Abstract
Objectives
Describe the trajectories of body mass index (BMI), waist circumference, and aerobic fitness in children and identify different outcomes of guideline-recommended physical activity (PA) in a subset of active children.
Methods
We recruited students from 10 public primary schools and obtained repeated measures of BMI, waist circumference, and aerobic fitness over 30 months. Aerobic fitness was measured with the Andersen test. We objectively measured physical activity behaviour with accelerometers and classified children as ‘physically active’ when they achieved ≥ 60 min of moderate-to-vigorous PA per day (guideline concordance). Univariate trajectories of BMI, waist circumference, and aerobic fitness were calculated for all children, and we constructed a multi-trajectory model comprising all outcomes in the subgroup of physically active children. The construct validity of all models was investigated by examining for between-group differences in cardiovascular disease risk factors obtained from fasting blood samples.
Results
Data from 1208 children (53% female) with a mean (SD) age of 8.4 (1.4) years were included. The univariate trajectory models identified three distinct trajectories for BMI, waist circumference, and aerobic fitness. The multi-trajectory model classified 9.1% of physically active children as following an ‘overweight/obese/low fitness’ trajectory. There were moderate-to-large differences in cardiovascular risk factors between all trajectory groups (p < 0.001; d = 0.4–1.20).
Conclusion
We identified distinct developmental trajectories of BMI, waist circumference, and aerobic fitness in children. Nearly one in 10 children who met PA guideline recommendations followed an unfavourable health trajectory. Health-related PA recommendations may be insufficient for some children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Children follow distinct developmental trajectories of BMI, waist circumference, and aerobic fitness. |
Nearly one in 10 children meeting guidelines for health-related physical activity follow an unfavourable health trajectory. |
Guideline recommendations for health-related PA may be insufficient for some children. |
1 Introduction
Achieving sufficient health-related physical activity (PA) is an effective strategy to prevent 26 chronic diseases including obesity, non-alcoholic fatty liver disease, cardiovascular diseases, hypertension, and type 2 diabetes [1]. Insufficient PA imposes a large socioeconomic burden, with physical inactivity costing the European economy an estimated €80 billion annually [2]. A 20% reduction in physical inactivity could save the European economy €16.1 billion per year [2].
Although the benefits of PA are established at the population level, the global prevalence of insufficient PA in adults is 27.5%. Inactivity is twice as common in high-income (36.8%) compared to low-income countries (16.2%) [3], and may be a key driver of geographic disparities in health conditions such as obesity [4].
Unfortunately, global PA estimates in children (4–11 years) suggest a similar pattern to adults. On average, children engage in 22–45 min of daily moderate-to-vigorous intensity PA (MVPA) [5], well below the 60 min recommended by PA guidelines from the World Health Organization and others [6, 7]. This is notable as PA behaviours developed in childhood track into adulthood [8].
However, heterogeneity in the individual responses to PA and limitations in previous studies challenge the interpretation of current evidence. There are large inter-individual differences in PA responses, with some people demonstrating negligible changes in aerobic capacity, anthropometrics, or disease risk markers, even when adhering to PA recommendations [9,10,11,12,13,14]. These individuals, often characterized as PA non-responders [9,10,11,12,13,14,15,16,17,18,19], may require a greater volume or intensity of activity, beyond general recommendations [9, 18, 20, 21], or may fail to respond to specific PA programs altogether [21]. This understanding of PA responsiveness is based on research in adults, with only a few small (n = 11–73) studies reporting differential exercise responses in young people with respect to insulin sensitivity [11], adiposity [12], as well as body mass index and waist circumference [19]. Whether children’s’ PA outcomes parallel that seen in adults remains to be established.
Understanding PA responsiveness is further complicated by the lack of a universal definition of ‘responders’ and ‘non-responders’. Our group has previously used tertile [12], quartile [22], or percentile [11] cut-points for PA non-response, while others have used clinical meaningful changes [10], or technical error [23]. Importantly, past research efforts have focused on exercise training and not habitual health-related PA behaviour. A better understanding of these concepts is fundamental to adoption of PA recommendations in preventive treatment and personalized medicine [24]. Specifically, the identification of longitudinal patterns in health-related outcomes would be beneficial. Recent evidence shows that children may follow distinct trajectories of body mass index (BMI) as they age and these patterns relate to cardiorespiratory fitness [25]. However, little is known about the development of BMI and other health-related outcomes in physically active children.
