Abstract
Introduction
Dental caries is the most common chronic disease worldwide, and various forms of fluoride are considered useful preventive tools. The production of nanoscale materials can significantly improve their mechanical and chemical properties. The present study compared the microhardness of primary tooth enamel after applying sodium fluoride varnish (conventional) and nano-sodium fluoride varnish.
Materials and methods
Sixty-eight sound canine teeth were selected in this experimental study. The teeth were mounted so that the buccal surface was exposed. A 3 × 3 mm square was obtained on the buccal surface of the crown of each tooth. Enamel surfaces were polished using sandpaper in the presence of water as a coolant. The samples were randomly divided into four groups (n = 17): G1, conventional 5% NaF; G2, 1% nano-NaF; G3, 5% nano-NaF; G4, control. The initial microhardness was measured. Before surface treatment with different fluoride compounds, the samples were placed in a demineralizing solution for two days, and the microhardness of all the samples was re-measured. Then G1, G2, and G3 were treated with the fluoride type specified for each group, and G4 was treated as a control (without treatment). Finally, pH cycling was applied, and the microhardness was measured again. Data were analyzed with SPSS 20, using Repeated measure ANOVA and post-hoc Tukey tests. P < 0.05 was considered significant.
Results
Repeated measure ANOVA showed that microharness of G1, G2, G3, and G4 was statistically significant different. Tukey tests showed that the microhardness of G1, G2, and G3 were not significantly different. However, these three groups exhibited significantly more microhardness than the control group (P = 0.024, P = 0.027, and P = 0.010).
Conclusion
There was no significant differences in enamel microhardness of deciduous teeth between conventional 5% NaF,1% nano-NaF and 5% nano-NaF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dental caries, the most prevalent chronic dental disease worldwide, affects 60–90% of school-aged children and a significant number of adults (Al Dehailan et al. 2016). Since dental caries is a multifactorial disease, many etiologic factors, such as diet, microorganisms, and host, play a role in the dental caries process (El-Desouky et al. 2021).
Early childhood caries is still one of the most prevalent and rapidly advancing microbial diseases worldwide, leading to tooth destruction and pain, increasing the risk of dental caries in the permanent teeth, and adversely affecting the children’s and their caregivers’ quality of life.
Recent treatments focus on remineralizing agents on incipient caries (Abdil-nafaa and Qasim 2020). Treatment of dental caries, especially in children, may require advanced skills and higher general anesthesia costs for patient management. Prevention is the most effective method for reducing dental caries and is more cost-effective than treatment (Molaasadolah et al. 2017). Based on preventive dentistry, fluoride used locally and systemically is the most effective strategy to prevent carious lesions.
Deciduous tooth enamel is thinner, more fragile, and softer due to having half the thickness of permanent teeth, less mineral content and higher organic matter, and more susceptibility to caries (Abdil-nafaa and Qasim 2020; Mohammadi and Far 2018) as well as less microhardness than permanent tooth enamel and absence of the typical crystalline structure on the outermost layer of deciduous tooth enamel (Tabari et al. 2013). Therefore, fluoride application is crucial to preventing the development and progression of caries in deciduous teeth (Al Dehailan et al. 2016; Mohammadi and Far 2018). Microhardness measurements of enamel can be evaluated by two different parameters, Knoop hardness number, and Vickers hardness number (Ten Cate 2004). The Vickers microhardness test (VMHT) is commonly employed to evaluate the hardness of materials using microhardness test loads, usually ranging from 1 to 1000 g. A square pyramid is utilized by VMHT to make a small impression on the tooth surface by applying a predetermined load for a specific period. Following a microscopic examination of the indentation, the microhardness number is computed using the indentation load and the area of the remaining impression (Sahiti et al.2020). The residual indentation created by VMHT forms a square shape that is simple and precise to measure using a microscope (Sandeep et al 2015).
The local application of fluoride has been demonstrated to be the most important method in reducing the occurrence and prevalence of caries. Fluoride interrupts the demineralization process, strengthens remineralization, inhibits bacterial enzymes present in dental plaque (Al Dehailan et al. 2016), and replaces hydroxide ions in hydroxyapatite with fluoride ions, which results in the formation of acid-resistant hydroxyfluorapatite crystals (Kooshki et al. 2019). Today, a wide variety of professionally applied topical fluoride products, including mouthwashes, gels, foams, drops, and varnishes, are available. Fluoride varnishes have several advantages over other topical fluoride treatments, such as effectiveness, relative safety, and ease of application (Al Dehailan et al. 2016).
