Abstract
Aim
To report on the prevalence, defect characteristics, and distribution of hypomineralised second primary molars (HSPM) in Gautam Budh Nagar, Uttar Pradesh, India and to report on possible association, if any, between HSPM and molar-incisor-hypomineralisation (MIH).
Methods
A cross-sectional survey included a random sample of 978, 6–8-year-old school children. EAPD diagnostic criteria for scoring MIH defects on first permanent molars (FPM) were adapted and used to score hypomineralisation defects in both FPM and second primary molars (SPM) by a single calibrated examiner. Comparative statistics for HSPM versus hypomineralised FPM were computed using a Chi square test. An odds ratio (OR) at 95 % confidence interval (CI) was used to test and any association between HSPM and MIH.
Results
An overall prevalence of 5.6 % (55/978) was reported for HSPM in the study population. Prevalence of MIH as hypomineralised FPM was 7.4 % (72/978). Concomitant presence of HSPM and MIH was observed in 32.73 % (18/55) of affected subjects. The presence of HSPM had significantly higher odds ratio for development of MIH (OR 7.82; 95 % CI = 4.18–14.65; p < 0.001). A greater severity of defects was observed in HSPM compared with affected FPM as greater number of affected surfaces presented with post-eruptive breakdown (PEB) in former compared to latter (p < 0.001).
Conclusion
The prevalence of HSPM in 6–8-year-old Indian children was 5.6 %. The severity of hypomineralisation was milder in FPM compared to SPM. The presence of HSPM was reported to have significantly higher odds for development of MIH in future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Developmental defects of enamel are commonly encountered clinical entities and may be qualitative (hypomineralisation) or quantitative (hypoplasia) (Jälevik and Norén 2000; William et al. 2006). Enamel hypomineralisation is identified visually as a demarcated opacity with a clear border with varying extensions and can be white, yellow, or brown in colour (Jälevik and Norén 2000; Weerheijm 2003). These demarcated opacities may present with/without breakdown (post-eruptive breakdown; PEB) (Weerheijm 2003). Although demarcated opacities may occur in any teeth of the dentition i.e., first permanent molars (FPM), permanent incisors (PIs), canines, premolars, second permanent molars, and second primary molars (SPM); FPM are the most commonly affected teeth (Elfrink et al. 2008, 2012; Lygidakis et al. 2010; Ghanim et al. 2011; Kühnisch et al. 2014). FPM may be affected in isolation or concomitantly with PIs and this combination is named as Molar Incisor Hypomineralisation (MIH) (Weerheijm 2003; Lygidakis et al. 2010) while the demarcated opacities in SPM have been termed Deciduous Molar Hypomineralisation (DMH) (Elfrink et al. 2008).
MIH has been defined as demarcated, qualitative developmental defect of enamel (DDE), affecting one or more permanent molars, with or without the involvement of the permanent incisor teeth (Weerheijm 2003). Recently, this condition has attracted interest of clinicians across the world probably because of the worrisome clinical picture and management challenges associated with it (Lygidakis 2010). It is very common for the affected teeth to present with post-eruptive breakdown (PEB), hypersensitivity, higher risk of caries development and progression and higher rates of restoration failures (Lygidakis 2010).
Although a number of research papers have addressed the causal association between several possible risk factors and MIH, the evidence is still limited to clearly label the risk markers for MIH. It has been postulated that a similar set of causative factors (i.e., preterm birth, low birth weight and/or poor gestational health) may play a role in development of HSPM and MIH because of overlapping periods of mineralization of FPM and SPM (Elfrink et al. 2012; 2014; Ghanim et al. 2013). Thus, the presence of HSPM may suggest the possibility of development of hypomineralisation in FPM in future (Elfrink et al. 2012). HSPM can serve as a useful risk marker for MIH and early identification can help to plan early preventive management protocol for MIH to avoid undue clinical sequelae (e.g., hypersensitivity, PEB, caries, and/or extractions).