Therefore, the objectives of this study were to: (1) describe the individual, developmental trajectories of body mass index (BMI), waist circumference, and aerobic fitness in children, (2) identify different outcomes to guideline-recommended PA by estimating multivariate trajectories of BMI, waist circumference, and aerobic fitness in a subset of active children, and (3) examine the construct validity of the trajectory groups by testing for differences in cardiovascular risk factors. We hypothesised that distinct trajectories would be evident for each outcome, and that the multivariate trajectory model would identify one or more subgroups of physically active children who follow an unfavourable health trajectory.
2 Methods
2.1 Study Design and Participants
This prospective longitudinal study was nested in the Childhood Health, Activity and Motor Performance School (CHAMPS-DK) study. The CHAMPS-DK study is an ongoing quasi-experimental trial evaluating the effects of physical education in primary school students. The study sample and procedures have been described in detail previously [26, 27]. Briefly, all public primary schools within the municipality of Svendborg, Denmark (N = 19) were invited, and ten schools participated in the study. Students attending four schools received the traditional quantity of physical education (90 min/week), while students in six schools underwent an extended physical education program totaling 270 min per week.
In the current analysis, we included data from baseline through the 30-month follow-up, and combined data across the two treatment arms into a common cohort. Anthropometric variables were measured at baseline, and after 6, 12, 18, 24, and 30 months. We measured aerobic fitness at baseline, 6 months, and 12, 18, and 30 months. Blood testing was performed at baseline and the 24-month follow-up, while physical activity behaviour was measured at 12 and 22 months.
The study was performed in accordance with the Declaration of Helsinki, approved by the Regional Scientific Ethical Committee of Southern Denmark (ID S-20080047), and registered with the Danish Data Protection Agency (J.nr. 2008-41-2240). All children gave verbal assent and all parents provided written informed consent to participate before study enrollment.
2.2 Physical Activity
We measured PA behaviour using the Actigraph GT3X accelerometer (Actigraph, Pensacola Florida) during 2 measurement periods, 1 year apart. Trained research staff instructed children and parents regarding appropriate use, and fit the accelerometers to each child’s right hip with a customized elastic belt. Children were instructed to wear the device from waking in the morning until they went to bed, except when bathing or swimming.
A customized software program (Propero, version 1.0.18, University of Southern Denmark, Odense, Denmark) processed all accelerometry data. Accelerations were recorded every 2 s and subsequently collapsed into 10-second epochs. Digitalized accelerometer signals were filtered with 0.25–2.5 HZ band limits to help eliminate accelerations not associated with human movement (e.g., vibration). To distinguish inactivity from periods of non-wear, we interpreted readings of zero activity lasting at least 30 consecutive minutes as ‘accelerometer non-worn’. We included physical activity data when the child’s wear time was at least 10 h per day on 4 or more days.
We estimated daily time spent in MVPA intensities using established cut-points [28]. This information was used to classify children as meeting recommended levels of health-related PA (at least 60 min of MVPA). Children were classified as ‘physically active’ when they averaged a minimum of 60 min of daily MVPA (i.e., guideline concordance) at both measurement periods.
2.3 Anthropometrics and Aerobic Fitness
Height and weight were measured with children wearing light clothes and barefoot. We measured height to the nearest 0.5 cm with a portable stadiometer (SECA 214, Seca Corporation, Hanover, MD, USA), and weight to the nearest 0.1 kg using a calibrated Tanita BWB-800S digital scale (Tanita Corporation, Tokyo, Japan). We calculated BMI as weight (kg)/height (m)2, and classified outcomes as normal weight, overweight, or with obesity according to criteria from the International Obesity Task Force [29].
Waist circumference was measured with a tape measure at the level of the umbilicus, to the nearest 0.5 centimetre (cm), following normal expiration. The measure was then repeated. If differences greater than 1 cm were identified, a third measure was obtained. We used the mean of the two closest measures. Waist circumference outcomes were used to classify children as normal weight, overweight, or with obesity using sex and age-adjusted criteria [30].
Cardiorespiratory fitness was measured with the Andersen test, a maximal running test developed for children [31]. Tests were conducted on an indoor court with wood flooring and 20-m running lanes marked out with cones and lines at each end of the lane. Children ran as fast as possible down the lane, touched behind the line with one hand, and turned and ran back in the opposite direction. After 15 s, children stopped immediately when hearing a whistle. Following 15 s of rest, the process repeated, with children attempting to cover the greatest distance possible. The test outcome was total distance run by each child in 10 min, and this was monitored by trained research staff. This test has good test–retest reliability and concurrent validity when compared with direct VO2max testing in a similar sample of children [32].
