Abstract
Background
Poor adherence to glaucoma medication regimens may be associated with subsequent optic nerve damage and irreversible visual loss. Specific barriers to effective patient adherence in low-middle income countries are not fully recognized and new disease-specific instruments to assess adherence have been developed.
Objective
The purpose of this cross-sectional study was to evaluate adherence of primary open-angle glaucoma (POAG) patients to treatment in a middle-income country.
Methods
POAG patients were recruited from the Glaucoma Service – Irmandade da Santa Casa de Misericordia de Sao Paulo, Sao Paulo, Brazil. Clinical and demographic data were retrieved from participants’ electronic records. All patients answered the Glaucoma Treatment Compliance Assessment Tool (GTCAT). This 27-item questionnaire was designed to evaluate multiple behavioral factors associated with glaucoma medication adherence.
Results
The sample comprised 96 patients with POAG. The mean age was 63.2 ± 8.9 years; 48 were male and 48 female; 55 (57.3%) were White, 36 (37.5%) African-Brazilian, and five (5.2 %) were of mixed color. Most patients (97.9%) had less than a high school degree and all had a family income < US$10,000. The GTCAT identified 69 (71.8%) patients who “sometimes forget to use drops,” 68 (70.8%) patients who “sometimes fall asleep before dosing time,” and 60 (62.5%) patients “whose drops aren’t with them at the time to take them”; 82 (85.4%) patients admitted to using “reminders to take medications.” Eighty-two (85.4%) patients agreed that “doctor answers my questions,” and 77 (80.5%) said “they are happy with their eye doctor.”
Conclusions
The GTCAT identified a number of mostly unintentional factors associated with adherence in this cohort of Brazilian patients. The data may impact on how to understand and improve adherence to ocular hypotensive treatment in the Brazilian population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A number of qualitative studies have evaluated adherence behaviors in glaucoma patients. Most of these studies were conducted in industrialized nations. |
There is a paucity of data on the barriers to optimal glaucoma medication adherence among glaucoma patients in developing countries. |
We identified a number of potential barriers to topical glaucoma therapy adherence in a middle-income country. |
Patient-specific factors associated with adherence can be used to develop customized interventions in order to optimize glaucoma adherence in these populations. |
1 Background
Primary open-angle glaucoma (POAG) is a chronic, multifactorial disease that can lead to irreversible vision loss if left untreated. The only effective treatment to prevent optic nerve damage and halt disease progression is to lower intraocular pressure (IOP) [1]. That goal is achieved mainly by the use of topical hypotensive medications, which include prostaglandin analogs, β-blockers, carbonic anhydrase inhibitors, α-adrenergic agonists, and parasympathomimetics. Not infrequently, patients have to take more than one medication, two or three times a day [2]. Despite the development of different combinations of drugs, the medical regimen can be very complex, making the compliance of patients to the prescribed therapy difficult. Indeed, evidence from pharmacy claims and self-reported data indicate that a number of patients do not take their medications as prescribed [3,4,5,6,7]. Poor adherence to glaucoma medication regimens may be associated with sub-optimal IOP control and subsequent visual field loss.
Patient non-adherence to a medical regimen can not only be a pervasive menace to individuals’ health and well-being, but carry a considerable economic burden to the healthcare systems as well [8]. Furthermore, efforts to improve adherence on an individual level are dependent on a number of key factors [8].
Although extensively studied in industrialized nations, specific barriers to effective patient adherence in low-middle income countries and underprivileged communities are not fully recognized [9,10,11]. Previous studies reported a noncompliance rate between 20 and 40% in Brazilian patients with glaucoma, and identified side effects of antiglaucoma drugs and the lack of information about the disease as the main factor for non-compliance [12, 13]. Adherence rates and beliefs about glaucoma can vary in different socio-cultural populations, reflecting the need to study these issues in specific populations [14]. Recently, a new disease-specific instrument to assess adherence has been developed. The Glaucoma Treatment Compliance Assessment Tool (GTCAT) was developed specifically for glaucoma patients and proved to be useful to evaluate patients' adherence to physician-prescribed regimens [15,16,17,18]. Hence, the purpose of this cross-sectional study was to evaluate the adherence of glaucoma patients to medical treatment in a middle-income country and to identify potential barriers to compliance with treatment.
