Abstract
Purpose of Review
We aimed to conduct a systematic review of studies exploring the relationship between prenatal alcohol exposure (PAE) and hypothalamic-pituitary-adrenal (HPA) axis functioning in the offspring in humans.
Recent Findings
Animal studies have demonstrated that PAE has long-term consequences in HPA axis activity in the offspring. Fewer studies have been conducted in humans.
Summary
Our systematic review identified 9 studies including infants/toddlers (n = 6) and children/adolescents (n = 3). Cortisol responses to stress were only studied in infants/toddlers (3 studies: painful stressors; 3 studies: social stressors). In infants/toddlers, PAE seems to be associated with a blunted response to painful stressors whereas an enhanced cortisol response to social stress is observed (only in boys). In children/adolescents, the normal cortisol circadian rhythm is altered in PAE participants with a FASD diagnosis, who show increased evening cortisol levels. These findings support the programming effects of alcohol on the HPA stress system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The developmental origins of disease or fetal programming model predicts that early exposures to a variety of adverse events and signals have life-long consequences for physical and mental health. Programming refers to the effects of an environmental signal acting during a sensitive developmental period to influence the development of specific physiological systems [1, 2•, 3]. The hypothalamic-pituitary-adrenal (HPA) axis is an extremely sensitive physiological system whose activation, with the consequent release of adrenocorticotropic hormone (ACTH) from the pituitary gland and glucocorticoids (corticosterone in rodents and mainly cortisol in humans) from the adrenal gland, is triggered by a wide range of psychological experiences and physiological perturbations (stressors) [4]. During fetal life, the HPA axis is developing and therefore susceptible to prenatal programming influences [1]. Exposure to stressors during the prenatal and early postnatal periods (early life stress) is a key factor that can induce long-term effects on offspring health through changes in glucocorticoid action and metabolism [2•].
In non-stressful conditions, a marked circadian rhythm in circulating levels of glucocorticoids is observed in most mammals, with higher levels during the period of activity, irrespective of whether they are diurnal or nocturnal animals: higher corticosterone levels are found in the rat in the evening, whereas in humans higher cortisol levels are found in the morning, just after waking [4]. Eighty to 90% of serum cortisol is bound to corticosteroid-binding globulin (CBG), approximately 5 to 10% is bound to albumin, and only 5% is unbound [5]. Salivary cortisol is gaining interest in Psychoneurondocrinology as it is non-invasive and directly reflects the biologically active serum unbound cortisol level, in contrast to total plasma cortisol, which requires to know CBG levels to infer its biological impact [5].
Prenatal alcohol exposure (PAE) is a public health concern due to direct ethanol effects on the brain (and body) of the fetus, causing fetal alcohol spectrum disorder (FASD) in the offspring [6•]. The global prevalence of alcohol use during pregnancy is estimated to be 10% and causes FASD in 0.77% of the global population and 2.0–5.0% in Europe and North America [7, 8]. FASD is a serious public health problem associated with high economic burden, with the mean estimated annual per-person costs of care being $24,308 for adults and $22,810 per child [9]. Moreover, exposure to alcohol during the prenatal or early postnatal periods also constitutes an early insult to the organism [10] that might produce long-lasting physiological and behavioral consequences in the offspring [3]. Mental health consequences of PAE include an increased risk of ADHD, intellectual disability, anxiety, depression, and conduct problems [11,12,13]. PAE can induce direct changes in the fetus as well as indirect changes by altering maternal endocrine function, all these changes resulting in early life programming of the HPA axis, which has been well studied in animal models [1].
In rodents, the regular consumption of high doses of ethanol during pregnancy not only raises the set point of HPA function in the mother by increasing both basal and stress levels of corticosterone but may also result in HPA hyper-responsiveness to stressors in the offspring [3]. After weaning, ethanol-exposed animals show higher baseline corticosterone levels, increased HPA responsiveness to stressors and/or delayed post-stress recovery of baseline levels compared to controls [10]. However, some sex differences in this programming effect of PAE have been observed, which may also vary depending on the nature of the stressor, the time course, and the endocrine end-point measured [3].
