Abstract
Background
Oxygen cost of running is largely influenced by endurance training strategies, including interval and continuous training. However, which training method better reduces the oxygen cost remains unknown.
Objective
This study aimed to systematically review the scientific literature and performs a meta-analysis to address the effects of different endurance training modalities on the oxygen cost of running.
Methods
A literature search on 3 databases (MEDLINE, SPORTDiscus and Web of Science) was conducted on February 28, 2019. After analysing 8028 resultant articles, studies were included if they met the following inclusion criteria: (a) studies were randomised controlled trials, (b) studies included trained runners without previous injuries (c) interventions lasted at least 6 weeks, with participants allocated to Interval (INT) or Continuous (CON) groups, and (d) oxygen cost was assessed pre- and post-training intervention. Six studies (seven trials) met the inclusion criteria and were included in the meta-analysis. This resulted in 295 participants (n = 200 INT; n = 95 CON training method). Standardised mean difference with 95% confidence intervals (CI) between INT and CON conditions and effect sizes were calculated. To assess the potential effects of moderator variables (such as, age, VO2max of participants, number of weeks of intervention) on main outcome (oxygen cost of running), subgroup analyses were performed.
Results
Comparing changes from pre- to post-intervention, oxygen cost improved to a greater extent in CON when compared to INT interventions (0.28 [95% CI 0.01, 0.54], Z = 2.05, p = 0.04, I2 = 30%). Oxygen cost improvements were larger in participants with higher VO2max (≥ 52.3 ml kg−1 min−1) (0.39 [95% CI 0.06, 0.72], Z = 2.34, p = 0.02), and in programs greater or equal to 8 weeks (0.35 [95% CI 0.03, 0.67], Z = 2.13, p = 0.03). When the total volume per week of INT was ≥ 23.2 min, there was a significant improvement favorable to CON (0.34 [95% CI 0.01, 0.61], Z = 2.02, p = 0.04).
Conclusion
Continuous training seems, overall, a better strategy than interval training to reduce the oxygen cost in recreational endurance runners. However, oxygen cost reductions are influenced by several variables including the duration of the program, runners’ aerobic capacity, the intervals duration and the volume of interval training per week. Practitioners and coaches should construct training programs that include both endurance training methods shown to be effective in reducing the oxygen cost of running.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Endurance running performance is reliant on a complex interaction of factors, such as cardiac output, oxygen delivery to working muscles and maximal oxygen uptake (VO2max) [1], that lead to efficient muscular work and result in a fast and effective running gait [2]. These factors disclose several aspects of running performance and are able to identify discrepancies between untrained and well-trained runners [3]. However, unraveling the differences between runners of matched ability has proved more challenging [4]. In this regard, the oxygen cost of running, commonly defined as the steady-state oxygen uptake required at a given submaximal speed [1], has been reported to most appropriately discriminate between performances in homogeneous groups of runners [5, 6]. Consequently, together with VO2max [7] and lactate threshold [8], the oxygen cost is considered a key factor for distance running success [9, 10].
The oxygen cost is largely determined by physiological factors [11], muscle fiber distribution [12], age [13], sex [14], anthropometric factors [15] and biomechanical variables [16]. Similarly, previous research has suggested that the oxygen cost may be influenced by different training strategies, including strength training [17] and endurance training modalities. This is because different training approaches have been reported to elicit changes in the functionality of skeletal muscle mitochondria (i.e. muscle respiratory capacity), which ultimately would imply less use of oxygen during exercise [3]. Other endurance training adaptations, including increased skeletal muscle buffer capacity and haematological changes (i.e. increased red cell mass [18]), may also improve oxygen delivery and utilisation [19].
Two of the most common endurance training strategies are interval training and continuous training methods [20]. However, despite the scientific evidence supporting the use of endurance training to reduce the oxygen cost, the effects of the training method used (interval vs. continuous) are still a matter of debate in the literature. On the one hand, several studies investigating the effects of interval training at intensities between 93–120% of the speed at VO2max and continuous training at the onset of blood lactate accumulation speed have reported similar running economy improvements of around 1–7% [21,22,23,24,25]. On the other hand, previous research using similar training strategies found no significant improvements at all [26, 27], while some authors suggest that the endurance training modality used exerts a trivial effect on the oxygen cost [19, 28]. At the same time, the effects of exercise intensity, frequency and duration of interval and continuous training on the oxygen cost are yet to be explored.
