Abstract
The role of dysplastic oral pre-cancers in oral squamous cell carcinoma development is well recognized, but the notion is not exclusive. Diagnostic gold standards in predicting malignant potentiality of such pre-cancers suffer from ambiguity due to inter- and intra-observer variability. In addressing such diagnostic challenges, combinatorial appraisement of molecular pathology attributes encompassing cancer hallmarks is thought to provide a wider analytical sense. Two major premalignant disorders, viz. oral leukoplakia and oral submucous fibrosis have been considered as candidate precursors of cancer here. This review highlights the molecular pathology signatures expressed in oral epithelial dysplasia and revisits the usefulness of combinatorial analysis of expressional pattern of existing molecular biomarkers in the context of proper selection of cardinal attributes from each cancer hallmark for better malignant potentiality assessment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oral squamous cell carcinoma (OSCC), the sixth largest cause of death due to malignancy in the world [95], is a complex multistep phenomenon. Its progression from benign hyperplasia to dysplasia [68], to carcinoma in situ, and then into OSCC is reported [3]. Although oral epithelial dysplasia (OED) is considered to be an intermediate step for transformation of varied pre-cancerous lesions in oral cancer development, interestingly OSCC can develop from non-dysplastic lesions too [3]. Among many oral premalignant disorders (PMDs), premalignant lesion like oral leukoplakia (OLK) and premalignant conditions like oral submucous fibrosis (OSF) are commonly prevalent and histopathological evaluation of their biopsy is the diagnostic gold standard. However, this diagnostic approach suffers from non-specificity as well as intra- and inter-observer variability [96]. In spite of significant development in molecular pathology, the lack of specific molecular markers in predicting the malignant potentiality of PMDs is remarkable. Current research focuses on more selective and specific marker expression which can provide a better insight. As OED is also considered as a histopathologic marker of the malignant potentiality of PMDs [89], the molecular mechanism of dysplasia in different PMDs to assess malignant potentiality of PMDs will be reviewed in this article. The importance of a combinatorial approach will also be revisited to evaluate the expression profile of prime molecules in the context of cancer hallmarks.
Definition and Classification of OED
For OED, the initial definition provided by Pindborg (1977) and Lumermann et al. (1995) has not been accepted due to a lack of objectivity [3]. Architectural and cytological changes were considered as the major attributes of OED [54]. Grading of oral epithelial dysplasia is currently performed by interpretation of the epithelial features, like loss of maturation and stratification of intact epithelia as well as cytological changes, consisting of cellular atypia in the epithelial tissue of the oral mucosa. Loss of cell adhesion, cellular apicobasal polarity, hyperplastic basal cells, drop-shaped rete ridges consisting of keratin pearls, increased number of mitotic figures, atypical mitotic figures, abnormally superficial mitoses, anisonucleosis, anisocytosis, pleomorphism, increased nuclear size and nuclear-cytoplasmic ratio, increased number and size of nucleoli and hyperchromasia, and dyskeratosis are a few other epithelial features [96]. Current research suggests that, inclusion of DNA ploidy status analysis when combined with conventional histopathological OED grading can potentiate the malignant potentiality prediction [86]. There are still few other criteria which are considered during grading of OED which are not included in the cluster of features currently accepted to evaluate degree of dysplasia, but can potentiate the classification [90].
OED can be divided into three types according to severity; mild, moderate, and severe dysplasia [97]. Mild dysplasia is associated with minor architectural disturbance where only the lower third of the epithelium is affected with cytological atypia. In moderate dysplasia, architectural disturbance invades up to the middle third of the epithelium, as well as cytological atypia being increased, whereas severe dysplasia is characterized by architectural disturbance that extends to more than two-thirds of the epithelium with many other changes of oral mucosa [97]. Gradations of OED, based on histopathological observations, have been augmented nowadays with clinicopathological features, immunohistochemical examinations by useful molecular markers, as well as newer clinical diagnostic and treatment modalities [33, 66]. Even the malignant potentiality of a dysplastic condition can be predicted through characterized molecular pathological features. Nuclear translocation of β -catenin in upper layer, as well as simultaneous loss of E-Cadherin in basaloid cells in the lower layer of a dysplastic keratinized tissue, indicates increased recurring and malignant potentiality [4].Along with immunohistochemistry-based studies, the expression profile of protein biomarkers using RNA-based or proteomics studies is also now often considered for better assessment [79]. The basis of molecular expression studies for dysplastic PMDs will be emphasized with OLK and OSF. The definition of OLK, as amended in the workshop of WHO Collaborating Centre for Oral Cancer and Precancer in 2005 by the working group, is that: ‘The term leukoplakia should be used to recognize white plaques of questionable risk having excluded (other) known diseases or disorders that carry no increased risk for cancer’ [68], whereas OSF is a chronic, premalignant condition, characterized by progressive submucosal fibrosis inside oral cavity [57].
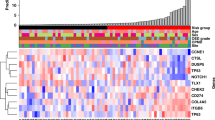
Current concepts to understand the molecular pathway of dysplasia in PMD and its correlation with malignant potentiality through expression studies of different molecular markers of PMDs are intriguing and rapidly evolving. In this review, cardinal molecules of cancer hallmarks will be highlighted to understand OED and associated carcinogenesis through mentioned dysplastic PMDs. An extensive literature search has described the expression features of genes in OED that could be indicative for malignant potentiality of the PMDs, but they suffer from non-specificity. Hence, combinatorial assessment of cardinal molecules from cancer hallmarks could be contributory and may be important in developing robust integrated biomarkers to assess the malignant potentiality of dysplastic PMDs. Table 1 shows the association between the genes involved in OED and cancer hallmarks. Figure 1 depicts the route of carcinogenesis through different grades of OED.