Stress and disturbances of the HPA axis are thought to contribute to negative mental health consequences including a greater risk of depression [14], impulsivity and risky decision-making behavior [15], and alcohol use disorders [16]. Therefore, it could be speculated that PAE contributes to the risk of addiction behaviors and alcohol use problems by programming effects on the HPA axis.
The main aim of our study was to conduct a systematic review on the effects of PAE on the HPA axis activity of the human offspring. We aimed to study both baseline and responsiveness measures.
Methods
Search Strategy
A systematic search was performed using PubMed (Medline), Scopus and PsycInfo (until June 2020). The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines were followed [17]. The following search terms were used: (alcohol OR ethanol) AND (pregnancy OR prenatal OR fetus OR fetal) AND (cortisol OR corticosterone OR corticotrop* OR ACTH OR HPA OR hypothalamic-pituitary-adrenal).
Inclusion and Exclusion Criteria
Studies were only included if they met the following hierarchical inclusion criteria: (1) cross-sectional or longitudinal (observational or experimental) studies conducted in humans that included information of alcohol exposure during pregnancy; (2) measurement of at least one HPA axis hormone in the offspring; (3) written in English or Spanish; (4) studies published between 1980 and June 2020.
The exclusion criteria were (1) other designs (case reports, systematic reviews), (2) lack of a control group (non-exposure or low alcohol exposure); (3) animal studies; (4) languages other than English or Spanish.
Data Collection and Extraction
The literature search, data collection, and extraction were conducted independently by two authors. Disagreements were solved by consensus. From the selected articles, we excluded those that did not meet our inclusion criteria or that met our exclusion criteria. Additionally, this systematic computerized search was completed by hand-checking studies through references of included studies and review articles on prenatal alcohol exposure and cortisol activity. The last search was conducted in June 2020.
Data Synthesis
A narrative synthesis of the included studies was performed. Studies will be grouped by ages of participants (infants/toddlers vs children/adolescents).
Results
A total of 1331 studies were identified, 764 in PubMed, 428 in Scopus, 158 in PsycINFO, and 1 through another source (hand-checking studies through references). After the removal of duplicates, titles that clearly did not include our study purpose were also removed. A total of 188 abstracts were retrieved for further scrutiny. Finally, 9 articles met our inclusion criteria and were included in this systematic review (Fig. 1).
The age of the participants differed between studies. Six out of 9 studies included infants or toddlers (from 3 days to 19 months), whereas 3 studies included children and adolescents (between 5 and 18 years old). All studies including infants or toddlers reported both baseline and reactivity cortisol measures, whereas in the studies with children and adolescents only baseline HPA axis measures were reported. In all studies, cortisol levels were measured in saliva (Table 1).
Studies Including Infants or Toddlers
The evaluation of alcohol consumption was retrospective in the studies by Ramsay et al. [18], Ouellet-Morin et al. [22•], and Jirikowic et al. [23] and prospective in the studies by Jacobson et al. [19], Haley et al. [20•], and Oberlander et al. [21]. As it can be seen in Table 1, the definitions of PAE differ between studies, which might use different cut-offs or instruments for defining alcohol exposure.
Three studies did not find significant differences in baseline cortisol in PAE subjects [18, 20•, 21], two studies reported higher cortisol levels in those infants with greater alcohol exposure [19, 23], while one study reported lower baseline cortisol in boys but not girls with PAE [22•]. In a recent study by Sarkar et al. [24•], both salivary ACTH and cortisol measures were determined in baseline conditions in the morning and evening. PAE children had a trend to higher ACTH levels in the morning and significantly higher levels in the evening, whereas cortisol levels were significantly higher at both times. No sex differences were evident.
