Abstract
Introduction
LV dysfunction develops early in hypertension, even previously to left ventricular remodeling.
Aims
To determine the frequency of morphologic and functional heart abnormalities associated to abnormal modified Tei Index in untreated hypertensive (HBP) patients (p) with preserved ejection fraction (pEF).
Methods
Case–control study. Three groups: (1) HBP without left ventricular hypertrophy (LVH); (2) HBP with LVH; (3) non-HBP controls. Ejection fraction >54 % identified pEF. LVH measured by Devereux method. Systolic and diastolic functions assessed by standard echocardiography and tissue Doppler. 2013 ESH/ESC Hypertension Guidelines normal values were considered. Tei index measured at the lateral and septal LV walls in apical 4-chamber view by tissue Doppler, value >0.40 considered abnormal. Statistical analysis: multifactorial ANOVA test adjusted by sex and age, p < 0.05 statistically significant.
Results
The study included 14 controls, 88 HBP p without LVH, and 19 HBP p with LVH. The HBP p sample mean age was 58.7 ± 13.5 years and 52 (44.1 %) were males. Mean Tei Index was 0.35 ± 0.03 in controls; 0.42 ± 0.05 in HBP without LVH; and 0.42 ± 0.06 in HBP with LVH (p < 0.025). Abnormal Tei Index was present in 2p (14.3 %) controls; 64 p (72.7 %) HBP without LVH; and 15 p (78.9 %) HBP with LVH (p < 0.0009). Tissue Doppler’s wave was 8.4 ± 0.9 cm/s in controls; 8 ± 1.6 cm/s in HBP without LVH and 7.8 ± 1.1 cm/s in HBP with LVH.
Conclusions
(1) Left ventricular dysfunction is frequent in HBP p, even without LVH; (2) modified tissue Doppler Tei index is a useful tool for the diagnosis of left ventricular dysfunction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
The detection of the clinical syndrome of heart failure with preserved ejection fraction (HFpEF) is more common in hypertensive patients. A multivariate analysis had shown for every elevation of 10 mmHg in systolic blood pressure a 13 % increase in the likelihood of developing heart failure with an ejection fraction greater than 45 %. Hypertension, female gender and new atrial fibrillation are the strongest predictors of new HFpEF [1].
Approximately 50 % of hypertensive patients have left ventricular geometry changes, and about one third of them could develope left ventricular hypertrophy, more often of the eccentric type. On the other hand, hypertensive patients may present both systolic and diastolic dysfunction, even in the absence of left ventricular hypertrophy, which can be evaluated by magnetic resonance imaging, myocardial perfusion or echocardiography, this technique being the most widespread applied in medical practice [2]. In the SILVHIA study diastolic function of hypertensive patients with and without left ventricular hypertrophy was evaluated and compared with normotensive subjects. The left ventricular diastolic function was impaired in both groups of hypertensive patients. The differences between the two groups of hypertensive individuals compared to normotensive subjects were statistically significant, but no difference was observed between hypertensive patients with and without left ventricular hypertrophy [3]. In another study the relationship between levels of plasma NT-proBNP and left ventricular diastolic dysfunction in hypertensive patients without systolic dysfunction was investigated. High end-diastolic left ventricular pressure measured by the ratio of transmitral early diastolic flow peak to septal and lateral mitral annulus average early peak diastolic velocities (E/e′ ratio) was considered a parameter suggestive of diastolic dysfunction, and patients with an E/e′ ratio greater than 15 had the highest average value of NT-proBNP in that study; so, when it was over 119 pg/ml had a sensitivity of 87 % and a specificity of 100 % for the prediction of a left ventricular end-diastolic pressure elevation [4]. In this line, the presence or development of diastolic dysfunction is associated with an increased incidence of heart failure during follow-up after adjustment for age, hypertension, diabetes and the presence of coronary artery disease [5].