Unfortunately not many papers have been published on HSPM and there is a dearth of data on prevalence, clinical presentation, and/or possible set of aetiological factors (Elfrink et al. 2008, 2012; Ghanim et al. 2013). Only two studies have addressed the possible association between HSPM and MIH (Elfrink et al. 2012; Ghanim et al. 2013). The results of these two studies were contradictory. Elfrink et al. (2012) found significantly higher odds of development of MIH among children with HSPM while Ghanim et al. (2013) reported no such positive association between MIH and HSPM. Keeping in mind the above-mentioned facts, an observational cross-sectional study on HSPM was designed with following objectives:
-
To report on prevalence, defect characteristics, and distribution of HSPM in a group of 6–8-year-old Indian school children.
-
To inter-compare the defect characteristics (type of defects, i.e., creamy white opacity/yellowish brown opacity/PEB; extent, distribution, and location of the individual defects) among HSPM and FPM.
-
To report on association, if any, between HSPM and MIH.
Materials and methods
Ethical consideration
This study was approved by ethical committee and review board of Santosh University, Ghaziabad, Uttar Pradesh, India. This study is part of a larger study on enamel hypomineralisation in primary and permanent dentition in India. Thus, ethical clearance for this study was sought as a part of the entire study.
Study location
The present study was conducted in Gautam Budh Nagar District, Uttar Pradesh, India. This city is located in northern India. The city has a population of approximately 1.7 million with a literacy rate of 82.2 % (Census of India 2011). The ground-water fluoride levels in the city range from 0.27 to1.2 ppm.
Recruitment of study population
The study population comprised a target sample of 1000, 6–8-year-old school children studying in private schools. Schools were selected randomly according to number of schools in each area to ensure varied geographical and socioeconomic coverage. A written description of the condition MIH and its effect on overall oral health was sent to the administrative authorities of the schools. Written permission was sought to conduct oral examinations in their schools. Informed parental consents were obtained by the school authorities. Cohorts of children born in year 2003–2006 and studying in selected schools in the academic year 2012–2013 were included. A stratified random sample was selected and every 5th child from the targeted age group was included.
Inclusion and exclusion criteria
Inclusion criteria were 6–8 years of age, presence of FPM and SPM, positive parental consent, and being in the school on the day of examination. Children with other developmental defects i.e., amelogenesis imperfecta, dentinogenesis imperfecta, tetracycline staining, or diffuse hypoplastic lesions (i.e., fluorosis) on index teeth were excluded from the study. Schools for children with special health care needs were excluded. Also, children with grossly broken down and/or missing FPM and/or SPM where causes of breakage or tooth loss could not be determined were excluded from study.
Training and calibration of examiner
The entire examination was conducted by an examiner (NM) actively involved in MIH research and clinical management. The details of calibration of the examiner have been published elsewhere (Mittal et al. 2014). The intra-examiner reliability was computed by re-examining 10 % of total sample on the last day of examination in respective schools. The kappa statistics for intra-examiner reliability were reported as excellent i.e., 0.92 (Landis and Koch 1977).
Study settings and diagnostic criteria
The examinations were conducted in the children’s respective schools. Examination was performed using a dental mirror, blunt probe, and a source of artificial light on clean teeth in wet conditions. EAPD diagnostic criteria for scoring MIH defects on FPM were adapted and used to score hypomineralisation defects on both FPM and SPM (Lygidakis et al. 2010). Surfaces examined included buccal, palatal/lingual, and occlusal. Defects with dimensions ≤2 mm were not considered. The extent of the defects was graded according to surface area of involvement, i.e., Defect 1 (<1/3rd of tooth surface area), Defect 2 (involving 1/3rd to 2/3rd of tooth surface area), Defect 3 (>2/3rd of tooth surface area). A tooth with PEB was considered to be more severely affected than a sound tooth and yellowish brown opacities were considered to be more severe than creamy white opacities.