Molecular Pathology Features of Dysplastic Oral PMDs
Impairment of Epithelial Progressive Maturation and Epithelial Mesenchymal Transitions (EMT) Features
Deregulation in Epithelial Master Regulator and EMT Markers
If molecular expressions are taken into account in respect to development, proliferation, maintenance, and maturation of stratified epithelia, p63 is considered as a master regulator [21]. It has a major impact on stemness preservation as well [13]. Increased expression of p63 protein and mRNA, as well as of its isoform ΔNp63 is noted not only in dysplasia, but also in impairment of epithelial maturation with the severity of oral dysplasia [17, 21, 55]. It was also found to be associated with EMT, a fundamental biological process embedded in development, wound healing, and metastasis [20]. Further simultaneous elevation of ΔNp63, podoplanin, and intraepithelial inflammatory cells in OED is reported to indicate its high malignant potentiality [76]. Loss of E- Cadherin, another fundamental feature of EMT is also seen in OED caused by OSF (16). It is used to grade OED to avoid confusion arising from intra-observer and inter-observer variability [99]. The association between E-Cadherin–catenin complex, especially β- and γ-catenin expression are deregulated with the grade of dysplasia leading to cytoplasmic dislocation of E-Cadherin [21, 51]. In addition, P-cadherin expression was found to be upregulated in moderate and severe dysplasia but in dysplasia adjacent to infiltrating carcinomas it is lost [98].
When adhesion molecules are taken into account, reduced but extended expression of CD44s throughout the dysplastic layers are noted which is indicative of malignant potentiality [10, 11]. Downregulation of CD44v7-8 is also known to be associated with increased malignant potentiality [8, 44]. Further CD44v6 is also reported to be downregulated in OED of PMDs [28]. In the context of impairment in the basement membrane, the focal breaks of laminin and collagen IV could be noted [78]. Discontinuous laminin 5 expressions along with increased expression of laminin 5 γ2 chain, with slightly altered thickness of mucosa are observed in OED [37]. Increasing expression of collagen XVII (BP180), a component responsible for keratinocyte adhesion and motility, can also be correlated according to the grade of dysplasia and may be linked to carcinogenesis, as it is induced by a tumor promoter, PMA [65]. Perlecan, another basement membrane molecule present in the cell border of parabasal cells in normal mucosa, migrates to the surface layer and deposits in the cytoplasm as well as in intercellular spaces with increased degree of dysplasia [32]. The intercellular deposit of perlecan is known to induce MMP-7, a component having E- Cadherin lysis potential. The coexpression of increased MMP-7 and perlecan has a crucial impact on the progression of dysplasia toward carcinoma [67]. Further, it has been reported that the expressions of MMP-1 and -9 in oral dysplastic lesions are associated with carcinogenesis [36]. MMP-2 along with MMP-9 overexpression and the loss of basal lamina collagen IV α chain indicate progression toward malignancy [20, 88].
Abberation in Cytokeratin Expressions
During assessment of deregulation in epithelial progressive maturation in dysplastic PMDs, the expression profiles of different cytokeratins are important. Studies showed the upregulation of CK1, CK2, CK6, and CK10 in suprabasal layers along with the same trend of CK5, CK 14, and CK17 in both basal and suprabasal layers in OED. CK15 and CK19 show downregulation only in the basal layer [12]. Extension of CK19 expression from basal layer to suprabasal layer is also an indication of OED which is known to be a marker of premalignant changes of oral epithelium [47] and its use is suggested in grading of OED [75]. Further, there are reports of downregulation of CK4 and CK13 in the suprabasal layer, where the former was found to be more specific, while marked loss of the latter is an indicator for dysplastic transformation, and its progression [44]. Another study showed increased CK 4 and CK 13 overexpression in OED [63], and interestingly, despite being a biomarker of dysplasia, downregulation of these two cytokeratins and cornulin shows ambiguity in the prediction of malignant transformation [79]. However, their aberrant expressions were found to be linked with impaired epithelium maturation too, with increased cell motility along with altered CK6, CK16, and CK17 expressions [77].
Cell Growth and Adhesion Markers
Integrins, the cell surface receptors responsible for cell–cell and cell–extracellular matrix adhesion as well as cell growth are important in assessing OED. The α9 integrin was found to be upregulated [30] and suprabasal expressions of α6β4 [27] and α3β1 were found to be altered [67]. In OED, cytoplasmic localization of claudin, one of the main tight junction forming proteins indicates loss of activity. It can be correlated with moderate to severe [15]. Basal and suprabasal TWIST expression, a downstream protein of FGF, in dysplastic OLK indicates malignant transformation [83]. Interestingly, while one reported no expression of alpha-smooth muscle actin (SMA) and vimentin in OED, another study finds SMA expression in high-risk OED [16, 23].
Cell Proliferation Markers
Cell proliferation is a fundamental criterion in maintaining epithelial functional homeostasis. The important epithelial proliferation markers, viz. MCM2, geminin, and KI 67 were found to be elevated in OED. MCM2 possesses efficiency for indicating malignant potentiality [91]. In dysplastic OLK, KI 67 is overexpressed, and expression was reported up to the superficial layer [48]. Frequency of upregulation of suprabasal KI67 expression in dysplasia adjacent to OSCC indicates severity of the lesion [29], whereas coexpression of KI 67 and p53 with increased dysplasia points toward increased chances of malignancy [31, 43]. Centromere-associated protein CENP-F, and another two proliferation markers, KI 67 and cyclin D1 are also upregulated in OED, and mainly in the superficial layer of dysplastic OLK [49]. Cyclins and cyclin-dependant kinases (CDK) are the important factors for cellular proliferation. Cyclin D, is found to be overexpressed in OSCC, but not in dysplastic epithelia, whereas Cyclin E is overexpressed in severe dysplasia and its progression. Again overexpression of cyclin D1 was also reported by many [49, 74]. Interestingly, CDK2 is not expressed in normal or dysplastic epithelium, but overexpressed in OSCC, whereas CDK4 expression is parallel with the degree of dysplasia in cases of OED [82]. Expression of HER2/neu was not found to have any contributory effect on OED-associated carcinogenesis [80] and its expression was found to be very low in OED too [25].