In the same context, systolic left ventricular function has being assessed by two-dimensional ultrasonographic methods, such as those derived from measurements of area and length of the cavity or volumetric methods based on Simpson’s rule which established the ejection fraction as the gold standard. With these methodologies it had been reported that systolic left ventricular function is preserved by more than 80 % of hypertensive patients. Moreover, although standard 2D echo Doppler and real time 3D echocardiography evaluation showed that the left ventricular mass index was greater and the diastolic function was worst in hypertensive subjects compared to healthy controls, the ejection fraction and the stroke volume were not significantly different between both groups [6, 7].
With these references, several groups of researchers, convinced that some of these concepts could be misguided, began to explore other methods of diagnosis that could explain these gaps of the conventional techniques, and at the same time, establish strategies to facilitate the diagnosis of early left ventricular dysfunction in patients with hypertension. Tissue Doppler and speckle tracking had emerged as very useful tools in this aspect. The Index of Left Ventricular Myocardial Performance, also known as TEI Index, described by this author in 1997, is a simple, reproducible, and noninvasive method to assess simultaneously left ventricular systolic and diastolic function, and has proven to possess a good correlation with invasive methods, being perhaps its best-known scope the clinical syndrome of heart failure with preserved systolic function [8].
Based on the evidence presented previously, this study hypothesized that LV dysfunction develops early in hypertension, even previously to left ventricular remodeling, which could be diagnosed precociously by the modified Tei index, favoring therapeutic strategies to prevent heart damage and improve cardiovascular prognosis.
The aim of this study is to determine the frequency of morphologic and functional heart abnormalities associated to a high modified Tei Index in untreated hypertensive patients with preserved ejection fraction.
2 Material and Methods
This is a descriptive cross-sectional study, with a prospectively collected sample conducted at the Cardiology Institute of the Sanatorio Británico SA in Rosario, Argentina. The study has been carried out in accordance with the Code of Ethics of the World Medical Association for experiments involving humans. Inclusion criteria were: (1) untreated essential hypertensive patients over 18 years of age of both sexes at their first consultation, (2) non hypertensive controls confirmed by 24 h ambulatory blood pressure monitoring over 18 years of age of both sexes, (3) 2D and M Mode echocardiography, mitral Doppler and tissue Doppler of sufficient quality to perform the calculation of the LV mass and evaluate LV diastolic and systolic function; (4) ejection fraction measured by the modified Simpson biplane method >54 %. Exclusion criteria were: (1) clinical cardiovascular disease that could impact on the development of left ventricular hypertrophy or ventricular dysfunction, such as aortic or mitral valve disease, congenital heart disease, renal insufficiency, morbid obesity or thyroid disease (2) prior clinical diagnosis of heart failure syndrome (3) medical history of ischemic heart disease or prior diagnosis of coronary artery disease, (4) treatment with drugs that affect the heart rate at rest, (5) rhythm disturbances like right or left bundle branch block, atrio-ventricular block, pre-excitation syndrome, or supraventricular arrhythmias. The patients sample was divided in three groups: (1) non hypertensive controls, (2) non-treated hypertensive patients without left ventricular hypertrophy, and (3) non-treated hypertensive patients with left ventricular hypertrophy.
For the diagnosis of hypertension the 2013 European Society of Hypertension/European Society of Cardiology Guidelines for the Management of Arterial Hypertension criteria was applied [9]. Clinical arterial blood pressure was measured with a digital sphygmomanometer (OMRON model HEM-705CPINT), and the average of three consecutive measurements 1 min apart after 5 min in the sitting position is reported. Ambulatory blood pressure monitoring was performed with a Meditech ABPM-05 device according to the recommendations of the 2014 European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability [10].
