Abstract
Whereas exercise training, as part of multidisciplinary rehabilitation, is a key component in the management of patients with chronic coronary syndrome (CCS) and/or congestive heart failure (CHF), physicians and exercise professionals disagree among themselves on the type and characteristics of the exercise to be prescribed to these patients, and the exercise prescriptions are not consistent with the international guidelines. This impacts the efficacy and quality of the intervention of rehabilitation. To overcome these barriers, a digital training and decision support system [i.e. EXercise Prescription in Everyday practice & Rehabilitative Training (EXPERT) tool], i.e. a stepwise aid to exercise prescription in patients with CCS and/or CHF, affected by concomitant risk factors and comorbidities, in the setting of multidisciplinary rehabilitation, was developed. The EXPERT working group members reviewed the literature and formulated exercise recommendations (exercise training intensity, frequency, volume, type, session and programme duration) and safety precautions for CCS and/or CHF (including heart transplantation). Also, highly prevalent comorbidities (e.g. peripheral arterial disease) or cardiac devices (e.g. pacemaker, implanted cardioverter defibrillator, left-ventricular assist device) were considered, as well as indications for the in-hospital phase (e.g. after coronary revascularisation or hospitalisation for CHF). The contributions of physical fitness, medications and adverse events during exercise testing were also considered. The EXPERT tool was developed on the basis of this evidence. In this paper, the exercise prescriptions for patients with CCS and/or CHF formulated for the EXPERT tool are presented. Finally, to demonstrate how the EXPERT tool proposes exercise prescriptions in patients with CCS and/or CHF with different combinations of CVD risk factors, three patient cases with solutions are presented.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Current exercise prescriptions to patients with cardiovascular disease are often not in line with official recommendations, and healthcare professionals/clinicians often disagree among themselves. |
To overcome these barriers, a digital training and decision support system (i.e. EXercise Prescription in Everyday practice & Rehabilitative Training (EXPERT) tool), i.e. a stepwise aid on exercise prescription in patients with chronic coronary syndrome (CCS) and/or congestive heart failure (CHF), taking into account concomitant risk factors, physical fitness and comorbidities, in the setting of multidisciplinary rehabilitation, was developed. |
In this paper, the exercise prescriptions for patients with CCS and/or CHF, with concomitant risk factors and comorbidities, formulated for the EXPERT tool are presented, with the aim to assist healthcare professionals/clinicians on how to tailor exercise prescription according to the patient’s phenotype. |
1 Introduction
Exercise training, as part of multidisciplinary rehabilitation, leads to significant improvements in functional capacity, muscle strength and endurance capacity, as well as quality of life in patients with chronic coronary syndrome (CCS) and/or congestive heart failure (CHF), thereby reducing cardiovascular event rates, hospitalisations and/or mortality [1,2,3,4,5,6,7,8,9,10].
Alongside dietary intervention, psychosocial support/counselling, smoking cessation and the prescription of cardioprotective medication, exercise training is classified as a type 1A intervention in the treatment of CCS and/or CHF, and its importance is endorsed by several international position statements and guidelines [11,12,13,14]. In general, it is recommended that patients with CCS and/or CHF perform at least 150 min of continuous low-to-moderate-intensity endurance exercise training per week, ideally spread over 3–5 days per week. An energy expenditure of 1000–2000 kcal per week should be achieved in this way, and endurance exercise training should be complemented by dynamic resistance exercise training two times per week at a moderate intensity [11,12,13,14,15,16].
Despite the availability of international exercise guidelines for the secondary prevention in CCS and CHF [11,12,13,14,15,16], a study from the European Association of Preventive Cardiology (EAPC) EXPERT (Exercise Prescription in Everyday practice & Rehabilitative Training) working group reported a significant inter-clinician variance in exercise prescription for these patients [17]. As an example, for the same patient recovering from coronary artery bypass graft (CABG) surgery with different comorbidities (including obesity, hypertension, type 2 diabetes, CHF) the prescribed exercise volume per programme ranged from 300 up to 9000 peak-effort training minutes, which is an unacceptable variance [17]. In subsequent studies, similar heterogeneous exercise prescriptions were shown for primary care physicians and physiotherapists [18, 19]. This indicates that state-of-the-art exercise prescription for patients with CCS and/or CHF is far from being well established and that clinicians and healthcare professionals need guidance that goes beyond existing guidelines and position statements (i.e. specifically how to tailor exercise interventions based on the patient’s cardiovascular disease (CVD) type, risk profile, physical fitness and medication intake).
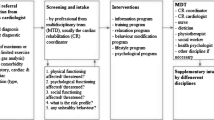
2 Exercise Training as a Component of Multidisciplinary Rehabilitation in CCS and/or CHF
Exercise training, which is the focus of this manuscript, is a component of the multidisciplinary rehabilitation of CCS and/or CHF. Hence, next to the optimisation of exercise prescription to these patients (by physiotherapists/clinical exercise physiologists/cardiac nurses), it is also key to optimise dietary intervention, psychosocial support, smoking cessation, medication prescription and occupational therapy (if needed) by dieticians, psychologists, pharmacists and occupational therapists, under the coordination of a cardiologist trained in cardiovascular rehabilitation (CR). However, this would be beyond the scope of this manuscript.
3 General Approach to Exercise Prescription in Chronic CCS and CHF
Next to anticipated improvements in endurance exercise capacity and muscle strength, exercise interventions should also be tailored to positively affect all modifiable cardiovascular risk factors, as well as to motivate patients to integrate physical activity and training into their lifestyles and to remain physically active throughout their lives. Even though detailed exercise recommendations for different CVD risk factors have been reported [20], tailoring the exercise training programme to each single patient according to their overall CVD risk profile remains difficult as the CVD risk factors and diseases are often considered separately. For example, to optimally reduce adipose tissue mass or arterial blood pressure, or to improve blood lipid profile or glycaemic control, more tailored exercise prescriptions are required [20]. Moreover, the co-existence of comorbidities, the intake of certain medications, physical deconditioning or the presence of abnormalities or adverse events during exercise testing warrant further individualised adjustments of these exercise prescriptions [21].
We therefore speculated that patients with CCS and/or CHF can benefit from a more standardised way of tailoring exercise prescription [21], aiming for greater clinical benefits, maintaining optimal medical safety and improving exercise adherence. As a result, clinicians and healthcare professionals involved in CR can now use a decision support system (EXPERT tool) that, on the basis of the variables provided in this system, suggests how exercise should be individually prescribed [22, 23]. Such an interactive digital decision support system can provide an exercise prescription but still leave the user the opportunity to fine-tune the programme, on the basis of specific patient characteristics or preferences, and the available infrastructure.
The aim of this manuscript was to provide a consensus statement for state-of-the-art exercise prescription and exercise training safety precautions for patients with CCS and/or CHF, as integrated into the EXPERT tool. Different CVD risk factors, comorbidities or devices, the intake of cardioprotective medications, adverse events during exercise testing and physical deconditioning are also taken into account. Finally, simulations of exercise prescriptions for these patients, as provided by the EXPERT tool, will be presented.
4 Methods
4.1 Formulation of Exercise Prescriptions and Construction of EXPERT Tool
Previously, details of the composition and activities of the EXPERT network working group (> 30 members out of > 10 European countries), and how exercise guidelines were collected from the literature, were provided [22]. Also, the development and functioning of the EXPERT tool, definitions for CVD risk factors and goals of CR have already been described in detail [22]. This project is endorsed by the European Association of Preventive Cardiology (EAPC) of the European Society of Cardiology.
In brief, working group members (see author list) were allocated to different topics according to their expertise [CCS, CHF, pacemaker, implantable cardioverter defibrillator (ICD), left-ventricular assist device (LVAD), peripheral arterial disease (PAD), heart transplantation], and were then requested to consult PubMed and/or Web of Science (up to February 2023) to: (1) define the criteria or definitions for the specific conditions, (2) identify the primary goal of exercise training interventions for each disease/condition, (3) provide exercise training recommendations and (4) highlight exercise safety precautions. These recommendations and definitions had to be based on (with decreasing level of evidence) current clinical guidelines and position statements from the European Society of Cardiology (ESC) and/or EAPC, meta-analyses, systematic reviews or randomised controlled trials. If not available, cohort studies, observational studies or expert opinions were also considered. The allocation of these experts to specific steering groups was based on their specific scientific/clinical expertise as indicated by their PubMed track records. All this information was handed over to the project coordinator, who, in collaboration with computer scientists from Hasselt University, developed the EXPERT tool (Fig. 1). This paper is an extension of a previous manuscript paper in which exercise prescriptions in (different combinations of) CVD risk factors were explained in detail [24].
4.2 Classification of Level of Evidence and Grades of Recommendation
To classify the level of evidence and the grade of recommendation for exercise prescription guidelines, the validated SIGN system was used throughout this paper, as shown in Supplementary Table 1 [25].
4.3 Classification of Exercise Training Intensity
Supplementary Table 2 presents the classification of exercise training intensity which is also used in the EXPERT tool [26].
4.4 Limitations of the EXPERT Tool
The EXPERT tool, version of July 2023, is prone to some limitations. The tool applies a classification of exercise training intensity as mentioned in Supplementary Table 2 [based mainly on heart rate (HR)], even though it is well established that the use of the ventilatory threshold (VT) leads to a far more precise determination of exercise intensity (more in line with personal exercise response) and a greater improvement in exercise tolerance [27]. However, the user of this tool can still adjust the target HR if desired (e.g. when the HR at VT2 has been assessed). In addition, the EXPERT tool generates an exercise prescription that ideally matches the CVD risk profile and medical treatment goals. However, it does not take into account the patient’s feasibility and adherence issues (e.g. attractiveness, capabilities, personal goals, fears, etc.) relating to this prescription: these remain to be finally decided or implemented by the user of the tool.
5 Consensus Statements from the EXPERT Network Working Group
5.1 Recommended Infrastructure and Knowledge/Skills of Healthcare Professionals
Patients with CCS and/or CHF are more prone to develop cardiovascular, metabolic or pulmonary complications during physical exercise. Therefore, it is advised that rehabilitation or exercise training facilities are specifically designed and equipped (Table 1), and healthcare professionals are properly educated [28]. Even though intravenous tubing and emergency drugs/solutions may not be administered or used by clinical exercise physiologists or physiotherapists, it is recommended that these materials should be available in peripheral or private practice settings: if a medical doctor is called for an emergency, these materials are then immediately available to that clinician (i.e. clinical exercise physiologists or physiotherapists do not administer or use them themselves). Although CR programmes within hospitals should be coordinated by a cardiologist, the direct assistance and guidance during exercise training to patients (especially in peripheral centres or private practices) is nearly always offered by allied healthcare professionals (such as physiotherapists, cardiac nurses, clinical exercise physiologists). To ensure sufficient patient safety, it is recommended that these allied healthcare professionals have acquired specific clinical competencies, composed of: core knowledge (e.g. clinical exercise physiology, pathology, pharmacology), professional behaviour, communication skills, abilities in supervised exercise training application, assessment/testing skills [e.g. HR and blood pressure (BP) measurement, exercise, functional capacity and muscle strength testing], physical activity planning and exercise prescription, abilities to lead and deliver the supervised exercise session, forward planning, management of emergency procedures (e.g. symptom recognition, care in case of syncope, resuscitation), service planning and management, as well as service evaluation [29]. Moreover, to optimise exercise prescription, cardiopulmonary exercise testing (CPET) is strongly recommended [27]. This will allow personalisation/fine-tuning of the endurance exercise intensity and energy expenditure targets, as well as the assessment of the medical safety of (high-intensity) endurance exercise.
