Abstract
Purpose of Review
Preterm birth is a significant worldwide health problem of uncertain origins. The extant body of literature examining environmental contaminant exposures in relation to preterm birth is extensive but results remain ambiguous for most organic pollutants, metals and metalloids, and air pollutants. In the present review, we examine recent epidemiologic studies investigating these associations and identify advances and the state of the science. Additionally, we highlight biological mechanisms of action in the pathway between chemical exposures and preterm birth, including inflammation, oxidative stress, and endocrine disruption, that deserve more attention in this context.
Recent Findings
Important advances have been made in the study of the environment and preterm birth, particularly in regard to exposure assessment methods, exploration of effect modification by co-morbidities and exposures, and in identification of windows of vulnerability during gestation. There is strong evidence for an association between maternal exposure to some persistent pesticides, lead, and fine particulate matter, but data on other contaminants is sparse and only suggestive trends can be noted.
Summary
Beyond replicating current findings, further work must be done to improve understanding of mechanisms underlying the associations observed between environmental chemical exposures and preterm birth. By examining windows of vulnerability, disaggregating preterm birth by phenotypes, and measuring biomarkers of mechanistic pathways in these epidemiologic studies, we can improve our ability to detect associations with exposure, provide additional evidence for causality in an observational setting, and identify opportunities for intervention.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Preterm birth (PTB) is an extensively studied perinatal outcome due to its prevalence, high societal costs, and poorly understood origins. Defined as delivery prior to 37 weeks gestation, PTB occurs in approximately 1 in 10 pregnancies worldwide and is one of the strongest predictors of neonatal mortality and morbidity [1]. Furthermore, PTB may mediate numerous later life adverse health outcomes, such as neurodevelopmental delays, asthma and allergy, and metabolic disease. There are known predictors, presentations, and hypothesized mechanisms of PTB, but knowledge of concrete causes remains minimal. The prevalence, costliness, and ambiguity surrounding this disease have led to scientific curiosity in the potential contribution of environmental chemical factors.
Exposures to organic pollutants, metals and metalloids, and air pollutants have the potential to increase risk of PTB through multiple pathways. Some of the most important mechanisms of action that have been investigated include inflammation, oxidative stress, and endocrine disruption, and each of these in turn has been linked to PTB. A large body of literature is devoted to this research [2,3,4], and, importantly, there have been recent efforts to identify the relevant biological mechanisms underlying these relationships in epidemiologic studies. By measuring biomarkers of mechanism, assessing windows of vulnerability to exposure, and examining associations with PTB phenotypes, research on environmental chemicals and PTB has advanced significantly.
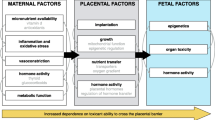
The intention of this review is first to describe inflammation, oxidative stress, and endocrine disruption as three potential pathways of chemical action in the pathway to PTB (Fig. 1) and to highlight recent studies that have advanced understanding of these mechanisms within the context of pregnancy (Table 1). Next, we present the state of the epidemiologic evidence examining the relationship between organic pollutants, metals and metalloids, and air pollutants. We review recent studies and discuss the major findings that support or refute an association with PTB and that point toward mechanisms.
Potential mechanisms of environmental chemical action in the path to preterm birth. Under ‘Consequences of disruption’, dashed borders represent biological changes that may be sensitive to exposures early in pregnancy, while solid borders reflect middle to late pregnancy windows of susceptibility. PPARs peroxisome proliferator-activated receptors; ROS reactive oxygen species; PPROM preterm premature rupture of the membranes; IUGR intrauterine growth restriction
Mechanisms of Chemical Action in the Etiology of PTB
While rodent studies can be helpful for understanding biological processes that may be related to PTB, they offer an insufficient model, as it is very difficult to cause them to deliver preterm [5, 6]. Thus, epidemiologic studies are especially valuable for studying this health outcome. This is true for studying associations with chemical exposures and for elucidating mechanisms. Beyond the utility of this model, studies of environmental chemicals and PTB that additionally investigate mechanisms can provide stronger arguments for causation in the observational setting, identify opportunities for interventions when remediating exposure is difficult or impossible, and improve the understanding of chemical toxicities in humans that may be extended to other disease. Here, we examine three potential mechanistic pathways that have received some attention in the study of environmental chemicals and PTB and deserve additional exploration in the future, including inflammation, oxidative stress, and endocrine disruption (Fig. 1). Additionally, we highlight consequences of these disrupted processes in pregnancy, potentially sensitive windows of vulnerability to exposure, and phenotypic presentations of PTB that would be expected to be more strongly associated with each pathway (e.g., spontaneous preterm labor, preterm premature rupture of the membranes [PPROM], preeclampsia, and intrauterine growth restriction [IUGR]).
Inflammation
Intrauterine bacterial infection is perhaps the best established cause of PTB [7]. Inflammatory pathways are thus one of the most well-studied mechanisms in the preterm pathway. Environmental contaminants have the potential to generate circulating or tissue-specific inflammation in several ways. First, particulate matter (metallic, endotoxin, or otherwise) may be engulfed by phagocytosis and lead to activation of T helper cells and release of cytokines [8]. Second, xenobiotic binding to certain receptors, such as peroxisome proliferator-activated receptors, can influence cytokine production as in the example of phthalate monoesters [9, 10]. Third, environmental chemicals have demonstrated capacity to cause epigenetic modification by way of DNA methylation, histone modifications, and/or perturbations in miRNA expression which can lead to changes in inflammatory responses [11]. Finally, these exposures can have adjuvant effects, exemplified by phthalates [12], which can increase the inflammation response to other stimuli.
While in many cases the exact cellular processes by which chemicals create inflammation are unknown, many exposures have been associated with inflammation in epidemiologic studies [13,14,15]. Changes in the systemic maternal or the intrauterine inflammatory milieu could have downstream consequences that precipitate PTB, e.g., by initiating a cascade of events leading to cervical ripening, rupture of the amniotic sac, or increased myometrial contractility [16]. These changes—sensitive to exposures later in pregnancy—may all precipitate spontaneous PTB either by initiating preterm labor or by causing PPROM.
Oxidative Stress
Oxidative stress, which can cause or be the consequence of increased inflammation, is another important mechanism that could link environmental chemical exposures to PTB. Many chemicals have the capacity to induce oxidative stress, either through: overproduction of reactive oxygen species (ROS) generated enzymatically (e.g., through upregulation of cytochrome P450 pathways) or non-enzymatically (e.g., through the Fenton reaction) [17, 18]; changes in mitochondrial membrane potential and permeability [19,20,21]; and impaired antioxidant function [22, 23]. Disturbance of the delicate balance between ROS and antioxidant defenses can have numerous downstream consequences in pregnancy. Early in gestation, oxidative stress can cause impaired invasion of the spiral arterioles into the maternal myometrium, resulting in poor placentation that can lead to preeclampsia or IUGR [24]. Elevated levels later in pregnancy could activate the maternal endothelium, part of a two-stage hypothesis underlying the onset of preeclampsia [25]; cause damage to the membranes resulting in premature rupture [26, 27]; create signaling changes in the cervix leading to shortening and spontaneous labor [28, 29]; and/or impact placental protein synthesis and nutrient transport that again lead to fetal growth restriction which can result in medically indicated PTB [30, 31].
Endocrine Disruption
Hormones carefully regulate nutrient transfer in pregnancy essential for growth of the fetus as well as timing of parturition. Disrupted fetal and placental thyroid hormone signaling has been observed in cases of IUGR [32]. Additionally, animal studies show that glucocorticoid administration during pregnancy leads to a clear dose-dependent decrease in size of the fetus [30], and similar associations have been observed in human populations [33]. Thus, thyroid and glucocorticoid hormones (e.g., cortisol) may be involved in the pathway to PTB with presentation of IUGR. Many chemicals have been linked to thyroid hormone disruption, potentially through receptor activity, particularly polychlorinated biphenyls (PCBs) and perfluorinated compounds [34, 35]. Additionally, extensive in vitro and animal evidence demonstrates that environmental contaminants have the potential to interfere with glucocorticoid signaling. For example, bisphenol A (BPA) and other phenols, phthalates, perfluorinated compounds, and some pesticides can interfere with the metabolism of glucocorticoids, thus raising circulating levels [37, 26]. Hormonal activity, and particularly that of the hypothalamic pituitary adrenal (HPA) axis, is additionally important in the timing of delivery. Corticotropin-releasing hormone (CRH) in the placenta has been hypothesized as crucial for timing of spontaneous parturition [38, 39]. Progesterone, estrogen, and cortisol pathways in the mother and fetus that interact to maintain homeostasis of CRH in pregnancy may thus be sensitive targets of chemical exposure [40].
Lastly, it is important to recognize that these pathways do not operate independently. Inflammation is tightly tied to hormonal regulation in pregnancy [16], and oxidative stress and inflammation have the potential to induce one another. These mechanisms may explain in part some of the associations observed in the following sections.
Environmental Chemicals and PTB
Organic Pollutants
Water Disinfection Byproducts (DBP)
A common method to disinfect drinking water is through the process of chlorination [41, 42]. The most abundant byproducts of this process are trihalomethanes (THMs) and exposure to these along with haloacetic acids (HAAs) has been studied in relation to PTB [43]. Grellier and colleagues reviewed the literature on exposure to water DBP and PTB in 2010 and concluded no association [44].
