Abstract
Purpose
This study aimed to analyze, through a hierarchical model, the risk factors associated with the recurrence of chemo-induced oral mucositis (OM) in children and adolescents.
Methods
A retrospective cohort with 31 individuals of both sexes, aged 1–18 years, who were undergoing chemotherapy, and presented OM lesions was conducted. Data collection included analysis of medical records, interviews, and intraoral examination. Information regarding patients’ socioeconomic and demographic profile, underlying disease, antineoplastic regimen, hematological condition, and oral health status were collected. To assess the association of independent variables with the outcome, the Chi-square, Fisher’s Exact, and Mann–Whitney tests were used, in addition to a binary logistic regression model, with a maximum error of 5% and a 95% confidence interval.
Results
Significant associations were observed between the history of OM and the diagnosis of the child/adolescent, neutrophil count, previous cancer treatments and the chemotherapy scheme in use (p < 0.05). Binary logistic regression revealed a 13.69 higher risk of developing OM recurrence in individuals who received high-dose methotrexate (MTX) therapy.
Conclusion
Socioeconomic and demographic factors did not influence OM recurrence. However, clinical variables, such as neutropenia, diagnosis of leukemia, and high-dose MTX protocols increase the chance of OM new cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chemotherapy (CT) is the most used therapy in the treatment of children and adolescents with cancer (Hendrawati et al. 2019; Gabriel et al. 2021). However, severe oral complications can arise depending on the type, dosage, and use frequency of chemotherapeutic agents. CT can be associated with multiple side effects that negatively interfere with the patient's quality of life, being oral mucositis (OM) is one of the most important and frequent antineoplastic treatment complications (Curra et al. 2018; Parra et al. 2019).
OM refers to erythematous or ulcerated lesions that can affect oral mucosa during cancer treatment, especially when the patient is submitted to certain CT schemes, such as protocols with methotrexate (MTX), 5-fluorouracil or cytarabine (Curra et al. 2021; Gabriel et al. 2021; Nakagaki et al. 2022; Hafner et al. 2023).OM signs and symptoms can include erythema, pain, changes in taste, hyposalivation, ulcerations, and bleeding. Pain associated with OM can lead to difficulties in speech and swallowing, affecting oral feeding (Donohoe et al. 2018). The OM incidence and severity differ for everyone. However, it is estimated that the occurrence of OM in children and adolescents under CT can reach up to 80% (Damascena et al. 2020; Curra et al. 2021; Gabriel et al. 2021; Domico et al. 2022; Hafner et al. 2023).
OM is a multifactorial condition, and its development depends on aspects related to cancer therapy and individual characteristics. Treatment variables that can affect the appearance of new OM symptoms include the type, dose, and schedule of administration of chemotherapeutic agents. Among the factors associated with the patient, age, sex, body mass index, type of cancer, changes in salivary production, and oral health problems were reported as possible influencers in the development of new episodes of this condition (Shankar et al. 2019).
It is well established in the literature that with each new cycle of CT, new episodes of OM may appear. However, little is known about the reasons that potentiate the recurrences of this condition (Donohoe et al. 2018). Given the above, this study aimed to analyze, through a hierarchical model, the risk factors for the recurrence of chemotherapy-induced OM.
Materials and methods
This study was developed in compliance with the Helsinki Declaration, and it was approved by the local Research Ethics Committee Involving Human Beings (Approval Number: 3.494.189). Informed consent was obtained from all research participants.
A retrospective cohort was carried out between August and December 2019 in a pediatric oncology unit of a reference hospital in the treatment of childhood and juvenile cancer in the state of Pernambuco, Brazil. The convenience sample included children and adolescents of both sexes, aged 1 to 18 years, submitted to chemotherapy, and with OM (grade ≥ 2). Patients with oral solid tumors, the presence of fungal, bacterial, or viral infections clinically evident in the oral cavity, or individuals with severe systemic conditions that prevented their participation in the study were excluded from the sample.