The focus of this paper is on CCS and CHF, since CCS may progress to CHF (and subsequently to heart transplantation). Moreover, as PAD is often co-existent in patients with CCS, this clinical condition is also discussed in this paper. Finally, patients with CHF are often also candidates for implantation of ICD, pacemaker and/or LVAD, so how to prescribe exercise in these cases is described in detail. The proposed exercise prescriptions are summarised in Table 2. Since CR is most often started after hospitalisation due to angina pectoris, acute coronary syndrome or decompensation in CHF, it is important to offer active mobilisation as early as possible (phase 1 CR), given sufficient medical safety [16].
5.2 Phase 1 Cardiovascular Rehabilitation
For definitions of diseases, see Table 3.
Intervention aim: To achieve early mobilisation, given sufficient medical safety. With prolonged bed rest, the associated maladaptation will lead to an excessive rise in HR during orthostatic stress, cardiac atrophy, reduced exercise capacity, decreased blood volume and muscle atrophy. A downward spiral of inactivity and deconditioning might occur.
Exercise training recommendations: Because some patients are so greatly deconditioned, graded programmes should be proposed. Early mobilisation as well as supervised and differentiated exercise training interventions should be provided in a supportive environment. Early mobilisation can be initiated when patients are haemodynamically stable and may include progressive therapeutic activities such as bed mobility exercises, sitting on the edge of the bed, standing, transferring to a chair and ambulation.
Because of a lack of data from randomised controlled trials, the below-mentioned recommendations are expert opinions (level of evidence: 4, grade of recommendations: D). In early mobilisation it is proposed to follow a stepped care plan, including pre-participation screening, what to assess during mobilisation and how to select exercise modalities.
Preparticipation Screening and Parameter Registration During Mobilisation in Phase 1 Cardiovascular Rehabilitation
In the early mobilisation of patients with CCS and/or CHF, it is important to assess the patient’s clinical status to verify the medical safety of such intervention, as well as to register significant parameters during mobilisation. These data are presented in Table 4.
How to Select and Progress Exercise Modalities in Phase 1 Cardiovascular Rehabilitation
Step 1
-
Note obstacles, barriers or challenges related to the patient and environment and plan appropriately (e.g. set up equipment – chairs, transfer belt, mobility aids, length of leads/lines).
-
Determine whether the benefits outweigh the risk (see pre-participation screening).
-
Obtain baseline vital signs (see ‘what to assess during mobilisation’).
Step 2
-
Use proper body mechanics during transfer and allow gradual change from lying to upright position. Encourage circulation exercises, i.e. foot and ankle, knee flexion/extension, before commencing more demanding mobilisation procedures.
-
Monitor closely. Watch for signs of fatigue, pain, dizziness, diaphoresis and intolerance during activity. Frequently ask the patient how he/she feels. Evaluate the patient’s status at each progression to determine whether to continue or stop. Determine the limiting factor of the mobilisation and any undesirable response(s). Use objective outcome measures to monitor progress, e.g. ease of transfer, sitting duration, walking distance, HR, RR, BP, oxygen saturation, Borg ratings of perceived exertion (RPE), and pain.
-
After mobilisation, monitor patients until vital signs have returned to pre-activity level.
Step 3
Intensity and duration of mobility/exercise sessions, and their progression, are further individualised according to response and tolerance:
-
1.
During patient care, e.g. during washing, turns and transfers (i.e. blood pressure, O2 saturation and ECG should stay normal or within normal ranges during such care, and should thus be followed/observed by the healthcare professional accordingly).
-
2.
Consider the inclusion of breathing exercises with or without a respiratory trainer set, stretching exercises, balance/coordination exercises for head, neck and trunk, sitting balance exercises (with sit to stand exercises), arm ergometry, weight bearing/weight shifting exercises (calf muscle strengthening, heel lift), walking in the room/corridor (begin walking practice with appropriate aids, increasing distance and frequency as patient tolerates) and individualised mobilisation prescription.
5.3 Phase 2 Cardiovascular Rehabilitation
5.3.1 Chronic Coronary Syndrome
Intervention aim: To increase the physical fitness and/or reduce/prevent angina pectoris (in case of stable angina pectoris) and thereby to improve prognosis (hospitalisation, cardiovascular re-event rate, mortality) and quality of life.
Exercise training recommendations [14, 16, 27, 30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66]: patients with CCS are generally advised to start with a session duration of 10 min in the initial stage (for up to maximally 2 weeks or ahead of cardiopulmonary exercise testing) at a low to moderate intensity, but gradually increase up to 20 min, if possible to 30–45 min in the improvement stage (from 2 up to 12 weeks) (level of evidence: 1, grade of recommendation: C). In the maintenance stage (after 8–10 weeks of CR) it is advised to complete exercise sessions of 20–45 min or even up to 60 min or more if tolerated (level of evidence: 1, grade of recommendation: C). For some outcomes (e.g. VO2peak, glycaemic control) a slight reduction in minimal exercise session duration (from 30 to 20 min) can be allowed to maintain the achieved benefits, particularly when a higher exercise intensity is applied. This does not, however, apply to every CVD risk factor and should thus be carefully considered and implemented. In the initial and improvement stage patients with CCS are advised to exercise 3–5 days per week (level of evidence: 1, grade of recommendation: B). This exercise frequency can be maintained or could be increased ≥ 5 days per week in the improvement stage (level of evidence: 1, grade of recommendation: B), while in the maintenance stage daily exercise should be promoted (level of evidence: 1, grade of recommendation: C). Patients with CCS are advised to perform endurance exercises at a moderate intensity. In some patients (e.g. patients with preserved physical fitness and absence of exercise-induced hypertension, myocardial ischaemia, or cardiac arrhythmias during exercise testing) high-intensity interval training (HIIT) can be offered as an alternative: HIIT has a similar adherence as moderate-intensity exercise training in patients with CCS [67]. In addition, cumulating evidence is showing that an up-titration of the exercise intensity during CR (as a progression) can elicit significantly greater clinical benefits [68, 69]. Hence, in some patients this can be considered. A minimal programme duration of 12 weeks should be achieved (level of evidence: 1, grade of recommendation: B), although a permanent increment in physical activity is recommended (level of evidence: 1, grade of recommendation: C). Resistance training should routinely be added to endurance exercise provided that patients are clinically stable, and only dynamic resistance training (in contrast to isometric strength training) is applied (see Sect. 5.3.7) (level of evidence: 1, grade of recommendation: C). Dynamic resistance training may be implemented by using specialised training devices in supervised institutions (e.g. prevention and rehabilitation centres) or simple devices like dumbbells, expanders and Therabands. In the initial stage resistance exercise intensity should be set at < 30% of one repetition maximum (1-RM) [RPE Borg ≤ 11], for five to ten repetitions per muscle group (one to three sets per unit), at a frequency of two to three training units per week (level of evidence: 1, grade of recommendation: B). In the first improvement stage, resistance exercise intensity should be set at 30–50% 1-RM, for 10–15 repetitions per muscle group (one to three sets per unit), at a frequency of two to three training units per week (level of evidence: 1, grade of recommendation: B). In the second improvement stage, resistance exercise intensity should be set at 40–60% 1-RM, for 10–15 repetitions per muscle group (one to three sets per unit), at a frequency of two to three training units per week (level of evidence: 1, grade of recommendation: B). In the third improvement stage (in selected patients in good clinical condition, with heavy physical employment, and/or those returning to sports) resistance exercise intensity should be set at 60–80% 1-RM, for eight to ten repetitions per muscle group (one to three sets per unit), at a frequency of two to three training units per week (level of evidence: 1, grade of recommendation: B).
Safety precautions: Safety precautions during exercise training depend on the clinical status of the patients [13, 14, 16]. Therefore, a distinction is made between all patients with CCS, patients after ACS, percutaneous coronary intervention (PCI) or CABG.
-
All patients with CCS: Endurance training intensity has to be set below the ischaemic threshold (if present) as defined by an exercise stress test before starting the training. The training modalities have to be individually adjusted for each patient with respect to clinical cardiovascular conditions (e.g. ischaemia, CHF, atrial fibrillation, PAD; for patients after ACS or after CABG see below), individual non-cardiac limitations [e.g. frailty, concomitant diseases such as chronic obstructive pulmonary disease (COPD), individual fitness] and individual preferences to increase motivation and adherence.
-
Patients after ACS: Participating in a centre-based, structured and multimodal CR programme is strongly advised for all patients after ACS to implement an individually adjusted training programme, to optimise all other aspects of secondary prevention (information and motivation for lifestyle changes, medication and self-control), and to early recognise and prevent potential complications (e.g. recurrent ischaemia, life-threatening cardiac arrhythmia, CHF) (level of evidence: 1, grade of recommendation: B).
-
Patients after CABG: Participating in a centre-based, structured and multimodal CR programme is strongly advised for all patients after CABG to implement an individually adjusted training programme, to optimise all other aspects of secondary prevention, and to prevent and to early recognise and treat potential complications (e.g. recurrent ischaemia due to early bypass dysfunction, arrhythmia, CHF, post-operative infections, wound healing problems, Dressler syndrome) (level of evidence: 1, grade of recommendation: B). In addition, exercise training has to be adjusted according to the time course of wound healing and all other potential complications (level of evidence: 1, grade of recommendation: C), and thoracic shear and pressure stress [e.g. unilateral weight lifting with one arm, excessive bilateral horizontal shoulder flexion/extension (with fixation cushion on chest if performed on a machine)] has to be strictly avoided during the first 6–8 weeks after thoracotomy/sternotomy (level of evidence: 1, grade of recommendation: C).
-
Patients after elective PCI: exercise training may be started immediately after healing of the punctured vessel. This may be as early as 1 day after the intervention (radial artery, level of evidence: 1, grade of recommendation: C), or 1 week after puncture of the femoral artery. However, all patients must be under regular supervision by their local physician (level of evidence: 1, grade of recommendation: C), participation in local cardiovascular prevention centres and/or professionally supervised “heart groups” is strongly advised (level of evidence: 1, grade of recommendation: C), and all public training centres must provide safety equipment including automated external defibrillators.
5.3.2 Congestive Heart Failure
Intervention aim: To improve exercise capacity, or to halt or slow the rate of any further decline in exercise capacity that, at least in part, will optimise long-term outcome and quality of life.