It is against this apparently contradictory background that this study systematically reviews the body of scientific literature of original research and performs a meta-analysis to assess the effects of different endurance training modalities on the oxygen cost. In addition, the study also analyses how other variables, including age, VO2max, and duration of effort and duration of intervention, may affect the incidence of interval and continuous training on running economy. We hypothesise that continuous training modalities will elicit greater oxygen cost reductions than interval training methods.
2 Methods
This meta-analysis followed the PRISMA statement for improved reporting of meta-analyses [21].
2.1 Search Strategy
A literature search was conducted on February 28, 2019 by two independent reviewers for the following databases: MEDLINE, SPORTDiscus and Web of Science. The keywords used in the search were: running economy, energy cost, metabolic cost, continuous training, interval training and runners. Abstracts and citations from scientific conferences were excluded.
Title, abstract and keyword search fields were searched using the following search strategy:
Running economy* OR energy cost* OR metabolic cost* AND continuous training* AND/OR interval training* AND runners.
Searches were limited to human trained participants and English language only publications. Identification, screening, eligibility assessments and inclusion of studies were performed independently by two reviewers (FGM and IY) with disagreement settled by consensus. All records of literature search were examined by title and abstract to exclude irrelevant records. Studies were selected following the eligibility criteria. Data including the publication details, participant characteristics (recreational runners), testing procedures, study design, description of intervention and results of the oxygen cost of running outcome were extracted from all eligible studies. If insufficient information was reported (e.g. VO2max of participants), the authors were contacted to confirm additional information about the included studies.
2.2 Inclusion Criteria
The summary of eligibility criteria is shown in Table 1.
2.2.1 Type of Study
Our meta-analysis included randomised controlled trials, written in English and published previous to February 28, 2019.
2.2.2 Type of Participants
The participants included in our meta-analysis were recreational runners without previous injuries or chronic diseases. No exclusion criteria were used for participant sex or baseline fitness. The classification of participants followed the criteria previously reported by De Pauw et al. 2013 [30], in terms of VO2max. The range established for recreational runners was 45–54.9 mL kg−1 min−1 of VO2max [30], which was similar to that of our participants (range 47.3–56.7 mL kg−1 min−1, Table 3).
2.2.3 Type of Interventions
Endurance training studies usually last between 6 and 12 weeks [31,32,33]. Therefore, to be included in our meta-analysis, training programs had to last at least a minimum of 6 weeks, with participants allocated to Interval (INT) and Continuous (CON) groups. Training programs were detailed in the corresponding Methods section, with duration, intensity and volume of each session recorded. Studies were excluded if experimental training programs were combined with other extra-training sessions.
2.2.4 Type of Outcome Measure
The outcome measure for this meta-analysis was the oxygen cost of running, which was measured on a treadmill.
2.3 Data Extraction
Two of the authors (FGM and IY) independently extracted characteristics of participants and training protocols using a standardised form. Results were compared and discrepancies were resolved by consensus or by consulting the senior author (JMG).
2.4 Final Study Selection
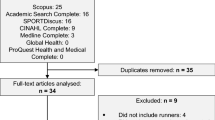
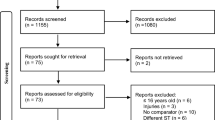
8028 potential manuscripts were identified following database examination (Fig. 1). References list of selected manuscripts were also examined for any other potentially eligible manuscripts. Following this examination, 3 potential manuscripts were added. After removal of duplicates and elimination of papers based on title and abstract screening, 101 studies remained. Only 6 out of 101 studies met the inclusion criteria and were, therefore, included in the meta-analysis (Fig. 1).
2.5 Quality assessment
The methodological quality of the studies was rated using the PEDro scale [34] and Oxford’s levels of quality [35] (Table 2). The PEDro scale consists of 11 items related to scientific rigor. Item 1 is rated as Yes/No, while Items 2–11 are rated using 0 (absent) or 1 (present), and a score out of 10 is obtained by summation. A score of ≥ 6 represents the threshold for studies with low risk of bias [36]. Given that the assessors are rarely blinded, and that is impossible to blind the participants and investigators in supervised exercise interventions the items related to blinding (5–7) were removed from the scale [37]. For this reason, the maximum result on the modified PEDro 8-point scale was 7 (highest score), as the first item is not included in the total score. The qualitative ratings were adjusted to that used in previous exercise-related systematic reviews [37, 38] as follows: 6–7 = “excellent”; 5 = “good”; 4 = “moderate”; and, 0–3 = “poor”.