The grading system used in the diagnosis of OM was the one recommended by the World health organization (WHO 1979), which graduates OM combining objective, subjective, and functional factors. To avoid false-positive diagnoses, only patients with OM grade ≥ 2 were included (Ye et al. 2013; Silva et al. 2018). The milestone for patient inclusion was grade 2 OM, characterized by the appearance of ulcers in the oral cavity, but with complete preservation of oral nutrition.
For data collection, semi-structured forms were elaborated, which sought to obtain information regarding the sociodemographic profile, the underlying disease, the type of cancer treatment, the hematological condition, as well as data on the oral health status. Information was obtained through patient/caregivers' reports, medical records evaluation, and patients’ clinical oral cavity assessment.
Patients’ oral health status was evaluated using the modified Visible Plaque Index (Mohebbi et al. 2008) and the Decayed, Missing, and Filled Index (DMFT/dmft) (Klein, Palmer 1937) for both permanent and primary dentition. The oral hygiene condition was considered as either good or bad, according to Mohebbi et al. (2008). Four trained and calibrated examiners evaluated all patients (intra and inter-examiner Kappa index of 0,90 and 0,82, respectively) and the clinical assessment was performed in the bed of inpatients at the beginning of each CT cycle.
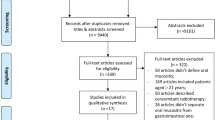
In addition, a hierarchical conceptual model was elaborated for this retrospective cohort study. The investigation of risk factors for a disease involves the collection of a considerable number of variables. Considering the possibility that one or more confounding variables may partially or totally explain the detected effect, it is essential to use a hierarchical model to identify independent risk factors.
Thus, the proposed model (Fig. 1) was outlined with the exposure variables divided into the following blocks: (a) distal social determinants—age, sex, skin color, family income, and parental education; (b) intermediate clinical–social determinants (indicators of access to the oral health service)—oral health status; (c) proximal determinants (biological and therapeutic factors)—hematological condition; type of cancer of the child/adolescent; chemotherapy scheme in use.
The results were expressed in tables with their respective absolute and relative frequencies. To verify the association between the studied variables, the Chi-square, Fischer Exact, and Mann–Whitney tests were used. Binary logistic regression was used to assess whether the proposed hierarchical model (Fig. 1) corresponded to the main risk factors for OM recurrence. Initially, simple models were made for each exposure variable, estimating crude association measures. In the case of therapeutic intervention, in addition to a simple model, adjusted models for age were also made since this factor is considered in the choice of individual therapies. Next, five models were evaluated, with successive addition of the variables of the determinant blocks. The nine variables present in the hierarchical model entered the multivariate model. All distal social determinants were included in multiple model 1. In multiple model 2, in addition to the significant distal social variables in model 1 (p < 0.05 in the Wald test), biological factors that reached p < 0.20 in simple models were included. Finally, in the other models, social determinants and significant biological factors that entered the previous model were included (p < 0.05), with the addition of therapeutic interventions with p < 0.20 in the simple models or in the models adjusted for age. Although the age variable was not significant in the simple model (p > 0.20), it was included in all multiple models to obtain age-adjusted measures of effect.
All tests were applied using a 95% confidence interval and a maximum error of 5%. The analyzes were performed in SPSS software, version 23.0 (SPSS Inc. Chicago, IL, USA).
Results
The study sample included 31 children and adolescents aged between 1 and 18 years old, of whom 67.7% were male, 58.1% were white, 80.6% had incomplete elementary school and 61.3% lived outside the state of Pernambuco. Regarding the characterization of caregivers and families, it was observed that 41.9% of caregivers had completed high school, 64.5% of families received up to 1 minimum wage per month and 61.3% of mothers had some type of paid occupation (Table 1).