Due to its sticky nature, it can remain in contact with the tooth surface for several hours, preventing new caries and the spread of previous caries. Fluoride varnish is a safe way to protect teeth and provides the highest and safest fluoride concentration. Children are at greater risk for swallowing fluoride gels and mouthwashes. Fluoride varnish appears to be a good local fluoride treatment (Kooshki et al. 2019).
In recent years, studies on nano compounds aimed to produce effective formulations to reduce the loss of minerals and increase the absorption of minerals (Danelon et al. 2015; Nozari et al. 2017). Nanotechnology is the engineering science and technology that entails synthesizing and applying materials with nanoscale shape and size. The development of nanomaterials for medical care is a significant branch of nanotechnology. Nanomaterials have unique physical properties such as homogeneity, conductivity, or special optical properties, making them proper materials in biology and materials science. Due to their high surface-to-volume ratio, nanomaterials exhibit different biomedical activities compared to materials with normal sizes (Yin et al. 2020).
Studies have shown that excessive fluoride consumption is associated with many skeletal, cardiovascular, and neurologic disorders and thyroid hormone imbalances. Today, fluoride therapy has raised major concerns about chronic toxicity potential, usually manifested as dental fluorosis. Since children may not be able to perform or understand the importance of emptying their mouth after topical fluoride application, it leads to repeated ingestion of small amounts of fluoride (Kheradpisheh et al. 2018; Mohammadi et al. 2017; Yousefi et al. 2018). Therefore, if the effectiveness of fluoride therapy in the enamel’s resistance against the progression of caries increases, it might be possible to reduce dental visits’ frequency for fluoride and achieve better results in preventing tooth caries.
Considering the high effectiveness of 1–5% nano-NaF, Jahanimoghadam et al. showed that it might be possible to reduce the fluoride dose for each dental session and achieve better results in preventing caries progression. Increasing the time intervals between fluoride therapy sessions is another advantage of nano-sodium fluoride, and for young children who do not cooperate properly is very crucial. This method might improve the cost-effectiveness of routine fluoride therapy sessions and make the treatment available to the public (Jahanimoghadam et al. 2023).
Several studies have been conducted on applying different materials, including nanosilver fluoride and nanohydroxyapatite, to increase the remineralization potential of incipient caries and prevent new caries (Danelon et al. 2015; El-Desouky et al. 2021; Nozari et al. 2017). Considering the effect of many nanoscale materials and since only one study evaluated the effect of nano-sodium fluoride on strengthening permanent teeth against dental caries (Fidya et al. 2015), and as there has been no research on the remineralization and measurement of the microhardness of the deciduous tooth enamel surface when nano-sodium fluoride is applied, Therefore, the objective of the present study was to determine the effect of nano-sodium fluoride (1–5%) on the microhardness of the deciduous tooth enamel surface in comparison with the application of conventional sodium fluoride varnish. The current study’s null hypothesis was that there was no significant difference in microhardeness of deciduous tooth enamel when comparing conventional and nano sodium fluoride varnish (1–5%).
Materials and methods
Preparation of samples
In this in vitro study, 68 primary canines without caries, restorations, hypoplasia, cracks, and wear were selected from children referred to the Department of Pediatric Dentistry, Kerman Faculty of Dentistry, and kept in buffered thymol solution. (pH = 7.0, 4 ºC) until used for the study. Before extraction, informed consent was obtained from the patients’ parents to use their children’s teeth for research.
The protocol of the study was approved by the Ethics Committee, Faculty of Dentistry, Kerman University of Medical Sciences, Kerman, Iran, under the code IR.KMU.REC.1400.569 and process No. 400000506.
The criteria for inclusion were children who needed extraction of deciduous canine teeth for therapeutic reasons, including orthodontics.They had not received topical fluoride during the last year, had no history of taking fluoride supplements, and their mothers did not use fluoride supplements during pregnancy.
At first, the enamel surface was examined under a magnifying glass for cracks, and the teeth with cracks were excluded from the study.