Exercise training recommendations [8, 13, 14, 16, 27, 30, 70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90]: Continuous endurance exercise at a moderate intensity is recommended as the core component of the rehabilitation intervention (level of evidence: 1, grade of recommendation: A). The lower and upper limits of the endurance training intensity in patients with CHF have, however, not been established yet. Aerobic training intensities as low as 40% of peak oxygen uptake (VO2peak) (≈ 25% VO2reserve) have been effective in improving exercise capacity in patients with CHF with a significantly reduced VO2peak (see below for definition). An endurance training intensity approaching the first ventilatory threshold (i.e. around 50–60% VO2peak) has been proposed as a safe lower limit. There is emerging evidence from clinical trials showing that patients with CHF also may be trained at intensities close to the second ventilatory threshold (critical power) without additional risk. Further investigations are needed to determine the optimal training intensity in representative patient populations. If an assessment of (an)aerobic metabolism by cardiopulmonary exercise testing is not available, relative effort intensities in the ‘moderate’ domain have been used: these are expressed as percentage of peak heart rate (%HRpeak) or percentage of heart rate reserve (%HRR), or according to Borg RPE scales. However, the equivalence of %HRR versus %VO2 reserve has been questioned in patients with CHF both on and off beta-blockers, since the exercise intensity domains derived from these parameters often disagree with the first and second ventilatory threshold (which is, in essence, the patient’s personal exercise intensity). High-intensity interval exercise might also be considered in some patients (level of evidence: 1, grade of recommendation: B). Generally, 15–40 min/day exercise sessions are advised, but shorter sessions are preferred at the beginning of the training programme in patients with poor exercise capacity, fatigue and/or recent haemodynamic instability (level of evidence: 1, grade of recommendation: A). The session duration should be progressed according to patients’ tolerance, trying to reach at least a 30-min session duration (level of evidence: 1, grade of recommendation: A). In most studies, a minimum of three sessions per week have been used, and stable patients in New York Heart Association (NYHA) class I–III had three to five sessions per week without adverse effects (level of evidence: 1, grade of recommendation: A). Even in patients with recent haemodynamic instability, starting an individually tailored training programme of three sessions per week has been shown to be safe (level of evidence: 1, grade of recommendation: A). When such an exercise programme is initiated, an attempt should be made to continuously increase the physical activity level (level of evidence: 1, grade of recommendation: A), although it remains difficult to define the minimal programme duration. A lifestyle approach by including common activities into the daily routine (e.g. walking instead of driving, climbing stairs rather than taking the elevator, engaging in active recreational pursuits) also is effective and to be recommended (level of evidence: 1, grade of recommendation: B). Alignment of activity modes with individual preferences and interests is most likely to increase patient’s adherence to sustained activity. Particular types of exercise training (e.g. dancing, yoga) have been shown to be well accepted and beneficial in terms of functional capacity. Exercise modes like running or jogging traditionally are considered to be contraindicated, since they are considered to be potentially very strenuous and often performed without supervision. However, further investigations are needed to clarify this point. In all patients with clinically stable CHF, dynamic resistance training should be included into the training programme as a supplement to endurance exercise training. Training intensity for resistance training is very similar to those for patients with CCS (see Sect. 5.3.1 for more details) and should include 8–10 exercises involving the large muscle groups and should consist of at least one set of 8–12 repetitions per exercise (type of evidence: 1, level of recommendation: A). Furthermore, resistance training should be performed as interval training, and single muscles should be trained step by step. On the basis of expert opinion, in patients with CHF, dynamic resistance training should preferably be guided by experienced exercise therapists or physiotherapists. In the rehabilitation of patients with CHF, and particularly in those with inspiratory muscle weakness [maximal inspiratory muscle strength (PImax) < 70%], inspiratory muscle training (IMT) may be clinically relevant, since the combination of aerobic/resistance/inspiratory training might be the optimal for patients with CHF (level of evidence: 2, grade of recommendation: B) [88]. IMT involves use of respiratory muscle-specific training devices to improve respiratory muscle function, thereby improving respiratory functional status and reducing dyspnoea. Respiratory muscle dysfunction predominantly has been observed in patients with advanced CHF. Modes of IMT usually involve inspiratory muscles, and training is performed at a percentage of PImax. Strength devices are pressure threshold load trainers. Devices targeting endurance include isocapnic hyperpnoea endurance trainers, or incremental inspiratory endurance trainers with computer biofeedback. In patients with CHF with poor exercise capacity, respiratory endurance training has been shown to improve respiratory muscle function, reduce dyspnoea and increase VO2peak as well as quality of life. IMT may thus be used in patients with CHF with low functional capacit When using inspiratory endurance trainers, an intensity of 60% of sustained PImax with a build-up towards a duration of 20–30 min and a frequency of 3 days per week for a minimum of 8–10 weeks has been proposed. If a pressure threshold trainer is used, respiratory training is usually started at 30% of PImax and readjusted every 7–10 days up to 60% of PImax. Training duration again should be 20–30 min/day, three to five times a week and for a minimum of 8 weeks.
Safety precautions: patients with CHF should be informed about the nature of cardiac prodromal symptoms and exercise-related warning symptoms including chest pain or discomfort, abnormal dyspnoea, dizziness or malaise and should seek prompt medical care if such symptoms develop. Regular follow-up depending on severity of CHF and the category of risk is recommended. Intensive isometric exercise such as heavy weight lifting can have a marked pressor effect and should be avoided [91]. Stopping exercise suddenly should be avoided as it may result in a precipitous drop in blood pressure. Patients with exertional dyspnoea, chest discomfort or palpitations need further examination, which includes exercise testing, echocardiography, Holter monitoring or combinations thereof.
5.3.3 Pacemaker, Implantable Cardioverter Defibrillator and Resynchronisation Therapy
Intervention aim: to increase physical fitness, and increase confidence during exercise, to improve mental health, quality of life and prognosis.
Exercise training recommendations [26, 92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120]: As proposed by clinical guidelines, sports with a low cardiovascular demand and no competitive context are allowed for all ICD and pacemaker patients (level of evidence: 3, grade of recommendation: D). Leisure-time recreational physical activities with low-to-moderate dynamic or static demand are also allowed. Recommendations restricting participation in these activities are primarily based on the fear of exercise-induced device or lead complications, lack of data regarding the effectiveness of device therapy in metabolic, autonomic or ischaemic conditions, and potential inappropriate antitachycardic pacing or shock delivery due to misclassification of sinus tachycardia as malignant arrhythmia. However, recent data suggest that these recommendations, particularly in younger, physically active patients (with congenital structural heart disease or channelopathies) and middle-aged patients with arrhythmogenic substrate due to ischaemic or dilated cardiomyopathy might be too restrictive. As yet, in athletes with ICD, competitive sports or strenuous exercise are still contraindicated. However, disqualifying young ICD patients from participating in sports without solid risk evidence might be unnecessary and advice should be based on an individualised risk–benefit decision [26]. The Heart Rhythm Society (HRS), European Heart Rhythm Association (EHRA) and Asia Pacific Heart Rhythm Society (APHRS) guidelines give several disease-specific recommendations to allow participation in competitive activities. Under exercise conditions, appropriate and inappropriate ICD shock delivery and antitachycardic stimulation occur frequently, but clinically relevant complications are rare even in patients with CHF (HF-ACTION trial) [104]. Nevertheless, regular intensive exercise can promote worsening of the course of underlying cardiac diseases [arrhythmogenic right ventricular cardiomyopathy (ARVC), dilated cardiomyopathy (DCM)]. During CR, supervised exercise training in ICD carriers can be safely performed (continuous moderate intensity, with a gradual build-up towards 45–60 min/day, at a frequency of 3–5 days per week) as well as home-based moderate-intensity endurance exercise during the subsequent outpatient period. To achieve an optimal adherence to the prescribed exercise intensity (i.e. within a certain range), monitoring equipment measuring HR behaviour can be considered. Aerobic interval training (i.e. interval training of a significantly lower intensity when compared with HIIT) in ICD patients leads to a significant increase in VO2peak and cycle ergometer workload as well as improvement in endothelial function. Furthermore, regular exercise training has been shown to have an important impact on the psychological stability of ICD patients.
There are no separate evidence-based training recommendations for ICD and pacemaker patients per se. Recommendations for exercise participation should be individualised based on the following modifiers:
-
1.
Underlying heart disease (coronary artery disease, congenital or acquired structural heart disease, channelopathies),
-
2.
Recent supraventricular and ventricular rhythm stability,
-
3.
Indication for device implantation (primary or secondary prevention),
-
4.
LV systolic and diastolic function,
-
5.
Revascularisation status,
-
6.
Settings of the device.
In addition, several limitations regarding the device system have to be considered, such as chronotropic incompetence, inappropriate sensor function for rate-adaptive pacing (under- or overresponsive), sinus tachycardia above the upper tracking limit [dual-chamber and cardiac resynchronisation therapy (CRT) devices], under- and oversensing (pacemaker and ICD), arrhythmias (ventricular or supraventricular extra beats, junctional rhythm, supraventricular and ventricular tachyarrhythmias) and/or changes in atrioventricular (AV) conduction.
Safety precautions: the main target here is to prevent inappropriate therapy delivery under exercise conditions, and maintain system integrity.
For all patients with ICD/pacemakers:
-
Leisure-time sports is only allowed from 6 weeks after implant to facilitate wound healing and lead fixation.
-
Prior to sports participation a stress test under controlled conditions should be performed.
-
Patients should be informed about the signs of arrhythmias, initiating loss of consciousness (dizziness, presyncope) and individual behaviour after therapy delivery.
-
Rigorous arm–shoulder movements (e.g. aggressive ipsilateral arm movements during handball, volleyball, basketball, racket sports, swimming, tennis) should be avoided.
-
Exercise-induced paroxysmal atrial fibrillation should be excluded by prior exercise testing and Holter electrocardiogram (ECG).
-
Sports with bodily contact are contraindicated due to possible device or lead failure (mechanical trauma including haematoma and lead fracture).
-
Electrostimulation in the proximity of the device as an additional training modality is contraindicated, although neuromuscular electrical stimulation to leg muscles has been shown to be a safe modality in ICD patients with advanced CHF.
-
Allow a good warm-up and cool-down during exercise sessions to optimise the chronotropic response.
For patients with antibradycardia pacemakers:
-
Stress testing of chronotropic competence prior to exercising and, if necessary, reprogramming (rate response mode) is recommended.
-
Stress testing for the exclusion of under-/oversensing and programming of the upper synchronisation frequency is recommended.
For patients with a cardiac resynchronisation device (CRT-D, CRT-P):
-
Control of left ventricular pacing threshold, AV delay (effectiveness of biventricular pacing) and effectiveness of rate response under metabolic conditions are recommended.
-
Patients should be informed about signs of progressive CHF due to exercising.
For patients with ICD:
-
Define the maximum exercise HR at least 10–20 beats below ICD intervention frequency (exercise testing and Holter ECG prior to exercise prescription needed).
-
Exercise modalities during which a short loss of consciousness is dangerous (e.g. swimming, diving, climbing) should be avoided in symptomatic patients with secondary preventive implantation indication or in patients with current ICD discharge within the last 3 months.
-
Prophylactic prescription of antiarrhythmic or bradycardic therapy should be contemplated.
-
After appropriate or inappropriate ICD discharge, advanced risk stratification should be performed before restarting exercising.
For athletes with ICD:
-
The desire of the athlete with ICD to continue athletic competition should be secondary to evaluating the suitability for strenuous exercise.
-
All recommendations should be based on an individual risk stratification including underlying genetic or structural heart disease, arrhythmogenic disposition and haemodynamic parameters.
-
Individual programming corresponding to the maximum exercise HR (ICD intervention frequency at least 10–20 beats above exercise HR measured by exercise testing and 24 h Holter monitoring).
-
Start at least 3 months after the ICD implantation or 3 months after the last ICD-treated arrhythmia with class IA sports (level of evidence: 2, grade of recommendation: C) or with higher peak static and dynamic components than class IA depending on the likelihood of appropriate and inappropriate shocks and the potential for device-related trauma in high-impact sports (level of evidence: 2, grade of recommendation: C).
5.3.4 Left-Ventricular Assist Device
Intervention aim: to achieve early mobilisation and improve functional/exercise capacity, and thereby to lead to an improvement in quality of life.
Exercise training recommendations [121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139]: patients with an LVAD should engage in cycle and/or treadmill exercise training at a continuous moderate intensity, with a gradual build-up towards 45–60 min/day, at a frequency of 3–5 days per week, for at least 8–10 weeks (with preferentially a further prolongation in exercise participation to maintain achieved benefits [level of evidence: 4, grade of recommendation: D]). In theory, patients with LVAD are patients with CHF and would thus benefit from resistance exercise training, as well as IMT (see Sect. 5.3.2).