2 Methods
2.1 Study Design
This was a cross-sectional, qualitative, uncontrolled, observational study of patients receiving eye care at the Glaucoma Service, Irmandade da Santa Casa de Misericordia de Sao Paulo, São Paulo, Brazil. This is a government-funded charity hospital that delivers healthcare to uninsured patients. From July to November 2020, consecutive patients were screened by the clinic staff to ensure the participants fulfilled the inclusion criteria and, after providing signed informed consent, were included in the study. The institution’s ethics committee for research in human beings approved the study, which was conducted according to Resolution 466/12, National Council of Health, Ministry of Health, Brazil and to the tenets of the Declaration of Helsinki (amended by the 64th WMA General Assembly, Fortaleza, Brazil, October 2013).
2.2 Participants’ Inclusion Criteria
In order to be included in the study, all participants had to have a diagnosis of POAG and to have been using hypotensive topical medications for at least 1 year. POAG was defined by typical optic disc features and correspondent visual field defects in patients with open-angles on gonioscopy. Optic disc signals included concentric or focal enlargement of the cup, focal thinning of the neural rim with or without a disc hemorrhage, or a visible wedge defect of the retinal nerve fiber layer. Correspondent visual field defects included one of the following criteria: three or more adjacent points on the pattern deviation plot with sensitivity decreased to a P < 5% level and at least one decreased to P < 1%; GHT (glaucoma hemifield test) flagged as outside normal limits; PSD (pattern standard deviation) with a value flagged as P < 5% on a Humphrey Visual Field Analyzer II (Carl Zeiss Meditec, Inc., Dublin, CA, USA), SITA (Swedish Interactive Threshold Algorithm) standard 24-2 program on a reliable exam. Reliability for the visual field test were taken to be < 20% fixation losses, < 15% false-negative errors, and < 15% false-positive errors. Determinations regarding fulfillment of inclusion criteria were made by an ophthalmologist.
2.3 Test Instrument
The reduced version of the GTCAT was used to assess the patients’ perceptions on adherence to medical treatment of glaucoma with hypotensive topical eye drops. Based on the Health Belief Model, this questionnaire was designed to evaluate multiple behavioral factors associated with glaucoma medication adherence, which includes 27 statements that evaluate benefits, barriers, cues-to-action, susceptibility, severity, health status, depression, patient-physician relationship, and self-reported adherence [15,16,17,18]. Responses to each statement are graded on a five-interval Likert-type scale response with anchoring definitions (from 1 = strongly disagree to 5 = strongly agree), where higher scores are indicative of more positive outcomes. The questionnaire was translated and validated to Brazilian-Portuguese [13].
2.4 Data Collection
Socio-demographic information were obtained by self-report and included gender, age, ethnicity, highest completed education level, yearly family income, other systemic comorbidities, and number of non-glaucoma medications. Clinical data were retrieved from the participants’ electronic records and comprised duration of glaucoma diagnosis, laterality, previous incisional or laser surgery, cup-to-disc ratio (C/D), and automated perimetry mean deviation (MD) and patter standard deviation (PSD) values.
The GTCAT was applied as an interview and completed after a regular appointment in an area other than the examination room by two of the authors (JCA and GSM) who were not directly involved in the care of the patients. Although field notes were allowed to collect the data, no video or audio recordings were made during the interview. Not infrequently, a family member would be present at the interview as long as he would not interfere with the patient’s answers.
