Abstract
Background
Overuse injuries are common in sporting children and adolescents. These injuries are a particular concern when they involve the epiphyseal–physeal–metaphyseal (EPM) complex given their potential to disturb skeletal growth. Specifically, the limits of mechanical tolerance of the EPM complex to repetitive stress may be exceeded by the intense and continuous training characteristic of many youth sports today.
Objective
This article describes the present status of knowledge on the occurrence and outcome of primary periphyseal stress injuries (PPSIs) affecting the EPM complex in the extremities of children and adolescents involved in youth sports.
Methods
A comprehensive review of the sports medicine literature was conducted to determine the nature and extent of PPSIs affecting the EPM complex of the extremities among youth sports participants and the potential for consequent skeletal growth disturbance and resultant limb deformity associated with these injuries.
Results
Our initial search uncovered 128 original published scientific articles reporting relevant data on PPSIs. There were 101 case reports/series, 19 cross-sectional, 1 case–control, and 7 cohort studies with relevant data. The case reports/series studies reported 448 patients with PPSIs involving the extremities. Children and adolescents representing a variety of high impact repetitive youth sports activities—including baseball, badminton, climbing, cricket, dance, gymnastics, rugby, soccer, swimming, tennis, and volleyball—may sustain PPSIs involving the shoulder, elbow, hand and wrist, knee, and ankle and foot. Although incidence data from prospective cohort studies are lacking, data arising from cross-sectional studies suggest that PPSIs may be common in select groups of youth athletes—including the shoulder in baseball players (0–36.6%), wrist in gymnasts (10–83%) and platform divers (52.6%), and fingers in rock climbers (5–58%). Notably, not all stress-related skeletal changes detected on imaging were symptomatic in these studies. When diagnosed and treated with an appropriate period of rest and rehabilitation, most patients studied were able to return to their sport activities. However, our data also show that 57/448 PPSIs (12.7%) produced growth disturbance, and that 28/448 patients (6.2%) underwent surgery for their injuries. Absence of treatment, delayed presentation and diagnosis, and non-compliance with a rest regimen were common in cases that produced growth disturbance.
Conclusions
PPSIs may affect the extremities of children and adolescents engaged in a variety of youth sports, especially at advanced levels of training and competition. Most skeletally immature patients with PPSIs respond well to timely treatment; however, in extreme cases, PPSIs can progress to produce skeletal growth disruption which may necessitate surgical intervention. Clearly, establishing the early diagnosis of PPSIs and providing timely treatment of these injuries are needed to ensure the skeletal health of youth sports participants. Rigorous prospective longitudinal epidemiological and imaging studies designed to provide incidence rates of PPSIs and to determine the effect of PPSIs on long-term skeletal health are also necessary.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Participants in a variety of youth sports and high impact repetitive activities may sustain PPSIs involving the shoulder, elbow, hand and wrist, knee, ankle and foot. |
Most PPSIs respond well to timely treatment. However, in the absence of proper treatment, some of these injuries progress to partial or complete premature physeal closure and limb deformity. |
Rigorous prospective longitudinal epidemiological and imaging studies of youth sports participants designed to provide incidence rates of PPSI and to determine the effect of PPSIs on skeletal health are necessary. |
1 Background
Participation in youth sports is increasingly popular for children and adolescents. Trends in youth sports over recent decades include increased duration and intensity of physical loading, earlier specialization and year-round training, and increased difficulty of skills practiced [1]. In addition to traditional sports, children and adolescents are increasingly visiting wilderness recreational destinations and participating in a growing number of adventure and extreme sports [2].
Today, intensive specialized sport training is often initiated at an early age when skeletal growth is still ongoing [3, 4]. It is not uncommon, for example, for children as young as 6–8 years of age to play organized hockey or soccer and travel with select teams to compete in other towns and communities [4]. Similarly, young athletes, ages 12–13 years, may train 15–20 h/week rock climbing or skate-boarding, or at regional training centers in sports such as tennis or gymnastics [4, 5].
Incentive for advanced training and competition for elite youth athletes is provided by international sporting federations [6]. For example, the International Olympic Committee recently introduced Youth Olympic Games for young athletes, ages 14–18, including adventure and extreme sports such as mountain biking and sport climbing [6, 7]. Mass media showcasing these sports are also helping to drive their popularity among youth.
The benefits for youth who engage in regular physical activity and sport include improved bone health, weight status, cardiorespiratory and muscular fitness, cognitive function, and a reduced risk of depression [8]. The potential benefits of ongoing sport participation in youth also include improved self-esteem, motor coordination, and social skills [9]. Nevertheless, year-round participation in youth sports which involves high levels of repetitive training fosters an environment where overuse injuries are likely to occur [10]. This may be especially true at the elite level given the intensive training programs and high-frequency participation in sporting events [4, 5, 11, 12].
Overuse injuries are common in youth sports and can counter the beneficial effects of sports participation at a young age if a child or adolescent is unable to participate because of the residual effects from prior injury [13, 14]. The concern is that the limit for mechanical tolerance of growing bones may be exceeded by the intense and continuous training characteristic of many youth sports today [15]. Overuse injuries of the extremities are a particular concern given the potential for growth disruption and resultant deformity of long bones, especially during periods of rapid growth [10, 15,16,17]. Since overuse injuries may involve one or more constituents of the epiphyseal–physeal–metaphyseal (EPM) complex [18, 19], it makes sense to collectively refer to these injuries as primary periphyseal stress injuries (PPSIs).
Parents want to know whether a given sport is safe for their children. Indeed, children and adolescents and everyone who works with them, whether they are parents, coaches, or medical personnel—including consultants, general practitioners, junior doctors, and medical students—need to have a better understanding of the extent of PPSI occurrence in youth athletes and the potential for skeletal growth disturbance associated with these injuries. This article describes the present status of knowledge on the occurrence and outcome of PPSIs affecting children and adolescents involved in youth sports.
2 Methods
A systematic review of the literature was performed applying the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines [20] (Fig. 1). The primary reference source for this study was the electronic database SCOPUS, which includes Medline and CINAHL databases. The literature search was limited to published, peer-reviewed reports—including case series and data arising from injury registries (> 4 cases), cross-sectional, case–control, and cohort studies—and involved the following search terms as well as extensive cross-referencing: growth plate injury, physeal injury, epiphyseal injury, epiphyseal plate injury, and metaphyseal injury in combination with athletic injuries, youth sports, injury, and injuries. Each title was searched manually for any focus on stress-related injuries involving one or more constituent parts of the EPM complex of the long bones in youth athletes. Only English-language articles published in peer-reviewed journals with an emphasis on human participants were initially included. Titles focusing on sport-related apophyseal injuries and those isolated to the cortex of the metaphysis or diaphysis were excluded. The reference lists of selected articles were manually searched using the same criteria. Based on these search criteria, 2530 articles were identified and 85 additional records were identified through other sources. Using the PRISMA guidelines [20], studies were selected based on appropriateness of topic and full-text options. The literature search was finalized on 10 January 2021 and yielded 128 articles which included data relevant to the study question (Fig. 1).
3 Results
Of 128 original published scientific articles reporting with relevant data on PPSIs, 101 were case reports and case series involving the upper and lower extremities of youth athletes. Further search uncovered 19 cross-sectional, 1 case–control, and 7 cohort studies with relevant data. Notably, there is a general pattern of increased number of original PPSI reports (case, cross-sectional, cohort) published per decade between 1950 and 2019 (Fig. 2). A description of our study results relative to study design is provided below prefaced by a review of current knowledge regarding the pathomechanism of PPSIs.
3.1 Pathomechanism
PPSIs can develop following repetitive submaximal stress causing microtrauma to one or more constituents of the EPM complex, particularly at the end of a long bone [21,22,23,24]. While the precise nature of chronic microtrauma in these injuries depends on their anatomical location, sport, and offending action, the forces tend to include one or more repetitive compressive, rotational, traction, tension, and/or shearing strains (see Table 1).
The most common radiographic or magnetic resonance imaging (MRI) finding is widening of the physis (Fig. 3) [21]. Initially, this injury was believed to be a stress reaction or stress fracture through the primary physis [25, 26]. In reality, the stress-related epiphyseal plate widening observed on imaging in the pediatric patient begins in the metaphysis with disruption of the normal metaphyseal blood supply [18, 21, 23, 27]. This metaphyseal stress injury is theorized to occur through repetitive loading, which alters metaphyseal perfusion and, in so doing, interferes with the apoptosis of the hypertrophied chondrocytes, which typically occurs in the zone of provisional calcification [18, 21, 22].
15-year-7-month-old boy who is a football place kicker. Reproduced from Laor et al. [21], with permission. A Frontal radiograph of right knee shows broad band of physeal widening of lateral aspect of distal femoral physis (arrow). B Corresponding coronal fast spin-echo proton density-weighted image with fat saturation shows broad area of lateral physeal widening of distal femur (arrow). Signal is isointense to that of rest of physis. C Frontal radiograph obtained 3 months after immobilization shows near-complete normalization of physeal widening
The hypertrophic zone and, by extension the physis, continue to widen because of ongoing growth in the germinal and proliferative zones [18]. These insults are reproduced in experimental animal models by the disruption of metaphyseal blood flow [23], and in skeletally immature children who participate in high-level sports and sustain repetitive trauma [27]. The resulting physeal widening, although it may mimic a non-displaced Salter–Harris type I fracture, is not a true fracture [21, 28]. On magnetic resonance imaging (MRI), there is no discontinuity or fluid-like signal intensity cleavage plane through the physeal cartilage to suggest fracture [21, 23].
The widening of the growth plate within the hypertrophic zone is usually reversible once normal metaphyseal perfusion is restored, as the resting and dividing cellular layers of the growth plate, and the attendant epiphyseal and metaphyseal blood supplies, are essentially undisturbed [21]. However, if metaphyseal stress injuries are undiagnosed or sub-optimally treated, progressive mechanical insults may lead to stress fractures involving one or more components of the EPM complex, especially if training is continued [16, 17, 24]. Although these injuries may eventually produce Salter–Harris type fracture patterns [29], their hallmark is a gradual onset of clinical symptoms [15,16,17].
In some instances, metaphyseal stress injuries and stress fractures involving the EPM complex may involve injury of the epiphysis and adjoining portion of the growth plate, which explains the reported cases of permanent growth arrest and long-term deformity [15,16,17, 21, 24]. In these injuries, damage to the epiphyseal-sided vessels may harmfully affect the resting or germinal zone of the physis which provides a ready stock of chondrocytes for the physis [28]. This injury may be localized and cause asymmetric growth, or it may involve the entire physis and cause a reduction in the rate of growth or complete cessation of further growth [21, 24]. In either case, premature closure and deformity of some or all of the physis may occur [21, 24].