Safety precautions: patients with LVAD are a heterogeneous patient population whose clinical condition can vary widely. Peak exercise capacity often remains limited (e.g. at 50% of prediction), while functional performance is better (e.g. at 80% of prediction). The most common complications are bleeding, thromboembolic events, driveline infections or right-sided CHF. In patients with a newly implanted LVAD system, the initiation of functional or exercise-oriented interventions should primarily be based on individual clinical conditions and disease progression. Before initiating functional and/or exercise therapy, patients must be in a clinically and haemodynamically stable condition. Exclusion criteria for exercise training include: low volume status with orthostatic response, bleeding, signs of systemic infection, ventricular arrhythmias and/or technical LVAD problems. Guidance should be provided by experienced, well-trained therapists who are familiar with the management of the LVAD systems used, general safety aspects and the specific emergency management. Before carrying out functional and exercise measures, the following safety aspects must be strictly observed: checking the batteries, checking the drive length and position, selecting and checking the attachment of the controller and batteries. When performing function and/or exercise-based measures, the following termination criteria must be observed: reduction in pump flow < 3 l/min, inappropriate increase in pump energy demand in watts (watch for thrombus formation), oxygen saturation < 90% (pulse oximeter), and bleeding (e.g. nose bleed). Special care is required in the selection of exercises and the choice of training equipment. When performing functional and sporting activities, rapid changes in body position (e.g. from sitting to standing with rapid blood volume shifts) should always be avoided due to blood volume shifts and the risk of suction events. All activities that carry an increased risk of bleeding should be strictly avoided (e.g. water sports, contact sports, competitive forms of play, etc.). Treadmill walking can also be dangerous to some patients (e.g. those with frailty in whom an increased fall risk may be present, and patients with (short) episodes of dizziness). Visualisation of the output/resistance curve of the device could be necessary in case of symptomatic syncope during exercise, particularly in hot conditions, and/or when the patient sweats profusely. HR monitoring is not valid for exercise prescription: the exercise intensity should be based on workload or Borg RPE.
5.3.5 Heart Transplantation
Intervention aim: to achieve early mobilisation and thereby to lead to an improvement in exercise capacity and life expectancy, and to improve physical performance in daily life activities.
Exercise training recommendations [140,141,142,143,144,145,146,147,148,149,150,151,152,153,154]: It is agreed that these patients should engage in continuous moderate-intensity exercise (at 40–59% VO2peak or 12–13 Borg RPE), for up to 30–60 min per session, at a frequency of minimally 3 days per week, for at least 20 weeks (with preferentially a further prolongation in exercise participation) (level of evidence: 3, grade of recommendation: C), if possible, and with a gradual build-up towards this intensity and volume of exercise. A good evaluation of exercise tolerance is strongly recommended at entry to CR, since a significant proportion of these patients can suffer from severe exercise intolerance (due to skeletal muscle dysfunction (as a result of, at least in part, anti-rejection therapy, corticoid myopathy and from deconditioning as a result of pre-operative physical inactivity). Cardiac reinnervation occurs in a subgroup of heart transplantation recipients, which is associated with higher peak HR and HRR as well as a greater exercise tolerance. Therefore, a regular assessment of the workload–HR relationship is important to re-establish the target HR during exercise training. In addition, resistance exercises should be considered as well due to the high likelihood of muscle weakness and/or wasting (level of evidence: 4, grade of recommendation: D). In this regard, resistance training up to 50–60% of 1-RM, for 10–20 repetitions per series and 3–6 series per large muscle group should be prescribed.
Safety precautions: the heart transplantation patient very often presents at CR with a delayed exercise-onset and exercise-offset HR response due to denervation. As a result, a warm-up period before each session and steady-state aerobic exercise is recommended at the beginning, and a slowed HR recovery after exercise may also occur. This denervation also gradually leads to an emptying of the catecholamine storage in the myocardium, meaning that the transplanted heart is then reliant on the stimulation of circulating catecholamines. Hence, these catecholamine receptors display an increased sensitivity. In an unfavourable case, this can lead to an increased incidence of cardiac arrhythmia. Therefore, particularly in the first weeks of CR, continuous ECG monitoring during exercise could be considered.
5.3.6 Peripheral Artery Disease
For definition, see Table 3.
Intervention aim: to improve pain-free walking distance and thereby lead to improvements in daily life activities and quality of life.
Exercise training recommendations [155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170]: exercise programmes in patients with PAD are of significant benefit compared with placebo or usual care in improving walking time and distance. Supervised exercise training should be performed over 30–45 min, in sessions performed at least three times per week for a minimum of 12 weeks (level of evidence: I, grade of recommendation: A). A regimen of walking to near-maximal pain provides the best improvement (level of evidence: IIa, grade of recommendation: A). Exercise training programmes that use intermittent walking to near-maximal claudication pain performed at a relatively low treadmill grade (i.e. 40% of maximal grade) or a relatively high grade (i.e. 80% of maximal grade) may both be used. However, the volume of exercise provided in terms of energy expenditure should be the same. The higher the intensity of exercise, the greater the cardiovascular responses, the higher the number of motor units recruited in the active muscles, and the greater the metabolic responses (level of evidence: IIa, grade of recommendation: C). The initial workload of the treadmill or speed during outdoor track walking should be set to a speed (and grade) that elicits claudication symptoms within 3–5 min. Patients walk at this workload until they achieve claudication of moderate severity, which is then followed by a brief period of standing or sitting to permit symptoms to resolve. The exercise–rest–exercise pattern should then be repeated throughout the exercise session (level of evidence: IIa, grade of recommendation: A). An improvement in exercise tolerance can be observed within 3 months after initiating the exercise prescription. However, exercise programmes longer than 6 months induced greater improvements in exercise tolerance (level of evidence: IIb, grade of recommendation: C). Training by walking results in greater increases in walking performance, when compared with mixed or alternative activity programmes, including cycling or resistance-type exercise. However, muscle atrophy related to chronically reduced perfusion to skeletal muscles and inactivity in patients with PAD markedly influences exercise performance and patient mobility. Patients with PAD benefit from resistance training as do patients with other forms of CVD, and its use, as tolerated, for general fitness is complementary to walking but not a substitute for it (see below for further details) (level of evidence: IIa, grade of recommendation: C). Adding upper body exercise to walking as is the case with pole striding training (e.g., Nordic walking) significantly improves the clinical indicators of cardiovascular fitness and quality of life, and decreases symptoms of claudication pain during exertion. Dynamic arm exercise training can be followed by similar improvement (pain-free and maximal walking distance) to that seen with treadmill walking exercise training (level of evidence: IIb, grade of recommendation: C). It is recommended to start arm exercise training at one work level (10 W) below the maximal level achieved during baseline arm ergometry test at a rate of 50 cycles per min. Intermittent exercise periods of 2 min can be applied, followed by two minutes of rest, for a total of up to 60 min. After 3 weeks of exercise training, the intensity can be increased to the work level in watts achieved during the baseline arm ergometry test. Thereafter a progressive increase in each cycle by 1 min every 2–3 weeks can be implemented during the training period with decreases in rest periods by 1 min, to a maximal volume of 5 min of exercise and 1 min of rest for 60 min (50 min of exercise). In this regard, moderate-to-high intensity resistance exercise, i.e. 60–80% of 1-RM, is advised. Monthly reassessments of muscle strength, and routine monitoring of HR and blood pressure (BP), are advised. Each exercise session, three sets (8–12 repetitions with 1–2 min rest intervals per set) of resistance exercise should be completed. Whole-body progressive resistance training incorporating six to eight exercises including the primary muscle groups involved in walking (e.g. gastrocnemius, tibialis anterior, quadriceps, hamstrings and gluteals) should then be targeted.
Safety precautions: although the majority of exercise trials have focussed on the efficacy of walking to pain as treatment, there is some evidence that inflammation accompanying the onset of claudication may theoretically contribute to further vascular endothelium damage, and thus not be optimal. Therefore, there is a compelling rationale for further definitive, robust trials of alternative/complementary exercise prescriptions and guidelines for PAD. It is important to pay attention to any poorly healing or non-healing wounds of the legs or feet, since they constitute a contraindication to exercise training due to the potential aggravation of the wounds during walking by reason of mechanical irritation. Because of the frequently concomitant clinical or occult coronary artery disease, it is advised to perform treadmill or bicycle exercise testing with 12-lead ECG monitoring before starting an exercise training program. The test should be repeated after improvement of symptoms and consideration given to alternative stress tests if exercise capacity is limited by claudication symptoms.
5.3.7 Resistance Training for Cardiovascular Disease: Safety Aspects
Although endurance exercise training is often the primary element of rehabilitation programmes to many patients with CCS or CHF, resistance training is considered as an important addition. This paragraph elaborates in greater detail how resistance training can be applied safely in these clinical conditions [169, 171,172,173,174,175,176,177,178,179,180,181,182].
Performing resistance exercise can lead to inappropriate BP increase. However, by taking into account the factors that cause a rise in BP under exercise conditions, this can be avoided. While static (isometric) loads are associated with a significant increase in BP, low to moderately dosed dynamic resistance exercises only result in a modest increase in BP, comparable to that seen in moderate-intensity endurance training. In addition to the exercise mode (isometric/isotonic component), the BP response depends on exercise intensity, (in relation to the individual maximum strength), the amount of the muscle mass used, the number and speed/rhythm of repetitions, the duration of loading as well as the number of sets and the resting period between sets. The Valsalva manoeuvre (a forced expiration invoked against the closed glottis) during resistance exercise causes a more pronounced rise in BP. Moreover, carrying out the Valsalva manoeuvre leads to an increase in intrathoracic pressure, and in turn to a decreased venous return and a potential reduction in cardiac output. The physiological response includes an increase in HR to maintain cardiac output and peripheral vasoconstriction to maintain BP, which otherwise may decrease with decreasing cardiac output. Furthermore, the termination of the compressed breathing causes a dramatic increase in venous return and subsequently an increase in cardiac output being forced through a constricted arterial vascular system. The resulting dramatic rise and drop in BP can limit myocardial oxygen delivery resulting in potentially dangerous arrhythmias and/or reduced perfusion of the coronary arteries leading to ischaemia. Therefore, the Valsalva manoeuvre should be avoided by exhaling during the contraction or exertion phase of the lift and inhaling during the relaxation phase. The resistance exercises should be performed in a rhythmical manner at a moderate controlled speed through a full range of motion, avoid a continuous, tensed-up grip, and if symptoms occur (vertigo, arrhythmias, dyspnoea, angina pectoris), training should be discontinued immediately. Additional special directions for the execution of resistance training should be given: use standardised exercises for mobilisation and stretching for warming up, preparation, and cooling down, and emphasise familiarisation with learning how the movement is performed correctly. Moreover, the assessment of muscle strength should be performed as soon as possible after a sufficiently thorough familiarisation. If exercise is being performed more than 3 days a week, 1-day breaks between training sessions of the same muscle groups should be planned.
5.3.8 Medications
Beta-blockers, alpha-blockers, vasodilators, simvastatin, sulfonylurea, meglitinide and exogenous insulin administration may all affect the acute response to exercise, for which modifications in exercise prescription could be proposed, as explained in a previous paper by this working group [24]. In patients with CCS or CHF taking anticoagulants, sports or exercise with direct bodily contact or prone to trauma should be avoided.