Neo-Angiogenic Attributes
Neo-angiogenesis is one of the major hallmarks of cancer. VEGF expression study and vessel counting are the major methods still followed for angiogenesis determination in PMDs [56]. Most of the studies suggest a positive correlation between increasing grade of dysplasia with increasing VEGF expression from basal to suprabasal layer and increased microvessel density (MVD). Conflicting reports are also noted about such correlation [18]. Interestingly, another study indicated that though expression of VEGF-A did not correlate with grade of dysplasia in PMDs [34], the mean MVD was greater in dysplastic conditions than non-dysplastic ones [62]. VEGF-A is also found to be more upregulated in dysplastic OLK than non-dysplastic OLK [26, 62]. Further an increase in furin and VEGF-C expression during normal to dysplastic change of the oral mucosa is considered important as increase in new blood vessel formation was detected. It also indicates the presence of neo-angiogenic switch in OED [69]. Study of tumorigenic angiogenesis through molecular expression of CD105 or endoglin is the current method to determine the malignant potentiality. In dysplastic OSF, its expression was found to be upregulated [7, 21]. Other important modulators of neo-angiogenesis, like, fibroblast growth factor (FGF), transforming growth factor (TGF)-β, tumor necrosis factor (TNF)-α, etc. [93], also manifest their role in growth stimulation. FGF-binding protein- 1, (FGFBP-1) may be considered as one of the important angiogenic factors which can induce FGF-2 and VEGF-1, which are found to be upregulated in angiogenesis [67]. FGF-2 and FGFR-2 mainly express in the basal and parabasal layers, but in OED, it extends to the entire level with increased severity and there is subsequent loss of FGF-1 [94]. TGF- α level also increases with increasing dysplasia [87]. Enzyme nitric oxide synthase (NOS), a component responsible for synthesis of NO and induced NOS, may have role in angiogenesis and is related to dysplasia; the expression of the latter is found to be increased with severity of OED [14, 73]. Decorin, a leucine-rich proteoglycan has a role in both proliferation and angiogenesis, is also overexpressed in OED [9] nuclear localization of which may indicate increased malignant potentiality [22].
Deregulation of Apoptosis
Apoptosis is a very complex phenomenon, which occurs by two major pathways, intrinsic and extrinsic. Apoptotic proteins, consisting of anti-apoptotic and pro-apoptotic factors regulate apoptosis in cells. Bcl-2-associated x proteins (Bax) like Bax, Bad, Bak, and Bcl-xS are pro-apoptotic and Bcl-2 and Bcl-xL are anti-apoptotic proteins. p53, an important regulator of genomic integrity initiates the molecular cascade of apoptosis, or activates DNA repair when required. c-myc, a proto-oncogene can also induce apoptosis with p53 [38]. In PMDs, suprabasal expression of p53 along with an increase in dysplasia is an indicator of malignancy [5, 19]. Reddy et al. suggested moderate and severe dysplastic lesions showing intracellular localization of p53 indicating increased malignant potentiality [71]. Kerdpon et al. also found increasing expression of p53 in normal to dysplasia to OSCC, and thus suggested its association with carcinogenesis [40]. Abraho et al. found p53 expression in the entire dysplastic area of oral lesions, but did not find any correlation in expression and the degree of dysplasia [1]. p73, a functional homolog of p53 also induces apoptosis and overexpression from the basal to suprabasal layer during normal to dysplastic to OSCC [17].
The expression profile of BCL-2 is controversial in OED. Loro et al. found decreased expression of BCL-2 in the basal layer of OED, but in severe dysplasia the loss is less pronounced [53], whereas Singh et al. suggested that an increase in the expression of BCL-2 is directly proportional to the degree of epithelial dysplasia, but is downregulated in differentiating carcinomas [84]. Upregulation of BCL-2 protein in dysplastic epithelium adjacent to an invasive tumor may also indicate its role in malignant transformation [35]. BCL-2 is also expressed in OLK with apparent dysplasia [70]. The expression profile of Bax in dysplastic lesions is similar to the normal ones, but with an increased degree of dysplasia, an inverse relationship is observed in Bcl-2/Bax ratio [52]. Survivin, an inhibitor of apoptosis was also found to be overexpressed in OED [64]. One study suggested increased expression of the component, while another study suggested p34cdc2-cyclin B1-mediated phosphorylation of survivin on Thr34 as the underlying cause of carcinogenesis [100, 101]. A proto-oncogene c-jun, important in apoptosis as well as cell cycle regulation is increased in OED, according to the degree of dysplasia [92]. The main executioner caspase of apoptosis, caspase 3 expression is not affected in dysplastic tissues [46].
Molecules Related to Growth-Stimulatory and Anti-growth Signaling Proteins
Self-sufficiency in growth signals and insensitivity to anti-growth signals are considered as two major hallmarks of cancer. Epidermal growth factor receptor (EGFR) and its ligand, Transforming Growth Factor alpha (TGF-α), and their receptors are few which are upregulated in carcinomas, but their expression is also dysregulated in OED. Two- to fourfold of EGFR gene amplification is found in OED [58]. In OLK, one study suggested linear correlation between EGFR overexpression in stratum spinosum with increasing degree of dysplasia [87]. Another stated that its expression is not associated with dysplasia. It did not also vary between smokers and non-smokers, and there was a positive correlation with malignant potential [72].
A number of events, namely loss of heterozygosity, hypermethylation, deletion, and mutation are found to be associated with OED. Heterogeneity in p21 expression in PMDs, along with overexpression in proliferating dysplasia, suggests its role in oral oncogenesis [2]. Both p16INK4a and p14ARF are inactivated in OED, but to a greater extent in the former which is found to be inactivated in dysplastic oral epithelial lesions by the deletion of exon 1α of the CDKN2A gene. This gene encodes p16 and p14ARF, and is supposed to be more evident in conversion from dysplasia to malignancy [81]. In proliferative verrucous OLK, loss of p16INK4a and p14ARF is more than other dysplastic OLK lesions with elevated p14ARF exon 1β deletions [41]. A cell cycle inhibitory protein p57 expression is downregulated in OED and leads to carcinogenesis [24]. Downregulation of p27 (Kip1) along with p53 indicates an increase in the malignant potentiality of OED [42].