2.6 Statistical Considerations
Meta-analytical procedures were applied to evaluate possible effects of INT and CON training on the oxygen cost of running. Standardised mean difference (SMD) with 95% Confidence Intervals (CI) between INT and CON conditions was calculated with RevMan 5.3.5 for Windows using a fixed effects model. During the screening of the selected studies, mean and standard deviations for the outcome measures were extracted. It was not necessary to contact the authors for further data. Significance for overall effect was set at p < 0.05. Heterogeneity of the analysed studies was assessed using an I-squared (I2) test. Significance level of I2 test was set at p < 0.05. I2 represents the proportion of effects that are due to heterogeneity as opposed to chance [39]. Thresholds for low, moderate and high levels of heterogeneity correspond to I2 values of 25, 50, and 75%, respectively. Within the controlled trial studies, a positive effect indicates a larger oxygen cost improvement in the CON group when compared to the INT group, while a negative effect means the opposite. For a clearer interpretation of the results, it is important to highlight that oxygen cost of running improvements means a reduced oxygen cost, thereby giving rise to the negative change. The calculated effect sizes (ES) were interpreted using the conventions outlined for SMD by Hopkins et al. [40] (small (> 0.2 and < 0.6); moderate (≥ 0.6 and < 1.2); large (≥ 1.2 and < 2) and very large (≥ 2 and < 4)).
2.6.1 Analysis of Moderator Variables
To assess the potential effects of moderator variables on main outcome (oxygen cost of running), subgroup analyses were performed. We used a random-effects model and selected potential moderators likely to influence the effects of training. Studies were divided into the following variables: age (Group 1, 23.7–33.1 years and Group 2, 33.1–49.2 years), VO2max of participants (Group 1, 47.3–52.2 ml kg−1 min−1 and Group 2, 52.3–56.7 ml kg−1 min−1) and number of weeks of intervention (Group 1, 6–7 weeks and Group 2, 8–16 weeks). At the same time, for the INT intervention, studies were divided for the duration of the interval (Group 1, 15 s−1 min and Group 2, 4–5 min) and the total exercise time per week (Group 1, 7.2–23.2 min and Group 2, 35.2–156 min). For the CON intervention, studies were divided by total exercise time per week (Group 1, 62.5–105 min and Group 2, 125.8–177 min). The division of the moderator variables was established to obtain a similar number of studies to those of subgroup analyses.
3 Results
3.1 Level of Evidence and Quality of the Studies
All the studies selected achieved the required standard to be considered to have a low risk of bias (PEDro score ≥ 6; Table 2) following the previous systematic reviews [37, 38]. Based on the Oxford Level of Evidence, 5 of the studies selected had an evidence of 2b. This was because confidence intervals were not reported. Only the study of Pugliese et al. [41] achieved an evidence level 1b (high-quality randomised controlled trial).
3.2 Characteristics of the Participants
Table 3 shows the participant characteristics of the six studies included in this meta-analysis (total sample size of 295 participants, 27.12% women). The total participants were randomised to either INT (n = 200) or CON (n = 95). Only two of the studies [42, 43] included men and women, while the rest of studies included only male participants [20, 22, 41, 44].
3.3 Characteristics of the Studies Selected
The outcome for this meta-analysis was the change in the oxygen cost of running measured during a steady-state run on a treadmill. Mean intervention duration was 8.5 weeks (range 6–16), with only one study having a duration longer than 8.5 weeks [44]. Mean training frequency was three times a week (range 2–3 times a week). Mean duration of the total training session was 45.6 min for INT (range 8.6–156 min) and 112 min for CON (range 62.5–177 min).
The intensity of the interventions of INT was prescribed as percentage of HRmax in one study [14], as a percentage of maximal aerobic speed (MAS) in two studies [20, 44], as a percentage of gas exchange threshold (GET) in one study [41], and as a percentage of maximal speed test [42, 43]. Regarding CON interventions, the intensity was prescribed as percentage of HRmax in two studies [22, 43], as a percentage of MAS [20], as a percentage of GET [41], and as a percentage of HR at intensity of second ventilatory threshold [44]. The study by Gunnarsson et al. [42] does not report the intensity of CON.
