Abstract
Background
To improve the understanding of the psychological impacts of anterior cruciate ligament (ACL) injury, a systematic review synthesizing the evidence on knee self-efficacy, fear avoidance beliefs and kinesiophobia following ACL injury is needed.
Objective
The aim of this systematic review was to investigate knee self-efficacy, fear avoidance beliefs and kinesiophobia following ACL injury, and compare these outcomes following management with rehabilitation alone, early and delayed ACL reconstruction (ACLR).
Methods
Seven databases were searched from inception to April 14, 2022. Articles were included if they assessed Tampa Scale of Kinesiophobia (TSK), Knee Self-Efficacy Scale (KSES), or Fear Avoidance Beliefs Questionnaire (FABQ). Risk of bias (RoB) was assessed using domain-based RoB tools (ROBINS-1, RoB 2, RoBANS), and GRADE-assessed certainty of evidence. Random-effects meta-analyses pooled outcomes, stratified by time post-injury (pre-operative, 3–6 months, 7–12 months, > 1–2 years, > 2–5 years, > 5 years).
Results
Seventy-three studies (70% high RoB) were included (study outcomes: TSK: 55; KSES: 22; FABQ: 5). Meta-analysis demonstrated worse kinesiophobia and self-efficacy pre-operatively (pooled mean [95% CI], TSK-11: 23.8 [22.2–25.3]; KSES: 5.0 [4.4–5.5]) compared with 3–6 months following ACLR (TSK-11: 19.6 [18.7–20.6]; KSES: 19.6 [18.6–20.6]). Meta-analysis suggests similar kinesiophobia > 3–6 months following early ACLR (19.8 [4.9]) versus delayed ACLR (17.2 [5.0]). Only one study assessed outcomes comparing ACLR with rehabilitation only.
Conclusions
Knee self-efficacy and kinesiophobia improved from pre-ACLR to 3–6 months following ACLR, with similar outcomes after 6 months. Since the overall evidence was weak, there is a need for high-quality observational and intervention studies focusing on psychological outcomes following ACL injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A total of 70% of studies were rated as high risk of bias, with overall GRADE evidence rated as very low. |
There was a distinct improvement in knee self-efficacy and kinesiophobia from pre-operative to 3–6 months following anterior cruciate ligament (ACL) reconstruction. |
Similar kinesiophobia scores were observed at 3–6 months and 7–12 months following reconstruction, whereas removal of an outlier resulted in better knee self-efficacy at 7–12 months compared with 3–6 months post-surgery. |
Only one study assessed outcomes after treatment with rehabilitation only. |
There is a need for high-quality observational and intervention studies focusing on psychological outcomes following ACL injury. |
1 Introduction
Anterior cruciate ligament (ACL) injuries are a devastating event sustained by active individuals [1,2,3], with impairments that reduce quality of life [4,5,6] and result in long-lasting knee difficulties [3, 4, 7, 8]. Historically, rehabilitation has focused on physical recovery; however, psychological factors such as confidence, self-efficacy, fear avoidance, and kinesiophobia are just as important given they affect all aspects of an individual’s recovery process [5]. The construct kinesiophobia has been defined as “an excessive, irrational, and debilitating fear of physical movement and activity resulting from feeling of vulnerability due to painful injury or re-injury” [9], self-efficacy aims to assess patients’ belief in their ability to perform specific tasks [10], and fear avoidance has been defined as the avoidance of specific movements or actions, conditioning negative reinforcement [11]. Previous research has determined that ACL-injured individuals commonly experience persistent fear of re-injury, due in part to a lack of confidence in their affected knee [12, 13]. Fear of re-injury and lack of confidence in the injured knee can effect kinesiophobia [13, 14] and knee self-efficacy [13]. Psychological measures may also differentiate between individuals who return to sport and those who do not more effectively than functional tasks such as hop testing [15, 16].
Early and delayed ACL reconstruction (ACLR) have resulted in similar long-term knee symptoms, physical activity, and knee function [17], but there is no current consensus on how these treatment strategies affect psychological recovery. Rehabilitation alone has demonstrated similar outcomes to early or delayed ACLR [18], with early rehabilitation reducing the occurrence of subsequent ACLR within these patients [19]. It cannot be assumed that physical and psychological outcomes are similar. Further, there may be an important interaction between worse psychological health and physical recovery [20,21,22], with only 15% of young athletes with high kinesiophobia meeting recommended isometric quadriceps strength limb symmetry values [21]. Additionally, modifiable treatment strategies may also play a role in an individual’s early and late psychological recovery [20]. Of concern, young athletes who experience kinesiophobia [21], low psychological readiness [12], and altered knee confidence [23] are at increased risk of sustaining a second ACL injury. A second ACL injury is an important concern because it is associated with worse long-term knee function, lower quality of life, physical inactivity, and a higher likelihood of knee osteoarthritis compared with primary ACL injury [24].
Evidence supporting the relationship between psychological factors and poor ACL injury outcomes is derived from studies with heterogeneous methodology [6, 25,26,27]. Some studies have a high risk of bias, use different assessment time points, and a variety of research designs [14, 21, 26, 28]. This limits the interpretation and clinical applicability of these findings. There is a need to consolidate these data to better understand how an individual’s psychological health progresses after ACL injury. Exploring potential differences in psychological outcomes following different treatment strategies for ACL injury may inform patient decision making regarding ACL treatment options. Therefore, the purpose of this systematic review was (i) to investigate knee self-efficacy, fear avoidance beliefs, and kinesiophobia following ACL injury; and (ii) to compare knee self-efficacy, fear avoidance beliefs and kinesiophobia following ACL injury between individuals managed with rehabilitation alone, early and delayed surgical approaches.
2 Methods
2.1 Study Design
This work is a systematic review with meta-analysis. This systematic review followed the Finding What Works in Health Care: Standards for Systematic Reviews Handbook [29] and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [30, 31]. This review was prospectively registered on the Open Science Framework (OSF), https://osf.io/2tezs/.
2.2 Information Sources
The databases searched comprised Medline (Ovid), Embase (Elsevier), CINAHL Complete (EBSCOhost), Web of Science Core Collection (Clarivate), Scopus (Elsevier), Cochrane Central Register of Controlled Trials (Cochrane Library), and SPORTDiscus with Full Text (EBSCOhost).
2.3 Search Strategy
The search was developed and conducted, with input from the other authors, by a professional medical librarian (LL) and included a mix of keywords and subject headings representing 'anterior cruciate ligament injuries,' ‘fear,’ ‘confidence,’ and ‘kinesiophobia,’ respectively. Search hedges or database filters were used to remove publication types such as systematic reviews, case studies, conference abstracts, editorials, letters, comments, and animal-only studies as was appropriate for each database. The original search was performed on July 17, 2020, with an updated search on April 14, 2022 and found 6192 citations. Bibliographies of selected studies were hand searched to identify relevant articles not found by the search strategies. The reference lists of the final included articles were reviewed and citation tracking in Web of Science or Scopus was used to identify relevant studies and those studies were added for full-text review. Complete reproducible search strategies, including date ranges and search filters, for all databases are detailed in the electronic supplementary materials (ESM), Appendix 1. After the search, all identified studies were uploaded into Covidence (Veritas Health Innovation, Melbourne, Australia), a software system for managing systematic reviews, and duplicates were removed by the software (n = 3794). A final set of 2398 citations were left to be screened in the title/abstract phase. Study selection was carried out independently by two authors.
2.4 Eligibility Criteria
ACL outcomes of interest included the Tampa Scale of Kinesiophobia (TSK), Knee Self-Efficacy Scale (KSES), and Fear Avoidance Beliefs Questionnaire (FABQ) (Table 1). These specific outcomes were chosen due to their frequency of use within research in ACL-injured populations, and previous research demonstrating that they are important constructs to measure in this population.
