Abstract
The incidence of cardiovascular diseases has significantly increased with the expansion of the industrialization of societies, which is notably linked to lifestyle changes and an unhealthy diet. Hence, determining the healthiest diet habits and supplements seems to be an appropriate way to decrease the global burden of cardiovascular diseases. Currently, caffeine, one of the most widely consumed compounds in the world, has emerged with some promising results in the treatment of numerous pathophysiological conditions of cardiovascular diseases. A literature search was conducted in PubMed, Scopus, Science Direct, Google Scholar, and Web of Science databases for the relevant articles regarding the pharmacology, preclinical, and clinical studies on the potential effects of caffeine on cardiovascular diseases. While caffeine could improve cardiovascular outcomes through several mechanisms of action, the literature review revealed controversial clinical effects of caffeine on blood pressure, cardiac arrhythmias, acute coronary syndrome, stable angina, and heart failure. In the case of dyslipidemia, coffee consumption increased total cholesterol, triglyceride, and low-density lipoprotein. Taken together, the existence of multiple confounding factors in the caffeine studies has resulted in inconclusive data interpretation. Further well-designed studies with adequate control of the confounding factors are warranted to draw a clear conclusion on the cardiovascular efficacy and safety of caffeine.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Cardiovascular diseases remain the leading cause of mortality in the world. |
We found conflicting evidence about the potential effects of caffeine on cardiovascular diseases. |
Well-designed studies are warranted to evaluate the impact of caffeine on cardiovascular outcomes. |
1 Introduction
Cardiovascular diseases (CVDs) are defined as a group of syndromes, including coronary heart disease, rheumatic heart disease, cerebrovascular disease, peripheral artery disease, and congenital heart disease. Despite the recent pharmacological and non-pharmacological progress in the management of CVDs, they still remain the most common cause of mortality in Western countries with a significant financial burden [1]. It has been predicted that the mortality rate would increase to more than 23.6 million per year by 2030 [2]. Historically, conventional cardiovascular drugs such as angiotensin II AT1 receptor blockers, angiotensin-converting enzyme inhibitors, calcium channel blockers, anticoagulants, and antiplatelet agents have been shown to decrease the mortality in a wide range of CVDs [3, 4]. Attempts have been made to find other medications with potential beneficial effects in the management of CVDs. In this regard, Tardif et al. in the Colchicine Cardiovascular Outcomes Trial showed that the initial addition of colchicine, an orally anti-gout medication, to the standard of care following myocardial infarction cost efficiently leads to better therapeutic outcomes [5, 6]. Furthermore, it has been shown that allopurinol, a xanthine oxidase inhibitor, could reduce the risk of cardiovascular events in elderly people with hypertension [7].
Caffeine, 1,3,7-trimethylpurine-2,6-dione, is the most commonly used psychoactive compound all around the world and is found in various beverages (tea, coffee, soda, and other energy drinks), cacao, chocolate, and different food products, including gums, cookies, sauces, and candies. Almost two-thirds of the US population uses caffeine in their daily life. It is a component of many prescription and non-prescription drugs because of its analgesic and anti-inflammatory effects [8, 9].
Pharmacologically, caffeine could enhance glutathione S-transferase activity, inhibit red blood cell membrane derangement and high-affinity adenosine triphosphate-dependent cyclic nucleotide transporters, and regulate gamma-amino butyric acid A receptors [10]. The beneficial cardiovascular effects of caffeine have been demonstrated in animal studies. For example, Agaty and Seif showed that caffeine consumption in male Wistar rats, at a dose of 25 mg/kg/day for 6 weeks resulted in improved cardiac inotropy by increasing the direct inotropic effect via ryanodine receptors without significant effects on the electrocardiogram [11]. While some previous studies did not show the beneficial effects of caffeine in the management of various pathophysiological conditions of CVDs, new studies supported the cardiovascular benefits [12, 13]. For example, a recent data analysis of 12 prospective cohort studies including 528,504 Asian individuals supported the cardiovascular benefits of coffee and green tea. During the follow-up period range of 6.5–22.7 years, 94,744 deaths were reported. Results showed that coffee intake (≥5 cups/day) is associated with a 24% (95% confidence interval [CI] 17–29) and 28% (95% CI 19–37%) lower risk of all-cause mortality, in men and women, respectively. Similar findings were observed between coffee consumption and cardiovascular mortality. Compared with non-drinkers, green tea intake (≥ 5 cups/day) is correlated with lower cardiovascular mortality in men (hazard ratio [HR] 0.79; 95% CI 0.68–0.91) and women (HR 0.78; 95% CI 0.68–0.90) [14]. Thus, performing a review to cover previous and new studies seems to be important. In the present updated review, we aimed to discuss the literature regarding the potential beneficial effects of caffeine in CVDs focusing on animal and human studies.
2 Literature Search Methods
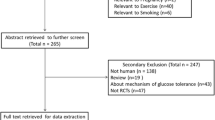
A literature search in PubMed, Scopus, Science Direct, Google Scholar, and Web of Science databases for the relevant articles regarding the pharmacology, preclinical, and clinical studies on the potential effects of caffeine in the management of CVDs from the databases inception to 10 February, 2023 was conducted. Our search terms were (‘caffeine’ OR ‘1, 3, 7-Trimethylpurine-2, 6-dione’ OR ‘methylxanthine’ OR ‘caffeinated beverage’ OR ‘caffeinated drink’ OR ‘coffee’ OR ‘tea’) AND (‘cardiovascular diseases’ OR ‘cardiovascular safety’ OR ‘cardiovascular efficacy’ OR ‘cardiovascular outcomes’ OR ‘pharmacology’ OR ‘mechanism of action’ OR ‘pharmacokinetic’ OR ‘hypertension’ OR ‘arrhythmia’ OR ‘dyslipidemia’ OR ‘acute coronary syndrome’ OR ‘unstable angina’ OR ‘myocardial infarction’ OR ‘stable angina’ OR ‘heart failure’). Duplicate publications, non-English written studies, commentaries, case reports, and irrelevant studies were excluded from the review. The related articles to our review have been discussed.
3 Mechanism of Action
It has been shown that caffeine has several physiological and pharmacological effects on different organs, such as kidney, respiratory system, and smooth and cardiac muscle. Additionally, high doses of caffeine have been shown to have neuroprotective properties against neurological disorders, such as Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, Huntington’s disease, and amyotrophic lateral sclerosis through activating the ryanodine receptor and inhibiting phosphodiesterase enzymes [15]. Caffeine could enhance muscle contractility via induction of sarcoplasmic reticulum calcium release, inhibit phosphodiesterase isoenzymes and cyclic monophosphate accumulation, inhibit glycogen phosphorylase in muscle and liver, antagonize adenosine receptors, stimulate the cellular membrane sodium/potassium pump, and impair phosphoinositide metabolism [16].