3.2 Case Reports/Series
Case reports and case series are numerator-based study designs and therefore cannot be used to generate incidence rates of PPSIs. However, they can provide useful information as to the existence and relative frequency of this condition, preferred or successful treatments, and clinical outcome. They can also provide important insights into injury etiology that are useful for injury prevention work [30]. Case data on PPSIs are discussed below relative to body location.
3.2.1 Shoulder
Baseball pitchers were the first youth athletes in whom a PPSI was reported. An overuse condition that affects the proximal humeral physis of the throwing arm of skeletally immature youth baseball pitchers, “Little Leaguer’s Shoulder (LLS),” was first described in 1953 by Dotter [25]. LLS is believed to stem from chronic repetitive micro-traumatic shear, torque, or traction forces imposed on the unossified cartilage of the proximal humeral physis [31]. Classic radiographic findings of LLS can include physeal widening of the proximal humeral physis, sclerosis of the proximal humeral metaphysis, and fragmentation of the lateral aspect of the proximal humeral metaphysis [32] (Fig. 4).
Little Leaguer’s shoulder. A, B Frontal radiograph of the symptomatic right shoulder from a 13-year-old boy who is a baseball pitcher and with 3 months of symptoms shows asymmetric widening (arrow) of the lateral portion of proximal humeral physis when compared to the normal medial portion (arrowhead). Note the subtle subjacent metaphyseal sclerosis of the right shoulder, which is asymmetric when compared to the asymptomatic left shoulder (B). C Oblique coronal T2-weighted image from a 15-year-old boy who is also a baseball pitcher and with acute on chronic symptoms shows focal physeal widening centrally (arrow) when compared to the more normal appearance of the peripheral physis (arrowhead). Note the reconstituted zone of provisional calcification (chevron) that reflects healing changes in response to conservative treatment (cessation of overhead throwing)
Overall, there were 33 case reports and series describing 197 cases of LLS in youth athletes, ages 10–19 years [25, 31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61]. While most commonly reported in male baseball pitchers, LLS also occurs in females [31, 57, 60, 61] and other baseball positions [31, 40, 45, 51, 53]. These injuries have also been reported in other overhead sports including badminton [54], cricket [56], football [48], gymnastics [57,58,59], tennis [31, 46], swimming, and volleyball [60, 61]. There is also a reported case of bilateral physeal stress lesions of the proximal clavicular physis in a skeletally immature male gymnast [62].
Notably, a case series study at a high-volume regional children’s hospital reported an annual increase in the number of patients diagnosed with LLS over a 14-year period [31], with a significant increasing trend in the presentation of patients diagnosed with LLS during 1999–2013 (P = 0.02). Specifically, the incidence of LLS, a reflection of the volume of LLS relative to overall departmental and divisional patient volume, increased approximately 8% per year on average (annual percentage change = 8.5; 95% CI 5.5–11.6) [31].
In the studies reviewed, treatment of LLS was conservative in all but one subject [37] who underwent an arthroscopic procedure to remove loose bodies related to avascular necrosis of the proximal humerus. Treatment generally involved rest from the exacerbating activity, including time off from the sport followed by a gradual return to activity. Several studies reported that injured players were encouraged not to pitch again until their physes have closed [33, 34, 56]. Physical therapy was prescribed to improve strength and throwing mechanics in some patients [2, 47, 49, 50, 53, 58]. The recommended length of rest typically varied from 6 weeks to 3 months, with full resolution of symptoms ranging from 6 weeks to 12 months. In several cases, the patient returned to a different position or sport [37, 43, 56]. Notably, a report of 95 patients with LLS found that the average time to full resolution of symptoms was 2.6 months, with an average time to return to competition of 4.2 months [31].
3.2.2 Elbow
Eight studies reported 22 PPSIs of the distal humerus and proximal radius involving 6 males, 10 females, and 6 males or females, ages 7–18 years [63,64,65,66,67,68,69,70]. Six of the eight studies [65,66,67,68,69,70] reported on injured gymnasts, whereas two studies [63, 64] involved baseball players.
PPSIs involving the longitudinal growth centers of the elbow were first reported in 1975 by Ellman [63] who documented angulation deformity of the radial head in four male baseball players. This injury was believed to reflect underlying growth disturbance involving the growth plate of the head of the radius which occurred following lateral compression forces arising from repetitive baseball throwing [63].
PPSIs involving the proximal radius have also been reported in 21 male and 21 female artistic gymnasts [65,66,67,68,69,70]. In gymnastics, full extension loading exercises cause maximal compressive forces to be transmitted through the lateral aspect of the radial head which can lead to depression and eventually partial growth arrest and stress fracture (Salter–Harris type IV/V) of the antero-lateral aspects of the proximal radius [66, 70].
Injury to the distal humerus of a skeletally immature baseball player was first reported by Podestra et al. [64] who treated a 7-year-old baseball player with distal humeral epiphyseal separation from excessive repetitive throwing. Oda et al. [68] reported an 11-year-old male gymnast with chronic slipping of the distal humeral epiphyses bilaterally. In this patient, it was believed that the repetitive biomechanical loading on the elbows during the vault induced injury to the growth plate bilaterally, with chronic progression to separation of the distal humeral epiphyses [68].
Conservative management was provided in 12 of 22 patients with elbow PPSIs that involved rest with or without long-arm casting, upper extremity weight-bearing restrictions, and physical therapy, with gradual return to former levels of activity in 6–12 weeks [63,64,65,66,67,68,69,70]. Ten patients underwent surgery including arthrotomy [63], reduction and internal fixation of the growth plate [63, 65, 69, 70], tension band wiring [68], excision of the radial head [63, 66], and proximal radial osteotomy [63]. Although 7 studies reported follow-up of injured athletes [63,64,65, 67,68,69,70], only 4 studies reported return to activity data, which ranged from 8 weeks to 8 months [64, 67, 69, 70]. Three studies reported 7 injured athletes withdrew from gymnasts pursuant to injury [65, 66, 70].
Five studies reported postsurgical follow-up time, which ranged from 0 to 120 months [63, 65, 68,69,70]. However, return to activity data for surgically managed athletes was sparse. Only 3 studies indicated whether the gymnasts actually returned to their sport [65, 69, 70]. In these studies, 4 patients continued with gymnastics [65, 69] and 3 retired from gymnastics [65, 70].
3.2.3 Wrist
Overall, there were 28 case reports and series describing 98 patients with PPSIs involving the distal radius and, infrequently, the ulna in young athletes, ages 10–22 years [71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97]. Both female (n = 65) and male (n = 33) athletes were involved. With the exception of three cases—in badminton, climbing, and break dancing [71,72,73]—the PPSIs involved the distal radius of female and male gymnasts [74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97]. This is perhaps not surprising given the repetitive compressive and rotational forces on the forearm in this sport and the greater cross-sectional area of the distal radius compared to the distal ulna. In the neutral position with neutral ulnar variance, 80% of axial loads are borne by the radius and 20% by the ulna [96]. In children and adolescents, the ulna tends to be relatively shorter than the radius at the carpus (i.e., ulnar-negative), which drastically increases the load on the distal radius [95]. In gymnasts, the result is disproportionate loading of the epiphysis and primary physis of the distal radius [19, 81].
Stress injuries affecting the distal radius of gymnasts were first reported in 1981 by Read [74] who treated stress fractures of the epiphysis and metaphysis in the distal radius of three female gymnasts, ages 12–16. In 1985, Roy et al. [26] described a stress reaction involving the distal radial growth plate in a series of male and female gymnasts, ages 10–17. Radiographic criteria included: widening of the growth plate, cystic changes of the metaphyseal aspect along the growth plate, a beaked distal volar and radial aspect of the physis, and haziness within the usually radiolucent area of the growth plate (Fig. 5) [26]. Following the early studies by Read [74] and Roy et al. [26], multiple case reports/case series studied this injury in young female and male gymnasts [75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97]. PPSIs of the distal radius in gymnasts are often referred to as “Gymnast wrist” [84, 87, 88, 96,97,98].
Gymnast wrist. A Radiograph and B line drawing of the wrist in a symptomatic female gymnast with findings of widening of the distal radial physis, and cystic changes and irregularity of the metaphyseal margin. Reproduced from Roy et al. [26], with permission
Management of wrist PPSIs has typically been conservative, involving rest from the exacerbating activity until resolution of symptoms and radiographic evidence of healing. Treatments prescribed to stabilize or otherwise immobilize the wrist joint included wrist taping [93], bracing [72, 94], splinting [85, 89], and use of a cast (e.g., short-spica cast, short arm cast, and palm-to-elbow cast) [71, 73, 75, 79, 82]. The rehabilitation programs employed in some patients aimed to improve strength and mobility [26, 76, 89]. Following appropriate rest and rehabilitation, the vast majority of patients were able to return to their sport. Time to recovery was reported in some studies and ranged from 1 week to 12 months [26, 71,72,73,74,75,76,77, 79, 82, 85, 87]. Several studies [74, 84, 87, 92] reported patients (n = 8) who dropped out of gymnastics pursuant to PPSI of the distal radius.
Surgery was performed on nine gymnasts and involved removal of loose bodies from the wrist in one patient [76], arthroscopic procedures with debridement of the torn portion of the triangular fibrocartilage complex (TFCC) in 1 patient [87], ulnar arthroplasty in 2 patients [80, 84], distal ulnar recession in 2 patients [84], and ulna shortening osteotomy in 3 patients [81, 87, 92]. Postoperatively, 5 of 9 gymnasts were able to return to full gymnastics activity within 4 weeks to 15 months. [76, 81, 84, 87]. Return to activity information was not provided for 3 patients [76, 80, 87], including one report which noted that the ulna shortening osteotomy was unsuccessful [87].
3.2.4 Hand/Fingers
Overall, there were 11 case reports and series describing 80 patients, including 65 males and 15 females, ages 11–17, with PPSIs involving the hand and fingers [16, 17, 72, 95, 99,100,101,102,103,104,105]. With the exception of 2 patients, both gymnasts [95], the remaining PPSIs involved the fingers of rock climbers. There was also one case of physeal growth arrest of the distal phalanx of the thumb in a skeletally immature pianist, presumably caused by accumulated repetitive trauma incurred during years of piano playing [106].
In addition to their observation of PPSIs involving the distal radius of skeletally immature female gymnasts, Dwek et al. [95] observed osseous abnormalities of the metacarpal heads in two gymnasts, including flattening and irregularities of the overlying articular surface. Dwek et al. [95] suggested that these findings were typical of avascular necrosis of the metacarpal head, likely from chronic impaction across the metacarpophalangeal joints during gymnastics [95].
Among reports of injuries involving climbers, the most frequent PPSI reported was a stress-related Salter–Harris type III fracture at the dorsal aspect of the middle phalanx, with injury to the middle finger being most common followed by the ring finger [16, 17, 101, 104, 105]. This injury distribution is supported by a biomechanical analysis during climbing, which reveals that the most significant fingertip forces are applied by the middle finger [107, 108].