Since 2010, there have been seven additional studies [45,46,47,48,49,50,51]. Three, conducted in Europe, used a method of exposure assessment that incorporated both measurements of THMs from public drinking water sources and individual level information on personal routes of exposure including ingestion, inhalation, and dermal absorption [45,46,47,48]. The study by Costet and colleagues was novel in that exposure was quantified from a biomarker of trichloroacetic acid measured in maternal urine [45]. None of these studies found an association between total THM and PTB.
The remaining three studies were US based and found small positive associations with water DBP and PTB [49,50,51]. In New York, total THM were measured from the public water source at multiple time points during pregnancy [49]. Although exposure was determined from public water source measures, this study was able to link the source with maternal residence, lending more confidence to the level of exposure being assigned to each woman. A modest association was detected between low levels of total THMs and PTB, but a null association was observed at higher levels. The remaining two studies did incorporate an individual component and used a representative water source to assign exposure, but also found similar small positive associations with some of the water DBP [51].
Persistent Organic Pollutants
Most of the literature examining an association between organic pollutants and PTB has focused on chemicals that persist in the environment and human body. Evidence of a relationship between persistent pesticides and PTB comes from studies of populations with high levels of exposure [52, 53]. A subset of studies from a recent review of environmental chemicals and PTB [54] were published since 2010 and show that overall, the literature supports an association between high levels of organochlorine pesticide exposure [55,56,57] and PTB with weaker or null associations for the remaining persistent pollutants [54, 58,59,60,61,62,63,64,65].
Studies published since that review [54] show consistent findings of the association between persistent pesticides and PTB with high exposures associated with increased risk, whereas the relationship with lower exposures is less clear. In a study conducted in Guadeloupe where there is widespread chlordecone use and environmental contamination, authors found an association with exposure as measured by maternal blood sample at delivery and increased risk of PTB [66]. However, a study conducted in Spain, where pesticide exposure was much lower, failed to show an association between first trimester maternal hexachlorobenzene levels and PTB [67].
Exposure to high levels of non-pesticide persistent pollutants does not show the same relationship, with generally null findings for dioxin exposure and PTB regardless of exposure burden. A chemical explosion in Seveso, Italy, led to unprecedented residential dioxin exposure providing the opportunity to investigate the health effects of high levels of this chemical [68]. Despite exposure to elevated levels of dioxin, an association with PTB could not be established in this cohort [68]. Similarly, in a population highly exposed to perfluorooctanoic acid as a result of industrial contamination of the drinking water, no association with PTB was found [69]. In contrast, a study of flame retardants showed a dose-response relationship with PTB [70]. Maternal blood samples were taken at the time of delivery and an increased risk of PTB was observed with increasing levels of polybrominated diphenyl ethers.
Non-persistent Organic Pollutants
Investigation of organophosphate pesticides in relation to PTB has been limited and no associations with PTB have been reported [71, 72]. Atrazine, another chemical used in agriculture, is applied as an herbicide, and can contaminate water supplies [73]. Early studies looking at atrazine assigned exposure based on measurements from water sources and found null or weak non-significant positive associations with PTB [74, 75]. Recent studies continue to use drinking water levels to assign atrazine exposure despite the ability to measure individual exposure from urine samples [76], and the evidence for atrazine being associated with increased PTB remains inconclusive [77].
Phthalates are used to increase flexibility in plastics and are also found in many personal care products. Human exposure to this group of chemicals is widespread through ingestion, dermal application, and inhalation [78]. There have been conflicting findings from early studies of phthalate metabolites and PTB with one study finding a protective association [79] and another finding a harmful one [80]. Since publication of these findings, there have been improvements in the assessment of phthalate exposures. In a recent nested case control study, multiple measures of nine phthalate metabolites were used to estimate exposure. In this study, the average phthalate metabolite levels from three urine samples collected from women during pregnancy (median of 10, 18, and 26 weeks gestation) were associated with increased risk of PTB [81]. Further, this study examined phenotypes of PTB and observed an even stronger association between phthalate levels and spontaneous PTB. A related study characterized the variability of phthalate metabolite levels across pregnancy [82]. In this study, each urinary phthalate measurement was treated as a distinct exposure to assess risk of PTB in relation to different windows of susceptibility during pregnancy. Results showed the strongest association with phthalate levels measured later in pregnancy.
BPA is another chemical identified as an endocrine disrupter that is in widespread use as a component of hard plastics and epoxy resins [78]. The first study to examine the relationship between BPA exposure and PTB was done using a maternal single spot urine collected during the third trimester and found a modest association of BPA with PTB [84]. These same investigators then used multiple measures of BPA from the same case cohort study referenced above with phthalates and found a weak and non-significant association with PTB [85].
Strengths of literature on non-persistent pollutants include several improvements in exposure assessment. Examples include the incorporation of personal information on routes of exposure of water DBP and use of multiple measurements of non-persistent chemicals like phthalates and BPA. Additionally, consideration of the timing of exposure and windows of susceptibility that may differ based on preterm phenotype aids in comparability across studies and confirmation of proposed biologic mechanisms. Limitations of the current evidence on organic pollutants and PTB include the continued use of ecological measures of exposure even when validated biomarkers exist that could quantify individual exposure. In some studies, individual-level exposure was measured, but using inappropriate exposure matrices, specifically regarding non-persistent chemicals, results in concerns about contamination [83, 86, 87]. Lastly, the consideration of combinations of related chemicals or metabolites with PTB would strengthen the literature.
Metals and Metalloids
Over the past several decades, there have been many studies that have examined the association between heavy metal exposures and adverse birth outcomes. The bulk of the early literature focused on high levels of exposure [88,89,90] with more recent studies examining lower levels consistent with non-occupational settings.
Lead
There is convincing evidence that lead exposure in high levels is associated with PTB [88]. The hypothesized mechanisms by which lead can lead to PTB fall into two categories: (1) by influencing hormone levels [91,92,93,94] and (2) inducing the production of reactive oxygen species [92, 93]. Since the elimination of lead in everyday exposures like fuel and paint, examination of lower levels of lead exposure has become more relevant [95]. Studies focused on these ambient levels of exposure that still persistent in the environment have shown inconsistent results possibly as the result of differences the timing of exposure assessment or type of biologic material utilized [96, 97]. In a study conducted in Mexico, exposure to lead was assessed during the first, second, and third trimester in maternal whole blood and plasma and the strongest associations with PTB were seen in early pregnancy [91]. Other studies with measures of lead during early pregnancy showed similar results [92, 93]. Results from studies assessing lead exposure across pregnancy show less consistent results, with the possibility of lead measurements later in pregnancy attenuating the effect [98, 99]. Two studies found differences in PTB by sex of the infant, but results were opposing with one finding a stronger association in girls and the other in boys [94, 98].
Mercury
The association between mercury exposure and PTB has been mixed. A study by Taylor and colleagues conducted in the UK found weak evidence of a protective effect of blood mercury levels measured in the mother early in pregnancy (median 11 weeks) and PTB, but this association attenuated in adjusted models [100]. In a study population of women who were predominantly African-American or of Caribbean decent, investigators found a protective effect of higher mercury levels in maternal urine during the last trimester of pregnancy, but the estimate was imprecise [101]. A slightly stronger effect was seen in cord blood measures in the same population.
Arsenic
Two of the studies reviewed looked at arsenic in drinking water and PTB. Neither used individual levels of exposure but were consistent with prior work that has found null or weak associations with PTB [102].
Cadmium
Early studies examining maternal cadmium exposure and PTB used either an ecological study design or suffered from small sample size and showed mixed results [103,104,105]. More recently, two large cohort studies conducted in China showed an association between higher levels of cadmium exposure and increased risk of PTB [106, 107]. A case cohort study of the more restrictive outcomes of preterm low birth weight also reported this association [108]. Cadmium is thought to alter zinc transport, which may trigger PTB [106, 107] and may also accumulate in the placenta where it can directly or indirectly affect the fetus [108]. None of the studies that reviewed mercury or arsenic proposed a hypothesized mechanism of action.
Strengths of the current literature include taking the timing of the metal exposure into account and examining lower levels of metal exposures that are more consistent with ambient exposure. Some studies measure metal exposures in more than one type of biological sample to estimate how correlated measures are across sample type, which may have implications on the interpretation of results from future studies as well as determining the best exposure matrix for each metal.
There are still many studies that use ecological data to estimate exposure to metals and metalloids, even when individual measures have been shown to be reliable, such as arsenic exposure measured in urine samples. Although some studies consider the timing of exposures, there are many studies that continue to compare measures taken from women at different times during pregnancy or only at delivery, which may not reflect exposure during pregnancy. This may be especially important for lead exposure which is thought to have a U-shaped curve during pregnancy with higher levels seen in the first and third trimester [109].
Air Pollutants
Criteria Air Pollutants
Papers published on air pollutants, including nitrogen dioxide (NO2), sulfur dioxide (SO2), ozone (O3), carbon monoxide (CO), and particulate matter (<2.5 μm, PM2.5 and <10um, PM10) up until January 2011 were meticulously examined by Stieb and colleagues [110]. Their pooled analysis using trimester-specific as well as entire pregnancy averages concluded that the most precise effect estimates were between third trimester exposures to CO and PM10 and PTB [110]. Since that time, many studies have been published on criteria air pollutants with notable improvements. Exposure assessment has been optimized by more broad application of land use regression modeling [111,112,113], implementation of satellite-imaging technology for the assessment of PM2.5 exposure [114,115,116], and in studies of PM2.5 exposure, examination of the individual components within the particulate fraction in attempt to identify the most harmful constituents [117,118,119,120].The study of windows of vulnerability to exposure has expanded as well, with many studies moving beyond examining trimester or month of exposure into measurement of the preconception exposures [121] or exposures in the days or hours immediately proximate to delivery [122,123,124]. In terms of outcome assessment, some research groups have made efforts to examine phenotypes of PTB. Potentially due to ease of assessment from medical record abstraction, the focus has been on PPROM [111, 125,126,127]. Finally, many recent studies place an emphasis on understanding effect modifiers in these relationships. These have included co-morbidities such as asthma and diabetes [117, 121, 128]; demographic factors like race, education level, and socioeconomic status [120, 123]; and community-level variables, e.g., urbanicity [129].