The teeth were mounted so that the buccal surface was exposed. A 3 × 3 mm square was obtained on the buccal surface of each tooth crown. The depth of the square separated from the teeth was 1 mm and only included tooth enamel. The enamel surfaces were ground flat with a silicon carbide disc (600-grit Al2O3 paper; Buehler Ltd,USA) for 20 s to eliminate the fluoride originally present in the outer layers of teeth and reduce inter-individual differences due to different oral environments. In this way, approximately 50–100 µm was removed from the surface enamel, which was prismless and mostly affected by the oral environment. Additionally, this process was monitored using a micrometer. Nano-sodium fluoride varnish was prepared in the Faculty of Pharmacy in Kerman by the Pharmaceutical Research Center in the Faculty of Pharmacy and in the Laboratory of Pharmaceutical Nanomaterials and Nanostructures.
Preparation of nano-sodium fluoride
This study is part of a series of studies being conducted in the process of patenting this nano sodium fluoride varnish. The effectiveness of enamel fluoride absorption using nano sodium fluoride varnish has been established based on the findings of the earlier study (Jahanimoghadam et.al 2023). The nano-fluoride varnish was prepared in the Laboratory of Nanomaterials and Nanostructures, Pharmaceutical Research Center, Kerman School of Pharmacy, Iran.
To make the varnish, ethanol was added to a carbomer powder or CMC (carboxymethyl cellulose) along with 3% or 6% mint plant extract. The mixture was placed on a stirrer (Heidolph Company, Germany) for 45 min, during which a few drops of 0.02 M NaOH solution and 0.01 g of chitosan (Merck Company, Germany) were added. The resulting solution was placed in the reflux system (Kimia Aghigh, Iran) to perform growth and nucleation processes. After adding certain amounts of sodium fluoride in specific weight concentrations, including 5%, 3%, 2%, and 1% under magnetic synchronous conditions at 30 °C for 2 h, the resulting gel was placed in the microwave (Samsung, Japan) at 300 watts for 6 min, and each time was immediately placed in an ultrasonic bath (Elma-ultrasonic, Germany) at 60 watts for 5 min To produce sodium fluoride nanostructures, reverse micelles were used as an aqueous solution of reactive raw materials that could be converted to insoluble nanoparticles. In this research, nanoparticles synthesized in micelles were obtained by various methods, including the hydrolysis of reactive raw materials using microwaves. Finally, solvent removal and subsequent calcination led to the production of the final product.
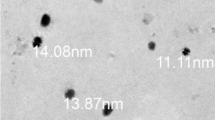
DLS (Dynamic Light Scattering) particle size analysis and SEM imaging are used to identify the prepared nanoparticles. FT-IR spectroscopy (Fourier-transform infrared spectroscopy) is also used to identify the chemical bonds in nanoparticles (Jahanimoghadam et al. 2023).
Surface treatment
The samples were randomly divided into four groups (n = 17). The initial microhardness was determined. Before the surface treatment with different fluoride compounds,the samples were incubated at 37 ºC for two days in a demineralizing solution, which was renewed every day: pH was adjusted to 4.4 using 1 M KOH, 0.05 M acetic acid, 2.2 mM NaH2PO4, and 2.2 mM CaCl2. A caries-like lesion was induced in the enamel samples. Then, the samples were washed with an artificial saliva syringe consisting of NaCl (2.9 g), CaCl2 (0.12 g), NaH2PO4 (0.13 g), NaN3 (5 mL) (2% ww) and placed in the artificial saliva container. Then, microhardness was determined again.
Group 1: In this group, 5% sodium fluoride varnish (Clinpro White Varnish, 3 M ESPE, USA) was used. Varnish application was carried out by cleaning the surface of the tooth with a special prophylaxis brush and dried with an air syringe. Then, the varnish was applied to the prepared enamel surface with a soft brush according to the manufacturer’s instructions (Kooshki et al. 2019) and the samples were incubated for 24 h in distilled water at 37 °C. Next, the varnish was removed from the surface of the samples with cotton dipped in 50% acetone (Merck Company, Germany) and washed with a syringe containing artificial saliva. The same procedures were carried out for the second and third groups, but instead of sodium fluoride, nano-sodium fluoride was applied with weight concentrations of 1–5%, respectively. The fourth group (control): No fluoride product was applied to the enamel samples in this group. The pH of the fluoride varnishes used in the study was determined at 7 by a pH Meter (Metrohm Company, PL-700PV, Indonesia). The samples were placed in a pH cycler for 24 h to simulate the oral environment.
