Abstract
Background
Untreated early childhood caries (ECC) can trigger a number of negative consequences, including pain, chewing difficulties, insufficient physical development and low academic performance. Therefore, ECC impacts the oral health-related to quality of life. That is why it is important to assess the ECC prevalence and to determine the associated risk factors.
Aim
The aim of this study was to investigate the relationship between early predictor factors and dental caries among 4-year-old French children, considering the socioeconomic factors, dietary and oral hygiene practices, the access and the follow-up by paediatric dentist.
Design
The study was a cross-sectional observation. A random sample of 4-year-old children was selected among 596 Moselle’s public nursery schools in north-eastern France. Data were gathered from clinical dental examinations and a structured questionnaire completed by parents.
Results
In total, 425 subjects with completed questionnaires and clinical examinations were included. The prevalence of ECC and S-ECC (Severe-ECC), including only cavitated lesions, d3mft, were 15.8% and 5.9%, respectively. Multivariable logistic regression modelling identified four main factors associated with a high risk of ECC that were sweet intake (adjusted odds ratio ORadjusted = 3.43, 95% CI = 1.57–7.53), brushing habits (ORadjusted = 2.25, 95% CI = 1.23–4.21), childcare arrangement (ORadjusted = 2.27, 95% CI = 1.23–4.21) and maternal educational level (ORadjusted = 1.87, 95% CI = 1.06–3.31). These four factors have a cumulative effect. Only 4% of children presented teeth restoration.
Conclusions
This study highlighted the impact of the family environment on the oral health status of the preschool children. The identification of the risk factors should allow to strengthen preventive measures and initiate oral health education program for children and their family.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Early childhood caries (ECC) remains a public health problem affecting a large number of children worldwide. ECC has been described as a chronic, dynamic, progressive infectious disease (Edelstein 2006). Caries is also characterised as a “complex” disease due to combined actions of genetic, environmental, microbiological factors and risk-conferring behaviours (Fontana and Wolff 2011). Dental caries development results from an imbalance of multiple risk factors and protective factors over time.
Following the American Academy of Pediatric Dentistry (Latest revision 2016), ECC is defined as “the presence of one or more decayed (non-cavitated lesions), missing (due to caries), or filled tooth surfaces” in any primary tooth in a child under 6 years of age. In children younger than 3-year-old, any sign of smooth-surface caries is indicative of severe early childhood caries (S-ECC). From ages 3 through 5, one or more cavitated, missing (due to caries), or filled smooth surfaces in primary maxillary anterior teeth or a decayed, missing, or filled score of ≥ 4 (age 3), ≥ 5 (age 4), or ≥ 6 (age 5) surfaces constitutes S-ECC (Drury et al. 1999).
Untreated ECC can trigger a number of negative consequences, including pain, chewing difficulties, reduced appetite leading to insufficient physical development especially weight loss and height growth delay. Low academic performance secondary to sleep problems, behavioural alteration and loss of school days were described. Indeed, Edelstein et al. (2006) showed that 86% of families reported that cavities interfered with their child’s ability to eat; 50% reported that it affected their child’s ability to sleep; and 32% reported that it affected their child’s ability to participate in school activities. Therefore, ECC impacts the oral health-related to quality of life.
Not many studies have assessed the caries situation of preschool children in France (Edelstein et al. 2006; Enjary et al. 2006; Tubert-Jeannin et al. 2008; Droz et al. 2006). This study aimed to investigate the relationship between early predictor factors and dental caries among 4-year-old children, considering the socioeconomic factors, dietary and oral hygiene practices, the access to healthcare and the follow-up by paediatric dentist.
Materials and methods
Study design
The study was a cross-sectional observation. A random sample of 4-year-old children was selected among 11,572 children in 596 Moselle’s public nursery schools in north-eastern France. The two-thirds of the population of this region (Moselle; 1044,486 inhabitants) are living in urban areas (724,146 inhabitants, 69.3%) and one-third in rural area (320,340 inhabitants, 30.7%).
The sample size estimation was based on the caries prevalence of 4-year-old children. The overall anticipated prevalence would be around 33%. The desired precision of estimation was set as 5%. With the confidence interval set as 95% (alpha = 0.05), 489 children were needed in this study.
The present investigation was based on a structured questionnaire completed by parents and a clinical examination. Our investigation was conducted at the mean time that the general examination of the French children performed at 4 years by health care professionals of the Department of Mother and Child Protection Services (nurse or doctor) in 2018.
The data collection was organised by department of Mother and Child Protection (MCP) Service of Moselle, using a questionnaire and an individual chart completed clinically onsite. Informed consent was obtained from the caregivers of the participants. The information could be crossed thanks to an anonymity number assigned to each child and noted on the questionnaire and the clinical observation sheet on the day of the child’s examination.