2.5 Statistical Analysis
All data were plotted on an Excel spreadsheet (Microsoft Corporation, Redmond, WA, USA) and statistical calculations made with the OpenEpi program version 3.03a. The results were reported as mean ± standard deviation, median with extreme values, and frequencies (%) when appropriate. Comparison of clinical and demographic data between adherents, neutrals, and non-adherents to medical therapy was done with the Chi-square χ2 test or Fisher's exact test in the analysis of contingency tables (categorical variables). The Kruskal–Wallis H test was used to compare continuous categories between the groups. A P value of less than 5% was considered to be of statistical significance.
3 Results
3.1 Demographic Features of the Sample
One hundred and five glaucoma patients were approached to do the study. Nine refused to participate because of lack of time or other reasons. The sample thus comprised 96 patients with POAG. The mean age was 63.2 ± 8.9 years; 48 were male and 48 female; 55 (57.3%) were White, 36 (37.5%) African-Brazilian, and five (5.2 %) were of mixed color; most patients (97.9%) had less than a high school degree and all had a yearly family income < US$10,000. Detailed clinical and demographic data from the sample are displayed in Table 1.
3.2 Glaucoma Treatment Compliance Assessment Tool (GTCAT) Results
The GTCAT identified 69 patients (71.9%) who “sometimes forget to use drops,” 68 patients (70.8%) who “sometimes fall asleep before dosing time,” and 61 patients (63.5%) “whose drops aren’t with them at the time to take them”; 82 patients (85.4%) who admitted to using “reminders to take medications.” Eighty-two patients (85.4%) agreed that “doctor answers my questions,” and 77 (80.5%) said “they are happy with their eye doctor.” At the lower end of the responses, 26 patients (27.0%) agreed with statement 22 (“I can afford my eye drops”) and 19 participants (19.8%) agreed with statement 27 (“over the past 4 weeks I have never felt blue, downhearted, or depressed”). Detailed information on the 27 statements of the GTCAT is given in Table 2.
We stratified the results of the responses according to each of the seven components of the GTCAT and some highlights of the results are presented here.
3.2.1 Barriers Due to Lack of Eye Drops
The GTCAT identified 69 patients (71.9%) who “sometimes forget to use drops”(statement 10), 68 patients (70.8%) who “sometimes fall asleep before dosing time” (statement 11), and 28 patients (29.1%) agreed with statement 13 (“sometimes I am out of drops”).
3.2.2 Self-Efficacy
Fifteen patients (15.6%) agreed with statement 14 (“I need assistance putting drops in my eyes”) and 26 patients (27.0%) agreed with “I can afford my eye drops” (statement 22).
3.2.3 Experience of Negative Effects of Glaucoma
Seventeen patients (17.7%) agreed with statement 8 (“If I lost the same amount of vision over the next five years as I have over the past five, it would have no effect on my quality of life”) and 20 patients (20.8%) agreed with statement 19 (“a friend or family member’s experience with eye drops has encouraged me to use my eye drops”).
3.2.4 Well-Being
Forty-four participants (45.8%) agreed with statement 16 (“my eye drops cause me no pain or discomfort”) and 52 patients (54.1%) agreed with statement 26 (“my overall health is excellent”).
3.2.5 General Glaucoma Knowledge
Three patients (3.1%)agreed with statement 1 (“my personal knowledge of the symptoms of glaucoma is excellent”) and 54 participants (56.2%) agreed with statement 2 (“a person can have glaucoma and not know it”).
3.2.6 Glaucoma Symptom Knowledge
Fifty-four patients (45.8%) agreed with statement 3 (“eye pain is a common symptom of glaucoma”) and 66 patients (68.7%) agreed with statement 5 (“vision lost from glaucoma is permanent”).
3.2.7 Cues-to-Action
Eight-two patients (85.4%) agreed with statement 23 (“I use reminders to take my eye-drop medications”).