The ultrasound studies were performed with an Esaote MyLab 7 ultrasound scanner provided by harmonic capability with a 2.5 MHz phase array multifrequency transducer with standardized protocol and conducting a tissue Doppler study by DP. The intraobserver variability was previously tested and the concordance was acceptable [11]. Echocardiographic parameters of two-dimensional images, standard and tissue Doppler images were post processed digitally by GT on blind condition. The left ventricular mass was assessed by the method of Devereux and indexed by body surface, and left ventricular hypertrophy was considered when its value was greater than 95 g/m2 in women and 115 g/m2 in men. The relative wall index was calculated as diastolic septal wall thickness plus diastolic left ventricular posterior wall thickness/diastolic left ventricular diameter, and a value ≤0.42 was considered normal. Diastolic function was assessed by conventional Doppler of the mitral valve orifice corrected by age and tissue Doppler of the interventricular septum and lateral wall at the mitral annulus level in the apical 4 chamber conventional view following the American Society of Echocardiography and the European Association of Echocardiography Guidelines [12, 13]. The ratio of transmitral early diastolic flow peak to septal and lateral mitral annulus average early diastolic peak velocities (E/e′ ratio) was measured as an indirect marker of left ventricular end diastolic pressure and a value ≥13 was considered abnormal. Systolic function was assessed by the average rate of systolic excursion (s wave) of the interventricular septum and lateral wall at the mitral annulus level in cm/s with tissue Doppler. End diastolic volume (EDV), end systolic volume (ESV), ejection fraction (EjF) and stroke volume (SV) were assessed by the modified Simpson biplane method and measured in ml and cardiac work (CW) was measured in g/min; and all were corrected by body surface area [14, 15]. Endocardial fractional shortening and midwall fractional shortening was measured according to the American Society of Echocardiography and the European Association of Echocardiography Guidelines [12, 13]. The TEI index was measured with tissue Doppler at the lateral and septal walls of the left ventricle in the apical 4-chamber view at the mitral annulus level, a methodology known as modified Tei index; three measurements were averaged in each wall of isovolumetric contraction time, ejection time and isovolumetric relaxation time, and a ratio >0.40 was considered abnormal [16–18] (Fig. 1).
Methodology for calculating the modified Tei index. Left image apical 4-chamber view showing tissue Doppler sample located at the interventricular septum at the mitral annulus level. Right image tissue Doppler spectrum in which s′, e′ and a′ waves are observed; the ejection time, isovolumic relaxation time and isovolumetric contraction time are delimited by yellow vertical lines. The formula for calculating modified Tei index, also known as myocardial performance index of the left ventricle, is equal to (isovolumic relaxation time + isovolumic contraction time)/ejection time. LV left ventricle, ET ejection time, IRT isovolumic relaxation time, ICT isovolumic contraction time
Statistical analysis: continuous variables are reported as means with their standard deviations and discrete variables as absolute values and percentages. For comparison between groups multifactorial ANOVA test adjusted by sex and age was applied, and a value of p < 0.05 was considered statistically significant.
3 Results
The study included 121 subjects of whom 14 were controls, 88 were untreated hypertensive patients without left ventricular hypertrophy (LVH), and 19 untreated hypertensive patients with LVH. The hypertension time evolution was 8.8 ± 9.3 years. The hypertensive patients sample mean age was 58.7 ± 13.5 years and 52 (44.1 %) of them were males. The mean body mass index of the hypertensive subjects sample was 28.7 ± 3.9 kg/m2 while the mean waist circumference was 99.5 ± 11.3 cm; at the same time 7 patients (5.9 %) were diabetics, 26 patients (22 %) were dyslipidemics, and 52 patients (44.1 %) smokers or former smokers. On the other side, the mean age of the controls was 46.5 ± 17.1 years and 6 subjects (42.9 %) were males. The Table 1 shows the baseline characteristics of controls, hypertensive patients without LVH and hypertensive patients with LVH.
The ejection fraction, the midwall fractional shortening and the endocardial fractional shortening of hypertensive patients with and without LVH was similar to that of control subjects, and the end diastolic volume, end systolic volume, stroke volume and stroke work were similar between controls subjects and hypertensive patients without LVH but hypertensive individuals with LVH had significantly higher end diastolic volume, stroke volume and stroke work than the other two groups (Table 2).
