Abstract
Introduction
Hypertension (HTN) is a co-morbidity that is commonly associated with heart failure with preserved ejection fraction (HFpEF). However, it remains unclear whether treatment of hypertension in HFpEF patients is associated with improved cardiovascular outcomes.
Aim
The purpose of this meta-analysis is to evaluate the association of anti-hypertensive medical therapy with cardiovascular outcomes in patients with HFpEF.
Methods
We performed a database search for studies reporting on the association of anti-hypertensive medications with cardiovascular outcomes and safety endpoints in patients with HFpEF. The databases searched include OVID Medline, Web of Science, and Embase. The primary endpoint was all-cause mortality. Secondary endpoints include cardiovascular (CV) mortality, worsening heart failure (HF), CV hospitalization, composite major adverse cardiovascular events (MACE), hyperkalemia, worsening renal function, and hypotension.
Results
A total of 12 studies with 14062 HFpEF participants (7010 treated with medical therapy versus 7052 treated with placebo) met inclusion criteria. Use of anti-hypertensive medications was not associated with lower all-cause mortality, CV mortality or CV hospitalization compared to treatment with placebo (OR 1.02, 95% CI 0.77–1.35; p = 0.9, OR 0.88, 95% CI 0.73–1.06; p = 0.19, OR 0.99, 95% CI 0.87–1.12; p = 0.83, OR 0.90, 95% CI 0.79–1.03; p = 0.11). Anti-hypertensive medications were not associated with lower risk of subsequent acute myocardial infarction (AMI) (OR 0.53, 95% CI 0.07–3.73; p = 0.5). Use of anti-hypertensive medications was associated with a statistically significant lower risk of MACE (OR 0.90, 95% CI 0.83–0.98; p = 0.02).
Conclusions
While treatment with anti-hypertensive medications was not associated with lower risk of all-cause mortality, their use may be associated with reduce risk of adverse cardiovascular outcomes in patients with HFpEF regardless of whether they have HTN. Additional high quality studies are required to clarify this association and determine the effect based on specific classes of medications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Approximately 1 in 4 individuals in developing nations suffer from hypertension (HTN), and nearly a third are asymptomatic upon diagnosis [1]. Chronic elevations in blood pressure results in increased afterload, which in turn can result in structural and functional changes to the heart [2]. Potentially substantial cardiovascular complications of HTN include coronary artery disease, heart failure (HF), atrial fibrillation, and aortic aneurysm. A specific classification of HF is heart failure with preserved ejection fraction (HFpEF), or diastolic heart failure with a left ventricular ejection fraction (LVEF) greater than 50% [3]. HFpEF, especially in patients with HTN, has posed a therapeutic challenge to physicians.
Given HTN is responsible for approximately 25% of HF cases, the presence of HF requires stricter goal-directed therapy [2]. However, HTN remains a difficult disease to treat especially with regards to pharmacological adherence given that patients are generally asymptomatic, the medications pose additional adverse side-effects and treatment is largely preventative [1]. Lifestyle changes, including targeting major modifiable risk factors (such as tobacco use, physical activity, diet), is the initial treatment of choice, but may not be enough. Thus, pharmacological therapy provides an adjunctive tool. Less than half of all HTN patients can be treated with monotherapy, and nearly a third require three or more agents [1]. Moreover, little is known regarding the cardiovascular (CV) benefits of these antihypertensive pharmacologic agents on patients with HFpEF.
In this paper, we summarize the evidence evaluating the impact of antihypertensive medications on HFpEF patients with regard to CV outcomes: all-cause mortality, CV mortality, worsening HF, CV hospitalization, composite major adverse cardiovascular events (MACE), acute myocardial infarction (AMI). Moreover, we summarize the impact of antihypertensive medications on adverse pharmacologic side-effects in HFpEF patients, especially hyperkalemia, worsening renal function, and hypotension.