2.4 Cardiovascular Risk Factors
Trained research staff obtained fasting morning blood samples from children at each primary school, wherein fasting status was confirmed with immediate plasma-glucose measures. We immediately stored the samples on ice and transported them to a lab, where they were pipetted, centrifuged, and stored at − 80 °C within 4 h. All analyses were performed in a certified laboratory at the University of Vienna using a Roche/Hitachi cobas c system (Roche, Mannheim, Germany). Cholesterol, triglycerides, and glucose were analyzed using enzymatic, colorimetric methods. Insulin was analyzed with a solid phase enzyme-labeled chemiluminescent immunometric assay. We calculated homeostasis assessment model-estimated insulin resistance (HOMA-IR) scores using the following formula: HOMA-IR = insulin (μU/mL) × glucose (mmol/L)/22.5 [33].
We measured systolic blood pressure at the left arm using an automated blood pressure monitor [Welch Allyn® (New York, USA) vital signs monitor 300 series with FlexiPort™]. Before assessing blood pressure, participants sat quietly for 5 min with flat feet on the floor. Blood pressure was then measured at 1-min intervals, until 3 stable measures, or 5 total measures were obtained. The mean of the last 3 measures was used for analysis.
We combined several cardiovascular risk factors into a clustered cardiovascular risk score. Clustered scores may be preferable to single risk factors to estimate cardiovascular health in children [34], and clustered risk tracks into young adulthood [35]. Recent research recommends the use of combined continuous risk factors to estimate the cardiometabolic risk in children [36]. We calculated clustered cardiovascular risk scores by summing the standardized scores of total cholesterol:HDL ratio, log triglycerides, log HOMA-IR, and systolic blood pressure [37, 38], and converting scores to positive values. Larger scores represent higher levels of cardiovascular disease risk.
2.5 Statistical Analyses
All analyses were conducted using Stata 15.1 software (StataCorp, College Station, TX, USA). We modeled univariate and multivariate trajectories, in two steps, using group-based trajectory and group-based multi-trajectory models. These person-centered statistical approaches identify clusters of individuals who follow similar patterns of change (i.e., trajectories) over time [39]. A specialized application of finite mixture modeling, group-based trajectory modeling can identify meaningful subgroups based on trajectory group membership [40, 41]. Multi-trajectory modeling further allows for the identification of latent clusters of individuals who follow similar trajectories across multiple outcomes of interest [42]. Group-based trajectory and multi-trajectory models use maximum likelihood estimation to approximate trajectory distributions and do not assume that a population comprises distinct groups; features that distinguish this approach from growth mixture modeling [40].
We excluded participants with less than three repeated measures, and modeled trajectories as a function of age. Group-based trajectory and multi-trajectory models handle missing data with maximum likelihood estimation, resulting in asymptotically unbiased parameter estimates when data are missing at random [40]. Step one of the analysis (objective 1) involved univariate modeling of data from all participants to estimate trajectories for each outcome (BMI, waist circumference, aerobic fitness) independently. We first constructed single class models applying a censored normal distribution and increased the number of classes and complexity of the polynomial distributions (e.g., linear, quadratic, cubic) until optimal models were identified. In step two (objective 2), we used data from the subgroup of physically active children who met guideline recommendations for health-related PA. We similarly constructed multi-trajectory models to represent the multivariate longitudinal courses of BMI, waist circumference, and aerobic fitness together as a function of age.
Initial judgements of optimal model specification were made using the Bayesian information criterion. However, decisions of model fit cannot be reduced to a single metric [40]. Our modeling decisions were also based on a combination of statistical and clinical judgments, and we subsequently tested the models using four a priori diagnostic criteria: (1) a minimum average posterior probability of group membership of 0.7; (2) close correspondence between the estimated group membership probability and the proportion of participants assigned to each group based on the posterior probability; (3) minimum odds of correct classification greater than five; and (4) precise confidence intervals around estimations of group membership probabilities [40, 41].
To explore the construct validity of the trajectory groups identified in the multi-trajectory model (objective 3), we generated descriptive statistics for clustered cardiovascular risk, stratified by trajectory class. Between-group differences between trajectory classes were examined with analysis of variance and standardized mean differences estimated with Cohen’s d statistics. Alpha was 5% for all inferential analyses.