Epiphyseal stress fracture of the finger phalanges among sport climbers is a climbing-specific injury which was first described by Hochholzer et al. [99] and Chell et al. [100]. Since then, there have been multiple case reports/series studies of this injury [16, 17, 72, 99,100,101,102,103,104,105]. PPSI may be a common injury in youth climbers who have finger pain. In one study, 14 of 20 youth (≥ 14 years of age) who presented with symptoms related to climbing showed an epiphyseal fatigue fracture on MRI, including one with bilateral injury [102].
One possible mechanism for epiphyseal fractures in the phalanges of young climbers could be the development of chronic microfractures on the dorsal epiphysis, because when the finger is flexed during climbing, particularly during crimping, maximum pressure is placed on the base of the middle phalanx [17]. During crimping, there is a translation of the base of the middle phalanx in relation to the head of the proximal phalanx [16]. This translation decreases the joint’s congruence and joint contact area and shifts the point of maximum pressure more dorsally, leading to an increased risk of PPSI [16, 109].
Treatment of the fingers was almost always conservative if the fracture was not widely displaced [16, 17, 101,102,103, 106, 107]. Most authors recommended an early functional treatment without immobilization for about 6–8 weeks [16, 17, 101, 104, 107]. Patients used their hands for daily living activities but refrained from any hand-related sport (not only climbing but also gymnastics, handball, volleyball, etc.) and manual work/labor. Two studies reported the use of finger splints for 2–3 weeks with good results [17, 72]. After clinical and radiographic/ultrasound assessment, gradual restart of sport-specific activities resumed after 8–12 weeks with good results [16, 17, 99, 101, 102, 105, 107]. Notably, patients experienced better results if treatment, including cessation of activity, began immediately after the onset of symptoms [16, 17].
Surgical treatment for repetitive stress-related fracture nonunion was performed in two climbers using a spot drilling epiphysiodesis technique. Both patients went on to fracture union after surgery, without complications, and returned to sport climbing within 3 months of treatment [104].
3.2.5 Knee
Overall, there were 13 case reports/series describing 26 patients, including 17 males and 9 females, ages 8–15, with PPSIs involving the distal femur, proximal tibia, or proximal fibula [21, 88, 110,111,112,113,114,115,116,117,118,119,120,121]. These injuries are believed to result from repeated compression, rotational, shearing, valgus, or varus forces on the knee ensuing from repetitive trauma during sports activities [110, 118, 120, 121]. Patients represented a wide range of youth sports including baseball [88], basketball [21, 110, 111], football [21], gymnastics [11, 21, 113], rugby [118], softball, running [119], soccer [21, 120], tennis [21, 121], as well as engagement in multiple sports [114,115,116]. There was also a report of one patient who participated in recreational sports only [117].
In most instances, imaging of knee PPSIs revealed metaphyseal stress injury of the distal femur and/or proximal tibia, including physeal widening and metaphyseal irregularities [21, 112,113,114,115, 117,118,119, 121] (Fig. 3). One study reported four patients—a gymnast, soccer player, and two multisport athletes—with stress injury of the proximal tibial epiphysis [116].
Management was generally conservative, and involved strict rest from the exacerbating activity with/without immobilization followed by gradual return to activity [21, 112, 116, 119, 121]. In some patients, restriction of movement was facilitated with the use of crutches [114], knee immobilizers [21, 112], or a long leg cast [21]. The duration of rest and gradual return to sport ranged from 4 to 20 weeks depending on the severity of the injury. One patient, who was noncompliant, developed varus deformity of the knees and had persistent knee pain at 4 year follow-up [21].
Surgery was performed in 7 patients [110, 111, 118, 120], which included exploratory surgery for premature closure of the lateral aspect of the right proximal tibial growth plate [110], correction of recurvatum, and valgus alignment of the knee arising from asymmetric premature closure of the proximal tibial growth plate [111], varus opening wedge osteotomy to restore the alignment of the proximal tibia [118], hemiepiphysiodesis with insertion of a medial tension band plate for guided growth and gradual correction of the deformity, and lateral distal femoral opening wedge osteotomy [120]. Length of patient follow-up ranged from 5 to 24 months during which time patients were able to return to their sporting activity [110, 118, 120]. One study reported excellent results 2 years post-surgery but did not indicate whether the 2 patients were able to return to their sport [111].
3.2.6 Ankle/Foot
Overall, 8 studies reported 25 PPSIs of the ankle and foot affecting youth athletes, ages 9–16 (2 males, 5 females, 18 M/F), involved in basketball [122], dance [123,124,125,126], dance/gymnastics [124], distance running [128], soccer [129], as well as those involved in multiple team sports [127].
Stress changes of the distal tibial physis were reported in a recreational dancer/gymnast [124] and in the distal tibia and/or fibula of 18 patients active in team sports such as soccer, basketball, and football [127].
Other PPSIs involved the feet and include the proximal first metatarsal in a basketball player, distance runner, and soccer player [122, 128, 129], second metatarsal in two dancers [123, 126], and a non-healing stress fracture of the proximal phalanges of the great toes in a ballet dancer [125].
Treatment was generally conservative and involved restriction of weight-bearing and gradual return to activity [122,123,124, 127, 128]. For some patients, treatment included shoe modification [122, 126], use of crutches [123], ankle cast followed by walking boot [124] ankle bracing [127], and physical therapy [129].
In one study [124], two dancers were able to return to activity without restrictions after 6 months, while in a second study, the dancer was not able to return to dancing until 13 months, but at a lower intensity [123].
Only one patient underwent surgery [125]. A ballet dancer underwent a closed reduction and Herbert screw insertion which was performed bilaterally to manage non-healing stress-induced fractures of the proximal phalanges of the great toes [125]. After 6 months, significant resolution of the symptoms and complete radiological union occurred, allowing a return to ballet training [125].
3.2.7 Bone Growth Disturbance
In the case reports/case series studies reviewed, there were 448 patients with PPSIs affecting the shoulder, elbow, wrist, hand/fingers, knee, and ankle and foot. Among these reports, there were 57 patients (12.7%) with radiographic evidence of bone growth disturbance involving the shoulder, elbow, wrist, hand and fingers, knee, foot and ankle [16, 17, 21, 40, 51, 58, 63, 65, 66, 70, 75, 80, 81, 84, 86, 87, 90, 92,93,94, 106, 110, 111, 118, 120, 123, 126] (Table 2). In these patients, the severity of the injury likely resulted from the absence of treatment, or delay in treatment, and/or non-compliance with treatment recommendations [21, 81, 102, 107].
Patients exhibiting PPSI growth-related complications represented a variety of sports including baseball [40, 51, 63], basketball [21, 110, 111], climbing [16, 17], dance [123, 126], football [21, 120], gymnastics [21, 58, 65, 66, 70, 75, 80, 81, 84, 86, 87, 90, 92,93,94], rugby [118], soccer [21, 120], and tennis [21] (Table 2).
Radiographic and/or MRI evidence of growth complications involving the proximal humerus includes varus and extension deformation [51] in a young baseball player and premature closure of the proximal humeral epiphysis in a baseball player and gymnast [58].
Radiographic and/or MRI evidence of growth complications following stress-related injury include flattening and anterior depression of the radial head epiphysis in baseball players [63] and gymnasts [65, 66, 70]. This growth disturbance likely occurred following physeal compression stresses, resulting in damage to the epiphyseal plate and subsequent angulation deformity [63, 66].
Numerous case reports provide radiographic and/or MRI evidence of growth disturbance at the distal radius [75, 80, 81, 84, 86, 87, 90, 92,93,94]. Chronic, untreated PPSI of the distal radius can lead to premature closure of the physis, resulting in growth arrest (Fig. 6). Serial radiographs show stress-related changes of the distal radial growth plate of the involved extremity, followed by the development of positive ulnar variance due to blunted growth or premature closure of the distal radial growth plate before that of the ulna [19, 92, 130, 131].
Fourteen-year-old female gymnast with chronic right wrist pain. Reproduced from Caine et al. [130], with permission. A Asymptomatic left wrist. B Symptomatic right wrist showing partial closure of the right distal radial physis, centrally and ulnarly, producing ulnar positive variance. The ulnar physis remains open
A Madelung or Madelung-like deformity (premature closure of the ulnar aspect of the distal radial growth plate) was described in three female gymnasts [80, 87, 93, 94]. Evidence of palmar and ulnar tilting of the distal radial articular surface, a mild form of Madelung-type deformity, has also been reported in several cases of skeletally immature gymnasts with PPSIs [26, 76, 81]. In one case involving a skeletally immature gymnast, radiographs showed widening of the radial aspect and premature closure of the ulnar aspect of the distal radial physis [90].
There are several instances of premature closure of the physis or deformities as a consequence of PPSIs that did not heal among skeletally immature climbers (Fig. 7) [16, 17]. In non-healing injuries, surgical spot drilling epiphysiodesis was performed [105]. The only other case report of growth disturbance in the finger, presumably as a consequence of repetitive loading, is in a piano player [106]. In this instance, it is likely that repeated contact at the radial aspect of the thumb results in tension and compression [106].
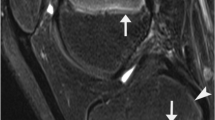
A 15-year-old climber with chronic pain in the proximal interphalangeal joint of his middle finger. A Radiograph and B sagittal magnetic resonance image of an old and malaligned growth plate fracture involving the middle phalanx of the middle finger. C A picture of the hand showing swelling and deformity of the proximal interphalangeal joint of the middle finger
There is radiographic and MRI evidence of stress-related growth disturbance, including secondary valgus and varus deformity involving the proximal tibia [21, 110, 111, 118] and distal femur [21, 120] in youth basketball, football, gymnastics, rugby, soccer, and tennis. The proximal tibia and distal femur contribute 55–70% to the growth of their respective bone, and thus, growth disturbance at these locations could result in substantial limb shortening or deformity [18, 21].
Radiographic and MRI evidence of PPSI-related bone growth disturbance in the feet has been reported in two female dancers [123, 126]. In a skeletally immature Flamenco dancer [123], serial radiographs over 13 months revealed premature closure and shortening of the second metatarsal. In the second dancer, radiographs and MRI revealed a shortened second metatarsal and premature growth plate closure. This growth disturbance likely occurred as a result of repetitive stress from dancing en pointe [126], whereas in the former patient, the premature closure likely resulted from repetitive vibratory stress, as the highest footplate pressures in Flamenco dance are exerted on the first and second metatarsal heads [132].
Information on treatment was unavailable for 5/57 patients who presented with bone growth disturbance, including 4 who dropped out [86, 87]. Treatment was conservative in 33 of 52 patients and involved rest from the offending activities and gradual return to activity. This was accomplished with the use of bracing [94], taping, [94], splinting [17], casting [21], crutches [120], knee immobilizers [21], physical rehabilitation [58], and pain-reducing modalities [93, 94].