2 Methods
2.1 Data Search
This systematic review was performed in adherence to the guidelines of the PRISMA statement (Preferred Reporting Items for Systematic Reviews and Meta-analyses). The review was performed using a protocol in May 2023. The primary endpoint was mortality. Secondary endpoints included CV mortality, worsening HF, CV hospitalization, composite MACE, AMI, hyperkalemia, worsening renal function, and hypotension.
2.2 Search Strategy
A systematic search was conducted using Ovid MEDLINE, EMBASE, Scopus, Web of Science, and Google Scholar for relevant literature that reported an association between use of anti-hypertensive medications and all-cause mortality, CV mortality, worsening HF, CV hospitalization, composite MACE, AMI, hyperkalemia, worsening renal function, and hypotension. The search was not restricted to time or publication status. Two independent reviewers (MA and MT) performed an electronic search using the following keywords: “hypertension”, “heart failure preserved ejection fraction”, “hfpef”, “antihypertensive medication”, “antihypertensive”, “antihypertension”, “outcomes”, “outcome”, “mortality”, and “Prediction”. The references of the screened studies, systematic reviews, review articles, and meta-analyses were manually reviewed for potential studies. After identifying relevant studies, the full texts of the selected articles were examined by both reviewers based on preplanned inclusion criteria. Disagreements were resolved by consensus.
2.3 Study Selection
Studies were selected using the PICO (patient/population, intervention, comparison and outcomes) format to include those that studied patients with HFpEF (Population), comparing use of antihypertensive medications (Intervention) to not using them (Comparison), and assessing for all-cause mortality, CV mortality, worsening HF, CV hospitalization, composite MACE, AMI, hyperkalemia, worsening renal function, and hypotension. (Outcomes). Studies that did not separate HFpEF and HFrEF populations were excluded. Patients with hypertrophic cardiomyopathy were excluded.
2.4 Data Extraction
Two reviewers (MA and MT) independently extracted the study data using a predefined data extraction sheet. Variables that were extracted from the studies included: lead author, year of publication, study design, total patients on antihypertension medications, total patients not on antihypertension medications, mean follow-up, mean age, mean LVEF, and gender.
2.5 Statistical Analysis
Meta-analysis was performed using Cochrane Review Manager (RevMan) software, version 5. We used a random-effects model to examine the association between strain imaging and outcomes, which were presented with an odds ratio (OR) with 95% confidence interval (CI). The extent of heterogeneity was determined by I2 (ranging from 0 to 100%). Statistical significance was considered with a P-value < 0.05 and all tests were 2-sided.
3 Results
3.1 Literature Search and Study Selection
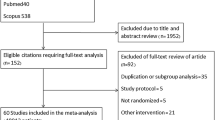
We identified 2376 eligible studies from our literature search. After screening all studies, 123 eligible studies were selected for full text review. 15 studies were identified to be eligible for meta-analysis for the planned outcomes. Details of the selection process is presented in Fig. 1.
3.2 Study and Patient Characteristics
A total of 12 studies with 14062 HFpEF participants (7010 treated with medical therapy versus 7052 treated with placebo) met inclusion criteria. Mean follow up was 31 months, mean age was 71 years, mean ejection fraction (EF) was 59% and 50.3% were females. Details of baseline demographic data is presented in Table 1.
Use of anti-hypertensive medications was not associated with lower all-cause mortality, CV mortality or CV hospitalization compared to treatment with placebo (OR 1.02, 95% CI 0.77–1.35; p = 0.9, OR 0.88, 95% CI 0.73–1.06; p = 0.19, OR 0.99, 95% CI 0.87–1.12; p = 0.83, OR 0.90, 95% CI 0.79–1.03; p = 0.11) (Figs. 2, 3, 4, 5). Anti-hypertensive medications were not associated with lower risk of subsequent acute myocardial infarction (AMI) (OR 0.53, 95% CI 0.07–3.73; p = 0.5) (Fig. 6).
Use of anti-hypertensive medications was associated with a statistically significant lower risk of MACE (OR 0.90, 95% CI 0.83–0.98; p = 0.02) (Fig. 7).