The study was approved by the Nancy–Metz regional education authority and the Ethical committee (protocol number: 18076-1232-18.08.21.60332). Written informed consent was obtained from the parents of the children.
Clinical examination
The clinical examinations were carried out by two examiners accompanied by a childcare nurse in each school. Examination equipment consisted of sterile single-use examination kits (mirror, probe, light and tongue depressor).
The training and calibration process included theoretical explanations and clinical examinations. Two experienced paediatric dentists supervised two examiners. During the examination, inter-examiner agreement was determined between the examiners and the experienced practitioners.
Dental caries was evaluated using the International Caries Detection and Assessment System (ICDAS). This index is used to evaluate caries beginning with the initial stage (white spot) and cavities (Pitts and Ekstrand 2013). In our study, code 1 was not used because air drying of the teeth cannot be performed and the teeth presenting a code 2 were noted d1t and the teeth with cavitated lesions (code 3–6) were noted d3t.
The dmft index (decayed, missing and filled primary teeth) was used to determine the severity of EEC according to the AAPD guidelines (American Academy of Pediatric Dentistry 2019–2020). ECC was diagnosed if 5 > d3mft ≥ 1. Severe-ECC (S-ECC) was assigned to children with d3mft ≥ 5. Teeth missing due to trauma or early exfoliation were excluded.
Dental structure abnormalities (enamel hypoplasia and deciduous molar hypomineralisation (DMH)) were researched but not analysed in this paper.
Dental plaque score was defined as visible on probing or naked eye. Bleeding score was defined as spontaneous or on probing.
Questionnaire
The questionnaire was translated into several languages (English, German, and Arabic) to (1) reduce linguistic barriers and maximise the participation rate and (2) not exclude children with migration background and obtain a representative population sample. It was transmitted to the families by the school teachers and retrieved during the general examination of the children by the nurses of the Department of maternal and child protection and health direction.
The questionnaire consisted of 5 sections, each of them included 4–13 questions, totaling 39 questions. It collected information related to family sociodemographic determinants, child oral health (tooth brushing habits, eating habits of the child and parents), parent’s knowledge of oral health dental, dental fear and access to dental oral health consultations.
Toothpaste category was defined as fluoridate (for adults or children), non-fluoridated or no toothpaste (Water). Brushing aid score from parents was defined as always, sometimes or never.
Residence area was defined as rural area, urban priority-education-network area or other urban areas.
Childcare arrangement is defined as childminder and child nursery, parents or grandparents.
Some items of the questionnaire were grouped together to obtain score.
-
Sweet intake score was defined as the cumulated number of the following factors (range 0–3): sweet consumption (≥ 1 per day), sweet drink (≥ 1 per day), and sweet drink at night after 1-year-old (breastfeeding, bottle). This score was dichotomised (1–3 vs. 0).
-
Tooth brushing score was defined as the presence of at least one of the two factors: beginning of regular brushing after 1-year-old or more or no regular brushing (vs. regular brushing since the first teeth appearance) and brushing rate (never or rarely vs. 1–2 times per day).
-
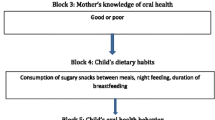
A risk score was defined as the cumulated number of four factors (range 0–4): sweet intake score, tooth brushing score, mother’s education and childcare arrangement.
Variables tested
The dependent variables were caries experience measured by d3mft index (3 levels: d3mft = 0, 1–4 and ≥ 5), dental plaque (2 levels: visible on probing, visible to naked eye), bleeding (2 levels: bleeding on probing, spontaneous bleeding). Our study assessed the associations of d3mft (dependent variable) with the following independent variables: gender (boy or girl), residency area (3 levels: rural, priory area, priority-education-network area, other urban areas), mother’s education (2 levels: university, bac or lower), childcare arrangement (3 levels: childminder and child nursery, parents, grandparents), sweet consumption (2 levels: < 1 per day, ≥ 1 per day), sweet drink (2 levels: < 1 per day, ≥ 1 per day), sweet drink at night after 1-year-old (2 levels: none or water, milk (including breastfeeding) and sweet drink), age at the beginning of regular brushing (3 levels: first teeth appearance, 1–2 years, > 3 years or no regular brushing), brushing rate (3 levels: 2 per day, 1 per day, never or rarely), toothpaste category (3 levels: fluoridated for adults or children, non-fluoridated, no toothpaste or water), brushing aid from parents (3 levels: always, sometimes, never), access to dentist (2 levels: no difficulty, with difficulty).