In each cycle, the demineralization solution was applied for 3 h, followed by rinsing and immersion in distilled water for 30 min. Then, the remineralization solution (pH = 7, 0.15 M KCl, 0.9 mM NaH2PO4, 2.2 mM CaCl2) was applied for 21 h and rinsed and immersed in distilled water for 30 min. The same procedure was repeated every day for 10 days (Kooshki et al. 2019). Microhardness was also determined after surface treatment (Fig. 1).
Diagram of the experimental phase. A Primary canines kept in buffered thymol solution. (pH = 7.0, 4 °C). B The samples with a standardized area of 3 × 3 mm were obtained. C The initial microhardness of samples was determined.D The samples with different fluoride compounds were incubated at 37 °C for 2 days in a demineralizing solution which was renewed every day E A caries-like lesion was induced in the enamel samples and they were placed in the artificial saliva container. F Microhardness was determined after demineralization. G The samples were subjected to different treatments (G1 to G4). HThe samples were placed in a pH cycler for 24 h to simulate the oral environment for 10 days. I Microhardness was determined after remineralization
In this study, microhardness was measured by a Vickers hardness tester (Zwick Roell/ZHVμ, UK). Indentation was carried out at three points, under a force of 300 g and for 15 s, which resulted in three numeric values for each sample; then, the mean of these values was considered as the microhardness of each sample. The standard applied in the Vickers test was the ASTM E384-22 Standard Test Method for Microindentation Hardness of Materials (Hardness AB 1999).
Statistical analysis
The necessary parameters for determining the sample size were derived from previous studies (Godoi et al. 2019; Kooshki et al. 2019) and finally the sample size was determined based on the sample size formula for a one-way analysis of variance was as follows:
Power = P[F(1,N-K,α,λ) > F(1,N-K,α)]
Power = P[F(1,N-K,α,λ) > F(1,N-K,α)]
where \(\lambda =\frac{{\sigma }_{m}^{2}}{{\sigma }^{2}}\)\({\sigma }_{m}^{2}=\sqrt{\frac{{({\mu }_{i}-{\overline{\mu }}_{w})}^{2}}{K}}\). Therefore, considering α = 0.05, k = 4, σ2 = 10, and power = 0.9, with 338.73 and 327.07 as the lowest and highest mean of the groups, respectively, and a sample size of n = 17 for each group. The sample size was calculated with PASS based on the mentioned formula.
Data were analyzed with SPSS 20. Descriptive analyses were carried out in all the groups using means and standard deviations. Repeated Measure ANOVA and post-hoc Tukey tests were used to assess the changes of microhardness mean due to the normality and stability of variance. P < 0.05 was considered the significance level.
Results
The means and standard deviations of initial microhardness, microhardness after demineralization, and microhardness after remineralization in groups G1, G2, G3, and G4 was presented in Table 1.
Repeated measure ANOVA showed that the mean microhardness in all the groups decreased after demineralization and increased after remineralization (P < 0.001) and the mean of microhardness of four groups was significantly different (P = 0.039). Furthermore, post-hoc Tukey tests were used for two-by-two comparisons in overall microhardness between the groups (Table 2).
Discussion
One-way ANOVA showed that although the means of initial microhardness and microhardness after demineralization in groups G1, G2, G3, and G4 were not statistically significant, the differences in mean microhardness after remineralization between the groups were significant (P = 0.002). post-hoc Tukey tests were utilized for pairwise comparisons of the groups, revealing no significant differences in microhardness among G1, G2, and G3. However, G1, G2, and G3 were significantly different from G4, and the three fluoride groups showed higher microhardness than the control group (G4). The enamel surface layer plays a significant role in the caries process (Molaasadolah et al. 2017). Microhardness test is a common method to investigate changes in tooth enamel surface after demineralization and remineralization cycles (Mohammadi and Far 2018).