Regarding individual criteria air pollutants, the greatest advances and the largest number of studies have focused on fine particulate matter (PM2.5). Since the review by Stieb et al., four additional reviews and meta-analyses have summarized the literature on these associations and all concluded that a positive association exists between exposure during pregnancy and PTB [130,131,132,133]. The majority of papers published since that review also suggest a positive association between PM2.5 exposure and PTB, although null and in some cases protective effects have been observed in well-designed studies [113, 114, 122, 134, 135]. Differences may be due to variation in study design and population, exposure assessment methods, measurement windows, and levels of exposure.
Studies examining variation in effects by characteristics of the study population have observed the greatest effect estimates in subjects with co-morbidities like asthma and diabetes [116, 121] and who have certain demographic characteristics (low education level, non-African-American, residing in large metropolitan areas) [120]. Width of windows of exposure varies greatly as well. Detection of positive associations between PM2.5 and PTB seems to suggest that exposure in the days or hours leading up to delivery may be most relevant [123, 124, 127, 136], although this has not been evident in all studies that had the capability of assessing this window specifically [122]. Exposure assessment approaches improve dramatically year to year as well, and for this exposure, two recent studies have captured exposure with satellite-based predictions, which have the ability to assign exposure to small geographic areas and more accurately capture exposures where ambient air monitors are more sparse (i.e., rural areas) [114, 115]. These studies had conflicting findings; however, as these methods improve they may provide more robust data on the association between PM2.5 and PTB.
Studies of PM2.5 also vary by exposure level, source, and composition of the particulate. In a study by the World Health Organization comparing associations in African, Asian, and Latin American countries, the only clear evidence of an association between PM2.5 and PTB was observed in China, where the range of exposure was widest and where some of the highest levels in the world were observed [137]. Though, this does not necessarily connote a stronger effect at higher levels. An analysis, examining non-linear associations with exposure in attempt to identify a threshold effect observed no statistical association for PM2.5 in linear or non-linear single-pollutant models [122]. Finally, an important evolution in this research is to examine sources and components of fractionated PM2.5. One study identified power plants as important sources of PM2.5 exposure and illustrated that proximity to these plants specifically was associated with increased risk of preterm delivery [138]. Additionally, two studies examining compounds present in PM2.5 fractions suggested that elemental carbon and SO4 specifically were associated with increased risk of PTB [111, 119]. Additional research studies designed to capture these elements combined will help improve the understanding of the role of exposure to PM2.5 in the etiology of PTB.
Associations with PM10 specifically are difficult to assess because not all studies examine both PM10 and PM2.5 fractions separately, thus many studies measuring PM10 alone may be capturing effects of the smaller particulate fraction. Previously, Stieb et al. concluded that there was an association between PM10 and PTB, but more recent studies are ambiguous. Of the studies that do report an association with PM10, only one measured PM2.5 concurrently [123] and noted that the strongest associations were with exposure very close to the time of delivery. Notably, two studies examined these associations within natural experiments. Balsa and colleagues examined pregnancy outcomes among individuals residing near an active volcano and observed strong associations with PM10 levels measured in the third trimester [139]. On the other hand, however, a study of elevated air pollution levels occurring during the Beijing Olympic games observed no association between ambient PM10 concentrations and PTB [140].
Studies of other criteria air pollutants are less conclusive, despite having made similar advancements by way of examining more specific exposure windows, non-linearity of associations, and multi-pollutant models. In regard to NO2, positive [111, 116, 117, 120, 122, 123, 129, 141,142,143,144,145] and null [112, 113, 127, 128, 135, 137, 140, 146,147,148,149,150,151,152,153,154] associations seem to be evenly mixed. Studies that have observed positive associations point toward the second trimester or the time period immediately preceding delivery as sensitive windows of exposure [122, 129, 143]. Also, evidence suggests that an association may exist only in urban populations or at a certain threshold of exposure [122, 129]. Additionally, one study showed that an association was between NO2 and PTB in a single-pollutant model, but when PM2.5 was added to the model, the association between PTB and NO2 became null [117]. Findings for O3, CO, and SO2 also remain inconclusive.
Polycyclic Aromatic Hydrocarbons and Volatile Organic Compounds
Fewer studies examine polycyclic aromatic hydrocarbons (PAHs) or volatile organic compounds (VOCs) because they are not as tightly regulated by the EPA and hence are not commonly captured by air monitors. PAHs are released during combustion processes from vehicles and industrial facilities, and they are also found in tobacco smoke and grilled meats and vegetables [155]. Thus, exposure occurs commonly through inhalation pathways but ambient monitors likely capture a smaller percentage of exposure compared to other air pollutants. Studies examining ambient PAH exposure in relation to PTB have identified significant associations between total PAHs as well as individual congeners, particularly with levels measured in the end of gestation [156, 157]. Additionally, a study measuring PAH concentrations in cord blood identified higher levels in pregnancies with adverse birth outcomes, including PTB [158]. While this research is suggestive, additional studies are necessary and would benefit from utilizing urinary biomarkers which capture total exposure through inhalation and ingestion pathways. Similarly, exposure to some VOCs in pregnancy, e.g., benzene or toluene, shows some evidence of an association with PTB but the data remains very limited [143, 151, 159,160,161].
Environmental Tobacco Smoke
Lastly, environmental tobacco smoke has been examined in several studies in relation to PTB. The association between PTB and maternal smoking has been established [162]; however, the risk associated with indirect exposure is less clear. A meta-analysis published in 2010 showed a slight positive association with PTB that was not statistically significant in adjusted models [163]. A more recent meta-analysis concluded otherwise, specifying that passive smoking in either the workplace or at home was associated with preterm delivery [164]. Of the largest of these studies published in recent years (>10,000 subjects), two report positive associations with PTB, particularly delivery <32 weeks gestation [165, 166] and one had null findings [167].
In 2008, Slama et al. addressed the overarching limitations of studies examining air pollutant exposures in relation to PTB and identified major research needs [168]. Many of these needs remain, including the need to better understand mechanisms underlying these observed associations, addressing co-exposure to multiple pollutants, and working from a unified methodological framework to improve comparability between studies [169]. Toward this end, Pereira and colleagues are implementing a series of studies with the same design to assess the relationship between gestational exposures to PM2.5 and PTB in different regions of the world [125, 126, 170]. The International Collaboration on Air Pollution and Pregnancy Outcomes is designed with the same aim, to unify methodologies across research studies to identify the relationship between ambient air pollutant exposures and adverse pregnancy outcomes [171]. These collaborative research efforts will be extremely informative in the coming years.
Conclusions
Although numerous studies have been published on the relationship between environmental chemical exposures and PTB, few individual compounds have sufficient evidence to conclude an association. The data suggest a strong association between PTB and fine particulate matter (PM2.5), lead, and dichlorodiphenyltrichloroethane (DDT) exposures in pregnancy—compounds for which there have also been the largest number of publications. However, for other chemicals, the overall findings are ambiguous. This is due both to small numbers of studies for some compounds as well as conflicting results. Future work on other compounds where there is strong evidence but not enough data—e.g., polycyclic aromatic hydrocarbons—is warranted.
Of the studies reviewed, many of the common limitations of environmental epidemiology studies exist. These include limited exposure assessment metrics (e.g., using a spot urine sample to assess non-persistent chemical exposures), small sample sizes and/or small numbers of cases, and failure to account for key confounders and/or co-exposures. We posit that although there has been some concerted effort in this direction, an additional limitation to this literature is the infrequent attention to mechanistic pathways underlying the relationships of interest. It would behoove future studies to focus on disentangling these mechanisms through one or more approaches. First, by examining windows of vulnerability during gestation, investigators can examine time points of exposure that may be reflective of specific pathways to delivery. The greatest progress in this arena has been made in the study of particulate matter, where investigators have leveraged the wealth of information available from ambient air monitors to examine acute exposures (i.e., the hours or days leading up to delivery) in relation to PTB [123, 124, 127, 136]. Identifying this sensitive window of exposure provides stronger evidence of a relationship between PM2.5 and PTB by highlighting a biologically plausible pathway (e.g., acute PM2.5 exposure causes oxidative stress or inflammation, which leads to membrane damage and PPROM). A second approach to identifying mechanism may be through examining associations with specific presentations of PTB, as opposed to looking at the 37-week cutoff alone, or at other cutoffs based on gestational age that may not necessarily be homogenous by mechanism. Again, progress has been made here in the realm of air pollution research by groups who have focused their efforts on examining associations with PPROM [125,126,127] and also to some extent, in the study of non-persistent organic pollutants such as BPA and phthalates [172, 173•]. Examining associations with phenotypes of PTB based on presentation enables both greater ability to detect effects and also identifies mechanisms that may be targeted for interventions. Finally, and most ideally, biomarkers of mechanistic intermediates can be measured concurrently with exposure to provide supportive evidence of causality if indeed an association with exposure exists.