Statistical analysis
The associations between d3mft (dependent variable, categorised into 3 levels: 0, 1–4, and ≥ 5) with various risk factors were assessed using the Chi2 test (for qualitative variables) or variance analysis (for continuous variables). Then, we assessed the associations of d3mft 1–4 (vs. 0), d3mft ≥ 5 (vs. 0), and d3mft ≥ 1(vs. 0) (dependent variables) with various risk factors using age–sex-adjusted odds ratios (ORas) and 95% confidence intervals (95% CI) computed with logistic regression models. To identify most potential risk factors for d3mft \(\ge\) 1, a multivariable logistic regression model was used to compute adjusted odds ratios (ORadjusted) by considering only the factors significantly associated with at least one of the previous dependent variables (P < 0.05); in this analysis, the stepwise forward procedure was utilised to retain only significant factors (P < 0.05). For the factors retained, we verified their one-dimensionality by factor analysis and their internal consistency by Cronbach’s alpha, which allowed a single risk score to be calculated as their cumulated number. A P value < 0.05 (2-sided) was considered statistically significant. All statistical analyses were performed with the Stata software package (Stata Corporation, College Station, Texas, USA, 2011).
Results
Figure 1 shows the flow chart of study participants: among the 681 children included in our study, 425 subjects (boys 54.3%, girls 45.7%) with completed questionnaires and clinical examinations were retained for statistical analysis (Fig. 1). The children’s mean age was 4.4 years (SD = 0.23).
The characteristics of the sample are presented in Table 1. The subjects in rural area, priority-education-network area and other urban areas represented 38.8%, 30.1% and 31.1%, respectively. The majority (59.3%) of mothers had low school education level (high school diploma or less). Many children were cared by their parents or grandparents (44.2% and 19.5%, respectively). 21.7% of children presented a d3mft \(\ge\) 1. The prevalence of ECC and S-ECC were 15.8% and 5.9%, respectively. The mean d3mft (cavitated lesions) and d1mft (non-cavitated lesions) were 0.76 (SD = 2.07) and 1.46 (SD = 2.72), respectively. 38.32% of children presented a d1d3mft ≥ 1. Dental plaque was visible to naked eye in 15.8% and on probing in 37.6% of children.
Table 1 further shows oral health behaviours: 22.6% of children started regular brushing teeth at the eruption of the first primary tooth; 11,5% of children never or rarely brushed their teeth; 40.4% of children always received help from their parents for tooth brushing; 49,7% of children had their teeth brushed twice a day; 85.2% of children used a fluoride toothpaste and 54.3% of children took sweet drinks (including milk, breastfeeding, soft drinks, e.g. fruit juices, carbonated drinks) frequently at bedtime.
Table 2 shows that, based on ORas, the d3mft ≥ 1 was strongly associated with sweet consumption (≥ 1 per day, ORas = 1.69, 95% CI = 1.04–2.73), sweet drink (≥ 1 per day, ORas = 2.23, 95% CI = 1.38–3.60), and sweet drink at night (ORas = 2.47, 95% CI = 1.50–4.07). The d3mft ≥ 1 was also associated with starting-regular-brushing age: ORas = 2.46, 95% (CI = 1.20–5.06) for since 1–2-year-old and ORas = 4.27 (95% CI = 1.91–9.58) for after 3-year-old/no regular brushing (vs. brushing after the first teeth eruption only). An increased risk of d3mft \(\ge\) 1 was also found for the children who never or rarely brushed their teeth (ORas = 2.48, 95% CI = 1.24–4.93).
Children with access difficulty to dentist had a 3-times higher risk to develop dental caries (ORs = 2.97, 95% CI = 1.48–5.93). Compared with children in rural area, those in priority-education-network area and other urban areas had a high risk (ORs = 6.33, 95% CI = 3.28–12.2 and ORs = 3.38, 95% CI = 1.71–6.68, respectively). Low mother’s education was associated with a 3-times higher risk to develop dental caries (ORs = 2.97, 95% CI = 1.73–5.09). Father education was not significantly associated with d3mft. Compared with the children cared by childminder and child nursery, those cared by their parents and grandparents were clearly more at higher risk (ORs = 4.03, 95% CI = 2.19–7.41 and ORs = 2.48, 95% CI = 1.18–5.20, respectively). Most of these factors were associated with both ECC (1 > d3mft ≥ 4) and S-ECC (d3mft ≥ 5).
