Abstract
Tissue heating is used for the treatment of health disorders. However, the benefits of this therapy depend heavily on the temperature reached in the tissues. Values outside the ideal range recommended for therapeutic effects may result in ineffective or tissue-damaging treatments. Thus, understanding the heat transfer process and knowing the temperature distribution in biological tissues are essential factors for this treatment to be applied safely and effectively. In this context, the numerical simulation becomes an interesting tool to understand the temperature field in the different tissues that make up the joint and, thus, to contribute to a better application of the thermal resources used in the clinical practice of physiotherapy. This study aimed to simulate the transient heat transfer in a canine knee joint during the application of a therapeutic heating feature and to investigate the effects of blood perfusion performed at a constant rate (A1 simulation) and as a function of tissue temperature distribution (A2 simulation). The heat diffusion equation was used to model the heat transfer phenomenon. The simulations were performed using the ANSYS-CFX® program. The results obtained from the simulations were compared with in vivo experimental data. The A1 simulation showed a maximum percentage difference of 25.6% compared to the experimental data. In contrast, the highest percentage difference found for the A2 simulation was 9.8%. In conclusion, the results suggest that simulation can be an important tool to evaluate the temperature behaviour of biological tissues during the application of thermal therapeutic resources.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Thermal heating features are commonly used in health to promote pain relief [1], to reduce oedema, to facilitate the healing process [2], to increase the extensibility of conjunctive tissue [3, 4] and to modify muscle tone [5]. In the clinical context, the main objective of such therapy is to promote tissue injury recovery conditions without damaging the tissue [6].
However, the success, safety and efficacy procedures involving heat transfer are highly dependent on understanding the thermal behaviour of different biological tissues. According to Chen et al. [7], heating agents must be able to increase the tissue temperature within a limit of 38–44 °C to produce the desired therapeutic effect. At temperatures above 45 °C, the protein damage is considerable, predisposing the individual to cell and tissue destruction. Thus, values outside of the recommended therapeutic range may result in ineffective treatment or thermal damage to the tissue [8]. Therefore, to use therapeutic heating efficiently and safely, it is essential that the heat transfer process in biological tissues is understood and that the temperature behaviour is determined the specific tissue type [9]. Although in vivo measurements of tissue temperature are used for this purpose, there are still great difficulties and risks associated with performing these temperature monitoring measures, mainly due to the invasive profile, the imprecision involved in the control of various parameters and the limitations of the measures [10].
However, studies investigating temperature behaviour in living tissues have grown since 1948, when Harry Pennes proposed the first bioheat transfer model that related the temperature of biological tissues to blood perfusion and metabolic heat generation [11]. The model was based on an experimental procedure, in which the temperature in the radial position of the forearm of nine individuals was measured. Temperatures were measured by thermocouples inserted in the forearms of individuals. No anaesthesia was applied to avoid effects on blood perfusion [12]. Since then, several alternative heat transfer models have been developed providing a quantitative analysis of the complex phenomenon of heat transfer in living tissues [12]. Since the publication of the heat transfer equation, due to its great simplicity and the ability to predict the temperature distribution reasonably well, the Pennes equation has been widely used for the analysis of a range of heat transfer phenomena in living tissues [13,14,15].
In the last two decades, the use of numerical simulations to solve complex health problems has become a reality due to the large spread of computer use and the relative ease of the application of numerical methods [16]. Numerical simulations are presented as a non-invasive and alternative form of temperature evaluation that is low cost and that enables the calculation, analysis and display of temperature changes that occur with time at any therapeutic target [10]. However, thus far, the vast majority of research has been directed at the assessment of tumour location and size [17] or the use of hyperthermia in cancer treatment [18]. There are few studies in the literature that evaluate the temperature distribution in the tissue during the application of thermal heating resources used for rehabilitation. In addition, the results obtained with the simulations are rarely compared with real data (experimental in vivo), which leaves doubt as to the accuracy of the simulated data. The present study reproduces a real therapeutic heating situation and compares simulated results with in vivo experimental data. In addition, conditions commonly adopted in simulation studies (the rate of blood perfusion assumed constant or as a function of temperature) are evaluated, showing the impact of these considerations on the simulation results.