The type of stressors also differed from studies. Three studies considered painful stressors such as routine inoculation [18], blood draw [19], or heel lance [21]. Three studies considered emotional stressors that include social interactions with the mother such as the still-face paradigm [20•, 23] or the unfamiliar situation [22•]. In these last two social stress experiments, the methodological approach was similar. First, there is a stage where the mother and child interact. Second, a stressful situation occurs: mother stopping the play and showing a still face (still-face paradigm); the appearance of a strange element in the room (clown woman, noisy robot) in the unfamiliar situation paradigm. This stressful situation is followed by a lack of interaction between the mother and child. Finally, there is a recovery stage with the mother and child returning to the normal interaction. It is also important to note that the duration of the stressor is shorter for painful stressors (seconds) than for emotional stressors (2–4 min), depending on the procedure. Most procedures including emotional stressors last about 15–20 min.
In relation to cortisol response to painful stimuli, a blunted cortisol response was observed in babies exposed to heel lance at 3 days of age [21] or routine inoculation at 2 months of age [18]. However, in the latter study alcohol-exposed showed higher baseline pre-stress levels of cortisol, and it is unclear whether altered pre-stress levels could have interfered with the response to the stressor. Any group difference was significant at 6 months. In another study, no cortisol response to blood withdrawal was observed in 1-year-old infants of mothers with differential PAE, but higher baseline levels were observed when heavy versus low alcohol exposure groups were considered [19].
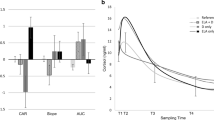
Two studies have analyzed potential sex differences in cortisol reactivity. Both reported a greater cortisol response in exposed versus non-exposed boys [20•, 22•]. However, in girls, no differences were found between exposed and non-exposed in one study [22•], whereas a blunted response in exposed girls was reported in another study [20•]. A final study did not assess potential sex differences, although included mostly female exposed participants (67%), and observed higher baseline cortisol levels in the PAE group, but a decrease during the still-face test, in contrast to the lack of changes in controls [23].
It appears that PAE increased baseline cortisol levels in infants, whereas it is unclear how the response to stressors is altered, mainly because the procedures elicited, if any, a mild cortisol response that can be confounded with the normal circadian rhythm. It cannot be ruled out higher pre-stress levels could interfere with the subsequent response to the acute stressor, particularly when the stressor is of low intensity.
Studies Including Children and Adolescents
Two studies included children and adolescents between 5 and 18 years old and retrospectively assessed PAE (Table 2). In the study by Keiver et al. [25], children with FASD participated in an 8-week motor skill development program with samples taken before and after the program. No influence of the program was found, but FASD children tended to show lower cortisol levels in the morning, but significantly higher levels in the afternoon and bedtime, and the effect appears to be restricted to those with higher levels of alcohol exposure. McLachlan et al. [26] studied a sample of PAE that included some subjects with FASD, and also evaluated early life adversity (ELA). As ELA was extremely frequent in PAE but not control group, they in fact studied the impact of PAE + ELA, showing a flattened slope from morning to evening levels of cortisol in the latter group, with a trend to lower levels in the morning and higher levels in the evening, in line with the previous study. Medication was also associated with lower morning cortisol concentrations.
Discussion
Our systematic review reveals that data are scarce and somehow contradictory, but nevertheless suggests that PAE may be associated with subtle abnormalities in HPA axis activity. In infants and toddlers, PAE seems to be associated with a blunted response to physical stressors whereas an enhanced cortisol response to social stress is detected in boys. In children and adolescents, an altered cortisol diurnal rhythm is observed in PAE participants with a FASD diagnosis, who show increased evening cortisol levels. All these findings are in accordance with the extensive evidence in animal models supporting the programming effects of alcohol on the HPA axis [27].
Although the included studies compared PAE vs non-exposed or low-exposed offspring, it is important to underscore that groups might also differ in other clinical variables (e.g., genetic vulnerability, comorbid use of other substances, psychopathology of the mother, malnutrition, and early postnatal stress) that might have an influence on HPA axis functioning. Tobacco use by mothers was present in most of the included studies. Some studies did not include the comorbid use of other substances during pregnancy [18, 20•, 25], or such data were not included in the statistical analysis [21, 23]. In one study, the criterion was to consume either alcohol, tobacco, or both [18]), and in the remaining work, the impact of consuming cocaine was also evaluated. In one study [19], reduced baseline cortisol levels were found in the offspring of mothers who were heavy cocaine users. A previous meta-analysis that compared the effect sizes of different prenatal adversities (stressful life events, alcohol, smoking, and other drugs) on the child cortisol secretion suggests a greater effect size for PAE [28].