3 Results
Data from 1207 children were used in the BMI and waist circumference trajectory analyses, while 1145 children contributed data to the aerobic fitness analysis. We classified 522 children as ‘physically active’ based on achieving at least 60 min of daily MVPA during both measurement periods. The baseline characteristics of physically active children and the entire sample are presented in Table 1. The group-based trajectory and group-based multi-trajectory models achieved adequate performance according to our predefined criteria; all posterior probability values were > 0.90, and odds of correct classification were > 9 (Table 2).
3.1 Univariate Trajectories of All Children
The BMI, waist circumference, and aerobic fitness models all identified three distinct trajectory groups with linear or quadratic polynomial distributions that increased as a function of age (Fig. 1a–c). We categorized the trajectory groups according to their relative distributions or overweight/obese status. BMI and waist circumference trajectory groups were labeled as ‘low’ (BMI 50.2%; waist circumference 55.9% of children), ‘moderate’ (BMI 39.3%; waist circumference 35.6% of children), or overweight/obese (BMI 10.5%; waist circumference 8.5% of children). Aerobic fitness trajectory groups were labeled as ‘low’ (14.8% of children), ‘moderate’ (49.1% of children) or ‘high’ (36.2% of children).
Developmental univariate trajectories of a body mass index, b waist circumference, and c aerobic fitness for all children from age 6–12.5 years with prevalence estimates. Point estimates are average scores, shaded regions indicate 95% confidence intervals. Dashed lines show cut-points for overweight classification1. 1Cut-points calculated using body mass index criteria [29] for body mass index panels and waist circumference criteria [30] for waist circumference panels
3.2 Multivariate Trajectories of Physically Active Children
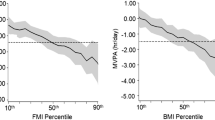
The multi-trajectory model identified three distinct linear or quadratic trajectory groups of children who met PA guideline recommendations. We categorized the trajectory groups according to their relative distributions or overweight/obese status (Fig. 2). Trajectory groups were labeled as normal weight/high fitness (48.4% of children), normal weight/moderate fitness (42.5% of children), and overweight/obese/low fitness (9.1% of children). Children in the overweight/obese/low fitness trajectory group tended to be overweight or with obesity according to BMI and waist circumference criteria and lower aerobic fitness compared to children in the other groups.
Developmental multivariate trajectories of body mass index, waist circumference, and aerobic fitness for physical activity guideline-concordant children from age 6–12.5 years showing three multi-trajectory classes with prevalence estimates. Point estimates are average scores, shaded regions indicate 95% confidence intervals. Dashed lines show cut-points for overweight classification. Cut-points calculated using body mass index criteria [29] for body mass index panels and waist circumference criteria [30] for waist circumference panels
3.3 Construct Validity
Mean differences in clustered cardiovascular risk scores between the trajectory groups are presented in Table 3. In the BMI and waist circumference models, we identified moderate-to-large (d range = 0.67–1.20) increases in clustered cardiovascular risk scores between the overweight/obese trajectory group and the ‘low’ and ‘moderate’ groups (p < 0.001). Similarly, the low aerobic fitness trajectory group had greater clustered cardiovascular risk than children in the moderate fitness (p < 0.001; d = 0.40) or high fitness (p < 0.001; d = 0.78) trajectory groups. In the multi-trajectory analysis, children assigned to the overweight/obese/low fitness trajectory group had increased clustered cardiovascular risk scores compared to children following normal weight/moderate fitness (p < 0.001; d = 0.79) and normal weight/high fitness (p < 0.001; d = 1.04) trajectories.
4 Discussion
The main findings of the study were the identification of (1) discrete developmental trajectories of BMI, waist circumference, and aerobic fitness in a general cohort of children; and (2) in physically active children, the classification of subgroups defined by different courses of BMI, waist circumference, and aerobic fitness identified by a multi-trajectory model. These subgroups may represent distinct phenotypes resulting from different responses to guideline-concordant PA behaviour. The construct validity of the trajectory groups in both the general and physically active cohorts was supported by moderate-to-large between-group differences in a clustered cardiovascular risk factor score.
The univariate analyses identified three distinct trajectory subgroups increasing as a function of age across each outcome measure. Noteworthy here, however, are the distinct trajectories identified within the cohort, which may at least in part explain the previously identified individual variability in longitudinal BMI trends in children [43, 44]. The increase in BMI approximated 0.2–0.4 kg/m2 per annum for the low- to high-trajectory groups, which accords with the expected median (~ 0.4 kg/m2) BMI-for-age trajectory estimated from a Danish cohort [45].