Role of Combinatorial Analysis of Molecular Expression in OED
In the context of value addition to analytical approaches for high-precision pathological grading of malignant potentiality of OED, association to biomarkers needs evaluation from different dimensions. Recent studies focus on the development of risk assessment tool using a combinatorial grading through computational analysis of clinico-epidemiological, demographic, and molecular perspectives [45]. When only clinicopathological aspects are considered, malignant potentiality could be assessed only after follow-up studies using the Kaplan–Meier method and log-rank test [39, 50]. Oral cancer-free survival (OCFS) studies in the OED are another approach. The study is determined using time-to-event analysis. Previously concurrent salivary marker detection was proposed as cancer diagnostic tool [59]. Analysis of gene profile data through multivariate predictive models generated for assessment of malignant potentiality has shown better prediction than existing models generated by clinicopathological risk factors [39]. However, it is a costly alternative. Hazard ratio analysis—when considered alone as a tool for the selection of biomarkers can assess increment in malignant potentiality, whereas Cox proportional hazard model was proposed to utilize clinical, demographic, and molecular factors to predict malignant potentiality [39]. The backward variable selection method was also used to generate a tool for assessing malignant potentiality of OED through selecting optimal combinations of biomarkers from biomarkers from the EGFR pathway in a recent study [60]. This method has limitations as it is confined within a particular hallmark. Utilization of tissue microarrays (TMA) for biomarker discovery is a novel, but a costly approach [60]. A recent study utilized computer-based stain separation techniques for intensity quantification in immunohistochemistry studies in search for molecular selection to predict malignant potentiality too [6]. So, when follow-up studies are not possible, or multilevel data required for such above-mentioned models are scarce, the proposition intends to hypothesize a molecular pathology-based computational tool for selection of cardinal biomarkers from different cancer hallmarks for better malignant potentiality prediction of oral PMDs, considering the role of each biomarker expression pattern noted in different studies associated with cancer hallmarks. The concept has been depicted in Fig. 2.
Conclusion
Proposing a specific biological threshold for predicting the transformation of PMDs with OED into carcinoma still suffers from ambiguity and is an open diagnostic challenge. Molecular expression studies provide information about the important roles of the genes and proteins expressed in the progression of dysplastic condition to carcinoma. Indeed, biomarker studies can help to find pathobiological thresholds to predict the irreversible changes towards malignancy. Differences in the reagents and protocol used, the clinical condition of the study subjects, site of biopsy taken etc., are of immense value in the context of addressing controversies by using the information on expression of biomarkers in OED and their significance. Each of the individual cancer hallmarks is often connected by multiple biological pathways and is interrelated. Even many molecules have a role in multiple biological mechanisms. Utilization of more than one of those molecules, especially cardinal molecular attribute to the cancer hallmarks, may provide an overall picture of onset of dysplasia and its progression toward malignancy. For example, abnormality in the onset of dysplasia was diagnosed by simultaneous expression study of p16/pRb/cyclin D1 [85], similarly many other pathways can be utilized by this way. Studies have also encountered the simultaneous expression of more than one biomarker. Another study showed that dual p53/p16INK4a and triple p53/p16INK4a/Ki-67 aberrations in dysplastic OLK have higher malignant potentiality [61]. Inclusion of mathematical modeling studies like principle component analysis also helps in the selection of two to three specific markers for accurate diseases grading. Therefore, implementation of conventional histopathological study along with multiple molecular expression features may help the pathologists to design combinatorial diagnostic markers for early diagnosis of malignant potentiality of OED in PMDs. The high-precision oral dysplasia grading embedded with a combinatorial approach will thus enable medical practitioners to predict the malignant potentiality with irreversible changes toward carcinoma (Fig. 2).
References
Abrahao AC, Bonelli BV, Nunes FD, Dias EP, Cabral MG (2011) Immunohistochemical expression of p53, p16 and hTERT in oral squamous cell carcinoma and potentially malignant disorders. Braz Oral Res 25:34–41
Agarwal S, Mathur M, Shukla NK, Ralhan R (1998) Expression of cyclin dependent kinase inhibitor p21waf1/cip1 in premalignant and malignant oral lesions: relationship with p53 status. Oral Oncol 34:353–360
Al-Swiahb JN, Chen CH, Chuang HC, Fang FM, Tasi HT, Chien CY (2010) Clinical, pathological and molecular determinants in squamous cell carcinoma of the oral cavity. Futur Oncol (London, England) 6:837–850. doi:10.2217/fon.10.35