There is mounting clinical evidence supporting the key role of inflammation in the pathogenesis of atherosclerosis and the progression of CVDs [16, 17]. Considering the role of oxidative stress mitochondrial dysfunction in many cardiac abnormalities, caffeine, as a rich source of antioxidants, could play a significant role in the management of CVDs [18]. Because of the structural similarity of the caffeine molecule with adenosine (purine backbone), it acts as a competitive antagonist for adenosine receptors, which could lead to anti-inflammatory and anti-apoptotic effects [19]. Caffeine could affect the entire cells and directly block phosphodiesterase enzymes. Additionally, it could bind to adenosine A2A and type 2 taste receptors, leading to increased cyclic adenosine monophosphate levels and activation of protein kinase A. Together, these pathways cause inhibition of proinflammatory responses and cardioprotective effects [20] (Fig. 1).
Anti-inflammatory effects of caffeine in cardiovascular diseases. Binding of caffeine to adenosine A2A receptor (A2AR) and type 2 taste receptor (TAS2R) leads to an increase in the cyclic adenosine monophosphate (cAMP) level. In addition, caffeine could directly block phosphodiesterase (PDE). The increase in the cAMP level leads to activation of protein kinase A (PKA), which results in inhibition of the proinflammatory response. AC adenylate cyclase, ADO adenosine, AMP adenosine monophosphate, ATP adenosine triphosphate, GαS G protein alpha subunit
4 Pharmacokinetics of Caffeine
In addition to the well-known oral administration route, there are intravenous and rectal pathways to administer caffeine, which are available as citrate, sodium benzoate, and ergotamine tartrate pharmaceutical salts. Absorption of caffeine is fast and almost complete with an absorption rate constant of close to 0.33 min-1 from the more basic environment of the small intestine as the unionized state. The presence of food or drink in the gastrointestinal (GI) tract can influence the extent of absorption. Because of the insignificant first-pass metabolism of caffeine, the time to reach the peak plasma concentration is only 30–120 minutes after oral administration. Caffeine is a water-soluble compound with hydrophobic characteristics and low protein binding (10–35%) facilitating its good inter/intracellular entry, distribution into body tissues, and considerable blood–brain barrier penetration [8].
Caffeine elimination obeys first-order linear kinetics and is effectively described by a one-compartment open model system. Until the metabolism of caffeine has been saturated, it majorly undergoes changes via cytochrome P450 1A2 biotransforming to a less toxic metabolite called paraxanthine (1,7-dimethylxanthine), which is eliminated mostly by renal excretion. Caffeine clearance roughly varies between 1 and 3 mg/kg/minute. However, in high doses, it is mainly reduced owing to its paraxanthine metabolite [8, 19]. Notably, there is inter-individual variability in the metabolism of caffeine. Recently, a study of 2278 people found that terminal metabolites of caffeine, such as urinary methyl uric acids (3-MU and 7-MU) and methylxanthines (3-MX and 7-MX), significantly reduce the likelihood of hypertension in their population [17].
5 Cardiovascular Benefits of Caffeine
5.1 Hypertension
There is a growing body of literature describing the prevalence and consequently imposed costs of hypertension, a crucial medical challenge defined as raised blood pressure, to the public health system worldwide [21]. According to the reports of the World Health Organization, there are more than 1.3 billion people with hypertension. It has been estimated that approximately half of individuals with hypertension are not aware of their disease. This issue could make the management of this common clinical condition more challenging. Currently, it is well known that poorly controlled hypertension is significantly associated with several cardiovascular complications, end-organ dysfunction, and mortality.
A series of studies aimed to evaluate the potential effects of caffeine on blood pressure. Based on an animal study, caffeine and caffeic acid combinations could lower blood pressure in Nω-Nitro-l-arginine-methylester-induced hypertensive rats [22]. In the case of human studies, there are controversial data regarding the association between the use of caffeine and caffeinated drinks and hypertension. A meta-analysis of 16 randomized controlled trials including 1010 individuals showed that the use of coffee (725 mL/day) and caffeine (410 mg/day) led to 2.04 mmHg (95% CI 1.10–2.99) and 0.73 mmHg (95% CI 0.14–1.31) increases in systolic and diastolic blood pressure, respectively [23]. Some efforts have been made to evaluate the effects of different doses of caffeine on blood pressure. A prospective cohort study on 63,257 participants aged 45–74 years showed an inverse U-shaped correlation between the amount of coffee consumption and blood pressure changes. They discovered that drinking less than 1 cup of coffee per week (HR 0.87, 95% CI 0.83–0.91 or more than two cups per day, HR 0.93, 95% CI 0.86–1.00) could reduce the risk of developing of hypertension compared with drinking 1 cup of coffee per day [24]. A random-effects dose–response meta-analysis of four studies involving 196,256 individuals with 41,184 recognized hypertension cases demonstrated a non-linear inverse dose–response relationship between coffee use and the risk of hypertension. Protective effects of caffeine were more pronounced in those who drank three cups of coffee per day [25].
