Abstract
Global cardiovascular (CV) risk assessment tries to answer the questions: who will benefit from intervention? And when should non-pharmacologic and pharmacologic treatment be started? Used for the assessment of CV risk in the presence of one main CV risk factor, the presence of previous CV disease, diabetes, chronic kidney disease, coronary heart disease and severely elevated single risk factors, are situations with a high or very high risk. For the majority of subjects without any of the above, a calculation of risk can help to decide the best management. The methodology of assessing global CV risk has both strength and limitations. Several computational methods have been developed to assess global CV risk but no risk estimation can consider all the potential risk factors. The most used score chart is the Framingham CardioVascular Risk Score, although in Europe the Systematic Coronary risk evaluation is widespread. The strengths of the global CV risk scores depend on the methodology applied at the time of construction: (a) appropriate statistical methods (representative sample, sufficient power, clear definition of the outcomes); (b) inclusion of appropriate risk factors (age, sex, conventional risk factors, and inclusion of others that can be relevant). Once developed, the function requires internal and external validity as well as calibration. There are several limitations, which have been solved with different approaches. In the case of hypertension, one element is introduced in the score charts, the presence of hypertension-induced organ damage offering a refinement of the approach to the global CV risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Global cardiovascular (CV) risk assessment tries to answer the questions: who will benefit from intervention? And when should non-pharmacologic and pharmacologic treatment be started? In this context, individuals at the highest levels of risk are those that gain most from risk factor management, if life expectancy is long enough to actually achieve the benefit. Although these individuals are those that gain most, the majority of deaths in a community come from those at lower levels of risk, simply because they are more numerous compared to high risk individuals, who develop fewer events in absolute terms. Used for the assessment of CV risk in the presence of one main CV risk factor, the presence of previous CV disease, diabetes, chronic kidney disease, coronary heart disease and severely elevated single risk factors, are situations with a high or very high risk. For the majority of subjects without any of the above, a calculation of risk can help to decide the best management. The methodology of assessing global CV risk has both strengths and limitations that limit their use.
2 Methods to Assess Global Cardiovascular Risk
Several computational methods have been developed to assess global CV risk but no risk estimation can consider all the potential risk factors [1]. The most used score chart is the Framingham CardioVascular Risk Score [2], although in Europe the systematic coronary risk evaluation [3] is widespread. Table 1 summarizes the most used score chart. These two, Framingham and SCORE and the others used, ASSIGN–SCORE [4], PROCAM [5], CUORE [6], QRISKI 1–2 [7, 8] and the pooled cohort studies equation [9], have been calculated from different populations with different age ranges, ethnic and socio-economic characteristics; some express the results as CV risk at 10 or 20 years and others in risk of mortality. Other differences include the age range and the presence or not of diabetics. To solve the problem of different populations some of the chart has been recalculated for specific countries with different levels of risk and the SCORE provides different charts for European countries with low, moderate and high risk. To avoid the problems of lack of diabetes or the limited age range, multiplication for correction factors are used, SCORE multiplies by four the risk of mortality to calculate the risk for CV disease.
3 Strengths and Limitations
The strengths of the global CV risk scores depend on the methodology applied at the time of construction [1]: (a) appropriate statistical methods (representative sample, sufficient power, clear definition of the outcomes); (b) inclusion of appropriate risk factors (age, sex, conventional risk factors, and inclusion of others that can be relevant). Once developed, the function requires internal and external validity as well as calibration. There are several limitations to the different charts, although these do not invalidate the utility of their use, but should however be considered when the decisions are based on the global CV risk.
3.1 Time Period Used for the Calculation
The majority of the charts were generated using baseline data from before 2000, with the exception of the QRISK2 which used data up to 2008. These old data introduce the bias of overestimating risk, since the secular trends of CV risk have diminished in the last decades.
3.2 Calculations of Risk
Practically all charts used the 10 year risk for coronary heart disease or total CV events, with the exception of the SCORE, which estimated 10-year risk of CV mortality. This limitation to mortality data causes one to use assumptions such as, for example, that the total CV disease is calculated from mortality multiplied by three for men and by four for women. In the case of older subjects a factor of three is used.
3.3 Age
Age is a relevant issue at the time to calculate the risk in both extremes of age. Young people will have very low estimated CV death risk. Decisions to treat based on global CV risk deals with the problem of a low absolute risk in young people even with multiple risk factors since risk is assessed for the following 10–20 years in the majority of the risk charts or scores. To solve this, other approaches such as the relative risk charts [10], the lifetime risk [7, 8] or the pooled cohort studies equation [9] are more suitable for young adults.
Likewise, older men will have estimated CV death risks exceeding 5–10 %, even when CV risk factors are low. In this case, SCORE multiplies mortality by three.
3.4 Women
Women usually have lower CV risk than men, and therefore for estimation of risk two things must be taken into account. First is that recommendation to estimate risk is delayed until fifty years of age in contrast with forty years, which is the starting point of estimating risk in men. Second, their risk is deferred by about 10 years rather than avoided.
3.5 Modifiers of Risk
Besides the main CV risk factors that are included in the charts, several modifiers of risk should be taken into account. The ESH Guidelines on CV prevention [10] use the SCORE charts but introduce some modifiers increasing the risk. These are: sedentary subjects, central obesity, socially deprived individuals and ethnic minorities, impaired fasting glucose or glucose intolerance, increased levels of triglycerides, fibrinogen, apolipoprotein B, lipoprotein (a) and high sensitivity C-reactive protein and family history of premature CVD.