Multivariable logistic regression modelling with stepwise forward procedure retaining only significant factors revealed that among various significant risk factors for d3mft ≥ 1, only four factors had significant ORadjusted (pseudo R2 = 10.7%): sweet intake score (3.43, 95% CI = 1.57–7.53), tooth brushing score (2.25, 95% CI = 1.23–4.21), low mother’s education (1.87, 95% CI = 1.06–3.31), and childcare by parents and grandparents (2.27, 95% CI = 1.23–4.21). Principal component analysis showed that these four factors were unidimensional (1st eigenvalue (0.74) much higher than the 2nd eigenvalue (0.057)). These factors had Cronbach’s alpha = 0.51 which showed that they were complementary. We could thus compute a single risk score defined as their cumulated number (range 0–4). The proportion of children with risk score 0, 1, 2, 3 and 4 were 4.0, 13.2, 20.7, 29.2 and 32.9%, respectively. Mother’s dental fear was significantly associated with d1d3mft ≥ 1.
Figure 2 shows that the proportion of children with d3mft \(\ge\) 1 increased from 0% for risk score = 0–25.8% for risk score = 3, and to 36.4% for risk score = 4 (P < 0.001). We obtained similar results when investigating the d1d3mft (data not shown).
Regarding dental plaque, we found that it was associated with age at the beginning of regular brushing (ORas = 1.78, 95% CI = 1.11–2.83 for ≥ 1 year or no regular brushing, vs. brushing established after the first teeth eruption), child’s age (ORas = 2.65 per 1-year increase, 95% CI = 1.13–6.20) and living in urban area (ORas = 3.05, 95% CI = 1.88–4.95 for priority-education-network area and ORas = 3.18, 95% CI = 1.96–5.15 for other urban areas, vs. rural area). Bleeding was associated with age at the beginning of regular brushing (ORas = 3.00, 95% CI = 1.08–8.31 for ≥ 3 years or no regular brushing, vs. brushing established after the first teeth eruption).
Discussion
In our study, 38.32% of children presented a d1d3mft ≥ 1. Even though there was a significant prevalence of cavitated lesions (d3 = 18.4%) the greatest prevalence was due to non-cavitated lesion (d1 = 32.71%). Without preventive care and follow-up, this enamel demineralisation could progress to cavitated lesion.
Although representative data were sparse, studies reported that the prevalence of ECC in 3- to 6-year-old children is 10.5% (dmfs > 0) in Sweden (Holmen et al. 2018), 25.5% in England (Abed et al. 2020), 19% in southern Italy (Nobile et al. 2014), 13.2% in Australia (Goldfeld et al. 2019) and 14.7% in Japan (Kato et al. 2017). In these studies, the authors only considered the cavitated lesions to calculate the ECC prevalence. Furthermore, the populations studied may differ from our sample in age and socioeconomic and cultural features as well as in risk factors of dental disease. The exclusion of the questionnaires that were not completed appropriately may underestimate our results.
In addition, proximal lesion could be undiagnosed in absence of radiographic examination in patients who have not interdental diastema. According to the authors, radiographic examination increased caries prevalence by 10% or more compared to visual only examination (Cortes et al. 2019; Mendes et al. 2012; Mejare 2005).
Factors influencing dental health include the elements of the triad adapted from Keyes and are expressed at the individual, family, and community levels. Each factor must incorporate a multilevel perspective as the model built by Fisher-Owens et al. (2007).
Furthermore, other studies described confounding factors, such as brushing before bedtime, fluoride exposure and daily intake of free sugars (Baghlaf et al. 2018). In our study, we showed that sweet intake, tooth brushing, low mother’s education and childcare arrangement are 4 cumulative factors which combining together multiplied by 5 the ECC risk.
The relationship between sweet intakes and carious lesions observed in our study was in accordance with several other studies (Plutzer and Keirse 2012; Kabil and Eltawil 2017; Harris et al. 2004; Ganesh et al. 2020). The consumption of soft drinks with high sugar content and acidity can contribute to detrimental oral health (dental caries and dental erosion) (Tahmassebi et al. 2014) and may also affect general health. They supply energy only, are of little nutritional benefit and increase risk of overweight, obesity, type 2 diabetes (Chi and Scott 2019; Tahmassebi and Banihani 2020). In our study, we demonstrated that sweet intake is a high-risk factor of ECC. Sweet intake grouped together sweet consumption (at least once per day), sweet drink (at least once per day) and drink at night after 1-year-old including milk, breastfeeding and soft drink. Similar results were reported in the literature (Baghlaf et al. 2018; Seow 2018; Chaffee and Cheng 2014; Branger et al. 2019), the relationship between food intake and caries is not a novel area of study.