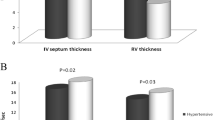
The mean left ventricular mass index (LVMI) of control subjects and hypertensive patients without LVH was significantly lower than in hypertensive patients with LVH (p < 0.005). At the same time, the relative wall index did not show significantly differences between the groups. Table 3 shows the results of the echocardiographic evaluation. The Tei Index was significantly more frequently abnormal in both groups of hypertensive patients compared to control subjects but any difference was detected between hypertensive patients with and without LVH. The observed differences were independent of differences in mean age and sex frequency observed among the three groups. The parameters of diastolic function like mean left atrial volume index, mean septal and lateral e′ wave velocities and mean E/e′ ratio were not significantly different in hypertensive subjects with and without LVH and controls. Results in the same direction were found with regard to systolic function measured as the mean of lateral and septal tissue Doppler’s wave.
4 Discussion
In 1995 C. Tei published a new non-invasive index for combined systolic and diastolic ventricular function evaluation, which was interrogated in many different scenarios like dilated cardiomyopathy, cardiac amyloidosis, Ebstein’s anomaly, in adults and fetus, in left ventricular and right ventricular dysfunction. This Doppler index was correlated to accepted indexes of left ventricular performance at cardiac catheterization in 34 patients with ischemic heart disease or idiopathic dilated cardiomyopathy and showed a statistically significant correlation with positive systolic peak dP/dt, negative diastolic peak dP/dt, and tau. So, the authors concluded that this simple, easily recordable, and noninvasive Doppler index of myocardial performance correlates with invasive measurements of left ventricular systolic and diastolic function [8, 16]. The methodology developed by C. Tei et al. to evaluate left ventricular performance requires obtaining two flow spectral images from conventional pulsed Doppler: mitral inflow and left ventricular outflow simultaneously with an electrocardiogram strip recording. Both velocities curves should be analyzed off line from those charts. The tissue Doppler derived Tei index has the advantage over the original research that all three intervals, ejection time, isovolumic relaxation time, and isovolumic contraction time could be obtained at the same time and simultaneously with an electrocardiogram strip recording so it could be processed off-line as well as on-line. The measurements could be performed at different levels of the 16 conventional left ventricular segments and the average of all them could be obtained [17].
The present study evaluated left ventricular function through the modified Tei index obtained in the septal and lateral mitral annulus in hypertensive patients with and without LVH and an ejection fraction higher than 54 % and compared the results to non-hypertensive controls. Both groups of hypertensive patients, independently of the presence of target organ damage, had significantly more frequently abnormal modified Tei index. At the same time, other parameters of diastolic left ventricular dysfunction like left atrial volume index, septal and lateral e′ tissue Doppler waves, and the E/e′ ratio were not more frequently abnormal in both hypertrophic and non-hypertrophic hypertensive patients compared to control subjects. In the same direction, systolic left ventricular function evaluated by the tissue Doppler s wave in the longitudinal axis was non-significantly reduced in hypertensive patients, although the decline was more significant in those with LVH. Any significant differences were detected in the ejection fraction, endocardial fractional shortening nor midwall fractional shortening neither between controls and hypertensives patients nor between hypertensive patients with and without LVH. Accordingly to this data, hypertension per se, even without the development of left ventricular structural remodeling, reduces systolic and diastolic function. The modified Tei index is a useful and accurate tool to diagnose these incipient and subtle abnormalities in hypertensive subjects with and ejection fraction over 54 %, and even more sensitive than other tissue Doppler parameters.
In concordance with this study, in a group of 306 new hypertensive subjects those with a Tei Index higher than 0.40 had a significantly increased left ventricular mass index and frequency of left ventricular hypertrophy, but the left ventricular ejection fraction was similar among groups. At the same time, these patients were older, had higher values of systolic and diastolic blood pressure, worst renal function, and higher levels of high-sensitivity troponin T, which is supposed to be a marker of myocardial damage, than patients with Tei index under 0.40. So the study by O. Kaypakli et al. confirms the low sensitivity to detect subtle left ventricular dysfunction in hypertensive patients with preserved ejection fraction by ultrasonographic volumetric derived parameters, and the need to have more efficient methods to this task like the modified Tei index [19].