3.4 Oxygen Cost Assessment (Main Effect)
The oxygen cost reduced to a greater extent in CON when compared to INT interventions (SMD = 0.28 [95% CI 0.01, 0.54], Z = 2.05, p = 0.04). The I2 test showed a non-significant heterogeneity among the included studies (I2 = 30%, p = 0.20). These results are displayed in Figure 2.
3.5 Effect of Moderator Variables
Between-group heterogeneity was found to be insignificant (p > 0.05) in the subgroup analysis. Table 4 shows the effect of moderator variables on oxygen cost of running. Oxygen cost reductions were larger in participants with higher VO2max (≥ 52.3 ml kg−1 min−1) (SMD = 0.39 [95% CI 0.06, 0.72], Z = 2.34, p = 0.02),in programs greater or equal to 8 weeks (SMD = 0.35 [95% CI 0.03, 0.67], Z = 2.13, p = 0.03) and in participants greater or equal to 33.8 years (SMD = 0.29 [95% CI − 0.05, 0.64], Z = 1.67, p = 0.09) favorable to CON interventions.
For INT interventions, studies prescribing intervals duration ≤ 1 min revealed no significant subgroup oxygen cost differences when compared to CON interventions (test for subgroup differences, p = 0.49, I2 = 0%). For studies prescribing intervals duration > 1 min, there was a significant reduction in oxygen cost favorable to INT compared to CON (SMD = − 0.59 [95% CI − 0.91,− 0.24], Z = 3.35, p = 0.0008, I2 = 80%, p = 0.002). However, when the total exercise time per week was ≥ 23.2 min in INT interventions, there was a significant reduction in oxygen cost favorable to CON (SMD = 0.34 [95% CI 0.01, 0.61], Z = 2.02, p = 0.04). The I2 test showed a non-significant heterogeneity among the included studies (I2 = 0%, p = 0.37).
For CON interventions, subgroup analyses revealed no significant subgroup differences (test for subgroup differences, p = 0.78, I2 = 0%) on oxygen cost when the total exercise time per week was divided into two groups (≤ 105 min or ≥ 106 min).
4 Discussion
The main finding of this systematic review was that continuous training (CON) improved the oxygen cost of running to a greater extent than interval training (INT) in recreational endurance runners. However, we found that oxygen cost reductions were influenced by several variables including the duration of the program, runners’ aerobic capacity, the intervals duration and the volume of interval training per week.
These results agree with the conclusions of previous studies reporting that continuous endurance training is an effective method to improve the oxygen cost in trained endurance runners [20, 21]. González-Mohíno et al. [20] suggest that the reduced oxygen cost observed after a CON training intervention may be due to an improved intracellular oxidative capacity (which implies an increased rate of lactate oxidation), and changes in the morphology and function of mitochondria [45]. However, it is known that oxygen cost reductions are greater at the intensities close to what runners routinely reach during training [46]. Therefore, part of the results may be explained by the fact that CON interventions imply higher volume of work (~ 80%) at intensities closer to the speed at which the oxygen cost is commonly assessed [8].
There are contradictory findings regarding INT training programs and its effects on the oxygen cost. Some researchers have reported no running economy improvements after an INT intervention [25, 47], whereas others have found the opposite [48]. Others, such as Billat et al. [23] have reported oxygen cost improvements when adding high intensity training to baseline running, although this effect seems to be lost when that high intensity training is performed too often. Similarly, Franch et al. [22] found that the oxygen cost significantly reduced after a training intervention using high intensity interval training at intensities of 94% and 106% of VO2max, but not when the intensity was 132% of VO2max. All this suggests that there must be an optimal amount of interval training volume and intensity in order to produce training adaptations below and above in which there are no further oxygen cost reductions. According to our results, that optimal amount lies somewhere below ~ 23 min per week, as greater volumes seem to have detrimental effects.
Similarly, we found that training programs greater or equal to 8 weeks elicited greater oxygen cost improvements than shorter interventions in both CON and INT. This result may be due to the higher volume of work completed in longer programs. Previous research has suggested that training volume is important to generate physiological adaptations [22], although whether the same running economy improvements would exist in programs of matched volume of work but different duration is debatable.
To the authors’ best knowledge, no research has yet investigated the effects of endurance training on the oxygen cost taking into account runners’ VO2max. Together with the oxygen cost and lactate threshold, VO2max is considered one of the factors that sets the upper limit for performance in endurance events [1, 28, 49, 50]. It has been suggested that exercise economy and VO2max are inversely related, as better oxygen cost values are usually related to lower values of VO2max and vice versa [51,52,53]. Interestingly, we found that athletes with VO2max values above 52.3 ml kg−1 min−1 showed greater oxygen cost reductions after a training intervention than runners with smaller values. One of the possible explanations may be that, due to the known inverse relationship between VO2max and oxygen cost [51, 52], runners with higher VO2max values present greater inefficiency values at baseline; thus, they have greater potential for improvement.