Tooth brushing has always been considered to be the primary and most effective way to prevent dental caries. Several studies have confirmed the association between tooth brushing and ECC (Aida et al. 2008; Gao et al. 2010; Zhang et al. 2020). However, other studies showed that there was no correlation between these two variables (Begzati et al. 2010; Zhou et al. 2011). Darmawikarta et al. (2014) and Sun et al. (2017) demonstrated that the major factor impacting the ECC risk is the introducing brushing at an early age. Our study confirmed this fact but only 22.6% of children started the brushing at the eruption of the first tooth. This percentage is relatively low compared to the rate described in Swedish children population, 95% of the parents had started to brush their children teeth at the age of 1 year (Boustedt et al. 2018). Tooth brushing always performed by the parents was not associated with the ECC risk (Boustedt et al. 2020) likewise in our study this factor failed to reach statistical significance. In our study, tooth brushing frequency was at borderline significance (p = 0.06). This result may be explained by the fact that the number of subjects included was lower than the calculated number of subjects required. Other studies reported mixed results, for example, Goldfeld et al. (2019) showed no evidence of an association between ECC prevalence and tooth brushing frequency. These results could be due to the use of self-reported data which have its limitations.
Furthermore, the use of fluoride-containing toothpaste is generally described like the most convenient and accepted tool to bring fluoride into the oral cavity (Boustedt et al. 2020; Marinho 2009) and an effective prevention measure of ECC (Mejare et al. 2015; Twetman and Dahr 2015; Walsh et al. 2019; Toumba et al. 2019). In our study, 85.2% of parents used fluoride toothpaste for their children. This factor was not correlated with ECC risk. This result was also described by Boustedt et al. (2020). The fact that in France, only 500 ppm fluoride-containing toothpaste is available for 4-year-old children, while the caries-preventive effect is statistically significant only for concentration of 1000 ppm and above (Toumba et al. 2019; Wong et al. 2011).
In medicine, patient’s education level is the best predictor of health conditions and health care behaviour in adults compared with other socioeconomic indicators such as income and employment (Laaksonen et al. 2005; Liu et al. 2011; Heima et al. 2015). Our finding that low mother’s education was associated with an increased ECC prevalence is consistent with the previously reported findings about lower paternal and/or maternal education levels (Kato et al. 2017; Baggio et al. 2015; Phillips et al. 2016; Campus et al. 2009; Poster et al. 2006). Educational background also affects health literacy and behaviour including dietary, tooth cleaning habits and health service utilisation frequency.
Socioeconomic status influences also the living conditions. Living in a more deprived neighbourhood was associated with higher caries risk (Droz et al. 2006; Aida et al. 2008; Hooley et al. 2012). Droz et al. (2006) also showed that geographic area was a predictor factor of ECC but in our study, the impact of this factor was more marked. Indeed, the prevalence of ECC was higher among children living in urban areas and especially in the education zone priority than those in rural areas.
In our study, we demonstrated that the home childcare or/and childminding by grandparents was an important contributor of child dental health. In France, childminder and nurseries represent an elevated cost, so childcare arrangement reflects the parents’ socioeconomic status. Perhaps in nursery, the control of children’s sugar intake is easier than at home. For example, sipping a bottle containing milk or juice throughout the day is maybe not considered a ‘snack’ by parents or grandparents. In addition, daytime breastfeeding or falling asleep during the nap with the bottle are not possible at the nurseries limiting fermentable carbohydrates exposure. These facts could explain the relationship between ECC prevalence and childcare arrangement.
In our study, only 4% of children presented teeth restoration, reflecting the low utilisation of dental services by preschool children. The prevalence of use of oral health service stagnated when compared to a previous French study (Droz et al., 2006). While our study did not focus on barriers to accessing dental care, some features and behaviours may explain the low frequency of treated tooth. The literature showed a relationship between socioeconomic status and the use of dental services (Edelstein 2000; Priesnitz et al. 2016). Furthermore, the need for dental care is not necessarily perceived: children appear to attend dental services when carious lesions are already occurring (Stormon et al. 2019) and/or when they induce painful and infectious complication. The low rate of dental care may manifest dental neglects(Katner et al. 2016) but also highlights the difficulties to access to dental care structures (Pegon-Machat et al. 2018).
Furthermore, paediatric dentistry, the expectation and behaviour of accompanying parents, and the need to be cost effective, may be stressful and fatiguing for dentists in daily dental practice (Klingberg and Broberg 2007; Ronneberg et al. 2015). Two factors were identified as barriers to the treatment of childhood caries: (1) the fact that preschool children’s coping skills limit their ability to accept dental care; and (2) dentists with negative personal feelings could think that providing care to young children can induce stress and be troublesome. They felt also time constrained (Pine et al. 2004). In France, the specialty of paediatric dentistry does not exist; according to one French study, only 24% of dental surgeons treated preschool children and did not perform pulp therapy of primary teeth including pulpotomy and pulpectomy (Muller-Bolla et al. 2018).