Data handling, record keeping and statistical analysis
The entire sets of data were first entered on structured pre-printed proforma, which had a provision to record each subject’s demographic details and tooth/surface record of defect type, extent and location. The data from the proforma sheets were first entered in Excel spreadsheets (Microsoft office®, Microsoft®, Redmond, Washington, USA) and then transported to SPSS® version 22 (IBM, New York, USA) for statistical analysis. Descriptive statistics were calculated to be expressed as mean ± SD and/or number (percentage). Comparative intra-group and inter-group statistics were computed using Pearson’s Chi square test. An odds ratio (OR) at 95 % confidence interval (CI) was used to test association between HSPM and MIH.
Results
Demographics and overall prevalence
A response rate of 97.8 % as a total of 978 subjects out of target sample size of 1000 who were examined was acheived. Mean age of the children was 6.45 ± 1.46 years. Most of the children were 6-year olds (p < 0.01; Table 1). However, no significant difference was observed with respect to the number of affected teeth and surfaces with respect to age and sex (Table 1). A total of 55/978 subjects presented with HSPM and so the prevalence in the study population was 5.62 %. At tooth level the prevalence of HSPM was 3.47 % (136/3912). Prevalence of MIH i.e., hypomineralised FPM was 7.36 % (72/978). At tooth level the prevalence of MIH was 5.09 % (199/3912).
Extent, distribution, and characteristics of defects in HSPM
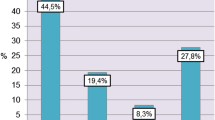
Mean number of affected teeth/subject was 2.47 ± 1.07 and similar figures for affected surfaces were 4.64 ± 3.22. Most of the subjects had a total of 2 HSPM (Table 2) and 3–6 affected surfaces (Fig. 1). Occlusal and buccal surfaces were equally involved (p > 0.05) while the lingual surfaces were the least (p < 0.001) (Table 2). Most of the affected surfaces (177/255; 69.4 %) presented with creamy white defects (Fig. 2; Table 3). A total of 77/255 (30.2 %) surfaces presented with PEB (Fig. 2). Atypical restorations/extractions because of hypomineralisation were not observed.
Inter-comparison of defect characteristics, extent, and distribution in HSPM and hypomineralised FPM
Quantitatively both HSPM and hypomineralised FPM similarly of affected teeth (p > 0.05); however, significantly greater number of surfaces were affected in hypomineralised FPM (Table 2). Similar pattern of surface distribution was observed for both HSPM and hypomineralised FPM as buccal and occlusal surfaces were equally affected while lingual surfaces were least commonly so in both the study groups (Table 2). However, HSPM were observed more often in mandibles compared with maxilla (p < 0.01) (Table 2). Greater severity of defects was observed in HSPM compared to affected FPM as greater number of affected surfaces presented with PEB in former compared to latter (p < 0.01) (Table 3).
Although creamy white opacities were the commonest type of defect in both HSPM and affected FPM; significantly greater number of affected surfaces presented with yellowish brown opacities in the former compared to the latter (p < 0.01) (Table 3). Considering the extent of involvement of tooth surface area by individual lesions; more extensive involvement was observed for HSPM (Table 3).
Association between MIH and HSPM (Table 4)
Concomitant presence of HSPM and MIH was observed in 32.73 % (18/55) of affected subjects. The presence of HSPM exhibited significantly higher odds ratio for MIH (OR 7.82; 95 % CI = 4.18–14.65; p < 0.001). After analyzing the data further with respect to number of HSPM/subject, it was found that the presence of single HSPM was not associated with MIH (p = 0.44), while subjects with ≥2 HSPM had significantly higher odds ratio for MIH (p < 0.001) (Table 3). A further data analysis to assess whether the presence of PEB in HSPM was associated with MIH showed that subjects with HSPM always had higher odds ratio for MIH regardless of the presence or absence of PEB (p < 0.001).