5.3.9 Adverse Events During Exercise Testing
The safety of exercise for patients with CVD is strongly related to having an exercise prescription based on an exercise test. In patients after ACS the incidence of life-threatening adverse events was zero in 277,721 patient-hours of CR exercise when based on an exercise test prescription, whereas two such adverse events occurred during 105,375 patient-hours when exercise training was not based on an exercise test [183]. Patients with CCS and those with CHF are more prone to the development of myocardial ischaemia. As myocardial ischaemia may increase the likelihood of cardiac arrhythmias in CCS and CHF (e.g. atrial fibrillation or ventricular tachyarrhythmia) and/or lead to a reduced cardiac contractility (e.g. reduced stroke volume), such possibilities should be ruled out by cardiopulmonary exercise testing. If such myocardial ischaemia with cardiac arrhythmias is noticed, it is advised to terminate the exercise test and postpone exercise training until clinically effective medical treatment is initiated. In addition, the BP response during exercise should be monitored closely to rule out exercise hypertension [e.g. if systolic blood pressure (SBP) rises > 200 mmHg at a workload of 100 W] [26] or a decrease in SBP during exercise.
5.3.10 Physical Fitness
It is generally recommended to start exercise training at a rather low exercise intensity, and to build it up to the originally recommended exercise intensity, in patients with a VO2peak < 75% of the predicted normal value, as explained in a previous paper by this working group [24].
6 Examples of Exercise Prescriptions for Patients with CCS and Those with CHF Using the EXPERT Tool
To demonstrate how the EXPERT tool [22, 23] proposes exercise prescriptions in patients with CCS and/or CHF with different combinations of CVD risk factors, three patient cases with solutions are presented in Table 5 (exercise safety precautions are not shown). The EXPERT tool always starts with the general recommendation for endurance exercise prescription in (secondary) prevention of CVD (150 min low-to-moderate-intensity endurance exercise training per week, spread over 3–5 days, expending 1000–2000 kcal, for a duration of at least 12 weeks) [16]. However, the tool further adjusts exercise prescription based on the input of further variables.
Case 1: A 75-year-old, slightly underweight [body mass index (BMI) 19.04 kg/m2], male is referred to multidisciplinary rehabilitation for CABG. In this patient, the primary aim is to improve physical fitness. It is therefore important to offer a sufficient exercise volume (> 150 min per week), to select a sufficient exercise intensity (moderate intensity, HR 95–105 bpm) and whole-body exercises (walking, stepping, rowing, cross-training), and to offer additional resistance exercise training (i.e. because of the low BMI and having undergone CABG, a lowered skeletal muscle mass may be present) [184]. However, the patient displays a significantly lowered physical fitness (e.g. VO2peak at 67% of predicted value). Therefore, it is advised to start at a lower endurance exercise intensity and build up towards moderate-intensity endurance training within a few weeks. The preparticipation screening also reveals arterial hypertension. As a result, reducing BP becomes an important additional rehabilitation goal. For these reasons, a build-up towards at least moderate-intensity endurance training, and with a sufficient exercise session duration (30–45 min) is warranted. Moreover, as the patient takes metformin, he should be considered to have type 2 diabetes. With these CVD risk factors, in theory, resistance exercise training (at least 21 sets) (leading to greater reductions in glycated haemoglobin (HbA1c)) is advised. However, the patient must be monitored carefully, taking into account potential issues that could lead to increased exercise risk (e.g. postoperative anaemia, sarcopenia or cachexia, BP medication).
Case 2: a 68-year-old obese male with preserved physical fitness is referred for multidisciplinary rehabilitation after PCI. As a result, the general recommendation for endurance exercise prescription after PCI (150 min low-to-moderate intensity endurance exercise training per week, spread over 3–5 days, expending 1000–2000 kcal, for a duration of at least 12 weeks, with the addition of resistance exercise training) is applicable. Because of the obese state (BMI 30.77 kg/m2), a significant energy expenditure by exercise training is warranted (> 1500 kcal per week) by offering whole-body exercises (e.g. walking, rowing, stepping, etc.) and by increasing the frequency and duration of the exercise sessions. A prolongation of the rehabilitation programme is then also indicated, as well as an appropriate dietary intervention.
Case 3: a 72-year-old female with preserved physical fitness is referred to multidisciplinary rehabilitation for heart failure with reduced ejection fraction (HFrEF) and CRT-P. As a result, the general recommendation for endurance exercise prescription in CHF (150 min low-to-moderate-intensity endurance exercise training per week, spread over 3–5 days, achieving 1000–2000 kcal, for a duration of at least 12 weeks, with the addition of resistance exercise training) is applicable. However, if the patient takes statins, and should thus be considered to experience dyslipidaemia, a total weekly energy expenditure > 900 kcal is desired. Finally, IMT should also be added in the exercise prescription. All precautions regarding patients with CRT-P should be considered.
7 Conclusion
In this manuscript, state-of-the-art exercise prescription, based on a robust review of evidence, has been proposed for patients with CCS and/or CHF, and associated co-morbidities. With the EXPERT tool, clinicians and healthcare professionals are assisted in the selection of proper exercise training modalities in these populations.
References
Rauch B, Davos CH, Doherty P, et al. The prognostic effect of cardiac rehabilitation in the era of acute revascularisation and statin therapy: a systematic review and meta-analysis of randomized and non-randomized studies—The Cardiac Rehabilitation Outcome Study (CROS). Eur J Prev Cardiol. 2016;23:1914–39.
Lewinter C, Doherty P, Gale CP, et al. Exercise-based cardiac rehabilitation in patients with heart failure: a meta-analysis of randomised controlled trials between 1999 and 2013. Eur J Prev Cardiol. 2015;22:1504–12.
Sibilitz KL, Berg SK, Tang LH et al. Exercise-based cardiac rehabilitation for adults after heart valve surgery. Cochrane Database Syst Rev 2016; 3: CD010876.
Lane R, Ellis B, Watson L, Leng GC. Exercise for intermittent claudication. Cochrane Database Syst Rev 2014; 7: CD000990.
Long L., Anderson L., Dewhirst AM, He J, Bridges C, Gandhi M, Taylor RS. Exercise-based cardiac rehabilitation for adults with stable angina. Cochrane Database Syst. Rev. 2018;2:CD012786.
Taylor RS, Walker S, Smart NA, et al. Impact of exercise rehabilitation on exercise capacity and quality-of-life in heart failure: individual participant meta-analysis. J Am Coll Cardiol. 2019;73:1430–3.
Long, L. Mordi IR, Bridges C et al. Exercise-based cardiac rehabilitation for adults with heart failure. Cochrane Database Syst Rev. 2019;1:CD003331.
Bjarnason-Wehrens B, Nebel R, Jensen K, et al. Exercise-based cardiac rehabilitation in patients with reduced left ventricular ejection fraction: The Cardiac Rehabilitation Outcome Study in Heart Failure (CROS-HF): a systematic review and meta-analysis. Eur J Prev Cardiol. 2020;27:929–52.
Ciani O, Piepoli M, Smart N, et al. Validation of exercise capacity as a surrogate endpoint in exercise-based rehabilitation for heart failure: a meta-analysis of randomized controlled trials. JACC Heart Fail. 2018;6:596–604.
Uddin J, Zwisler AD, Lewinter C, et al. Predictors of exercise capacity following exercise-based rehabilitation in patients with coronary heart disease and heart failure: A meta-regression analysis. Eur J Prev Cardiol. 2016;23:683–93.
Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. Eur J Prev Cardiol. 2016;23:NP1-96.
Eckel RH,Jakicic JM, Ard JD, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2960–84.
Rauch B, Salzwedel A, Bjarnason-Wehrens B, et al. Cardiac rehabilitation in German speaking countries of Europe—evidence-based guidelines from Germany, Austria and Switzerland LLKardReha-DACH-Part 1. J Clin Med. 2021;10:2192.
Schwaab B, Bjarnason-Wehrens B, Meng K, et al. Cardiac rehabilitation in German speaking countries of Europe—evidence-based guidelines from Germany, Austria and Switzerland LLKardReha-DACH-Part 2. J Clin Med. 2021;10:3071.
Corra U, Piepoli MF, Carre F, et al. Secondary prevention through cardiac rehabilitation: physical activity counselling and exercise training: Key components of the position paper from the cardiac rehabilitation section of the European Association of Cardiovascular Prevention and Rehabilitation. Eur Heart J. 2010;31:1967–74.
Ambrosetti M, Abreu A, Corrà U, et al. Secondary prevention through comprehensive cardiovascular rehabilitation: from knowledge to implementation. 2020 update. A position paper from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2020:2047487320913379. https://doi.org/10.1177/2047487320913379. (epub ahead of print).
Hansen D, Rovelo Ruiz G, Doherty P, et al. Do clinicians prescribe exercise similarly in patients with different cardiovascular diseases? Findings from the EAPC EXPERT working group survey. Eur J Prev Cardiol. 2018;25:682–91.
Foccardi G, Hansen D, Quinto G, et al. How do General Practitioners assess physical activity and prescribe exercise in patients with different cardiovascular diseases? An Italian pilot study. Eur J Prev Cardiol. 2020:2047487320925221. https://doi.org/10.1177/2047487320925221. (epub ahead of print).
Marinus N, Cornelissen V, Meesen R, Coninx K, Hansen D. Are exercise prescriptions for patients with cardiovascular disease, made by physiotherapists, in agreement with European recommendations? Eur J Cardiovasc Nurs. 2023;13:zvad065. https://doi.org/10.1093/eurjcn/zvad065. (epub ahead of print).
Vanhees L, Geladas N, Hansen D, et al. Importance of characteristics and modalities of physical activity and exercise in the management of cardiovascular health in individuals with cardiovascular risk factors. Recommendations from the European Association for Cardiovascular Prevention and Rehabilitation (Part II). Eur J Prev Cardiol. 2012;19:1005–33.
Hansen D, Piepoli MF, Doehner W. The importance of rehabilitation in the secondary prevention of cardiovascular disease. Eur J Prev Cardiol. 2019;26:273–6.
Hansen D, Dendale P, Coninx K, et al. The European Association of Preventive Cardiology Exercise Prescription in Everyday Practice and Rehabilitative Training (EXPERT) tool: a digital training and decision support system for optimized exercise prescription in cardiovascular disease. Concept, definitions and construction methodology. Eur J Prev Cardiol. 2017; 24: 1017–31.
Hansen D, Dendale P, Coninx K. The EAPC EXPERT tool. Eur Heart J. 2017;38:2318–20.
Hansen D, Niebauer N, Cornelissen V, et al. Exercise prescription in patients with different combinations of cardiovascular disease risk factors: a consensus statement from the EXPERT working group. Sports Med. 2018;48:1781–97.
Harbour R, Miller J. A new system for grading recommendations in evidence based guidelines. BMJ. 2001;323:334–6.
Pelliccia A, Sharma S, Gati S, et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J. 2021;42:17–96.
Hansen D, Abreu A, Ambrosetti M, et al. Exercise intensity assessment and prescription in cardiovascular rehabilitation and beyond: why and how: a position statement from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2022;29:230–45.
Myers J, Arena R, Franklin B, et al; American Heart Association Committee on Exercise, Cardiac Rehabilitation, and Prevention of the Council on Clinical Cardiology, the Council on Nutrition, Physical Activity, and Metabolism, and the Council on Cardiovascular Nursing. Recommendations for clinical exercise laboratories: a scientific statement from the American Heart Association. Circulation. 2009;119:3144–61.
Abreu A, Frederix I, Dendale P, et al. Standardization and quality improvement of secondary prevention through cardiovascular rehabilitation programmes in Europe: the avenue towards EAPC accreditation programme: a position statement of the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology (EAPC). Eur J Prev Cardiol. 2020;1:2047487320924912. https://doi.org/10.1177/2047487320924912.