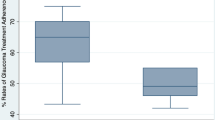
3.3 Risk Factors for Poor Adherence
A comparison of the clinical and demographic differences between adherents, neutrals, and non-adherents is presented in the Online Supplemental Material (OSM). In short, the analysis revealed that those who “sometimes forget to use drops” (statement 10) are older than those who do not forget (65.3 ± 8.1 and 58.4 ± 8.2 years of age, respectively, P = 0.001) as well as those who “sometimes fall asleep before dosing time” (statement 11) as compared to patients who do not fall sleep (65.3 ± 8.1 and 60.4 ± 10.7 years of age, respectively, P = 0.016). Patients who disagreed with statement 22 (“I can afford my eye drops”) were older as compared to those who agreed (64.5 ± 9.4 and 60.0 ± 7.8 years of age, respectively, P = 0.037) and had significantly lower family income than those who agreed with that statement (US$7344 and US$9700, respectively, P < 0.001).
4 Discussion
The results of this study revealed that most patients (71.9%) reported having forgotten to take their medication in the last month (statement 10) – only 23.9% disagreed with question 9 (“Over the last month I have not missed taking my eye drops”). Using the same questionnaire, Abe et al. reported a 42.1% rate of agreement with statement 10 and 23.7% of disagreement with statement 9 [13]. As opposed to the participants included in our study, the sample in that study was comprised of patients recruited from a private hospital, and all had both a high income and higher education. The number of non-compliant patients is also high when compared to that in industrialized countries. In a prospective, cross-sectional survey with a population in Ann Arbor, MI, USA and Baltimore, MD, USA, only 27% of the sample reported poor adherence to hypotensive medication adherence among glaucoma patients [19]. The sample included patients from private practice, and most had at least a high school degree, as opposed to the patients in our study [19]. Self-reports tend to overestimate adherence behavior compared with other assessment methods and generally have high specificity but low sensitivity [20]. It is likely that patients in this sample reported greater levels of non-adherence because they face greater barriers than their counterparts living in high-income countries.
Forgetfulness (71.8%), falling sleep (70.8%), and not having the medication near (63.5%) were the three main factors associated with non-adherence in this study. As a silent affliction, glaucoma causes symptoms mostly in advanced disease [21]. Most patients with early and moderate disease can easily become complacent over time as they became accustomed to feeling well and not having any visual symptoms to remind them to take their medicines. For some patients with chronic systemic diseases, adding a new medication to the regular regimen can make it more difficult to remember to take their medications, until they have a well-established routine for the new therapy. Interruptions to routine daily life—such as holidays—or social events can cause some to forget to take their medication. Others can be distracted by something that needs their immediate attention at the time they usually take their medication. Besides, oversleeping or falling sleep can be an issue with medications taken first thing in the morning or at bed time [22, 23]. These same issues might affect glaucoma patients with regard to topical medications.
At the same time, 85.4% of patients used some remainders to take their medication. Some medications that can be stored in plain view (e.g., on top of a night stand) or can be taken “attached” to usual daily routines (such as brushing teeth) are easier to remember than medicines that have to be stored out of view (such as latanoprost, which needs to be kept in the refrigerator). There are some strategies that help patients to remind them to take their medicines. An emergency supply or an extra bottle of the eye drops at the workplace can help patients to not miss a single dose. Alarms that can be set up in mobile phones or smartphone apps specifically to help with remembering medicines can be useful [23, 24]. Nevertheless, these strategies can be more difficult for the elderly.
Only 27% of patients agreed with “I can afford my eye drops,” meaning that most patients have to rely on free dispensing of medications for uninterrupted treatment. All participants in the study had a yearly family income of less than US$10,000, and those who disagreed with the questions had lower incomes as compared to those who agreed. This observation concurs with previous reports [25]. Comprehensively, we could expect some financial difficulty when it comes to purchasing medications. In the USA, up to 32% of older patients take less medication than prescribed to avoid costs, and not having prescription drug coverage is a significant risk factor for cost-related non-adherence [26]. In Brazil, the Unified Health System provides free dispensing of medicines—and that includes a number of hypotensive eye drops—by the local unities of the Specialized Component of Pharmaceutical Assistance. However, the lack of specific medications is relatively common, especially in the city of Sao Paulo [27]. The rising cost of hypotensive medications poses additional challenges for glaucoma patients, who require long-term treatment and may be forced to purchase prescribed medications because of their high cost. That is a worrisome issue in low-middle income nations.