Corrective surgery was performed in 19 patients [63, 65, 66, 81, 84, 92, 93, 110, 111, 118, 120]. Most patients were able to return to their sport within 2–36 months of surgery [81, 84, 87, 90, 110, 111, 118, 120]. Several athletes choose to retire after surgery or otherwise participate at a less competitive level [65, 70, 92]. Information on return to activity was not provided for several patients who underwent surgery [63, 66, 75, 80].
3.3 Cross-Sectional Studies
Table 3 summarizes the results of 19 imaging studies which provide prevalence estimates or comparative data on PPSIs involving the shoulder, wrist and fingers of baseball players [133,134,135], divers [136], gymnasts [26, 27, 137,138,139,140,141,142,143,144,145,146], and climbers [147,148,149,150,151]. Cross-sectional data are also provided in one case series study [26] and one case–control study [135]. Notably, none of the cross-sectional studies focused or otherwise reported on lower extremity PPSIs among skeletally immature athletes.
Perusal of Table 3 reveals a wide range of training and competitive levels including recreational athletes [133, 148], club-level competitive athletes [26, 134, 135, 139, 142,143,144, 149, 150], specialized training school [27, 141], and elite- or national-level competitive athletes [136,137,138, 140, 147,148,149,150]. Although prevalence estimates of PPSIs are reported in most of these studies, comparison of these studies is compromised by differences in how and whether symptoms were reported.
3.3.1 Unknown Symptomatology
In imaging studies which did not report current or past symptoms, the prevalence of radiographic abnormalities consistent with PPSIs ranged from 5 to 83% [27, 51, 135, 137, 139, 140, 148, 149]. Athletes in this category included baseball players (prevalence range 0–21.7%) [133, 135], divers (52.6%) [136], gymnasts (10–83%) [27, 137, 139, 140], and climbers (5–47%) [148, 149, 151]. Notably, the prevalence of stress reaction (e.g., subchondral sclerosis/increased thickness of physis) was greater in German Junior National Team (GJNT) climbers (47%) than recreational climbers (RC) (28%).
3.3.2 Proportion of Asymptomatic Cases with PPSIs
One study reported prevalence of radiographic abnormalities consistent with PPSIs in skeletally immature athletes who were asymptomatic [26]. Roy et al. [26] reported minimal widening and irregularity of the distal radial growth plate in 30.8% of asymptomatic club-level competitive gymnasts.
3.3.3 Proportion of Symptomatic Cases with PPSIs
Among skeletally immature athletes who were symptomatic (with positive history of pain and/or current pain), the prevalence of PPSI was 36.6% among youth baseball players [134], 58% among competitive youth climbers [150], and 72.4% among nationally ranked youth climbers [147].
3.3.4 Proportion of Prevalent PPSIs that were Symptomatic
Another approach has been to report the proportion of prevalent cases of PPSIs which were characterized by a positive history of related symptoms [142,143,144]. DiFiori et al. [142] reported a 25% prevalence of PPSIs among club-level gymnasts and that 81.8% (9/11) of these reported a history of wrist pain. However, a similar proportion of those without radiographic evidence of PPSI (25/33; 75.8%) also had wrist pain. In a follow-up study of competitive gymnasts, DiFiori et al. [143] reported a prevalence of 51% of stress injury to the distal radial physis of at least grade 2 (one or more of the following: cystic changes, metaphyseal sclerosis, striations, or beaking of the metaphysis). In this study, wrist pain prevalence was significantly related to the grade of radiographic injury. Finally, Guerra et al. [144] reported a 65% prevalence of wrist physeal injury among club-level competitive gymnasts; of these, 82% were symptomatic.
The healthy distal radial physis is characterized by a thin center surrounded by thicker borders [145]. Notably, Kraan et al. [145] reported that of the ten gymnasts with the highest distal radial physeal volumes in their study, nine were symptomatic. These results are consistent with those of Zhang et al. [136] who found a significantly greater thickness of the epiphyseal plate in skeletally immature divers with radiographic evidence of PPSI (Group A) compared to those without irregular widening (Group B), and with controls (Group C) (A > B > C; P = 0.0001).
Several cross-sectional studies provide further insight into the potential for growth disturbance and deformity associated with PPSI in select groups of skeletally immature athletes, with prevalence rates of PPSIs associated with growth disturbance ranging from 1.7 to 5.0% [27, 141, 147, 149].
Shih et al. [27] reported partial closure of the distal radial growth plate with bridge formation in the left radius of two (2/47; 4.3%) gymnasts. Chang et al. [141] reported three (3/176; 1.7%) Chinese Opera students who showed early partial closure of the distal radial physis. Notably, students with fused physes in this study had a mean ulnar variance which was significantly greater in gymnasts when compared to the control group (P < 0.05); 8.2% (14 of 170 wrists) had exceedingly large (> + 3 mm) ulnar positive variance [141].
Among youth climbers, Schlegel et al. [147] reported one patient (1/29;3.4%) with premature closure of the physis of the proximal phalanx of the thumb, while Garcia et al. [149] reported MRI evidence showing early transphyseal bone bridging in a skeletally immature climber (1/20;5%) which can lead to finger-shortening and angular deformities. Notably, Bartschi et al. [150] reported that among 16 youth climbers seen in their practice for epiphyseal pain between 2006 and 2018, and in whom the index injury was left untreated, 8 climbers (8/16; 50%) developed growth plate damage and articular surface incongruency with permanent impairment of the injured finger.
3.4 Cohort Studies
Compared to cross-sectional studies (numerator-based designs), prospective and historical studies (denominator-based designs) provide the best opportunity to provide data designed to answer the question regarding “how big is the problem?” Unfortunately, most cohort studies of injuries affecting youth athletes fail to provide details related to overuse injuries, particularly PPSI [152, 153].
Our review uncovered only a handful of cohort studies which reported data on PPSIs [5, 130, 154,155,156,157,158] (Table 4). In these studies, calculated clinical incidence of PPSIs was 4.4 per 100 athletes among baseball players [154], and ranged from 1.27–71.4 PPSIs per 100 athletes among gymnasts [130, 155,156,157], with the highest clinical incidence reported among elite-level gymnasts monitored regularly over 9 years [155]. Comparability of these results is compromised, however, since clinical incidence rates do not account for potential variation in exposure of participants to risk for injury [159]. Although Schöffl et al. [5, 158] reported only one PPSI in their follow-up studies of youth climbers, the clinical incidence of stress reaction of the fingers of GJNT members in these studies was 80 per 100 participants.
Based on their single-season shoulder MRI-based study of Little League baseball players, Holt et al. [154] reported that eight players (34.8%) had new or worsening findings on their post-season MRI when compared to preseason MRI. MRI findings included partial rotator cuff tear (5), proximal humeral periphyseal edema with physeal widening (1), labral tear (1), and acromioclavicular joint edema.
Four cohort studies report PPSIs sustained by competitive male and/or female gymnasts [130, 155,156,157]. Lishen and Jianhua [155] reported on injuries affecting elite Chinese gymnasts followed clinically and with routine radiography over nine years (1972–1980). During the follow-up period, 6 of 18 girls and 8 of 10 boys (14 patients total, including 6 with bilateral injuries = 20 wrists) developed progressive wrist pathology including periphyseal stress changes of the distal radial growth plate with accompanying decreased range of motion at the wrist. Eventually, radiographs revealed hindered radial growth and a relatively lengthened ulna, and findings of posttraumatic osteoarthritis (OA) in the wrist joints. However, the authors did not indicate the criteria for OA.
Caine et al. [156] reported 147 injuries affecting 50 U.S. club-level female gymnasts over 1 year. Dixon and Fricker [157] reported a total of 572 injuries affecting a total of 162 Australian elite male and female gymnasts over a 10-year period. Notably, chronic injuries represented 44.2% and 39.0% of all injuries in the U.S. and Australian gymnasts, respectively [156, 157].
Although the studies of American and Australian gymnasts reported on injuries affecting all body regions, only upper extremities PPSIs of female athletes were reported in these studies (4 and 3 PPSIs affecting the distal radius of American and Australian gymnasts, respectively). In contrast, Caine et al. [130] found only 1 PPSI in their 3-year study of club-level gymnasts. Notably, unlike their previous study [156], access to medical records of gymnasts was not provided in this study.
Two studies of youth climbers indicate that adaptive stress reactions in the fingers of competitive climbers are common [5, 158]. Schöffl et al. [158] conducted a 5-year radiographic follow-up study of GJNT and recreational rock climbers with data points in 1999 and 2004. Although adaptive stress reaction of the phalangeal periphyseal area was prevalent among recreational climbers on both occasions, only one climber developed a PPSI. No climbers in this study developed OA (as defined by a Kellgren–Lawrence grade ≥ 2).
In their 11-year follow-up of the GJNT rock climbers (2 data collection points: 1999 and 2011), Schöffl et al. [5] found that both of the PPSIs recorded in 1999 (one in the GJNT) had healed without consequences. In 2011, adaptive stress reactions were found in 12 of 15 (80%) of the GJNT compared to 15 of 19 (79%) of the GJNT in 1999. Signs of early stage OA were seen in 4/15 of the GJNT climbers (27%) in 2011 compared to 1/19 (5%) in 1999. Significant statistical association was found between the development of early onset OA and overall total training years (P = 0.024), use of campus board training in 1999 (P = 0.033), and climbing level (P = 0.030).
Data from several studies of youth climbers indicate an increase in proportion of finger PPSIs over time [102, 107, 109]. Over a 2-year period (2017–18). Lutter et al. [109] conducted a clinical follow-up study of injuries among 436 climbing patients. They compared these data with two prior study populations followed during 1998–2001 [107] and 2009–2012 [102] and found an increase in the proportion of finger PPSIs. Finger PPSIs were seen in 0.8% of cases between 1998 and 2001 [107], 3.4% of all cases during 2009–2012 [102], and were present in 7.3% of all finger injuries during 2017–2018 [109].
4 Discussion
4.1 Injury Occurrence
A primary purpose of this systematic review was to describe the present status of knowledge on the occurrence of PPSIs affecting children and adolescents involved in youth sports. Our review uncovered data from case reports and series, case–control, cross-sectional, and cohort studies which provide important information related to this question.
4.1.1 Case Reports/Series
Overall, our review includes 101 case reports/case series describing 448 patients with PPSIs involving the shoulder, elbow, hand and wrist, knee, ankle and foot. Most patients were male (73%), likely reflecting the greater participation of male than female patients, especially in baseball. Patients representing a variety of sports and high impact repetitive activities—including baseball, badminton, climbing, cricket, dance, gymnastics, rugby, soccer, swimming, tennis, and volleyball—may sustain PPSIs. Although youth participating in advanced or elite-level sports appear particularly at risk, skeletally immature non-elite and recreational athletes were not spared from incurring PPSIs [5, 133, 142, 148, 158].