Bjarnason-Wehrens B, Schwaab B, Reiss N, et al. Resistance training in patients with coronary artery disease, heart failure, and valvular heart disease: a review with special emphasis on old age, frailty, and physical limitations. J Cardiopulm Rehabil Prev. 2022;42:304–15.
Banz WJ, Maher AM, Thompson WG, Bassett DR, Moore W, Ashraf M, et al. Effects of resistance versus aerobic training on coronary artery disease risk factors. Exp Biol Med. 2003;228:434–40.
Berkhuysen MA, Nieuwland W, Buunk BP, Sanderman R, Viersma JW, Rispens P. Effect of high- versus low-frequency exercise training in multidisciplinary cardiac rehabilitation on health-related quality of life. J Cardiopulm Rehabil. 1999;19:22–8.
Bjarnason-Wehrens B, Mayer-Berger W, Meister ER, Baum K, Hambrecht R, Gielen S. Recommendations for resistance exercise in cardiac rehabilitation. Recommendations of the German Federation for Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil 2004; 11: 352–361.
Blair SN, Kohl HW 3rd, Barlow CE, Paffenbarger RS Jr, Gibbons LW and Macera CA. Changes in physical fitness and all-cause mortality. A prospective study of healthy and unhealthy men. JAMA 1995; 273:1093–1098.
Brooks N, Layne JE, Gordon PL, Roubenoff R, Nelson ME, Castaneda-Sceppa C. Strength training improves muscle quality and insulin sensitivity in Hispanic older adults with type 2 diabetes. Int J Med Sci. 2007;4:19–27.
Castaneda C, Layne JE, Munoz-Orians L, Gordon PL, Walsmith J, Foldvari M, et al. A randomized controlled trial of resistance exercise training to improve glycemic control in older adults with type 2 diabetes. Diabetes Care. 2002;25:2335–41.
Cornish AK, Broadbent S, Cheema BS. Interval training for patients with coronary artery disease: a systematic review. Eur J Appl Physiol. 2011;11(4):579–89.
Dunbar CC, Robertson RJ, Baun R, Blandin MF, Metz K, Burdett R, et al. The validity of regulating exercise intensity by ratings of perceived exertion. Med Sci Sports Exerc. 1992;24:94–9.
Farsidfar F, Kasikcioglu E, Oflaz H, Kasikcioglu D, Meric M, Umman S. Effects of different intensities of acute exercise on flow-mediated dilatation in patients with coronary artery disease. Int J Cardiol. 2008;124:372–4.
Goel K, Lennon RJ, Tilbury RT, et al. Impact of cardiac rehabilitation on mortality and cardiovascular events after percutaneous coronary intervention in the community. Circulation. 2011;123:2344–52.
Hambrecht R, Niebauer J, Marburger C, Grunze M, Kalberer B, Hauer K, et al. Various intensities of leisure time physical activity in patients with coronary artery disease: effects on cardiorespiratory fitness and progression of coronary atherosclerotic lesions. J Am Coll Cardiol. 1993;22:468–77.
Hammill BG, Curtis LH, Schulman KA, Whellan DJ. Relationship between cardiac rehabilitation and long-term risks of death and myocardial infarction among elderly Medicare beneficiaries. Circulation. 2010;121:63–70.
Dibben G, Faulkner J, Oldridge N, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2021;11(11):CD001800.
Kallings LV, Leijon M, Hellénius ML, Ståhle A. Physical activity on prescription in primary health care: a follow-up of physical activity level and quality of life. Scand J Med Sci Sports. 2008;18:154–61.
Kang J, Chaloupka EC, Biren GB, Mastrangelo MA, Hoffman JR. Regulating intensity using perceived exertion: effect of exercise duration. Eur J Appl Physiol. 2009;105:445–51.
Karlsdottir AE, Foster C, Porcari JP, Palmer-McLean K, White-Kube R, Backes RC. Hemodynamic responses during aerobic and resistance exercise. J Cardiopulm Rehabil. 2002;22:170–7.
Karmisholt K and Gotzsche PC. Physical activity for secondary prevention of disease. Systematic reviews of randomized trials. Dan Med Bull 2005;52:90–94.
Latham NK, Bennett DA, Stretton CM, Anderson CS. Systematic review of progressive resistance strength training in older adults. J Gerontol A Biol Sci Med Sci. 2004;59:48–61.
Munk PS, Staal EM, Butt N, Isaksen K, Larsen AI. High-intensity interval training may reduce in-stent restenosis following percutaneous coronary intervention with stent implantation: a randomized controlled trial evaluating the relationship to endothelial function and inflammation. Am Heart J. 2009;158:734–41.
Narici MV, Reeves ND, Morse CI, Maganaris CN. Muscular adaptions to resistance exercise in the elderly. J Musculoskelet Neuronal Interact. 2004;4:161–4.
Niebauer J, Hambrecht R, Velich T, Hauer K, Marburger C, Kalberer B, et al. Attenuated progression of coronary artery disease after 6 years of multifactorial risk intervention: role of physical exercise. Circulation. 1997;96:2534–41.
Nieuwland W, Berkhuysen MA, van Veldhuisen DJ, Brügemann J, Landsman MLJ, van Sonderen E, et al. Differential effects of high-frequency versus low-frequency exercise training in rehabilitation of patients with coronary artery disease. J Am Coll Cardiol. 2000;36:202–7.
Pack QR, Goel K, Lahr BD, et al. Participation in cardiac rehabilitation and survival after coronary artery bypass graft surgery: a community based study. Circulation. 2013;128:590–7.
Perk J, Backer GD, Gohlke H, Graham I, Zeljko R, Verschuren M, Albus C, Benlian P, Boysen G, Cifkova R, Deaton C, Ebrahim S, Fisher M, Germano G, Hobbs R, Hoes A, Karadeniz S, Mezzani A, Prescott E, Ryden L, Scherer M, Syvänne M, Scholte Op Reimer WJM, Vrints C, Wood D, Zaamorano JL, Zannad F. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012) EHJ; 2012.
Rauch B, Riemer T, Schwaab B, et al. Short-term comprehensive cardiac rehabilitation after AMI is associated with reduced 1-year mortality: results from the OMEGA study. Eur J Prev Cardiol. 2013. https://doi.org/10.1177/2047487313486040.
Soga Y, Yokoi H, Ando K, Shirai S, Sakai K, Kondo K, et al. Safety of early exercise training after elective coronary stenting in patients with stable coronary artery disease. Eur J Cardiovasc Prev Rehabil. 2010;17:230–4.
Suaya JA, Stason WB, Ades PA, et al. Cardiac rehabilitation and survival in older coronary patients. J Am Coll Cardiol. 2009;54:25–33.
Taylor RS, Brown A, Ebrahim S, Joliffe J, Noorani H, Rees K, Skidmre B, Stone JA, Thompson DR, Oldridge N. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004;116:682–92.
Tokmakidis SP, Volaklis KA. Training and detraining effects of a combined-strength and aerobic exercise programme on blood lipids in patients with coronary artery disease. J Cardiopulm Rehabil. 2003;23:193–200.
Vanhees L, Stevens A, Schepers D, Defoor J, Rademakers F, Fagard R. Determinants of the effects of physical training and of the complications requiring resuscitation during exercise in patients with cardiovascular disease. Eur J Cardiovasc Prev Rehabil. 2004;11:304–12.
Vanhees L, Stevens A. Exercise intensity: a matter of measuring or of talking? J Cardiopulm Rehabil. 2006;26(2):78–9.
Vanhees L, Rauch B, Piepoli M, van Buuren F, Takken T, Börjesson M, Bjarnason-Wehrens B, Doherty P, Dugmore D, Halle M (on behalf of the writing group of the EACPR). Importance of characteristics and modalities of physical activity and exercise in the management of cardiovascular disease (Part III). Eur J Prev Cardiol. 2013.
Vona M, Codeluppi GM, Iannino T, Ferrari E, Bogousslavsky J, von Segesser LK. Effects of different types of exercise training followed by detraining on endothelium-dependent dilatation in patients with recent myocardial infarction. Circulation. 2009;119:1601–8.
West RR, Jones DA, Henderson AH. Rehabilitation after myocardial infarction trial (RAMIT): multi-centre randomised controlled trial of comprehensive cardiac rehabilitation in patients following acute myocardial infarction. Heart. 2012;98:637–44.
Williams MA, Haskell WL, Ades PA, et al. Resistance exercise in individuals with and without cardiovascular disease: 2007 update: a scientific statement from the American Heart Association Council on Clinical Cardiology and Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2007;116:572–84.
Wisløff U, Støylen A, Loennechen JP, et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation. 2007;115:3086–94.
Taylor JL, Holland DJ, Keating SE, Bonikowske AR, Coombes JS. Adherence to high intensity interval training in cardiac rehabilitation: a review and recommendation. J Cardiopulm Rehabil Prev. 2021;41:61–77.
Sabbahi A, Canada JM, Babu AS, et al. Exercise training in cardiac rehabilitation: Setting the right intensity for optimal benefit. Prog Cardiovasc Dis. 2022;70:58–65.
Taylor JL, Bonikowske AR, Olson TP. Optimizing outcomes in cardiac rehabilitation: the importance of exercise intensity. Front Cardiovasc Med. 2021;8: 734278.
Austin J, Williams R, Ross L, et al. Randomised controlled trial of cardiac rehabilitation in elderly patients with heart failure. Eur J Heart Fail. 2005;7:411–7.
Belardinelli R, Georgiou D, Scocco V, et al. Low intensity exercise training in patients with chronic heart failure. J Am Coll Cardiol. 1995;26:975–82.
Belardinelli R, Georgiou D, Cianci G, et al. Exercise training improves left ventricular diastolic filling in patients with dilated cardiomyopathy. Clinical and prognostic implications. Circulation. 1995;91:2775–84.
Bjarnason-Wehrens B, Mayer-Berger W, Meister ER, et al. Recommendations for resistance exercise in cardiac rehabilitation. Recommendations of the German Federation for Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil. 2004;11:352–61.
Carvalho VO, Mezzani A. Aerobic exercise training intensity in patients with chronic heart failure: principles of assessment and prescription. Eur J Cardiovasc Prev Rehab. 2011;18:5–14.
Conraads VM, Beckers P. Exercise training in heart failure: practical guidance. Heart. 2010;96:2025–31.
Davies EJ, Moxham T, Rees K, et al. Exercise based rehabilitation for heart failure. Cochrane Database Syst Rev. 2010;(4):CD003331.
Demopoulos L, Bijou R, Fergus I, et al. Exercise training in patients with severe congestive heart failure: enhancing peak aerobic capacity while minimizing the increase in ventricular wall stress. J Am Coll Cardiol. 1997;29:597–603.
Dubach P, Myers J, Dziekan G, et al. Effect of high intensity exercise training on central hemodynamic responses to exercise in men with reduced left ventricular function. J Am Coll Cardiol. 1997;29:1591–8.
Laoutaris ID, Dritsas A, Brown MD, et al. Immune response to inspiratory muscle training in patients with chronic heart failure. Eur J Cardiovasc Prev Rehabil. 2007;14:679–85.
Mezzani A, Agostoni P, Cohen-Solal A, et al. Standards for the use of cardiopulmonary exercise testing for the functional evaluation of cardiac patients: a report from the Exercise Physiology Section of the European Association for Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil. 2009;16:249–67.
Mezzani A, Corrà U, Giordano A, et al. The upper intensity limit for prolonged aerobic exercise in chronic heart failure. Med Sci Sports Exerc. 2010;42:633–9.
O’Connor CM, Whellan DJMD, Lee KL, et al. Efficacy and safety of exercise training in patients with chronic heart failure. HF-ACTION randomized controlled trial. JAMA. 2009;301:1439–50.