Some investigations have tried to evaluate factors involved in the response of patients to the use of caffeine. It has been proposed that patients with hypertension may be more susceptible to caffeine use. In this regard, Hartley et al. in a double-blind, placebo, crossover, randomized controlled trial showed that caffeine administration at a dose of 3.3 mg per kg averagely equal to 260 mg/kg or a fixed 250 mg in non-hypertensive individuals had no clinically meaningful effects on blood pressure, while a significant increase in blood pressure was observed in those with a recent diagnosis of stage 1 hypertension [26]. Pincomb et al. indicated that administration of 3.3 mg/kg of caffeine is associated with a considerable increase in diastolic blood pressure in patients with borderline hypertension compared with control patients (+8.4 vs +3.8 mmHg, P = 0.0001) [27]. Recently, the Japan Collaborative Cohort study aimed to address cardiovascular safety issues following the long-term intake of caffeinated beverages on 18,609 participants aged 40–79 years and showed a significant correlation between coffee consumption and the risk of cardiovascular death in those with grade 2–3 hypertension with multivariable HRs of 0.98 (95% CI 0.67–1.43) for < 1 cup/day, 0.74 (95% CI 0.37–1.46) for 1 cup/day, and 2.05 (95% CI 1.17–3.59) for ≥ 2 cups/day, in comparison with non-coffee drinkers. No correlation was found between coffee consumption and cardiovascular mortality in participants with optimal and normal blood pressure, high‐normal blood pressure, or grade 1 hypertension. Green tea consumption was not associated with an increased risk of cardiovascular death across any blood pressure categories [28]. To evaluate the long-term cardiovascular effects of caffeine, data of 6076 elderly hypertensive patients from the National Health and Nutrition Examination Survey were analyzed and 2200 all-cause and 765 cardiovascular mortality cases were detected during the follow-up of 6.86 ± 0.12 years. In this study, caffeine intake was evaluated by dietary recall interviews. The participant with moderate caffeine intake (200 to < 300 mg/day) had a lower risk of all-cause (HR 0.70, 95% CI 0.56–0.87) and cardiovascular (HR 0.55, 95% CI 0.39–0.77) mortality. These beneficial effects of caffeine on all-cause mortality were not significant in those with poorly controlled blood pressure [29]. These studies supported the hypothesis that clinical outcomes of caffeine and caffeinated beverages depend on the level of blood pressure control. This report also showed that the use of moderate caffeine intake (200 to < 300 mg/day) could reduce all-cause mortality risk in female patients, but not in male patients (HR 0.65, 95% CI 0.50–0.85) [29]. Another prospective study in 29,985 postmenopausal normotensive women revealed that neither caffeinated coffee consumption (2–3 cups per day) nor caffeine administration (196 mg/day) had a clinically meaningful effect on systolic or diastolic blood pressure [30].
Another probable predisposing factor is the level of stress in individuals. A randomized double-blind crossover trial among 31 male medical students showed that stress and caffeine additively increase blood pressure (low risk, + 9/5 mm Hg; high risk + 10/6 mm Hg). In addition, 46% of high-risk cases experienced mean systolic blood pressure ≥ 140 mm Hg after caffeine consumption. As a result, in those with high environmental stressors, epidemiologic markers for developing hypertension such as positive parental history and borderline hypertension should be considered [31]. In line with these reports, Bennett et al. evaluated the bio-behavioral effects of anhydrous caffeine 3.3 mg/kg among 52 normotensive adults aged 21.4 ± 0.3 years. The results showed a significant increase during stress followed by a decrease in the recovery phase. Caffeine administration, however, has been shown to increase systolic blood pressure during stress response and delay recovery [32]. These findings also highlighted the effects of stress levels on patients’ clinical response to caffeine and their possibly developing hypertension. A cohort study with 8780 participants found that drinking caffeinated coffee at least twice a day (150 mL/day) reduced the risk of hypertension only in non-smokers [33].
Surprisingly, similar to every clinical response of patients to pharmacological agents, the role of genotype variations has been proposed to play a key role in the response of patients to caffeine use. Recently, a study in 19,133 members showed that administration of coffee, particularly in people with the cytochrome P450 1A2 rs762551 AC + CC genotype, was associated with a lower risk of hypertension (odds ratio 0.678, 95% CI 0.722–900, P = 0.0001) [34]. The effects of caffeine on blood pressure are not obvious and depend on various factors, such as the level of stress, genetic variations, smoking, and the presence of hypertension.
5.2 Arrhythmia
Clinicians commonly face the problem of treating patients with cardiac arrhythmias and their complications. Consequently, identification of arrhythmia etiology seems to be an important step in decreasing arrhythmia.
The arrhythmogenic effects of caffeine have been widely shown in many animal studies. A study in canine models revealed that the arrhythmogenesis property of caffeine is dose dependent. In this regard, injection of low-dose caffeine leads to benign arrhythmias most probably due to vagal stimulation, while administration of a high dose is associated with more severe arrhythmias, such as ventricular tachycardia, atrial fibrillation (AF), and ventricular premature contractions [35]. Another study in rat models was conducted to examine the toxicity of injected caffeine. The results showed that administration of 15 mg/kg/min of caffeine leads to sinus tachycardia and ectopic beats in the heart [36]. To evaluate safety concerns, a study in rabbits showed continuous infusion of caffeine at a dose of 1 mg/kg/min is correlated with an increased risk of ventricular tachycardia [37].
Several cohort and cross-sectional studies have been carried out to determine the relationship between the use of caffeine and caffeinated drinks and arrhythmia. A study was conducted to assess the incidence of arrhythmias in 33,638 female individuals with no history of CVD or AF. The data analysis showed that there was no significant association between the use of caffeine with an incident of AF (P = 0.45) [38]. Mostofsky et al., in contrast, examined data from 57,053 people over a 13.5-year period. The data analysis showed an inverse association between the levels of coffee consumption and the incidents of AF with HRs of 0.93, 0.88, 0.86, 0.84, 0.79, and 0.79 for < 1 cup per day, 1 cup per day, 2–3 cups per day, 4–5 cups per day, 6–7 cups per day, and > 7 cups per day (P-linear trend = 0.02) [39]. Larsson et al. aimed to evaluate the correlation between coffee consumption and AF in two prospective cohorts, and to summarize available evidence using a meta-analysis. Results from two prospective cohort studies including 41,881 men and 34,594 women showed that coffee consumption did not increase the risk of AF. Similar findings have been demonstrated in the meta-analysis including six cohort studies with a total of 10,406 patients with AF among 248,910 individuals [40]. In the Klatsky et al. cohort study in 130,054 persons with previous data about coffee habits, coffee and caffeine intake reduced the risk of hospitalization for arrhythmias, mainly supraventricular arrhythmias [41]. In another cross-sectional study, no report of premature beats with a low consumption of coffee was observed [42]. A randomized double-blind clinical trial on 51 patients with left ventricular dysfunction showed that there was no significant association between the use of 500 mg of caffeine with the incidence of ventricular (P = 0.47) and supraventricular premature beats (P = 0.44) [43]. Another study carried out on 101 participants showed no significant association between the use of different amounts of caffeine (200 mg/day, 200–400 mg/day, and >400 mg/day) with arrhythmia [44]. Similarly, an evaluation of 47,949 individuals demonstrated no significant correlation between the amount of caffeine with the incident of AF or atrial flutter in a 5-year follow-up period [45]. According to a systematic review and meta-analysis of seven human studies and two animal studies, the overall relative risk of ventricular premature beats was 1.00 (95% CI 0.94–1.06; I (2) 13.5%, P for heterogeneity = 0.32) in human studies, while a notable mean difference of − 2.15 mA in the ventricular fibrillation threshold was observed in animal studies (95% CI − 3.43 to − 0.87; I (2) 0.0%, P for heterogeneity = 0.37). The observed difference between animal and human studies is most likely owing to higher doses of caffeine (35 mg/kg) [46]. While no correlation between coffee consumption and the risk of arrhythmias was reported in some clinical studies, some new studies suggested an inverse correlation between moderate caffeinated coffee drinking and the risk of AF.
