty in diagnosing acute rejection in pancreatic allografts.
However, despite the nearly universal adoption of induction therapy for pancreas transplantation, available data supporting its use is somewhat limited and often extrapolated from trials conducted in renal transplant recipients. Only two multicenter randomized trials of induction therapy have been performed in pancreas transplant recipients, and both of these utilized daclizumab, an anti-CD25 (interleukin-2 receptor) monoclonal antibody that has subsequently been withdrawn from the market. The first of these, the PIVOT trial, compared daclizumab to no induction in SPK transplant recipients treated with corticosteroid, tacrolimus, and mycophenolate mofetil (MMF) as maintenance therapy [5, 6]. Similar rates of acute rejection, kidney graft loss, and pancreas graft loss were seen in both the daclizumab induction and no induction groups, at both 6-month and 3-year time points. A second multicenter induction trial was published in 2003, comparing no induction to induction with interleukin-2 receptor antagonists (59 % of induction group recipients) or T cell-depleting induction (41 % of induction group) [7]. As with the earlier trial, there were no significant differences in patient or graft survival at 1 year between the induction and no induction groups. There was a trend towards a lower rate of biopsy-proven acute cellular rejection within the first year of transplant (13 versus 21 %, p = 0.08), but it did not reach significance [7].
In addition to these multicenter trials, a number of single-center randomized trials of induction therapy versus no induction in pancreas transplant recipients have been conducted over the last 20 years [8–10]. Corroborating the results of the multicenter trials, a large single-center trial of interleukin-2 receptor antagonists as induction therapy also failed to find any improvement in graft survival, acute rejection rates or patient survival in the induction versus no induction groups at 6 months post-transplant [8]. Similarly, a study comparing induction with rabbit anti-thymocyte globulin (thymoglobulin) versus no induction in SPK transplant recipients found equivalent levels of graft and patient survival in both groups, although there was a significantly lower rate of biopsy-proven renal allograft rejection in the group that received induction therapy (36 versus 76 %, p < 0.01) [10]. These somewhat ambivalent findings were also reflected in a large retrospective analysis of registry data examining 6860 SPK transplant recipients in the USA. This registry analysis found that regardless of whether no induction, alemtuzumab induction, thymoglobulin induction, or basiliximab induction was employed, there was no significant difference in patient survival, pancreas or renal allograft survival, or delayed renal graft function. However, use of any induction therapy was definitely associated with higher rates of rehospitalization within 6 months of transplant, likely due to heightened risks of infectious complications [11••].
Over the last decade, SRTR data reveals a clear trend away from the use of interleukin-2 receptor antagonists (e.g., basiliximab) for induction in pancreas transplant recipients and towards T cell-depleting induction agents such as alemtuzumab and thymoglobulin. During the past 10 years, use of interleukin-2 receptor antagonists has dropped by half (to 10 % of pancreas recipients), whereas almost 80 % of pancreas recipients now receive induction with some form of T cell-depleting agent [1••]. Several single-center retrospective analyses of interleukin-2 receptor antagonists versus T cell-depleting agents as pancreas transplant induction agents have been published. Bazerbachi et al. compared thymoglobulin induction with basiliximab induction in SPK transplant recipients, demonstrating lower rates of acute rejection both at 3 months and at 1 year post-transplant with thymoglobulin, although there was no statistically significant difference in renal or pancreatic allograft survival between these two induction regimens [12]. In contrast, Magliocca et al. published a similar retrospective trial of alemtuzumab induction versus basiliximab in SPK transplant recipients at the University of Wisconsin, and they found no difference in the rates of graft survival or acute rejection between the two induction regimens, although there was a higher rate of cytomegalovirus (CMV) viremia in the recipients treated with alemtuzumab [13, 14].
