Abstract
Background
Interventions utilising the Nordic hamstring exercise (NHE) have resulted in reductions in the incidence of hamstring strain injury (HSI). Subsequently, quantifying eccentric knee flexor strength during performance of the NHE to identify an association with the occurrence of future HSI has become increasingly common; however, the data to date are equivocal.
Objective
To systematically review the association between pre-season eccentric knee flexor strength quantified during performance of the NHE and the occurrence of future HSI.
Design
Systematic review and meta-analysis.
Data sources
CINAHL, Cochrane Library, Medline Complete, Embase, Web of Science and SPORTDiscus databases were searched from January 2013 to January 10, 2020.
Eligibility criteria for selecting studies
Prospective cohort studies which assessed the association between pre-season eccentric knee flexor strength quantified during performance of the NHE and the occurrence of future HSI.
Methods
Following database search, article retrieval and title and abstract screening, articles were assessed for eligibility against pre-defined criteria then assessed for risk of bias. Meta-analysis was used to pool data across studies, with meta-regression utilised where possible.
Results
A total of six articles were included in the meta-analysis, encompassing 1100 participants. Comparison of eccentric knee flexor strength during performance of the NHE in 156 injured participants and the 944 uninjured participants revealed no significant differences, regardless of whether strength was expressed as absolute (N), relative to body mass (N kg−1) or between-limb asymmetry (%). Meta-regression analysis revealed that the observed effect sizes were generally not moderated by age, mass, height, strength, or sport played.
Conclusion
Eccentric knee flexor strength quantified during performance of the NHE during pre-season provides limited information about the occurrence of a future HSI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Meta-analysis of six studies (156 prospective HSIs and 944 uninjured participants) found no difference in pre-season eccentric knee flexor strength quantified during performance of the Nordic hamstring exercise (NHE)between prospectively injured and uninjured participants |
Irrespective of whether pre-season eccentric knee flexor strength quantified during performance of the NHE was expressed in absolute (N) or relative (N kg−1) terms or as a between-limb asymmetry (%) there was no difference between prospectively injured and uninjured participants |
Accounting for potential effect modifiers (sport played, age, height, mass, average cohort NHE strength) did not alter the findings |
1 Introduction
Hamstring strain injury (HSI) is the most common injury in a number of running-based sports [1,2,3] and has a high recurrence rate compared to other lower limb muscles [2, 4]. Previous injury (which leads to subsequent unavailability for training and/or matches) influences subsequent injury risk [5] and impacts team’s success [6]. Furthermore prior HSI adversely effects individual performance [7] and physical output [8] upon return from injury. As a result, strategies to mitigate the risk of HSI occurrence have received significant attention in the literature.
A central component of injury prevention models [9, 10] is the identification of factors that can provide an indication of an individual’s risk of future injury and research on risk factors for HSI has increased in recent times [11]. Whilst these risk factors can be extrinsic or intrinsic variables [12] those which are modifiable are of most interest as they can be altered via intervention. Of the modifiable factors examined, the magnitude of hamstring strength, and various associated ratios (e.g. hamstring to quadriceps strength ratio, between-limb asymmetry) are commonly reported in the literature [11]; however, the findings are often conflicting across studies. Factors contributing to inconsistent findings include different strength testing methodologies, the range of variables reported (e.g. peak force, limb symmetry, hamstring to quadriceps ratio) and the different cohorts examined. Subsequently, drawing inferences from the existing literature is difficult.
The Nordic hamstring exercise (NHE), a common partner-assisted eccentric strength training exercise for the knee flexors, has been shown to reduce the likelihood of sustaining a HSI across a number of cohorts [13, 14]. Recently, a device which quantifies eccentric knee flexor strength during the performance of the NHE in the field [15] has become prominent. It has been hypothesised that quantifying eccentric knee flexor strength during the NHE may provide information about an individual’s risk of HSI as high force lengthening contractions of the hamstrings during high speed running are presumed to be implicated in the aetiology of HSI. An initial prospective cohort study to test this hypothesis, conducted in elite Australian Football, identified a greater risk of future HSI in those who had lower levels of eccentric knee flexor strength during the NHE, compared to stronger athletes [16]. Whilst this initial finding was subsequently confirmed in a cohort of Australian soccer players [17], further studies in Qatari soccer [18], Australian rugby union [19], Australian Football [20], and Gaelic Football [21] have been conflicting. Similarly, whilst greater between-limb asymmetry in eccentric strength during NHE has been reported to increase HSI risk previously [19], this is not a consistent finding [16,17,18, 20, 21].