Discussion
The EAPD criteria (Lygidakis et al. 2010) were adopted to diagnose and score hypomineralisation defects of SPM (Elfrink et al. 2012; Ghanim et al. 2013). These criteria have been developed for MIH and are currently considered to be a standard and validated criterion for diagnosing and recording MIH. The same criteria were employed for scoring hypomineralisation on HSPM as well. This was completed to help standardize the research on HSPM, to allow comparison with recently published research papers on HSPM (Elfrink et al. 2012; Ghanim et al. 2013) and to facilitate inter-comparison among HSPM and MIH in the present study population. Further, EAPD criteria are the best consensus based criteria to score hypomineralisation (Lygidakis et al. 2010).
A prevalence rate of 5.6 % for HSPM was found and is the first study to report on the prevalence of HSPM in an Indian population. The results herein are comparable to the prevalence of HSPM in Iraq (Ghanim et al. 2013) and the Netherlands (Elfrink et al. 2008). On the other hand, another recent study also from the Netherlands employing similar criteria reported a much higher prevalence of HSPM (Elfrink et al. 2012). In the most recent study from the Netherlands (Elfrink et al. 2012), standardised intraoral photographs were employed for recording hypomineralisation defects. Whereas in rest of the studies (including the present study), direct clinical examination was employed (Elfrink et al. 2008; Ghanim et al. 2013). As the validity and reproducibility of intraoral photographs for recording hypomineralisation defects has been proven (Elfrink et al. 2009), the reasons for a higher prevalence for HSPM in second Dutch report remain unclear.
Another fact to be borne in mind while comparing the prevalence data between previous reports is the difference in the age group of cohorts recruited. In the older children, the presence of caries may have interfered with establishing the diagnosis of hypomineralisation. In the present study, grossly broken down/missing teeth were excluded where causes of breakage/loss could not be determined. This could have contributed to under-reporting of atypical restorations/extraction owing to hypomineralisation in our report.
Various other reports on the prevalence of demarcated opacities in the primary dentition have noted wide variations in prevalence rates, i.e., 1.6–27 % (Nation et al. 1987; Weeks et al. 1993; Li et al. 1995; Kanchanakamol et al. 1996; Seow et al. 1996; Rugg-Gunn et al. 1998; Slayton et al. 2001; Montero et al. 2003; Lunardelli and Peres 2005; Chaves et al. 2007; Farsi 2010). A direct comparison with those reports is not possible due to non-uniform recording criteria, different index teeth, and differences in age group of cohorts recruited. Nevertheless, the prevalence of MIH in the present study is in line with the previously published reports from India (Parikh et al. 2012; Mittal et al. 2014).
Quantitatively a similar extent of hypomineralisation was reported for both primary and permanent molars. Similar data for affected teeth were reported for both primary and permanent molars. But, this similarity was not found when the individual defect characteristics were compared. Greater severity was reported for primary molars as significantly greater number of surfaces presented with yellowish brown opacities and PEB in the former compared to latter. Direct conclusions based on these results i.e., enamel hypomineralisation manifests to a greater severity in primary molars should be drawn with caution. This is because of the variable time periods for which these two types of teeth in comparison have been present in the oral cavity. SPMs erupt earlier than FPM (Butler 1967; McDonald and Avery 2004). At the age when the subjects were examined in the present study, SPM would have been present in the oral cavity for a much longer duration compared to FPM. The observed trend of greater severity in SPM may be because of the effect of masticatory forces which acted for a much longer duration on SPM rather than the actual differences in the defect characteristics among the two sets of teeth.
Previously only two studies have addressed the association between HSPM and MIH (Ghanim et al. 2013; Elfrink et al. 2012). The results of our study are in agreement with those of Elfrink et al. (2012) and at variance with those of Ghanim et al. (2013). Conflicting results obtained by Ghanim et al. (2013) could be because of an older age group, small sample size, and much higher prevalence of MIH in their study population. Ghanim et al. (2013) in their study advised caution in considering the results of their study owing to an older age group employed where hypomineralisation defects could have been masked by the presence of caries.