Two new acts in the nomenclature of French social security coverage could improve the link between families and dental practitioners: pregnant counselling since 2014 and first counselling for 3-year-old children since 2019, but it remains too late for the children. Indeed, the AAPD and the EAPD recommend the first dental counselling before the first birthday so the teamwork involving paediatric dentists and the early childhood health professionals is essential (Table 3).
Conclusion
This study highlighted the impact of the family environment on the oral health status of the preschool children. The results confirmed the relationship between sweet intake, brushing habits, childcare arrangement and maternal educational level and ECC. The identification of these risk factors should allow to strengthen preventive measures and initiate therapeutic education programs for children and their family. Adapting to each family, the objective should be to improve the oral health literacy skills of the caregivers.
References
Abed R, Bernabe E, Sabbah W. Family impacts of severe dental caries among children in the United Kingdom. Int J Environ Res Public Health. 2020;17:109.
Aida J, Ando Y, Oosaka M, Niimi K, Morita M. Contributions of social context to inequality in dental caries: a multilevel analysis of Japanese 3-year-old children. Community Dent Oral Epidemiol. 2008;36:149–56.
American Academy of Pediatric Dentistry. Policy on early childhood caries (ECC): classifications, consequences, and preventive strategies. Oral Health Polices. The reference manual of Pediatric Dentistry. 2019–2020/P.71–73.
Baggio S, Abarca M, Bodenmann P, Gehri M, Madrid C. Early childhood caries in Switzerland: a marker of social inequalities. BMC Oral Health. 2015;15:82.
Baghlaf K, Muirhead V, Moynihan P, Weston-Price S, Pine C. Free sugars consumption around bedtime and dental caries in children: a systematic review. JDR Clin Trans Rese. 2018;3(2):118–29.
Begzati A, Berisha M, Mega K. Early childhood caries in preschool children of Kosovo-a serious public health problem. BMC Public Health. 2010;10:788.
Boustedt K, Roswall J, Twetman S, Dahlgren J. Influence of mode of delivery, family and nursing determinants on early childhood caries development: a prospective cohort study. Acta OdontolScand. 2018;28:1–5.
Boustedt K, Dahlgren J, Twetman S, Roswall J. Tooth brushing habits and prevalence of early childhood caries: a prospective cohort study. Eur Arch Paediatr Dent. 2020;2:155–9.
Branger B, Camelot F, Droz D, Houbiers B, Marchalot A, Bruel H, Laczny E, Clément C. Breastfeeding and early childhood caries. Review of the literature, recommendations and prevention. Arch Pediatr. 2019;26(8): 497–503.
Campus G, Solinas G, STrohmenger L, Cagetti MG, Senna A? Minelli L, Majori S, Montagna MT, Reali D, Castiglia P, Collaborating Study Group. National pathfinder survey on children’s oral heath in Italy: pattern and severity of caries disease in 4-year-olds. Caries Res. 2009; 43:155–62.
Chaffee BW, Cheng A. Global research trends on early-life feeding practices and early childhood caries: a systematic review. J Oral Dis. 2014;2014:675658.
Chi DL, Scott JM. Added sugar and dental caries in children: a scientific update and future steps. Dent Clin N Am. 2019;63:17–33.
Cortes A, Ekstrand KM, Martignon S. Visual and radiographic merged-ICDAS caries progression pattern in 2–6 years old Colombian children: two-year follow-up. Int J Paediatr Dent. 2019;29:203–12.
Darmawikarta D, Chen Y, Carsley S, Birken CS, Parkin PC, Schroth RJ. Maguire JL, TARGet Kids! Collaboration. Factors associated with dental care utilization in early childhood. Pediatrics. 2014; 133:1594–600.
Droz D, Gueguen R, Bruncher P, Gerhard J-L, Roland E. Enquête épidémiologique sur la santé buccodentaire d’enfants âgés de 4 ans scolarisés en école maternelle. Arch Pediatr. 2006;13(9):1222–9.
Drury TF, Horowitz AM, Ismail AI, Maertens MP, Rozier RG, Selwitz RH. Diagnosing and reporting early childhood caries for research purposes. J Public Health Dent. 1999;59(3):192–7.
Edelstein BL. Access to dental care for Head Start enrollees. J Public Health Dent. 2000;60:221–9.
Edelstein B. The dental caries pandemic and disparities problem. BMC Oral Health. 2006;6(1):S2.
Edelstein BE, Vargas CM, Candelaria D, Vemuri M. Experience and policy implications of children presenting with dental emergencies to US pediatric dentistry training programs. Pediatr Dent. 2006;28(5):431–7.
Enjary C, Tubert-Jeannin S, Manevy R, Roger-Leroi V, Riordan PJ. Dental status and measures of deprivation in Clermont-Ferrand. France Community Dent Oral Epidemiol. 2006;34(5):363–71.