Worth mentioning is the study published by Ferguson, McElrath, and Meeker in which mechanism is investigated under all three of these approaches [174]. In that study, phthalate exposure biomarkers were measured at four time points during pregnancy (windows of vulnerability); associations were examined with phenotypes of PTB (presentation phenotypes); and indices of mechanistic intermediates were measured under multiple hypothesized pathways, including inflammation, oxidative stress, and endocrine disruption (biomarkers of mechanism). In that study, the authors established an association between some phthalate metabolites and specifically spontaneous PTB, with associations that were greatest in magnitude with exposure measured late in pregnancy [172]. Additionally, they demonstrated that urinary phthalate metabolites were associated with oxidative stress biomarkers, particularly 8-isoprostane, and that 8-isoprostane concentrations during pregnancy were associated with spontaneous preterm delivery [175, 176]. Finally, the authors developed and applied novel mediation methods and showed that, statistically, oxidative stress, as indicated by 8-isoprostane, may account for upwards of 50% of the association between some phthalate metabolites and PTB [177••].
These additional steps beyond the analysis of association between exposure and outcome provide greater weight to the analysis and can provide feedback into the obstetrics community to further understanding of the complex pregnancy outcome that is PTB. Additional studies with this type of framework are necessary for establishing more concrete connections with environmental chemical exposures. By examining windows of vulnerability, presentation phenotypes, and biomarkers of mechanism, we may also reduce variability in published associations and have a greater chance at replicating study findings. This work will strengthen the evidence supporting associations between environmental chemical exposures and PTB and help us to identify opportunities for remediating exposures or implementing interventions to prevent this serious public health problem.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Behrman RE, Butler AS. Preterm birth: causes, consequences, and prevention. Institute of medicine (US) committee on understanding premature birth and assuring healthy outcomes. In: Behrman RE, Butler AS, editors. Washington (DC): National Academies Press (US); 2007.
Ferguson KK, O'Neill MS, Meeker JD. Environmental contaminant exposures and preterm birth: a comprehensive review. Journal of Toxicology and Environmental Health, Part B. 2013;16(2):69–113.
Wigle DT, Arbuckle TE, Turner MC, Berube A, Yang Q, Liu S, et al. Epidemiologic evidence of relationships between reproductive and child health outcomes and environmental chemical contaminants. Journal of Toxicology and Environmental Health, Part B. 2008;11(5–6):373–517.
Translational toxicology: defining a new therapeutic discipline. In: Hughes CL, Waters MD, editors. Springer international publishing. Switzerland; 2016.
Cha J, Bartos A, Egashira M, Haraguchi H, Saito-Fujita T, Leishman E, et al. Combinatory approaches prevent preterm birth profoundly exacerbated by gene-environment interactions. J Clin Invest. 2013;123(9):4063–75.
Kaga N, Katsuki Y, Obata M, Shibutani Y. Repeated administration of low-dose lipopolysaccharide induces preterm delivery in mice: a model for human preterm parturition and for assessment of the therapeutic ability of drugs against preterm delivery. Am J Obstet Gynecol. 1996;174(2):754–9.
Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371(9606):75–84.
Vadillo-Ortega F, Osornio-Vargas A, Buxton MA, Sánchez BN, Rojas-Bracho L, Viveros-Alcaráz M, et al. Air pollution, inflammation and preterm birth: a potential mechanistic link. Med Hypotheses. 2014;82(2):219–24.
Jiang C, Ting AT, Seed B. PPAR-γ agonists inhibit production of monocyte inflammatory cytokines. Nature. 1998;391(6662):82–6.
Peraza MA, Burdick AD, Marin HE, Gonzalez FJ, Peters JM. The toxicology of ligands for peroxisome proliferator-activated receptors (PPAR). Toxicol Sci. 2006;90(2):269–95.
Lin VW, Baccarelli AA, Burris HH. Epigenetics—a potential mediator between air pollution and preterm birth. Environmental epigenetics. 2016;2(1):dvv008.
Larsen ST, Hansen JS, Hansen EW, Clausen PA, Nielsen GD. Airway inflammation and adjuvant effect after repeated airborne exposures to di-(2-ethylhexyl) phthalate and ovalbumin in BALB/c mice. Toxicology. 2007;235(1):119–29.
Hajat A, Allison M, Diez-Roux AV, Jenny NS, Jorgensen NW, Szpiro AA, et al. Long-term exposure to air pollution and markers of inflammation, coagulation, and endothelial activation: a repeat-measures analysis in the multi-ethnic study of atherosclerosis (MESA). Epidemiology (Cambridge, Mass). 2015;26(3):310–20.
Kannan S, Misra DP, Dvonch JT, Krishnakumar A. Exposures to airborne particulate matter and adverse perinatal outcomes: a biologically plausible mechanistic framework for exploring potential. Ciencia & saude coletiva. 2007;12(6):1591–602.
Nachman R, Mao G, Zhang X, Hong X, Chen Z, Soria C, et al. Intrauterine inflammation and maternal exposure to ambient PM2. 5 during preconception and specific periods of pregnancy: The Boston Birth Cohort. Environ Health Perspect. 2016;124(10):1608–1615.
Challis JR, Lockwood CJ, Myatt L, Norman JE, Strauss JF, Petraglia F. Inflammation and pregnancy. Reprod Sci. 2009;16(2):206–15.
Stohs S, Bagchi D. Oxidative mechanisms in the toxicity of metal ions. Free Radic Biol Med. 1995;18(2):321–36.
Valavanidis A, Vlahogianni T, Dassenakis M, Scoullos M. Molecular biomarkers of oxidative stress in aquatic organisms in relation to toxic environmental pollutants. Ecotoxicol Environ Saf. 2006;64(2):178–89.
Chen X, Wang J, Qin Q, Jiang Y, Yang G, Rao K, et al. Mono-2-ethylhexyl phthalate induced loss of mitochondrial membrane potential and activation of Caspase3 in HepG2 cells. Environ Toxicol Pharmacol. 2012;33(3):421–30.
Rosado-Berrios CA, Vélez C, Zayas B. Mitochondrial permeability and toxicity of diethylhexyl and monoethylhexyl phthalates on TK6 human lymphoblasts cells. Toxicol in Vitro. 2011;25(8):2010–6.
Cadenas E, Davies KJ. Mitochondrial free radical generation, oxidative stress, and aging. Free Radic Biol Med. 2000;29(3):222–30.
López O, Hernández AF, Rodrigo L, Gil F, Pena G, Serrano JL, et al. Changes in antioxidant enzymes in humans with long-term exposure to pesticides. Toxicol Lett. 2007;171(3):146–53.
Ahamed M, Siddiqui M. Low level lead exposure and oxidative stress: current opinions. Clin Chim Acta. 2007;383(1):57–64.
Burton GJ, Jauniaux E. Placental oxidative stress: from miscarriage to preeclampsia. J Soc Gynecol Investig. 2004;11(6):342–52.
Roberts JM, Hubel CA. Is oxidative stress the link in the two-stage model of pre-eclampsia? Lancet. 1999;354(9181):788–9.
Longini M, Perrone S, Vezzosi P, Marzocchi B, Kenanidis A, Centini G, et al. Association between oxidative stress in pregnancy and preterm premature rupture of membranes. Clin Biochem. 2007;40(11):793–7.
Woods J. Reactive oxygen species and preterm premature rupture of membranes—a review. Placenta. 2001;22:S38–44.
Sanders AP, Burris HH, Just AC, Motta V, Svensson K, Mercado-Garcia A, et al. microRNA expression in the cervix during pregnancy is associated with length of gestation. Epigenetics. 2015;10(3):221–8.
Venkatesh K, Cantonwine D, Ferguson K, Arjona M, Meeker JD, McElrath TF. Inflammatory and oxidative stress markers associated with decreased cervical length in pregnancy. Am J Reprod Immunol. 2016;76(5):376–82.
Jones H, Powell T, Jansson T. Regulation of placental nutrient transport–a review. Placenta. 2007;28(8):763–74.
Burton G, Yung H-W, Cindrova-Davies T, Charnock-Jones D. Placental endoplasmic reticulum stress and oxidative stress in the pathophysiology of unexplained intrauterine growth restriction and early onset preeclampsia. Placenta. 2009;30:43–8.
Kilby M, Verhaeg J, Gittoes N, Somerset D, Clark P, Franklyn J. Circulating thyroid hormone concentrations and placental thyroid hormone receptor expression in normal human pregnancy and pregnancy complicated by intrauterine growth restriction (IUGR). The Journal of Clinical Endocrinology & Metabolism. 1998;83(8):2964–71.
Ali Khan A, Rodriguez A, Kaakinen M, Pouta A, Hartikainen AL, Jarvelin MR. Does in utero exposure to synthetic glucocorticoids influence birthweight, head circumference and birth length? A systematic review of current evidence in humans. Paediatr Perinat Epidemiol. 2011;25(1):20–36.
Boas M, Feldt-Rasmussen U, Main KM. Thyroid effects of endocrine disrupting chemicals. Mol Cell Endocrinol. 2012;355(2):240–8.
Steenland K, Fletcher T, Savitz DA. Epidemiologic evidence on the health effects of perfluorooctanoic acid (PFOA). Environ Health Perspect. 2010;1100-8
Sargis RM, Johnson DN, Choudhury RA, Brady MJ. Environmental endocrine disruptors promote adipogenesis in the 3 t3-l1 cell line through glucocorticoid receptor activation. Obesity. 2010;18(7):1283–8.
Ye L, Guo J, Ge R-S. Environmental pollutants and hydroxysteroid dehydrogenases. Vitam Horm. 2014;94:349–90.