Alvarado CG et al (2011) Nuclear translocation of beta-catenin synchronized with loss of E-cadherin in oral epithelial dysplasia with a characteristic two-phase appearance. Histopathology 59:283–291. doi:10.1111/j.1365-2559.2011.03929.x
Angiero F et al (2008) Expression of p16, p53 and Ki-67 proteins in the progression of epithelial dysplasia of the oral cavity. Anticancer Res 28:2535–2539
Anura A et al (2014) Computer-aided molecular pathology interpretation in exploring prospective markers for oral sub-mucous fibrosis progression. Head Neck. doi:10.1002/hed.23962
Anura A, Das RK, Pal M, Paul RR, Ray AK, Chatterjee J (2014) Correlated analysis of semi-quantitative immunohistochemical features of E-cadherin, VEGF and CD105 in assessing malignant potentiality of Oral submucous fibrosis. Pathol Res Pract 210:1054–1063. doi:10.1016/j.prp.2014.06.009
Bahar R, Kunishi M, Kayada Y, Yoshiga K (1997) CD44 variant 6 (CD44v6) expression as a progression marker in benign, premalignant and malignant oral epithelial tissues. Int J Oral Maxillofacc Surg 26:443–446
Banerjee AG, Bhattacharyya I, Lydiatt WM, Vishwanatha JK (2003) Aberrant expression and localization of decorin in human oral dysplasia and squamous cell carcinoma. Cancer Res 63:7769–7776
Bankfalvi A, Krassort M, Buchwalow IB, Vegh A, Felszeghy E, Piffko J (2002) Gains and losses of adhesion molecules (CD44, E-cadherin, and beta-catenin) during oral carcinogenesis and tumour progression. J Pathol 198:343–351. doi:10.1002/path.1204
Bankfalvi A, Krassort M, Vegh A, Felszeghy E, Piffko J (2002) Deranged expression of the E-cadherin/beta-catenin complex and the epidermal growth factor receptor in the clinical evolution and progression of oral squamous cell carcinomas. J Oral Pathol Med 31:450–457
Bloor B, Seddon S, Morgan P (2001) Gene expression of differentiation-specific keratins in oral epithelial dysplasia and squamous cell carcinoma. Oral Oncol 37:251–261
Bortoluzzi MC, Yurgel LS, Dekker NP, Jordan RC, Regezi JA (2004) Assessment of p63 expression in oral squamous cell carcinomas and dysplasias Oral Surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 98:698–704
Brennan PA, Palacios-Callender M, Sinclair D, Spedding AV, Zaki GA (2000) Does expression of inducible nitric oxide synthase correlate with severity of oral epithelial dysplasia? J Cranio-maxillo-fac Surg 28:44–48. doi:10.1054/jcms.2000.0108
Carvalho Mde V, Pereira Jdos S, Costa Ade L, de Souza LB, Freitas Rde A, Miguel MC (2010) Alterations in the immunoexpression of claudin-1 between different grades of oral epithelial dysplasias. Arch Oral Biol 55:261–267. doi:10.1016/j.archoralbio.2010.02.001
Chaudhary M, Gadbail AR, Vidhale G, Mankar Gadbail MP, Gondivkar SM, Gawande M, Patil S (2012) Comparison of myofibroblasts expression in oral squamous cell carcinoma, verrucous carcinoma, high risk epithelial dysplasia, low risk epithelial dysplasia and normal oral mucosa. Head Neck Pathol 6:305–313. doi:10.1007/s12105-012-0335-x
Chen YK, Hsue SS, Lin LM (2005) Expression of p63 protein and mRNA in oral epithelial dysplasia. J Oral Pathol Med 34:232–239
Choi S, Myers JN (2008) Molecular pathogenesis of oral squamous cell carcinoma: implications for therapy. J Dent Res 87:14–32
Cruz I et al (2002) Suprabasal p53 immunoexpression is strongly associated with high grade dysplasia and risk for malignant transformation in potentially malignant oral lesions from Northern Ireland. J Clin Pathol 55:98–104
Das RK et al (2013) Epithelio-mesenchymal transitional attributes in oral sub-mucous fibrosis. Exp Mol Pathol 95:259–269. doi:10.1016/j.yexmp.2013.08.006
Das RK et al (2010) Assessment of malignant potential of oral submucous fibrosis through evaluation of p63, E-cadherin and CD105 expression. J Clin Pathol 63:894–899
Dil N, Banerjee AG (2011) A role for aberrantly expressed nuclear localized decorin in migration and invasion of dysplastic and malignant oral epithelial cells. Head Neck Oncol 3:44. doi:10.1186/1758-3284-3-44
Etemad-Moghadam S, Khalili M, Tirgary F, Alaeddini M (2009) Evaluation of myofibroblasts in oral epithelia l dysplasia and squamous cell carcinoma. J Oral Pathol Med 38:639–643. doi:10.1111/j.1600-0714.2009.00768.x
Fan GK, Chen J, Ping F, Geng Y (2006) Immunohistochemical analysis of P57(kip2), p53 and hsp60 expressions in premalignant and malignant oral tissues. Oral Oncol 42:147–153. doi:10.1016/j.oraloncology.2005.06.017
Fong Y, Chou SJ, Hung KF, Wu HT, Kao SY (2008) An investigation of the differential expression of Her2/neu gene expression in normal oral mucosa, epithelial dysplasia, and oral squamous cell carcinoma in Taiwan. J Chin Med Assoc 71:123–127. doi:10.1016/s1726-4901(08)70003-0
Gandolfo M, Keszler A, Lanfranchi H, Itoiz ME (2011) Increased subepithelial vascularization and VEGF expression reveal potentially malignant changes in human oral mucosa lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 111:486–493. doi:10.1016/j.tripleo.2010.11.018
Garzino-Demo P, Carrozzo M, Trusolino L, Savoia P, Gandolfo S, Marchisio PC (1998) Altered expression of alpha 6 integrin subunit in oral squamous cell carcinoma and oral potentially malignant lesions. Oral Oncol 34:204–210