A limitation of case reports and case series is that these studies provide no information on the population at risk and therefore cannot be used to generate prevalence or incidence rates. However, the sheer volume of cases reported raises concern regarding the extent of PPSI occurrence among youth. A logical question follows: what is the rate of PPSI among skeletally immature athletes?
4.1.2 Cross-Sectional Studies
Results from cross-sectional studies (see Table 3) indicate a troubling prevalence of PPSIs in select groups of skeletally immature competitive athletes—including baseball players (shoulder: 0–36.6%), divers (wrist: 52.6%), gymnasts (wrist: 10–85%), and rock climbers (fingers: 17.2–58%). The only cross-sectional study reporting no patients with PPSI was a radiographic study of youth recreational pitchers [133]. Notably, no cross-sectional studies reported on PPSIs affecting the lower extremity of skeletally immature athletes.
The prevalence of PPSIs reported in the cross-sectional studies was variable depending on whether symptoms were unknown (5–83%), whether patients were asymptomatic (30.8–52.6%), or symptomatic (36.6–72.4%), and on the proportion of cases that were symptomatic (51–81.8%). Notably, not all youth with radiographic or MRI findings consistent with PPSI are necessarily symptomatic. Furthermore, this does not account for the fact that the presence or absence of “symptoms” is subjective, and athletes may under-report their symptoms due to concerns over the inability to continue their sport.
A limitation of the cross-sectional studies reviewed is that they typically include only subjects available at the time of the survey. Thus, for example, individuals with PPSI and associated pain may not be represented in the study sample, because they dropped out earlier (i.e., the survey is of “survivors” only).
4.1.3 Cohort Studies
Only a few cohort studies (see Table 4) reported prospective or retrospective data on PPSIs affecting youth, including baseball players, gymnasts, and rock climbers [5, 130, 154,155,156,157,158]. Using count data, these studies reported from 1 to 20 incident cases of PPSI arising during study follow-up ranging from one season to 12 years. Since data did not permit calculation of PPSI incidence for these studies, we calculated clinical incidence of PPSIs from the available data; these ranged from 1.7 to 71.4 PPSIs per 100 athletes [154,155,156,157]. The highest rate of PPSIs was documented in elite gymnasts who were monitored radiographically over 9 years [155]. A limitation of these results is that clinical incidence does not account for the potential variance in the exposure of participants to risk of injury [159].
Historically, the frequency and incidence of traumatic growth plate fractures and PPSIs have been underreported in cohort studies of youth sports injuries [15, 160]. These injuries have traditionally been included in other categories of injury such as fractures or overuse injuries [15, 153]. Additionally, overuse injuries are underestimated in the literature as most of the epidemiological studies define injury as requiring a time loss from participation [13]. Consequently, the number and nature of PPSIs have not been explicitly reported in epidemiological studies of youth sports injuries. In response to this oversight, the International Olympic Committee recently published a consensus statement on methods for recording and reporting of epidemiological data on injury and illness in sport recommending that “physis injury” (including apophyseal injuries) should be a separate category of tissue and pathology types of injury [161]. Important to this approach will be the distinction between primary periphyseal (site of long bone growth) and apophyseal (contribute to bone shape) injuries [15], and between sudden and gradual onset injuries in each sub-category.
4.1.4 Trend Analysis
Several clinicians have observed an increasing number of patients with PPSIs treated in their clinical practices and suggest that these cases may be on the rise [10, 13, 18, 127, 162]. In Fig. 2, we showed a general pattern of increased number of original PPSI reports published per decade between 1950 and 2019. Heyworth et al. [31] showed that the incidence of LLS treated at a regional children’s hospital increased significantly in the period 1999–2013. Also, Lutter et al. [109] reported an increased proportion of finger PPSIs in skeletally immature rock climbers seen at a medical center over a 20-year period (1998–2018).
It is reasonable to expect that the frequency or rate of PPSIs is increasing given the trends discussed previously [1,2,3,4,5]. However, it is also possible that the increased reporting of patients with PPSIs is a reflection of the explosive nature of medical publishing and international research activity, rather than an actual epidemiological phenomenon. Increased reporting of PPSIs may also reflect an increasing public health and clinical awareness of the potential for this injury type. There remains a concern that PPSIs constitute a growing problem among youth athletes, but epidemiological studies are needed to investigate this possibility.
4.2 Injury Outcome
A secondary purpose of this systematic review was to describe the present status of knowledge on the outcome of PPSIs affecting youth sports participants. To elucidate on the outcome of PPSIs, we reviewed data on injury management, presence of growth disturbance, use of surgery, and potential long-term health effects of PPSI.
4.2.1 Injury Management
The nature and extent of information provided on injury management varied considerably across studies. However, some generalizations are possible. In the case literature reviewed, PPSIs were almost universally treated with rest from the exacerbating activity to allow healing. In many patients, rest from the activity included time off from the sport followed by a gradual return to activity. Length of time off before return to activity was variable, ranging from 1 week to 13 months, depending on factors such as injury location, injury severity, whether the patient underwent surgery, and timing of initiation of treatment relative to injury onset.
When necessary, joint immobilization was prescribed to ensure sufficient rest. A variety of treatment modalities were used to ensure the rest of the affected structure including slings, splinting, casting, crutches, knee immobilizers, ankle bracing, and shoe modification. Some studies also reported the use of physical therapy and programs to improve strength, range of motion, and movement mechanics.
Reasonably, initiation of physical therapy and progressive rehabilitation programs should await symptom resolution and, preferably, radiographic evidence of healing, noting that it may lag behind clinical improvement by weeks to months. For example, Laor et al. [21] caution that children with physeal widening in the knee from a stress injury should not undergo physical therapy and progressive rehabilitation as they would risk subsequent malalignment [21]. Similarly, it has also been suggested that the injured throwing athlete does not return to pitching activity until the proximal humeral physis had fused [33, 34, 36, 56], while others stress that the athlete should be asymptomatic before return to play [32, 37, 45].
4.2.2 Bone Growth Disturbance
A concern with PPSIs is their potential for skeletal growth disruption and future deformity [10, 15,16,17]. Most case reports and case series of PPSIs reviewed indicate that this injury resolved with rest during short follow-up and did not produce growth disturbance or deformity. However, as summarized in Table 2, there were 57 cases (12.7%) of disturbed skeletal growth arising from the case reports/series that provide imaging evidence of bone growth disturbance involving the shoulder, elbow, wrist, hand and fingers, knee, foot and ankle of skeletally immature athletes. Sports impacted by these injuries include baseball, basketball, dance, football, gymnastics, rock climbing, and rugby. Additionally, symmetric blunted growth across the growth plate may go unrecognized and underdiagnosed when the duration of follow-up is short (insufficient time to produce limb-length discrepancy) and direct comparison with the asymptomatic (non-dominant side) is unavailable to allow detection of subtle shortening.
Several cross-sectional studies provided evidence of growth disturbance of the distal radius in gymnasts [27] and Chinese opera students [141], and in the proximal phalanx of the thumb and proximal interphalangeal joint of climbers [148, 150]. In these studies, calculated prevalence rates of PPSIs associated with bone growth disturbance ranged from 1.7 to 5.0% [27, 141, 147, 149].
Only two cohort studies reported evidence of bone growth disturbance. Among incident injuries reported, Caine et al. [130] reported a gymnast with premature closure of the right distal radial growth plate. Lishen and Jianhua [155] reported six of eight female and eight of ten male gymnasts followed with routine radiography over 9 years (1972–80) who developed progressive pathology of the distal radius resulting in hindered radial growth and a relatively lengthened ulna [155].
These results make sense according to existing biologic knowledge as, in experimental studies, prolonged intensive physical loading is associated with inhibition of linear bone growth [163,164,165,166]. This injury may be localized and cause asymmetric growth and secondary deformity, or it may involve the entire physis and result in hindered growth or a complete cessation of growth. In either case, premature closure of some or all of the physis may occur [18, 24].
4.2.3 Surgery
Of the 448 patients treated for PPSIs, as reported in the case reports and series, 28 patients (6.2%) underwent surgery for their injury. With the exception of one patient who was treated surgically [37], 196 patients with PPSIs involving the shoulder were treated conservatively. Similarly, only 1 patient with a PPSI of the foot and ankle was treated surgically [125]. In contrast, 11/47 patients with elbow PPSIs, 8/98 patients with wrist PPSIs, and 7/26 patients with knee PPSIs were treated surgically to correct growth disturbance and/or secondary deformity (e.g., proximal radial osteotomy, ulnar shortening osteotomy, open wedge osteotomy of the right distal femur, and surgically guided growth).
Information on time to return to activity following surgery was not uniformly provided in the studies reviewed, generally indicating considerable variation depending on such factors as injury location and type of surgery performed. Time to return to activity following surgery appeared to be greatest for the knee (range = 5–24 months) followed by the wrist (range = 1–15 months) and fingers (≥ 3 months).
4.2.4 Long-Term Health Outcome
PPSIs can counter the beneficial effects of sports participation at a young age if the child or adolescent is unable to continue to participate as a result of the residual effects of injury [13, 14, 150]. Although not consistently reported in the case literature, return to the sport and eventually at former levels of participation following treatment of PPSIs was common. Nevertheless, some patients found it necessary to change position, for example from pitcher to fielder [32, 37, 43, 56], or participate at a less competitive level following PPSI [92, 123]. There are also reports of patients who retired from their sport pursuant to PPSI [65, 66, 69, 70, 74, 75, 84, 87], or who were otherwise lost to follow-up [43, 46, 81, 88, 129].
A concern related to PPSIs is that acquired limb-length discrepancy, angular deformity, or altered joint biomechanics may cause significant long-term morbidity and disability [163,164,165,166,]. Specifically, OA may result from chondral damage at the time of growth plate injury, articular incongruity, or joint malalignment [14]. For example, leg length inequality of the lower extremities, a condition which may contribute to the development of radiographic knee and hip OA by causing asymmetrical joint mechanics between limbs during weight-bearing activities, may arise from a stress-injured physis [167,168,169]. To compensate for leg length inequality, movement patterns may differ between limbs (i.e., the longer limb may exhibit greater knee flexion or hip adduction during stance than the shorter limb to attempt to functionally shorten the longer limb) [170]. Changes in movement patterns to equalize limbs may result in altered or magnified forces across lower extremity joints, leading to the development of OA [171].
Limited longitudinal research involving elite-level gymnasts [155] and rock climbers [5, 17, 158] attests to the potential for early onset OA to develop secondary to PPSIs in skeletally immature athletes. However, the incidence of sport-related PPSIs leading to early onset OA is largely unknown [171]. Follow-up of stress-injured youth athletes into their early adult years is needed to examine this relationship [14, 171].