Therefore, the aim of this study was to systematically review the association between pre-season eccentric knee flexor strength quantified during the performance of the NHE and the occurrence of future HSI. A secondary aim is to determine whether larger between-limb asymmetry in eccentric knee flexor strength is associated with future HSI.
2 Methods
2.1 Trial Registration
This review was submitted for registration with the International Prospective Register of Systematic Reviews on December 12, 2019 and was registered on April 28, 2020 (PROSPERO ID registration number: CRD42020158618).
2.2 Literature Search Strategy
The literature search and study selection process were conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines. A comprehensive search of CINAHL, Cochrane Library, Medline Complete, Embase, Web of Science and SPORTDiscus databases was conducted from January 2013 to January 10, 2020. The search was restricted to articles published from 2013 onwards as the first report of the device used to measure eccentric knee flexor strength during the NHE was published in 2013 [15]. The search strategy, including key terms and controlled vocabulary (i.e. Medical Subject Headings [MeSH] terms) can be found in Supplementary Table S1. The search terms were determined to align with the research question and aims of the review. Following retrieval all citations were imported into EndNote X9 (Thomson Reuters, New York City, NY, USA) where duplicated removal was performed.
2.3 Study Selection
The title and abstract of retrieved articles were screened for inclusion by two authors (RGT, JTH) using Rayyan [22]. Following the title and abstract screening, a full-text review was completed to determine eligibility by two authors (FPB, JTH). Included in the current review were prospective cohort studies that quantified eccentric knee flexor strength during performance of the NHE and reported appropriate summary statistics (i.e. measures of central tendency and variation). The population investigated was those participating in sport of any level. Studies were included if they reported data separately for participants who did and did not sustain a subsequent HSI during a defined follow-up period. Only peer-reviewed publications in English were considered. Hand-searching of the reference list was performed on all included studies to identify any other potential articles for inclusion (only articles published form 2013 onwards were considered for inclusion in line with the search strategy).
2.4 Risk of Bias Assessment
The Quality in Prognosis Studies (QUIPS) tools [23] was used to assess risk of bias of all included studies, per previous similar systematic reviews [11]. Two authors (RGT, NvD) applied the QUIPS to each individual study, with any discrepancy between scoring discussed between these authors to reach a consensus. If a consensus could not be reached in this manner, a third author (FPB) was used to resolve the dispute.
An individual study was considered to have a low risk of bias if five of the six domains defined in the QUIPS tool (study participation, study attrition, prognostic factor measurement, outcome measurement, study confounding, statistical analysis and reporting) were assessed as having a low risk of bias (defined as a score of ≥ 75% for individual criteria under each domain). Any study that was determined to have a high risk of bias in the outcome measurement domain was automatically assigned a high risk of bias.
2.5 Data Extraction
Data pertaining to participant characteristics, including age, height, mass, sport, history of HSI and level of competition were extracted. Additional methodological details were also extracted, including the definition used to determine the occurrence of a HSI, the NHE strength testing protocol, time of testing, and the length of participant follow-up. Measures of sample size, central tendency (typically a mean value) and variance (typically standard deviation) related to NHE strength in groups of individuals who did and did not sustain a HSI were also extracted. Specifically, the following knee flexor strength data, quantified during performance of the NHE were obtained: absolute knee flexor strength (N), knee flexor strength normalised to body mass (N kg−1), and between-limb asymmetry in knee flexor strength (%). Since between-limb asymmetry was computed differently between studies, we sought data from the corresponding authors to compute between-limb asymmetry (%) according to the following equation:
where Asymmetryi was the ith participant’s between-limb asymmetry (%), Limbmax was maximum force value generated by either limb, and Limbmin was the maximum force value generated by the weaker limb. Due to the positively skewed nature of asymmetry data, a log transformation was applied to the raw data to create a normally distributed variable:
where Transformedi is the ith participant’s log-transformed asymmetry score and ln is the natural logarithm. Note that these log-transformed data were used for all subsequent analysis involving between-limb asymmetry.
2.6 Data Analysis
Meta-analysis and meta-regression were conducted using the “meta” [24] and “metafor” [25] packages in R [26]. Data pertaining to the primary outcome (i.e. eccentric knee flexor strength or limb-asymmetry data) were converted to standardised mean differences (SMD) and 95% confidence intervals (CI). These data were pooled across studies using a random effects model, with a restricted maximum likelihood method used to estimate variance. Each pooled effect size was interpreted as trivial (< 0.20), small (0.20–0.49), moderate (0.50–0.79) or large (≥ 0.80) [27]. For each meta-analysis, visual inspection of funnel plots was used to assess publication bias and heterogeneity was evaluated using the I2 statistic. Meta-analyses were conducted for prospectively injured limbs compared to the uninjured control group limbs for all outcomes (i.e. absolute knee flexor strength, body mass normalised knee flexor strength and between-limb asymmetry).