Piepoli MF, Davos C, Francis DP, et al. Exercise training meta-analysis of trials in patients with chronic heart failure (ExTraMATCH). BMJ. 2004;328:189–93.
Piepoli MF, Corrà U, Benzer W, et al. Secondary prevention through cardiac rehabilitation: from knowledge to implementation. A position paper from the Cardiac Rehabilitation Section of the European Association of Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil. 2010;17:1–17.
Piepoli MF, Conraads V, Corrà U, et al. Exercise training in heart failure: from theory to practice. A consensus document of the Heart Failure Association and the European Association for Cardiovascular Prevention and Rehabilitation. Eur J Heart Fail. 2011;13:347–57.
Rees K, Taylor RRS, Singh S, et al. Exercise based rehabilitation for heart failure. Cochrane Database of Systematic Reviews, Issue 4, 2009. Copyright © 2009 The Cochrane Collaboration. Published, John Wiley & Sons, Ltd. https://doi.org/10.1002/14651858. CD003331.pub2.
Ellingsen Ø, Halle M, Conraads V, et al. High-intensity interval training in patients with heart failure with reduced ejection fraction. Circulation. 2017;135:839–49.
Laoutaris ID, Piotrowicz E, Kallistratos MS, ARISTOS-HF trial, et al. Combined aerobic/resistance/inspiratory muscle training as the “optimum” exercise programme for patients with chronic heart failure: ARISTOS-HF randomized clinical trial. Eur J Prev Cardiol. 2021;28:1626–35.
Ambrosy AP, Cerbin LP, DeVore AD, et al. Aerobic exercise training and general health status in ambulatory heart failure patients with a reduced ejection fraction—findings from the Heart Failure and A Controlled Trial Investigating Outcomes of Exercise Training (HF-ACTION) trial. Am Heart J. 2017;186:130–8.
Delgado B, Novo A, Lopes I, et al. The effects of early rehabilitation on functional exercise tolerance in decompensated heart failure patients: Results of a multicenter randomized controlled trial (ERIC-HF study). Clin Rehabil. 2022;36:813–21.
Wan HY, Weavil JC, Thurston TS, et al. The exercise pressor reflex and chemoreflex interaction: cardiovascular implications for the exercising human. J Physiol. 2020;598:2311–21.
Pelliccia A, Fagard R, Bjørnstad HH, et al. Study Group of Sports Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology; Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology Recommendations for competitive sports participation in athletes with cardiovascular disease. A consensus document from the Study Group of Sports Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur Heart J. 2005;26:1422–45.
Heidbüchel H, Corrado D, Biffi A, Hoffmann E, Panhuyzen-Goedkoop N, Hoogsteen J, Delise P, Hoff PI, Pelliccia A, et al. Recommendations for participation in leisure-time physical activity and competitive sports of patients with arrhythmias and potentially arrhythmogenic conditions Part II: ventricular arrhythmias, channelopathies and implantable defibrillators. Eur J Cardiovasc Prev Rehabil. 2006;13:676–86.
Priori SG, Wilde AA, Horie M, et al. HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes: document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013. Heart Rhythm. 2013;10:1932–63.
Zipes DP, Link MS, Ackerman MJ, et al; American Heart Association Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology, Council on Cardiovascular Disease in the Young, Council on Cardiovascular and Stroke Nursing, Council on Functional Genomics and Translational Biology, and the American College of Cardiology. Eligibility and Disqualification Recommendations for Competitive Athletes with Cardiovascular Abnormalities: Task Force 9: Arrhythmias and Conduction Defects: A Scientific Statement from the American Heart Association and American College of Cardiology. Circulation. 2015;132:e315–25.
Vollmann D, Lüthje L, Zabel M. Inappropriate implantable cardioverter-defibrillator therapy during exercise: what is the mechanism? Heart Rhythm. 2009;6:718–9.
Daubert JP, Zareba W, Cannom DS, et al. Inappropriate implantable cardioverter-defibrillator shocks in MADIT II: frequency, mechanisms, predictors, and survival impact. J Am Coll Cardiol. 2008;51:1357–65.
Heidbüchel H. Implantable cardioverter defibrillator therapy in athletes. Cardiol Clin. 2007;25:467–82.
Heidbuchel H, Carré F. Exercise and competitive sports in patients with an implantable cardioverter-defibrillator. Eur Heart J. 2014;35:3097–102.
Lampert R, Olshansky B, Heidbuchel H, et al. Safety of sports for athletes with implantable cardioverter-defibrillators: results of a prospective, multinational registry. Circulation. 2013;127:2021–30.
Ponamgi SP, DeSimone CV, Ackerman MJ. Athletes with implantable cardioverter defibrillators. Clin Sports Med. 2015;34:473–87.
Prutkin JM, Ackerman MJ, Drezner JA. Athletes with implantable cardioverter defibrillators: can they return to competitive sports? Heart. 2016;102:93–4.
Lampert R, Cannom D, Olshansky B. Safety of sports participation in patients with implantable cardioverter defibrillators: a survey of heart rhythm society members. J Cardiovasc Electrophysiol. 2006;17:11–5.
Piccini JP, Hellkamp AS, Whellan DJ, et al. Exercise training and implantable cardioverter-defibrillator shocks in patients with heart failure: results from HF-ACTION (Heart Failure and A Controlled Trial Investigating Outcomes of Exercise TraiNing). JACC Heart Fail. 2013;1:142–8.
James CA, Bhonsale A, Tichnell C, et al. Exercise increases age-related penetrance and arrhythmic risk in arrhythmogenic right ventricular dysplasia/cardiomyopathy-associated desmosomal mutation carriers. J Am Coll Cardiol. 2013;62:1290–7.
Fitchet A, Doherty PJ, Bundy C, et al. Comprehensive cardiac rehabilitation programme for implantable cardioverter-defibrillator patients: a randomised controlled trial. Heart. 2003;89:155–60.
Haennel RG. Exercise rehabilitation for chronic heart failure patienfambrots with cardiac device implants. Cardiopulm Phys Ther J. 2012;23:23–8.
Fan S, Lyon CE, Savage PD, et al. Outcomes and adverse events among patients with implantable cardiac defibrillators in cardiac rehabilitation: a case-controlled study. J Cardiopulm Rehabil Prev. 2009;29:40–3.
Hussein NA, Thomas MA. Rehabilitation of patients with implantable cardioverter/defibrillator: a literature review. Acta Cardiol. 2008;63:249–57.
Dougherty CM, Glenny RW, Burr RL, et al. Prospective randomized trial of moderately strenuous aerobic exercise after an implantable cardioverter defibrillator. Circulation. 2015;131:1835–42.
Dougherty CM, Luttrell MN, Burr RL, et al. Adherence to an aerobic exercise intervention after an implantable cardioverter defibrillator (ICD). Pacing Clin Electrophysiol. 2016;39:128–39.
Vanhees L, Kornaat M, Defoor J, et al. Effect of exercise training in patients with an implantable cardioverter defibrillator. Eur Heart J. 2004;25:1120–6.
Belardinelli R, Capestro F, Misiani A, et al. Moderate exercise training improves functional capacity, quality of life, and endothelium-dependent vasodilation in chronic heart failure patients with implantable cardioverter defibrillators and cardiac resynchronization therapy. Eur J Cardiovasc Prev Rehabil. 2006;13:818–25.
Isaksen K, Munk PS, Valborgland T, et al. Aerobic interval training in patients with heart failure and an implantable cardioverter defibrillator: a controlled study evaluating feasibility and effect. Eur J Prev Cardiol. 2015;22:296–303.
Isaksen K, Morken IM, Munk PS, et al. Exercise training and cardiac rehabilitation in patients with implantable cardioverter defibrillators: a review of current literature focusing on safety, effects of exercise training, and the psychological impact of programme participation. Eur J Prev Cardiol. 2012;19:804–12.
La Gerche A, Schmied CM. Atrial fibrillation in athletes and the interplay between exercise and health. Eur Heart J. 2013;34:3599–602.
Siu CW, Tse HF, Lau CP. Inappropriate implantable cardioverter defibrillator shock from a transcutaneous muscle stimulation device therapy. J Interv Card Electrophysiol. 2005;13:73–5.
Kamiya K, Satoh A, Niwano S, et al. Safety of neuromuscular electrical stimulation in patients implanted with cardioverter defibrillators. J Electrocardiol. 2016;49:99–101.
Sims DB, Mignatti A, Colombo PC, et al. Rate responsive pacing using cardiac resynchronization therapy in patients with chronotropic incompetence and chronic heart failure. Europace. 2011;13:1459–63.
Pedretti RFE, Iliou MC, Israel CW, et al. Comprehensive multicomponent cardiac rehabilitation in cardiac implantable electronic devices recipients: a consensus document from the European Association of Preventive Cardiology (EAPC; Secondary prevention and rehabilitation section) and European Heart Rhythm Association (EHRA). Eur J Prev Cardiol. 2021;28:1736–52.
Ben Gal T, Piepoli M, Corrà U, et al. Exercise programs for LVAD supported patients: A snapshot from the ESC affiliated countries. Int J Cardiol. 2015;201:215–9.
de Jonge N, Kirkels H, Lahpor JR, et al. Exercise performance in patients with end-stage heart failure after implantation of a left ventricular assist device and after heart transplantation: an outlook for permanent assisting? J Am Coll Cardiol. 2001;37:1794–9.
Haft J, Armstrong W, Dyke DB, et al. Hemodynamic and exercise performance with pulsatile and continuous-flow left ventricular assist devices. Circulation. 2007;116(11 Suppl):I8-15.
Hayes K, Leet AS, Bradley SJ, et al. Effects of exercise training on exercise capacity and quality of life in patients with a left ventricular assist device: a preliminary randomized controlled trial. J Heart Lung Transplant. 2012;31:729–34.
Hu SX, Keogh AM, Macdonald PS, et al. Interaction between physical activity and continuous-flow left ventricular assist device function in outpatients. J Card Fail. 2013;19:169–75.
Jakovljevic DG, Birks EJ, George RS, et al. Relationship between peak cardiac pumping capability and selected exercise-derived prognostic indicators in patients treated with left ventricular assist devices. Eur J Heart Fail. 2011;13:992–9.
Jaski BE, Lingle RJ, Kim J, et al. Comparison of functional capacity in patients with end-stage heart failure following implantation of a left ventricular assist device versus heart transplantation: results of the experience with left ventricular assist device with exercise trial. J Heart Lung Transplant. 1999;18:1031–40.
Kugler C, Malehsa D, Schrader E, et al. A multi-modal intervention in management of left ventricular assist device outpatients: dietary counselling, controlled exercise and psychosocial support. Eur J Cardiothorac Surg. 2012;42:1026–32.
Laoutaris ID, Dritsas A, Adamopoulos S, et al. Benefits of physical training on exercise capacity, inspiratory muscle function, and quality of life in patients with ventricular assist devices long-term postimplantation. Eur J Cardiovasc Prev Rehabil. 2011;18:33–40.
Nicholson C, Paz JC. Total artificial heart and physical therapy management. Cardiopulm Phys Ther J. 2010;21:13–21.
Marko C, Danzinger G, Käferbäck M, et al. Safety and efficacy of cardiac rehabilitation for patients with continuous flow left ventricular assist devices. Eur J Prev Cardiol. 2015;22:1378–84.
Pruijsten RV, Lok SI, Kirkels HH, et al. Functional and haemodynamic recovery after implantation of continuous-flow left ventricular assist devices in comparison with pulsatile left ventricular assist devices in patients with end-stage heart failure. Eur J Heart Fail. 2012;14:319–25.