McLean M, Bisits A, Davies J, Woods R, Lowry P, Smith R. A placental clock controlling the length of human pregnancy. Nat Med. 1995;1(5):460–3.
Wadhwa PD, Garite TJ, Porto M, Glynn L, Chicz-DeMet A, Dunkel-Schetter C, et al. Placental corticotropin-releasing hormone (CRH), spontaneous preterm birth, and fetal growth restriction: a prospective investigation. Am J Obstet Gynecol. 2004;191(4):1063–9.
Challis JR, Matthews SG, Gibb W, Lye SJ. Endocrine and paracrine regulation of birth at term and preterm 1. Endocr Rev. 2000;21(5):514–50.
Cutler D, Miller G. The role of public health improvements in health advances: the twentieth-century United States. Demography. 2005;42(1):1–22.
Wigle DT. Safe drinking water: a public health challenge. Chronic Dis Can. 1998;19(3):103–7.
Nieuwenhuijsen MJ, Toledano MB, Eaton NE, Fawell J, Elliott P. Chlorination disinfection byproducts in water and their association with adverse reproductive outcomes: a review. Occup Environ Med. 2000;57(2):73–85.
Grellier J, Bennett J, Patelarou E, Smith RB, Toledano MB, Rushton L, et al. Exposure to disinfection by-products, fetal growth, and prematurity: a systematic review and meta-analysis. Epidemiology. 2010;21(3):300–13.
Costet N, Garlantezec R, Monfort C, Rouget F, Gagniere B, Chevrier C, et al. Environmental and urinary markers of prenatal exposure to drinking water disinfection by-products, fetal growth, and duration of gestation in the PELAGIE birth cohort (Brittany, France, 2002-2006). Am J Epidemiol. 2012;175(4):263–75.
• Kogevinas M, Bustamante M, Gracia-Lavedan E, Ballester F, Cordier S, Costet N, et al. Drinking water disinfection by-products, genetic polymorphisms, and birth outcomes in a European mother-child cohort study. Epidemiology. 2016;27(6):903–11. Large, multi-country study investigating the association between water disinfection byproducts and preterm birth. Used individual level information on water consumption, water-related activities, and route of exposure
Patelarou E, Kargaki S, Stephanou EG, Nieuwenhuijsen M, Sourtzi P, Gracia E, et al. Exposure to brominated trihalomethanes in drinking water and reproductive outcomes. Occup Environ Med. 2011;68(6):438–45.
Villanueva CM, Gracia-Lavedan E, Ibarluzea J, Santa Marina L, Ballester F, Llop S, et al. Exposure to trihalomethanes through different water uses and birth weight, small for gestational age, and preterm delivery in Spain. Environ Health Perspect. 2011;119(12):1824–30.
Kumar S, Forand S, Babcock G, Richter W, Hart T, Hwang SA. Total trihalomethanes in public drinking water supply and birth outcomes: a cross-sectional study. Matern Child Health J. 2014;18(4):996–1006.
Rivera-Nunez Z, Wright JM. Association of brominated trihalomethane and haloacetic acid exposure with fetal growth and preterm delivery in Massachusetts. J Occup Environ Med. 2013;55(10):1125–34.
Horton BJ, Luben TJ, Herring AH, Savitz DA, Singer PC, Weinberg HS, et al. The effect of water disinfection by-products on pregnancy outcomes in two southeastern US communities. J Occup Environ Med. 2011;53(10):1172–8.
Berkowitz GS, Lapinski RH, Wolff MS. The role of DDE and polychlorinated biphenyl levels in preterm birth. Arch Environ Contam Toxicol. 1996;30(1):139–41.
Longnecker MP, Klebanoff MA, Zhou H, Brock JW. Association between maternal serum concentration of the DDT metabolite DDE and preterm and small-for-gestational-age babies at birth. Lancet. 2001;358(9276):110–4.
Ferguson KK, O'Neill MS, Meeker JD. Environmental contaminant exposures and preterm birth: a comprehensive review. J Toxicol Environ Health B Crit Rev. 2013;16(2):69–113.
Wojtyniak BJ, Rabczenko D, Jonsson BA, Zvezday V, Pedersen HS, Rylander L, et al. Association of maternal serum concentrations of 2,2', 4,4'5,5'-hexachlorobiphenyl (CB-153) and 1,1-dichloro-2,2-bis (p-chlorophenyl)-ethylene (p,p'-DDE) levels with birth weight, gestational age and preterm births in Inuit and European populations. Environ Health. 2010;9:56.
Bergonzi R, De Palma G, Specchia C, Dinolfo M, Tomasi C, Frusca T, et al. Persistent organochlorine compounds in fetal and maternal tissues: evaluation of their potential influence on several indicators of fetal growth and health. Sci Total Environ. 2011;409(15):2888–93.
Pathak R, Ahmed RS, Tripathi AK, Guleria K, Sharma CS, Makhijani SD, et al. Maternal and cord blood levels of organochlorine pesticides: association with preterm labor. Clin Biochem. 2009;42(7–8):746–9.
Arbuckle TE, Kubwabo C, Walker M, Davis K, Lalonde K, Kosarac I, et al. Umbilical cord blood levels of perfluoroalkyl acids and polybrominated flame retardants. Int J Hyg Environ Health. 2013;216(2):184–94.
Chen MH, Ha EH, Wen TW, Su YN, Lien GW, Chen CY, et al. Perfluorinated compounds in umbilical cord blood and adverse birth outcomes. PLoS One. 2012;7(8):e42474.
Hamm MP, Cherry NM, Chan E, Martin JW, Burstyn I. Maternal exposure to perfluorinated acids and fetal growth. J Expo Sci Environ Epidemiol. 2010;20(7):589–97.
• Savitz DA, Stein CR, Bartell SM, Elston B, Gong J, Shin HM, et al. Perfluorooctanoic acid exposure and pregnancy outcome in a highly exposed community. Epidemiology. 2012;23(3):386–92. Used modeling techniques to improve exposure assessment of perflourinated compounds in a highly exposed cohort. Incorporated data from individual serum levels, historical exposure, environmental factors, and industrial operations to quantify exposure levels of participants in the study
Savitz DA, Stein CR, Elston B, Wellenius GA, Bartell SM, Shin HM, et al. Relationship of perfluorooctanoic acid exposure to pregnancy outcome based on birth records in the mid-Ohio Valley. Environ Health Persp. 2012;120:1201–7.
Whitworth KW, Haug LS, Baird DD, Becher G, Hoppin JA, Skjaerven R, et al. Perfluorinated compounds in relation to birth weight in the Norwegian mother and child cohort study. Am J Epidemiol. 2012;175:1209–16.
Wu K, Xu X, Liu J, Guo Y, Li Y, Huo X. Polybrominated diphenyl ethers in umbilical cord blood and relevant factors in neonates from Guiyu. China Environ Sci Technol. 2010;44(2):813–9.
Wu K, Xu X, Peng L, Liu J, Guo Y, Huo X. Association between maternal exposure to perfluorooctanoic acid (PFOA) from electronic waste recycling and neonatal health outcomes. Environ Int. 2012;48:1–8.
Kadhel P, Monfort C, Costet N, Rouget F, Thome JP, Multigner L, et al. Chlordecone exposure, length of gestation, and risk of preterm birth. Am J Epidemiol. 2014;179(5):536–44.
Basterrechea M, Lertxundi A, Iniguez C, Mendez M, Murcia M, Mozo I, et al. Prenatal exposure to hexachlorobenzene (HCB) and reproductive effects in a multicentre birth cohort in Spain. Sci Total Environ. 2014;466-467:770–6.
• Wesselink A, Warner M, Samuels S, Parigi A, Brambilla P, Mocarelli P, et al. Maternal dioxin exposure and pregnancy outcomes over 30 years of follow-up in Seveso. Environ Int. 2014;63:143-148. Utilized data from an industrial accident that allowed for the study of residential exposure to dioxin at unprecedented levels and preterm birth.
Darrow LA, Stein CR, Steenland K. Serum perfluorooctanoic acid and perfluorooctane sulfonate concentrations in relation to birth outcomes in the mid-Ohio Valley, 2005-2010. Environ Health Perspect. 2013;121(10):1207–13.
Peltier MR, Koo HC, Getahun D, Menon R. Does exposure to flame retardants increase the risk for preterm birth? J Reprod Immunol. 2015;107:20–5.
Eskenazi B, Harley K, Bradman A, Weltzien E, Jewell NP, Barr DB, et al. Association of in utero organophosphate pesticide exposure and fetal growth and length of gestation in an agricultural population. Environ Health Perspect. 2004;112(10):1116–24.
Sathyanarayana S, Basso O, Karr CJ, Lozano P, Alavanja M, Sandler DP, et al. Maternal pesticide use and birth weight in the agricultural health study. J Agromedicine. 2010;15(2):127–36.
Kuang Z, McConnell LL, Torrents A, Meritt D, Tobash S. Atmospheric deposition of pesticides to an agricultural watershed of the Chesapeake Bay. J Environ Qual. 2003;32(5):1611–22.
Ochoa-Acuna H, Frankenberger J, Hahn L, Carbajo C. Drinking-water herbicide exposure in Indiana and prevalence of small-for-gestational-age and preterm delivery. Environ Health Perspect. 2009;117(10):1619–24.
Villanueva CM, Durand G, Coutte MB, Chevrier C, Cordier S. Atrazine in municipal drinking water and risk of low birth weight, preterm delivery, and small-for-gestational-age status. Occup Environ Med. 2005;62(6):400–5.