When questioned about the family history of cancer, 67,7% of the sample reported having a family member affected by the disease. Regarding the diagnosis and treatment of the children and adolescents included, 61,3% were diagnosed with Leukemia, 71% had already undergone previous cycles of chemotherapy and 58,1% were receiving MTX in high doses as a chemotherapy protocol. The hematological parameters were out of the normal range in most of the research participants, noticing these abnormalities in 80.6% of the white blood cells and platelet count and in 67.7% of the neutrophils count. As for OM, 58.1% had already had previous episodes, 87.1% were diagnosed with cases of OM grade II at the time of the research, and 71% needed analgesic medication due to pain in the oral cavity (Table 2).
The perception of the oral health of children and adolescents was also investigated, showing that 32.3% reported gingival bleeding, 16.1% reported bad breath and bad taste in mouth and 29% had cutting edges in teeth. As for brushing frequency and flossing, 87.1% reported brushing up to 2 times a day and only 3.2% reported flossing daily. The Visible Plaque Index evaluation revealed that 90.3% of the sample had a poor oral hygiene condition. DMFT/dmft results showed that 67.7% of participants who had permanent dentition had a low caries index, as well as 29% of those with primary dentition (Table 2).
Among individuals with a history of recurrence of OM, 52.4% were female and the prevalence was higher in the group aged between 1 and 12 years, corresponding to 55.6% of children and adolescents who had new episodes of OM. Likewise, there was a greater prevalence of the history of OM among white individuals (72.2%), with a family income of up to one minimum wage (55%), with working fathers and mothers (68.2 and 63.2%, respectively) and living on an own home (54.5%). A greater number of OM recurrence cases occurred in participants who were not diagnosed with leukemia (83.3%), with altered hematological parameters, who brushed their teeth up to twice a day (55.6%), that used pain killers (63.6%), who had previously undergone cycles of chemotherapy (72.7%) and who were receiving MTX in high doses (88.9%). When Pearson's chi-square, Fisher's Exact and Mann–Whitney tests were applied, it was possible to observe significant associations between the history of OM and the diagnosis of the child / adolescent, the neutrophils count, previous oncological treatments, and chemotherapy scheme (p < 0.05), as seen in Table 3.
Binary regression analysis showed that the variables child/adolescent diagnosis (p = 0.025) and chemotherapy scheme (p < 0,001) maintained statistical significance. In addition, it was found that individuals who received a chemotherapy protocol with high doses of MTX were 13.69 times more likely to develop recurrences of oral mucositis (Table 4).
Discussion
Given the clinical impact associated with OM, it is important to understand which factors can influence its appearance and recurrence, to provide effective prevention and treatment options (Curra et al. 2018). However, clinical research in this field is challenging due to the large number of variables related to patients and treatment, in addition to the specific approach that the child and adolescent population demands (Allen et al. 2018).
When considering the gender and age of the participants in this research, there was no association between these variables and cases of recurrence of OM. This absence of association corroborates data from other studies, reinforcing that there is no relationship between the development of new cases of OM and the age or sex of the patient (Allen et al. 2018).
However, it is suggested that younger patients may develop more recurrent episodes of OM and with a more severe presentation than older patients. Chemotherapeutic agents usually have a predilection for poorly differentiated cells or for cells with high rates of cell turnover. Therefore, due to the rapid cell division observed in children and adolescents, it is believed that this population is more susceptible to a higher incidence and more severe cases of OM, but these same characteristics also favor a faster repair time of the lesions (Damascena et al. 2018). The failure to observe this difference in the present study is probably related to the age group used, since the sample was entirely composed of children and adolescents, excluding adult patients.
A less favored socioeconomic status and lower level of education are usually related to a greater number of oral diseases, which could increase the risk of the appearance of OM (Hendrawati et al. 2019). However, the results of this study showed that recurrent cases of OM are unrelated to education and family income, in accordance with previous studies (Murshid et al. 2017; Velten et al. 2017).
When analyzing the variables related to oral hygiene habits and the oral health profile of the studied population, it was observed that the data found did not present a statistical association when related to the recurrence of OM. Despite the absence of associations, most of the sample studied presented oral hygiene classified as poor, a fact that is frequently observed among children and adolescents diagnosed with cancer. Irregular oral hygiene habits may explain these findings, since the routine of health care for patients with cancer is complex and, sometimes, oral health is not seen as a priority (Ali, Nurelhuda 2019).