Corresponding with the univariate analyses, the multi-trajectory model identified three distinct trajectory subgroups within the cohort of physically active children. Using the 60-min of daily MVPA criteria, we identified 522 guideline-concordant children. Within this cohort, approximately half (48.4%) of the children followed a ‘normal weight/high fitness’ trajectory, indicated by lower increments in BMI and WC and higher increments in aerobic fitness with increasing age. Conversely, nearly one in 10 (9.1%) physically active children were identified as members of the ‘overweight/obese/low fitness’ subgroup indicated by higher increments in BMI and waist circumference, as well as lower increments in aerobic fitness over time. This observation is concerning as it suggests that a relatively large proportion of children who adhere to guideline recommendations for health-related physical activity continue to experience overweight/obesity and relatively low aerobic fitness.
It has long been acknowledged that the PA response is dependent on the parameters of training including exercise duration, mode, intensity and frequency [14, 18]. Children identified as potential ‘low-responders’ likely require additional PA ‘dosages’ or alternate variations in training parameters to achieve health benefits from PA participation. It is important to note, however, that the outcomes in this study (BMI, waist circumference, aerobic fitness) are influenced by several additional factors such as energy intake [46,47,48], genetics [49,50,51,52,53], and environmental stressors [54, 55]. Consequently, the outcomes identified in this study were likely affected by these factors. Reflecting on this reality, future health guideline recommendations for young people should consider a comprehensive perspective and include multifaceted health recommendations of key health behaviours such as physical activity, sedentary behaviour, and nutrition. Efforts to construct more comprehensive physical activity guidelines with recommendations for activity intensity, mode, and frequency [56], as well as other health behaviours [57] are now appearing and should be encouraged moving forward.
This study had a number of strengths including the large sample size, modeling of univariate and multivariate trajectories, objective measures of physical activity behaviour, and the ability to validate the model result against cardiovascular disease risk factors. While prior studies of exercise response have focused on changes in solitary outcomes from exercise training in adults, the current study estimated multiple concurrent outcomes associated with habitual health-related physical activity in children using a novel multi-trajectory approach.
Despite these strengths, there were also a number of study limitations. We were unable to account for all factors with potential to influence the study outcomes. In particular, the lack of energy intake information is a potential source of residual confounding in the analysis. The measurement of energy intake in epidemiological studies is challenging [58], especially in children [59]. Energy intake information would likely provide a more balanced perspective on developmental trajectories of BMI, waist circumference, and aerobic fitness and better explain the variability in PA outcomes. Despite the relatively large sample size, we were unable to examine for sex-based differences. The potential role of sex in these outcomes may be particularly relevant with the older children in this cohort (~ 9–11 years) for whom sex differences in anthropometry [45] and PA participation [38] are more likely to emerge. The role of sex in exercise responsiveness will be an important priority for future research.
Inherent limitations of hip-mounted accelerometry include the inability to quantify some movements such as cycling and swimming. It is, therefore, possible that we underestimated the number of children meeting PA guideline recommendations and our classification of physically active children may have been overly conservative. The episodic measurement of PA often requires the assumption that outcomes represent typical behaviour, which can be difficult to establish. However, objective measures of PA are preferred over self-reported approaches, and we followed best practices for accelerometry and applied established cut-points to distinguish between different PA intensities. Moreover, our ‘physically active’ classification required children to achieve at least 60 min of MVPA during two measurement periods 10 months apart, thus increasing confidence in the validity of the judgements.
5 Conclusions
The findings of this study revealed distinct developmental trajectories in BMI, waist circumference, and aerobic fitness in children. Among children meeting health-related PA guideline recommendations, nearly one in 10 children followed an ‘overweight/obese/low fitness’ trajectory; this may indicate that the responsiveness to guideline-recommended PA is low in some children. We observed moderate-to-large differences in a clustered cardiovascular risk score between all trajectory groups. These findings demonstrate that individual responses to PA may be established at a young age and as such, can pose a challenge for health practitioners involved in educating children and parents. Importantly, these results also suggest that current health-related PA recommendations may be insufficient for some children and future studies are needed to see if this is the case. Future research should also seek to identify modifiable factors associated with low PA response and examine the effects of alternatives to traditional PA guideline recommendations, including different PA interventions and the role of dietary regimes.
References
Pedersen BK, Saltin B. Exercise as medicine—evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports. 2015;25(Suppl 3):1–72.