Godge PY, Poonja LS (2011) Quantitative assessment of expression of cell adhesion molecule (CD44) splice variants: CD44 standard (CD44s) and v5, v6 isoforms in oral leukoplakias: an immunohistochemical study. Indian J Dent Res 22:493–494. doi:10.4103/0970-9290.87080
Gonzalez-Moles MA, Ruiz-Avila I, Rodriguez-Archilla A, Martinez-Lara I (2000) Suprabasal expression of Ki-67 antigen as a marker for the presence and severity of oral epithelial dysplasia. Head Neck 22:658–661
Hakkinen L, Kainulainen T, Salo T, Grenman R, Larjava H (1999) Expression of integrin alpha9 subunit and tenascin in oral leukoplakia, lichen planus, and squamous cell carcinoma. Oral Dis 5:210–217
Humayun S, Prasad VR (2011) Expression of p53 protein and ki-67 antigen in oral premalignant lesions and oral squamous cell carcinomas: an immunohistochemical study. Natl J Maxillofac Surg 2:38–46. doi:10.4103/0975-5950.85852
Ikarashi T, Ida-Yonemochi H, Ohshiro K, Cheng J, Saku T (2004) Intraepithelial expression of perlecan, a basement membrane-type heparan sulfate proteoglycan reflects dysplastic changes of the oral mucosal epithelium. J Oral Pathol Med 33:87–95
Izumo T (2011) Oral premalignant lesions: from the pathological viewpoint. Int J Clin Oncol 16:15–26. doi:10.1007/s10147-010-0169-z
Johnstone S, Logan RM (2007) Expression of vascular endothelial growth factor (VEGF) in normal oral mucosa, oral dysplasia and oral squamous cell carcinoma. Int J Oral Maxillofac Surg 36:263–266. doi:10.1016/j.ijom.2006.09.017
Jordan RC, Catzavelos GC, Barrett AW, Speight PM (1996) Differential expression of bcl-2 and bax in squamous cell carcinomas of the oral cavity. Eur J Cancer Part B 32B:394–400
Jordan RC, Macabeo-Ong M, Shiboski CH, Dekker N, Ginzinger DG, Wong DT, Schmidt BL (2004) Overexpression of matrix metalloproteinase-1 and -9 mRNA is associated with progression of oral dysplasia to cancer. Clin Cancer Res 10:6460–6465. doi:10.1158/1078-0432.ccr-04-0656
Kainulainen T, Autio-Harmainen H, Oikarinen A, Salo S, Tryggvason K, Salo T (1997) Altered distribution and synthesis of laminin-5 (kalinin) in oral lichen planus, epithelial dysplasias and squamous cell carcinomas. Br J Dermatol 136:331–336
Kam P, Ferch N (2000) Apoptosis: mechanisms and clinical implications. Anaesthesia 55:1081–1093
Kaur J et al (2014) S100A7 overexpression is a predictive marker for high risk of malignant transformation in oral dysplasia. Int J Cancer 134:1379–1388. doi:10.1002/ijc.28473
Kerdpon D, Rich AM, Reade PC (1997) Expression of p53 in oral mucosal hyperplasia, dysplasia and squamous cell carcinoma. Oral Dis 3:86–92
Kresty LA, Mallery SR, Knobloch TJ, Song H, Lloyd M, Casto BC, Weghorst CM (2002) Alterations of p16(INK4a) and p14(ARF) in patients with severe oral epithelial dysplasia. Cancer Res 62:5295–5300
Kudo Y et al (2000) Reduced expression of p27(Kip1) correlates with an early stage of cancer invasion in oral squamous cell carcinoma. Cancer Lett 151:217–222
Kumar P, Kane S, Rathod GP (2012) Coexpression of p53 and Ki 67 and lack of c-erbB2 expression in oral leukoplakias in India. Braz Oral Res 26:228–234
Kuo MY, Cheng SJ, Chen HM, Kok SH, Hahn LJ, Chiang CP (1998) Expression of CD44s, CD44v5, CD44v6 and CD44v7-8 in betel quid chewing-associated oral premalignant lesions and squamous cell carcinomas in Taiwan. J Oral Pathol Med 27:428–433
Lee CH et al (2011) Intercountry prevalences and practices of betel-quid use in south, southeast and eastern Asia regions and associated oral preneoplastic disorders: an international collaborative study by Asian betel-quid consortium of south and east Asia. Int J Cancer 129:1741–1751. doi:10.1002/ijc.25809
Li SX, Chai L, Cai ZG, Jin LJ, Chen Y, Wu HR, Sun Z (2012) Expression of survivin and caspase 3 in oral squamous cell carcinoma and peritumoral tissue. Asian Pacific J Cancer Prev 13:5027–5031
Lindberg K, Rheinwald JG (1989) Suprabasal 40 kd keratin (K19) expression as an immunohistologic marker of premalignancy in oral epithelium. Am J Pathol 134:89–98
Liu SC, Klein-Szanto AJ (2000) Markers of proliferation in normal and leukoplakic oral epithelia. Oral Oncol 36:145–151
Liu SC et al (1998) Markers of cell proliferation in normal epithelia and dysplastic leukoplakias of the oral cavity. Cancer Epidemiol Biomark Prev 7:597–603
Liu W et al (2012) Oral cancer development in patients with leukoplakia–clinicopathological factors affecting outcome. PLoS One 7:e34773. doi:10.1371/journal.pone.0034773
Lo Muzio L et al (2009) beta- and gamma-catenin expression in oral dysplasia. Oral Oncol 45:501–504. doi:10.1016/j.oraloncology.2008.06.004
Loro LL, Johannessen AC, Vintermyr OK (2002) Decreased expression of bcl-2 in moderate and severe oral epithelia dysplasias. Oral Oncol 38:691–698
Loro LL, Johannessen AC, Vintermyr OK (2005) Loss of BCL-2 in the progression of oral cancer is not attributable to mutations. J Clin Pathol 58:1157–1162. doi:10.1136/jcp.2004.021709
Manchanda A, Shetty DC (2012) Reproducibility of grading systems in oral epithelial dysplasia. Med Oral Patol Oral Cir Bucal 17:e935–e942
Matsubara R et al (2011) Increased DeltaNp63 expression is predictive of malignant transformation in oral epithelial dysplasia and poor prognosis in oral squamous cell carcinoma. Int J Oncol 39:1391–1399. doi:10.3892/ijo.2011.1151