Inclusion criteria consisted of (i) studies that assessed an eligible outcome (TSK, KSES, or FABQ) in ACL-injured individuals (first or second ACL injury) at any time point; and (ii) articles written in English.
Exclusion criteria consisted of (i) studies that included patients with three or more concomitant ligament ruptures or knee dislocation on the involved knee; (ii) studies that included patients with a history of three or more ACL ruptures on the same knee; (iii) studies that included any synthetic or enhanced ligament grafting for ACLR (example: Ligament Advanced Reinforcement System [LARS] ligament/GORE-TEX enhanced, Leeds-Keio); (iv) systematic reviews, meta-analyses, qualitative studies, clinical commentaries, case reports, editorials, conference abstracts, or letters to the editor; (v) grey literature (i.e., abstracts theses, or dissertations).
2.5 Study Selection
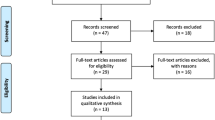
Training for each reviewer was performed prior to screening, consisting of blinded screening of title, abstract, and full text of five studies, followed by group discussion of inclusion and exclusion of articles. Following training, title and abstracts were randomly partitioned into five equal groups. These five equal groups were screened by five groups of two blinded independent reviewers (GB, RZ, CR, VK, HW, NM, CG, SD, AR, and TS) using pre-defined inclusion and exclusion criteria. Following abstract screening, the same two reviewers for each group then performed blinded (to each reviewer) full-text review of articles following title and abstract screening. If any duplicate cohort data were identified between papers or data was reported from more than one follow-up within the same time interval, data from the time point with the largest sample size was included in the meta-analysis. Any conflicts were first discussed between both reviewers; if a consensus could not be reached another reviewer (SF) was utilized to determine final study eligibility. Following full-text review, a hand search of eligible articles was performed for any studies missed within the initial search. The study selection process is presented by flowchart as per PRISMA guidelines (Fig. 1). For papers not published in English that met the inclusion criteria during the title/abstract screening, the abstracts were reviewed for usable data. Due to restrictions in funding, we chose not to have these papers translated and they were excluded at the full-text screening phase.
2.6 Data Extraction
Eligible articles were divided amongst five pairs of reviewers and data were extracted into customized Excel spreadsheets independently by each pair of reviewers (GB, RZ, CR, VK, HW, NM, CG, AR, SD, and SF). If consensus could not be reached for data extraction, a third reviewer (TS) resolved data discrepancies. If data were vague and further detail was needed, authors were contacted to provide clarification on two occasions, 2 weeks apart. If authors did not respond following second contact, specific data were considered not reported.
Data extraction included authors, journal, year published, study design, sample size, follow-up time points/length, injury/surgery history, concomitant injury and treatment, ACL injury treatment, psychological outcomes. Outcome measures were extracted as reported by each study. If outcome measures were reported at the subscale level, scores were calculated following data extraction.
2.7 Anterior Cruciate Ligament (ACL) Treatment Strategies
For the purposes of between-group comparisons, we established prior definitions of ACL treatment strategies. Early ACLR was defined as ACLR within a mean 6 months of ACL injury without trialing exercise therapy or following a period of ‘pre-habilitation’ with the intention of undergoing surgery on completion. Delayed ACLR was defined as ACLR following a trial of management with exercise therapy (i.e., rehabilitation alone). Patients may have ‘crossed-over’ to ACL surgery for a number of reasons including episodes of functional knee instability, patient choice, surgeon recommendations, and inability to meet strength/functional milestones.
2.8 Risk of Bias and Evidence Synthesis
Risk of bias (RoB) was assessed using domain-based RoB tools specific to study design, including the Cochrane Risk of Bias tool for randomized trials (RoB 2) for randomized control trials, Risk of Bias tool In Non-randomized Studies of Interventions (ROBINS-I) for pre-post and quasi-experimental studies, and the Risk of Bias Assessment tool for Nonrandomized Studies (RoBANS) for observational studies [32,33,34]. Two independent reviewers (GB, RZ, CR, VK, HW, NM, CG, AR) assessed each study for RoB. If consensus could not be reached for data extraction, a third reviewer (TS) resolved RoB discrepancies. The strength of the evidence for pooled data per outcome was derived based on RoB judgment of the individual studies according to methods adapted from Teirlinck et al. [35]. Specifically:
-
Strong evidence: Data are provided by two or more studies in which 100% of the studies have a low risk of bias judgement in all assessed RoB domains.
-
Moderate evidence: Data are provided by two or more studies in which ≤ 25% of the studies have a moderate, high or unclear risk of bias in one or more assessed RoB domain.
-
Weak evidence: Data are provided by two or more studies in which > 25% of the studies have a moderate, high or unclear risk of bias in one or more assessed RoB domain.
-
Limited evidence: Data are provided by one study irrespective of RoB judgment in all assessed RoB domains.
The Cochrane Grading of Recommendations, Assessment, Development and Evaluations (GRADE) scale was used to assess the certainty of the evidence for each meta-analysis estimate comparing overall, time and treatment groups of interest [36]. GRADE consists of six criteria (study design, risk of bias, inconsistency, indirectness, imprecision, publication bias, and upgrading factors), scored from − 2 to + 2. Quality of evidence scores are aggregated based on these criteria: very low, low, moderate, and high [36].
2.9 Deviation from Protocol
The original a priori protocol included the ACL Return to Sport (ACL-RSI) outcome measure. However, due to the large number of eligible studies reporting ACL-RSI outcomes, findings will be reported in a subsequent manuscript. Further, the protocol was designed to allow an additional meta-analysis using individual patient data (IPD) if IPD were received from at least 50% of studies. However, this threshold was not met so an aggregate meta-analysis was performed. Within the IPD meta-analysis, specific line items from the ACL quality-of-life outcome measure (ACL-QoL) addressing psychological constructs were designated for analyses. However, this required sharing of raw data and was not viable for an aggregate meta-analysis.
2.10 Statistical Analyses
Aggregated data were descriptively summarized using counts (percentages) and medians (ranges). If a study reported two subgroups for an outcome, the subgroup outcomes were combined using The Cochrane Handbook for Systematic Reviews of Interventions formula to obtain the mean and standard deviation estimates [37]. If a study only reported 95% confidence intervals without standard deviations, standard deviations were estimated using the square root of the sample size and corresponding t scores for the meta-analyses [37]. If a study reported median and quantiles, minimum and maximum, or interquartile range, outcome data were converted to mean and standard deviation through the method by McGrath et al. for the meta-analyses [38]. Time units (e.g., days, months, and years) were converted to the same unit for the meta-analyses.
A meta-analysis was performed using aggregate DerSimonian and Laird random effect models with inverse variance weighting stratified by time since ACL injury (e.g., pre-operative or prior to rehabilitation, 3–6 months, 7–12 months, > 1–2 years, > 2–5 years, > 5 years), and between group differences were assessed through a random effects Q-ANOVA. Specific time points were stratified based on typical rehabilitation recovery phases. Studies reporting TSK outcomes were stratified based on instrument version (i.e., TSK-11, TSK-13, TSK-17) for meta-analyses. Heterogeneity was assessed through overall Tau score, I2 (heterogeneous: ≥ 50%), with a priori alpha of p < 0.10. As only four studies reported FABQ outcomes, with no overlap in time since ACL injury, FABQ outcomes were not included in the meta-analyses and were reported descriptively. Due to the low number of studies reporting TSK scores in specific treatment groups at a given follow-up time point, TSK comparisons between treatment groups were made descriptively. Meta-regressions were performed to investigate the explanation of variance of different confounders, which included ACL treatment group, percent female, mean age, and percent of participants with concomitant knee injuries. Only ACL treatment group and age were evaluated for KSES, due to the small number of studies reporting other potential confounders. Funnel plots were generated to assess for publication bias. Sensitivity meta-analyses excluding high RoB studies were performed. Following funnel plot analyses, one outlier was noted in the KSES analyses. Another sensitivity analysis was performed excluding the outlier. All analyses were performed in R version 4.02 (R Core Team [2013]. R: A language and environment for statistical computing) with the meta package used for all meta-analyses.