This study aims to simulate the transient heat transfer in the canine knee joint during the application of a heating therapeutic resource and to evaluate the temperature behaviour in different tissue layers. Additionally, this study is intended to investigate the effects of blood perfusion performed at a constant rate and as a function of tissue temperature distribution.
2 Materials and methods
2.1 Geometric model and mesh generation
The knee joint’s geometry is an irregular structure and cannot be represented as a combination of flat objects; therefore, the structure’s temperature distribution cannot be obtained analytically. Thus, the use of an alternative method, such as numerical simulation, becomes inevitable.
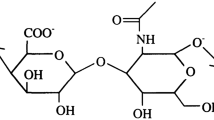
The geometric model of the canine knee joint was created based on a photographic record of a cross section of an anatomical part (Fig. 1a). Prior to developing the model, the various tissues that make up the joint of the canine knee were established by visual inspection. The skin, the subcutaneous tissue, the fat and muscle tissue, the pericapsular region and the intra-articular cavity (consisting of the tibiofemoral regions, ligaments and bone) were all considered as members of the joint structure. The geometric model was developed with the help of the SolidWorks® program, in which each region was bounded on the imported photographic record. An exception was made for the epidermis layer, the boundaries of which, due to the layer’s thinness, could not be determined in the image. Thus, this layer was generated based on the thickness values available in the literature (8 × 10−5 m) [9]. To correspond to the actual size of the canine knee joint, the model was adjusted to scale by means of a measuring instrument included in the photographic image. The geometric model was developed with a thickness of 0.5 mm. This was the smallest thickness allowed by the simulation software. The geometric model can be observed in Fig. 1b.
After the development of computational domain, the meshes were built using ANSYS Meshing, a tool available in the ANSYS Workbench® platform. According to the literature, mesh generation is one of the most critical aspects of the simulation. High or very small numbers of elements can result in long simulation times or inaccurate results, respectively [19]. The simulations were started with less-refined meshes composed of prismatic quadrangular elements. Subsequently, the initial coarse meshes were gradually refined until the average changes in the temperature results in tissues were lower than 1%. Refinements followed the criteria of the length value of the mesh element, as described in the literature [20]. For the choice of the ideal mesh, the solution was considered to be independent of the mesh with a percentage difference lower than 1% between the results obtained with the previous coarse mesh and the subsequent refined mesh. Among the three evaluated meshes, the intermediate mesh, which had 29,002 elements and 68,442 knots, filled the criteria cited above; therefore, it was chosen to perform the simulations. The chosen mesh for the heating process simulation can be observed in Fig. 2.
2.2 Mathematic model
The heat diffusion equation was used to model the heat transfer phenomenon in solid tissues during therapeutic heating conditions (Eq. 1). The software provides conditions for the relevant physiological terms (metabolism and perfusion) to be included in the diffusion equation, as source terms, in the same way as in the Pennes equation [11]. The additional source terms of heat conduction equation arising in thermal energy equation were introduced by means of UDF (user-defined function) functionality of the ANSYS (Eq. 2). The equations can be described as:
where: ρ and cp represent the specific mass (kg m−3) and the specific heat of the tissue (J kg−1 °C−1), respectively. cpb is the specific heat of blood (J kg−1 °C−1); ρb represents the blood specific mass (kg m−3); w is the blood perfusion (s−1); k is the thermal conductivity of each tissue (W m−1 °C−1); \(q_{\text{met}}^{ \cdot }\) is the volumetric rate of metabolic heat (W m−3), \(q_{\text{w}}^{ \cdot }\) is the blood perfusion rate of tissue (W m−3); and Tref and Tissue are the reference and tissue temperatures, respectively.