A limitation of the works included in our systematic review is that other factors such as maternal malnutrition, which is closely linked to high levels of alcohol consumption, were not controlled. Animal studies point out that prenatal maternal malnutrition per se alters the activity of the HPA axis of the offspring under both baseline and stress conditions [29]. Another limitation is that most of the studies did not control for other early life adversities such as childhood abuse or neglect, which might be associated with blunted HPA axis responses [30, 31]. Preterm birth is another factor that might contribute to altered HPA axis responses including an increased basal secretion rate of cortisol and a blunted response to psychosocial stress [32]. Other potential confounders of HPA axis activity in the offspring are body-mass index [33] or anxiety, depressive or externalizing disorders [34], which might be associated with blunted cortisol responses. Therefore, it is important to take into account that other factors frequently associated with the PAE might also contribute to the altered HPA axis functioning in the offspring.
The greater HPA axis reactivity to social stress of PAE in boys might be considered a marker of the vulnerability of the offspring of women who have been exposed to alcohol during pregnancy.
The impact of PAE on the offspring is likely to involve multiple mechanisms as both ethanol and its main metabolite (acetaldehyde) can cross the placenta and have access to the fetus. Therefore, the drug can alter the mother’s physiological systems, including the endocrine and immune systems, as well as directly impact the fetus, being particularly relevant the direct effects on the developing brain of the fetus. Alcohol can directly alter neurotransmission, be toxic for neurons, in great part by enhancing oxidative stress, and affect epigenetic processes, including DNA methylation [35]. The precise mechanisms involved in the long-term effects of PAE on the HPA axis have been explored in animal models, but are still poorly known, although DNA methylation of HPA-related genes might be involved [27]. Interestingly, in one of the 9 studies that were included in our systematic review, higher DNA methylation of two genes (proopiomelanocorticortin [POMC] and period 2 [PER2]) was observed in both PAE mothers and children, which suggests that moderate to heavy alcohol use during pregnancy induces epigenetic marks to reduce the gene expression in POMC and PER2 genes of exposed children [24•]. It would be of great interest to know whether higher POMC gene methylation is also observed in the anterior pituitary, as the POMC peptide is the precursor of ACTH.
Early life adversity is another variable that might induce epigenetic changes that could contribute to the risk of mental illnesses and addiction behaviors during adolescence and adulthood [36]. In line with this hypothesis, previous studies including children of alcoholics have reported a blunted cortisol reactivity and increased methylation of the serotonin transporter (SLC6A4) gene [37]. One of the 9 studies included in our review suggests that early life stress is a moderator of HPA axis functioning, as children and adolescents with early life adversity show more pathological cortisol diurnal rhythms [26]. However, this study also suggests that protective factors (e.g., living in a quality, stable home) may buffer altered cortisol regulation, underscoring the need of an early assessment and intervention for PAE children.
The low number of studies exploring the relationship between PAE and HPA axis functioning in human populations when compared to the evidence from animal models is an important limitation. Cortisol reactivity to stress was mainly explored in infants and toddlers, although conclusions are hampered because the stressors used were of very low intensity and did not trigger a clear cortisol response. Studies that included children and adolescents did not assess HPA axis reactivity and future studies need to address this issue using ecologically relevant stressors. However, studies in children, but more particularly in adolescents, are still more complex than in infants, as previous studies suggest that children of fathers with an alcohol use disorder show a blunted cortisol response to stress [37, 38] and a greater risk to engage in risky substance use during adolescence [38]. In most of the studies including children and adolescents, PAE was equated to FASD diagnosis, whereas in studies including infants and toddlers, PAE was defined taking into account the level of alcohol intake by the mother. These different approaches make also more difficult to compare both types of studies, because the selection of FASD cases would include a more severe phenotype when compared to only considering levels of alcohol consumption during pregnancy. Therefore, longitudinal studies are needed following cohorts of PAE children to allow the study of different levels of outcome in terms of PAE and long-term consequences (no exposure vs PAE without a FASD vs PAE with a FASD). Moreover, more studies controlling the precise timing (first, second, or third trimester) and pattern (binge intake, spaced consumption) of ethanol intake are needed. It is also important that future studies explore HPA axis measures that have been less studied (e.g., ACTH concentrations, CAR), as well as to correlate HPA axis abnormalities with behavioral aspects.