Michailidou EZ, Markopoulos AK, Antoniades DZ (2008) Mast cells and angiogenesis in oral malignant and premalignant lesions. Open Dent J 2:126–132. doi:10.2174/1874210600802010126
Moutasim KA et al (2011) Betel-derived alkaloid up-regulates keratinocyte alphavbeta6 integrin expression and promotes oral submucous fibrosis. J Pathol 223:366–377
Nagatsuka H, Ishiwari Y, Tsujigiwa H, Nakano K, Nagai N (2001) Quantitation of epidermal growth factor receptor gene amplification by competitive polymerase chain reaction in pre-malignant and malignant oral epithelial lesions. Oral Oncol 37:599–604
Nagler R, Bahar G, Shpitzer T, Feinmesser R (2006) Concomitant analysis of salivary tumor markers—a new diagnostic tool for oral cancer. Clin Cancer Res 12:3979–3984. doi:10.1158/1078-0432.ccr-05-2412
Nankivell P et al (2013) Tetraspanins CD9 and CD151, epidermal growth factor receptor and cyclooxygenase-2 expression predict malignant progression in oral epithelial dysplasia. Br J Cancer 109:2864–2874. doi:10.1038/bjc.2013.600
Nasser W, Flechtenmacher C, Holzinger D, Hofele C, Bosch FX (2011) Aberrant expression of p53, p16INK4a and Ki-67 as basic biomarker for malignant progression of oral leukoplakias. J Oral Pathol Med 40:629–635. doi:10.1111/j.1600-0714.2011.01026.x
Nayak S et al (2012) VEGF-A immunohistochemical and mRNA expression in tissues and its serum levels in potentially malignant oral lesions and oral squamous cell carcinomas. Oral Oncol 48:233–239. doi:10.1016/j.oraloncology.2011.10.003
Ohkura S et al (2005) Differential expression of the keratin-4, -13, -14, -17 and transglutaminase 3 genes during the development of oral squamous cell carcinoma from leukoplakia. Oral Oncol 41:607–613. doi:10.1016/j.oraloncology.2005.01.011
Oluwadara O, Giacomelli L, Christensen R, Kossan G, Avezova R, Chiappelli F (2009) LCK, survivin and PI-3K in the molecular biomarker profiling of oral lichen planus and oral squamous cell carcinoma. Bioinformation 4:249–257
Parikka M, Kainulainen T, Tasanen K, Vaananen A, Bruckner-Tuderman L, Salo T (2003) Alterations of collagen XVII expression during transformation of oral epithelium to dysplasia and carcinoma. J Histochem Cytochem 51:921–929
Pereira Jdos S, Carvalho Mde V, Henriques AC, de Queiroz Camara TH, Miguel MC, FreitasRde A (2011) Epidemiology and correlation of the clinicopathological features in oral epithelial dysplasia: analysis of 173 cases. Ann Diagn Pathol 15:98–102. doi:10.1016/j.anndiagpath.2010.08.008
Pitiyage G, Tilakaratne WM, Tavassoli M, Warnakulasuriya S (2009) Molecular markers in oral epithelial dysplasia: review. J oral Pathol Med 38:737–752. doi:10.1111/j.1600-0714.2009.00804.x
Poh CF, Ng S, Berean KW, Williams PM, Rosin MP, Zhang L (2008) Biopsy and histopathologic diagnosis of oral premalignant and malignant lesions. Journal (Canadian Dental Association) 74:283–288
Raica M, Cimpean AM, Ribatti D (1990) Angiogenesis in pre-malignant conditions. Eur J Cancer (Oxford, England) 45:1924–1934. doi:10.1016/j.ejca.2009.04.007
Ravi D, Nalinakumari KR, Rajaram RS, Nair MK, Pillai MR (1996) Expression of programmed cell death regulatory p53 and bcl-2 proteins in oral lesions. Cancer Lett 105:139–146
Reddy VM, Kamath A, Radhakrishnan RA (2012) p53 immunoprofiling of potentially malignant oral disorders: a case series analysis. Indian J Cancer 49:27–32. doi:10.4103/0019-509x.98913
Ribeiro DC, Gleber-Netto FO, Sousa SF, Bernardes VD, Guimaraes-Abreu MH, Aguiar MC (2012) Immunohistochemical expression of EGFR in oral leukoplakia: association with clinicopathological features and cellular proliferation. Med Oral Patol Oral Cir Bucal 17:e739–e744
Ridnour LA, Isenberg JS, Espey MG, Thomas DD, Roberts DD, Wink DA (2005) Nitric oxide regulates angiogenesis through a functional switch involving thrombospondin-1. Proc Natl Acad Sci USA 102:13147–13152. doi:10.1073/pnas.0502979102
Rousseau A, Lim MS, Lin Z, Jordan RC (2001) Frequent cyclin D1 gene amplification and protein overexpression in oral epithelial dysplasias. Oral Oncol 37:268–275
Safadi RA, Musleh AS, Al-Khateeb TH, Hamasha AA (2010) Analysis of immunohistochemical expression of k19 in oral epithelial dysplasia and oral squamous cell carcinoma using color deconvolution-image analysis method. Head Neck Pathol 4:282–289. doi:10.1007/s12105-010-0210-6
Saintigny P et al (2009) ΔNp63 overexpression, alone and in combination with other biomarkers, predicts the development of oral cancer in patients with leukoplakia. Clin Cancer Res 15:6284–6291
Sakamoto K et al (2011) Down-regulation of keratin 4 and keratin 13 expression in oral squamous cell carcinoma and epithelial dysplasia: a clue for histopathogenesis. Histopathology 58:531–542. doi:10.1111/j.1365-2559.2011.03759.x
Santos-Garcia A, Abad-Hernandez MM, Fonseca-Sanchez E, Julian-Gonzalez R, Galindo-Villardon P, Cruz-Hernandez JJ, Bullon-Sopelana A (2006) E-cadherin, laminin and collagen IV expression in the evolution from dysplasia to oral squamous cell carcinoma. Med Oral Patol Oral Cir Bucal 11:E100–E105
Schaaij-Visser TB, Bremmer JF, Braakhuis BJ, Heck AJ, Slijper M, van der Waal I, Brakenhoff RH (2010) Evaluation of cornulin, keratin 4, keratin 13 expression and grade of dysplasia for predicting malignant progression of oral leukoplakia. Oral Oncol 46:123–127. doi:10.1016/j.oraloncology.2009.11.012