Rectal temperature (38.1 °C), considered as the reference temperature (Tref), and the temperatures used as initial conditions (Ti) of each tissue layer were removed from the Araújo study [9] (Table 1). According to the author, the initial temperatures were considered to be equal to the average of the experimental temperatures obtained in thermal neutrality condition (24.7 °C) [9]. The initial temperature was adopted from the bone, based on the innermost region where the temperature was measured in this study (the region of the cruciate ligaments).
Because the present study has as a specific objective to evaluate the effects of considering the blood perfusion rate (\(q_{\text{w}}^{ \cdot }\)) constant or as a function of temperature (Eq. 2), the simulations were performed with different considerations of flow rate. The simulation of the therapeutic heating that considered the blood perfusion rate to be constant was termed “A1 simulation” and the simulation that considered the blood perfusion rate as a function of temperature was termed “A2 simulation”.
2.3 Tissue properties and numerical simulation
The physiological and thermophysical properties adopted to perform the simulations were considered from the average of published data and were taken from the Araújo study [9]. The values of the variables used for each layer are shown in Table 1. All properties were considered constant for the execution of the simulations.
The simulations of the temperature behaviour of the knee joint were performed in transient therapeutic heating conditions. To perform the simulations, a second type of boundary condition was adopted in the upper and lower sides of the articulation, corresponding to a perfectly isolated or adiabatic surface. This measure assured that the heat transfer occurred only in the two-dimensional cross-sectional plane of the canine knee. On the outside face of the geometric model (i.e. the epidermis), the average heat flow of a thermal blanket (215.7 W m−2) was adopted as a boundary condition [9]. The simulations were performed considering a thermal blanket (50 cm × 29 cm) with an output power of 35.2 W, an average power of 31.2 W and automatic temperature control in the 40–66 °C range. The average temperature was set to 57.6 °C, and a 40-min treatment time was considered. The information regarding the external heating source and the time used to heat the canine knee, adopted for the implementation of the simulations, were taken from the experimental study by [9].
Once this model consists of different tissue layers, it is necessary to define the interface conditions between the various tissues. Thus, conservative heat flow was assigned between the tissue interfaces. The numerical simulation of the canine knee in the heating conditions was performed using the ANSYS-CFX® program.
According to the literature, the results of the numerical solution when compared to the reality of a physical problem may present some error related to the use of differential equations that do not adequately represent the phenomenon. For this reason, physical validation must be performed in order to demonstrate the fidelity of the mathematical model to the physical problem [19]. In the present study, the physical validation of the canine knee simulations was performed comparing the obtained results from the simulations with the average values of temperature measured from an experimental in vivo study [9]. Experimental measurements were performed on 10 adult dogs. The experimental protocol was approved by the Ethics Committee of the Universidade Federal de Minas Gerais (protocol 127/05). Ten conventional-type K thermocouples (previously calibrated) were used to perform the measurements. The sites of placement of the thermocouples were: skin surface, subcutaneous region, adipose tissue, periarticular musculature (medially and laterally), pericapsular region and intra-articular cavity. One thermocouple was inserted into the rectal mucosa to control body temperature in dogs. The heating process was conducted for 40 min, and temperatures were measured throughout this period.
According to the literature [21], the uncertainty of measurement is evaluated according to either a “Type A” or a “Type B” method of evaluation. The Type A evaluation of standard uncertainty is the method of evaluating the uncertainty by the statistical analysis of a series of observations. In this case, the standard uncertainty is the experimental standard deviation of the mean. The Type B evaluation of standard uncertainty is the method of evaluating the uncertainty by means other than the statistical analysis of a series of observations. In this case, the evaluation of the standard uncertainty is based on some other scientific knowledge. Values belonging to this category may be derived, for example, from experience with or general knowledge of the behaviour and properties of relevant materials and instruments. According to Cornacchia et al. [22], uncertainty evaluated using thermocouples type K can be considered as 1.1 °C.
In cases where a normal (Gaussian) distribution can be attributed and the standard uncertainty associated with the output estimate has sufficient reliability, the standard coverage factor k = 2 shall be used. The assigned expanded uncertainty corresponds to a coverage probability of approximately 95%.