Research ISaCACfEaB. The economic cost of physical inactivity in Europe; 2015.
Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1.9 million participants. The Lancet Global health. 2018;6(10):e1077–86.
Bluher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019;15(5):288–98.
Ekelund U, Luan J, Sherar LB, Esliger DW, Griew P, Cooper A, et al. Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents. JAMA. 2012;307(7):704–12.
World Health Organization. Global recommendations on physical activity for health. Geneva: World Health Organization; 2010. p. 17–21.
Strong WB, Malina RM, Blimkie CJ, Daniels SR, Dishman RK, Gutin B, et al. Evidence based physical activity for school-age youth. J Pediatr. 2005;146(6):732–7.
Telama R, Yang X, Leskinen E, Kankaanpaa A, Hirvensalo M, Tammelin T, et al. Tracking of physical activity from early childhood through youth into adulthood. Med Sci Sports Exerc. 2014;46(5):955–62.
Montero D, Lundby C. Refuting the myth of non-response to exercise training: ‘non-responders’ do respond to higher dose of training. J Physiol. 2017;595(11):3377–87.
Pandey A, Swift DL, McGuire DK, Ayers CR, Neeland IJ, Blair SN, et al. Metabolic effects of exercise training among fitness-nonresponsive patients with type 2 diabetes: the HART-D study. Diabetes Care. 2015;38(8):1494–501.
Blizzard LeBlanc DR, Rioux BV, Pelech C, Moffatt TL, Kimber DE, Duhamel TA, et al. Exercise-induced irisin release as a determinant of the metabolic response to exercise training in obese youth: the EXIT trial. Physiol Rep. 2017;5(23):e13539.
Senechal M, Rempel M, Duhamel TA, MacIntosh AC, Hay J, Wicklow B, et al. Fitness is a determinant of the metabolic response to endurance training in adolescents at risk of type 2 diabetes mellitus. Obesity (Silver Spring, Md). 2015;23(4):823–32.
Sparks LM. Exercise training response heterogeneity: physiological and molecular insights. Diabetologia. 2017;60(12):2329–36.
de Lannoy L, Clarke J, Stotz PJ, Ross R. Effects of intensity and amount of exercise on measures of insulin and glucose: analysis of inter-individual variability. PLoS One. 2017;12(5):e0177095.
Alvarez C, Ramirez-Campillo R, Ramirez-Velez R, Izquierdo M. Prevalence of non-responders for glucose control markers after 10 weeks of high-intensity interval training in adult women with higher and lower insulin resistance. Front Physiol. 2017;8:479.
Bouchard C, An P, Rice T, Skinner JS, Wilmore JH, Gagnon J, et al. Familial aggregation of VO(2max) response to exercise training: results from the HERITAGE Family Study. J Appl Physiol. 1999;87(3):1003–8.
Bouchard C, Blair SN, Church TS, Earnest CP, Hagberg JM, Hakkinen K, et al. Adverse metabolic response to regular exercise: is it a rare or common occurrence? PLoS One. 2012;7(5):e37887.
Ross R, de Lannoy L, Stotz PJ. Separate effects of intensity and amount of exercise on interindividual cardiorespiratory fitness response. Mayo Clin Proc. 2015;90(11):1506–14.
Alvarez C, Ramirez-Campillo R, Ramirez-Velez R, Izquierdo M. Effects of 6-week high-intensity interval training in schoolchildren with insulin resistance: influence of biological maturation on metabolic, body composition. Cardiovascular and performance non-responses. Front Physiol. 2017;8:444.
Church TS, Earnest CP, Skinner JS, Blair SN. Effects of different doses of physical activity on cardiorespiratory fitness among sedentary, overweight or obese postmenopausal women with elevated blood pressure: a randomized controlled trial. JAMA. 2007;297(19):2081–91.
Timmons JA, Knudsen S, Rankinen T, Koch LG, Sarzynski M, Jensen T, et al. Using molecular classification to predict gains in maximal aerobic capacity following endurance exercise training in humans. J Appl Physiol. 2010;108(6):1487–96.
Senechal M, Swift DL, Johannsen NM, Blair SN, Earnest CP, Lavie CJ, et al. Changes in body fat distribution and fitness are associated with changes in hemoglobin A1c after 9 months of exercise training: results from the HART-D study. Diabetes Care. 2013;36(9):2843–9.
Ross R, Goodpaster BH, Koch LG, Sarzynski MA, Kohrt WM, Johannsen NM, et al. Precision exercise medicine: understanding exercise response variability. Br J Sports Med. 2019;53:1141–53.