There was a non-significant trend toward lower risk of worsening HF in patients treated with anti-hypertensive medications with subgroup analysis demonstrating this association to be statistically significant in mixed populations of HFpEF patients with or without HTN but not significant in studies evaluating only HFpEF patients with HTN (OR 0.87, 95% CI 0.78–0.97; p = 0.02 versus OR 0.57, 95% CI 0.18–1.86; p = 0.35) (Fig. 8).
When testing the use of individual antihypertensive medications, they were associated with a lower risk of worsening HF and CV hospitalization (OR 0.86, 95% CI 0.77–0.96; p = 0.01; OR 0.88, 95% CI 0.80–0.96; p < 0.01) (Figs. 9, 10). These associations were primarily driven by use of mineralocorticoid receptor antagonists (MRAs) and angiotensin receptor blockers (ARBs) and not angiotensin-converting enzyme inhibitors (ACEs). The heterogeneity for these analyses were low (I2 = 0%).
Use of antihypertensive medications was associated with a significantly higher risk of hyperkalemia and worsening renal function (OR 3.10, 95% CI 1.57–6.13; p < 0.01; OR 1.81, 95% CI 1.48–2.23; p < 0.01). Use of antihypertensive medications was not associated with a significant risk of hypotension (OR 1.37, 95% CI 0.75–2.52; p-0.31) (Figs. 11, 12, 13).
4 Discussion
This systematic review and meta-analysis evaluated the role of antihypertensive medications on HFpEF patients with regards to adverse CV outcomes, as well as the impact of these standard medical therapies on potential adverse side effects. The main findings were as follows: (a) anti-hypertensive medication use was not associated with lower all-cause mortality, CV mortality, CV hospitalization or AMI; (b) use of anti-hypertensive medications was associated with a statistically significant lower risk of MACE; (c) there was a non-significant trend toward lower risk of worsening HF with the use of anti-hypertensive medications however subgroup analysis demonstrated this association to be statistically significant in mixed populations of HFpEF patients with and without HTN; (d) mineralocorticoid receptor antagonists (MRAs) and angiotensin receptor blockers (ARBs) but not angiotensin-converting enzyme inhibitors (ACEs) were associated with a lower risk of worsening HF and CV hospitalization; (e) Use of antihypertensive medications was associated with a significantly higher risk of hyperkalemia and worsening renal function, but not hypotension.
HTN remains one of the leading etiologies for the development of HFpEF [1, 4,5,6]. The 2015 SPRINT trial further demonstrated that patient’s undergoing blood pressure control of at least a target systolic blood pressure of 120mmHg or less had a reduced progression to heart failure compared to those with less intensive control [7]. Thus, current class 1 guidelines recommend titrating antihypertensive medications to attain target blood pressure values in patients with HTN and HFpEF as to prevent worsening HF and/or HF exacerbations [8]. However, little is known on the impact of antihypertensive medications on CV outcomes in HFpEF patients. The traditional pathophysiology behind development of HFpEF in HTN patients emphasizes the role of increased afterload on the LV, resulting in LV hypertrophy. This hypertrophied myocardium not only results in diastolic dysfunction, but also reduced capillary density, increasing risk of ischemia and conduction disorders. Thus, it is theorized LV mass and hypertrophy are predictors of adverse outcomes, and the risk can be reduced with LV hypertrophy regression [9, 10].