In addition, it is known that the reduction in salivary flow, a finding widely observed in patients undergoing chemotherapy, favors the accumulation of bacterial plaque in the oral cavity, potentializing the installation of oral diseases, especially when there is no professional monitoring (Decker et al. 2018; Parra et al. 2019). The literature also reports that maintaining good oral health throughout antineoplastic treatment can result in better oral status for these children, thus minimizing oral complications resulting from therapy that compromises the general quality of life of these patients (Kapoor et al. 2019).
Another relevant topic is the monitoring of hematological rates, a routine procedure during cancer treatment. The behavior of these rates, especially of neutrophil count, appears to be relevant in the appearance and recurrence of OM. In a study by Allen et al. (2018), it was observed that neutropenia is an important OM predictor. It was seen an association between the fall in neutrophil count and the appearance of OM injuries, with neutropenic children and adolescents subject to a 7.5 times greater risk of developing OM.
Inadequate neutrophil count or function may result in impaired ability to promote an adequate inflammatory response to the cytotoxic effects that chemotherapeutic agents cause on the oral mucosa, thus explaining the higher chance of occurrence of OM cases (Allen et al. 2018; Palomo-Colli et al. 2018). In this study, the bivariate analysis revealed a significant association between the neutrophil count and the history of OM. However, after applying the binary logistic regression model, the variable was unable to demonstrate its importance in explaining the outcome.
Children and adolescents with hematological neoplasms, especially leukemias, experience OM more frequently than those with solid tumors. It is mainly related to the disease treatment protocols, which commonly include drugs with a high potential for oral toxicity, such as cytarabine, etoposide, and MTX. Data show that individuals diagnosed with hematological malignancies have a seven times greater risk of developing OM (Carréon-Burciaga et al. 2018; Allen et al. 2018; Garrocho-Rangel et al. 2019). This study confirms these findings; however, it was not possible to verify statistical significance in our data after the application of the logistic regression model.
MTX is a key agent for the treatment of childhood and adolescent neoplasms, especially the hematological ones. High-dose MTX protocols can significantly increase cure rates and improve patients' prognosis, but the risk of complications also increases (Heil 2019). Research shows that chemotherapy regimens containing 5 g/m2 or more of MTX characterize high doses of the medication, being highly associated with side effects, such as MO (Sajith et al. 2019).
Scientific evidence shows the existence of a strong association between the administration of high doses of MTX and the risk of developing OM. In addition to causing damage to cancer cells, high-dose MTX therapy also causes damage to normal tissues, especially those characterized by high cellular renewal rates, as the oral mucosa (Alnuaimi et al. 2018; Garrocho-Rangel et al. 2019). The literature also suggests that the greater susceptibility to toxic effects related to MTX in some individuals can be explained by a genetic variation, altering the pharmacokinetics of the chemotherapeutic drug, and predisposing to the appearance of side effects (Oosterom et al. 2018).
The present study corroborates these statements, making it possible to demonstrate that patients who use this drug in high doses have a 13 times greater risk of developing OM recurrence. Therefore, although the management of toxicities associated with MTX in high doses remains a challenge (Sajith et al. 2019), it is recommended that individuals who use this drug protocol receive special attention, to establish preventive and therapeutic conducts for OM.
Ultimately, this study has some limitations; therefore, the results should be interpreted with caution—the sample size is small, and the sampling process was convenience-based. Consequently, the findings should not be extrapolated, and it is recommended that further studies on the recurrence of OM be conducted.
Conclusions
Considering the limitations of the present study, the following conclusions can be made regarding the studied sample:
-
Socioeconomic and demographic factors, such as sex, age, education, and family income, did not influence the recurrence of OM cases.
-
The presence of neutropenia and the diagnosis of leukemia influence the occurrence of new cases of OM.