In addition, contact with corresponding authors enabled the determination of which injured participants had suffered a HSI in the 12 months prior to testing, which was subsequently used to perform subgroup analysis on “recurrent” and “non-recurrent” injuries for each of the aforementioned outcome variables. Athletes were classified as “recurrent” if they had suffered a HSI (in the 12 months prior to testing) in the same leg that was injured within the study follow-up period.
Where possible, a meta-regression was performed to assess the impact of other potential effect modifiers, including the sport played, mean age, height and mass of each cohort as reported within each study. Meta-regression was also performed for the average strength of each cohort, which was determined by computing the mean (weighted by sample size) of the injured limbs, contralateral uninjured limb and control group absolute knee flexor strength.
3 Results
3.1 Search Strategy
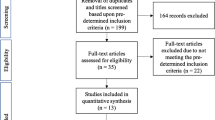
The search results are presented in Fig. 1. The initial search yielded 3585 items from all databases. After duplicate removal and title and abstract screening, 12 articles underwent independent application of the selection criteria, resulting in 6 articles in the systematic review and meta-analysis.
3.2 Risk of Bias Assessment
Only one [21] of the six included studies presented with a high risk of bias, with all others presenting a low risk. Full details of the scoring for the QUIPS tool for all included studies are provided in Supplementary Table S2.
3.3 Description of Studies
3.3.1 Participants
Across the 6 included studies, a total of 1100 male participants were included in the meta-analysis (weighted mean ± pooled SD; age = 25 ± 4 years; height = 1.83 ± 0.07 m; mass = 84 ± 9 kg). Of the included participants, 156 participants suffered a prospective unilateral HSI, and 944 participants remained uninjured during the follow-up periods. Two studies [17, 18] investigated elite soccer players (n = 376 participants, n = 55 injured) and another two studies [16, 20] investigated elite Australian Football players (n = 362 participants, n = 53 injured). The two remaining studies investigated elite Gaelic Football players [21] (n = 184 participants, n = 28 injured) or elite and sub-elite Rugby Union players [19] (n = 178 participants, n = 20 injured). Participant characteristics are summarised in Supplementary Table S3.
3.3.2 Testing Protocol
All studies conducted testing during the pre-season period, with three studies conducting knee flexor strength testing at the start of pre-season [16, 17, 20] and the remaining three studies conducting testing within pre-season [18, 19, 21]. All studies used the same protocol, involving one set of three maximal effort repetitions of the NHE on a Nordic testing device.
3.3.3 Injury Monitoring
Athletes were monitored for HSI occurrences after pre-season testing for periods of ~ 3 months [21], ~ 6 months [19] or 10 months [16,17,18, 20]. Two studies included only magnetic resonance imaging (MRI) confirmed HSIs [16, 20], two studies included a mix of HSIs diagnosed via either imaging (MRI or ultrasound) confirmation or physical/clinical examination [18, 19], one study included injuries confirmed by clinical examination [17], whilst the remaining study [21] reported only that injuries were diagnosed by the club physiotherapists or medical doctor. For all included studies, the occurrence of HSIs in the 12 months prior to testing was also recorded. Note that details of the testing protocol and injury surveillance of each study are provided in Supplementary Table S4.
3.3.4 Outcome Variables
Five [16,17,18, 20, 21] of the included studies calculated the average peak force (across the three repetitions), whilst one study [19] only reported the peak force (i.e. the highest force value recorded across the entire set of three repetitions). All studies reported absolute knee flexor strength (N) and knee flexor strength normalised to body mass (N kg−1). Between-limb asymmetry was reported by all studies albeit computed via different equations. Two studies [18, 20] reported between-limb imbalance in N, whilst the remaining studies expressed asymmetry as a percentage [16, 17, 19, 21]. As described in Sect. 2.5, original data were obtained from authors to recompute limb-asymmetry (in accordance with Eq. 1 for subsequent meta-analysis). One study [17] also reported knee flexor strength as torque (Nm) by accounting for the shank length. Since none of the other included studies had such data available, torque was not included in further analysis.