Bazal et al. evaluated the link between caffeinated coffee drinking and risk of AF in two Spanish cohort studies including 18,983 and 6479 individuals. In the first and second cohort studies, 97 and 250 cases of AF were detected during median follow-up periods of 10.3 and 4.4 years, respectively. A data analysis of these prospective Mediterranean cohorts revealed an inverse correlation between caffeinated coffee drinking (1–7 cups/week) and the risk of AF (HR 0.60, 95% CI 0.44–0.82) [47]. Recently, the long-term effects of three types of coffee on CVD and mortality were evaluated using the UK Biobank database. A total of 449,563 individuals with a median age of 58 years were followed for 12.5 ± 0.7 years. All coffee types significantly reduced all-cause death and the maximum risk decline was detected with a daily intake of 2–3 cups for decaffeinated coffee (HR 0.86, 95% CI 0.81–0.91, P < 0.0001); instant coffee (HR 0.89, 95% CI 0.86–0.93, P < 0.0001), and ground coffee (HR 0.73, 95% CI 0.69–0.78, P < 0.0001). Similarly, compared with non-drinkers, all coffee subtypes significantly decreased the risk of CVDs (the lowest risk was 2–3 cups/day for decaffeinated coffee, P = 0.0093; instant coffee, P < 0.000; and ground, P < 0.0001). In contrast to decaffeinated coffee, 2–3 cups/day of instant coffee (HR 0.88, 95% CI 0.85–0.92, P < 0.0001) and 4–5 cups/day of ground coffee (HR 0.83, 95% CI 0.76–0.91, P < 0.0001) led to a significant reduction in the incidence of arrhythmia [48].
5.3 Dyslipidemia
Dyslipidemia is known as an increased level of total cholesterol, triglycerides, low-density lipoprotein (LDL), and decreased high-density lipoprotein (HDL). Dyslipidemia plays an important role in CVDs, such as acute coronary syndrome (ACS) and hypertension [49]. Dyslipidemia and its complications cause significant mortality and considerable cost to the healthcare system [50]. The main cause of atherosclerosis is a high level of LDL in the serum [51]. Dyslipidemia plays an important role in the development of atherosclerosis, which could lead to a wide range of CVDs [52].
A study in male Sprague-Dawley rats showed that 0.12 g/100 g body weight/day freeze-dried instant coffee led to significantly higher triglyceride levels and lower HDL-cholesterol levels compared with the control group [53]. A randomized placebo-controlled clinical trial in women aged 30–50 years with a body mass index of more than 30 kg/m2 showed that use of green coffee bean extract with elastic resistance band training could reduce serum levels of HDL and total cholesterol (P = 0.023 and P = 0.006). Moreover, the use of green coffee bean extract significantly decreased total cholesterol (P = 0.041) [54]. A systematic review and meta-analysis of 12 randomized controlled trials showed that the use of coffee is significantly associated with increased serum levels of total cholesterol (P = 0.017), triglycerides (P = 0.006), and low-density lipoprotein (P = 0.003). Whereas, it has no significant effect on HDL (P = 0.707). Although there was a smaller increase in total cholesterol, triglycerides, LDL, and HDL in the mean use of fewer than 5 cups of coffee per day, the results showed that a high consumption of caffeine (≥ 6 cups per day) was related to high levels of total cholesterol, triglycerides, LDL, and HDL [55]. Similarly, another meta-analysis of 12 studies including 1017 individuals showed that coffee consumption for 45 days led to 8.1 mg/dL (P < 0.001), 5.4 mg/dL (P = 0.009), and 12.6 mg/dL (P = 0.007) increases in total cholesterol, LDL, and triglycerides, respectively. Those who had hyperlipidemia were more susceptible to the cholesterol-raising effect of coffee. Additionally, a meta-regression analysis revealed a positive dose–response relationship between coffee intake and TC, LDL, and triglyceride levels [56]. Petrovic et al. evaluated the associations between caffeine-derived metabolites and plasma lipids using population-based data from northern Belgium (n = 1987; 1055 [53%] female participants) and three Swiss cities (n = 990; 523 [53%] female participants). Interestingly, a data analysis showed a positive correlation between plasma and urinary caffeine, paraxanthine, and theophylline with plasma lipids, probably owing to the sympathomimetic function of methylxanthines [57].
A local community-based cohort was carried out to evaluate the effect of genetic differentials among coffee consumers. The results showed that there was an inverse relationship between coffee consumption and the incidence of dyslipidemia in female participants (odds ratio: 0.768, 95% CI 0.645–0.914, P = 0.0030). Moreover, it was revealed that these beneficial effects on the risk of dyslipidemia from coffee consumption are genotype dependent. In this regard, they discovered that female individuals with the minor alleles of ADORA1 rs10800901 (P = 0.0168), ADORA2B rs2779212 (P = 0.0004), and ADORA3 rs2786967 (P = 0.0384) benefit more from coffee on the risk of dyslipidemia, whereas male participants with the minor allele of ADORA3A rs3393 have a lower risk [58]. According to most of the studies, the use of caffeine and coffee could increase total cholesterol; however, sex, genetic factors, and effects of other ingredients in coffee should be considered for achieving more confident results.
5.4 Acute Coronary Syndrome
Acute coronary syndrome is the most common clinical manifestation of cardiac disease. It is mainly due to atherosclerotic plaques that form in coronary arteries over several years. This atherosclerotic plaque is made up of cholesterol, macrophages, and fibrous tissues, and it can cause artery occlusion [59, 60]. The progression of the disease to more advanced and clinically symptomatic phases would take several years and the rupture of highly developed plaque causes ACS [61]. Similar to other CVDs, some cases of ACS have been reported following the use of caffeine and caffeinated drinks.