5 Conclusions
Skeletally immature athletes representing a variety of sports and high impact repetitive activities—including baseball, badminton, climbing, cricket, dance, gymnastics, rugby, soccer, swimming, tennis, and volleyball—may sustain PPSIs involving the shoulder, elbow, hand and wrist, knee, ankle and foot.
Although incidence data from prospective cohort studies are lacking, data arising from cross-sectional studies suggest that PPSIs may be common in select groups of youth athletes—including the shoulder in baseball players, wrist in gymnasts and platform divers, and fingers in rock climbers. Multiple case reports and case series report PPSIs affecting the lower extremity, including those associated with bone growth disturbance; however, no cross-sectional studies focused on lower extremity PPSIs.
Most reported PPSIs appear to respond well to timely treatment, but our research also revealed multiple cases which progressed to skeletal growth disruption and deformity. Of particular concern are PPSIs which affect weight-bearing joints given their potential for growth disruption. Establishing a clear diagnosis of PPSI and providing timely treatment is of great significance in ensuring the skeletal health of skeletally immature athletes. Prospective longitudinal studies, with imaging follow-up, are needed to better elucidate the incidence of PPSIs and how these may impact long-term musculoskeletal health. In this regard, explicit inclusion of PPSIs as an injury type in injury surveillance is essential.
References
Caine DJ. Are kids having a rough time of it in sports? Br J Sports Med. 2010;44:1–3.
Caine DJ, Provance AJ. Pediatric and adolescent injury in adventure and extreme sports. Res Sports Med. 2018;26:5–19.
Maffulli N. Children in sport: questions and controversies. In: Maffulli N, editor. Color Atlas and Text of Sports Medicine in Children and Adolescence. London: Mosby-Wolfe; 1995. p. 7–14.
Maffulli N, Caine D. The epidemiology of children’s team sports injuries. In: Maffulli N, Caine D, editors. Epidemiology of pediatric sports injuries: team sports. Med sport sci, vol 49. Basel: Karger; 2005. p. 1–8.
Schöffl V, Hoffmann P, Imhoff A, Kupper T, Schöffl I, Hochholzer T, et al. Long-term radiographic adaptations to stress of high-level and recreational rock climbing in former adolescent athletes. An 11-year prospective longitudinal study. Orthop J Sports Med. 2018;6:1–9.
Steffen K, Engebretsen L. More data needed on injury risk among elite young athletes. Br J Sports Med. 2010;44:485–9.
Youth Olympic Games. https://www.olympic.org/youth-olympic-games. Accessed 1 Mar 2020
U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans, 2nd Edition. Washington, DC: U.S. Department of Health and Human Services; 2018. https://health.gov/paguidelines/second-edition/pdf/Physical_Activity_Guidelines_2nd_edition.pdf. Accessed 1 Feb 1 2020.
Emery CA. Injury prevention in kids’ adventure and extreme sports: future directions. Res Sports Med. 2018;26(Supple. 1):199–211.
DiFiori JP. Overuse injury of the physis: a “growing” problem. Clin J Sport Med. 2010;20:336–7.
Armstrong N, McManus AM. Preface. The elite young athlete. Med Sport Sci. 2011;56:1–3.
Sabato T, Walch T, Caine D. The elite young athlete: strategies to ensure physical and emotional health. Open Access J Sports Med. 2016;7:99–113.
DiFiori JP, Benjamin HJ, Brenner J, Gregory A, Jayanthi N, Landry JL, et al. Overuse injuries and burnout in youth sports: a position statement from the American Medical Society for Sports Medicine. Clin J Sport Med. 2014;24:3–20.
Maffulli N, Longo UG, Gougoulias N, Loppini M, Denaro V. Long-term health outcomes of youth sports injuries. Br J Sports Med. 2010;44:21–5.
Caine D, DiFiori J, Maffulli N. Physeal injuries in children’s and youth sports: reasons for concern? Br J Sports Med. 2006;40:749–60.
Schöeffl L, Schöeffl V. Epiphyseal stress fractures in the fingers of adolescents: biomechanics, pathomechanisms, and risk factors. Eur J Sports Med. 2015;3:27–37.
Hochholzer Th, Schöffl V. Epiphyseal fractures of the finger middle joints in young sport climbers. Wilderness Environ Med. 2005;16:139–42.
Ogden JA. Skeletal injury in the child. New York: Springer; 2000.
Caine D, Howe W, Ross W, Bergman G. Does repetitive physical loading inhibit radial growth in female gymnasts. Clin J Sport Med. 1997;7:102–8.
Moher D. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Ann Intern Med. 2013. https://doi.org/10.7326/0003-4819-151-4-200908180-00135.
Laor T, Wall EJ, Vu LP. Physeal widening in the knee due to stress injury in child athletes. Am J Roentgenol. 2006;186:1260–4.
Bedoya MA, Jaramillo D, Chauvin NA. Overuse injuries in children. Top Magn Reson Imaging. 2015;24:67–81.
Jaramillo D, Laor T, Zaleske DJ. Indirect trauma to the growth plate: results of MR imaging after epiphyseal and metaphyseal injury in rabbits. Radiology. 1993;187:171–8.
Nguyen JC, Markhardt BK, Merrow AC, Dwek JR. Imaging of pediatric growth plate disturbances. RG. 2017;17:1791–812.
Dotter WE. Little leaguer’s shoulder. Guthrie Clin Bull. 1953;23:68–72.
Roy S, Caine D, Singer K. Stress changes of the distal radial epiphysis in young gymnasts. A report of twenty-one cases and a review of the literature. Am J Sports Med. 1985;13:301–8.
Shih C, Chang CY, Penn IW. Chronically stressed wrists in adolescent gymnasts: MR imaging appearance. Radiology. 1995;195:855–9.
Dwek JR, Chung CB. Lower extremity overuse injuries in pediatric athletes: clinical presentation, imaging findings and treatment. Clin Imaging. 2013;37:836–46.
Salter RB, Harris WR. Injuries involving the epiphyseal plate. J Bone Jt Surg. 1963;45A:587–622.
Cummings P, Weiss NS. Case series and exposure series: the role of studies without controls in providing information about the etiology of injury or disease injury prevention. Inj Prev. 1998;4:54–7.
Heyworth BE, Kramer DE, Martin DJ, Kocher MS, Bae DS. Trends in the presentation, management, and outcomes of little league shoulder. Am J Sports Med. 2016;44:1431–8.
Hansen NM Jr. Epiphyseal changes in the proximal humerus of an adolescent baseball pitcher: a case report. Am J Sports Med. 1982;10:380–4.
Adams JE. Little league shoulder: osteochondrosis of the proximal humeral epiphysis in boy baseball pitchers. Calif Med. 1966;105:22–5.
Torg JS. The little league pitcher. Am Fam Phys. 1972;6:71–6.
Cahill BR. Little league shoulder: rotational stress fracture of proximal epiphysis. J Sports Med. 1974;2:150–2.
Tullos HS, Fain RH. Little leaguer shoulder: lesions of the proximal epiphyseal plate. J Sports Med. 1974;2:152–3.
Lipscomb AB. Baseball pitching injuries in growing athletes. J Sports Med. 1975;3:25–34.
Barnett LS. Little league shoulder syndrome. Proximal humeral epiphysiolysis in adolescent baseball pitchers—a case report. J Bone Jt Surg (USA). 1985;67:495–6.
Albert MJ, Drvaric DM. Little league shoulder: case report. Orthopaedics. 1990;13:779–81.
Carson WG, Gasser SI. Little leaguer’s shoulder. A report of 23 cases. Am J Sports Med. 1998;26:575–80.
Ricci AR, Mason DE. Little league shoulder: case report and literature review. Del Med J. 2004;76:11–4.
Flemming JL, Hollingsworth CL, Squire DL, Bisset JS. Little leaguer’s shoulder. Skelet Radiol. 2004;33:352–4.
Hatem SF, Recht MP, Profitt B. MRI of little leaguer’s shoulder. Skelet Radiol. 2006;35:103–6.
Song JC, Lazarus ML, Song AP. MRI findings in little leaguer’s shoulder. Skelet Radiol. 2006;35:107–9.
Popkin CA, Posada A, Clifford PD. Little leaguer’s shoulder. Clin Imaging. 2006;30:365–7.
Obembe O, Gaskin CM, Taffoni MJ, Anderson MW. Little leaguer’s shoulder (proximal epiphysiolysis): MRI findings in four boys. Pediatr Radiol. 2007;37:885–9.
Anton C, Podberesky DJ. Little league shoulder: a growth plate injury. Pediatr Radiol. 2010;40(Supple 1):S54.
Domes CM, Petering R, Chesnutt JC, Mirarchi A. Concurrent little leaguer’s elbow and shoulder in a 15-year-old baseball pitcher and football quarterback. Orthop. 2012;35(1):e10–97.
Reeder MT, Smith B. Little league shoulder. J Am Osteopath Assoc. 2015;115:522.
Wasylynko D. Chronic pain due to little leaguer’s shoulder in an adolescent baseball pitcher: a case report. Can Chiropr Assoc. 2015;59:383–9.
Hosokawa Y, Mihata T, Yasuo Itami Y, Neo M, Doi M. Little leaguer’s shoulder can cause severe three-dimensional humeral deformity. Clin Orthop Surg. 2017;9:537–41.
Zipser MC, Sum JC, Wilcox AG. Little league shoulder in a 15-year-old male baseball pitcher. J Orthop Sports Phys Ther. 2018;48:51.
Greenburg EM, Turner C, Huse C, Ganley TJ, McClure T, Lawrence JT. Salter–Harris fracture of the proximal humerus in an adolescent gymnast. J Orthop Sports Phys Therap. 2018;48(9):729.
Boyd KT, Batt ME. Stress fracture of the proximal humeral epiphysis in an elite junior badminton player. Br J Sports Med. 1997;31:252–3.
Kirimura K, Nageo M, Sugiyama M. High incidence of posterior glenoid dysplasia of the shoulder in young baseball players. J Shoulder Elbow Surg. 2019;28:82–7.
Drescher WR, Falliner A, Zantop T, et al. Little league shoulder syndrome in an adolescent cricket player. Br J Sports Med. 2004;38:E14.
Daldorf PG, Bryan WJ. Displaced Salter–Harris type 1 injury in a gymnast. A slipped capital humeral epiphysis. Orthop Rev. 1994;23:538–41.
Ejnisman B, Andreoli V, Pochini ADC, et al. Proximal humeral epiphysiolysis in a gymnast. Acta Orthop Bras. 2007;15(5):290–1.
Kosnik M, Paulseth S, Abzug A. Salter–Harris fracture of the proximal humerus in an adolescent gymnast. J Orthop Sports Phys Ther. 2018;48(9):729.
Johnson JN, Houchin G. Adolescent athlete’s shoulder. A case series of proximal humeral epiphysiolysis in nonthrowing athletes. Clin J Sports Med. 2006;16:84–6.