4 The Case of Hypertension
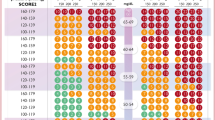
In hypertension, quantification of global CV risk is now generally accepted and integrated in the ESH-ESC guidelines from 2003 [11]. This combines three components: BP levels, coexistence of other CV risk factors and presence of clinical or subclinical organ damage (Fig. 1). The group with previous CV events, diabetes, renal disease or severe elevated single factor is only a small fraction of the hypertensives that represent high or very high CV risk. The remaining requires the use of models to estimate CV risk. Risk assessment of hypertension included specific elements derived from the presence of early target organ damage (TOD). The inclusion of TOD introduces a new dimension that seems to improve the prognostic value of the classic components of risk charts [12].
Stratification of total CV risk in hypertension. CV cardiovascular, CVD cardiovascular disease, CKD chronic kidney disease, DBP diastolic blood pressure, HT hypertension, OD organ damage, RF risk factor, SBP systolic blood pressure. Figure reproduced with permission from European Society of Hypertension
ESH-ESC system also has several limitations besides those present in general in the global CV risk charts. First, is how the organ damage is evaluated, for example at the time to assess the presence or not of left ventricular hypertrophy. This is quite different if the method is ECG or echocardiography, which has superior sensibility to detect the hypertrophy. Likewise, whether to assess only heart or kidney or to include vascular assessment with carotid-intima thickness or pulse wave velocity. Second, is the lack of quantification of risk derived from the presence of TOD. Third, any threshold of risk is arbitrary and to trigger certain interventions is problematic since risk is a continuum. Fourth, it only considers office BP instead of the widely used out-of-office BP, which has a better relationship with the presence of TOD and CV risk. Finally, one question is still unsolved: the fact that the BP included in the chart was under antihypertensive treatment. Some time ago, D’Agostino [13] published the equivalence of risk score of stroke using Framingham data between subjects with and without antihypertensive treatment. For example, the risk of stroke in untreated men with BP of 166–175 mmHg was similar to BP values of 143–150 mmHg in treated subjects.
Despite all of these the ESH-ESC Guidelines recommended that in asymptomatic subjects with hypertension, but free of CV disease, chronic kidney disease and diabetes, total CV risk stratification using the SCORE model as a minimal requirement (evidence class I, level B). As there is evidence that TOD predicts CV death independently of SCORE, a search for TOD should be considered, particularly in individuals at moderate risk (evidence class IIa, level B). Finally, it is recommended that decisions on treatment strategies depend on the initial level of total CV risk (evidence class I, level B).
5 Conclusions
Overall, more research is required to quantify the clinical benefits and cost effectiveness of such an approach. However, a greater problem is the underutilization of CVD prevention in clinical practice. New computer based assistance as well apps can help to easily implement it. Then, rather than competing over which is the best method, it is better to encourage their use.
References
Cooney MT, Dudina AL, Graham IM. Value and limitations of existing scores for the assessment of cardiovascular risk: a review for physicians. J Am Coll Cardiol. 2009;54:1209–27.
D’Agostino RB Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–53.
Conroy RM, Pyorala K, Fitzgerald AP, Sans S, Menotti A, De Backer G, De Bacquer D, Ducimetiere P, Jousilahti P, Keil U, Njolstad I, Oganov RG, Thomsen T, Tunstall-Pedoe H, Tverdal A, Wedel H, Whincup P, Wilhelmsen L, Graham IM, Group Sp. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003;24:987–1003.
Woodward M, Brindle P, Tunstall-Pedoe H, Estimation Sgor. Adding social deprivation and family history to cardiovascular risk assessment: the ASSIGN score from the Scottish Heart Health Extended Cohort (SHHEC). Heart. 2007;93:172–176.
Assmann G, Cullen P, Schulte H. Simple scoring scheme for calculating the risk of acute coronary events based on the 10-year follow-up of the prospective cardiovascular Munster (PROCAM) study. Circulation. 2002;105:310–5.
Giampaoli S. CUORE: a sustainable cardiovascular disease prevention strategy. Eur J Cardiovasc Prev Rehabil. 2007;14:161–2.
Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, May M, Brindle P. Derivation and validation of QRISK, a new cardiovascular disease risk score for the United Kingdom: prospective open cohort study. BMJ. 2007;335:136.
Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, Minhas R, Sheikh A, Brindle P. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ. 2008;336:1475–82.
Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB Sr, Gibbons R, American College of Cardiology, American Heart Association Task Force on Practice Guidelines, et al. ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;2014(63):2935–59.
Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, et al. European Guidelines on cardiovascular disease prevention in clinical practice: The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2012;33:1635–701.
Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F, Members Task Force. ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;2013(31):1281–357.
Sehestedt T, Jeppesen J, Hansen TW, Wachtell K, Ibsen H, Torp-Pedersen C, Hildebrandt P, Olsen MH. Risk prediction is improved by adding markers of subclinical organ damage to SCORE. Eur Heart J. 2010;31:883–91.
D’Agostino RB, Wolf PA, Belanger AJ, Kannel WB. Stroke risk profile: adjustment for antihypertensive medication. The Framingham Study. Stroke. 1994;25:40–3.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This article does not contain any studies with human participants or animals performed by any of the authors. The author declares that he has no conflict of interest. The paper did not receive any funding.
Rights and permissions
About this article
Cite this article
Redon, J. Global Cardiovascular Risk Assessment: Strengths and Limitations. High Blood Press Cardiovasc Prev 23, 87–90 (2016). https://doi.org/10.1007/s40292-016-0139-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-016-0139-2