None of the included studies measured cortisol levels in hair. Future studies might consider the addition of this HPA axis measure that is an index of long-term cumulative cortisol levels [39, 40]. Although there are no studies exploring whether PAE is associated with increased concentrations of cortisol of hair in the offspring, previous studies have reported an association between maternal trauma exposure during pregnancy and hair cortisol concentrations in the offspring at the age of 3 years [41].
Conclusions
Our systematic review showed some evidence for programming effects of PAE on the HPA axis in humans, although results in animal models and humans are not always concordant. Most studies in rodents are suggestive of enhanced baseline and stress-induced HPA activity, whereas the results in humans point to reduce responsiveness. However, both reduced and enhanced HPA activity might results in vulnerability to certain pathologies. The findings pointing to a negative effect of PAE on the HPA axis reactivity in the human offspring could be considered a neuroendocrine marker of vulnerability that could position those children to suffer from stress-related negative outcomes in the future, including a risk of psychopathology and addictive behaviors. Future studies are needed to explore whether these HPA axis abnormalities in PAE children are associated with an increased risk of alcohol consumption or mental health problems during adolescence and young adulthood.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Howland MA, Sandman CA, Glynn LM. Developmental origins of the human hypothalamic-pituitary-adrenal axis. Expert Rev Endocrinol Metab. 2017;12:321–39.
• Reynolds RM, Labad J, Buss C, Ghaemmaghami P, Räikkönen K. Transmitting biological effects of stress in utero: implications for mother and offspring. Psychoneuroendocrinology. 2013;38:1843–9. Important review summarizing the glucocorticoid programming hypothesis dealing with prenatal stress and offspring outcomes.
Zhang X, Sliwowska JH, Weinberg J. Prenatal alcohol exposure and fetal programming: effects on neuroendocrine and immune function. Exp Biol Med. 2005;230:376–88.
Armario A. The hypothalamic-pituitary-adrenal axis: what can it tell us about stressors? CNS Neurol Disord - Drug Targets. 2006;5:485–501.
Inder WJ, Dimeski G, Russell A. Measurement of salivary cortisol in 2012 - laboratory techniques and clinical indications. Clin Endocrinol (Oxf) [Internet]. 2012;77:645–651.
• Thibaut F, Chagraoui A, Buckley L, Gressier F, Labad J, Lamy S, et al. WFSBP * and IAWMH ** guidelines for the treatment of alcohol use disorders in pregnant women. World J Biol Psychiatry. 2019;20:17–50. Key guidelines on the managament of alcohol use disorders in pregnant women.
Wozniak JR, Riley EP, Charness ME. Diagnosis, epidemiology, assessment, pathophysiology, and management of fetal alcohol spectrum disorders. Lancet Neurol. 2019;18:760–70.
Popova S, Lange S, Probst C, Gmel G, Rehm J. Estimation of national, regional, and global prevalence of alcohol use during pregnancy and fetal alcohol syndrome: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e290–9. https://doi.org/10.1016/S2214-109X(17)30021-9.
Greenmyer JR, Klug MG, Kambeitz C, Popova S, Burd L. A multicountry updated assessment of the economic impact of fetal alcohol spectrum disorder: costs for children and adults. J Addict Med. 2018;12:466–73.
Hellemans KGC, Sliwowska JH, Verma P, Weinberg J. Prenatal alcohol exposure: fetal programming and later life vulnerability to stress, depression and anxiety disorders. Neurosci Biobehav Rev. 2010;34:791–807.