In 60 non-treated new diagnosed hypertensive patients K. Takasaki et al. showed that between many clinical and ultrasonographic variables the Tei index was the only independently correlated with left ventricular mass index in a multiple regression analysis. At the same time, isovolumic contraction time and isovolumic relaxation time were independently correlated to left ventricular mass index, being the former strongest, whereas no correlation was detected with ejection time. An interesting point is that any relationship was found out between left ventricular mass index and ejection fraction. The differences between the geometric LV patterns and LV dysfunction were also analyzed, and the Tei index and isovolumic contraction time were significantly greater in subjects with concentric hypertrophy than in the other three geometric patterns. There were no significant differences in the ejection time among the four groups while the isovolumic relaxation time was significantly higher in concentric hypertrophy patients than in groups with normal geometry or concentric remodeling [20]. A limitation of the study of K. Takasaki et al. is that control non-hypertensive patients were not included. In the present study, the modified Tei Index was significantly higher in all hypertensive patients, independently of the presence or not of left ventricular hypertrophy, which means that LV dysfunction is related to the hypertensive disease itself, although an elevated Tei index was significantly more frequent in hypertensive patients with left ventricular hypertrophy.
The lack of relationship between left ventricular remodeling and dysfunction was confirmed in other scenarios, as showed by the study of A. Zwain et al. in which a group of thirty normal body mass index subjects were compared to thirty obese individuals, all of them neither hypertensives nor diabetics. In both groups left ventricular mass index was measured by the Devereux formula and left ventricular function was evaluated through the Tei index. There were any significant differences in the myocardial performance index between control and obese subjects groups and any correlation between this variable and left ventricular mass index [21]. Although this study surprisingly did not show any difference in left ventricular mass index nor in the eccentricity index between the controls subjects and obese patients, which is a limitation of the publication of A. Zwain et al., it supports the concept that in different clinical conditions left ventricular dysfunction could develope independently of left ventricular remodeling, probably due to the hemodynamic, neurohumoral or metabolic burden of the diseases themselves, and that the Tei index is a useful tool to detect this subtle early abnormalities. In the present study any statistically significant differences were observed in the body mass index between the three groups, therefore, the observed Tei index data are not justified by differences in body size.
5 Limitations
Performing a tissue Doppler echocardiography requires the availability of appropriate equipment and trained operators. Since hypertension is a condition basically assisted in primary care, to have this kind of resources is a limitation for wide dissemination of the procedure. However, considering that three out of four hypertensive patients without left ventricular hypertrophy with preserved ejection fraction have a modified abnormal Tei index, and it is not associated with other significant changes in the parameters that evaluate left ventricular function, incorporating the methodology into the routine ultrasound scanning should be an option to consider. The assessment of diastolic function, combined with the evaluation of systolic left ventricular function, have proven to be valuable tools to stratify the risk of heart failure hospitalizations and cardiovascular mortality in hypertensive patients and general population; and even though the initial ultrasonographic techniques like Doppler of mitral valve orifice did not provide incremental information when left ventricular hypertrophy is present, new procedures including tissue Doppler and 2 and 3-D speckle tracking seem positively modify this horizon [5, 22–24].
The mean lateral and septal walls diastolic e′ wave at longitudinal’ 4 chamber view obtained by tissue Doppler were lower, while the ratio of transmitral early diastolic flow peak to septal and lateral mitral annulus average early diastolic peak velocities (E/e′ ratio) was higher in hypertensive patients with LVH compared to the other two groups, but the differences between them did not reached statistical significance. Results in the same direction were obtained with regard to the average rate of systolic excursion (s wave) of the interventricular septum and lateral wall at the mitral annulus level with tissue Doppler which was lower than controls and hypertensive patients without LVH. The absence of distinctness in these parameters of diastolic and systolic function could be explain by the statistical power of the sample, so a type 2 error could be another limitation of the present study.
An analysis of the baseline characteristics of the sample shows that hypertensive patients were significantly older than control subjects and at the same time there were statistically significant differences in the ages of the three groups. Aware of these data an ANOVA test adjusted by sex and age was applied, and in fact, this adjustment increased the differences between groups. So, the significantly greater presence of LV dysfunction in hypertensive patients without LVH than in controls was not due to the sample characteristics. On the other side, the patients included in the study had predominantly isolated systolic hypertension since although ABPM diastolic blood pressure was higher in hypertensive patients than in controls, the mean 24 h was lower than 80 mmHg, and even hypertensive patients had higher diastolic blood pressures than controls the differences were not statistically significant.