In the present study, subjects with the HSPM were reported to have an odds ratio of 7.8 for presenting with MIH. Interestingly, when these data were further analyzed for calculating the odds ratio for children with varying numbers of HSPM, a significant association was found only for children with ≥2 HSPM (p < 0.001). Children with single HSPM were not found to have a significant risk of developing MIH (OR = 2.3, 95 % CI = 0.2–19.0; p = 0.44). Nevertheless, small sample size caution generalization of results. This finding is in agreement with Elfrink et al. (2012) where an increase in odds ratio was reported with a larger number of HSPM. On the other hand when the data were analyzed with respect to severity of defects (mild versus severe), slightly higher values of odds ratio were reported for mild cases (8.9) compared with severe ones (6.8). But, it is to be noted that a significant risk for developing MIH was reported for both type of defects. This finding of the present study agrees with those of Elfrink et al. (2012). Previously, it has been reported that the onset and severity of hypomineralisation defects are inter-related (Fargell et al. 2013) as the insult during mineralization/maturation, milder is the hypomineralisation. Thus, the aetiological insult causing milder hypomineralisation defects on SPM must have occurred during latter stages of mineralization/maturation, overlapping with earlier phases of active mineralization of FPM when the ameloblasts are most active. This may explain why higher odds of developing MIH were reported for children presenting with milder form of HSPM.
Depending upon the timing on aetiological insult, hypomineralisation may manifest in any teeth of the dentition. The inter-relationship between HSPM and MIH is possible owing to overlapping periods of mineralization of two types of teeth i.e., SPM and FPM. The results of our study give weight to this hypothesis which has been suggested and tested previously. Owing to earlier eruption of SPM and possibility of early clinical examination, MIH can be predicted prior to eruption of FPM which are scheduled to erupt later. In case of increased risk of development of MIH i.e., presence of HSPM, a targeted preventive approach can be planned and the parents can be guided to help efficient management of MIH. Further long-term prospective observational studies are necessary to establish the predictive value of HSPM for forecasting MIH in permanent dentition.
Conclusions
The prevalence of HSPM in 6–8-year-old Indian children was 5.6 %. The severity of hypomineralisation was milder in FPM compared to spm in this age group. The presence of HSPM (especially mild HSPM and ≥2 HSPM) was reported to have significantly higher odds (OR: 7.82) of development of MIH in future.
References
Butler PM. Comparison of the development of the second deciduous molar and the first permanent molar in man. Arch Oral Biol. 1967;12:1245–60.
Census of India 2011. http://censusindia.gov.in/PopulationFinder [Last accessed on 21st April 2014].
Chaves AMB, Rosenblatt A, Oliveira OFB. Enamel defects and its relation to life course events in primary dentition of Brazilian children: a longitudinal study. Community Dent Health. 2007;24:31–6.
Elfrink ME, Schuller AA, Weerheijm KL, et al. Hypomineralised second primary molars: prevalence data in Dutch 5-year-olds. Caries Res. 2008;42:282–5.
Elfrink MEC, Veerkamp JSJ, Aartman IHA, et al. Validity of scoring caries and primary molar hypomineralisation (HSPM) on intraoral photographs. Eur Arch Paediatr Dent. 2009;10:5–10.
Elfrink ME, ten Cate JM, Jadoe VW, et al. Deciduous molar hypomineralisation and molar incisor hypomineralisation. J Dent Res. 2012;91:551–5.
Elfrink MEC, Moll HA, Kiefte-de Jong JC, et al. Pre- and postnatal determinants of deciduous molar hypomineralisation in 6-year-old children. The Generation R Study. PLoS One. 2014;9:e91057.
Fargell TG, Salmon P, Melin L, Noren JG. Onset of molar incisor hypomineralisation (MIH). Swed Dent J. 2013;3:61–70.
Farsi N. Developmental enamel defects and their association with dental caries in preschoolers in Jeddah Saudi Arabia. Oral Health Prev Dent. 2010;8:85–92.
Ghanim A, Morgan M, Marinõ R, et al. Molar-incisor hypomineralisation: prevalence and defect characteristics in Iraqi children. Int J Paediatr Dent. 2011;21:413–21.