Microhardness assessment is a simple, rapid, and non-destructive method capable of repeated measurements. Many techniques, including the VMHT, can measure enamel microhardness. This method has high accuracy, quantitative measurement capability, the possibility of applying force with different sizes and re-measuring the hardness of samples in a certain period, and it is suitable for determining the hardness of very fragile materials such as tooth structure (Meshki et al. 2021; Molaasadolah et al. 2017). Therefore, the Vickers test was used in this study. pH cycle by creating acid challenges helps stimulate the dynamics of remineralization–demineralization of the oral environment in vitro (Azadi et al. 2021; Meshki et al. 2021; Molaasadolah et al. 2017).
Nanomaterials possess good bioavailability and bioactivity and high reactivity. Therefore, these particles have excellent surface adhesion and strong protein binding. As an experimental material, nano-sodium fluoride has greater penetration into enamel and dentin due to the small size of nanoparticles (Fidya et al. 2015). The preparation of nano-sodium fluoride was carried out with the method described by Jahanimoghadam et al. (2023). Many in vitro studies have compared the effect of different materials on increasing the microhardness of tooth enamel, both on extracted human permanent teeth or animal teeth (Godoi et al. 2019; Kooshki et al. 2019; Oliveira et al. 2019). Due to the differences in the structure of deciduous and permanent teeth, a similar study on deciduous teeth is possible. In vitro studies enable inexpensive, rapid, yet exact evaluation of any innovation in a highly controlled environment, which is a key component in validating product activity.
Surface microhardness is an indirect method that complements direct measures of mineral gain and loss (Nadar et al. 2022). The effect of nano-sodium fluoride on the microhardening of deciduous tooth enamel has not been examined, so the present study compared the microhardness of deciduous tooth enamel after applying sodium fluoride varnish (conventional) and nano-sodium fluoride varnish. In this study, fluoride varnish was considered as a reference since it is safe and well tolerated by children (Al Dehailan et al. 2016; Kooshki et al. 2019). Additionally, the American Academy of Pediatric Dentistry (AAPD) recommends its application for children < 6 due to its effectiveness in preventing dental caries in children at high caries risk (American Academy of Pediatric Dentistry 2013). Also, Azadi et al. reported that fluoride varnish is better than fluoride mouthwash and toothpaste in enhancing the microhardness of incipient caries in deciduous teeth (Azadi et al. 2021). Oliveira et al., in the microscopic analysis, reported that the calcium fluoride layer created by fluoride varnish was more uniform and less rough than a fluoride gel (2019).
Several studies have examined the effects of fluoride varnish on the remineralization of incipient caries. Their results showed that the microhardness of tooth enamel increases after the application of different concentrations of fluoride varnish (Azadi et al. 2021; Kooshki et al. 2019; Meshki et al. 2021;Molaasadolah et al. 2017; Mohammadi and Far 2018), consistent with the present study. The increase in microhardness of tooth enamel varies depending on the study method, different demineralizing and remineralizing solutions, and the type of varnish used. 5% sodium fluoride varnish (Clinpro White Varnish, 3 M ESPE, USA) applied in this study contains functional tricalcium phosphate (Bhadoria et al. 2020; Godoi et al. 2019; Tuloglu et al. 2016). Tricalcium phosphate is derived from the combination of beta-calcium phosphate with sodium laureth sulfate (Bhadoria et al. 2020; Godoi et al. 2019), which activates enamel remineralization, increases the deposition of minerals on the surface of tooth enamel, and boosts the remineralization of the subsurface lesion body by releasing calcium and phosphate ions in saliva (Godoi et al. 2019). Adding tricalcium phosphate to fluoride toothpaste increases fluoride binding to enamel and dentin and facilitates remineralization (Tuloglu et al. 2016). Al-Amoudi et al. compared the effects of 5% sodium fluoride varnish with tricalcium phosphate (Clinpro White) and conventional 5% sodium fluoride varnish (DuraShield) on the microhardness of deciduous tooth enamel and showed that adding tricalcium phosphate significantly improved the protective quality of fluoride varnish (AlAmoudi et al. 2013). Bhadoria et al. reported that tricalcium phosphate paste had higher remineralization potential than CPP-ACP with fluoride (2020).
In the present study, despite functional tricalcium phosphate in Clinpro White fluoride varnish, the microhardness of nano-sodium fluoride, even at 1% concentration, was higher than Clinpro fluoride varnish, which is in line with the finding that the presence of CPP-ACPF nanocomplexes and combination with fluoride would explain the superior ability of MI varnish compared to Clinpro White fluoride varnish in inhibiting demineralization (Nadar et al. 2022). The CPP-ACPF consists of amorphous electroneutral nanocomplexes, and their hydrodynamic radius allows rapid diffusion out of the varnish to enter the porosities of an enamel subsurface lesion through intraprismatic spaces, favoring remineralization (Nadar et al. 2022).