Jenkinson E, Roush MB. Shoulder pain in a female volleyball player. Syllabus of the 6th American Medical Society for Sports Medicine Annual Meeting; 1996.
Carson JT, McCambridge TM, Carrino JA, McFarland EG. Case report: bilateral epiphyseal clavicular stress-related lesions in a male gymnast. Clin Orthop Relat Res. 2012;470:307–11.
Ellman H. Anterior angulation deformity of the radial head. An unusual lesion occurring in juvenile baseball players. J Bone Jt Surg Am. 1975;57:776–8.
Podestra L, Sherman MF, Bonamo JR. Distal humeral epiphyseal separation in a young athlete. A case report. Arch Phys Med Rehabil. 1993;74:1216–8.
Chan D, Aldridge MJ, Maffulli N, Davies AM. Chronic stress injuries of the elbow in young gymnasts. Br J Radiol. 1991;64:1111–8.
Maffulli N, Chan D, Aldridge MJ. Derangement of the articular surfaces of the elbow in young gymnasts. J Ped Orthop. 1992;12:344–50.
Huckaby MC, Kruse D, Gibbs LH. MRI findings of proximal radial physeal injury in a gymnast. Pediatr Radiol. 2012;42:1395–400.
Oda R, Fujiwara H, Ichimaru K, Morihara T, Ikeda T, Kubo T. Chronic slipping of bilateral humeral epiphyses in a gymnastist. J Pediatr Orthop B. 2015;24:67–70.
Miller SM, Wyatt CW, Ellis HB, Wilson PL. Proximal radial epiphyseal injuries in gymnasts. Pediatric Research in Sports Medicine Annual Meeting, Dallas, TX, January 26–28; 2017.
Santelli J, McCambridge T, Valasek AE, Standford K. Proximal radial head fractures in young gymnasts. Clin J Sport Med. 2019;29:e1–3.
Inagaki H, Inoue G. Stress fracture of the scaphoid combined with the distal radial epiphysiolysis. Br J Sports Med. 1997;31:256–7.
Kwon SW, Hong SJ, Nho JH, Moon S, Jung KJ. Physeal fracture in the wrist and hand due to stress injury in a child climber. Med. 2018;97:34.
Gerber SP, Griffin PP, Simmons BP. Case Report: Breakdancer’s wrist. J Ped Orthop. 1986;6:98–9.
Read MT. Stress fractures of the distal radius in adolescent gymnasts. Br J Sports Med. 1981;15:272–6.
Fliegel CP. Stress related widening of the radial growth plate in adolescents. Ann Radiol. 1986;29:374–6.
Carter SR, Aldridge MJ. Stress injury of the distal radial growth plate. J Bone Jt Surg (GB). 1988;70:834–6.
Carter SR, Aldridge MJ, Fitzgerald R, Davies AM. Stress changes of the wrist in gymnasts. Br J Radiol. 1988;61:109–12.
Resnick DL. Case 6: a12-year-old gymnast with intermittent pain in the wrist. Radiographics. 1988;8(2):246–8.
Yong-Hing K, Wedge JN, Bowen CV. Chronic injury to the distal ulnar and radial growth plates in an adolescent gymnast. J Bone Jt Surg (USA). 1988;70:1087–9.
Vender MI, Watson K. Acquired Madelung-like deformity in a gymnast. J Hand Surg (USA). 1988;13:19–21.
Albanese SA, Palmer AK, Kerr DR, Carpenter CW, Lisi D, Levinsohn M. Wrist pain and distal growth plate closure of the radius in gymnasts. J Ped Orthop. 1989;9:23–8.
Ruggles DL, Peterson HA, Scott SG. Radial growth plate injury in a female gymnast. Med Sci Sports Exerc. 1991;23:393–6.
Li DK, Lloyd-Smith R. Wrist pain in an adolescent gymnast. Clin J Sports Med. 1991;1:259–61.
Tolat AR, Sanderson PL, DeSmet L, Stanley JK. The gymnast’s wrist: acquired positive ulnar variance following chronic epiphyseal injury. J Hand Surg. 1992;17:678–81.
Carek PJ, Fumich RM. Stress fracture of the distal radius. Not just a risk for elite gymnasts. Phys Sportsmed. 1992;20(5):115–8.
Nattiv A, Mandelbaum BR. Injuries and special concerns in female gymnasts. Detecting, treating, and preventing common problems. Phys Sportsmed. 1993;21:66–82.
De Smet L, Claessens A, Fabrey G. Gymnast wrist. Acta Orthop Belg. 1993;59:377–80.
Liebling MS, Berdon WE, Ruzal-Shapiro C, Levin TL, Roye D, Wilkinson R. Gymnast’s wrist (pseudorickets growth plate abnormality) in adolescent athletes: findings on plain films and MR imaging. AJR. 1995;164:157–9.
DiFiori JP, Mandelbaum BR. Wrist pain in a young gymnasts: unusual radiographic findings and MRI evidence of growth plate injury. Med Sci Sports Exerc. 1996;28:1453–8.
Bak K, Boeckstyns M. Epiphysiodesis for bilateral irregular closure of the distal radial physis in a gymnast. Scand J Med Sci Sports. 1997;7:363–6.
Frizzell JB, Brunet G. Stress changes of the distal radial physis. Can Assoc Radiol J. 1997;48:54–5.
Howe WB, Caine D, Bergman GD, Keeler LW. Wrist pain—gymnastics. Med Sci Sports Exerc. 1997;29:S151.
Brooks TJ. Madelung deformity in a collegiate gymnast: a case report. J Athl Train. 2001;36:170–3.
Barkdell T, Annunziata CC. Acquired Madelung-type deformity in a gymnast. Med Sci Sports Exerc. 2007;39(5):S133–4.
Dwek JR, Cardoso F, Chung CR. MR Imaging of overuse injuries in the skeletally immature gymnasts: spectrum of soft-tissue and osseous lesions in the hand and wrists. Pediatr Radiol. 2009;39:1310–6.
Poletto ED, Pollock AN. Radial epiphysitis (aka Gymnast Wrist). Pediatr Emerg Care. 2012;28(5):484–5.
Ashwell ZR, Richardson ML. Case report: gymnast’s wrist in a 12-year-old female with MRI correlation. Radiol Case Rep. 2019;14:360–4.
Mauck B, Kelly D, Sheffer B, Rambo A, Calandruccio JH. Gymnast’s wrist (distal radial physeal stress syndrome). Orthop Clin N Am. 2020;51:493–7.
Hochholzer T, Schöffl V, Krause R. Finger-epiphysen-verletzungen jugendlicher sportkletterer. Sport Orthop Traumatol. 1997;13:100–3.
Chell J, Stevens K, Preston B, Davis TRC. Bilateral fractures of the middle phalanx of the middle finger in an adolescent climber. Am J Sports Med. 1999;27:817–9.
Bayer T, Schöffl VR, Lenhart M, Herold T. Epiphyseal stress fractures of finger phalanges in adolescent climbing athletes: a 3.0-Teslas magnetic resonance imaging evaluation. Skelet Radiol. 2013;42:1521–5.
Schöffl V, Popp D, Kupper T, Schöffl I. Injury trends in rock climbers: evaluation of a case series of 911 injuries between 2009–2012. Wildern Environ Med. 2015;26:62–7.
Desaldeleer AS, Le Nen D. Bilateral fracture of the base of the middle phalanx in a climber: literature review and a case report. Orthop Traumatol Surg Res. 2016;102(3):409–11.
El-Sheikh Y, Lutter C, Schöffl I, Schöffl V. Surgical management of proximal interphalangeal joint repetitive stress epiphyseal fracture nonunion in elite sport climbers. J Hand Surg Am. 2018;43(6):572.e1-572.e5. https://doi.org/10.1016/j.jhsa.2017.10.009.
Halsey T, Johnson M, Jones G. Epiphyseal stress fractures of the fingers in an adolescent climber: a potential “Maslow’s Hammer” in terms of clinical reasoning. Curr Sports Med Rep. 2019;18:431–3.
Attkiss KJ, Bunckle HJ. Physeal growth arrest of the distal phalanx of the thumb in an adolescent pianist: a case report. J Hand Surg. 1998;23A:532–5.
Schoffl V, Hochholzer T, Winkerlmann H, Strecker W. Pulley injuries in rock climbers. Wildern Environ Med. 2003;41:94–100
Quaine F, Vigouroux L, Martin L. Effect of simulated rock climbing finger postures on force sharing among the fingers. Clin Biomech. 2003;18:365–8.
Lutter C, Tischer T, Hotfiel T, Frank L, Enz A, Simon N, et al. Current trends in sport climbing injuries after the inclusion into the Olympic program. Analysis of 633 injuries within the years 2017/2018. MLTJ. 2020;2:201–10.
Sato T, Shinozaki T, Fukudo T, Watanabe H, Aoki J, Yanagawa T, et al. Atypical growth plate closure: a possible chronic Salter and Harris type V injury. J Pediatr Orthop. 2002;11:155–8.
Domzalski M, Mackenzie W. Growth arrest of the proximal tibial physis with recurvatum and valgus deformity of the knee. Knee. 2009;16:412–6.
Wall EJ. Knee injury: gymnastics. Med Sci Sports Exerc. 1997;29(suppl):S152.
Blatnik TR, Briskin S. Bilateral knee pain in a high-level gymnast. Clin J Sport Med. 2013;23:77–9.
Godshall RW, Hansen CA, Rising DC. Stress fractures through the distal femoral epiphysis in athletes. A previously unreported entity. Am J Sports Med. 1981;9:114–6.
Borders H. Physeal stress injury. Pediatr Adolesc MSK MRI, J Herman Kan, pp. 78–83.
Tony G, Charron A, Tins B, Lalam R, Tyrrell PNM, Singh J, et al. Intra-epiphyseal stress injury of the proximal tibial epiphysis: preliminary experience of magnetic resonance imaging findings. Eur J Radiol. 2014;83:2051–7.
Ehara S. Physeal stress injury to the knee. AJR. 2006;187:W554.
Nanni M, Butt S, Mansour R. Stress-induced Salter–Harris I growth plate injury of the proximal tibia: first report. Skelet Radiol. 2005;34:405–10.
Cahill BR. Stress fracture of the proximal tibial epiphysis: a case report. Am J Sports Med. 1977;5:186–7.
Dempewolf M, Kwan K, Sherman B, Schlechter J. Youth kicker’s knee: lateral distal femoral hemi-physeal arrest secondary to chronic repetitive microtrauma. J Am Acad Orthop Surg. 2019;3:1–6.
Weber PC. Salter–Harris type II stress fracture in a young athlete. Orthopaedics. 1988;11:309–11.
Kadel NJ, Goldstein J, Hewberg AH, Trempman E. Salter–Harris stress fracture of the proximal first metatarsal: a case report. Foot Ankle Intern. 2001;22:252–5.