Several studies comparing alemtuzumab and thymoglobulin as induction agents have been conducted. One single-center randomized controlled trial by Farney et al. evaluated the two induction regimens in a mixed study population of patients receiving either a kidney transplant alone or a simultaneous pancreas-kidney transplant [15•, 16, 17]. A 5-year follow-up revealed no significant differences between the two groups for patient, renal graft, or pancreatic graft survival. Likewise, there was no difference in glomerular filtration rate, hemoglobin A1c, or C-peptide levels after 5 years in either induction group. However, there was a non-significant trend towards decreased rates of acute rejection (21 % alemtuzumab versus 44 % thymoglobulin, p = 0.12) and major infections (39 versus 67 %, p = 0.13) with alemtuzumab use, and the rates of CMV viremia were significantly lower with alemtuzumab (0 versus 17 %, p = 0.05) [15•]. Furthermore, a preliminary analysis found alemtuzumab induction was more cost-effective than thymoglobulin ($1474 versus $4996, p < 0.001) [16]. A second single-center randomized trial also compared alemtuzumab with thymoglobulin induction. Recipients of alemtuzumab induction received tacrolimus monotherapy as maintenance immunosuppression, whereas those receiving thymoglobulin received tacrolimus + MMF + steroids as maintenance [18]. In contrast to the trial by Farney et al., this study found no difference in either allograft survival or rates of pancreatic or kidney acute rejection [18]. Another single-center retrospective trial also found no difference in rejection rates or graft survival between thymoglobulin and alemtuzumab induction [19].
In summary, few studies of induction therapy have demonstrated an impact on graft or patient survival. Several trials have demonstrated a potential benefit with lower rates of early acute rejection in patients treated with T cell-depleting induction agents such as alemtuzumab and thymoglobulin. Additionally, some evidence suggests that induction therapy lowers the risk of recurrent autoimmune diabetes in type 1 diabetics receiving pancreas transplants [20•]. These benefits may be at the cost of increased rates of CMV viremia, ranging from 16 to 46 % in published studies (although at least one group found a similar low rate of tissue-invasive CMV regardless of whether induction is used) [4, 7].
Steroid Withdrawal and Steroid-Sparing Regimens
Another important trend in pancreas transplant immunosuppression over the past decade is growth in the number of patients receiving steroid-sparing regimens or regimens with a rapid steroid withdrawal (usually defined as within 14 days post-transplant). According to SRTR data, since 1998 the rate of corticosteroid usage at the time of pancreas transplant has plummeted from 93.7 to 65.7 %, and a similar growth was observed in the percentage of pancreas transplant patients receiving steroid-sparing maintenance immunosuppression [1••, 3]. Corticosteroids not only promote hyperglycemia and post-transplant diabetes, but additionally induce hypertension and hyperlipidemia, which together serve to increase the cardiovascular risk of pancreas transplant recipients [21]. Death with a functioning graft is the leading cause of graft loss in SPK transplant recipients, and the vast majority of these recipient deaths are due to cardiovascular causes [2], suggesting any change in immunosuppression that alters these cardiovascular risks would be desirable.
Many studies of steroid-sparing pancreas transplant immunosuppression have been published, mostly as non-randomized retrospective case series [22–35]. Perhaps the largest retrospective review of over 27,000 pancreas transplants in the UNOS database found that steroid maintenance therapy was significantly associated with an increased risk of infectious complications compared to recipients receiving steroid-free maintenance immunosuppression. It was not associated with any significant difference in long-term patient or graft survival [36••].