Easey KE, Dyer ML, Timpson NJ, Munafò MR. Prenatal alcohol exposure and offspring mental health: a systematic review. Drug Alcohol Depend. 2019;197:344–53.
Khoury JE, Jamieson B, Milligan K. Risk for childhood internalizing and externalizing behavior problems in the context of prenatal alcohol exposure: a meta-analysis and comprehensive examination of moderators. Alcohol Clin Exp Res. 2018;42:1358–77. https://doi.org/10.1111/acer.13805.
Weyrauch D, Schwartz M, Hart B, Klug MG, Burd L. Comorbid mental disorders in fetal alcohol spectrum disorders: a systematic review. J Dev Behav Pediatr. 2017;38:283–91.
Tafet GE, Nemeroff CB. The links between stress and depression: psychoneuroendocrinological, genetic, and environmental interactions. J Neuropsychiatry Clin Neurosci. 2016;28:77–88. https://doi.org/10.1176/appi.neuropsych.15030053.
van den Bos R, Harteveld M, Stoop H. Stress and decision-making in humans: performance is related to cortisol reactivity, albeit differently in men and women. Psychoneuroendocrinology. 2009;34:1449–58.
Lee RS, Oswald LM, Wand GS. Early life stress as a predictor of co-occurring alcohol use disorder and post-traumatic stress disorder. Alcohol Res Curr Rev. 2018;39:147–59.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339. https://doi.org/10.1136/bmj.b2535.
Ramsay DS, Bendersky MI, Lewis M. Effect of prenatal alcohol and cigarette exposure on two- and six-month-old infants’ adrenocortical reactivity to stress. J Pediatr Psychol. 1996;21:833–40.
Jacobson SW, Bihun JT, Chiodo LM. Effects of prenatal alcohol and cocaine exposure on infant cortisol levels. Dev Psychopathol. 1999;11:195–208.
• Haley DW, Handmaker NS, Lowe J. Infant stress reactivity and prenatal alcohol exposure. Alcohol Clin Exp Res. 2006;30:2055–64. This study explores the relationship between prenatal alcohol exposure and cortisol stress reactivity to an emotional stressor in the offspring.
Oberlander TF, Jacobson SW, Weinberg J, Grunau RE, Molteno CD, Jacobson JL. Prenatal alcohol exposure alters biobehavioral reactivity to pain in newborns. Alcohol Clin Exp Res. 2010;34:681–92.
• Ouellet-Morin I, Dionne G, Lupien SJ, Muckle G, Côté S, Pérusse D, et al. Prenatal alcohol exposure and cortisol activity in 19-month-old toddlers: an investigation of the moderating effects of sex and testosterone. Psychopharmacology. 2011;214:297–307. Largest study to explore the association between prenatal alcohol exposure and cortisol reactivity to an emotional stressor in the offspring.
Jirikowic T, Chen M, Nash J, Gendler B, Olson HC. Regulatory behaviors and stress reactivity among infants at high risk for fetal alcohol Spectrum disorders: an exploratory study. J Ment Health Res Intellect Disabil. 2016;9:171–88.
• Sarkar DK, Gangisetty O, Wozniak JR, Eckerle JK, Georgieff MK, Foroud TM, et al. Persistent changes in stress-regulatory genes in pregnant women or children exposed prenatally to alcohol. Alcohol Clin Exp Res. 2019;43:1887–97. This study exploring the contribution of prenatal alcohol exposure to stress measures in children and adolescents has included both salivary cortisol and salivary ACTH measures, and is the only study that has also included DNA methylation data in both mothers and offspring.
Keiver K, Bertram CP, Orr AP, Clarren S. Salivary cortisol levels are elevated in the afternoon and at bedtime in children with prenatal alcohol exposure. Alcohol. 2015;49:79–87.
McLachlan K, Rasmussen C, Oberlander TF, Loock C, Pei J, Andrew G, et al. Dysregulation of the cortisol diurnal rhythm following prenatal alcohol exposure and early life adversity. Alcohol. 2016;53:9–18.