Levent and Yolcu reported a case of NSTEMI with no medical history of chronic diseases after consumption of 500-mL energy drinks consisting of caffeine [62]. A large well-documented study, in contrast, found no evidence of caffeine-related adverse events in patients with ACS. A randomized controlled trial on 103 patients with acute STEMI showed that short-term use of 352.5 ± 90 mg of caffeine was considered to be safe regarding cardiovascular adverse effects [63]. A cohort prospective study was carried out in 1085 patients with prior acute myocardial infarction or unstable angina to evaluate the effects of 12.5 mL/day of coffee drink and mortality risk. The result showed that consuming 1–3 cups of coffee per day is associated with an 81% lower risk of mortality [64]. In line with these results, a systematic review and meta-analysis of prospective studies evaluated the relationship between coffee intake and mortality in patients with a history of acute myocardial infarction. The results showed that use of 1–2 cups and > 2 cups per day was associated with a risk ratio of 0.79 (95% CI 0.66–0.94, P = 0.008) and 0.54 (95% CI 0.45–0.65, P = 0.00001) compared with non-coffee drinkers. Moreover, comparing effects of heavy coffee drinkers with light coffee drinkers showed a risk ratio of 0.69 (95% CI 0.58–0.83, P < 0.0001) [65]. The well-designed studies have shown the mortality benefits of caffeine in patients with ACS. In addition, it has been hypothesized that caffeine could improve ticagrelor-related dyspnea by an antagonist of adenosine [66]. In the Surma et al. recent study, the anti-inflammatory properties and clinical importance of tea and coffee have been discussed. The authors concluded that despite controversial results of clinical studies, tea and coffee might reduce inflammatory biomarkers and prevent atherosclerotic CVDs and other inflammatory diseases [67]. According to the Chieng et al. study, mild-to-moderate coffee consumption (2–3 cups daily) could reduce the risk of coronary heart disease, arrhythmia, heart failure (HF), and cardiovascular death. Both studies have suggested habitual coffee and tea consumption as part of a healthy lifestyle [68].
5.5 Stable Angina
Current therapeutic strategies reduce the ischemic burden and improve prognosis in patients with chronic stable angina. It has been proposed that caffeine may have beneficial effects in patients with chronic stable angina. In a rat model, caffeine has been shown to stimulate the production of prostaglandin I2 as a vasodilator from blood vessels in a rat model and increase cardiac output, stroke volume, and cardiac contractility [69]. Based on this possible pharmacological mechanism, the acute coffee intake on exercise-induced angina was studied in 17 men with coronary artery disease using a double-blind treadmill protocol. A data analysis showed that the use of 1 and 2 cups of caffeinated coffee led to an increase in exercise duration until the onset of angina (8% and 12%, respectively, P < 0.05); however, decaffeinated coffee had no effect. Rate pressure product and the extent of ST-segment depression at angina were similar following ingestion of caffeinated and decaffeinated coffee [70]. It seems that a low-to-moderate amount of coffee could increase the time to onset of angina in patients with chronic stable angina.
5.6 Heart Failure
Heart failure is one of the main causes of mortality and morbidity worldwide. The American College of Cardiology Foundation/American Heart Association defined HF as a complex clinical syndrome characterized by any structural or functional heart abnormality [71]. The prevalence of HF is more than 5.8 million in the USA [72]. The effects of caffeine on HF have been evaluated in some animal studies. It has been shown that caffeine could increase basal renin secretion through an intrarenal adenosine receptor blockage leading to increased symptomatic activity. Another study was carried out in rats to evaluate the effects of both acute and short-term caffeine use on heart performance. First, caffeine with a loading dose of 10 mg/kg followed by 150 g/min over 40 minutes increased heart rate and left ventricular peak systolic pressure; however, no significant effect was observed on cardiac contractility. Moreover, it could increase plasma norepinephrine, epinephrine, and renin activity levels. To evaluate the effects of short-term effects, administration of caffeine (0.1%) for 10 days has no significant effect on cardiac time-pressure variables, or hemodynamic or renal excretory function parameters, while it could increase renal renin secretion [73].
Human studies have been conducted to evaluate the effects of caffeine and coffee on HF. A study in humans examined the caffeine effect on exercise duration in HF. Ten patients with HF used 4 mg/kg of caffeine on 2 separate days in a double-blind, randomized, crossover design. The results of this study suggest that using caffeine increases exercise performance alongside duration, and this can improve patients’ quality of life [74]. Bodar et al. prospectively evaluated the correlation between coffee and HF in 20,433 male patients with a mean age of 66.4 ± 9.2 years. During a mean follow-up of 9.3 years, 901 patients with a new diagnosis of HF were detected. A data analysis revealed no significant correlation between coffee (P for linear trend = 0.47) and caffeine (P for linear trend = 0.34) intake and the risk of HF in the US population [75]. Similarly, a Mendelian randomization study found no correlation between coffee consumption and HF [76]. A systematic review and meta-analysis including 140,220 patients demonstrated that ingesting 4 cups of coffee per day could be protective against HF [77]. The studies investigating the potential benefits of caffeine in the CVDs are summarized in Table 1.
6 Limitations
There may be some limitations to the current comprehensive review. First, the quality and quantity of studies on the potential effects of caffeine in the management of various CVDs vary significantly, which makes it difficult to draw a clear conclusion. Second, different caffeine sources, doses, and durations were used in the studies. In addition, the potential effects of additional ingredients and confounding dietary factors on CVDs should not be ignored. Third, the majority of studies had a heterogonous population, which can affect the net results. Finally, while we attempted to discuss the available evidence, relevant research may be overlooked because of the nature of the review articles.
7 Conclusions
This review addressed the current literature regarding pharmacological, preclinical, and clinical studies on the potential effects of caffeine in the CVDs as well as its potential beneficial and harmful effects. The content of the present review should be interpreted with caution because of the existence of multiple confounding factors in the caffeine studies. Despite the potential pharmacological benefits of caffeine on CVDs, there is still conflicting clinical evidence regarding the efficacy and safety of caffeine on CVDs. Insufficient standardization of dose, duration, and regularity of caffeine intake in different studies, other ingredients of caffeinated beverages, and dietary factors as well as the demographic and clinical data of individuals, such as sex, genetic variations, smoking, obesity, comorbidities, and other confounding factors may affect the results. Caffeine seems to be safe in individuals without significant CVDs, as far as available evidence shows. Performing further well-designed cohort studies and randomized controlled trials with large sample sizes and adequate control of the confounding factors is recommended to evaluate the cardiovascular safety and efficacy of caffeine. The direction of future research should also be aimed at determining the appropriate amount of caffeine intake in individuals with and without CVDs.