3 Results
A total of 2398 titles and abstracts were screened, with 73 studies [1, 3, 14,15,16, 20, 23, 39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103] included in the systematic review and 62 studies [1, 3, 15, 16, 20, 23, 39,40,41,42, 44,45,46,47,48,49,50,51, 53,54,55,56, 58,59,60,61,62, 64,65,66,67, 69, 70, 72,73,74,75,76, 81,82,83, 85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101, 103] included in the meta-analysis (Fig. 1). A total of 55 studies reported TSK scores (TSK-11 = 28; TSK-13 = 1; TSK-17 = 25; version not specified = 1), [1, 15, 20, 23, 39,40,41,42, 46,47,48,49,50,51,52,53, 55,56,57, 59,60,61,62, 64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79, 82, 83, 85,86,87,88,89, 93,94,95,96, 99,100,101, 103] 22 studies reported KSES scores [3, 14,15,16, 20, 41, 43,44,45, 52,53,54, 58, 80,81,82, 90,91,92, 97, 98, 104], and five studies reported FABQ scores [24, 56, 64, 102, 104]. A total of 44 studies were cross-sectional [1, 3, 20, 23, 39, 41, 43, 46, 47, 50, 54,55,56, 59, 60, 62, 63, 66,67,68,69,70,71,72, 75,76,77,78, 83,84,85,86,87, 90, 92,93,94,95,96,97,98,99, 101, 102], 14 studies were prospective cohorts [14, 15, 48, 49, 52, 53, 58, 61, 73, 74, 79,80,81, 88], seven were randomized controlled trials [57, 60, 82, 91, 100, 103, 104], four were case control [40, 45, 64, 92], three were retrospective cohorts [44, 51, 89], and two were case series [42, 65] (Table 2). A total of 7179 patients were included, with a percent female of 71% (range of 0–100%) and a mean age range of 16–46 years. Twelve (20%) studies were included in the delayed ACLR treatment group [14, 39, 40, 44, 49, 61, 68, 75, 81, 88, 97, 105].
3.1 Risk of Bias
Out of 64 observational cohort, case series, or cross-sectional studies [1, 3, 14, 15, 20, 23, 39,40,41,42,43, 45,46,47,48,49,50,51, 54,55,56, 58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81, 83,84,85,86,87,88,89,90, 92,93,94,95,96,97,98,99, 101, 102], 44 were high RoB [3, 14, 15, 39, 43, 45,46,47,48,49,50, 54,55,56, 58,59,60,61,62,63,64,65,66,67,68, 72, 73, 75, 76, 78,79,80,81, 87, 90, 92, 94, 97,98,99, 101, 102], and 20 were low RoB (Appendix 2A, see ESM) [1, 20, 23, 40,41,42, 51, 69,70,71, 74, 77, 83,84,85,86, 88, 89, 93, 95, 96]. Common sources of bias included inability to control for confounding, inadequate exposure measurement, and selective outcome reporting. Out of the two controlled intervention studies, both were high RoB [52, 53] (Appendix 2B, see ESM). Out of the seven randomized control trials [57, 82, 88, 91, 100, 103, 104], four were graded as high RoB [82, 88, 91, 104] and three were graded as low RoB [57, 100, 103]. Common sources of bias included allocation concealment, missing data reporting, and result reporting (Appendix 2C, see ESM). According to the Teirlinck et al. [35] strength of evidence, studies demonstrated weak evidence for TSK, KSES, and FABQ outcomes for all time points. The GRADE scale determined that the certainty of the pooled estimates for both TSK and KSES was very low, due to the high RoB of publications, inconsistency, and imprecision in reporting (Appendix 3, see ESM).
3.2 Tampa Scale of Kinesiophobia
TSK-17 meta-analyses demonstrated differences in scores between time points (pre-operative: 39.8 [95% CI 35.9–43.8]; 3–6 months: 34.6 [95% CI 31.0–38.2]; 7–12 months: 33.2 [95% CI 29.3–37.2]; > 1–2 years: 33.3 [95% CI 31.1–35.6]; > 2–5 years: 34.0 [95% CI 32.1–35.9]; > 5 years: 31.5 [95% CI 29.5–33.4]; Q = 14.9; p = 0.011) (Fig. 2a). Between pre-operative and 3–6 months, TSK-17 scores improved by a mean 5.3 points. Meta-regression of early and delayed ACLR and percent female demonstrated no explanation of meta-analysis variance (R2 = 0.0). Meta-regression of ACL treatment group, percent female, age, and percent with concomitant knee injuries demonstrated over 50% explanation of meta-analysis variance (R2 = 0.83). Funnel plots demonstrated no publication biases (Appendices 4–6, see ESM).
TSK-11 meta-analyses also demonstrated differences in scores between time points (pre-operative: 23.8 [95% CI 22.3–25.3]; 3–6 months: 19.6 [95% CI 18.6–20.7]; 7–12 months: 17.9 [95% CI 15.2–20.6]; > 2–5 years: 22.3 [95% CI 11.9–32.7]; I2 = 97.6%, p < 0.001; Q = 22.8, p < 0.001) (Fig. 2b). TSK-11 scores improved between pre-operative and 3–6-month follow-up by a mean of 4.1 points. Meta-regression of ACL treatment group and percent female demonstrated no explanation of meta-analysis variance (R2 = 0.0). Meta-regression of ACL treatment group, percent female, age, and percent of concomitant knee injuries explained 0.73 (R2) of meta-analysis variance. Funnel plots demonstrated no publication biases (see ESM).
3.3 Knee Self-Efficacy Scale
KSES meta-analyses demonstrated differences in pooled scores between follow-up time points (pre-operative: 5.0 [95% CI 4.4–5.5]; 3–6 months: 6.4 [95% CI 5.5–7.4]; 7–12 months: 7.5 [95% CI 6.8–8.2]; Q = 32.0; p < 0.001) (Fig. 3). KSES scores improved between pre-operative and 3–6-month follow-up by a mean of 1.5 points and between pre-operative and 7–12 months by 2.5 points. No studies included in the meta-analysis reported KSES scores > 12 months after ACLR. Meta-regression of ACL treatment group and percent female demonstrated no explanation of meta-analysis variance (R2 = 0.0).
3.4 Fear-Avoidance Belief Questionnaire
One study reported FABQ scores at injury (mean: 18.5 [SD 6.9]) and 3 months (mean: 16.1 [SD 8.2]) [104]. One study reported FABQ scores at 1 year post-injury (mean: 12.9 [SD 5.3]) [84]. At > 5 years following ACL injury, three studies reported FABQ scores ranging from median of 8.0 to 11.0 [56, 64, 102].
3.5 Early ACL Reconstruction (ACLR), Delayed ACLR, and Rehabilitation Alone
Only two TSK-11 studies could be summarized at any time points concerning delayed ACL treatment, which were for the 3–6-month time point [49, 61]. Participants in both studies performed exercise therapy for at least 10 sessions prior to delayed ACLR [49, 61]. The early ACL treatment group reported a median TSK-11 of 19.8 (4.9) and the delayed ACLR group a median of 17.2 (5.0) for the 3–6-month time point [49, 61]. Only one study reported outcomes (TSK-17) following treatment with rehabilitation only, and this was > 5 years following injury with a mean of 32 (SD 7) [88].