6 Conclusions
This study shows that non-treated hypertensive patients have both abnormal systolic and diastolic function early in the development of their condition. The Left Ventricular Myocardial Performance Index, also known as TEI Index, and the tissue Doppler version called modified Tei index, are efficient tools to detect such subtle abnormalities. While the guidelines of clinical practice in hypertension do not introduce the concept of cardiac dysfunction for cardiovascular risk stratification, the recently published guidelines of the European Societies of Cardiology and Hypertension support to assess ventricular function with tissue Doppler depending on availability [9]. In this context, the modified TEI index, as a simple and reproducible tool evaluating simultaneously systolic and diastolic function, could become an essential procedure in assessing hypertensive patients with preserved ejection fraction.
References
Lee DS, Gona P, Vasan RS, Larson MG, Benjamin EJ, Wang TJ, Tu JV, Levy D. Relation of disease pathogenesis and risk factors to heart failure with preserved or reduced ejection fraction. Insights from the Framingham Heart Study of the National Heart, Lung, and Blood Institute. Circulation. 2009;119:3070–7.
Piskorz D, Citta L, Citta N, Citta P, Keller L, Bongarzoni L, Mata L, Tommasi A. Association of systolic dysfunction with left ventricular hypertrophy and diastolic dysfunction in hypertensive patients. Rev Fac Cien Med Univ Nac Cordoba. 2014;71:158–64.
Müller-Brunotte R, Kahan T, Malmqvist K, Ring M, Edner M. Tissue velocity echocardiography shows early improvement in diastolic function with irbesartan and atenolol therapy in patients with hypertensive left ventricular hypertrophy. Results from the Swedish Irbesartan Left Ventricular Hypertrophy Investigation vs Atenolol (SILVHIA). Am J Hypertens. 2006;19:927–36.
Ceyhan C, Unal S, Yenisey C, Tekten T, Ceyhan FB. The role of N terminal pro-brain natriuretic peptide in the evaluation of left ventricular diastolic dysfunction: correlation with echocardiographic indexes in hypertensive patients. Int J Cardiovasc Imaging. 2008;24:153–259.
Kane J, Karon BL, Mahoney DW, Redfield MM, Roger VL, Burnett JC Jr, Jacobsen SJ, Rodehefler RJ. Progression of left ventricular diastolic dysfunction and risk of heart failure. JAMA. 2011;306:856–63.
Bella JN, Palmieri V, Liu JE, Kitzman DW, Oberman A, Hunt SC, Hopkins PN, Rao DC, Arnett DK, Devereux RB, Hypertension Genetic Epidemiology Network Study Group. Relationship between left ventricular diastolic relaxation and systolic function in hypertension: the Hypertension Genetic Epidemiology Network (HyperGEN) Study. Hypertension. 2001;38:424–8.
Galderisi M, Esposito R, Schiano-Lomoriello V, Santoro A, Ippolito R, Schiattarella P, Strazullo O, de Simone G. Correlates of global area strain in native hypertensive patients: a three-dimensional speckle-tracking echocardiography study. Eur Heart J Cardiovasc Imag. 2012;13:730–8.
Tei C, Nishimura RA, Seward JB, Tajik AJ. Noninvasive Doppler-derived myocardial performance index: correlation with simultaneous measurements of cardiac catheterization measurement. J Am Soc Echocardiogr. 1997;10:169–78.
Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F, Task Force Members. 2013 ESH/ESC guidelines for the management of arterial hypertension. The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:1281–357.
Parati G, Stergiou G, O’Brien E, Asmar R, Beilin L, Bilo G, Clement D, de la Sierra A, de Leeuw P, Dolan E, Fagard R, Graves J, Head GA, Imai Y, Kario K, Lurbe E, Mallion JM, Mancia G, Mengden T, Myers M, Ogedegbe G, Ohkubo T, Omboni S, Palatini P, Redon J, Ruilope LM, Shennan A, Staessen JA, vanMontfrans G, Verdecchia P, Waeber B, Wang J, Zanchetti A, Zhang Y. European society of hypertension working group on blood pressure monitoring and cardiovascular variability. J Hypertens. 2014;32:1359–66.