The GTCAT revealed that many patients knew little about glaucoma. Only 3% of patients agreed with statement 1 (“my personal knowledge of the symptoms of glaucoma is excellent”) and 61.3% agreed or were neutral with statement 3 (“eye pain is a common symptom of glaucoma”). Conversely, most patients (68.7%) were aware of the fact that glaucoma can lead to irreversible blindness (statement 5), and 77% agreed with statement 4 (“major vision loss can be prevented with treatment”). Many patients feel that being aware of the purpose of their medications and being conscientious about the benefits derived from taking them can help patients to remember to take them [23, 24]. As long as the patient is aware that the eye drops are the only means for preventing them from going blind from glaucoma they are more likely to remember to take them. In this regard, the doctor has the responsibility of ensuring that their patients are aware of the potential benefits of the continuous use of the medications as the only means to prevent blindness.
As to statement 24 (“my doctor answer my questions”), 85.4% agreed a little or a lot; 88.5% were in agreement with “I completely agree with my doctor’s diagnosis of glaucoma in my eyes,” and 78.1% reported “I am happy with my eye doctor.” The lack of good communication is often thought to be a common cause of non-compliance, particularly in older patients with memory disorders, which make them unable to follow a complex set of instructions. Particularly in glaucoma patients, provider education about how to administer eye drops and patient adherence self-efficacy was found to be positively associated with adherence [28]. The doctor–patient relationship seems to be an important variable in adherence, including the process of prescribing. In addition, compliance seems to be related to the quality, duration, and frequency of interaction between the patient and his doctor. The physician's attitude towards the patient and his ability to elicit and respect the patient’s concerns, to provide appropriate information, and demonstrate empathy are of the utmost importance [29]. It seems paradoxical that most patients reported positive metrics in the aforementioned items about communication with their doctors and at the same had high rates of non-adherence. One possibility is that most barriers to non-adherence in the study were related to unintentional factors such as forgetfulness, falling sleep, and financial issues. Those are barriers that can hardly be overcome by the doctor–patient relationship.
Most patients (88.5%) disagreed with statement 7 (“I have lost none of my vision due to glaucoma”); 78% felt that progressive loss of vision over the next 5 years would have an effect on their quality of life (statement 8). These observations can be a reflection of the patients’ personal experience with struggling with the disease for a long time. Overall, the sample comprised a large number of patients with advanced disease and poor vision (Table 1).
With regard to patients’ perception of general health and well-being, 54.1% felt their general health was excellent (statement 26) and 71.9% acknowledged some degree of sadness/depression (statement 27). In the elderly, depression especially affects patients with chronic diseases and cognitive impairment, causing suffering, family disruption, and disability, and at the same time it worsens the outcomes of many illnesses and increases mortality [30]. Psychosocial adversity such as economic impoverishment, disabilities, isolation, and sadness can contribute to physiological changes, further increasing susceptibility to or triggering depression in vulnerable older persons [30]. A recent literature review found an association between glaucoma and depression; advanced disease stage, older age, female sex, and more rapid visual loss progression were recognized as potential risk factors [31]. It comes as no surprise that most patients in the study felt some degree of depression. In addition to advanced age, poor vision, and the disease itself, financial concerns related to a lack of economic resources common to people living in developing countries adds to the manifestation of depression. Depression is associated with poor adherence to medication across a range of chronic diseases, and in order to improve compliance, it must be assessed in specific conditions [32].