Ghanim A, Manton D, Marinõ R, et al. Prevalence of demarcated hypomineralisation defects in second primary molars in Iraqi children. Int J Paediatr Dent. 2013;23:48–55.
Jälevik B, Norén JG. Enamel hypomineralisation of permanent first molars: a morphological study and survey of possible aetiological factors. Int J Paediatr Dent. 2000;10:278–89.
Kanchanakamol U, Tuongratanaphan S, Tuongratanaphan S, et al. Prevalence of developmental enamel defects and dental caries in rural pre-school Thai children. Community Dent Health. 1996;13:204–7.
Kühnisch J, Heitmüller D, Thiering E, et al. Proportion and extent of manifestation of molar-incisor hypomineralisations according to different phenotypes. J Public Health Dent. 2014;74:42–9.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Li Y, Navia JM, Bian JY. Prevalence and distribution of developmental enamel defects in primary dentition of chinese children 3-5 years old. Community Dent Oral Epidemiol. 1995;23:72–9.
Lunardelli SE, Peres MA. Prevalence and distribution of developmental enamel defects in the primary dentition of pre-school children. Braz Oral Res. 2005;19:144–9.
Lygidakis NA. Treatment modalities in children with teeth affected by molar-incisor enamel hypomineralisation (MIH): a systematic review. Eur Arch Paediatr Dent. 2010;11:65–74.
Lygidakis NA, Wong F, Jälevik B, et al. Best clinical practice guidance for clinicians dealing with children presenting with Molar-Incisor-Hypomineralisation (MIH): an EAPD Policy Document. Eur Arch Paediatr Dent. 2010;11:75–81.
McDonald RE, Avery DR. Development and morphology of the primary teeth. In: McDonald RE, Avery DR, editors. Dentistry for the child and adolescent. 8th ed. St. Louis: The C.V. Mosby Co.; 2004. p. 53.
Mittal NP, Goyal A, Gauba K, et al. Molar incisor hypomineralisation: prevalence and clinical presentation in school children of the northern region of India. Eur Arch Paediatr Dent. 2014;15:11–8.
Montero MJ, Douglass JM, Mathieu GM. Prevalence of dental caries and enamel defects in Connecticut head start children. Pediatr Dent. 2003;25:235–9.
Nation WA, Matsson L, Peterson JE. Developmental enamel defects of the primary dentition in a group of Californian children. J Dent Child. 1987;54:330–4.
Parikh DR, Ganesh M, Bhaskar V. Prevalence and characteristics of Molar Incisor Hypomineralisation (MIH) in the child population residing in Gandhinagar, Gujarat India. Eur Arch Paediatr Dent. 2012;13:21–6.
Rugg-Gunn AJ, Al-Mohammadi SM, Butler TJ. Malnutrition and developmental defects of enamel in 2- to 6-year-old Saudi boys. Caries Res. 1998;32:181–92.
Seow WK, Amaratunge A, Bennett R, et al. Dental health of aboriginal pre-school children in Brisbane Australia. Community Dent Oral Epidemiol. 1996;24:187–90.
Slayton RL, Warren JJ, Kanellis MJ, et al. Prevalence of enamel hypoplasia and isolated opacities in the primary dentition. Pediatr Dent. 2001;23:32–6.
Weerheijm KL. Molar incisor hypomineralisation (MIH). Eur J Paediatr Dent. 2003;4:114–20.
Weeks KJ, Milsom KM, Lennon MA. Enamel defects in 4-to-5 year-old children in fluoridated and non-fluoridated parts of Cheshire UK. Caries Res. 1993;27:317–20.
William V, Messer LB, Burrow MF. Molar incisor hypomineralisation: review and recommendations for clinical management. Pediatr Dent. 2006;28:224–32.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mittal, N., Sharma, B.B. Hypomineralised second primary molars: prevalence, defect characteristics and possible association with Molar Incisor Hypomineralisation in Indian children. Eur Arch Paediatr Dent 16, 441–447 (2015). https://doi.org/10.1007/s40368-015-0190-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40368-015-0190-z