Piskorz D, Tommasi A. La disfunción diastólica en pacientes hipertensos no es debida a hipertrofia ventricular izquierda. Ins Card. 2011;6:2–7.
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, Reichek N. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986;57:450–8.
Devereux RB, Pini R, Aurigemma GP, Roman MJ. Measurement of left ventricular mass: methodology and expertise. J Hypertens. 1997;15:801–9.
Lang RM, Biering M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ, Chamber Quantification Writing Group, American Society of Echocardiography’s Guidelines and Standards Committee, European Association of Echocardiography. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a Branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–63.
Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelista A. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr. 2009;22:107–33.
Tei C. New non-invasive index for combined systolic and diastolic ventricular function. J Cardiol. 1995;26:396–404.
Galiuto L, Ignone G, DeMaria A. Contraction and relaxation velocities of the normal left ventricle using pulsed-wave tissue Doppler echocardiography. Am J Cardiol. 1998;81:609–14.
Keser N, Yildiz S, Kurtoğ N, Dindar I. Modified TEI index: a promising parameter in essential hypertension? Echocardiography. 2005;22:296–304.
Kaypakli O, Gur M, Gozukara MY, Ucar H, Kivrak A, Şeker T, Şahin DY, Elbasan Z, Türkoğlu C, Çayli M. Association between high-sensitivity troponin T, left ventricular hypertrophy, and myocardial performance index. Herz. 2015;40:1004–10.
Takasaki K, Miyata M, Imamura M, Yuasa T, Kuwahara E, Kubota K, Kono M, Ueya N, Horizoe Y, Chaen H, Mizukami N, Kisanuki A, Hamasaki S, Tei C. Left ventricular dysfunction assessed by cardiac time interval analysis among different geometric patterns in untreated hypertension. Circ J. 2012;76:1409–14.
Zwain AA, Noaman AH, Al Esawi RW, Ponoth P. Myocardial performance index (MPI) is not influenced by increased left ventricular mass in healthy obese men. Cardiovasc Revasc Med. 2013;14:18–22.
De Simone G, Izzo R, Chinali M, De Marco M, Casalnuovo G, Rozza F, Girfoglio D, Iovino GL, Trimarco B, De Luca N. Does information on systolic and diastolic function improve prediction of a cardiovascular event by left ventricular hypertrophy in arterial hypertension? Hypertension. 2010;56:99–104.
Mogelbang R, Sogaard P, Pedersen SA, Olsen NT, Marott JL, Schnohr P, Goetze JP, Jensen JS. Cardiac dysfunction assessed by echocardiographic tissue Doppler imaging is an independent predictor of mortality in the general population. Circulation. 2009;119:2679–85.
Sharp AS, Tapp RJ, Thom SA, Francis DP, Hughes AD, Stanton AV, Zambanini A, O’Brien E, Chaturvedi N, Lyons S, Byrd S, Poulter NR, Sever PS, Mayet J, ASCOT Investigators. Tissue Doppler E/E′ ratio is a powerful predictor of primary cardiac events in a hypertensive population: an ASCOT sub-study. Eur Heart J. 2010;31:747–52.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was not presented previously as a whole or a part anywhere.
This study and its authors do not have sources of support, grants, equipment, drugs, or any combination of these.
The authors disclose funding received for this work from any organization.
The authors disclose any potential conflicts of interest or financial interests relevant to the research.
This study did not involve animals.
This study has been carried out in accordance with the Code of Ethics of the World Medical Association for experiments involving humans and the 1964 Helsinki declaration and its later amendments.
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Tissera, G., Piskorz, D., Citta, L. et al. Morphologic and Functional Heart Abnormalities Associated to High Modified Tei Index in Hypertensive Patients. High Blood Press Cardiovasc Prev 23, 373–380 (2016). https://doi.org/10.1007/s40292-016-0167-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-016-0167-y