3.6 Sensitivity Analyses
Including only low RoB studies for the pooled TSK-17 and TSK-11 meta-analyses observed no differences in scores between follow-up time points. Excluding the outlier from the KSES meta-analyses demonstrated a reduced pooled score at 6 months post-injury (pre-operative: 5.0 [95% CI 4.4–5.5]; 3–6 months: 6.0 [95% CI 5.1–6.8]; 6–12 months: 7.5 [95% CI 6.8–8.2]; I2 = 97.4%, p < 0.001) compared with the primary meta-analysis. For further detail, please refer to Appendix 7 in the ESM.
4 Discussion
There was a distinct improvement in kinesiophobia and knee self-efficacy from pre-operative to 3–6 months following ACLR. The limited studies available suggest that FABQ may also improve from pre-operative to 3–6 months following ACLR. This improvement may be expected as patients progress from the acute postoperative phase to more advanced stages of rehabilitation. Similar scores were reported at 3–6 months and 7–12 months following ACLR for all outcomes. There is a need for further research on psychological outcomes following early ACLR, delayed ACLR, and rehabilitation only.
Both the TSK-17 and TSK-11 demonstrated a clinically significant (> 4-point change in TSK scores) [106] improvement in knee kinesiophobia from pre-operative to 3–6 months following ACLR. Similar kinesiophobia scores were observed between 3–6 months, 7–12 months, > 1–2 years, and > 2–5 years after ACLR. While only a single time interval could be compared between early and delayed ACLR patients, these groups demonstrated similar TSK scores at 6 months. Only two studies [1, 61] longitudinally followed ACL patients from injury to 1 year, which demonstrated similar scores between 3–6 months and 7–12 months. The plateau in kinesiophobia scores after a period of 3–6 months following injury is comparable to outcomes for shoulder dislocation [107] or Achilles tendon rupture [108]. These findings suggest that, on average, knee kinesiophobia is low and stabilized 6 months following ACLR, and remains similar over time. Another possible explanation is that once patients progress from the acute recovery phase, further improvements in kinesiophobia may require specific interventions. As rehabilitation does not traditionally target these psychological constructs, addressing psychological aspects of recovery may provide an opportunity to improve patient outcomes. Potential interventions to improve kinesiophobia include pre-operative education [109], knee bracing [110], or cognitive behavioral therapy [111]. The TSK meta-regression found that 73–83% of variance was explained by older age, increased kinesiophobia at ACL injury, and presence of concomitant injuries. These findings are similar to patients with knee osteoarthritis and patella dislocation [2, 112]. As there was high heterogeneity in the meta-analyses, this could be explained by different patient samples, including patients that were older at ACL injury and studies including a high prevalence of concomitant knee injuries. Increased age and concomitant knee injuries have previously been associated with increased kinesiophobia in ACL patient populations [113]. Increased kinesiophobia has been associated with worse knee quality of life and return to sport [113]. Older ACL-injured patients who have concomitant knee injuries may require targeted interventions to reduce kinesiophobia in the first 6 months following injury.
Twenty-one studies were included that evaluated knee self-efficacy with the KSES pre-operatively, at 3–6 months or 7–12 months after ACLR. All but one of the included studies were graded as high RoB. There was a 1.4-point decrease from pre-operative to 3–6 months and a 1.1-point decrease from 3–6 months to 7–12 months. These changes cannot be currently interpreted for clinical meaningfulness, but are statistically beyond the standard error of measurement [3, 16]. Self-efficacy refers to the patient’s beliefs in performing specific movements, tasks, or actions [10]. As ACLR patients who return to sport are likely do so around 1 year following surgery, these findings may reflect increases in the patients’ belief in their ability to perform sporting activities. Worse knee self-efficacy has been related to worse patient-reported outcomes and return to sport [14, 80]. On average, knee self-efficacy will improve after 3 months, so patients should be monitored for prolonged low levels of knee self-efficacy that exceed 3 months post-ACLR. Patients reporting low self-efficacy may require further rehabilitation time or specific psychological interventions prior to focusing on returning to sport [91].
Only five studies reported FABQ scores following ACL injury. There was a 6-point decrease in FABQ from pre-operative to 1 year following ACLR. A further 1-point decrease in FABQ was reported 5 years following ACLR. Currently, there is not an established minimal clinically important difference (MCID) for the FABQ outcome measure in knee-injured patients. However, a 6-point reduction may be clinically meaningful while a 1-point decrease is unlikely to be clinically relevant. While not validated in knee injury populations, FABQ scores > 14 in low back pain patients is associated with high levels of fear avoidance behavior [114]. Studies in our review did not report FABQ scores < 14 until after 6 months following injury, suggesting that fear avoidance may remain high in the first 6 months post-surgery.
The results from this systematic review necessitate future research. Over two-thirds of included studies were graded as high RoB, with overall weak evidence for all outcomes. Specific methodological domains with a high RoB prevalence included a lack of control of confounders for control intervention, a majority being observational studies, and poor reporting of missing data in all study designs. Given the recent identified importance of psychological recovery for ACL-injured athletes [40, 115], high-quality studies are needed to assess kinesiophobia, knee self-efficacy, and fear avoidance beliefs over time. The KSES and FABQ require studies to establish MCIDs within knee injury populations, to improve clinical outcome interpretation. The data did not allow comparisons between early and delayed ACL treatment and only one study assessed outcomes following treatment with rehabilitation alone. Further comparisons are needed between different ACL injury treatments and their effect on psychological recovery. Understanding the impact of psychological interventions is also needed for older patients with concomitant knee injuries prior to 6 months following ACL injury. Future research should focus on understanding the impacts of improving kinesiophobia, self-efficacy, and fear avoidance on other outcomes, such as health-related quality of life, anxiety and depression, sport and activity participation, and re-injury rates.
The results of this systematic review and meta-analysis have clinical implications. Patients should be monitored for kinesiophobia, knee self-efficacy, or fear avoidance following ACL injury and throughout the rehabilitation process. If kinesiophobia, knee self-efficacy, or fear avoidance does not improve and stabilize after 6 months following ACL injury and surgery, further examination and patient discussion is required to understand the causes underlying these patient-reported findings. While kinesiophobia, knee self-efficacy, and fear avoidance report different psychological constructs [9,10,11], only the TSK has established MCID [106] and therefore at this time it is recommended that the TSK should be administered.
We acknowledge a number of study limitations. The inclusion of only peer-reviewed published work excludes potential grey literature findings, which decreases the scope of these findings. Only studies written in English were included in this systematic review, decreasing the breadth of the included literature. The initial protocol involved performing an individual participant meta-analysis. Due to the paucity of individual participant data obtained, in accordance with the a priori protocol, only aggregated meta-analyses were performed. The initial protocol included further psychological knee outcomes. However, as a substantial number of studies were eligible, a separate systematic review was initiated. Knee injuries that involved three or more ligament ruptures were excluded from the review, which decreases the generalizability of these findings to all ACL injuries. Most included studies were cross-sectional; thus, ACLR longitudinal change and outcome responsiveness cannot be inferred from these results. Differences in outcomes by time points are not connected by longitudinal patient data, decreasing the clinical utility of these data. A large proportion of studies were graded as high RoB, decreasing the viability of these findings. Additionally, kinesiophobia was assessed with three different versions of the TSK, which decreased the precision in comparing time intervals, specifically concerning the meta-regressions and between early and delayed surgical groups. The TSK has not undergone English validation in ACL populations and these results should be interpreted with caution. The FABQ and KSES do not report MCID, which decreases the clinical interpretability of these findings. While all studies were included in the meta-analyses, sensitivity analyses were performed excluding high RoB studies, demonstrating similar results. The meta-analyses reported high heterogeneity, decreasing the weight of these inferences.