The average percentage difference between the simulations and the experimental data was calculated for each of the tissue layers at different time instants. A smaller average percentage difference or one equal to 10% was considered acceptable, as the experimental measurements are subject to errors due to various difficulties involved in controlling the parameters. For a measurement to be performed without errors, the following would be required: 1—a perfect measurement system; 2—a controlled and perfectly stable environment; 3—a perfect operator and 4—that the measure had a single value that was perfectly definable and stable. However, in practice, it is not common that these conditions occur separately and even less common that they occur simultaneously [23]. Thus, to a greater or lesser extent, there will always be a measurement error, which justifies the adopted percentage difference consideration. Furthermore, thermophysical and physiological properties related to the heat biotransfer process are greatly discrepant in the literature. These differences demonstrate that uncertainties still exist in the experimental measurements of these properties.
3 Results and discussion
Figure 3 shows the temperature behaviour of each tissue during the A1 and A2 simulations and in the in vivo experiment. In A1 simulation, it was noted that in some cases, the 500-s threshold simulation curve behaviour approached the behaviour of the experimental curve. However, in the subsequent seconds, it was possible to note divergences between the simulated and experimental temperatures. It was also observed that simulated temperatures tended to increase during the analysed period, while the experimental temperatures tended to stabilize. This result can be explained due to the fact that the blood perfusion rate was considered as a constant value in A1 simulation. Thus, adding the value of the blood perfusion rate to the metabolism and heat received in the heating, the trend was that all tissues continuously heated up in the simulated case. In the experiment, the perfusion rate depended on the temperature of the tissue (which varied over time). The higher the temperature of the tissue was, the smaller the amount of heat supplied by the blood to the tissue, to an extent that blood could remove heat from the tissue (at a temperature above the reference temperature of 38.1 °C). According to the literature, the distribution and behaviour of tissue temperature can be highly modified by the cooling effect produced by increased blood flow in the region [24, 25]. Therefore, in reality, as the tissue heats up, the rate of heat supplied by the blood to the tissue decreases. When the temperature exceeds 38.1 °C (the reference temperature considered in this study), the blood starts to remove heat from the system until a time that the power source for the heating and the metabolism equals the heat loss by perfusion rate, and the system reaches the steady state (i.e. temperature stabilization).
In evaluating the temperature curves of A2 simulation, we note that, unlike the A1 simulation, all tissues had profiles similar to the experimental data. It was noted that, despite the fact that the tissue temperatures continued to be overestimated in the A2 simulation in relation to the data measured in vivo, the simulated temperature curve remained within the expanded uncertainty range for a longer period of time than in A1 simulation, with the exception of the subcutaneous and medial muscle layers after 1000 s.
Comparisons of the average percentage differences found between temperatures in the A1 and A2 simulation and the experimental data are listed in Table 2. The average percentage A1 simulation differences were greater than 10% for all layers and were greater in the region of the subcutaneous tissue (25.6%) and lower in the fat and bone tissues (13.8% and 13.9%, respectively). The simulated temperatures were overestimated, indicating a model difficulty in representing the measured experimental data. Thus, the results show that the conditions adopted for the A1 simulation (which differs from Penne’s biothermal model in which temperature-dependent perfusion is assumed) were not suitable to represent the canine knee temperature behaviour during tissue heating situations. However, it is noted that all of percentage differences in the A2 simulation were less than 10%. The largest percentage difference can be seen in the subcutaneous (9.7%). The smallest difference was obtained by fat and bone tissues (3.4%). Furthermore, it can be noted that temperature values when simulating the perfusion rate varying with temperature in the heating regime were much closer to the experimental data. Thus, there is evidence that modelling with blood perfusion varying as a function of temperature better represents the real phenomenon, resulting in values closer to the experimental data. However, considerations of the blood perfusion rate are controversial in the literature. Some studies have adopted the blood perfusion rate constant and other studies consider as function of temperature. However, given the paucity of experimental data for comparison, it is not possible to assess the impact of this consideration on the found studies.