Buford TW, Roberts MD, Church TS. Toward exercise as personalized medicine. Sports Med (Auckland, NZ). 2013;43(3):157–65.
Lopes VP, Utesch T, Rodrigues LP. Classes of developmental trajectories of body mass index: differences in motor competence and cardiorespiratory fitness. J Sports Sci. 2020;38(6):619–25.
Wedderkopp N, Jespersen E, Franz C, Klakk H, Heidemann M, Christiansen C, et al. Study protocol. The childhood health, activity, and motor performance school study Denmark (The CHAMPS-study DK). BMC Pediatr. 2012;12:128.
Moller N, Tarp J, Kamelarczyk E, Brond J, Klakk H, Wedderkopp N. Do extra compulsory physical education lessons mean more physically active children—findings from the childhood health, activity, and motor performance school study Denmark (The CHAMPS-study DK). Int J Behav Nutr Phys Act. 2014;11(1):121.
Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci. 2008;26(14):1557–65.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320(7244):1240–3.
Fredriks AM, van Buuren S, Fekkes M, Verloove-Vanhorick SP, Wit JM. Are age references for waist circumference, hip circumference and waist-hip ratio in Dutch children useful in clinical practice? Eur J Pediatr. 2005;164(4):216–22.
Andersen LB, Andersen TE, Andersen E, Anderssen SA. An intermittent running test to estimate maximal oxygen uptake: the Andersen test. J Sports Med Phys Fit. 2008;48(4):434–7.
Ahler T, Bendiksen M, Krustrup P, Wedderkopp N. Aerobic fitness testing in 6- to 9-year-old children: reliability and validity of a modified Yo-Yo IR1 test and the Andersen test. Eur J Appl Physiol. 2012;112(3):871–6.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9.
Andersen LB, Wedderkopp N, Hansen HS, Cooper AR, Froberg K. Biological cardiovascular risk factors cluster in Danish children and adolescents: the European Youth Heart Study. Prev Med. 2003;37(4):363–7.
Andersen LB, Hasselstrom H, Gronfeldt V, Hansen SE, Karsten F. The relationship between physical fitness and clustered risk, and tracking of clustered risk from adolescence to young adulthood: eight years follow-up in the Danish Youth and Sport Study. Int J Behav Nutr Phys Act. 2004;1(1):6.
Andersen LB, Lauersen JB, Brond JC, Anderssen SA, Sardinha LB, Steene-Johannessen J, et al. A new approach to define and diagnose cardiometabolic disorder in children. J Diabetes Res. 2015;2015:539835.
Klakk H, Grontved A, Moller NC, Heidemann M, Andersen LB, Wedderkopp N. Prospective association of adiposity and cardiorespiratory fitness with cardiovascular risk factors in healthy children. Scand J Med Sci Sports. 2014;24(4):e275–82.
Hebert JJ, Klakk H, Moller NC, Grontved A, Andersen LB, Wedderkopp N. The Prospective Association of Organized Sports Participation with cardiovascular disease risk in children (the CHAMPS Study-DK). Mayo Clin Proc. 2017;92(1):57–65.
Laursen B, Hoff E. Person-centered and variable-centered approaches to longitudinal data. Merrill Palmer Q. 2006;52(3):377–89.
Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109–38.
Nagin D. Group-based modeling of development. Cambridge: Harvard University Press; 2005.
Nagin DS, Jones BL, Passos VL, Tremblay RE. Group-based multi-trajectory modeling. Stat Methods Med Res. 2018;27(7):2015–23.
Freedman DS, Lawman HG, Galuska DA, Goodman AB, Berenson GS. Tracking and variability in childhood levels of BMI: the Bogalusa Heart study. Obesity (Silver Spring, Md). 2018;26(7):1197–202.
Brannsether B, Eide GE, Roelants M, Bjerknes R, Juliusson PB. BMI and BMI SDS in childhood: annual increments and conditional change. Ann Hum Biol. 2017;44(1):28–33.
Tinggaard J, Aksglaede L, Sorensen K, Mouritsen A, Wohlfahrt-Veje C, Hagen CP, et al. The 2014 Danish references from birth to 20 years for height, weight and body mass index. Acta Paediatr. 2014;103(2):214–24.
Thivel D, Chaput JP. Are post-exercise appetite sensations and energy intake coupled in children and adolescents? Sports Med. 2014;44(6):735–41.