5 Conclusion
Knee self-efficacy and kinesiophobia improved from pre-ACLR to 3–6 months following ACLR, with the included limited studies suggesting that fear avoidance also improves during this time period. Knee self-efficacy and kinesiophobia remained relatively stable over the preceding year. Older age at injury and concomitant injuries, such as meniscus and medial collateral ligament injuries, may increase knee kinesiophobia and may benefit from targeted interventions prior to 6 months following injury. The high RoB, heterogeneity, and cross-sectional nature of these studies reduce the clinical weight of these findings. Sports medicine clinicians should consider monitor knee self-efficacy, kinesiophobia, and fear avoidance following ACLR. Patients that report poor knee self-efficacy, kinesiophobia, and fear avoidance following the acute stage of rehabilitation may benefit from targeted interventions to improve these psychological constructs. Since the overall evidence was weak, there is a need for high-quality observational and intervention studies focusing on psychological outcomes following ACL injury.
References
Lentz TA, Zeppieri G Jr, George SZ, Tillman SM, Moser MW, Farmer KW, et al. Comparison of physical impairment, functional, and psychosocial measures based on fear of reinjury/lack of confidence and return-to-sport status after ACL reconstruction. Am J Sports Med. 2015;43(2):345–53.
Hart HF, Collins NJ, Ackland DC, Crossley KM. Is impaired knee confidence related to worse kinesiophobia, symptoms, and physical function in people with knee osteoarthritis after anterior cruciate ligament reconstruction? J Sci Med Sport. 2015;18(5):512–7.
Thomeé P, Währborg P, Börjesson M, Thomeé R, Eriksson B, Karlsson J. A new instrument for measuring self-efficacy in patients with an anterior cruciate ligament injury. Scand J Med Sci Sport. 2006;16(3):181–7.
Culvenor AG, Lai CC, Gabbe BJ, Makdissi M, Collins NJ, Vicenzino B, et al. Patellofemoral osteoarthritis is prevalent and associated with worse symptoms and function after hamstring tendon autograft ACL reconstruction. Br J Sport Med. 2014;48(6):435–9.
Truong LK, Mosewich AD, Holt CJ, Le CY, Miciak M, Whittaker JL. Psychological, social and contextual factors across recovery stages following a sport-related knee injury: a scoping review. Br J Sport Med. 2020;54(19):1149–56.
Culvenor AG, Collins NJ, Guermazi A, Cook JL, Vicenzino B, Khan KM, et al. Early knee osteoarthritis is evident one year following anterior cruciate ligament reconstruction: a magnetic resonance imaging evaluation. Arthritis Rheum. 2015;67(4):946–55.
Filbay S, Ackerman I, Russell T, Crossley K. Return to sport matters—longer-term quality of life after ACL reconstruction in people with knee difficulties. Scand J Med Sci Sport. 2017;27(5):514–24.
Filbay S, Culvenor A, Ackerman I, Russell T, Crossley K. Quality of life in anterior cruciate ligament-deficient individuals: a systematic review and meta-analysis. Br J Sport Med. 2015;49(16):1033–41.
Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191.
Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52(2):157–68.
Kori S. Kinesiophobia: a new view of chronic pain behavior. Pain Manag. 1990;3:35–43.
McPherson AL, Feller JA, Hewett TE, Webster KE. Psychological readiness to return to sport is associated with second anterior cruciate ligament injuries. Am J Sport Med. 2019;47(4):857–62.
Montalvo AM, Schneider DK, Yut L, Webster KE, Beynnon B, Kocher MS, et al. “What’s my risk of sustaining an ACL injury while playing sports?” A systematic review with meta-analysis. Br J Sport Med. 2019;53(16):1003–12.
Piussi R, Beischer S, Thomeé R, Hamrin SE. Superior knee self-efficacy and quality of life throughout the first year in patients who recover symmetrical muscle function after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020;28(2):555–67.
Flosadottir V, Frobell R, Roos EM, Ageberg E. Impact of treatment strategy and physical performance on future knee-related self-efficacy in individuals with ACL injury. BMC Musculoskelet Disord. 2018;19(1):1–9.
Thomeé P, Währborg P, Börjesson M, Thomeé R, Eriksson B, Karlsson J. Self-efficacy, symptoms and physical activity in patients with an anterior cruciate ligament injury: a prospective study. Scand J Med Sci Sport. 2007;17(3):238–45.
Smith TO, Davies L, Hing CB. Early versus delayed surgery for anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2010;18(3):304–11.
Filbay SR, Roos EM, Frobell RB, Roemer F, Ranstam J, Lohmander LS. Delaying ACL reconstruction and treating with exercise therapy alone may alter prognostic factors for 5-year outcome: an exploratory analysis of the KANON trial. Br J Sport Med. 2017;51(22):1622–9.
Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med. 2010;363(4):331–42.
Ardern CL, Österberg A, Tagesson S, Gauffin H, Webster KE, Kvist J. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br J Sport Med. 2014;48(22):1613–9.
Tagesson S, Kvist J. Greater fear of re-injury and increased tibial translation in patients who later sustain an ACL graft rupture or a contralateral ACL rupture: a pilot study. J Sport Sci. 2016;34(2):125–32.
Chmielewski TL, Jones D, Day T, Tillman SM, Lentz TA, George SZ. The association of pain and fear of movement/reinjury with function during anterior cruciate ligament reconstruction rehabilitation. J Orthop Sport Phys Ther. 2008;38(12):746–53.
Tichonova A, Rimdeikienė I, Petruševičienė D, Lendraitienė E. The relationship between pain catastrophizing, kinesiophobia and subjective knee function during rehabilitation following anterior cruciate ligament reconstruction and meniscectomy: a pilot study. Medicina. 2016;52(4):229–37.
Ross CA, Clifford A, Louw QA. Factors informing fear of reinjury after anterior cruciate ligament reconstruction. Physiother Theory Pract. 2017;33(2):103–14.
Montalvo AM, Schneider DK, Webster KE, Yut L, Galloway MT, Heidt RS Jr, et al. Anterior cruciate ligament injury risk in sport: a systematic review and meta-analysis of injury incidence by sex and sport classification. J Athl Train. 2019;54(5):472–82.
Langford JL, Webster KE, Feller JA. A prospective longitudinal study to assess psychological changes following anterior cruciate ligament reconstruction surgery. Br J Sport Med. 2009;43(5):377–8.
Wellsandt E, Failla MJ, Axe MJ, Snyder-Mackler L. Does anterior cruciate ligament reconstruction improve functional and radiographic outcomes over nonoperative management 5 years after injury? Am J Sport Med. 2018;46(9):2103–12.
Filbay SR, Ackerman IN, Dhupelia S, Arden NK, Crossley KM. Quality of life in symptomatic individuals after anterior cruciate ligament reconstruction, with and without radiographic knee osteoarthritis. J Orthop Sport Phys Ther. 2018;48(5):398–408.
Morton S, Berg A, Levit L, Eden J. Finding what works in health care: standards for systematic reviews. 2011.
Moher D, Altman DG, Liberati A, Tetzlaff J. PRISMA statement. Epidemiology. 2011;22(1):128.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, The PRISMA, et al. statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:372.
Minozzi S, Cinquini M, Gianola S, Gonzalez-Lorenzo M, Banzi R. The revised Cochrane risk of bias tool for randomized trials (RoB 2) showed low interrater reliability and challenges in its application. J Clin Epidemiol. 2020;126:37–44.