Weinberg J, Sliwowska JH, Lan N, Hellemans KGC. Prenatal alcohol exposure: Foetal programming, the hypothalamic-pituitary-adrenal axis and sex differences in outcome. J Neuroendocrinol. 2008;20:470–88.
Pearson J, Tarabulsy GM, Bussières EL. Foetal programming and cortisol secretion in early childhood: a meta-analysis of different programming variables. Infant Behav Dev. 2015;40:204–15.
Léonhardt M, Lesage J, Dufourny L, Dickès-Coopman A, Montel V, Dupouy JP. Perinatal maternal food restriction induces alterations in hypothalamo-pituitary-adrenal axis activity and in plasma corticosterone-binding globulin capacity of weaning rat pups. Neuroendocrinology. 2002;75:45–54.
Kuras YI, Assaf N, Thoma MV, Gianferante D, Hanlin L, Chen X, et al. Blunted diurnal cortisol activity in healthy adults with childhood adversity. Front Hum Neurosci. 2017;11:574.
Carpenter LL, Carvalho JP, Tyrka AR, Wier LM, Mello AF, Mello MF, et al. Decreased adrenocorticotropic hormone and cortisol responses to stress in healthy adults reporting significant childhood maltreatment. Biol Psychiatry. 2007;62:1080–7.
Finken MJJ, van der Voorn B, Hollanders JJ, Ruys CA, de Waard M, van Goudoever JB, et al. Programming of the hypothalamus-pituitary-adrenal axis by very preterm birth. Ann Nutr Metab. 2017;70:170–4.
Ruttle PL, Javaras KN, Klein MH, Armstrong JM, Burk LR, Essex MJ. Concurrent and longitudinal associations between diurnal cortisol and body mass index across adolescence. J Adolesc Health. 2013;52:731–7.
Stadelmann S, Jaeger S, Matuschek T, Bae YJ, von Klitzing K, Klein AM, et al. Endocrinological and subjective stress responses in children with depressive, anxiety, or externalizing disorders. Dev Psychopathol. 2018;30:605–22.
Ehrhart F, Roozen S, Verbeek J, Koek G, Kok G, van Kranen H, et al. Review and gap analysis: molecular pathways leading to fetal alcohol spectrum disorders. Mol Psychiatry. 2019;24:10–7.
Cruceanu C, Matosin N, Binder EB. Interactions of early-life stress with the genome and epigenome: from prenatal stress to psychiatric disorders. Curr Opin Behav Sci. 2017;14:167–71.
Timothy A, Benegal V, Shankarappa B, Saxena S, Jain S, Purushottam M. Influence of early adversity on cortisol reactivity, SLC6A4 methylation and externalizing behavior in children of alcoholics. Prog Neuro-Psychopharmacology Biol Psychiatry. 2019;94:109649.
Evans BE, Greaves-Lord K, Euser AS, Thissen S, Tulen JHM, Franken IHA, et al. Stress reactivity as a prospective predictor of risky substance use during adolescence. J Stud Alcohol Drugs. 2016;77:208–19.
Russell E, Koren G, Rieder M, Van Uum S. Hair cortisol as a biological marker of chronic stress: current status, future directions and unanswered questions. Psychoneuroendocrinology. 2012;37:589–601.
Stalder T, Steudte-Schmiedgen S, Alexander N, Klucken T, Vater A, Wichmann S, et al. Stress-related and basic determinants of hair cortisol in humans: a meta-analysis. Psychoneuroendocrinology. 2017;77:261–74.
Slopen N, Roberts AL, LeWinn KZ, Bush NR, Rovnaghi CR, Tylavsky F, et al. Maternal experiences of trauma and hair cortisol in early childhood in a prospective cohort. Psychoneuroendocrinology. 2018;98:168–76.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Gender & Addiction
Rights and permissions
About this article
Cite this article
Díaz-Miranda, E., Nadal, R., Armario, A. et al. Prenatal Alcohol Exposure and Hypothalamic-Pituitary-Adrenal Axis Activity of the Offspring in Humans: a Systematic Review. Curr Addict Rep 8, 81–88 (2021). https://doi.org/10.1007/s40429-020-00349-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-020-00349-1