3.4 Strength Outcomes Quantified During the Performance of the NHE
3.4.1 Absolute Knee Flexor Strength
No significant differences in absolute knee flexor strength were observed between the prospectively injured limbs and the uninjured control group (SMD = − 0.22, 95% CI = − 0.50 to 0.05; Fig. 2a) or the recurrent injured limbs compared to the uninjured control group (SMD = − 0.32, 95% CI = − 0.77 to 0.13; Fig. 2b).
Standardised mean differences (SMD) of absolute eccentric knee flexor strength (N) quantified during performance of the Nordic hamstring exercise for hamstring strain injured limbs compared to the uninjured control group. Data are sub-grouped for a all injuries, b recurrent injuries, c non-recurrent injuries. Recurrent injury classification was achieved through author contact and was defined as athletes that suffered a hamstring strain injury (HSI) in the 12 months prior to test, and then suffered a subsequent HSI in the same leg during the follow-up period. Note that for one study [18], the recurrent and non-recurrent injured-group limbs could only be identified on a player-season level, not an individual participant level (due to participant de-identification). Due to 3 players in this study suffering injuries across both assessed seasons, the sum of recurrent and non-recurrent injuries exceeds the total amount of injuries reported in panel a
3.4.2 Normalised Knee Flexor Strength
Normalising knee flexor strength to body mass had no effect on any outcome, and the pooled effect sizes were almost identical to the absolute knee flexor strength. Specifically, effect size remained small for all injured limbs (SMD = − 0.23, 95%CI = − 0.55 to 0.10; Fig. 3a) or recurrently injured limbs (SMD = − 0.32, 95%CI = − 0.90 to 0.26; Fig. 3b) when compared to the uninjured group.
Standardised mean differences (SMD) of body mass normalised eccentric knee flexor strength (N kg−1) quantified during performance of the Nordic hamstring exercise for hamstring strain injured limbs compared to the uninjured control group. Data are sub-grouped for a all injuries, b recurrent injuries, c non-recurrent injuries. Recurrent injury classification was achieved through author contact and was defined as athletes that suffered a hamstring strain injury (HSI) in the 12 months prior to test, and then suffered a subsequent HSI in the same leg during the follow-up period. Note that for one study [18], the recurrent and non-recurrent injured-group limbs could only be identified on a player-season level, not an individual participant level (due to participant de-identification). Due to 3 players in this study suffering injuries across both assessed seasons, the sum of recurrent and non-recurrent injuries exceeds the total amount of injuries reported in panel a
3.4.3 Limb Asymmetry in NHE Strength
No significant differences in between-limb knee flexor strength asymmetry were found between all injured participants (SMD = 0.01, 95%CI = − 0.24 to 0.25; Fig. 4a) or recurrently injured participants (SMD = 0.28, 95%CI = − 0.14 to 0.70; Fig. 4b) compared to the uninjured group.
Standardised mean differences (SMD) of log-transformed between-limb asymmetry (%) of eccentric knee flexor strength quantified during performance of the Nordic hamstring exercise for hamstring strain injured limbs compared to the uninjured control group. Data are sub-grouped for a all injuries, b recurrent injuries, c non-recurrent injuries. Recurrent injury classification was achieved through author contact and was defined as athletes that suffered a hamstring strain injury (HSI) in the 12 months prior to test, and then suffered a subsequent HSI in the same leg during the follow-up period. Note that for one study [18], the recurrent and non-recurrent injured-group limbs could only be identified on a player-season level, not an individual participant level (due to participant de-identification). Due to 3 players in this study suffering injuries across both assessed seasons, the sum of recurrent and non-recurrent injuries exceeds the total amount of injuries reported in panel a
3.4.4 Meta-regression
No significant relationships between absolute knee flexor strength and any covariate investigated (sport played, athlete age, height and mass or average absolute NHE strength of cohort) were found (p ≥ 0.26). For between-limb asymmetry, a significant effect was found for average age (p = 0.007), but not any other variable (p ≥ 0.24). Visualisation of regression relationships for continuous variables is provided in Fig. 5, whilst a full summary of meta-regression statistical results is provided in Supplementary Table S5.
Meta-regression of eccentric knee flexor strength quantified during performance of the Nordic hamstring exercise (NHE) standardised mean difference (SMD), between prospectively hamstring strain injured and uninjured limbs and continuous covariates. Regression analysis was conducted for eccentric knee flexor strength presented in absolute terms (top row, positive SMD indicates greater strength in injured limbs) or between-limb asymmetry (bottom row, positive SMD indicates greater asymmetry in the injured group). Bubbles, data points representing each study (size of each bubble is inversely proportional to the standard error of the study); black line, regression line of best fit; grey shaded area, 95% confidence interval of regression line
4 Discussion
This systematic review and meta-analysis are the first to comprehensively synthesise the available data pertaining to eccentric knee flexor strength quantified during performance of the NHE and the occurrence of future HSI. Overall, our analysis of 1100 participants revealed that pre-season knee flexor strength quantified during performance of the NHE was not associated with HSI. This finding was consistent regardless of whether strength was expressed as absolute, body mass normalised, or as a limb-asymmetry percentage. Additionally, our meta-regression analysis found that these findings were generally not moderated by the sports played, or the average height, mass or strength of each cohort.