Although the majority of data supporting steroid-sparing immunosuppression or early steroid withdrawal is challenged, several high-quality randomized trials and meta-analyses have been conducted. A Cochrane database meta-analysis on steroid avoidance or withdrawal for pancreas transplant recipients was recently published in 2014 [37•] and identified three randomized controlled trials (RCTs) of steroid-sparing or steroid-minimizing immunosuppression in pancreas transplant patients [38–40]. In the first, Gruessner et al. examined chronic maintenance immunosuppression with steroids versus withdrawal of steroids within 4 to 8 weeks post transplant in a mixed group of SPK and pancreas-after-kidney transplant recipients [39]. The main finding was that neither acute rejection rates nor graft loss increased with the cessation of steroids. The only notable difference between the treatment groups was a reduction in cholesterol levels noted at a 6-month follow-up in the steroid withdrawal group [39]. Subsequently, this same center published in abstract form a later randomized trial comparing rapid steroid withdrawal (within 4 days of transplant) with late withdrawal (over a period of 6 months) in a separate group of SPK transplant recipients who received induction therapy with thymoglobulin [40]. There was no difference in graft survival in either group, although the serum lipid profile was better in the group rapidly weaned off steroids [40]. In the last of these studies, Cantarovich et al. at Nantes University Hospital compared steroid-sparing immunosuppression with late steroid withdrawal at post-op day 90 in a group of SPK transplant recipients [38]. There was no difference in biopsy-proven acute rejection rates, pancreas or kidney graft survival, or patient survival between the steroid and steroid-free regimens. In contrast to the earlier trials, no difference in lipid profile was noted between the two groups. There were a significantly higher number of urinary tract infections in the late withdrawal group compared to the steroid avoidance group. Renal function (as measured by serum creatinine level at 1 year) was significantly worse in the group of recipients treated with the steroid-free regimen [38]. Thus, none of these randomized trials demonstrated an adverse impact of steroid withdrawal on graft survival, and the majority demonstrates possible cardiovascular benefits (and possibly decreased rates of infectious complications) with early steroid withdrawal or steroid-sparing regimens.
A central weakness of all three trials is the short-term follow-up of 6 months to 1 year. The finding of higher serum creatinine levels 1 year after transplant in SPK recipients treated with the steroid-sparing regimen in the Cantarovich et al. trial might be a concerning indicator of later consequences of steroid avoidance. Given the available data, it is unsurprising that the Cochrane review determined that insufficient evidence for benefit or harm of steroid withdrawal in pancreas transplantation can be identified [37•].
mTOR Inhibitors
The use of mTor inhibitors in pancreas transplant was first described in 2000 [41] and is now incorporated in maintenance immunosuppression regimens at many centers. mTOR inhibitors were swiftly embraced by many pancreas transplant centers as a result of presumed lower nephrotoxicity. Within 2 years of introduction, initial mTOR inhibitor use increased from 1 to 19 % of all adult pancreas transplant recipients [3]. Subsequent enthusiasm has waned somewhat over the past decade, and now, the latest SRTR data suggests that only 7 % of pancreas transplant recipients are started with de novo mTOR inhibitors as part of their immunosuppression regimen [1••].
While corticosteroids and calcineurin inhibitors (CNI) are mainstays of pancreas transplant immunosuppression, both induce hyperglycemia and diabetes [21]. mTOR inhibitors may offer a potential means of minimizing or even eliminating diabetes-inducing drugs from pancreas transplant immunosuppression regimens. For example, many corticosteroid-sparing immunosuppression regimens depend on T cell-depleting induction therapy (usually thymoglobulin) with maintenance immunosuppression based on the combination of low-dose CNI (usually tacrolimus) and either sirolimus or everolimus [19, 30, 42–44]. Other investigators have described using everolimus in a steroid-free protocol to reduce CNI dosage [45, 46]. Sirolimus has also been used as a rescue therapy in pancreas transplant recipients who develop chronic allograft nephropathy from CNI nephrotoxicity, with improved renal function after conversion to sirolimus [47–49]. Although wound healing and post-op fluid collections are concerns with mTOR inhibitor use, at least one randomized trial found no difference in early complication rate in SPK transplant recipients treated with tacrolimus/MMF versus tacrolimus/sirolimus maintenance immunosuppression [50]. Furthermore, although mTOR inhibitors are known to exacerbate proteinuria, at least one study of SPK transplant recipients on a regimen including sirolimus found no increase in proteinuria or serum creatinine compared to those receiving conventional immunosuppression [51].