Chevrier C, Limon G, Monfort C, Rouget F, Garlantezec R, Petit C, et al. Urinary biomarkers of prenatal atrazine exposure and adverse birth outcomes in the PELAGIE birth cohort. Environ Health Perspect. 2011;119(7):1034–41.
Rinsky JL, Hopenhayn C, Golla V, Browning S, Bush HM. Atrazine exposure in public drinking water and preterm birth. Public Health Rep. 2012;127(1):72–80.
CDC. Fourth national report of human exposure to environmental chemicals. Atlanta, GA: Centers for Disease Control and Prevention; 2009. https://www.cdc.gov/exposurereport/pdf/fourthreport.pdf. Accessed 01/24/2017.
Adibi JJ, Hauser R, Williams PL, Whyatt RM, Calafat AM, Nelson H, et al. Maternal urinary metabolites of Di-(2-ethylhexyl) phthalate in relation to the timing of labor in a US multicenter pregnancy cohort study. Am J Epidemiol. 2009;169(8):1015–24.
Meeker JD, Hu H, Cantonwine DE, Lamadrid-Figueroa H, Calafat AM, Ettinger AS, et al. Urinary phthalate metabolites in relation to preterm birth in Mexico city. Environ Health Perspect. 2009;117(10):1587–92.
Ferguson KK, McElrath TF, Meeker JD. Environmental phthalate exposure and preterm birth. JAMA Pediatr. 2014;168(1):61–7.
Ferguson KK, McElrath TF, Ko YA, Mukherjee B, Meeker JD. Variability in urinary phthalate metabolite levels across pregnancy and sensitive windows of exposure for the risk of preterm birth. Environ Int. 2014;70:118–24.
Huang Y, Li J, Garcia JM, Lin H, Wang Y, Yan P, et al. Phthalate levels in cord blood are associated with preterm delivery and fetal growth parameters in Chinese women. PLoS One. 2014;9(2):e87430.
Cantonwine D, Meeker JD, Hu H, Sanchez BN, Lamadrid-Figueroa H, Mercado-Garcia A, et al. Bisphenol a exposure in Mexico City and risk of prematurity: a pilot nested case control study. Environ Health. 2010;9:62.
Cantonwine DE, Ferguson KK, Mukherjee B, McElrath TF, Meeker JD. Urinary bisphenol a levels during pregnancy and risk of preterm birth. Environ Health Perspect. 2015;123(9):895–901.
Behnia F, Peltier M, Getahun D, Watson C, Saade G, Menon R. High bisphenol a (BPA) concentration in the maternal, but not fetal, compartment increases the risk of spontaneous preterm delivery. J Matern Fetal Neonatal Med. 2016;29(22):3583–9.
Calafat AM. Contemporary issues in exposure assessment using biomonitoring. Current Epidemiology Reports. 2016;3(2):145–53.
Andrews KW, Savitz DA, Hertz-Picciotto I. Prenatal lead exposure in relation to gestational age and birth weight: a review of epidemiologic studies. Am J Ind Med. 1994;26(1):13–32.
Ahmad SA, Sayed MH, Barua S, Khan MH, Faruquee MH, Jalil A, et al. Arsenic in drinking water and pregnancy outcomes. Environ Health Perspect. 2001;109(6):629–31.
Nishijo M, Nakagawa H, Honda R, Tanebe K, Saito S, Teranishi H, et al. Effects of maternal exposure to cadmium on pregnancy outcome and breast milk. Occup Environ Med. 2002;59(6):394–6. discussion 7
Cantonwine D, Hu H, Sanchez BN, Lamadrid-Figueroa H, Smith D, Ettinger AS, et al. Critical windows of fetal lead exposure: adverse impacts on length of gestation and risk of premature delivery. J Occup Environ Med. 2010;52(11):1106–11.
Vigeh M, Yokoyama K, Seyedaghamiri Z, Shinohara A, Matsukawa T, Chiba M, et al. Blood lead at currently acceptable levels may cause preterm labour. Occup Environ Med. 2011;68(3):231–4.
Taylor CM, Golding J, Emond AM. Adverse effects of maternal lead levels on birth outcomes in the ALSPAC study: a prospective birth cohort study. BJOG. 2015;122(3):322–8.
Zhang B, Xia W, Li Y, Bassig BA, Zhou A, Wang Y, et al. Prenatal exposure to lead in relation to risk of preterm low birth weight: a matched case-control study in China. Reprod Toxicol. 2015;57:190–5.
Brown MJ, Margolis S. Lead in drinking water and human blood lead levels in the United States. MMWR Suppl. 2012;61(4):1–9.
Sowers M, Jannausch M, Scholl T, Li W, Kemp FW, Bogden JD. Blood lead concentrations and pregnancy outcomes. Arch Environ Health. 2002;57(5):489–95.
Falcon M, Vinas P, Luna A. Placental lead and outcome of pregnancy. Toxicology. 2003;185(1–2):59–66.
Perkins M, Wright RO, Amarasiriwardena CJ, Jayawardene I, Rifas-Shiman SL, Oken E. Very low maternal lead level in pregnancy and birth outcomes in an eastern Massachusetts population. Ann Epidemiol. 2014;24(12):915–9.
Zhu M, Fitzgerald EF, Gelberg KH, Lin S, Druschel CM. Maternal low-level lead exposure and fetal growth. Environ Health Perspect. 2010;118(10):1471–5.
Taylor CM, Golding J, Emond AM. Blood mercury levels and fish consumption in pregnancy: risks and benefits for birth outcomes in a prospective observational birth cohort. Int J Hyg Environ Health. 2016;219(6):513–20.
Bashore CJ, Geer LA, He X, Puett R, Parsons PJ, Palmer CD, et al. Maternal mercury exposure, season of conception and adverse birth outcomes in an urban immigrant community in Brooklyn, New York. USA Int J Environ Res Public Health. 2014;11(8):8414–42.
Myers SL, Lobdell DT, Liu Z, Xia Y, Ren H, Li Y, et al. Maternal drinking water arsenic exposure and perinatal outcomes in inner Mongolia. China J Epidemiol Community Health. 2010;64(4):325–9.
Zhang YL, Zhao YC, Wang JX, Zhu HD, Liu QF, Fan YG, et al. Effect of environmental exposure to cadmium on pregnancy outcome and fetal growth: a study on healthy pregnant women in China. J Environ Sci Health A Tox Hazard Subst Environ Eng. 2004;39(9):2507–15.
Landgren O. Environmental pollution and delivery outcome in southern Sweden: a study with central registries. Acta Paediatr. 1996;85(11):1361–4.
Fagher U, Laudanski T, Schutz A, Sipowicz M, Akerlund M. The relationship between cadmium and lead burdens and preterm labor. Int J Gynaecol Obstet. 1993;40(2):109–14.
Wang H, Liu L, Hu YF, Hao JH, Chen YH, Su PY, et al. Association of maternal serum cadmium level during pregnancy with risk of preterm birth in a Chinese population. Environ Pollut. 2016;216:851–7.
Yang J, Huo W, Zhang B, Zheng T, Li Y, Pan X, et al. Maternal urinary cadmium concentrations in relation to preterm birth in the healthy baby cohort study in China. Environ Int. 2016;94:300–6.
Huang K, Li H, Zhang B, Zheng T, Li Y, Zhou A, et al. Prenatal cadmium exposure and preterm low birth weight in China. J Expo Sci Environ Epidemiol. 2016. [epub ahead of print].
Hertz-Picciotto I, Schramm M, Watt-Morse M, Chantala K, Anderson J, Osterloh J. Patterns and determinants of blood lead during pregnancy. Am J Epidemiol. 2000;152(9):829–37.
Stieb DM, Chen L, Eshoul M, Judek S. Ambient air pollution, birth weight and preterm birth: a systematic review and meta-analysis. Environ Res. 2012;117:100–11.
Dadvand P, Basagaña X, Figueras F, Martinez D, Beelen R, Cirach M, et al. Air pollution and preterm premature rupture of membranes: a spatiotemporal analysis. Am J Epidemiol. 2014;179(2):200–7.
Panasevich S, Håberg SE, Aamodt G, London SJ, Stigum H, Nystad W, et al. Association between pregnancy exposure to air pollution and birth weight in selected areas of Norway. Archives of Public Health. 2016;74(1):26.
Stieb DM, Chen L, Hystad P, Beckerman BS, Jerrett M, Tjepkema M, et al. A national study of the association between traffic-related air pollution and adverse pregnancy outcomes in Canada, 1999–2008. Environ Res. 2016;148:513–26.
• Hyder A, Lee HJ, Ebisu K, Koutrakis P, Belanger K, Bell ML. PM2.5 exposure and birth outcomes: use of satellite-and monitor-based data. Epidemiology (Cambridge, Mass). 2014;25(1):58. This paper utilized satellite data to estimate particulate matter exposures in small geospatial areas and examined associations by week of exposure in pregnancy.
Kloog I, Melly SJ, Ridgway WL, Coull BA, Schwartz J. Using new satellite based exposure methods to study the association between pregnancy PM2.5 exposure, premature birth and birth weight in Massachusetts. Environ Health. 2012;11(1):1.
Lavigne E, Yasseen AS, Stieb DM, Hystad P, van Donkelaar A, Martin RV, et al. Ambient air pollution and adverse birth outcomes: differences by maternal comorbidities. Environ Res. 2016;148:457–66.