Several studies have tested the fluoride varnish compared to nanosilver fluoride in deciduous teeth. El-Desouky et al. (2021) reported that nanosilver fluoride (NSF) and fluoride varnish were effective in resisting enamel demineralization despite a higher percentage of microhardness changes and difference in lesion depth in the fluoride varnish group without significant difference. The protective effect of NSF can be explained by the very small particle size of AgNPs, which facilitates the penetration of the material into the tooth enamel structure and leads to the maximization of its protective effect.
Similarly, Teixeira et al. showed no significant difference between toothpaste containing NSF and sodium fluoride (NaF) toothpaste in preventing demineralization (Teixeira et al. 2018).
In this study, although NaF exhibited a lower percentage of microhardness changes, this can be explained by the different pH-cycle protocols and the frequent application of toothpaste slurry before each pH cycle, which can enhance the effect of the materials used.
Nozari et al. reported that the samples treated with nanosilver fluoride had the highest level of surface hardness compared to fluoride varnish and nanohydroxyapatite paste (n-HAP). NaF varnish and n-HAP paste were similar in incipient caries remineralization (2017). This finding might be due to the different design of the study, which focused on comparing the remineralization of induced enamel carious lesions rather than the ability of the tested materials to prevent enamel demineralization.
In the present study, although the greater increase in microhardness after applying 5% nano-sodium fluoride (290.965 ± 48.406) and 1% nano-sodium fluoride (282.818 ± 51.911) compared to the conventional 5% sodium fluoride group (276.618 ± 53.281) was not statistically significant, the effect of nano-sodium fluoride is noticeable. This finding is not consistent with the results of Fidya et al. (2015), who reported no significant difference in the effects of nanoNaF to 5% NaF concerning enamel surface hardness, which could be due to the different preparation method of nano-sodium fluoride and using permanent teeth in that study.
Fidya et al. also investigated the fluoride content of enamel samples treated with NaF and nanoNaF- in permanent teeth subjected to demineralization and remineralization cycles to evaluate the resistance of permanent teeth against dental caries. They concluded that applying nanoNaF could increase fluoride and fluorapatite content compared to applying NaF (Fidya et al. 2015). These results are consistent with the findings of Jahanimoghadam’s study (Jahanimoghadam et al. 2023).
The present study employed the same nano-sodium fluoride production method as Jahanimoghadam’s and reported no significant differences in primary tooth enamel microhardness between the NanoNaF and NaF groups. This finding may be because despite the smaller particle size and easier penetration of nanoparticles, the in vitro-prepared NanoNaF has a production mechanism different from the more complex and advanced methods for NaF production in the industry.
Jahanimoghadam et al. reported no significant differences in fluoride element between samples treated with different concentrations of nano sodium fluoride (1–5%) (2023), consistent with our findings. This might help produce nano-sodium fluoride varnishes with very low fluoride concentrations that still exhibit high fluoride content and high microhardness when applied to the tooth structure, reducing the risk of potential toxicity related to fluoride ingestion during fluoride therapy sessions. In addition, it is possible to reduce dental visits for fluoride, which is beneficial in preventing caries in young, uncooperative children (Jahanimoghadam et al. 2016). Also, Jahanimoghadam et al. reported no significant difference in the amount of fluoride in sound enamel samples with demineralized enamel in each group, indicating the effectiveness of fluoride therapy before and after the onset of incipient caries (2023).
However, more in vitro studies are recommended to confirm these findings, especially in the oral cavity, to consider variables that cannot be simulated in the laboratory.
Since this study was in vitro, simulating oral functions such as swallowing and chewing was not possible. Also, due to the significant role of factors related to the remineralization process, such as the flow rate of saliva and the composition and buffering capacity of saliva, a complete simulation is not expected. More in-vitro and in-vivo studies are recommended to evaluate different aspects of enamel strength against caries after applying nano-NaF.
Conclusion
Considering the limitations of the present study, the following conclusions can be made:
-
Results from the invitro study indicated that there were no significant differences in enamel microhardness of deciduous teeth between conventional 5% NaF,1% nano-NaF and 5% nano-NaF.