Shybut TB, Rose DJ, Strongwater AM. Second metatarsal physeal arrest in an adolescent Flamenco dancer: a case report. Foot Ankle Int. 2008;29:859–62.
Bernholdt DL, Garzon-Muvdi J, Chhabra A, McFarland EG. Stress fracture of the distal tibial physis in an adolescent recreational dancer. Am J Sports Med. 2013;41:1649–52.
Csonka A, Sikarinkul E, Gargyan I, Boa K, Varga E. Operative management of bilateral Salter–Harris type III fractures of the proximal phalanges of the great toes of a 10-year-old female ballet dancer: a case report. J Pediatr Orthop B. 2016;25:393–6.
Shah S. Premature growth plate closure in a ballet dancer en Pointe. Clin J Sport Med. 2017;27(5):e69–71.
Wall EJ. Growth plate overuse syndrome of the ankle in athletes. Med Sci Sports Exerc. 1997;5:299.
Percy EC, Gamble FO. An epiphyseal stress fracture of the foot and shin splints in an anomalous calf muscle in a runner. Br J Sports Med. 1980;14:110–3.
Schapiro A, Laor T. ‘Soccer toe:’ Chronic physeal injury of the great toe metatarsal in a skeletally immature child—a case report. SA J Radiol. 2020;24(1):1834. https://doi.org/10.4102/sajr.v24i1.1834.
Caine D, Knutzen K, Howe W, Keeler L, Sheppard L, Heinrichs D, et al. A three-year epidemiological study of injuries affecting young female gymnasts. Phys Ther Sport. 2003;4:10–23.
DiFiori JP, Caine DJ, Malina RM. Wrist pain, distal radial physeal injury, and ulnar variance in the young gymnast. Am J Sports Med. 2006;34:840–9.
Bejjami FJ, Halpern N, Pio A, Dominguez R, Voloshin A, Frankel VH. Musculoskeletal demands on Flamenco dancers: a clinical and biomechanical study. Foot Ankle. 1988;8:254–6.
Torg JS, Pollack H, Sweterlitsch P. The effect of competitive pitching on the shoulders and elbows of baseball players. Pediatrics. 1972;49:267–72.
Kanematsu Y, Matsuura T, Kashiwaguchi S, Iwase T, Suzue N, Iwame T, et al. Epidemiology of shoulder injuries in young baseball players and grading of radiologic findings of Little Leaguer’s shoulder. J Med Investig. 2015;62:123–5.
Pennock AT, Dwek J, Levy E, Stearns P, Manning J, Dennis MM, et al. Shoulder MRI abnormalities in asymptomatic little league baseball players. Orthop J Sports Med. 2018;6(2):2325967118756825.
Zhang C, Shen S, Zhang W, Qiu L, Qingying W, Wang F, et al. Effect of long-term diving on the morphology and growth of the distal radial epiphyseal plate of young divers: a magnetic resonance imaging study. Clin J Sports Med. 2019;29(4):312–7.
Auberge T, Zenny JC, Duvallet A, Godefroy D, Horreard P, Chevrot A. Study of bone maturation and osteo-articular lesions in top level sportsmen: a review of 105 cases. J Radiol (Paris). 1984;65:555–61.
Szot Z, Boron Z, Galaj Z. Overloading changes in the motor system occurring in elite gymnasts. Int J Sports Med. 1985;6:36–40.
Caine D, Roy S, Singer KM, Broekhoff J. Stress changes of the distal radial growth plate. A radiographic survey of 60 young competitive gymnasts and an epidemiologic review of the related literature. Am J Sports Med. 1992;20:290–8.
DeSmet L, Claessons A, Lefevre J, Beunen J. Gymnast wrist: an epidemiological survey of the ulnar variance in elite female gymnasts. Am J Sports Med. 1994;22:846–50.
Chang CY, Shih C, Penn IW, Tiu CM, Chang T, Wu JJ. Wrist injuries in adolescent gymnasts of a Chinese opera school: radiographic survey. Radiology. 1995;195:861–4.
DiFiori JP, Puffer JC, Mandelbaum BR, Dorey F. Distal radial growth plate injury and positive ulnar variance in non-elite gymnasts. Am J Sports Med. 1997;25:763–8.
DiFiori JP, Puffer JP, Aish B, Dorey F. Wrist pain, distal radial physeal injury, and ulnar variance in young gymnasts: does a relationship exist? Am J Sports Med. 2002;30:879–85.
Guerra MRV, Estelles JRD, Abdouni YA, Falcochio DF, Rosa JRP, Catani LH. Frequency of wrist growth plate injury in young gymnasts at a training center. Acta Orthop Bras. 2016;24:204–7.
Kraan RBJ, Kox LS, Mens MA, Kuijer PPFM, Maas M. Damage of the distal radial physis in young gymnasts: can three-dimensional assessment of physeal volume on MRI serve as a biomarker? Eur Radiol. 2019;29:6364–71.
Kraan RBJ, Kox LS, Oostra RJ, Kuijer PPFM, Maas M. The distal radial physis: exploring normal anatomy on MRI enables interpretation of stress related changes in young gymnasts. Eur J Sport Sci. 2020;20:1197–205.
Schlegel C, Buchler U, Kriemler S. Finger injuries of elite rock climbers. Schweizerische Zeitschrift fur Sportsmeizin und Sportstraumatologies. 2002;50(1):7–10.
Schöffl V, Hochholzer T, Imhoff A. Radiographic changes in the hands and fingers of young, high-level climbers. Am J Sports Med. 2004;32(7):1688–94.
Garcia K, Jarmillo D, Rubesova E. Ultrasound evaluation of stress injuries and physiological adaptations in the fingers of adolescent competitive rock climbers. Pediatr Radiol. 2018;48:366–73.
Bartschi N, Scheibler A, Schweizer A. Symptomatic epiphyseal sprains and stress fractures of the finger phalanges in adolescent sport climbers. Hand Surg Rehab. 2019;38:251–6.
Meyers RN, Howell DR, Provance AJ. The association of finger growth plate injury history and speed climbing in youth competition climbers. Wilderness Environ Med. 2020;17:812.
Sabato T, Caine D. Epidemiology of injury in community club and youth sports organizations. In: Caine D, Purcell L, editors. Injury in pediatric and adolescent sport: epidemiology, treatment and prevention. Switzerland: Springer Publishers; 2006.
Caine D, Caine C, Maffulli N. Incidence and distribution of pediatric sport-related injuries. Clin J Sport Med. 2006;16:501–14.
Holt JB, Stearns PH, Bastrom TP, Dennis MM, Dwek JR, Pennock AT. The curse of the all-star team: a single-season prospective shoulder MRI study of Little League baseball players. J Pediatr Orthop. 2020;40(1):e19-24.
Lishen Q, Jianhua O. Epiphyseal injury in gymnasts. Chin J Sports Med. 1983;2:7–12.
Caine D, Cochrane B, Caine C, Zemper E. An epidemiological investigation of injuries affecting young competitive female gymnasts. Am J Sports Med. 1989;17:811–20.
Dixon M, Fricker P. Injuries to elite gymnasts over 10 years. Med Sci Sports Exerc. 1993;25:1322–9.
Schöffl V, Hochholzer T, Imhoff A, Schöffl L. Radiographic adaptations to the stress of high-level rock climbing in junior athletes: a 5-year longitudinal study of the German junior national team and a group of rectreational climbers. Am J Sports Med. 2007;35(1):86–92.
Knowles SB, Marshall SW, Guskiewicz KM. Issues in estimating risks and rates in sports injury research. J Athl Train. 2006;41:207–15.
Materne O, Chamari K, Farooq A, Weir A, Hölmich P, Bahr R, et al. Injury incidence and burden in a youth elite football academy: a four-season prospective study of 551 players aged from under 9 to under 19 years. Br J Sports Med. 2020. https://doi.org/10.1136/bjsports-2020-102859.
Bahr R, Clarsen B, Derman W, Dvorak J, Emery CA, Finch CF, et al. International Olympic Committee consensus statement: methods for recording and reporting of epidemiological data on injury and illness in sport 2020 (including STROBE Extension for Sport Injury and Illness Surveillance (STROBE-SIIS)). Br J Sports Med. 2020;54:372–89.
Micheli LJ, Klein JD. Sports injuries in children and adolescents. Br J Sports Med. 1991;25:6–9.
Tipton CM, Matthes RD, Maynard JA. Influence of chronic exercise on rat bones. Med Sci Sports Exerc. 1972;4:55.
Kiiskinen A. Physical training and connective tissues in young mice: physical properties of Achilles tendons and long bones. Growth. 1977;41:123–37.
Simon MR. The effects of dynamic loading on the growth of epiphyseal cartilage in the rat. Acta Anat. 1978;102:176–83.
Matsuda JJ, Zernicke RF, Vailas AC, Barnard RJ. Structural and mechanical adaptation of immature bone to strenuous exercise. J Appl Physiol. 1986;60:2028–34.
Friberg O. Clinical symptoms and biomechanics of lumbar spine and hip joint in leg length inequality. Spine. 1983;8:643–51.
McCaw ST, Bates BT. Biomechanical implications of mild leg length inequality. Br J Sports Med. 1991;25:10–3.
Morscher E. Etiology and pathophysiology of leg length discrepancies. Prog Orthop Surg. 1977;1:9–19.
Golightly YM, Allen KD, Helmick CG, Schwartz TA, Renner JB, Jordan JM. Hazard of incident and progressive knee and hip radiographic osteoarthritis and chronic joint symptoms in individuals with and without limb length inequality. J Rheumatol. 2010;3(7):2133–40.
Caine DJ, Golightly YM. Osteoarthritis as an outcome of paediatric sport: an epidemiological perspective. Br J Sport Med. 2011;45:298–303.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dennis Caine, Rachel Meyers, Jie Nguyen, Volker Schöffl, and Nicola Maffulli declare that they have no competing interests.
Funding
No sources of funding were used to assist in the preparation of this article.
Authorship contributions
DC wrote the first draft of the manuscript. RM assisted with the systematic search and retrieval of the literature following PRISMA guidelines. She also developed the PRISMA flowchart. VS and NM provided clinical interpretation of case studies reviewed and assisted with the development of the summary tables. JN provided imaging and clinical interpretation of case studies and assisted with the development of the summary and supplementary tables. RM, JN, VS, and NM assisted with revisions of the original manuscript. All authors read and approved the final manuscript.
Data availability statement
Supplementary information in the form of six summary tables (Supplementary Information Tables S1–S6) is available to authorized users [see title page for information] or from the author on request. These summary tables correspond to results discussed in Sects. 3.2.1–3.2.6.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Caine, D., Meyers, R., Nguyen, J. et al. Primary Periphyseal Stress Injuries in Young Athletes: A Systematic Review. Sports Med 52, 741–772 (2022). https://doi.org/10.1007/s40279-021-01511-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-021-01511-z