The importance of eccentric knee flexor strength in HSI has been investigated extensively in the literature. Specifically, the NHE has received significant attention recently, as its implementation as a training intervention has been consistently shown to reduce the incidence of HSI, relative to groups that do not perform the exercise [13, 14]. It is therefore conceivable that the measurement of knee flexor strength during the NHE may offer insight into the risk of subsequent HSI. The first study in this area of research found that lower eccentric knee flexor strength during the NHE at the start of pre-season was associated with increased HSI risk in the subsequent season in a cohort of Australian Football players [16]. Further work across a number of different football codes [17,18,19,20,21], however, has been conflicting. Our meta-analysis combined these data and revealed, overall, no significant differences in eccentric knee flexor strength quantified during performance of the NHE between the prospectively injured limbs and either the contralateral uninjured limbs or the uninjured control group. Whilst this suggests there is no relationship between eccentric knee flexor strength quantified during performance of the NHE and future HSI, it is important to put these findings into context.
Our a-priori power analysis suggested the six studies would achieve adequate power (> 90%) to detect a moderate effect size (0.50), even with a conservative within-study sample size estimate, and assuming the presence of high between-study heterogeneity (Supplementary Figure S1). The results from the current meta-analysis therefore indicate that if there is any effect of eccentric knee flexor strength, quantified during performance of the NHE, on future HSI risk, the effect is at most small. The current meta-analysis, however, was not sufficiently powered to detect small effect sizes (i.e. 0.20). Since the pooled effect sizes observed in this analysis were small for all comparisons, we cannot definitively conclude that there are no differences in NHE strength between injured and uninjured legs, but rather that any differences (if they do exist) are likely to be small, at most. Studies with larger sample sizes would be required to detect such small effects; however, the clinical utility of such data is limited. For context, the small effect sizes observed in the meta-analysis correspond to pooled mean differences of − 18 N (95%CI = − 40 to 4 N) or − 0.22 N kg−1 (95%CI = − 0.54 to 0.10 N kg−1) between the injured limbs and the uninjured control groups. Importantly, the minimal detectable change of the Nordic hamstring device has been reported to be > 60 N [15].
Despite the well-documented benefit of performing eccentric knee flexor exercises for reducing HSI risk [28, 29], it is clear that measurement of eccentric knee flexor strength alone cannot predict HSI occurrence [20], and likely interacts with other factors such as age and previous history of HSI [16, 17, 19]. We attempted to account for these factors via meta-regression or subgroup analysis, respectively; however, due to the multi-factorial nature of HSI, there are many other potentially influential factors that were unaccounted for in our analysis. For example, shorter biceps femoris long head fascicle lengths have been shown to be associated with greater risk of HSI [17]. Isokinetic eccentric hamstring training [30], as well as the NHE [31,32,33,34,35,36], have been shown to not only increase eccentric knee flexor strength, but also increase biceps femoris long head fascicle lengths. However, there are numerous other methods by which eccentric knee flexor strength can be improved, some of which are associated with shortening of biceps femoris long head fascicle lengths (thus conceivably increasing HSI risk), such as concentric isokinetic exercise [30]. Additionally, muscle fascicle lengths are rapidly adaptable to both training and de-training [30,31,32], and changes across a playing season, particularly in those with a prior HSI [37]. Subsequently, future work investigating HSI risk factors should aim to comprehensively assess as many prospective factors as possible (in addition to eccentric knee flexor strength), including muscle architecture and accounting for exposure [38, 39].
One important result of our analysis is the consistency of our findings across various methods of expressing eccentric knee flexor strength quantified during performance of the NHE. Debate around the normalisation of NHE knee flexor strength data has been presented in the literature, with some authors arguing that the most commonly expressed metric of absolute strength is fundamentally flawed due to failure to account for differing body mass and/or lever arms between individuals [40]. However, all studies included in our analysis also reported body mass normalised knee flexor strength, and our meta-analysis showed a very similar relationship to HSI between absolute and normalised strength (Figs. 2, 3, 5, Supplementary Figure S5). Additionally, our meta-regression showed that body mass and height had no moderating effect on the results of our analysis. However, it is important to acknowledge that our meta-regression assessed the relationship between the average characteristics of each cohort (i.e. age, height, mass and strength) and the effect size between the injured and uninjured groups. Subsequently, a more detailed analysis incorporating individual data points may be needed to more comprehensively determine the value of normalisation of NHE knee flexor strength data to mass, height, lever length or an allometric scaling approach.