Several agents have demonstrated LV hypertrophy regression, with medications targeting the renin-angiotensin-aldosterone system (RAAS) system demonstrating the greatest results [11,12,13,14]. However, our results demonstrate antihypertensive agents were associated with reduction in MACE but not associated with reduction in all-cause mortality, CV mortality, CV hospitalization or AMI. Our results demonstrated that there was a trend toward lower risk of worsening HF with the use of anti-hypertensive medications; however, it was nonsignificant. These results have been reaffirmed in several groundbreaking trials, such as I-PRESERVE, CHARM-Preserved, PARAGON-HF, OPTIMIZE-HF and TOPCAT trials, all of which demonstrated no significant difference in the primary adverse CV endpoints with the use of their respectively studied antihypertensive agents [15,16,17,18,19]. Moreover, subgroup analyses with certain antihypertensive agents suggested majority of the benefit may have favored patients with an ejection fraction of 40–49%, and mid-range ejection fractions have shown clinical features resembling heart failure and a reduced ejection fraction (HFrEF) rather than HFpEF [19,20,21,22]. Thus, even though our subgroup analysis demonstrated MRAs and ARBs were associated with lower risk of worsening HF and CV hospitalization, the scope of this paper did not further analyze by ejection fraction range, which could limit the generalizability of the results. Nonetheless, the lack of overall improvement in CV outcomes in HFpEF patients with antihypertensive medications questions if the pathophysiology linking HTN and HFpEF is as simplified as hypertrophied myocardium.
An additional emerging model delineating the role HTN plays in HFpEF focuses on systemic inflammation. The inflammation from HTN results in coronary microvascular endothelial dysfunction, resulting in decreased protein kinase G activity, which results in cardiomyocyte hypertrophy and ventricular stiffening [23, 24]. Thus, improving CV mortality in HFpEF and HTN patients may be due to combating the proinflammatory state of HFpEF. The remarkable EMPEROR-Preserved trial demonstrated the ability of Empagliflozin to reduce the combined risk of CV death or hospitalization in HFpEF patients with/without diabetes [25]. As a sodium–glucose cotransporter 2 inhibitor (SGLT2i), empagliflozin reduces epicardial adipose tissue and alters adipokine signaling, impacts cardiomyocyte ionic homeostasis and reduce myofilament stiffness and extracellular matrix remodeling, all of which further reduces inflammation and oxidative stress [26]. Given SGLT2i are not classified as traditional antihypertensive agents, they were not extensively studied in this paper. However, they demonstrate the need for further investigation on the pathophysiology connecting HFpEF and HTN.
Similar to all medications, antihypertensive agents do not come without their unique adverse side effect profiles. Our results demonstrate the use of antihypertensive medications was associated with a significantly higher risk of hyperkalemia and worsening renal function. Similar results were seen in previous trials [18]. However, these side-effects could be combated with close and frequent monitoring. Thus, it is beneficial to adopt an individualized and patient-centered approach in the management of patients with HFpEF.
5 Conclusion/Future Direction
Our present systematic review and meta-analysis has important clinical implications. HFpEF remains a challenging entity to treat, and the use of antihypertensive medications are not associated with overall reduction in adverse CV outcomes, with the exception of MACE and a trend toward reduction in worsening HF. Lastly, standard medical therapy with antihypertensive agents do pose significant side effects and require close monitoring. Despite the results of this recent meta-analysis, several questions regarding HFpEF remain unanswered with regards to subgroup analysis of various antihypertensive agents across CV outcomes and ejection fraction ranges, and we need more evidence before we can extend these findings (and recommendations) to patients.
6 Limitations
Our review has several limitations. First, not all studies specified the type of antihypertensive agent. Second, not all studies specified the etiology of HFpEF or ejection fraction range. Third, there was heterogenicity with regard to long-term follow-up period. Forth, only a few studies distinguished between all-cause and CV mortality. Additional high-quality studies are required to elucidate the association of the use of antihypertensive agents in HFpEF patients with other cardiovascular outcomes.
References
Ashley EA, Niebauer J. Cardiology explained. Remedica Copyright © 2004, Remedica.: London; 2004.
Tackling G, Borhade MB. Hypertensive Heart Disease, in StatPearls. StatPearls Publishing Copyright © 2023, StatPearls Publishing LLC.: Treasure Island (FL); 2023. Ineligible companies. Disclosure: Mahesh Borhade declares no relevant financial relationships with ineligible companies.
Gazewood JD, Turner PL. Heart failure with preserved ejection fraction: diagnosis and management. Am Fam Physician. 2017;96(9):582–8.
Chobanian AV, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–71.