However, the relationships between VO2max and the oxygen cost and how they change after CON and INT training interventions are still a matter of debate in the scientific literature. For example, whereas Pugliese et al. [41] found that the oxygen cost decreased in CON and INT interventions (while VO2peak decreased only in the INT group), Gunnarsson et al. [42] found an improvement of VO2max after an INT intervention (with no oxygen cost changes). Similarly, Schaun et al. [44] found an improvement of VO2max in both CON and INT intervention while the oxygen cost worsened in both groups. Lastly, González-Mohíno et al. [20] found that the oxygen cost reduced and the VO2max decreased after a CON intervention. Since a typical endurance training program is a combination of both interval and continuous training, longitudinal data of studies lasting several years where different training methods are combined are needed to properly assess the effects of different approaches on the oxygen cost and VO2max.
It is necessary to acknowledge several limitations to the present study. These include the wide variety of different protocols for both INT and CON training interventions, since this prevented us from drawing a definitive conclusion from the results. Another important limitation was the lack of statistical power of some of the studies that resulted in equivocal findings in relation to INT interventions [54].
5 Conclusion
This is the first review to analyse the effects of different endurance training modalities on the oxygen cost of running. We found that continuous training is, overall, a better strategy than interval training to reduce the oxygen cost in recreational endurance runners. However, there are a number of variables that seem to influence oxygen cost reductions. As such, we found that oxygen cost improvements were larger in participants with higher VO2max (≥ 52.3 ml kg−1 min−1) than in those with lower values. Similarly, training programs lasting 8 or more weeks had greater effects on oxygen cost improvements than shorter ones. We also found that when prescribing intervals duration > 1 min, INT was more effective than CON for reducing the oxygen cost. However, when the total exercise time per week of the INT interventions was ≥ 23.2 min, CON interventions implied greater oxygen cost improvements.
5.1 Practical Applications
Endurance training methods (CON and INT) are effective in reducing oxygen cost in recreational endurance runners. For future research purposes, we recommend that researchers carry out studies in find the optimal load amounts of both endurance training methods that lead to substantial reduction of oxygen cost. In addition to these endurance training methods, other training strategies have been shown to be effective in the oxygen cost reduction. For example, exercises in strength training, including low to high intensity resistance exercises and plyometric exercises, are an appropriate means of reducing the oxygen cost of running [17, 55]. Therefore, due to their ability to reduce the oxygen cost of running and improve endurance performance, we recommend incorporating the above-mentioned strategies into the training programs of recreational endurance runners.
References
Nummela A, Keränen T, Mikkelsson L. Factors related to top running speed and economy. Int J Sports Med. 2007;28:655–61.
Joyner MJ. Modeling: optimal marathon performance on the basis of physiological factors. J Appl Physiol. 1991;70:683–7.
Saunders PU, Pyne DB, Telford RD, Hawley JA. Factors affecting running economy in trained distance runners. Sports Med. 2004;34(7):465–85.
Santos-Concejero J, Tam N, Granados C, Irazusta J, Bidaurrazaga-Letona I, Zaballa-Lili J, et al. Stride angle as a novel indicator of running economy in well-trained runners. J Strength Cond Res. 2014;28(7):1889–95.
Pate R, Macera C, Bailey S, Bartoli W, Powell K. Physiological, anthropometric, and training correlates of running economy. Med Sci Sports Exerc. 1992;24:1128–33.
Lucia A, Esteve-Lanao J, Oliván J, Gómez-Gallego F, San Juan AF, Santiago C, et al. Physiological characteristics of the best Eritrean runners-exceptional running economy. Appl Physiol Nutr Metab. 2006;31:530–40.
Billat V, Demarle A, Slawinski J, Paiva M, Koralsztein J. Physical and training characteristics of top-class marathon runners. Med Sci Sports Exerc. 2001;33:2089–97.
Enoksen E, Tjelta AR, Tjelta LI. Distribution of training volume and intensity of elite male and female track and marathon runners. Int J Sports Sci Coach. 2011;6:273–93.