Despite the key insights provided by this study, our meta-analysis is not without limitations. First, the comprehensiveness of our search strategy cannot be guaranteed; thus, it is possible that some relevant literature was not obtained. However, given that only six articles were obtained from our search, it is unlikely there is additional literature that would have not been identified via citation tracking and reference list searching. In these six included articles, the risk of bias cannot be completely avoided. However, our quality assessment revealed a high risk of bias for only one study [21] which received this classification due to a lack of clear definition of the outcome (HSI) and a lack of consideration of potential important confounders within the analysis. A meta-analysis and meta-regression of only six studies presents some additional limitations which must be acknowledged, including sparse-data bias [41, 42] and publication bias. Evaluation of publication bias was done via visual inspection of funnel plots, yet such an approach can offer only limited insight with a low number of studies. However, our power analysis suggested that five studies were sufficient to detect a moderate (≥ 0.50) effect size with > 80% power for our control group comparisons (Figs. 2, 3, 4) and contralateral limb comparisons (Supplementary Figure S2), even in the presence of high between-study heterogeneity (Supplementary Figure S1). Further to this, our analysis suggests that an estimated 19 studies would be needed to obtain adequate statistical power to detect small (0.20) effect sizes for control group comparisons (Supplementary Figure S3). It should also be noted that the analysis pertaining to recurrent injuries is particularly impacted by the small number of recurrent injuries (n = 37), and thus an even greater number of studies would be needed to substantiate these findings. Furthermore, additional studies would also increase the veracity of the findings from our meta-regression, which is commonly recommended to include at least 10 studies [43]. Subsequently, our meta-analysis and meta-regression provides a much-needed synthesis of the presently available data for clinicians, until such a time that these additional studies would be completed. Based on our findings, clinicians should be aware that such future studies, if they are conducted, are expected to demonstrate substantial heterogeneity (Supplementary Figure S4). Finally, it is important to recognise that our meta-analysis pertains specifically to pre-season knee flexor strength measures with follow-up periods of between ~ 3 and 10 months. It is possible that more frequent strength tests (e.g. in-season) over longer periods may yield different findings. Additionally, other methods of eccentric knee flexor strength assessment [44, 45] may provide alternative conclusions if prospective data were available.
5 Conclusions
Based on the available evidence, this systematic review and meta-analysis showed that pre-season eccentric knee flexor strength quantified during performance of the NHE is not associated with future HSI. This finding was consistent regardless of whether knee flexor strength was expressed in absolute terms, normalised to body mass, or expressed as a between-limb asymmetry. Despite the promising early work in the area, our pooled analysis of 1100 participants suggests that knee flexor strength quantified during performance of the NHE alone provides limited insight about future HSI.
Change history
08 May 2021
A Correction to this paper has been published: https://doi.org/10.1007/s40279-021-01485-y
References
Ekstrand J, Walden M, Hagglund M. Hamstring injuries have increased by 4% annually in men’s professional football, since 2001: a 13-year longitudinal analysis of the UEFA Elite Club injury study. Br J Sports Med. 2016;50(12):731–7.
Orchard JW, Seward H, Orchard JJ. Results of 2 decades of injury surveillance and public release of data in the Australian Football League. Am J Sports Med. 2013;41(4):734–41.
Roe M, Murphy JC, Gissane C, et al. Time to get our four priorities right: an 8-year prospective investigation of 1326 player-seasons to identify the frequency, nature, and burden of time-loss injuries in elite Gaelic football. PeerJ. 2018;6:e4895.
Hallén A, Ekstrand J. Return to play following muscle injuries in professional footballers. J Sports Sci. 2014;32(13):1229–36.
Ruddy JD, Pietsch S, Maniar N, et al. Session availability as a result of prior injury impacts the risk of subsequent non-contact lower limb injury in elite male Australian footballers. Front Physiol. 2019;10:737.
Hoffman DT, Dwyer DB, Bowe SJ, et al. Is injury associated with team performance in elite Australian football? 20 years of player injury and team performance data that include measures of individual player value. Br J Sports Med. 2020;54(8):475–9.