Fisher-Owens SA, Gansky SA, Platt LJ, Weintraub JA, Soobader MJ, Bramlett MD, Newacheck PW. Influences on children’s oral health: a conceptual model. Pediatrics. 2007;120:e510–20.
Fontana M, Wolff M. Translating the caries management paradigm into practice: challenges and opportunities. J Calif Dent Assoc. 2011;39(10):702–8.
Ganesh A, Sampath V, Sivanandam BP, Sangeetha H, Ramesh A. Risk factors for early childhood caries in toddlers: an institution-based study. Cureus. 2020;12(4):e7516.
Gao XL, Hsu CY, Xu YC, Loh T, Koh D, Hwarng HB. Behavioral pathways explaining oral health disparity in children. J Dent Res. 2010;89:985–90.
Goldfeld S, Francis KL, Hoq M, Do L, O’Connor E, Mensah F. The impact of policy modifiable factors on inequalities in rates of child dental caries in Australia. Int J Enviro Res Public Health. 2019;16(11):1970.
Harris R, Nicoll AD, Adair PM, Pine CM. Risk factors for dental caries in young children: a systematic review of the literature. Community Dental Health. 2004; 21/71–85.
Heima M, Lee W, Milgrom P, Nelson S. Caregiver’s education level and child’s dental caries in African Americans: a path analytic study. Caries Res. 2015;49(2):177–83.
Holmen A, StrömbergU, Häkansson G, Twetman S. Effect of risk-based payment model on caries inequalities in preschool children assessed by geo-mapping. BMC Oral Health. 2018; 18:3.
Hooley M, Skouteris H, Boganin C, Satur J, Kilpatrick N. Parental influence and the development of dental caries in children aged 0–6 years: a systematic review of the literature. J Dent. 2012;40:873–85.
Kabil NS, Eltawil S. Prioritizing the risk factors of severe early childhood caries. Dent J (Basel). 2017;5(1):4.
Katner D, Brown C, Fournier S. Considerations in identifying pediatric dental neglect and the legal obligation to report. JADA. 2016;147(10):812–6.
Kato H, Tanaka K, Shimizu K, Nagata C, Furukawa S, Arakawa M, Miyake Y. Parental occupations, educational levels, and income and prevalence of dental caries in 3-year-old Japanese children. Environ Health Prev Med. 2017;22(1):80.
Klingberg G, Broberg AG. Dental fear/anxiety and dental behavior management problems in children and adolescents: a review of prevalence and concomitant psychological factors. Int J Paediatr Dent. 2007;17:391–406.
Laaksonen M, Rahkonen O, Karvonen S, Lahelma E. Socioeconomic status and smoking: analyzing inequalities with multiple indicators. Eur J Public Health. 2005;15:262–9.
Liu Q, Wang M, Guo J, Li J, Li C, Qian M. Effect of socioeconomic status on secondary prevention of stroke. Int J Qual Health Care. 2011;23:405–12.
Marinho VC. Cochrane reviews of randomized trials of fluoride therapies for preventing dental caries. Eur Arch Paediatr Dent. 2009;10:183–91.
Mejare I. Bitewing examination to detect caries in children and adolescents-when and how often? Dent Update. 2005;32:588–90.
Mejare IA, Klingberg G, Mowafi FK, Stecksen-Blicks C, Twetman SH, Tranaeus SH. A systematic map of systematics reviews in paediatric dentistry-what do we really know? PLoS ONE. 2015;10(2):e0117537.
Mendes FM, Novaes TF, Matos R, et al. Radiographic and laser fluorescence methods have no benefits for detecting caries in primary teeth. Caries Res. 2012;46:536–43.
Muller Bolla M, Clauss F, Davit-Beal T, Manière MC, Sixou JL, Vital S. Prise en charge bucco-dentaire des enfants et des adolescents. Le Chirurgien-Dentiste de France. 2018; n°1806–180.
Nobile CGA, Fortunato L, Bianco A, Pileggi C, Pavia M. Pattern and severity of early childhood caries in Southern Italy: a preschool-based cross-sectional study. BMC Public Health. 2014;14:206.
Pegon-Machat E, Jourdan D, Tubert-Jeannin S. Inégalités en santé orale: déterminants de l’accès à la prévention et aux soins en France. Santé Publique. 2018;30(2):243–51.
Phillips M, Masterson E, Sabbah W. Association between child caries and maternal health-related behaviours. Community Dent Health. 2016;33:133–7.