This study has more than a few limitations. The application of the questionnaire on the same day and immediately after the appointment can have introduced bias. The information given to patients with regard to the test results and functional status of their eyesight—especially when viewed as bad news—could potentially interfere with the questionnaire responses related to ‘perceived severity’ and ‘susceptibility.’ Using a doctor to play the role of an interviewer could have overestimated patient’s adherence behavior in that patients might have felt intimidated by their presence. We have tried to minimize this potential bias using doctors who were not involved in the immediate care of the patients. The GTCAT is a Likert-scale that restricts all possible responses to only 5 values (disagree a lot, disagree a little, neutral opinion, agree a little, and agree a lot). The use of an open-ended feedback questionnaire could have produced more information than a restricted Likert-scale survey items. Moreover, the study setting could limit generalizability of the findings to the general Brazilian population – given that the participants in this study were uninsured, this study may overestimate some barriers compared to the general population.
In summary, the GTCAT identified a number of mostly unintentional factors associated with adherence in this cohort of Brazilian patients. The data may impact on how to understand and improve adherence to ocular hypotensive treatment in the Brazilian population and to some extent to those nations similarly ranked as middle-income countries.
References
Heijl A, Leske MC, Bengtsson B, et al. Early Manifest Glaucoma Trial Group. Reduction of intraocular pressure and glaucoma progression. Results from the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2002;120:1268–79.
Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120:701–13 (discussion 829–30).
Dreer L, Girkin C, Mansberger S. Determinants of medication adherence to topical glaucoma therapy. J Glaucoma. 2012;21:234–40.
Patel SC, Spaeth GL. Compliance in patients prescribed eye drops for glaucoma. Ophthalmic Surg. 1995;26:233–6.
Friedman DS, Quigley HA, Gelb L, et al. Using pharmacy claims data to study adherence to glaucoma medications: methodology and findings of the Glaucoma Adherence and Persistency Study (GAPS). Investig Ophthalmol Vis Sci. 2007;48:5052–7.
Feehan M, Munger MA, Cooper DK, et al. Adherence to glaucoma medications over 12 months in two US community pharmacy chains. J Clin Med. 2016;5:79.
Newman-Casey PA, Blachley T, Lee PP, et al. Patterns of glaucoma medication adherence over four years of follow-up. Ophthalmol. 2015;122:2010–21.
Martin LR, Williams SL, Haskard KB, Dimatteo MR. The challenge of patient adherence. Ther Clin Risk Manag. 2005;1:189–99.
Killeen OJ, Pillai MR, Udayakumar B, et al. Understanding barriers to glaucoma treatment adherence among participants in South India. Ophthal Epidemiol. 2020;27:200–8.
Tshivhase S, Khoza LB. Challenges contributing to loss to follow-up as experienced by glaucoma patients in the Vhembe District of Limpopo Province, South Africa. Open Public Health J. 2020;13:531–7.
Guven S, Koylu MT, Mumcuoglu T. Adherence to glaucoma medication, illness perceptions, and beliefs about glaucoma: attitudinal perspectives among Turkish population. Eur J Ophthalmol. 2021;31:469–76.
Silva LR, de Paula JS, Rocha EM, Rodrigues ML. Factors related to glaucoma treatment compliance: patients’ opinions from a University Hospital. Arq Bras Oftalmol. 2010;73:116–9.
Abe RY, Wen L de C, Barker GT, Mansberger SL. Psychometric properties of the glaucoma treatment compliance assessment tool (GTCAT) in a Brazilian population. J Glaucoma. 2018;27:257–65.
Rees G, Chong XL, Cheung CY, et al. Beliefs and adherence to glaucoma treatment: a comparison of patients from diverse cultures. J Glaucoma. 2014;23:293–8.
Mansberger SL, Sheppler CR, McClure TM, et al. Psychometrics of a new questionnaire to assess glaucoma adherence: the Glaucoma Treatment Compliance Assessment Tool (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2013;111:1–16.
Barker GT, Cook PF, Schmiege SJ, et al. Psychometric properties of the Glaucoma Treatment Compliance Assessment Tool in a multicenter trial. Am J Ophthalmol. 2015;159:1092–9.