Other trials have employed mTOR inhibitors as a substitute for MMF, seeking to avoid the leukopenia and GI toxicity often associated with MMF. Ciancio et al. at the University of Miami conducted a randomized single-center trial of sirolimus versus MMF in SPK transplant recipients also receiving low-dose tacrolimus and corticosteroid immunosuppression [52]. Compared to MMF, freedom from biopsy-proven acute kidney or pancreas rejection was superior for sirolimus at both 1 year and 10 year time points. However, there was no significant difference in overall patient or graft survival between the sirolimus and MMF groups [52]. Sageshima et al. conducted a similar retrospective study using everolimus rather than sirolimus, and compared to MMF maintenance therapy there was equivalent short-term patient and graft survival [53•]. Everolimus and sirolimus may have a role in pancreas transplant patients who develop leukopenia or GI intolerance associated with MMF use [21].
Finally, mTOR inhibitors may enable the escalation of immunosuppression in immunologically challenging pancreas transplant recipients. For example, one retrospective study found that in an immunologically high-risk recipient population (i.e., young recipients of pancreas transplants alone), addition of sirolimus to conventional maintenance immunosuppression with long-term prednisone, tacrolimus and MMF was associated with higher rates of long-term graft survival [54].
Costimulatory Blockade
The newest strategy to minimize toxicity in pancreas transplant immunosuppression is the use of costimulatory blockade agents. These agents are utilized to eliminate chronic exposure to CNI, since maintenance therapy with CNI such as tacrolimus or cyclosporine is associated with nephrotoxicity and a host of metabolic side effects including hyperglycemia [21, 46]. In one study of pancreas transplant alone, high tacrolimus levels (>12 mg/dL) at 6 months post transplant was the only independent risk factor associated with decline in native renal function [55]. As a result, many efforts have focused on regimens that do not rely on calcineurin inhibitors. One of the most promising regimens utilizes belatacept, a costimulatory blockade drug that suppresses alloresponses by blocking the critical CD28 costimulatory signals required for full activation of alloreactive T cells [56]. In renal transplant recipients, belatacept was shown to improve long-term renal allograft function compared to conventional treatment with CNI-based immunosuppression [57]. However, these long-term superior outcomes come at the cost of an increased incidence of early rejection.
The potential utilization of belatacept for pancreas transplant immunosuppression was first demonstrated by the Indiana University group, which published a case report of two SPK transplant recipients who developed CNI toxicity with the standard tacrolimus-based maintenance immunosuppression, and were subsequently transitioned successfully to CNI-sparing belatacept maintenance therapy with improved renal function and no pancreas or renal allograft rejection [58••]. Outcomes of belatacept-based immunosuppression for pancreas transplant recipients will be more fully evaluated in the Clinical Trials in Organ Transplantation 15 (CTOT-15) trial, which utilized a calcineurin-inhibitor sparing regimen with belatacept maintenance therapy in SPK transplant recipients. The findings of this trial are expected to be published in Spring 2016.