-
The results of this invitro study revealed that 1% nano-NaF and 5% nano-NaF are effective as well as conventional 5% NaF regarding enamel microhardness of deciduous teeth.
-
Fluoride therapy in children can be conducted using nano sodium fluoride varnish.
References
Abdil-nafaa SA, Qasim AA. The effect of silver diamine fluoride and fluoride varnish on roughness of primary teeth enamel (an in vitro study). Al-Rafidain Dental Journal. 2020;20(2):296–307.
Al Dehailan L, Martinez-Mier EA, Lippert F. The effect of fluoride varnishes on caries lesions: an in vitro investigation. Clin Oral Invest. 2016;20:1655–62.
AlAmoudi SA, Pani SC, AlOmari M. The effect of the addition of tricalcium phosphate to 5% sodium fluoride varnishes on the microhardness of enamel of primary teeth. Int J Dentistry. 2013. https://doi.org/10.1155/2013/486358.
American Academy of Pediatric Dentistry. Guideline on fluoride therapy. Pediatr Dent. 2013;35(5):E165–8.
Azadi P, Sarlak H, Nourmohammadi S. Comparing enamel microhardness in decidous teeth with primary carious lesions after applying three fluoride containing materials in vitro. J Arak Univ Med Sci. 2021;24(2):256–67.
Bhadoria N, Gunwal MK, Kukreja R, Maran S, Devendrappa SN, Singla S. An in vitro evaluation of remineralization potential of functionalized tricalcium phosphate paste and CPP-ACPF on artificial white spot lesion in primary and permanent enamel. Int J Clin Pediatric Dentistry. 2020;13(6):579.
Danelon M, Pessan JP, Neto FN, de Camargo ER, Delbem AC. Effect of toothpaste with nano-sized trimetaphosphate on dental caries: in situ study. J Dent. 2015;43(7):806–13.
El-Desouky D, Hanno A, Dowidar K, Hamza SA, El-Desouky LM. Evaluation of the anticariogenic effect of nano silver fluoride on demineralization of enamel in primary teeth (an in vitro study). Alexandria Dent J 46(2):153–159. https://doi.org/10.21608/ADJALEXU.2020.20537.1017.
Fidya F, Rachmawati R, Effendi MC, Dewi NKAF. The effect of NAF 5% and NANONaF to the permanent tooth endurance toward dental caries. J Int Dent Med Res. 2015;8(2):34.
Godoi FA, Carlos NR, Bridi EC, Amaral FL, França FM, Turssi CP, Kantovitz KR, Basting RT. Remineralizing effect of commercial fluoride varnishes on artificial enamel lesions. Braz Oral Res. 2019;27:33.
Hardness AB. Standard test method for microindentation hardness of materials. ASTM Committee: West Conshohocken PA USA. 1999;384:399.
Jahanimoghadam F, Poureslami H, Shamsaddin H, Horri A, Khazaeli P, Mahvic AH. Effect of ER: Yag laser on sodium fluoride varnish uptake by primary tooth enamel: an in-vitro study. Fluoride. 2016;49(4):538.
Jahanimoghadam F, Gisour EF, Dehesh T, Hasheminejad J, Ranjbar M. A comparison of conventional sodium fluoride varnish and nano sodium fluoride gel regarding fluoride uptake into enamel of deciduous teeth: an in-vitro study with sem-edx analysis. Fluoride. 2023;56(1):41–54.
Kheradpisheh Z, Mirzaei M, Mahvi AH, Mokhtari M, Azizi R, Fallahzadeh H, Ehrampoush MH. Impact of drinking water fluoride on human thyroid hormones: a case—control study. Sci Rep. 2018;8(1):2674. https://doi.org/10.1038/s41598-018-20696-4. (PMID:29422493;PMCID:PMC5805681).
Kooshki F, Pajoohan S, Kamareh S. Effects of treatment with three types of varnish remineralizing agents on the microhardness of demineralized enamel surface. J Clin Exp Dent. 2019;11(7): e630.
Meshki R, Basir L, Rahbar N, Kazempour M. Comparison of the effect of fluoride gel and two toothpastes with different materials on remineralization of initial carious lesions in primary teeth. J Family Med Primary Care. 2021;10(9):3309.