Thivel D, Blundell JE, Duche P, Morio B. Acute exercise and subsequent nutritional adaptations: what about obese youths? Sports Med. 2012;42(7):607–13.
Thivel D, Metz L, Julien A, Morio B, Duche P. Obese but not lean adolescents spontaneously decrease energy intake after intensive exercise. Physiol Behav. 2014;123:41–6.
Bouchard C. Individual differences in the response to regular exercise. Int J Obes Relat Metab Disord. 1995;19(Suppl 4):S5–8.
Bouchard C, Rankinen T. Individual differences in response to regular physical activity. Med Sci Sports Exerc. 2001;33(6 Suppl):S446–51 (discussion S52-3).
Bouchard C, Tremblay A, Despres JP, Theriault G, Nadeau A, Lupien PJ, et al. The response to exercise with constant energy intake in identical twins. Obes Res. 1994;2(5):400–10.
Bouchard C, Tremblay A. Genetic influences on the response of body fat and fat distribution to positive and negative energy balances in human identical twins. J Nutr. 1997;127(5 Suppl):943S–7S.
Bouchard C, Tremblay A, Despres JP, Nadeau A, Lupien PJ, Theriault G, et al. The response to long-term overfeeding in identical twins. N Engl J Med. 1990;322(21):1477–82.
Silva RPM, Barros CLM, Mendes TT, Garcia ES, Valenti VE, de Abreu LC, et al. The influence of a hot environment on physiological stress responses in exercise until exhaustion. PLoS One. 2019;14(2):e0209510.
Ball D, Burrows C, Sargeant AJ. Human power output during repeated sprint cycle exercise: the influence of thermal stress. Eur J Appl Physiol Occup Physiol. 1999;79(4):360–6.
Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The physical activity guidelines for Americans. JAMA. 2018;320(19):2020–8.
Tremblay MS, Carson V, Chaput JP, Connor Gorber S, Dinh T, Duggan M, et al. Canadian 24-hour movement guidelines for children and youth: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2016;41(6 Suppl 3):S311–27.
Ioannidis JPA. The challenge of reforming nutritional epidemiologic research. JAMA. 2018;320(10):969–70.
Baranowski T, Smith M, Baranowski J, Wang DT, Doyle C, Lin LS, et al. Low validity of a seven-item fruit and vegetable food frequency questionnaire among third-grade students. J Am Diet Assoc. 1997;97(1):66–8.
Acknowledgements
The authors gratefully acknowledge the valuable work of numerous students who assisted with data collection in the CHAMPS study DK. We also thank the participating children, their parents, and teachers in the schools involved in the project. We are grateful for the cooperation with The Svendborg Project, Sport Study Sydfyn, and the Municipality of Svendborg. Finally, we wish to acknowledge members of the CHAMPS-study DK not listed as co-authors in this paper: E. Jespersen, M. Heidemann, C.T. Rexen, and C. Franz.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have nothing to disclose.
Funding
The CHAMPS-study DK was funded by the TRYG Foundation, University College Lillebaelt, University of Southern Denmark, The Nordea Foundation, The IMK foundation, The Region of Southern Denmark, The Egmont Foundation, The A.J. Andersen Foundation, The Danish Rheumatism Association, Østifternes Foundation, Brd. Hartmann’s Foundation, TEAM Denmark, The Danish Chiropractor Foundation, and The Nordic Institute of Chiropractic and Clinical Biomechanics. The funding sources played no role in the design, conduct, or reporting of this study.
Author contributions
JJH, MS, TF, and NW conceived the research questions and designed the analysis. NCM, HK, and NW acquired data. JJH conducted the data analysis and drafted the original manuscript. All authors interpreted the data, provided critical revisions of the manuscript, and approved the final version to be published.
Data Availability
Data are available from the CHAMPS Study Steering Committee upon reasonable request. Legal and ethical restrictions apply. Interested parties may contact Dr. Niels Christian Møller (nmoller@health.sdu.dk), and the following information will be required at the time of application: a description of how the data will be used, securely managed, and permanently deleted.
Rights and permissions
About this article
Cite this article
Hébert, J.J., Sénéchal, M., Fairchild, T. et al. Developmental Trajectories of Body Mass Index, Waist Circumference, and Aerobic Fitness in Youth: Implications for Physical Activity Guideline Recommendations (CHAMPS Study-DK). Sports Med 50, 2253–2261 (2020). https://doi.org/10.1007/s40279-020-01335-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-020-01335-3