Barker GT, Mansberger SL. Psychometric Properties of the Reduced Version of the Glaucoma Treatment Compliance Assessment Tool (GTCAT). Ophthalm Epidemiol. 2019;26:55–62.
Sanchez FG, Mansberger SL, Newman-Casey PA. Predicting adherence with the glaucoma treatment compliance assessment tool. J Glaucoma. 2020;29:1017–24.
Newman-Casey PA, Robin AL, Blachley T, et al. Most common barriers to glaucoma medication adherence: a cross-sectional survey. Ophthalmology. 2015;122:1308–16.
Stirratt MJ, Dunbar-Jacob J, Crane HM, et al. Self-report measures of medication adherence behavior: recommendations on optimal use. Transl Behav Med. 2015;5:470–82.
Shah YS, Cheng M, Mihailovic A, et al. Patient-reported symptoms demonstrating an association with severity of visual field damage in glaucoma. Ophthalmology. 2022;129:388–96.
Jimmy B, Jose J. Patient medication adherence: measures in daily practice. Oman Med J. 2011;26:155–9.
Kini V, Ho PM. Interventions to improve medication adherence: a review. JAMA. 2018;320:2461–73.
Cross AJ, Elliott RA, Petrie K, et al. Interventions for improving medication-taking ability and adherence in older adults prescribed multiple medications. Cochrane Database Syst Rev. 2020;5:CD012419.
Delavar A, Radha Saseendrakumar B, Weinreb RN, Baxter SL. Racial and ethnic disparities in cost-related barriers to medication adherence among patients with glaucoma enrolled in the National Institutes of Health All of Us Research Program. JAMA Ophthalmol. 2022;140:354–61.
Briesacher BA, Gurwitz JH, Soumerai SB. Patients at-risk for cost-related medication nonadherence: a review of the literature. J Gen Intern Med. 2007;22:864–71.
Guerra G. População fica sem medicamentos nas farmácias de alto custo: o que fazer? Consultor Jurídico 2022 https://www.conjur.com.br/2022-mar-28/gabriela-guerra-farmacia-alto-custo. Assessed 22 Oct 2022.
Sleath B, Blalock SJ, Carpenter DM, et al. Ophthalmologist-patient communication, self-efficacy, and glaucoma medication adherence. Ophthalmology. 2015;122:748–54.
Vermeire E, Hearnshaw H, Van Royen P, Denekens J. Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther. 2001;26:331–42.
Alexopoulos GS. Depression in the elderly. Lancet. 2005;365:1961–70.
Stamatiou ME, Kazantzis D, Theodossiadis P, Chatziralli I. Depression in glaucoma patients: a review of the literature. Semin Ophthalmol. 2021;37:29–35.
Grenard JL, Munjas BA, Adams JL, et al. Depression and medication adherence in the treatment of chronic diseases in the United States: a meta-analysis. J Gen Intern Med. 2011;26:1175–82.
Acknowledgements
This research was presented in part at the 2021 Association for Research in Vision and Ophthalmology Virtual Meeting.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Data availability
Data available on request due to privacy/ethical restrictions.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
Julia C. Andrade, Guilherme S. Motta, and Niro Kasahara declare that they have no conflicts of interest that might be relevant to the contents of this article.
Ethics approval
The institutional ethics committee approved the study.
Consent to participate
All participants signed informed consent to participate in the study.
Consent to publish
Not applicable.
Code availability
Not applicable.
Authors’ contribution
All authors contributed equally to the study conception and design. Julia C. Andrade and Guilherme S. Motta performed data collection and analysis. Niro Kasahara wrote the first draft of the manuscript. All authors read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
da Costa Andrade, J., Motta, G.S. & Kasahara, N. Perspectives on Adherence to Glaucoma Medical Therapy in Brazilian Patients. Pharm Med 37, 377–384 (2023). https://doi.org/10.1007/s40290-023-00482-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40290-023-00482-y