Mohammadi N, Far MH. Effect of fluoridated varnish and silver diamine fluoride on enamel demineralization resistance in primary dentition. J Indian Soc Pedod Prev Dentistry. 2018;36(3):257–61.
Mohammadi AA, Yousefi M, Yaseri M, Jalilzadeh M, Mahvi AH. Skeletal fluorosis in relation to drinking water in rural areas of west Azerbaijan. Iran Sci Rep. 2017;7(1):17300. https://doi.org/10.1038/s41598-017-17328-8. (PMID:29229915;PMCID:PMC5725489).
Molaasadolah F, Eskandarion S, Ehsani A, Sanginan M. In vitro evaluation of enamel microhardness after application of two types of fluoride varnish. J Clin Diagn Res: JCDR. 2017;11(8):ZC64.
Nadar BG, Yavagal PC, Velangi CS, Yavagal CM, Basavaraj SP. Efficacy of casein phosphopeptide-amorphous calcium phosphate varnish in remineralizing white spot lesions: a systematic review and meta-analysis. Dent Res J (Isfahan). 2022;19:48.
Nozari A, Ajami S, Rafiei A, Niazi E. Impact of nano hydroxyapatite, nano silver fluoride and sodium fluoride varnish on primary teeth enamel remineralization: an in vitro study. J ClinAnd Diagn Res: JCDR. 2017;11(9):ZC97.
Oliveira MR, Oliveira PH, Oliveira LH, Horliana AC, Cesar PF, Moura SK, Bussadori SK. Microhardness of bovine enamel after different fluoride application protocols. Dent Mater J. 2019;38(1):61–7.
Sahiti JS, Krishna NV, Prasad SD, Kumar CS, Kumar SS, Babu KSC. Comparative evaluation of enamel microhardness after using two different remineralizing agents on artificially demineralized human enamel: an in vitro study. J Clin Transl Res. 2020;6(3):87–91.
Sandeep T, Darshana D, Mithra HN. Comparative evaluation of effect of various remineralizing agents on bleached enamel surface: an in vitro study. J Pharm Sci Innov. 2015;4:324–8.
Tabari M, Alaghemand H, Rabiee M, Khefri S, Ahadi MS, Nikpour MR (2013) The effect of silicone oil and nano-hydroxyapatite/chitosan powder on microhardness and surface structure of primary teeth enamel after iron drop consumption. Journal of Dental School, Shahid Beheshti University of Medical Sciences. 31(3):138–47. “https://journals.sbmu.ac.ir/dentistry/article/view/29106”
Teixeira JA, Santos Júnior VE, MeloJúnior PC, Arnaud M, Lima MG, Flores MA, Stamford TC, Dias Pereira JR, Ribeiro Targino AG, Galembeck A, Rosenblatt A. Effects of a new nano-silver fluoride-containing dentifrice on demineralization of enamel and Streptococcus mutans adhesion and acidogenicity. Int J Dentistry. 2018;8:2018. https://doi.org/10.1155/2018/1351925.
Ten Cate JM. Fluorides in caries prevention and control: empiricism or science. Caries Res. 2004;38(3):254–7. https://doi.org/10.1159/000077763.
Tuloglu N, Bayrak S, Tunc ES, Ozer F. Effect of fluoride varnish with added casein phosphopeptide-amorphous calcium phosphate on the acid resistance of the primary enamel. BMC Oral Health. 2016;16(1):1–7.
Yin IX, Zhao IS, Mei ML, Li Q, Yu OY, Chu CH. Use of silver nanomaterials for caries prevention: a concise review. Int J Nanomed. 2020;6:3181–91.
Yousefi M, Yaseri M, Nabizadeh R, Hooshmand E, Jalilzadeh M, Mahvi AH, Mohammadi AA. Association of hypertension, body mass index, and waist circumference with fluoride intake; water drinking in residents of fluoride endemic areas. Iran Biol Trace Element Res. 2018;185:282–8.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jahanimoghadam, F., Gisour, E.F., Ranjbar, M. et al. A comparison of conventional sodium fluoride varnish and nano-sodium fluoride varnish regarding enamel microhardness of deciduous teeth: an in-vitro study. Eur Arch Paediatr Dent (2024). https://doi.org/10.1007/s40368-024-00942-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40368-024-00942-2