References
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics: 2013 update: a report from the American Heart Association. Circulation. 2013. https://doi.org/10.1161/CIR.0b013e31828124ad.
Writing Committee: Smith Jr SC, Collins A, Ferrari R, Holmes Jr DR, Logstrup S, et al. Our time: a call to save preventable death from cardiovascular disease (heart disease and stroke). Eur Heart J. 2012. https://doi.org/10.1016/j.gheart.2012.08.002.
Keyhan G, Chen SF, Pilote L. Angiotensin-converting enzyme inhibitors and survival in women and men with heart failure. Eur J Heart Fail. 2007. https://doi.org/10.1016/j.ejheart.2007.03.004.
Khan MS, Fonarow GC, Ahmed A, Greene SJ, Vaduganathan M, Khan H, et al. Dose of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers and outcomes in heart failure: a meta-analysis. Circ Heart Fail. 2017. https://doi.org/10.1161/circheartfailure.117.003956.
Bouabdallaoui N, Tardif J-C, Waters DD, Pinto FJ, Maggioni AP, Diaz R, et al. Time-to-treatment initiation of colchicine and cardiovascular outcomes after myocardial infarction in the Colchicine Cardiovascular Outcomes Trial (COLCOT). Eur Heart J. 2020. https://doi.org/10.1093/eurheartj/ehaa659.
Samuel M, Tardif J-C, Khairy P, Roubille F, Waters DD, Grégoire JC, et al. Cost-effectiveness of low-dose colchicine after myocardial infarction in the Colchicine Cardiovascular Outcomes Trial (COLCOT). Eur Heart J Qual Care Clin Outcomes. 2021. https://doi.org/10.1093/ehjqcco/qcaa045.
Annink KV, Franz AR, Derks JB, Rudiger M, Bel FV, Benders MJ. Allopurinol: old drug, new indication in neonates? Curr Pharm Des. 2017. https://doi.org/10.2174/1381612823666170918123307.
Willson C. The clinical toxicology of caffeine: a review and case study. Toxicol Rep. 2018. https://doi.org/10.1016/j.toxrep.2018.11.002.
Nationa Coffee Association. National coffee drinking trends. New York: National Coffee Association; 2014.
Oñatibia-Astibia A, Franco R, Martínez-Pinilla E. Health benefits of methylxanthines in neurodegenerative diseases. Mol Nutr Food Res. 2017;61:1600670.
El Agaty S, Seif A. Cardiovascular effects of long-term caffeine administration in aged rats. Irish J Med Sci. 2015. https://doi.org/10.1007/s11845-014-1098-z.
Voskoboinik A, Koh Y, Kistler PM. Cardiovascular effects of caffeinated beverages. Trends Cardiovasc Med. 2019. https://doi.org/10.1016/j.tcm.2018.09.019.
Chou TM, Benowitz NL. Caffeine and coffee: effects on health and cardiovascular disease. Comp Biochem Physiol C Pharmacol Toxicol Endocrinol. 1994;109:173.
Shin S, Lee JE, Loftfield E, Shu X-O, Abe SK, Rahman MS, et al. Coffee and tea consumption and mortality from all causes, cardiovascular disease and cancer: a pooled analysis of prospective studies from the Asia Cohort Consortium. Int J Epidemiol. 2022. https://doi.org/10.1093/ije/dyab161.
Kolahdouzan M, Hamadeh MJ. The neuroprotective effects of caffeine in neurodegenerative diseases. CNS Neurosci Ther. 2017. https://doi.org/10.1111/cns.12684.
Magkos F, Kavouras SA. Caffeine use in sports, pharmacokinetics in man, and cellular mechanisms of action. Crit Rev Food Sci Nutr. 2005. https://doi.org/10.1080/1040-830491379245.
Ngueta G. Caffeine and caffeine metabolites in relation to hypertension in US adults. Eur J Clin Nutr. 2020. https://doi.org/10.1038/s41430-019-0430-0.
Dhalla NS, Temsah RM, Netticadan T. Role of oxidative stress in cardiovascular diseases. J Hypertens. 2000. https://doi.org/10.1097/00004872-200018060-00002.
Alsabri SG, Mari WO, Younes S, Alsadawi MA, Oroszi TL. Kinetic and dynamic description of caffeine. J Caffeine Adenosine Res. 2018.
Fisone G, Borgkvist A, Usiello A. Caffeine as a psychomotor stimulant: mechanism of action. Cell Mol Life Sci. 2004;61:857.
Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020. https://doi.org/10.1038/s41581-019-0244-2.
Oboh G, Ojueromi OO, Ademosun AO, Omayone TP, Oyagbemi AA, Ajibade TO, et al. Effects of caffeine and caffeic acid on selected biochemical parameters in L-NAME-induced hypertensive rats. J Food Biochem. 2021. https://doi.org/10.1111/jfbc.13384.
Noordzij M, Uiterwaal CS, Arends LR, Kok FJ, Grobbee DE, Geleijnse JM. Blood pressure response to chronic intake of coffee and caffeine: a meta-analysis of randomized controlled trials. J Hypertens. 2005. https://doi.org/10.1097/01.hjh.0000166828.94699.1d.
Chei C-L, Loh JK, Soh A, Yuan J-M, Koh W-P. Coffee, tea, caffeine, and risk of hypertension: the Singapore Chinese Health Study. Eur J Nutr. 2018. https://doi.org/10.1007/s00394-017-1412-4.
D’Elia L, La Fata E, Galletti F, Scalfi L, Strazzullo P. Coffee consumption and risk of hypertension: a dose–response meta-analysis of prospective studies. Eur J Nutr. 2019. https://doi.org/10.1007/s00394-017-1591-z.
Hartley TR, Sung BH, Pincomb GA, Whitsett TL, Wilson MF, Lovallo WR. Hypertension risk status and effect of caffeine on blood pressure. Hypertension. 2000. https://doi.org/10.1161/01.hyp.36.1.137.
Pincomb GA, Lovallo WR, McKey BS, Sung BH, Passey RB, Everson SA, et al. Acute blood pressure elevations with caffeine in men with borderline systemic hypertension. Am J Cardiol. 1996. https://doi.org/10.1016/s0002-9149(97)89392-7.
Teramoto M, Yamagishi K, Muraki I, Tamakoshi A, Iso H. Coffee and green tea consumption and cardiovascular disease mortality among people with and without hypertension. J Am Heart Assoc. 2023. https://doi.org/10.1161/JAHA.122.026477.