-
Chemotherapy schemes with high-dose MTX significantly increased the risk of recurrent OM.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Ali MH, Nurelhuda NM. Oral health status and its determinants in children with Leukaemia at the radiation and isotope center Khartoum state, Sudan. Sudan J Paediatr. 2019. https://doi.org/10.24911/SJP.106-1568288518.
Allen G, Logan R, Revesz T, et al. The Prevalence and investigation of risk factors of oral mucositis in a pediatric oncology inpatient population; a prospective study. J Pediatr Hematol Oncol. 2018. https://doi.org/10.1097/MPH.0000000000000970.
Alnuaimi E, Al Halabi M, Khamis A, et al. Oral health problems in leukaemic paediatric patients in the United Arab emirates: a retrospective study. Eur J Paediatr Dent. 2018. https://doi.org/10.23804/ejpd.2018.19.03.11.
Carréon-Burciaga RG, Castañeda-Castaneira E, González-González R, et al. Severity of oral mucositis in children following chemotherapy and radiotherapy and its implications at a single oncology centre in Durango state. Mexico Int J Pediatr. 2018. https://doi.org/10.1155/2018/3252765.
Curra M, Soares Junior LAV, Martins MD, et al. Chemotherapy protocols and incidence of oral mucositis. Integr Rev Einstein. 2018. https://doi.org/10.1590/s1679-45082018rw4007.
Curra M, Gabriel AF, Ferreira MBC, et al. Incidence and risk factors for oral mucositis in pediatric patients receiving chemotherapy. Support Care Cancer. 2021. https://doi.org/10.1007/s00520-021-06199-5.
Damascena LCL, Lucena NNN, Ribeiro ILA, et al. Factors contributing to the duration of chemotherapy-induced severe oral mucositis in oncopediatric patient. Int J Environ Res Pub Health. 2018. https://doi.org/10.3390/ijerph15061153.
Damascena LCL, Lucena NNN, Ribeiro ILA, et al. Severe Oral mucositis in pediatric cancer patients: survival analysis and predictive factors. Int J Environ Res Pub Health. 2020. https://doi.org/10.3390/ijerph17041235.
Decker AM, Taichman LS, D’Silva NJ, et al. Periodontal treatment in cancer patients: an interdisciplinary approach. Curr Oral Health Rep. 2018. https://doi.org/10.1007/s40496-018-0164-4.
Docimo R, Anastasio MD, Bensi C. Chemotherapy-induced oral mucositis in children and adolescents: a systematic review. Eur Arch Paediatr Dent. 2022. https://doi.org/10.1007/s40368-022-00727-5.
Donohoe C, Bosi J, Sykes A, et al. Clinical characteristics of children and adolescents undergoing hematopoietic cell transplantation who develop oral mucositis. Oncol Nurs Forum. 2018. https://doi.org/10.1188/18.ONF.457-462.
Gabirel AF, Silveira FM, Curra M, et al. Risk factors associated with the development of oral mucositis in pediatric oncology patients: systematic review and meta-analysis. Oral Dis. 2021. https://doi.org/10.1111/odi.13863.
Garrocho-Rangel JA, Herrera-Moncada M, Márquez-Preciado R, et al. Oral mucositis in paediatric acute lymphoblastic leucemia patients receiving methotrexate-based chemotherapy: case series. Eur J Paediatr Dent. 2018. https://doi.org/10.23804/ejpd.2018.19.03.13.
Hafner D, Hrast P, Tomazevic T, et al. Photobiomodulation for chemotherapy-induced oral mucositis in pediatric patients. Biomolecules. 2023. https://doi.org/10.3390/biom13030418.
Heil SG. Genetics of high-dose methotrexate-induced oral mucositis: current perspectives. Pharmacogenomics. 2019. https://doi.org/10.2217/pgs-2019-0062.
Hendrawati S, Nurhidayah I, Mediani HS, et al. The incidence of mucositis in children with chemotherapy treatment. JNC. 2019;2(1):23–31.