Conclusion
Advances in transplant immunosuppression over the past 20 years can be credited with many of the notable improvements in pancreas allograft and patient survival. Many of these innovations seek to eliminate components of traditional immunosuppression (such as prednisone and tacrolimus) that are known to cause hyperglycemia, diabetes, increased cardiovascular risk (via hyperlipidemia and hypertension), and nephrotoxicity. The widespread adoption of both induction therapy and steroid-sparing/early steroid withdrawal regimens exemplifies these developments. mTOR inhibitors such as sirolimus have also been employed to achieve similar goals. Finally, belatacept is the first novel transplant immunosuppression drug in almost two decades, and it also offers a potential means of eliminating nephrotoxic maintenance immunosuppression with tacrolimus. Fifty years after the first successful human pancreas transplant, there still remains no consensus on the “gold standard” immunosuppression regimen for pancreas transplant recipients. Even less is known about the proper immunosuppressive management of sensitized pancreas transplant recipients, a group at high risk of rejection and graft loss. Much of the published evidence that guided the development of current pancreas transplant immunosuppression regimens is either conflicting, based on non-randomized patients, or otherwise of marginal quality. Further research is therefore vitally necessary to better delineate the ideal immunosuppression regimen for pancreas transplant recipients.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Kandaswamy R, Skeans MA, Gustafson SK, et al. Pancreas. Am J Transplant. 2016;16 Suppl 2:47–68. This latest report from the Scientific Registry of Transplant Recipients captures many of the important trends in changing immunosuppression management for pancreas transplants over the past decade.
Gruessner AC. 2011 update on pancreas transplantation: comprehensive trend analysis of 25,000 cases followed up over the course of twenty-four years at the International Pancreas Transplant Registry (IPTR). Rev Diabet Stud. 2011;8:6–16.
Israni AK, Skeans MA, Gustafson SK, et al. OPTN/SRTR 2012 Annual Data Report: pancreas. Am J Transplant. 2014;14 Suppl 1:45–68.
Niederhaus SV, Kaufman DB, Odorico JS. Induction therapy in pancreas transplantation. Transpl Int. 2013;26:704–14.
Stratta RJ, Alloway RR, Hodge E, et al. A multicenter, open-label, comparative trial of two daclizumab dosing strategies vs. no antibody induction in combination with tacrolimus, mycophenolate mofetil, and steroids for the prevention of acute rejection in simultaneous kidney-pancreas transplant recipients: interim analysis. Clin Transplant. 2002;16:60–8.
Stratta RJ, Alloway RR, Lo A, et al. A prospective, randomized, multicenter study evaluating the safety and efficacy of two dosing regimens of daclizumab compared to no antibody induction in simultaneous kidney-pancreas transplantation: results at 3 years. Transplant Proc. 2005;37:3531–4.
Kaufman DB, Iii GW, Bruce DS, et al. Prospective, randomized, multi-center trial of antibody induction therapy in simultaneous pancreas-kidney transplantation. Am J Transplant. 2003;3:855–64.
Lo A, Stratta RJ, Alloway RR, et al. Initial clinical experience with interleukin-2 receptor antagonist induction in combination with tacrolimus, mycophenolate mofetil and steroids in simultaneous kidney-pancreas transplantation. Transpl Int. 2001;14:396–404.
Desai DM, Scandling JD, Knoppel C, et al. Low-dose OKT3 treatment for rejection/induction in kidney and kidney-pancreas transplantation. Transplant Proc. 1998;30:1552–4.
Cantarovich D, Karam G, Giral-Classe M, et al. Randomized comparison of triple therapy and antithymocyte globulin induction treatment after simultaneous pancreas-kidney transplantation. Kidney Int. 1998;54:1351–6.
Zachariah M, Gregg A, Schold J, et al. Alemtuzumab induction in simultaneous pancreas and kidney transplantation. Clin Transplant. 2013;27:693–700. This analysis of registry data of simultaneous pancreas-kidney transplant recipients shows no benefit in graft survival or overall patient survival in recipients treated with basiliximab, alemtuzumab or thymoglobulin induction compared to recipients receiving no induction.
Bazerbachi F, Selzner M, Boehnert MU, et al. Thymoglobulin versus basiliximab induction therapy for simultaneous kidney-pancreas transplantation: impact on rejection, graft function, and long-term outcome. Transplantation. 2011;92:1039–43.
Magliocca JF, Odorico JS, Pirsch JD, et al. A comparison of alemtuzumab with basiliximab induction in simultaneous pancreas-kidney transplantation. Am J Transplant. 2008;8:1702–10.