Chen S, Li J, Gao M, Li D, Shen R, Lyu L, et al. Association of caffeine intake with all-cause and cardiovascular mortality in elderly patients with hypertension. Frontier Nutr. 2022. https://doi.org/10.3389/fnut.2022.1023345.
Rhee JJ, Qin F, Hedlin HK, Chang TI, Bird CE, Zaslavsky O, et al. Coffee and caffeine consumption and the risk of hypertension in postmenopausal women. Am J Clin Nutr. 2016. https://doi.org/10.3945/ajcn.115.120147.
Shepard JD, al’absi M, Whitsett TL, Passey RB, Lovallo WR. Additive pressor effects of caffeine and stress in male medical students at risk for hypertension. Am J Hypertens. 2000. https://doi.org/10.1016/s0895-7061(99)00217-4.
Bennett JM, Rodrigues IM, Klein LC. Effects of caffeine and stress on biomarkers of cardiovascular disease in healthy men and women with a family history of hypertension. Stress Health. 2013. https://doi.org/10.1002/smi.2486.
Miranda AM, Goulart AC, Benseñor IM, Lotufo PA, Marchioni DM. Coffee consumption and risk of hypertension: a prospective analysis in the cohort study. Clin Nutr. 2021. https://doi.org/10.1016/j.clnu.2020.05.052.
Hou C-C, Tantoh DM, Lin C-C, Chen P-H, Yang H-J, Liaw Y-P. Association between hypertension and coffee drinking based on CYP1A2 rs762551 single nucleotide polymorphism in Taiwanese. Nutr Metabol. 2021. https://doi.org/10.1186/s12986-021-00605-9.
Mehta A, Jain A, Mehta M, Billie M. Caffeine and cardiac arrhythmias: an experimental study in dogs with review of literature. Acta Cardiol. 1997.
Strubelt O, Strubelt MO, Diederich K-W. Experimental treatment of the acute cardiovascular toxicity of caffeine. J Toxicol. 1999. https://doi.org/10.1081/clt-100102405.
Ishida S, Ito M, Takahashi N, Fujino T, Akimitsu T, Saikawa T. Caffeine induces ventricular tachyarrhythmias possibly due to triggered activity in rabbits in vivo. Jpn Circ J. 1996. https://doi.org/10.1253/jcj.60.157.
Conen D, Chiuve SE, Everett BM, Zhang SM, Buring JE, Albert CM. Caffeine consumption and incident atrial fibrillation in women. Am J Clin Nutr. 2010. https://doi.org/10.3945/ajcn.2010.29627.
Mostofsky E, Johansen MB, Lundbye-Christensen S, Tjønneland A, Mittleman MA, Overvad K. Risk of atrial fibrillation associated with coffee intake: findings from the Danish Diet, Cancer, and Health Study. Eur J Prevent Cardiol. 2016. https://doi.org/10.1177/2047487315624524.
Larsson SC, Drca N, Jensen-Urstad M, Wolk A. Coffee consumption is not associated with increased risk of atrial fibrillation: results from two prospective cohorts and a meta-analysis. BMC Med. 2015. https://doi.org/10.1186/s12916-015-0447-8.
Klatsky AL, Hasan AS, Armstrong MA, Udaltsova N, Morton C. Coffee, caffeine, and risk of hospitalization for arrhythmias. Permanente J. 2011. https://doi.org/10.7812/tpp/11-020.
Dixit S, Stein PK, Dewland TA, Dukes JW, Vittinghoff E, Heckbert SR, et al. Consumption of caffeinated products and cardiac ectopy. J Am Heart Assoc. 2016. https://doi.org/10.1161/jaha.115.002503.
Zuchinali P, Souza GC, Pimentel M, Chemello D, Zimerman A, Giaretta V, et al. Short-term effects of high-dose caffeine on cardiac arrhythmias in patients with heart failure: a randomized clinical trial. JAMA Intern Med. 2016. https://doi.org/10.1001/jamainternmed.2016.6374.
Posch MI, Kay MD, Harhash AA, Huang JJ, Krupinski EA, Abidov A, et al. Daily caffeine consumption is associated with decreased incidence of symptoms and hemodynamic changes during pharmacologic stress with regadenoson. J Nucl Med Technol. 2020. https://doi.org/10.2967/jnmt.118.225219.
Frost L, Vestergaard P. Caffeine and risk of atrial fibrillation or flutter: the Danish Diet, Cancer, and Health Study. Am J Clin Nutr. 2005. https://doi.org/10.1093/ajcn/81.3.578.
Zuchinali P, Ribeiro PA, Pimentel M, da Rosa PR, Zimerman LI, Rohde LE. Effect of caffeine on ventricular arrhythmia: a systematic review and meta-analysis of experimental and clinical studies. Europace. 2016. https://doi.org/10.1093/europace/euv261.
Bazal P, Gea A, Navarro A, Salas-Salvadó J, Corella D, Alonso-Gómez A, et al. Caffeinated coffee consumption and risk of atrial fibrillation in two Spanish cohorts. Eur J Prevent Cardiol. 2021. https://doi.org/10.1177/2047487320909065.
Chieng D, Canovas R, Segan L, Sugumar H, Voskoboinik A, Prabhu S, et al. The impact of coffee subtypes on incident cardiovascular disease, arrhythmias, and mortality: long-term outcomes from the UK Biobank. Eur J Prevent Cardiol. 2022. https://doi.org/10.1093/eurjpc/zwac189.
Rouhani MH, Rashidi-Pourfard N, Salehi-Abargouei A, Karimi M, Haghighatdoost F. Effects of egg consumption on blood lipids: a systematic review and meta-analysis of randomized clinical trials. J Am Coll Nutr. 2018. https://doi.org/10.1080/07315724.2017.1366878.
Smith G. Epidemiology of dyslipidemia and economic burden on the healthcare system. Am J Manage Care. 2007.
Bhandari S, Gupta P, Quinn P, Sandhu J, Hakimi A, Jones D, et al. Pleiotropic effects of statins in hypercholesterolaemia: a prospective observational study using a lipoproteomic based approach. Lancet. 2015. https://doi.org/10.1016/s0140-6736(15)60336-1.
Koene RJ, Prizment AE, Blaes A, Konety SH. Shared risk factors in cardiovascular disease and cancer. Circulation. 2016. https://doi.org/10.1161/circulationaha.115.020406.
Choi E-Y, Cho Y-O. Interaction of physical trainings and coffee intakes in fuel utilization during exercise in rats. Nutr Res Pract. 2013. https://doi.org/10.4162/nrp.2013.7.3.178.