• Laurent O, Hu J, Li L, Kleeman MJ, Bartell SM, Cockburn M, et al. A statewide nested case-control study of preterm birth and air pollution by source and composition: California, 2001–2008. Environ Health Perspect Published Online First. 2016;19. This study examined source (e.g., roadways, meat cooking) and composition (e.g., nitrate, organic carbon) of particulate matter specifically in relation to preterm birth.
Pereira G, Bell ML, Lee HJ, Koutrakis P, Belanger K. Sources of fine particulate matter and risk of preterm birth in Connecticut, 2000-2006: a longitudinal study. Environmental Health Perspectives (Online). 2014;122(10):1117.
• Rappazzo KM, Daniels JL, Messer LC, Poole C, Lobdell DT. Exposure to elemental carbon, organic carbon, nitrate, and sulfate fractions of fine particulate matter and risk of preterm birth in New Jersey, Ohio, and Pennsylvania (2000–2005). Environ Health Perspect. 2015;123(10):1059. This paper examined fractions of PM2.5 in relation to preterm birth
Hao H, Chang HH, Holmes HA, Mulholland JA, Klein M, Darrow LA, et al. Air pollution and preterm birth in the US state of Georgia (2002–2006): associations with concentrations of 11 ambient air pollutants estimated by combining community multiscale air quality model (CMAQ) simulations with stationary monitor measurements. Environ Health Perspect. 2016;124(6):875.
Mendola P, Wallace M, Hwang BS, Liu D, Robledo C, Mӓnnistӧ T, et al. Preterm birth and air pollution: Critical windows of exposure for women with asthma. J Allergy Clin Immunol. 2016;138(2):432–440.e5.
• Li S, Guo Y, Williams G. Acute impact of hourly ambient air pollution on preterm birth. Environ Health Perspect. 2016;124(10):1623–9. This paper examined hourly exposures of criteria air pollutants in the window immediately preceding onset of labor.
Padula AM, Mortimer KM, Tager IB, Hammond SK, Lurmann FW, Yang W, et al. Traffic-related air pollution and risk of preterm birth in the San Joaquin Valley of California. Ann Epidemiol. 2014;24(12):888–95. e4
Rappazzo KM, Daniels JL, Messer LC, Poole C, Lobdell DT. Exposure to fine particulate matter during pregnancy and risk of preterm birth among women in New Jersey, Ohio, and Pennsylvania, 2000-2005. Environmental Health Perspectives (Online). 2014;122(9):992.
Pereira G, Bell ML, Belanger K, de Klerk N. Fine particulate matter and risk of preterm birth and pre-labor rupture of membranes in Perth, Western Australia 1997–2007: a longitudinal study. Environ Int. 2014;73:143–9.
Pereira G, Evans KA, Rich DQ, Bracken MB, Bell ML. Fine particulates, preterm birth, and membrane rupture in Rochester. NY Epidemiology. 2016;27(1):66–73.
• Wallace ME, Grantz KL, Liu D, Zhu Y, Kim SS, Mendola P. Exposure to ambient air pollution and premature rupture of membranes. Am J Epidemiol. 2016. This paper examined acute exposure to criteria air pollutants by focusing on the 8 days and 5 hours preceding delivery, and focused on one specific presentation of preterm birth (PPROM).
Lin Y-T, Jung C-R, Lee YL, Hwang B-F. Associations between ozone and preterm birth in women who develop gestational diabetes. Am J Epidemiol. 2015;181(4):280–7.
Bertin M, Chevrier C, Serrano T, Monfort C, Rouget F, Cordier S, et al. Association between prenatal exposure to traffic-related air pollution and preterm birth in the PELAGIE mother–child cohort, Brittany, France. Does the urban–rural context matter? Environ Res. 2015;142:17–24.
Lamichhane DK, Leem J-H, Lee J-Y, Kim H-C. A meta-analysis of exposure to particulate matter and adverse birth outcomes. Environ Health Toxicol. 2015;30
Sapkota A, Chelikowsky AP, Nachman KE, Cohen AJ, Ritz B. Exposure to particulate matter and adverse birth outcomes: a comprehensive review and meta-analysis. Air Quality, Atmosphere & Health. 2012;5(4):369–81.
Sun X, Luo X, Zhao C, Zhang B, Tao J, Yang Z, et al. The associations between birth weight and exposure to fine particulate matter (PM 2.5) and its chemical constituents during pregnancy: a meta-analysis. Environ Pollut. 2016;211:38–47.
Zhu X, Liu Y, Chen Y, Yao C, Che Z, Cao J. Maternal exposure to fine particulate matter (PM2. 5) and pregnancy outcomes: a meta-analysis. Environ Sci Pollut Res. 2015;22(5):3383–96.
Gray SC, Edwards SE, Schultz BD, Miranda ML. Assessing the impact of race, social factors and air pollution on birth outcomes: a population-based study. Environ Health. 2014;13(1):1.
Johnson S, Bobb JF, Ito K, Savitz DA, Elston B, Shmool J, et al. Ambient fine particulate matter, nitrogen dioxide, and preterm birth in New York City. Environ Health Perspect. 2016;124(8):1283–90.
Symanski E, Davila M, McHugh MK, Waller DK, Zhang X, Lai D. Maternal exposure to fine particulate pollution during narrow gestational periods and newborn health in Harris County, Texas. Matern Child Health J. 2014;18(8):2003–12.
Fleischer. Outdoor air pollution, preterm birth, and low birth weight: analysis of the World Health Organization global survey on maternal and perinatal health (vol 122, pg 425, 2014). Environ Health Perspect. 2014;122(6):A151-A.
Ha S, Hu H, Roth J, Kan H, Xu X. Associations between residential proximity to power plants and adverse birth outcomes. Am J Epidemiol. 2015;182(3):215–24.
Balsa AI, Caffera M, Bloomfield J. Exposures to particulate matter from the eruptions of the Puyehue Volcano and birth outcomes in Montevideo, Uruguay. Environ Health Perspect. 2016.
Huang C, Nichols C, Liu Y, Zhang Y, Liu X, Gao S, et al. Ambient air pollution and adverse birth outcomes: a natural experiment study. Popul Health Metrics. 2015;13(1):1.
Candela S, Ranzi A, Bonvicini L, Baldacchini F, Marzaroli P, Evangelista A, et al. Air pollution from incinerators and reproductive outcomes: a multisite study. Epidemiology. 2013;24(6):863–70.
Capobussi M, Tettamanti R, Marcolin L, Piovesan L, Bronzin S, Gattoni ME, et al. Air pollution impact on pregnancy outcomes in Como, Italy. J Occup Environ Med. 2016;58(1):47–52.
Estarlich M, Ballester F, Davdand P, Llop S, Esplugues A, Fernández-Somoano A, et al. Exposure to ambient air pollution during pregnancy and preterm birth: a Spanish multicenter birth cohort study. Environ Res. 2016;147:50–8.
Olsson D, Ekström M, Forsberg B. Temporal variation in air pollution concentrations and preterm birth—a population based epidemiological study. Int J Environ Res Public Health. 2012;9(1):272–85.
Trasande L, Wong K, Roy A, Savitz DA, Thurston G. Exploring prenatal outdoor air pollution, birth outcomes and neonatal health care utilization in a nationally representative sample. Journal of Exposure Science and Environmental Epidemiology. 2013;23(3):315–21.
Arroyo V, Díaz J, Ortiz C, Carmona R, Sáez M, Linares C. Short term effect of air pollution, noise and heat waves on preterm births in Madrid (Spain). Environ Res. 2016;145:162–8.
Baker P, Agius R. Air pollution exposure and adverse pregnancy outcomes in a large UK birth cohort: use of a novel spatio-temporal modelling technique. Scand J Work Environ Health. 2014;40(5):518.
Dibben C, Clemens T. Place of work and residential exposure to ambient air pollution and birth outcomes in Scotland, using geographically fine pollution climate mapping estimates. Environ Res. 2015;140:535–41.
Olsson D, Mogren I, Eneroth K, Forsberg B. Traffic pollution at the home address and pregnancy outcomes in Stockholm. Sweden BMJ open. 2015;5(8):e007034.
Olsson D, Mogren I, Forsberg B. Air pollution exposure in early pregnancy and adverse pregnancy outcomes: a register-based cohort study. BMJ Open. 2013;3(2):e001955.
Poirier A, Dodds L, Dummer T, Rainham D, Maguire B, Johnson M. Maternal exposure to air pollution and adverse birth outcomes in Halifax. Nova Scotia J Occup Environ Med. 2015;57(12):1291–8.
Qian Z, Liang S, Yang S, Trevathan E, Huang Z, Yang R, et al. Ambient air pollution and preterm birth: a prospective birth cohort study in Wuhan. China Int J Hyg Environ Health. 2016;219(2):195–203.
Schifano P, Lallo A, Asta F, De Sario M, Davoli M, Michelozzi P. Effect of ambient temperature and air pollutants on the risk of preterm birth, Rome 2001–2010. Environ Int. 2013;61:77–87.
van den Hooven EH, Pierik FH, de Kluizenaar Y, Willemsen SP, Hofman A, van Ratingen SW, et al. Air pollution exposure during pregnancy, ultrasound measures of fetal growth, and adverse birth outcomes: a prospective cohort study. Environ Health Perspect. 2012;120(1):150.
ATSDR. Toxicological profile for polycyclic aromatic hydrocarbons Atlanta: agency for toxic substances and disease registry; 1995 [09/26/2014]. Available from: http://www.atsdr.cdc.gov/toxprofiles/tp.asp?id=122&tid=25.