Kapoor G, Goswami M, Sharma S, et al. Assessment of oral health status of children with Leukemia: a cross-sectional study. Spec Care Dent. 2019. https://doi.org/10.1111/scd.12419.
Klein H, Palmer CE. Dental caries in American Indian children. Pub Health Bull. 1937;25(6):996–8.
Mohebbi SZ, Virtanen JI, Murtomaa H, et al. Mothers as facilitators of oral hygiene in early childhood. Int J Paediatr Dent. 2008. https://doi.org/10.1111/j.1365-263X.2007.00861.x.
Murshid EZ, Azizalrahman TA, Aljoha AJ. Oral mucositis in leukemic Saudi children following chemotherapy. Saudi J Dent Res. 2017. https://doi.org/10.1016/j.sjdr.2016.10.004.
Nakagaki M, Kennedy GA, Gavin NC, et al. The incidence of severe oral mucositis in patients undergoing different conditioning regimens in haematopoietic stem cell transplantation. Support Care Cancer. 2022. https://doi.org/10.1007/s00520-022-07328-4.
Oosterom N, Berrevoets M, Hoed MAH, et al. The role of genetic polymorphisms in the thymidylate synthase (TYMS) gene in methotrexate-induced oral mucositis in children with acute lymphoblastic leucemia. Pharmacogenet Genom. 2018. https://doi.org/10.1097/FPC.0000000000000352.
Palomo-colli MA, Soltero-Becerril DC, Juarez L, et al. Oral mucositis in children with cancer and their relationship with limitation of activities. Gaceta Mexicana De Oncol. 2018. https://doi.org/10.24875/j.gamo.M19000167.
Parra JJ, Alvarado MC, Monsalve P, et al. Oral health in children with acute lymphoblastic leukaemia: before and after chemotherapy treatment. Eur Arch Paediatr Dent. 2019. https://doi.org/10.1007/s40368-019-00454-4.
Sajith M, Pawar A, Bafna V, et al. Serum methotrexate level and side effects of high dose methotrexate infusion in pediatric patients with acute lymphoblastic Leukaemia (all). Indian J Hematol Blood Transfus. 2019. https://doi.org/10.1007/s12288-019-01144-3.
Shankar A, Roy S, Bhandari M, et al. Current trends in management of oral mucositis in cancer treatment. Asian Pac J Cancer Preven. 2019. https://doi.org/10.22034/APJCP.2017.18.8.2019.
Silva VCR, Silveira FMM, Monteiro MGB, et al. Photodynamic therapy for treatment of oral mucositis: pilot study with pediatric patients undergoing chemotherapy. Photodiagn Photodyn Ther. 2018. https://doi.org/10.1016/j.pdpdt.2017.11.010.
Velten DB, Zandonade E, Miotto MHMB. Prevalence of oral manifestations in children and adolescents with câncer submitted to chemotherapy. BMC Oral Health. 2017. https://doi.org/10.1186/s12903-016-0331-8.
World Health Organization. WHO handbook for reporting results of cancer treatment. Geneva: World Health Organization; 1979. Series number 48.
Ye Y, Carlsson G, Agholme MB, et al. Oral bacterial community dynamics in paediatric patients with malignancies in relation to chemotherapy-related oral mucositis: a prospective study. Clin Microbiol Infect. 2013. https://doi.org/10.1111/1469-0691.12287.
Acknowledgements
The authors would like to thank the Oncohematology sector at Oswaldo Cruz University Hospital for allowing the study and the medical, dental, and nursing teams for contributing to its execution. We would also like to thank the Coordination for the Improvement of Higher Education Personnel (CAPES), for granting a scholarship during the development of this research.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
de Macêdo, T.S., de Melo, M.C.F., Ferreira, A.K.A. et al. Chemotherapy-induced oral mucositis: hierarchical analysis of recurrence factors. Eur Arch Paediatr Dent 25, 589–596 (2024). https://doi.org/10.1007/s40368-024-00919-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40368-024-00919-1