Xiao et al. [26] performed numerical simulations to assess the contributions of temperature fields in normal and pathological knees on the effect of heating. The geometric model used for simulation considered only the skin, muscle, bone and blood vessels. Considerations of blood perfusion and metabolism were made only in the muscle and were disregarded in other tissues. The blood perfusion was considered constant. In this study, the simulated heating methods have not been well described, and the adopted criteria used for determining heat flow as a boundary condition were not made explicit in this work. This fact prevents the reproduction of this study in research and clinical practice. In addition to these limitations, the study does not perform physical model validation. According to Versteeg and Malalasekera [14], physical validation should be conducted to demonstrate the fidelity of the mathematical model in terms of the physical problem.
Xue et al. [27] computationally evaluated the effects of the major blood vessels of the human knee joint during the cooling and heating processes. For this purpose, a simplified three-dimensional model of the knee containing skin, muscle, bone and blood vessel has been developed. For simulations of the cooling and heating processes, the authors considered the presences of cold and heated liquids as boundary conditions. The characteristics of the simulated resources were not described in the study, which does not extend the results observed for correlations with clinical practice. Furthermore, the simulation results were not compared or correlated with either experimental or clinical data. In the simulations, the authors considered blood flow rate as a function of temperature. However, this consideration was performed only in the muscle layer. Based on the results found in this study, it should be noted that the blood flow rate influences the temperature behaviour in all tissue layers.
In Table 2, it can be observed that the epidermis, subcutaneous tissue, medial and lateral muscles and pericapsular end region showed temperatures above the limit recommended for therapeutic heating (38–45 °C) [7]. The epidermis presented the highest final temperature obtained with the simulation (49.8 °C), corresponding to the highest elevation in temperature, which was expected due to this structure’s close proximity with the heat flux boundary condition. The lowest simulated temperature and temperature rise occurred in the bone region (43.8 °C). In the A2 simulation, unlike what occurred in the A1 simulation, the final temperature values were within the appropriate temperature range for the benefits of heating that are provided without tissue damage. Similar to A1 simulation, the epidermal layers and bone area achieved the higher and lower final temperatures (43.8 °C and 39.8 °C, respectively). The occurrence of the lowest temperature in the bone region can be explained by the fact that the layer is located more internally and is overlapped by layers that hinder heat transfer to this region. According to the literature, little heat is transferred into the innermost regions due to the thermal resistance conferred by the skin and the subcutaneous and adipose tissues [28]. For Pardasani and Adlakha [29], the skin and subcutaneous and adipose tissues act as an insulating barrier for the body and, therefore, influence the degree of internal tissue temperature variation. The muscle layer, a frequent target of physical therapy, had high temperatures of 42.1 °C in the medial layer and 41.3 °C in the side layer. Draper et al. [30] reported that the physiological effects of tissue heating are dependent on the residual temperature changes in the tissues. The increase in tissue temperature, considered as mild heating, is able to increase the metabolic rate of the heated tissue. The moderate heat, characterized by an increase of 2–3 °C in the tissues, promotes a greater metabolic response and increases the blood circulation to dissipate heat. For temperature increases higher than 4 °C, vigorous heating is achieved, and tissue stiffness is reduced [30].
Figure 4 shows the temperature field of the A2 simulation in the cross-sectional plane of the canine knee joint. The epidermis region achieves the highest temperatures, reaching 45 °C at some locations. Moving towards the centre of the model, it can be noted that the temperatures decrease, reaching a minimum temperature of 35.9 °C. Therefore, from the outermost tissue layers to the innermost, the temperature gradient decreases. This result is consistent with studies in the literature that consider the surface heating methods, such as thermal blankets, as not being capable of efficiently heating tissues located at depths greater than 2 cm [31]. This fact is a function of the intolerance of the individual, the heating resistance of the tissue and the local body’s response to increased tissue temperature (i.e. vasodilation).