Padula AM, Noth EM, Hammond SK, Lurmann FW, Yang W, Tager IB, et al. Exposure to airborne polycyclic aromatic hydrocarbons during pregnancy and risk of preterm birth. Environ Res. 2014;135:221–6.
Wilhelm M, Ghosh JK, Su J, Cockburn M, Jerrett M, Ritz B. Traffic-related air toxics and preterm birth: a population-based case-control study in Los Angeles County. California Environ Health. 2011;10:89.
Guo Y, Huo X, Wu K, Liu J, Zhang Y, Xu X. Carcinogenic polycyclic aromatic hydrocarbons in umbilical cord blood of human neonates from Guiyu, China. Sci Total Environ. 2012;427-428:35–40.
Forand SP, Lewis-Michl EL, Gomez MI. Adverse birth outcomes and maternal exposure to trichloroethylene and tetrachloroethylene through soil vapor intrusion in New York state. Environ Health Perspect. 2012;120(4):616.
Porter TR, Kent ST, Su W, Beck HM, Gohlke JM. Spatiotemporal association between birth outcomes and coke production and steel making facilities in Alabama, USA: a cross-sectional study. Environ Health. 2014;13(1):1.
Ghosh JKC, Wilhelm M, Ritz B. Effects of residential indoor air quality and household ventilation on preterm birth and term low birth weight in Los Angeles County. California Am J Public Health. 2013;103(4):686–94.
Ion R, Bernal AL. Smoking and preterm birth. Reprod Sci. 2015;22(8):918–26.
Salmasi G, Grady R, Jones J, McDonald SD. Environmental tobacco smoke exposure and perinatal outcomes: a systematic review and meta-analyses. Acta Obstet Gynecol Scand. 2010;89(4):423–41.
Cui H, Gong T-T, Liu C-X, Wu Q-J. Associations between passive maternal smoking during pregnancy and preterm birth: evidence from a meta-analysis of observational studies. PLoS One. 2016;11(1):e0147848.
Crane J, Keough M, Murphy P, Burrage L, Hutchens D. Effects of environmental tobacco smoke on perinatal outcomes: a retrospective cohort study. BJOG. 2011;118(7):865–71.
Qiu J, He X, Cui H, Zhang C, Zhang H, Dang Y, et al. Passive smoking and preterm birth in urban China. Am J Epidemiol. 2014;180(1):94–102.
Ion RC, Wills AK, Bernal AL. Environmental tobacco smoke exposure in pregnancy is associated with earlier delivery and reduced birth weight. Reprod Sci. 2015:1933719115612135.
Slama R, Darrow L, Parker J, Woodruff TJ, Strickland M, Nieuwenhuijsen M, et al. Meeting report: atmospheric pollution and human reproduction. Environ Health Persp. 2008;116(6):791–8.
Zeger SL. Invited commentary: epidemiologic studies of the health associations of environmental exposures with preterm birth. Am J Epidemiol. 2011:kwr405.
Pereira G, Belanger K, Ebisu K, Bell ML. Fine particulate matter and risk of preterm birth in Connecticut in 2000–2006: a longitudinal study. Am J Epidemiol. 2013:kwt216.
Parker JD, Rich DQ, Glinianaia SV, Leem JH,Wartenberg D, Bell ML, et al. The international collaboration on air pollution and pregnancy outcomes: initial results. Environ Health Perspect. 2011;119(7):1023–8.
• Ferguson KK, McElrath TF, Ko Y-A, Mukherjee B, Meeker JD. Variability in urinary phthalate metabolite levels across pregnancy and sensitive windows of exposure for the risk of preterm birth. Environ Int. 2014;70:118–24. Adds to the literature characterizing variability in phthalate levels across pregnancy. Serves as the first study to examine utilize longitudinally collected exposure data to explore differences in the association of phthalates and preterm birth at different times of exposure during pregnancy. The association between phthalate metabolites and preterm birth using multiple measures of exposure collected longitudinally across pregnancy
• Cantonwine DE, Ferguson KK, Mukherjee B, McElrath TF, Meeker JD. Urinary bisphenol A levels during pregnancy and risk of preterm birth. Environ health Perspect. 2015; 123(9) :895 .Serves as the first study to examine the association between BPA exposure and preterm birth using multiple measures of exposure collected longitudinally across pregnancy. Further explored the association with BPA and preterm birth by assessing differences by infant sex.
Ferguson KK, McElrath TF, Meeker JD. Environmental phthalate exposure and preterm birth. JAMA Pediatr. 2014;168(1):61–8.
Ferguson KK, McElrath TF, Chen Y-H, Mukherjee B, Meeker JD. Urinary phthalate metabolites and biomarkers of oxidative stress in pregnant women: a repeated measures analysis. Environ Health Perspect. 2015;123(3):210–6.
Ferguson KK, McElrath TF, Chen Y-H, Loch-Caruso R, Mukherjee B, Meeker JD. Repeated measures of urinary oxidative stress biomarkers during pregnancy and preterm birth. Am J Obstet Gynecol. 2015;212(2):208.e1-8.
•• Ferguson KK, Chen Y-H, VanderWeele TJ, McElrath TF, Meeker JD, Mukherjee B. Mediation of the relationship between maternal phthalate exposure and preterm birth by oxidative stress with repeated measurements across pregnancy. Environ Health Perspect. 2016. This study examined windows of vulnerability to exposure during pregnancy, spontaneous preterm birth specifically, and examined 8-isoprostane as a biomarker of oxidative stress to demonstrate statistical mediation of the phthalate-preterm birth association.
Darrow LA, Stein CR, Steenland K. Serum perfluorooctanoic acid and perfluorooctane sulfonate concentrations in relation to birth outcomes in the mid-Ohio Valley, 2005–2010. Environ Health Perspect. 2013;121(10):1207.
Albouy-Llaty M, Limousi F, Carles C, Dupuis A, Rabouan S, Migeot V. Association between exposure to endocrine disruptors in drinking water and preterm birth, taking neighborhood deprivation into account: a historic cohort study. Int J Environ Res Public Health. 2016; 13(8).
Cantonwine D, Meeker JD, Hu H, Sanchez BN, Lamadrid-Figueroa H, Mercado-Garcia A, et al. Bisphenol a exposure in Mexico City and risk of prematurity: a pilot nested case control study. Environ Health. 2010b;9:62.
Ruckart PZ, Bove FJ, Maslia M. Evaluation of contaminated drinking water and preterm birth, small for gestational age, and birth weight at Marine Corps Base Camp Lejeune, North Carolina: a cross-sectional study. Environ Health. 2014;13(1):1.
Cantonwine D, Hu H, Sanchez BN, Lamadrid-Figueroa H, Smith D, Ettinger AS, et al. Critical windows of fetal lead exposure: adverse impacts on length of gestation and risk of premature delivery. J Occup Environ Med. 2010a;52(11):1106–11.
Shi X, Ayotte JD, Onda A, Miller S, Rees J, Gilbert-Diamond D, et al. Geospatial association between adverse birth outcomes and arsenic in groundwater in New Hampshire. USA Environ Geochem Health. 2015;37(2):333–51.
Le HQ, Batterman SA, Wirth JJ, Wahl RL, Hoggatt KJ, Sadeghnejad A, et al. Air pollutant exposure and preterm and term small-for-gestational-age births in Detroit, Michigan: long-term trends and associations. Environ Int. 2012;44:7–17.
Lee P-C, Roberts JM, Catov JM, Talbott EO, Ritz B. First trimester exposure to ambient air pollution, pregnancy complications and adverse birth outcomes in Allegheny County, PA. Matern Child Health J. 2013;17(3):545–55.
Pereira G, Bracken MB, Bell ML. Particulate air pollution, fetal growth and gestational length: the influence of residential mobility in pregnancy. Environ Res. 2016;147:269–74.
Schifano P, Asta F, Dadvand P, Davoli M, Basagana X, Michelozzi P. Heat and air pollution exposure as triggers of delivery: a survival analysis of population-based pregnancy cohorts in Rome and Barcelona. Environ Int. 2016;88:153–9.
Symanski E, McHugh MK, Zhang X, Craft ES, Lai D. Evaluating narrow windows of maternal exposure to ozone and preterm birth in a large urban area in Southeast Texas. J Expo Sci Environ Epidemiol 2016;26(2):167–72.
Chang HH, Reich BJ, Miranda ML. Time-to-event analysis of fine particle air pollution and preterm birth: results from North Carolina, 2001–2005. Am J Epidemiol. 2012;175(2):91–8.
DeFranco E, Moravec W, Xu F, Hall E, Hossain M, Haynes EN, et al. Exposure to airborne particulate matter during pregnancy is associated with preterm birth: a population-based cohort study. Environ Health. 2016;15(1):1.
Arffin F, AL-Bayaty FH, Hassan J. Environmental tobacco smoke and stress as risk factors for miscarriage and preterm births. Arch Gynecol Obstet. 2012;286(5):1187–91.
Luo Y-J, Wen X-Z, Ding P, He Y-H, Xie C-B, Liu T, et al. Interaction between maternal passive smoking during pregnancy and CYP1A1 and GSTs polymorphisms on spontaneous preterm delivery. PLoS One. 2012;7(11):e49155.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Kelly K. Ferguson and Helen B. Chin each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Environmental Epidemiology
Rights and permissions
About this article
Cite this article
Ferguson, K.K., Chin, H.B. Environmental Chemicals and Preterm Birth: Biological Mechanisms and the State of the Science. Curr Epidemiol Rep 4, 56–71 (2017). https://doi.org/10.1007/s40471-017-0099-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40471-017-0099-7