Pascual J, Pirsch JD, Odorico JS, et al. Alemtuzumab induction and antibody-mediated kidney rejection after simultaneous pancreas-kidney transplantation. Transplantation. 2009;87:125–32.
Stratta RJ, Rogers J, Orlando G, et al. Depleting antibody induction in simultaneous pancreas-kidney transplantation: a prospective single-center comparison of alemtuzumab versus rabbit anti-thymocyte globulin. Expert Opin Biol Ther. 2014;14:1723–30. In this prospective randomized trial, recipients of simultaneous pancreas-kidney transplants received either alemtuzumab or thymoglobulin induction immunosuppression. There were no significant differences in 5 year patient, pancreatic graft or renal graft survival, although there was a trend for improved acute rejection and lower rates of major infection with alemtuzumab.
Farney A, Sundberg A, Moore P, et al. A randomized trial of alemtuzumab vs. anti-thymocyte globulin induction in renal and pancreas transplantation. Clin Transplant. 2008;22:41–9.
Farney AC, Doares W, Rogers J, et al. A randomized trial of alemtuzumab versus antithymocyte globulin induction in renal and pancreas transplantation. Transplantation. 2009;88:810–9.
Bosmuller C, Ollinger R, Sieb M, et al. Tacrolimus monotherapy following alemtuzumab induction in combined kidney-pancreas transplantation: results of a prospective randomized trial. Ann Transplant. 2012;17:45–51.
Kaufman DB, Leventhal JR, Gallon LG, et al. Alemtuzumab induction and prednisone-free maintenance immunotherapy in simultaneous pancreas-kidney transplantation comparison with rabbit antithymocyte globulin induction—long-term results. Am J Transplant. 2006;6:331–9.
Vendrame F, Hopfner YY, Diamantopoulos S, et al. Risk factors for type 1 diabetes recurrence in immunosuppressed recipients of simultaneous pancreas-kidney transplants. Am J Transplant. 2015. Lack of induction immunosuppression was one of the risk factors associated with recurrent type 1 diabetes in recipients of simultaneous pancreas-kidney transplants.
Rangel EB. The metabolic and toxicological considerations for immunosuppressive drugs used during pancreas transplantation. Expert Opin Drug Metab Toxicol. 2012;8:1531–48.
Aoun M, Eschewege P, Hamoudi Y, et al. Very early steroid withdrawal in simultaneous pancreas-kidney transplants. Nephrol Dial Transplant. 2007;22:899–905.
Fridell JA, Agarwal A, Powelson JA, et al. Steroid withdrawal for pancreas after kidney transplantation in recipients on maintenance prednisone immunosuppression. Transplantation. 2006;82:389–92.
Jordan ML, Chakrabarti P, Luke P, et al. Results of pancreas transplantation after steroid withdrawal under tacrolimus immunosuppression. Transplantation. 2000;69:265–71.
Kahl A, Bechstein WO, Lorenz F, et al. Long-term prednisolone withdrawal after pancreas and kidney transplantation in patients treated with ATG, tacrolimus, and mycophenolate mofetil. Transplant Proc. 2001;33:1694–5.
Knight RJ, Kerman RH, McKissick E, et al. A pilot study of immunosuppression minimization after pancreas-kidney transplantation utilizing thymoglobulin induction and sirolimus maintenance therapy. Transplant Proc. 2005;37:3538–41.
Knight RJ, Podder H, Kerman RH, et al. Comparing an early corticosteroid/late calcineurin-free immunosuppression protocol to a sirolimus-, cyclosporine A-, and prednisone-based regimen for pancreas-kidney transplantation. Transplantation. 2010;89:727–32.
Luzi L, Picena Sereni L, Battezzati A, et al. Metabolic effects of a corticosteroid-free immunosuppressive regimen in recipients of pancreatic transplant. Transplantation. 2003;75:2018–23.