Levy D, et al. The progression from hypertension to congestive heart failure. JAMA. 1996;275(20):1557–62.
Vasan RS, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med. 2001;345(18):1291–7.
Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, Reboussin DM, Rahman M, Oparil S, Lewis CE, Kimmel PL, Johnson KC, Goff DC Jr, Fine LJ, Cutler JA, Cushman WC, Cheung AK, Ambrosius WT. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103–16.
Heidenreich PA, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2022;145(18):e895–1032.
Verdecchia P, et al. Left ventricular mass and cardiovascular morbidity in essential hypertension: the MAVI study. J Am Coll Cardiol. 2001;38(7):1829–35.
Levy D, et al. Prognostic implications of baseline electrocardiographic features and their serial changes in subjects with left ventricular hypertrophy. Circulation. 1994;90(4):1786–93.
Devereux RB, et al. Regression of hypertensive left ventricular hypertrophy by losartan compared with atenolol: the Losartan Intervention for Endpoint Reduction in Hypertension (LIFE) trial. Circulation. 2004;110(11):1456–62.
Dahlöf B, Pennert K, Hansson L. Reversal of left ventricular hypertrophy in hypertensive patients: a metaanalysis of 109 treatment studies. Oxford: Oxford University Press; 1992.
Klingbeil AU, et al. A meta-analysis of the effects of treatment on left ventricular mass in essential hypertension. Am J Med. 2003;115(1):41–6.
Ruilope LM, Schmieder RE. Left ventricular hypertrophy and clinical outcomes in hypertensive patients. Am J Hypertens. 2008;21(5):500–8.
Massie BM, et al. Irbesartan in patients with heart failure and preserved ejection fraction. N Engl J Med. 2008;359(23):2456–67.
Yusuf S, et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-Preserved Trial. Lancet. 2003;362(9386):777–81.
Hernandez AF, et al. Clinical effectiveness of beta-blockers in heart failure: findings from the OPTIMIZE-HF (Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure) Registry. J Am Coll Cardiol. 2009;53(2):184–92.
Pitt B, et al. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014;370(15):1383–92.
Solomon SD, et al. Angiotensin–neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med. 2019;381(17):1609–20.
Lund LH, et al. Heart failure with mid-range ejection fraction in CHARM: characteristics, outcomes and effect of candesartan across the entire ejection fraction spectrum. Eur J Heart Fail. 2018;20(8):1230–9.
Butler J, Anker SD, Packer M. Redefining heart failure with a reduced ejection fraction. JAMA. 2019;322(18):1761–2.
Pascual-Figal DA, et al. Mid-range left ventricular ejection fraction: clinical profile and cause of death in ambulatory patients with chronic heart failure. Int J Cardiol. 2017;240:265–70.
Paulus WJ, Tschöpe C. A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J Am Coll Cardiol. 2013;62(4):263–71.
van Heerebeek L, et al. Low myocardial protein kinase G activity in heart failure with preserved ejection fraction. Circulation. 2012;126(7):830–9.
Anker SD, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. 2021;385(16):1451–61.
Pandey AK, et al. Mechanisms of benefits of sodium-glucose cotransporter 2 inhibitors in heart failure with preserved ejection fraction. Eur Heart J. 2023;44(37):3640–51.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflict of interest
The authors report no relevant conflicts of interest.
Compliance with ethical standards (guidelines statement)
The systematic review was conducted with a protocol in accordance with the Preferred Reporting of Items for Systematic reviews and Meta-Analyses (PRISMA) statement.
Ethical approval
The study is a systematic review and meta-analysis; no ethical approval was required.
Data availability
Not applicable.
Rights and permissions
About this article
Cite this article
Al-Sadawi, M., Tao, M., Dhaliwal, S. et al. Safety and Efficacy of Anti-Hypertensive Medications in Patients with Heart Failure with Preserved Ejection Fraction: A Systematic Review and Meta-analysis. High Blood Press Cardiovasc Prev 31, 239–249 (2024). https://doi.org/10.1007/s40292-024-00646-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-024-00646-0