Kim SY, Park JE, Lee YJ, Seo H-J, Sheen S-S, Hahn S, et al. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol. 2013;66(4):408–14.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;12:355.
Teirlinck C, Dorleijn D, Bos P, Rijkels-Otters J, Bierma-Zeinstra S, Luijsterburg P. Prognostic factors for progression of osteoarthritis of the hip: a systematic review. Arthritis Res Ther. 2019;21(1):1–19.
Group GW. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490.
Collaboration TC. Cochrane handbook for systematic reviews of interventions version 5.0.2. In: J. H, GS, editors.: The Cochrane Collaboration; 2009.
McGrath S, Zhao X, Steele R, Thombs BD, Benedetti A, Collaboration DSD. Estimating the sample mean and standard deviation from commonly reported quantiles in meta-analysis. Stat Methods Med Res. 2020;29(9):2520–37.
Alswat MM, Khojah O, Alswat AM, Alghamdi A, Almadani MS, Alshibely A, et al. Returning to sport after anterior cruciate ligament reconstruction in physically active individuals. Cureus. 2020;12:9.
Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Am J Sport Med. 2013;41(7):1549–58.
Ardern CL, Österberg A, Sonesson S, Gauffin H, Webster KE, Kvist J. Satisfaction with knee function after primary anterior cruciate ligament reconstruction is associated with self-efficacy, quality of life, and returning to the preinjury physical activity. Arthroscopy. 2016;32(8):1631-8.e3.
Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Sports participation 2 years after anterior cruciate ligament reconstruction in athletes who had not returned to sport at 1 year: a prospective follow-up of physical function and psychological factors in 122 athletes. Am J Sport Med. 2015;43(4):848–56.
Baez SE, Hoch MC, Hoch JM. Psychological factors are associated with return to pre-injury levels of sport and physical activity after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2020;28(2):495–501.
Beischer S, Hamrin Senorski E, Thomeé C, Samuelsson K, Thomeé R. How is psychological outcome related to knee function and return to sport among adolescent athletes after anterior cruciate ligament reconstruction? Am J Sports Med. 2019;47(7):1567–75.
Beischer S, Hamrin Senorski E, Thomeé C, Samuelsson K, Thomeé R. Knee strength, hop performance and self-efficacy at 4 months are associated with symmetrical knee muscle function in young athletes 1 year after an anterior cruciate ligament reconstruction. BMJ Open Sport Exerc Med. 2019;5(1): e000504.
Burland JP, Howard JS, Lepley AS, DiStefano LJ, Lepley LK, Frechette L. What are our patients really telling us? Psychological constructs associated with patient-reported outcomes after anterior cruciate ligament reconstruction. J Athl Train. 2020;55(7):707–16.
Chen T, Zhang P, Li Y, Webster K, Zhang J, Yao W, et al. Translation, cultural adaptation and validation of simplified Chinese version of the anterior cruciate ligament return to sport after injury (ACL-RSI) scale. PLoS ONE. 2017;12(8): e0183095.
Chmielewski TL, George SZ. Fear avoidance and self-efficacy at 4 weeks after ACL reconstruction are associated with early impairment resolution and readiness for advanced rehabilitation. Knee Surg Sports Traumatol Arthrosc. 2019;27(2):397–404.
Chmielewski TL, Zeppieri G Jr, Lentz TA, Tillman SM, Moser MW, Indelicato PA, et al. Longitudinal changes in psychosocial factors and their association with knee pain and function after anterior cruciate ligament reconstruction. Phys Ther. 2011;91(9):1355–66.
Clifford AM, Buckley E, O’Farrell D, Louw Q, Moloney C. Fear of movement in patients after anterior cruciate ligament reconstruction. Phys Pract Res. 2017;38(2):113–20.
Culvenor AG, Collins NJ, Vicenzino B, Cook JL, Whitehead TS, Morris HG, et al. Predictors and effects of patellofemoral pain following hamstring-tendon ACL reconstruction. J Sci Med Sport. 2016;19(7):518–23.
Coronado RA, Sterling EK, Fenster DE, Bird ML, Heritage AJ, Woosley VL, et al. Cognitive-behavioral-based physical therapy to enhance return to sport after anterior cruciate ligament reconstruction: An open pilot study. Phys Ther Sport. 2020;42:82–90.
Courtot L, Ferre F, Reina N, Marot V, Chiron P, Berard E, et al. Patient participation during anterior cruciate ligament reconstruction improves comprehension, satisfaction, and functional outcomes: a simple way to improve our practices. Orthop J Sports Med. 2019;7(4):2325967119841089.
Ezzat AM, Whittaker JL, Brussoni M, Mâsse LC, Emery CA. The English Knee Self-Efficacy Scale is a valid and reliable measure for knee-specific self-efficacy in individuals with a sport-related knee injury in the past 5 years. Knee Surg Sports Traumatol Arthrosc. 2021;29(2):616–26.
Faleide AGH, Inderhaug E, Vervaat W, Breivik K, Bogen BE, Mo IF, et al. Anterior cruciate ligament-return to sport after injury scale: validation of the Norwegian language version. Knee Surg Sports Traumatol Arthrosc. 2020;28(8):2634–43.
Genoese F, Baez SE, Heebner N, Hoch MC, Hoch JM. The relationship between injury-related fear and visuomotor reaction time in individuals with a history of anterior cruciate ligament reconstruction. J Sport Rehabil. 2020;30(3):353–9.
Gholami M, Kamali F, Mirzeai M, Motealleh A, Shamsi M. Effects of kinesio tape on kinesiophobia, balance and functional performance of athletes with post anterior cruciate ligament reconstruction: a pilot clinical trial. BMC Sports Sci Med Rehabil. 2020;12:57.
Hamrin Senorski E, Samuelsson K, Thomeé C, Beischer S, Karlsson J, Thomeé R. Return to knee-strenuous sport after anterior cruciate ligament reconstruction: a report from a rehabilitation outcome registry of patient characteristics. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1364–74.
Harput G, Tok D, Ulusoy B, Eraslan L, Yildiz TI, Turgut E, et al. Translation and cross-cultural adaptation of the anterior cruciate ligament-return to sport after injury (ACL-RSI) scale into Turkish. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):159–64.
Harput G, Ulusoy B, Ozer H, Baltaci G, Richards J. External supports improve knee performance in anterior cruciate ligament reconstructed individuals with higher kinesiophobia levels. Knee. 2016;23(5):807–12.
Hartigan EH, Lynch AD, Logerstedt DS, Chmielewski TL, Snyder-Mackler L. Kinesiophobia after anterior cruciate ligament rupture and reconstruction: noncopers versus potential copers. J Orthop Sport Phys Ther. 2013;43(11):821–32.
Hirohata K, Aizawa J, Furuya H, Mitomo S, Ohmi T, Ohji S, et al. The Japanese version of the anterior cruciate ligament-return to sport after injury (ACL-RSI) scale has acceptable validity and reliability. Knee Surg Sports Traumatol Arthrosc. 2020;28(8):2519–25.
Hoch JM, Houston MN, Baez SE, Hoch MC. Fear-avoidance beliefs and health-related quality of life in post-ACL reconstruction and healthy athletes: a case–control study. J Sport Rehabil. 2020;29(6):772–6.
Hoch JM, Sinnott CW, Robinson KP, Perkins WO, Hartman JW. The examination of patient-reported outcomes and postural control measures in patients with and without a history of ACL reconstruction: a case control study. J Sport Rehabil. 2018;27(2):170–6.