Malheiro J, Martins L, Fonseca I, et al. Steroid withdrawal in simultaneous pancreas-kidney transplantation: a 7-year report. Transplant Proc. 2009;41:909–12.
Rajab A, Pelletier RP, Ferguson RM, et al. Steroid-free maintenance immunosuppression with rapamune and low-dose neoral in pancreas transplant recipients. Transplantation. 2007;84:1131–7.
Reddy KS, Devarapalli Y, Mazur M, et al. Alemtuzumab with rapid steroid taper in simultaneous kidney and pancreas transplantation: comparison to induction with antithymocyte globulin. Transplant Proc. 2010;42:2006–8.
Sundberg AK, Roskopf JA, Hartmann EL, et al. Pilot study of rapid steroid elimination with alemtuzumab induction therapy in kidney and pancreas transplantation. Transplant Proc. 2005;37:1294–6.
Tanchanco R, Krishnamurthi V, Winans C, et al. Beneficial outcomes of a steroid-free regimen with thymoglobulin induction in pancreas-kidney transplantation. Transplant Proc. 2008;40:1551–4.
Uemura T, Ramprasad V, Matsushima K, et al. Single dose of alemtuzumab induction with steroid-free maintenance immunosuppression in pancreas transplantation. Transplantation. 2011;92:678–85.
Vessal G, Wiland AM, Philosophe B, et al. Early steroid withdrawal in solitary pancreas transplantation results in equivalent graft and patient survival compared with maintenance steroid therapy. Clin Transplant. 2007;21:491–7.
Amodu LI, Tiwari M, Levy A, et al. Steroid maintenance is associated with an increased risk of infections but has no effect on patient and graft survival in pancreas transplantation: A retrospective review of the UNOS database. Pancreatology. 2015;15:554–62. In this retrospective analysis of UNOS database data on pancreas and kidney-pancreas transplant recipients, the use of maintenance steroids increased the risk of infectious complications but did not decrease the rate of patient death or graft loss.
Montero N, Webster AC, Royuela A, et al. Steroid avoidance or withdrawal for pancreas and pancreas with kidney transplant recipients. Cochrane Database Syst Rev. 2014;9, CD007669. This Cochrane Database review found no compelling evidence in the literature to recommend use of steroids in pancreas transplant recipients.
Cantarovich D, Karam G, Hourmant M, et al. Steroid avoidance versus steroid withdrawal after simultaneous pancreas-kidney transplantation. Am J Transplant. 2005;5:1332–8.
Gruessner RW, Sutherland DE, Parr E, et al. A prospective, randomized, open-label study of steroid withdrawal in pancreas transplantation-a preliminary report with 6-month follow-up. Transplant Proc. 2001;33:1663–4.
Kandaswamy R, Khwaja K, Gruessner AC, et al. A prospective, randomized trial of steroid-free maintenance vs. delayed steroid withdrawal, using a sirolimus/tacrolimus regimen in simultaneous pancreas-kidney transplants (SPK) [abstract no: 1474]. Am J Transplant. 2003;3:1.
McAlister VC, Gao Z, Peltekian K, et al. Sirolimus-tacrolimus combination immunosuppression. Lancet. 2000;355:376–7.
Gallon LG, Winoto J, Chhabra D, et al. Long-term renal transplant function in recipient of simultaneous kidney and pancreas transplant maintained with two prednisone-free maintenance immunosuppressive combinations: tacrolimus/mycophenolate mofetil versus tacrolimus/sirolimus. Transplantation. 2007;83:1324–9.
Freise CE, Kang SM, Feng S, et al. Excellent short-term results with steroid-free maintenance immunosuppression in low-risk simultaneous pancreas-kidney transplantation. Arch Surg. 2003;138:1121–5. discussion 1125–1126.