Pine CM, Adair PM, Burnside G, Nicoll AD, Gillett A, Borges-Yanez A, Broukal Z, Brown J, Declerck D, Ping FX, Gugushe T, Hunsrisakhun J, Lo ECM, Naidoo SNyandindi U, Poulsen VJ, Razanamihaja N, SPlieth C, Sutton BK, Soo TC, Whelton H. Barriers to the treatment of childhood caries perceived by dentists working in different countries. Community Dent Health. 2004; 21(1): 112–120.
Pitts NB, Ekstrand KR. International Caries Detection and Assessment System (ICDAS) and its International Caries Classification and Management System (ICCMS)—methods for staging of the caries process and enabling dentists to manage caries. Community Dent Oral Epidemiol. 2013;41:41–52.
Plutzer K, Keirse MJNC. Influence of first-time mothers ‘early employment on severe early childhood caries in their child. Int J Pediatr. 2012;8:26–32.
Poster WJ, Pendrys DG, Morse DE, Zhang H, Mayne ST. Associations of ethnicity/race and socioeconomic status with early childhood caries patterns. J Public Health. 2006;66:23–9.
Priesnitz MC, Celeste RK, Pereira MJ, Pires CA, Feldens CA, Kramer PF. Neighborhood determinants of caries experience in preschool children: a multilevel study. Caries Res. 2016;50:455–61.
Rønneberg A, Strøm K, Skaare AB, Willumsen T, Espelid I. Dentist’s self-perceived stress and difficulties when performing restorative treatment in children. Eur Arch Paediatr Dent. 2015;16:341–7.
Seow WK. Early childhood caries. Pediatr Clin N Am. 2018;65:941–54.
Stormon N, Ford PJ, Laloo R. Oral health in the longitudinal study of Australian children: an age, period, and cohort analysis. Int J Paediatr Dent. 2019;29:404–12.
Sun X, Bernabe E, Liu X, Gallagher JE, Zheng S. Early life factors and dental caries in 5-year-old children in China. J Dent. 2017;64:73–9.
Tahmassebi JF, BaniHani A. Impact of soft drinks to health and economy a critical review. Eur Arch Paediatr Dent. 2020;21:109–17.
Tahmassebi JF, Kandiah P, Sukeri S. The effects of fruit smoothies on enamel erosion. Eur Arch Paediatr Dent. 2014;15:175–81.
Toumba KJ, Twetman S, Splieth C, Parnell C, van Loveren C, Lygidakis NA. Guidelines on the use of fluoride for caries prevention in children: an updated EAPD policy document. Eur Arch Paediatr Dent. 2019;20:507–16.
Tubert-Jeannin S, Lecuyer M-M, Manevy R, et al. Évaluation après un an d’un programme de promotion de la santé orale à l’école maternelle. Santé publique. 2008;20(1):7–17.
Twetman S, Dahr V. Evidence of effectiveness of current therapies to prevent and treat early childhood caries. Pediatr Dent. 2015;37:246–53.
Walsh T, Worthington HV, Glenny AM, Marinho VCC, Jeroncic A. Fluoride toothpastes of different concentrations for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2019;3(3):CD007868.
Wong MC, Clarkson J, Glenny AM, Lo ECM, Marinho VCC, Tsang BWK, Walsh T, Worthington HV. Cochrane reviews on the benefits/risks of fluoride toothpastes. J Dent Res. 2011;90:573–9.
Zhang M, Zhang X, Zhang Y, Li Y, Shao C, Xiong S, Lan J, Wang Z. Assessment of risk factors for early childhood caries at different ages in Shandong, China and reflections on oral health education: a cross-sectional study. BMC Oral Health. 2020;20:139.
Zhou Y, Lin HC, Lo C, Wong MC. Risk indicators for early childhood caries in 2-year-old children in southern China. Aus Dent J. 2011;56:33–9.
Acknowledgements
We thank the nurses, the teachers, the children and their parents, the medicine doctors, Dr. Jean Louis Gerhard, Dr. Damien Gonthier, and Olivier Cottet DASEN of Moselle who authorised the investigators to intervene in schools.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
MH and DD drafted the manuscript. PB and DD conceived the project. AL and AD collected the data, supervised by MH and DD; KC and AC performed the statistical analyses. KC helped draft the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethics approval
The study was approved by the Ethical committee (Protocol Number: 18076-1232-18.08.21.60332) and the Nancy-Metz regional education authority.
Consent to participate
Written informed consent was obtained from the parents of the children.
Consent to publication
All the authors have agreed upon the manuscript content and consent to publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hernandez, M., Chau, K., Charissou, A. et al. Early predictors of childhood caries among 4-year-old children: a population-based study in north-eastern France. Eur Arch Paediatr Dent 22, 833–842 (2021). https://doi.org/10.1007/s40368-021-00627-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40368-021-00627-0