Verrall GM, Kalairajah Y, Slavotinek JP, et al. Assessment of player performance following return to sport after hamstring muscle strain injury. J Sci Med Sport. 2006;9(1–2):87–90.
Whiteley R, Massey A, Gabbett T, et al. Match high-speed running distances are often suppressed after return from hamstring strain injury in professional footballers. Sports Health. 2020. https://doi.org/10.1177/1941738120964456 ([Online ahead of print]).
van Mechelen W, Hlobil H, Kemper HC. Incidence, severity, aetiology and prevention of sports injuries. A review of concepts. Sports Med. 1992;14(2):82–99.
Finch C. A new framework for research leading to sports injury prevention. J Sci Med Sport. 2006;9(1–2):3–9.
Green B, Bourne MN, van Dyk N, et al. Recalibrating the risk of hamstring strain injury (HSI)—a 2020 systematic review and meta-analysis of risk factors for index and recurrent HSI in sport. Br J Sports Med. 2020;2020:4.
Bahr R, Holme I. Risk factors for sports injuries–a methodological approach. Br J Sports Med. 2003;37(5):384–92.
van Dyk N, Behan FP, Whiteley R. Including the Nordic hamstring exercise in injury prevention programmes halves the rate of hamstring injuries: a systematic review and meta-analysis of 8459 athletes. Br J Sports Med. 2019;53(21):1362–70.
Al Attar WSA, Soomro N, Sinclair PJ, et al. Effect of injury prevention programs that include the nordic hamstring exercise on hamstring injury rates in soccer players: a systematic review and meta-analysis. Sports Med. 2017;47(5):907–16.
Opar DA, Piatkowski T, Williams MD, et al. A novel device using the Nordic hamstring exercise to assess eccentric knee flexor strength: a reliability and retrospective injury study. J Orthop Sports Phys Ther. 2013;43(9):636–40.
Opar DA, Williams MD, Timmins RG, et al. Eccentric hamstring strength and hamstring injury risk in Australian footballers. Med Sci Sports Exerc. 2015;47(4):857–65.
Timmins RG, Bourne MN, Shield AJ, et al. Short biceps femoris fascicles and eccentric knee flexor weakness increase the risk of hamstring injury in elite football (soccer): a prospective cohort study. Br J Sports Med. 2016;50(24):1524–35.
van Dyk N, Bahr R, Burnett AF, et al. A comprehensive strength testing protocol offers no clinical value in predicting risk of hamstring injury: a prospective cohort study of 413 professional football players. Br J Sports Med. 2017;51(23):1695–702.
Bourne MN, Opar DA, Williams MD, et al. Eccentric knee flexor strength and risk of hamstring injuries in rugby union: a prospective study. Am J Sports Med. 2015;43(11):2663–70.
Ruddy JD, Shield AJ, Maniar N, et al. Predictive modeling of hamstring strain injuries in elite Australian footballers. Med Sci Sports Exerc. 2018;50(5):906–14.
Roe M, Delahunt E, McHugh M, et al. Association between eccentric knee flexor strength and hamstring injury risk in 185 elite Gaelic football players. Scand J Med Sci Sports. 2020;30(3):515–22.
Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210.
Hayden JA, van der Windt DA, Cartwright JL, et al. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158(4):280–6.
Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22(4):153–60.
Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36(3):48.
R Development Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2020.
Cohen J. Statistical power analysis for the behavioral sciences: Lawrence Erlbaum; 1988. https://doi.org/10.4324/9780203771587
Petersen J, Thorborg K, Nielsen MB, et al. Preventive effect of eccentric training on acute hamstring injuries in men’s soccer: a cluster-randomized controlled trial. Am J Sports Med. 2011;39(11):2296–303.
van der Horst N, Smits DW, Petersen J, et al. The preventive effect of the nordic hamstring exercise on hamstring injuries in amateur soccer players: a randomized controlled trial. Am J Sports Med. 2015;43(6):1316–23.
Timmins RG, Ruddy JD, Presland J, et al. Architectural changes of the biceps femoris after concentric or eccentric training. Med Sci Sports Exerc. 2016;48(3):499–508.
Presland JD, Timmins RG, Bourne MN, et al. The effect of Nordic hamstring exercise training volume on biceps femoris long head architectural adaptation. Scand J Med Sci Sports. 2018;28(7):1775–83.
Pollard CW, Opar DA, Williams MD, et al. Razor hamstring curl and Nordic hamstring exercise architectural adaptations: Impact of exercise selection and intensity. Scand J Med Sci Sports. 2019;29(5):706–15.