Kaufman DB, Leventhal JR, Koffron AJ, et al. A prospective study of rapid corticosteroid elimination in simultaneous pancreas-kidney transplantation: comparison of two maintenance immunosuppression protocols: tacrolimus/mycophenolate mofetil versus tacrolimus/sirolimus. Transplantation. 2002;73:169–77.
di Francesco F, Cautero N, Vincenzi P, et al. One year follow-up of steroid-free immunosuppression plus everolimus in isolated pancreas transplantation. Transplantation. 2008;86:1146–7.
Rangel EB. Tacrolimus in pancreas transplant: a focus on toxicity, diabetogenic effect and drug-drug interactions. Expert Opin Drug Metab Toxicol. 2014;10:1585–605.
Laham G, Sleiman S, Soler Pujol G, et al. Conversion to sirolimus allows preservation of renal function in kidney and kidney-pancreas allograft recipients. Transplant Proc. 2010;42:309–13.
Gautam A, Morrissey PE, Gohh R, et al. Experience with sirolimus for calcineurin minimization/elimination in pancreas-after-kidney transplantation. Transplant Proc. 2005;37:3542–3.
Matias P, Araujo MR, Romao Jr JE, et al. Conversion to sirolimus in kidney-pancreas and pancreas transplantation. Transplant Proc. 2008;40:3601–5.
Girman P, Lipar K, Koznarova R, et al. Similar early complication rate in simultaneous pancreas and kidney recipients on tacrolimus/mycophenolate mofetil versus tacrolimus/sirolimus immunosuppressive regimens. Transplant Proc. 2010;42:1999–2002.
Kandula P, Fridell J, Taber TE, et al. Impact of tacrolimus-sirolimus maintenance immunosuppression on proteinuria and kidney function in pancreas transplant alone recipients. Transplantation. 2012;94:940–6.
Ciancio G, Sageshima J, Chen L, et al. Advantage of rapamycin over mycophenolate mofetil when used with tacrolimus for simultaneous pancreas kidney transplants: randomized, single-center trial at 10 years. Am J Transplant. 2012;12:3363–76.
Sageshima J, Ciancio G, Chen L, et al. Everolimus with low-dose tacrolimus in simultaneous pancreas and kidney transplantation. Clin Transplant. 2014;28:797–801. This non-randomized retrospective case series shows good outcomes can be obtained using combined maintenance everolimus and low-dose tacrolimus in a mycophenolate mofetil-sparing regimen.
Porubsky M, Gruessner AC, Rana A, et al. Excellent outcomes can be achieved in young pancreas transplant alone recipients by addition of sirolimus to maintenance immunosuppression regimen. Transplant Proc. 2014;46:1932–5.
Chatzizacharias NA, Vaidya A, Sinha S, et al. Risk analysis for deterioration of renal function after pancreas alone transplant. Clin Transplant. 2012;26:387–92.
Larsen CP, Pearson TC, Adams AB, et al. Rational development of LEA29Y (belatacept), a high-affinity variant of CTLA4-Ig with potent immunosuppressive properties. Am J Transplant. 2005;5:443–53.
Vincenti F, Charpentier B, Vanrenterghem Y, et al. A phase III study of belatacept-based immunosuppression regimens versus cyclosporine in renal transplant recipients (BENEFIT study). Am J Transplant. 2010;10:535–46.
Mujtaba MA, Sharfuddin AA, Taber T, et al. Conversion from tacrolimus to belatacept to prevent the progression of chronic kidney disease in pancreas transplantation: case report of two patients. Am J Transplant. 2014;14:2657–61. The successful conversion of a kidney-pancreas transplant recipient suffering calcineurin inhibitor-toxicity to a tacrolimus-sparing immunosuppression regimen based on belatacept is described.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pancreas Transplantation
Rights and permissions
About this article
Cite this article
Kitchens, W.H., Turgeon, N.A. Immunosuppression in Pancreas Transplantation: What Has Changed in 20 Years?. Curr Transpl Rep 3, 154–160 (2016). https://doi.org/10.1007/s40472-016-0098-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40472-016-0098-5