4 Conclusion
The present study simulated the heat transfer in the knee joint during canine therapeutic heating. Transient simulations were performed, considering: 1—a constant blood perfusion rate (A1 simulation) and 2—blood perfusion rate as a function of temperature (A2 simulation). The A1 simulation results in shorter computational time. However, the present study shows that this consideration is not consistent with the in vivo experimental data. The blood perfusion rate as a function of temperature is a nonlinear problem resulting in higher computation requirements. Despite this, the results of the simulation that adopted this condition obtained a better approximation with the experimental data. Since the implementation of the blood perfusion rate as function of temperature is not unanimous among published studies, this study provides information on the need to adopt this condition.
To reduce the uncertainty of the simulations in future studies, the other thermophysical and physiological properties can be considered as a function of temperature and the boundary condition can be altered and the heat losses from the thermal blanket to the environment considered.
References
Espinoza HJG, Bustamante IP, Perez SJM (2010) Revisión sistemática sobre el efecto analgésico de la crioterapia en el manejo del dolor de origen músculo esquelético [Systematic review of the analgesic effect of cryotherapy in the management of musculoskeletal pain]. Rev Soc Esp Dolor 15:242–252
Allen RJ (2006) Physical agents used in the management of chronic pain by physical therapists. Phys Med Rehabil Clin N Am 17:315–345
Nakano J, Yamabayashi C, Scott A, Reid D (2012) The effect of heat applied with stretch to increase range of motion: a systematic review. Phys Ther Sport 13:80–188
Dragone L, Heinrichs K, Levine D, Tucker T, Millis D (2014) Superficial thermal modalities. In: Millis D, Lelive D (eds) Can rehabilitation and physical therapy, 2nd edn. Saunders, pp 312–317
Hanks J, Lelive D, Bockstahler B (2015) Physical agent modalities in physical therapy and rehabilitation of small animals. Vet Clin N Am Small Anim Pract 45:29–44
Habash RWY, Bansal R, Krewski D, Alhafid HT (2006) Thermal therapy, part 1: an introduction to thermal therapy. Crit Rev Biomed Eng 34:459–489
Chen MM, Holmes KR (1980) Microvascular contributions in tissue heat transfer. Ann N Y Acad Sci 335:137–150
Jeon BJ, Choi HG (2015) Numerical analysis for the conjugate heat transfer of skin under contrast therapy. Int J Heat Mass Transf 86:388–396
Araújo AR (2009) Formulação e validação de um modelo térmico para estimativa da temperatura intra-articular. [Formulation and validation of a thermal model to estimate the intra -articular temperature.] Thesis (Ph.D in Mechanical Engineering) Tese (doutorado em Engenharia Mecânica). Universidade Federal de Minas Gerais. Departamento de Engenharia Mecânica. http://www.dominiopublico.gov.br/download/texto/cp140973.pdf
Trobec R, Sterk M, Almawed S, Veselko M (2008) Computer simulation of topical knee cooling. Comput Biol Med 38:1076–1083
Pennes HH (1948) Analysis of tissue and arterial blood temperatures in the resting human forearm. J Appl Physiol 1(2):93–122
Valvano JW Bioheat transfer. http://users.ece.utexas.edu/~valvano/research/jwv.pdf. Accessed 14 May 2016
Fu ZJ, Xi Q, Ling L, Cao CY (2017) Numerical investigation on the effect of tumor on the thermal behavior inside the skin tissue. Int J Heat Mass Transf 108:1154–1163
Joukar A, Nammakie E, Niroomand-Oscuii H (2015) A comparative study of thermal effects of 3 types of laser in eye: 3D simulation with bioheatequation. J Therm Biol 49–50:74–81
Lin Y et al (2015) Investigation of factors affecting hypothermic pelvic tissue cooling using bio-heat simulation based on MRI-segmented anatomic models. Comput Methods Programs Biomed 122:76–88