Bourne MN, Duhig SJ, Timmins RG, et al. Impact of the Nordic hamstring and hip extension exercises on hamstring architecture and morphology: implications for injury prevention. Br J Sports Med. 2017;51(5):469–77.
Lacome M, Avrillon S, Cholley Y, et al. Hamstring eccentric strengthening program: does training volume matter? Int J Sports Physiol Perform. 2019;2019:1–27.
Alonso-Fernandez D, Docampo-Blanco P, Martinez-Fernandez J. Changes in muscle architecture of biceps femoris induced by eccentric strength training with nordic hamstring exercise. Scand J Med Sci Sports. 2018;28(1):88–94.
Ribeiro-Alvares JB, Marques VB, Vaz MA, et al. Four weeks of Nordic hamstring exercise reduce muscle injury risk factors in young adults. J Strength Cond Res. 2018;32(5):1254–62.
Timmins RG, Bourne MN, Hickey JT, et al. Effect of prior injury on changes to biceps femoris architecture across an Australian Football League season. Med Sci Sports Exerc. 2017;49(10):2102–9.
Ruddy JD, Pollard CW, Timmins RG, et al. Running exposure is associated with the risk of hamstring strain injury in elite Australian footballers. Br J Sports Med. 2018;52(14):919–28.
Duhig S, Shield AJ, Opar D, et al. Effect of high-speed running on hamstring strain injury risk. Br J Sports Med. 2016;50(24):1536–40.
Buchheit M, Cholley Y, Nagel M, et al. The effect of body mass on eccentric knee-flexor strength assessed with an instrumented Nordic hamstring device (NordBord) in football players. Int J Sports Physiol Perform. 2016;11(6):721–6.
Greenland S, Mansournia MA, Altman DG. Sparse data bias: a problem hiding in plain sight. BMJ. 2016;352:i1981.
Lin L. Bias caused by sampling error in meta-analysis with small sample sizes. PLoS ONE. 2018;13(9):e0204056.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane handbook for systematic reviews of interventions version 6.0 (updated July 2019). Cochrane; 2019. www.training.cochrane.org/handbook.
Hickey JT, Hickey PF, Maniar N, et al. A novel apparatus to measure knee flexor strength during various hamstring exercises: a reliability and retrospective injury study. J Orthop Sports Phys Ther. 2018;48(2):72–80.
Hegyi A, Lahti J, Giacomo JP, et al. Impact of hip flexion angle on unilateral and bilateral nordic hamstring exercise torque and high-density electromyography activity. J Orthop Sports Phys Ther. 2019;49(8):584–92.
IntHout J, Ioannidis JP, Rovers MM, et al. Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open. 2016;6(7):e010247.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist in the preparation of this article.
Conflict of interest
Dr David Opar is listed as a co-inventor on a patent filed for a field-testing device of eccentric hamstring strength (PCT/AU2012/001041.2012) and is a minority shareholder in Vald Performance Pty Ltd, the company responsible for commercialising the device. The association between measures derived from the device and future hamstring strain injury is directly examined in this manuscript. Dr Opar is also the Chair of the Vald Performance Research Committee, a role that is unpaid. Dr Opar has received funding from Vald Performance for research unrelated to the current manuscript. Dr Opar’s brother and brother-in-law are employees of Vald Performance. Dr Opar’s brother is a minority shareholder in Vald Performance Pty Ltd. Ryan Timmins, Fearghal Behan, Jack Hickey, Nicol van Dyk, Kara Price and Nirav Maniar declare that they have no conflicts of interest relevant to the content of this review.
Availability of data and material
Access to data and/or material can be sought via contacting the corresponding author.
Code availability
Not applicable.
Authorship contributions
DAO, RGT, FPB, JTH, NM conceived the study. DAO, FPB and KP completed study protocol and registration. DAO and RGT completed database searches and extraction. RGT and JTH completed title and abstract screening. FPB and JTH completed full text review. RGT, NvD and FPB completed risk of bias assessment. NM, JTH and NvD completed data extraction. NM and JTH completed data analysis. DAO drafted the Introduction and Methods. NM drafted the Results and Discussion. All authors reviewed, revised and approved the final manuscript.
Additional information
The original artilce has been updated: Due to authors middle name udpate.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Opar, D.A., Timmins, R.G., Behan, F.P. et al. Is Pre-season Eccentric Strength Testing During the Nordic Hamstring Exercise Associated with Future Hamstring Strain Injury? A Systematic Review and Meta-analysis. Sports Med 51, 1935–1945 (2021). https://doi.org/10.1007/s40279-021-01474-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-021-01474-1