Joreitz R, Lynch A, Popchak A, Irrgang J. Criterion-based rehabilitation program with return to sport testing following acl reconstruction: a case series. Int J Sports Phys Ther. 2020;15(6):1151–73.
Kuenze C, Bell DR, Grindstaff TL, Lisee CM, Birchmeier T, Triplett A, et al. A Comparison of psychological readiness and patient-reported function between sexes after anterior cruciate ligament reconstruction. J Athl Train. 2020;56(2):164–9.
Kvist J, Ek A, Sporrstedt K, Good L. Fear of re-injury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg Sport Traumatol Arthrosc. 2005;13(5):393–7.
Kvist J, Österberg A, Gauffin H, Tagesson S, Webster K, Ardern C. Translation and measurement properties of the Swedish version of ACL-Return to Sports after Injury questionnaire. Scand J Med Sci Sports. 2013;23(5):568–75.
Lentz TA, Tillman SM, Indelicato PA, Moser MW, George SZ, Chmielewski TL. Factors associated with function after anterior cruciate ligament reconstruction. Sports Health. 2009;1(1):47–53.
Lentz TA, Zeppieri G Jr, Tillman SM, Indelicato PA, Moser MW, George SZ, et al. Return to preinjury sports participation following anterior cruciate ligament reconstruction: contributions of demographic, knee impairment, and self-report measures. J Orthop Sports Phys Ther. 2012;42(11):893–901.
Lisee CM, DiSanti JS, Chan M, Ling J, Erickson K, Shingles M, et al. Gender differences in psychological responses to recovery after anterior cruciate ligament reconstruction before return to sport. J Athl Train. 2020;55(10):1098–105.
Luc-Harkey BA, Franz JR, Losina E, Pietrosimone B. Association between kinesiophobia and walking gait characteristics in physically active individuals with anterior cruciate ligament reconstruction. Gait Posture. 2018;64:220–5.
Meierbachtol A, Obermeier M, Yungtum W, Bottoms J, Paur E, Nelson BJ, et al. Injury-related fears during the return-to-sport phase of ACL reconstruction rehabilitation. Orthop J Sports Med. 2020;8(3):2325967120909385.
Müller U, Krüger-Franke M, Schmidt M, Rosemeyer B. Predictive parameters for return to pre-injury level of sport 6 months following anterior cruciate ligament reconstruction surgery. Knee Surg Sports Traumatol Arthrosc. 2015;23(12):3623–31.
Norte GE, Hertel J, Saliba SA, Diduch DR, Hart JM. Quadriceps function and patient-reported outcomes after anterior cruciate ligament reconstruction in patients with or without knee osteoarthritis. J Athl Train. 2018;53(10):965–75.
Norte GE, Solaas H, Saliba SA, Goetschius J, Slater LV, Hart JM. The relationships between kinesiophobia and clinical outcomes after ACL reconstruction differ by self-reported physical activity engagement. Phys Ther Sport. 2019;40:1–9.
Ohji S, Aizawa J, Hirohata K, Mitomo S, Ohmi T, Jinno T, et al. Athletic identity and sport commitment in athletes after anterior cruciate ligament reconstruction who have returned to sports at their pre-injury level of competition. BMC Sports Sci Med Rehabil. 2021;13(1):37.
Silva LO, Mendes LMR, Lima POP, Almeida GPL. Translation, cross-adaptation and measurement properties of the Brazilian version of the ACL-RSI Scale and ACL-QoL Questionnaire in patients with anterior cruciate ligament reconstruction. Braz J Phys Ther. 2018;22(2):127–34.
Paterno MV, Flynn K, Thomas S, Schmitt LC. Self-reported fear predicts functional performance and second ACL injury after ACL reconstruction and return to sport: a pilot study. Sports Health. 2018;10(3):228–33.
Piussi R, Broman D, Musslinder E, Beischer S, Thomeé R, Hamrin SE. Recovery of preoperative absolute knee extension and flexion strength after ACL reconstruction. BMC Sports Sci Med Rehabil. 2020;12(1):77.
Pua YH, Low J, Woon EL, Tay OS, Cheong P, Thumboo J, et al. Knee performance and self-efficacy trajectory curves after ACL reconstruction: a longitudinal study. Phys Ther Sport. 2021;49:157–63.
Rhim HC, Lee SJ, Jeon JS, Kim G, Lee KY, Lee JH, et al. Effectiveness of modeling videos on psychological responses of patients following anterior cruciate ligament reconstruction: a pilot randomized trial. Medicine (Baltimore). 2020;99(45): e23158.
Roe C, Jacobs C, Kline P, Lucas K, Johnson D, Ireland ML, et al. Correlations of single-leg performance tests to patient-reported outcomes after primary anterior cruciate ligament reconstruction. Clin J Sport Med. 2021;31(5):e265–70.
Ross MD. The relationship between functional levels and fear-avoidance beliefs following anterior cruciate ligament reconstruction. J Orthop Traumatol. 2010;11(4):237–43.
Sala-Barat E, Álvarez-Díaz P, Alentorn-Geli E, Webster KE, Cugat R, Tomás-Sabado J. Translation, cross-cultural adaptation, validation, and measurement properties of the Spanish version of the anterior cruciate ligament-return to sport after injury (ACL-RSI-Sp) scale. Knee Surg Sports Traumatol Arthrosc. 2020;28(3):833–9.
Slagers AJ, Reininga IH, van den Akker-Scheek I. The Dutch language anterior cruciate ligament return to sport after injury scale (ACL-RSI)—validity and reliability. J Sports Sci. 2017;35(4):393–401.
Tajdini H, Letafatkar A, Brewer BW, Hosseinzadeh M. Association between kinesiophobia and gait asymmetry after ACL reconstruction: implications for prevention of reinjury. Int J Environ Res Public Health. 2021;18(6):3264.
Tengman E, Brax Olofsson L, Nilsson KG, Tegner Y, Lundgren L, Häger CK. Anterior cruciate ligament injury after more than 20 years: I. Physical activity level and knee function. Scand J Med Sci Sports. 2014;24(6):e491-500.
Theunissen W, van der Steen MC, Liu WY, Janssen RPA. Timing of anterior cruciate ligament reconstruction and preoperative pain are important predictors for postoperative kinesiophobia. Knee Surg Sports Traumatol Arthrosc. 2020;28(8):2502–10.
Thomeé P, Währborg P, Börjesson M, Thomeé R, Eriksson B, Karlsson J. Self-efficacy of knee function as a pre-operative predictor of outcome 1 year after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008;16(2):118–27.
Thomeé P, Währborg P, Börjesson M, Thomeé R, Eriksson BI, Karlsson J. A randomized, controlled study of a rehabilitation model to improve knee-function self-efficacy with ACL injury. J Sport Rehabil. 2010;19(2):200–13.
Thomeé P, Währborg P, Börjesson M, Thomeé R, Eriksson BI, Karlsson J. Determinants of self-efficacy in the rehabilitation of patients with anterior cruciate ligament injury. J Rehabil Med. 2007;39(6):486–92.
Tortoli E, Francini L, Giovannico G, Ramponi C. Translation, cross-cultural adaptation and validation of the Italian version of the anterior cruciate ligament-return to sport after injury (ACL-RSI) scale. Knee Surg Sports Traumatol Arthrosc. 2020;1:1–7.
Trigsted SM, Cook DB, Pickett KA, Cadmus-Bertram L, Dunn WR, Bell DR. Greater fear of reinjury is related to stiffened jump-landing biomechanics and muscle activation in women after ACL reconstruction. Knee Surg Sport Traumatol Arthrosc. 2018;26(12):3682–9.