Rashkovska A, Trobec RK, Avbelj V, Veselko M (2013) Knee temperatures measured in vivo after arthroscopic ACL reconstruction followed by cryotherapy with gel-packs or computer controlled heat extraction. Knee Surg Sports Traumatol Arthrosc 22:2048–2056
Das K, Singh R, Mishra SC (2013) Numerical analysis for determination of the presence of a tumor and estimation of its size and location in a tissue. J Therm Biol 38:32–40
Gupta PK, Singh J, Rai KN (2013) A numerical study on heat transfer in tissues during hyperthermia. Math Comput Model 57:1018–1037
Versteeg HK, Malalasekera W (2007) An introduction to computational fluid dynamics: the finite volume method, 2nd edn. Prentice Hall, Englewood Cliffs
Celik IB, Ghia U, Roache PJ, Freitas CJ, Coleman H, Raad PE (2008) Procedure for estimation and reporting of uncertainty due to discretization in CFD applications. J Fluids Eng 130:078001-1–078001-4
European Accreditation Laboratory Committee (2013) Evaluation of the uncertainty of measurement in calibration, vol 2, pp 1–75
Cornacchia TM, Carvalho VE, de Las Casas EB, Andrade RM, Cimini Jr CA (2003) Thermal properties determination of esthetic restorative materials. In: Proceedings of the COBEM, 17th international congress of mechanical engineering. November 10–14, 2003, São Paulo, SP, Brazil
Júnior, AAG, Sousa, AR (2008) Fundamentos de Metrologia Científica e Industrial. Manole, 1ª edição
Lehmann JF, Silverman DR, Baum BA, Kirk NL, Johnston VC (1966) Temperature distributions in the human thigh, produced by infrared, hot pack and microware applications. Arch Phys Med Rehabil 47(5):291–299
Draper DO, Castro JL, Feland B, Schulthies S, Eggett D (2004) Shortware diathermy and prolonged stretching increase hamstring flexibility more than prolonged stretching alone. J Orthop Sports Phys Ther 34:13–20
Xiao J, He Z, Yang Y, Chen B, Deng Z, Liu J (2011) Investigation on three-dimensional temperature field of human knee considering anatomical structure. Int J Heat Mass Transf 54:1851–1860
Xue X, He ZZ, Liu J (2013) Computational study of thermal effects of large blood vessels in human knee joint. Comput Biol Med 43:63–72
Robertson VJ, Low J, Ward A, Reed A (2006) Electrotherapy explained: principles and practice, 4th edn. Elsevier, Butterworth-Heinemann, Amsterdam
Pardasani KR, Adlakha N (1995) Coaxial circular sector elements to study two dimensional heat distribuition problem in dermal gegions of humam limbs. Math Comput Model 22:127–140
Draper DO, Hawkes AR, Johnson AW, Diede MT, Rigby JH (2013) Muscle heating with megapulse ii shortwave diathermy and rebound diathermy. J Athl Train 48:477–482
Steiss JE, Levine D (2005) Physical agent modalities. Vet Clin N Am Small Anim Pract 35:1317–1333
Author contributions
FSS, ARA and RH conceived the concept of the study. FSS, MOC and LLB contributed to the data acquisition. FSS, MOC, LLB and RH performed the formal analysis. FSS and RH contributed to the funding acquisition. FSS, MOC, LLB and ARA performed the investigation. FSS, MOC, LLB and RH contributed to the methodology. FSS and RH administered the project. FSS, ARA and RH contributed to the resources. FSS, MOC and LLB were involved in software management. Supervision was done by ARA and RH. FSS, MOC, LLB, ARA and RH contributed equally in writing—original draft, review and editing.
Acknowledgements
This work was supported by the Fundação de Amparo à Pesquisa do Estado de Minas Gerais (FAPEMIG) under Grant APQ-02059-14 and Phd scholarship; PIBIC/CNPq under Grant 120222/2014-0.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Technical Editor: Estevam Barbosa Las Casas.
Rights and permissions
About this article
Cite this article
da Silva, F.S., Castro, M.O., Bernardes, L.L. et al. Numerical simulation of temperature variations in a canine knee joint during therapeutic heating. J Braz. Soc. Mech. Sci. Eng. 40, 486 (2018). https://doi.org/10.1007/s40430-018-1404-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40430-018-1404-1