Seifi S, Shafaei SN, Nosrati K, Ariaeifar B (2009) Lack of elevated HER2/neu expression in epithelial dysplasia and oral squamous cell carcinoma in Iran. Asian Pacific J Cancer Prev 10:661–664
Shahnavaz SA, Bradley G, Regezi JA, Thakker N, Gao L, Hogg D, Jordan RC (2001) Patterns of CDKN2A gene loss in sequential oral epithelial dysplasias and carcinomas. Cancer Res 61:2371–2375
Shintani S, Mihara M, Nakahara Y, Kiyota A, Ueyama Y, Matsumura T, Wong DT (2002) Expression of cell cycle control proteins in normal epithelium, premalignant and malignant lesions of oral cavity. Oral Oncol 38:235–243
Silva BS, Yamamoto FP, Pontes FS, Cury SE, Fonseca FP, Pontes HA, Pinto-Junior DD (2012) TWIST and p- Akt immunoexpression in normal oral epithelium, oral dysplasia and in oral squamous cell carcinoma. Med Oral Patol Oral Cir Bucal 17:e29–e34
Singh BB, Chandler FW Jr, Whitaker SB, Forbes-Nelson AE (1998) Immunohistochemical evaluation of bcl-2 oncoprotein in oral dysplasia and carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 85:692–698
Soni S et al (2005) Alterations of rb pathway components are frequent events in patients with oral epithelial dysplasia and predict clinical outcome in patients with squamous cell carcinoma. Oncology 68:314–325. doi:10.1159/000086970
Sperandio M et al (2013) Predictive value of dysplasia grading and DNA ploidy in malignant transformation of oral potentially malignant disorders. Cancer Prev Res (Phila) 6:822–831. doi:10.1158/1940-6207.capr-13-0001
Srinivasan M, Jewell SD (2001) Evaluation of TGF-alpha and EGFR expression in oral leukoplakia and oral submucous fibrosis by quantitative immunohistochemistry. Oncology 61:284–292
Tamamura R, Nagatsuka H, Siar CH, Katase N, Naito I, Sado Y, Nagai N (2013) Comparative analysis of basal lamina type IV collagen alpha chains, matrix metalloproteinases-2 and -9 expressions in oral dysplasia and invasive carcinoma. Acta Histochem 115:113–119. doi:10.1016/j.acthis.2012.05.001
Thomas V, Rema Devi S, Jeyaseelan V, Jeyseelan L (2012) Mucosal disorders with oral epithelial dysplasia risk-development of a simple screening tool for general health care setting. Oral Oncol 48:671–677. doi:10.1016/j.oraloncology.2012.02.011
Tilakaratne WM, Sherriff M, Morgan PR, Odell EW (2011) Grading oral epithelial dysplasia: analysis of individual features. J Oral Pathol Med 40:533–540. doi:10.1111/j.1600-0714.2011.01033.x
Torres-Rendon A, Roy S, Craig GT, Speight PM (2009) Expression of Mcm2, geminin and Ki67 in normal oral mucosa, oral epithelial dysplasias and their corresponding squamous-cell carcinomas. Br J Cancer 100:1128–1134. doi:10.1038/sj.bjc.6604967
Turatti E, da Costa NA, de Magalhaes MH, de Sousa SO (2005) Assessment of c-Jun, c-Fos and cyclin D1 in premalignant and malignant oral lesions. J Oral Sci 47:71–76
Vered M, Allon I, Dayan D (2009) Maspin, p53, p63, and Ki-67 in epithelial lesions of the tongue: from hyperplasia through dysplasia to carcinoma. J Oral Pathol Med 38:314–320. doi:10.1111/j.1600-0714.2008.00698.x
Wakulich C, Jackson-Boeters L, Daley TD, Wysocki GP (2002) Immunohistochemical localization of growth factors fibroblast growth factor-1 and fibroblast growth factor-2 and receptors fibroblast growth factor receptor-2 and fibroblast growth factor receptor-3 in normal oral epithelium, epithelial dysplasias, and squamous cell carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 93:573–579
Warnakulasuriya S (2009) Global epidemiology of oral and oropharyngeal cancer. Oral Oncol 45:309–316. doi:10.1016/j.oraloncology.2008.06.002
Warnakulasuriya S, Johnson NW, van der Waal I (2007) Nomenclature and classification of potentially malignant disorders of the oral mucosa. J Oral Pathol Med 36:575–580. doi:10.1111/j.1600-0714.2007.00582.x
Warnakulasuriya S, Reibel J, Bouquot J, Dabelsteen E (2008) Oral epithelial dysplasia classification systems: predictive value, utility, weaknesses and scope for improvement. J Oral Pathol Med 37:127–133. doi:10.1111/j.1600-0714.2007.00584.x
Williams HK, Sanders DS, Jankowski JA, Landini G, Brown AM (1998) Expression of cadherins and catenins in oral epithelial dysplasia and squamous cell carcinoma. J Oral Pathol Med 27:308–317
Yogesh T, Narayan T, Shreedhar B, Shashidara R, Leekymohanty (2011) The expression of E-cadherin and cathepsin-D in normal oral mucosa, oral epithelial dysplasia and oral squamous cell carcinoma: a comparative analysis between immunohistochemistry and routine Histopathology. J Oral Maxillofac Pathol 15:288–294. doi:10.4103/0973-029x.86689
Zhou S et al (2008) The phosphorylation of survivin Thr34 by p34cdc2 in carcinogenesis of oral submucous fibrosis. Oncol Rep 20:1085–1091
Zhou S et al (2010) Survivin as a potential early marker in the carcinogenesis of oral submucous fibrosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109:575–581. doi:10.1016/j.tripleo.2009.10.054
Author information
Authors and Affiliations
Corresponding author
Additional information
Endorsed by Jyotirmoy Chatterjee.
Rights and permissions
About this article
Cite this article
Banerjee, S., Chatterjee, J. Molecular Pathology Signatures in Predicting Malignant Potentiality of Dysplastic Oral Pre-cancers. Springer Science Reviews 3, 127–136 (2015). https://doi.org/10.1007/s40362-015-0033-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40362-015-0033-7