Rogers JG, Aaronson KD, Boyle AJ, et al. Continuous flow left ventricular assist device improves functional capacity and quality of life of advanced heart failure patients. J Am Coll Cardiol. 2010;27:55.
Scheiderer R, Belden C, Schwab D, et al. Exercise guidelines for inpatients following ventricular assist device placement: a systematic review of the literature. Cardiopulm Phys Ther J. 2013;24:35–42.
Grosman-Rimon L, Lalonde SD, Sieh N, et al. Exercise rehabilitation in ventricular assist device recipients: a meta-analysis of effects on physiological and clinical outcomes. Heart Fail Rev. 2019;24:55–67.
Reiss N, Schmidt T, Langheim E, et al. Inpatient cardiac rehabilitation of LVAD patients-updated recommendations from the working group of the German Society for prevention and rehabilitation of cardiovascular diseases. Thorac Cardiovasc Surg. 2021;69:70–82.
Adamopoulos S, Corrà U, Laoutaris ID et al. Exercise training in patients with ventricular assist devices: a review of the evidence and practical advice. A position paper from the committee on exercise physiology and training and the Committee of Advanced Heart Failure of the heart failure Association of the European Society of Cardiology. Eur J Heart Fail. 2019;21:3–13.
Mahfood Haddad T, Saurav A, Smer A, et al. Cardiac rehabilitation in patients with left ventricular assist device: a systematic review and meta-analysis. J Cardiopulm Rehabil Prev. 2017;37:390–6.
Yamamoto S, Hotta K, Ota E, et al. Exercise-based cardiac rehabilitation for people with implantable ventricular assist devices. Cochrane Database Syst Rev.2018;9:CD012222.
Braith RW, Edwards DG. Exercise following heart transplantation. Sports Med. 2000;30:171–92.
Carvalho VO, Bocchi EA, Guimarães GV. Aerobic exercise prescription in adult heart transplant recipients: a review. Cardiovasc Ther. 2011;29:322–6.
Hsieh PL, Wu YT, Chao WJ. Effects of exercise training in heart transplant recipients: a meta-analysis. Cardiology. 2011;120:27–35.
Haykowsky M, Taylor D, Kim D, et al. Exercise training improves aerobic capacity and skeletal muscle function in heart transplant recipients. Am J Transplant. 2009;9:734–9.
Kavanagh T, Mertens DJ, Shephard RJ, et al. Long-term cardiorespiratory results of exercise training following cardiac transplantation. Am J Cardiol. 2003;91:190–4.
Kobashigawa JA, Leaf DA, Lee N, et al. A controlled trial of exercise rehabilitation after heart transplantation. N Engl J Med. 1999;340:272–7.
Niset G, Hermans L, Depelchin P. Exercise and heart transplantation. A review. Sports Med. 1991;12:359–79.
Piepoli MF, Guazzi M, Boriani G, et al. Exercise intolerance in chronic heart failure: mechanisms and therapies. Part I & 2. Eur J Cardiovasc Prev Rehabil. 2010;17:637–42.
Shephard RJ, Kavanagh T, Mertens DJ, et al. The place of perceived exertion ratings in exercise prescription for cardiac transplant patients before and after training. Br J Sports Med. 1996;30:116–21.
Squires RW. Exercise therapy for cardiac transplant recipients. Prog Cardiovasc Dis. 2011;53:429–36.
Tegtbur U, Busse MW, Jung K, et al. Phase III rehabilitation after heart transplantation. Z Kardiol. 2003;92:908–15.
Vanhees L, De Sutter J, Geladas N, et al. Importance of characteristics and modalities of physical activity and exercise in defining the benefits to cardiovascular health within the general population: recommendations from the EACPR (Part I). Eur J Prev Cardiol. 2012;19:670–86.
Rosenbaum AN, Kremers WK, Schirger JA, et al. Association between early cardiac rehabilitation and long-term survival in cardiac transplant recipients. Mayo Clin Proc. 2016;91:149–56.
Anderson L, Nguyen TT, Dall CH, et al. Exercise-based cardiac rehabilitation in heart transplant recipients. Cochrane Database Syst Rev. 2017;4:CD012264.
Didsbury M, McGee RG, Tong A, et al. Exercise training in solid organ transplant recipients: a systematic review and meta-analysis. Transplantation. 2013;95:679–87.
Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. J Am Coll Cardiol. 2006;47:1239–312.
Fokkenrood HJ, Bendermacher BL, Lauret GJ, et al. Supervised exercise therapy versus non-supervised exercise therapy for intermittent claudication. Cochrane Database Syst Rev. 2013;8:CD005263.
Gardner AW, Poehlman ET. Exercise rehabilitation programs for the treatment of claudication pain. A meta-analysis. JAMA. 1995;274:975–80.
Leng GC, Fowler B, Ernst E. Exercise for intermittent claudication. Cochrane Database Syst Rev. 2000:CD000990.
Watson L, Ellis B, Leng GC. Exercise for intermittent claudication. Cochrane Database Syst Rev. 2008:CD000990.
Gardner AW, Montgomery PS, Flinn WR, et al. The effect of exercise intensity on the response to exercise rehabilitation in patients with intermittent claudication. J Vasc Surg. 2005;42:702–9.
Hiatt WR, Wolfel EE, Meier RH, et al. Superiority of treadmill walking exercise versus strength training for patients with peripheral arterial disease. Implications for the mechanism of the training response. Circulation. 1994;90:1866–74.
Sanderson B, Askew C, Stewart I, et al. Short-term effects of cycle and treadmill training on exercise tolerance in peripheral arterial disease. J Vasc Surg. 2006;44:119–27.
Parmenter BJ, Raymond J, Dinnen P, et al. High-intensity progressive resistance training improves flat-ground walking in older adults with symptomatic peripheral arterial disease. J Am Geriatr Soc. 2013;61:1964–70.
Parmenter BJ, Raymond J, Dinnen P, et al. A systematic review of randomized controlled trials: walking versus alternative exercise prescription as treatment for intermittent claudication. Atherosclerosis. 2011;218:1–12.
American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med Sci Sports Exerc. 2009;41:687–708.
Askew CD, Parmenter B, Leicht AS, et al. Exercise & Sports Science Australia (ESSA) position statement on exercise prescription for patients with peripheral arterial disease and intermittent claudication. J Sci Med Sport. 2013.
Collins EG, Langbein WE, Orebaugh C, et al. Cardiovascular training effect associated with polestriding exercise in patients with peripheral arterial disease. J Cardiovasc Nurs. 2005;20:177–85.
Treat-Jacobson D, Bronas UG, Leon AS. Efficacy of arm-ergometry versus treadmill exercise training to improve walking distance in patients with claudication. Vasc Med. 2009;14:203–13.
Andreozzi GM, Martini R, Cordova R, et al. Circulating levels of cytokines (IL-6 and IL-1beta) in patients with intermittent claudication, at rest, after maximal exercise treadmill test and during restore phase. Could they be progression markers of the disease? Int Angiol. 2007;26:245–52.
NICE guidance 2012. https://www.nice.org.uk/guidance/cg147/chapter/Recommendations#management-of-intermittent-claudication.
Lamotte M, Niset G, van de Borne P. The effect of different intensity modalities of resistance training on beat-to-beat blood pressure in cardiac patients. Eur J Cardiovasc Prev Rehabil. 2005;12:12–7.
de Sousa NM, Magosso RF, Dipp T, et al. Continuous blood pressure response at different intensities in leg press exercise. Eur J Prev Cardiol. 2014;21:1324–31.
de Souza NS, Gomides RS, da Silva GV, et al. Intraarterial blood pressure response in hypertensive subjects during low- and high-intensity resistance exercise. Clinics. 2010;65:271–7.
Gjøvaag TF, Mirtaheri P, Simon K, et al. Hemodynamic responses to resistance exercise in patients with coronary artery disease. Med Sci Sports Exerc. 2016;48:581–8.
Sardeli AV, do Carmo Santos L, Ferreira MLV, et al. Cardiovascular responses to different resistance exercise protocols in elderly. Int J Sports Med. 2017;38:928–36.
Gjøvaag T, Hjelmeland AK, Oygard JB, et al. Acute hemodynamic and cardiovascular responses following resistance exercise to voluntary exhaustion. Effects of different loadings and exercise durations. J Sports Med Phys Fitness. 2016;56:616–63.
Lamotte M, Fleury F, Pirard M, Jamon A, et al. Acute cardiovascular response to resistance training during cardiac rehabilitation: effect of repetition speed and rest periods. Eur J Cardiovasc Prev Rehabil. 2010;17:329–36.
Mitchell JH, Payne FC, Saltin B, et al. The role of muscle mass in the cardiovascular response to static contractions. J Physiol. 1980;309:45–54.
Fleck S, Falkel J, Harman E. Cardiovascular responses during resistance training. Med Sci Sports Exerc. 1989;21:114.
Lind AR, McNicol GW. Muscular factors which determine the cardiovascular responses to sustained and rhythmic exercise. Can Med Assoc J. 1967;96:706–15.
Williams MA, Haskell WL, Ades PA, et al; American Heart Association Council on Clinical Cardiology; American Heart Association Council on Nutrition, Physical Activity, and Metabolism. Resistance exercise in individuals with and without cardiovascular disease: 2007 update: a scientific statement from the American Heart Association Council on Clinical Cardiology and Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2007;116:572–84.
Hansen D, Abreu A, Doherty P, et al. Dynamic strength training intensity in cardiovascular rehabilitation: is it time to reconsider clinical practice? A systematic review. Eur J Prev Cardiol. 2019;26:1483–92.
NHS National Audit of Cardiac Rehabilitation 2022. http://www.cardiacrehabilitation.org.uk/current-annual-report.htm.
Hansen D, Linsen L, Verboven K, et al. Magnitude of muscle wasting early after on-pump coronary artery bypass graft surgery and exploration of aetiology. Exp Physiol. 2015;100:818–28.
Neumann FJ, Sousa-Uva M, Ahlsson A, et al; ESC Scientific Document Group. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40:87–165.
Thygesen K, Alpert JS, Jaffe AS, et al; ESC Scientific Document Group. Fourth universal definition of myocardial infarction (2018). Eur Heart J. 2019;40237–69.
Ponikowski P, Voors AA, Anker SD, et al; ESC Scientific Document Group. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129–2200.
Aboyans V, Ricco JB, Bartelink MEL, et al.; ESC Scientific Document Group. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS): document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries. Endorsed by: the European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur Heart J. 2018;39:763–816.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception or design of the work, contributed to the acquisition, analysis or interpretation of data for the work drafted the manuscript, and critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Corresponding author
Ethics declarations
Funding
The realisation of the proof of concept of the EXPERT tool was supported by an UHasselt Industrial Research Fund (IOF) Proof of Concept (PoC) project. This work was supported by the Flemish Research Fund (FWO, FWO-ICA: G0F4220N).
Conflict of interest
The authors disclose that there are no financial or non-financial interests that are directly or indirectly related to the work submitted for publication.
Additional information
EXPERT stands for ‘EXercise Prescription in Everyday practice & Rehabilitative Training’. This working group is endorsed by the European Association of Preventive Cardiology (EAPC).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hansen, D., Beckers, P., Neunhäuserer, D. et al. Standardised Exercise Prescription for Patients with Chronic Coronary Syndrome and/or Heart Failure: A Consensus Statement from the EXPERT Working Group. Sports Med 53, 2013–2037 (2023). https://doi.org/10.1007/s40279-023-01909-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-023-01909-x