Tripp DA, Stanish W, Ebel-Lam A, Brewer BW, Birchard J. Fear of reinjury, negative affect, and catastrophizing predicting return to sport in recreational athletes with anterior cruciate ligament injuries at 1 year postsurgery. Rehabil Psychol. 2007;52(1):74–81.
Üşen A, Tolu S. Factors affecting the femoral cartilage thickness after anterior cruciate ligament reconstruction. Indian J Orthop. 2021;55(2):352–9.
van Lankveld W, van Melick N, Habets B, Pronk Y, Staal JB, van Cingel R. Cross-cultural adaptation and measurement properties of the Dutch knee self efficacy scale (K-SES). BMC Sports Sci Med Rehabil. 2019;11:3.
van Melick N, Pronk Y, Nijhuis-van der Sanden M, Rutten S, van Tienen T, Hoogeboom T. Meeting movement quantity or quality return to sport criteria is associated with reduced second ACL injury rate. J Orthop Res. 2021;40(1):117–28.
Van Wyngaarden JJ, Jacobs C, Thompson K, Eads M, Johnson D, Ireland ML, et al. Quadriceps strength and kinesiophobia predict long-term function after ACL reconstruction: a cross-sectional pilot study. Sports Health. 2021;13(3):251–7.
Zaffagnini S, Russo RL, Marcheggiani Muccioli GM, Marcacci M. The Videoinsight® method: improving rehabilitation following anterior cruciate ligament reconstruction—a preliminary study. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):851–8.
Ueda Y, Matsushita T, Shibata Y, Takiguchi K, Ono K, Kida A, et al. Satisfaction with playing pre-injury sports 1 year after anterior cruciate ligament reconstruction using a hamstring autograft. Knee. 2021;33:282–9.
Barchek AR, Dlugonski D, Baez SE, Hoch MC, Hoch J. The relationship between injury-related fear and physical activity in people with a history of anterior cruciate ligament reconstruction. Phys Ther Sport. 2021;50:201–5.
Baez S, Cormier M, Andreatta R, Gribble P, Hoch JM. Implementation of In vivo exposure therapy to decrease injury-related fear in females with a history of ACL-reconstruction: a pilot study. Phys Ther Spoer. 2021;52:217–23.
Levinger P, Hallam K, Fraser D, Pile R, Ardern C, Moreira B, et al. A novel web-support intervention to promote recovery following anterior cruciate ligament reconstruction: a pilot randomised controlled trial. Phys Ther Sport. 2017;27:29–37.
George SZ, Lentz TA, Zeppieri G, Lee D, Chmielewski TL. Analysis of shortened versions of the tampa scale for kinesiophobia and pain catastrophizing scale for patients after anterior cruciate ligament reconstruction. Clin J Pain. 2012;28(1):73–80.
Woby SR, Roach NK, Urmston M, Watson PJ. Psychometric properties of the TSK-11: a shortened version of the Tampa Scale for Kinesiophobia. Pain. 2005;117(1–2):137–44.
Olds M, Webster KE. Factor structure of the shoulder instability return to sport after injury scale: performance confidence, reinjury fear and risk, emotions, rehabilitation and surgery. Am J Sport Med. 2021;49(10):2737–42.
Olsson N, Karlsson J, Eriksson B, Brorsson A, Lundberg M, Silbernagel K. A bility to perform a single heel-rise is significantly related to patient-reported outcome after A chilles tendon rupture. Scand J Med Sci Sport. 2014;24(1):152–8.
Brewer BW, Van Raalte JL, Cornelius AE. An interactive cognitive-behavioural multimedia program favourably affects pain and kinesiophobia during rehabilitation after anterior cruciate ligament surgery: an effectiveness trial. Int J Sport Exerc Psychol. 2021:1:1–23.
Priore LB, Lack S, Garcia C, Azevedo FM, de Oliveira SD. Two weeks of wearing a knee brace compared with minimal intervention on kinesiophobia at 2 and 6 weeks in people with patellofemoral pain: a randomized controlled trial. Arch Phys Med Rehabil. 2020;101(4):613–23.
Cai L, Gao H, Xu H, Wang Y, Lyu P, Liu Y. Does a program based on cognitive behavioral therapy affect kinesiophobia in patients following total knee arthroplasty? A randomized, controlled trial with a 6-month follow-up. J Arthroplast. 2018;33(3):704–10.
Sanchis-Alfonso V, Montesinos-Berry E, Monllau JC, Merchant AC. Results of isolated lateral retinacular reconstruction for iatrogenic medial patellar instability. Arthroscopy. 2015;31(3):422–7.
Flanigan DC, Everhart JS, Pedroza A, Smith T, Kaeding CC. Fear of reinjury (kinesiophobia) and persistent knee symptoms are common factors for lack of return to sport after anterior cruciate ligament reconstruction. Arthroscopy. 2013;29(8):1322–9.
George SZ, Fritz JM, Childs JD. Investigation of elevated fear-avoidance beliefs for patients with low back pain: a secondary analysis involving patients enrolled in physical therapy clinical trials. J Orthop Sport Phys Ther. 2008;38(2):50–8.
Sonesson S, Kvist J, Ardern C, Österberg A, Silbernagel KG. Psychological factors are important to return to pre-injury sport activity after anterior cruciate ligament reconstruction: expect and motivate to satisfy. Knee Surg Sport Traumatol Arthrosc. 2017;25(5):1375–84.
Mansfield CB, Selhorst M. The effects of fear-avoidance beliefs on anterior knee pain and physical therapy visit count for young individuals: a retrospective study. Phys Ther Sport. 2018;34:187–91.
Williamson E. Fear avoidance beliefs questionnaire (FABQ). Aust J Physiother. 2006;52(2):149.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
GSC was supported by the NIHR Biomedical Research Centre, Oxford, and Cancer Research UK (programme grant: C49297/A27294). SRF is funded by a National Health and Medical Research Council (NHMRC) Investigator Grant (#1194428).
Conflicts of interests and competing interests
Garrett Scott Bullock, Tim Sell, Ryan Zerega, Charles Reiter, Victoria King, Hailey Wrona, Nilani Mills, Charlotte Ganderton, Steven Duhig, Anu Räisäsen, Leila Ledbetter, Gary S. Collins, Joanna Kvist and Stephanie R. Filbay declare that they have no conflicts of interest relevant to the content of this review.
Availability of data and material
None.
Code availability
Not applicable.
Authors’ contributions
GSB, TCS, JK, SRF conceived the study idea. GSB, TCS, GSC, LL, JK, SRF were involved in design and planning. GB, RZ, CR, VK, SD, HW, NM, CG, AR screened articles and assessed risk of bias. GB, RZ, CR, VK, HW, SD, NM, CG, AR performed data extraction. GSB, SRF wrote the first draft of the manuscript. GSB, TCS, RZ, CR, VK, HW, NM, CG, SD, AR, LL, GSC, JK, SRF critically revised the manuscript. GSB, TCS, RZ, CR, VK, HW, NM, CG, SD, AR, LL, GSC, JK, SRF approved the final version of the manuscript. All authors read and approved the final manuscript.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Patient public involvement
Five authors are researchers and clinicians who treat anterior cruciate ligament (ACL) injury patients, and four authors are researchers who have sustained ACL injuries and have undergone ACL rehabilitation and surgery. A series of symposiums are planned at various sports medicine conferences to help further educate clinicians on this topic.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bullock, G.S., Sell, T.C., Zarega, R. et al. Kinesiophobia, Knee Self-Efficacy, and Fear Avoidance Beliefs in People with ACL Injury: A Systematic Review and Meta-Analysis. Sports Med 52, 3001–3019 (2022). https://doi.org/10.1007/s40279-022-01739-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-022-01739-3