Banitalebi E, Rahimi A, Faramarzi M, Ghahfarrokhi MM. The effects of elastic resistance band training and green coffee bean extract supplement on novel combined indices of cardiometabolic risk in obese women. Res Pharm Sci. 2019. https://doi.org/10.4103/1735-5362.268202.
Du Y, Lv Y, Zha W, Hong X, Luo Q. Effect of coffee consumption on dyslipidemia: a meta-analysis of randomized controlled trials. Nutr Metab Cardiovasc Dis. 2020. https://doi.org/10.1016/j.numecd.2020.08.017.
Cai L, Ma D, Zhang Y, Liu Z, Wang P. The effect of coffee consumption on serum lipids: a meta-analysis of randomized controlled trials. Eur J Clin Nutr. 2012. https://doi.org/10.1038/ejcn.2012.68.
Petrovic D, Pruijm M, Ponte B, Dhayat NA, Ackermann D, Ehret G, et al. Investigating the relations between caffeine-derived metabolites and plasma lipids in 2 population-based studies. Mayo Clin Proc. 2021;96:3071–85.
Han J, Shon J, Hwang J-Y, Park YJ. Effects of coffee intake on dyslipidemia risk according to genetic variants in the adora gene family among Korean adults. Nutrients. 2020. https://doi.org/10.3390/nu12020493.
Boersma E, Mercado N, Poldermans D, Gardien M, Vos J, Simoons ML. Acute myocardial infarction. Lancet. 2003. https://doi.org/10.1016/s0140-6736(03)12712-2.
Mackman N. Triggers, targets and treatments for thrombosis. Nature. 2008. https://doi.org/10.1038/nature06797.
Braunwald E, Morrow DA. Unstable angina: is it time for a requiem? Circulation. 2013. https://doi.org/10.1161/circulationaha.113.001258.
Levent S, Yolcu S. A rare adverse effect of energy drinks: non-ST-elevation myocardial infarction. Hong Kong J Emerg Med. 2018. https://doi.org/10.1177/1024907917751302.
Richardson T, Baker J, Thomas P, Meckes C, Rozkovec A, Kerr D. Randomized control trial investigating the influence of coffee on heart rate variability in patients with ST-segment elevation myocardial infarction. QJM. 2009. https://doi.org/10.1093/qjmed/hcp072.
Miranda AM, Goulart AC, Bensenor IM, Lotufo PA, Marchioni DM. Moderate coffee consumption is associated with lower risk of mortality in prior acute coronary syndrome patients: a prospective analysis in the ERICO cohort. Int J Food Sci Nutr. 2021. https://doi.org/10.1080/09637486.2020.1862069.
Brown OI, Allgar V, Wong KYK. Coffee reduces the risk of death after acute myocardial infarction: a meta-analysis. Coron Artery Dis. 2016. https://doi.org/10.1097/mca.0000000000000397.
Lindholm D, Storey RF, Christersson C, Halvorsen S, Grove EL, Braun OÖ, et al. Design and rationale of TROCADERO: a trial of caffeine to alleviate dyspnea related to ticagrelor. Am Heart J. 2015. https://doi.org/10.1016/j.ahj.2015.06.014.
Surma S, Sahebkar A, Banach M. Coffee or tea: Anti-inflammatory properties in the context of atherosclerotic cardiovascular disease prevention. Pharmacol Res. 2022. https://doi.org/10.1016/j.phrs.2022.106596.
Chieng D, Kistler PM. Coffee and tea on cardiovascular disease (CVD) prevention. Trends Cardiovasc Med. 2022. https://doi.org/10.1016/j.tcm.2021.08.004.
Naderali E, Poyser N. The effect of caffeine on prostaglandin output from the perfused mesenteric vascular bed of the rat. Prostagland Leukot Essent Fatty Acids. 1994. https://doi.org/10.1016/0952-3278(94)90058-2.
Piters KM, Colombo A, Olson HG, Butman SM. Effect of coffee on exercise-induced angina pectoris due to coronary artery disease in habitual coffee drinkers. Am J Cardiol. 1985. https://doi.org/10.1016/0002-9149(85)90360-1.
Clyde W, Jessup Y, Bozkurt B. ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013. https://doi.org/10.1016/j.jacc.2013.05.019.
Roger VL. Epidemiology of heart failure. Circ Res. 2013. https://doi.org/10.1161/circresaha.113.300268.
Tofovic SP, Kusaka H, Rominski B, Jackson EK. Caffeine increases renal renin secretion in a rat model of genetic heart failure. J Cardiovasc Pharmacol. 1999. https://doi.org/10.1097/00005344-199903000-00015.
Notarius CF, Morris B, Floras JS. Caffeine prolongs exercise duration in heart failure. J Cardiac Fail. 2006. https://doi.org/10.1016/j.cardfail.2005.12.005.
Bodar V, Chen J, Sesso HD, Gaziano JM, Djoussé L. Coffee consumption and risk of heart failure in the Physicians’ Health Study. Clin Nutr ESPEN. 2020. https://doi.org/10.1016/j.clnesp.2020.09.216.
van Oort S, Beulens JW, van Ballegooijen AJ, Handoko ML, Larsson SC. Modifiable lifestyle factors and heart failure: a Mendelian randomization study. Am Heart J. 2020. https://doi.org/10.1016/j.ahj.2020.06.007.
Mostofsky E, Rice MS, Levitan EB, Mittleman MA. Habitual coffee consumption and risk of heart failure: a dose-response meta-analysis. Circ Heart Fail. 2012. https://doi.org/10.1161/circheartfailure.112.967299.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this article.
Conflicts of interest/competing interests
Sajad Khiali, Amin Agabalazadeh, Hadi Sahrai, Hossein Bannazadeh Baghi, Gholamreza Rahbari Banaeian , and Taher Entezari-Maleki have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Dvailability of data and material
Data sharing is not applicable to this article as no datasets were generated.
Code availability
Not applicable.
Authors’ contributions
SK, AA, and HS searched the literature and wrote the manuscript; TE, HB, and GR reviewed and revised the manuscript; and TE selected the literature and designed, revised, and edited the manuscript. All of the authors have read and approved the final manuscript.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khiali, S., Agabalazadeh, A., Sahrai, H. et al. Effect of Caffeine Consumption on Cardiovascular Disease: An Updated Review. Pharm Med 37, 139–151 (2023). https://doi.org/10.1007/s40290-023-00466-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40290-023-00466-y