Conley DL, Krahenbuhl GS. Running economy and distance running performance of highly trained athletes. Med Sci Sports Exerc. 1980;12:357–60.
Di Pampero PE, Atchou G, Brückner JC, Moia C. The energetics of endurance running. Eur J Appl Physiol Occup Physiol. 1986;55:259–66.
Mayhew JL. Oxygen cost and energy expenditure of running in trained runners. Br J Sports Med. 1977;11(3):116–21.
Bosco C, Montanari G, Ribacchi R, Giovenali P, Latteri F, Iachelli G, Cortili G. Relationship between the efficiency of muscular work during jumping and the energetics of running. Eur J Appl Physiol Occup Physiol. 1987;56(2):138–43.
Krahenbuhl GS, Pangrazi RP. Characteristics associated with running performance in young boys. Med Sci Sports Exerc. 1983;15(6):486–90.
Bransford DR, Howley ET. Oxygen cost of running in trained and untrained men and women. Med Sci Sports Exerc. 1977;9:41–4.
Bergh U, Sjödin B, Forsberg A, Svedenhag J. The relationship between body mass and oxygen uptake during running in humans. Med Sci Sports Exerc. 1991;23(2):205–11.
Santos-Concejero J, Tam N, Granados C, Irazusta J, Bidaurrazaga-Letona I, Zabala-Lili J, Gil SM. Interaction effects of stride angle and strike pattern on running economy. Int J Sports Med. 2014;35(13):1118–23.
Balsalobre-Fernández C, Santos-Concejero J, Grivas GV. Effects of strength training on running economy in highly trained runners: a systematic review with meta-analysis of controlled trials. J Strength Cond Res. 2016;30(8):2361–2368.
Levine BD, Stray-Gundersen J. “Living high-training low”: effect of moderate-altitude acclimatization with low-altitude training on performance. J Appl Physiol. 1997;83(1):102–12.
Barnes KR, Kilding AE. Strategies to improve running economy. Sports Med. 2015;45(1):37–56.
González-Mohíno F, González-Ravé JM, Juárez D, Fernández FA, Barragán Castellanos R, Newton RU. Effects of continuous and interval training on running economy, maximal aerobic speed and gait kinematics in recreational runners. J Strength Cond Res. 2016;30(4):1059–66.
Sjodin B, Jacobs I, Svedenhag J. Changes in onset of blood lactate accumulation (OBLA) and muscle enzymes after training at OBLA. Eur J Appl Physiol. 1982;49(1):45–57.
Franch J, Madsen K, Djurhuus MS, Pedersen PK. Improved running economy following intensified training correlates with reduced ventilatory demands. Med Sci Sports Exerc. 1998;30(8):1250–6.
Billat VL, Flechet B, Petit B, Muriaux G, Koralsztein JP. Interval training at VO2max: effects on aerobic performance and overtraining markers. Med Sci Sports Exerc. 1999;31(1):156–63.
Slawinski J, Demarle A, Koralsztein JP, Billat V. Effect of supra- lactate threshold training on the relationship between mechanical stride descriptors and aerobic energy cost in trained runners. Arch Physiol Biochem. 2001;109(2):110–6.
Barnes KR, Hopkins WG, McGuigan MR, Kilding AE. Effects of different uphill interval-training programs on running economy and performance. Int J Sports Physiol Perform. 2013;8(6):639–47.
Yoshida T, Udo M, Chida M, Ichioka M, Makiguchi K, Yagamuchi T. Specificity of physiological adaptation to endurance training in distance runners and competitive walkers. Eur J Appl Physiol. 1990;61(3–4):197–201.
Smith TP, McNaughton LR, Marshall KJ. Effects of 4-week training using Vmax/Tmax on VO2max and performance in athletes. Med Sci Sports Exerc. 1999;31(6):892–6.
Morgan DW, Martin PE, Krahenbuhl GS. Factors affecting running economy. Sports Med. 1989;7(5):310–30.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7).
Pauw KD, Roelands B, Cheung SS, De Geus B, Rietjens G, Meeusen R. Guidelines to classify subject groups in sport-science research. Int J Sports Physiol Perform. 2013;8(2):111–22.
Conley D, Krahenbuhl G, Burkett L, Millar AL. Following Steve Scott: physiological changes accompanying training. Phys Sportsmed. 1984;12(1):103–6.
Overend TJ, Paterson DH, Cunningham DA. The effect of interval and continuous training on the aerobic parameters. Can J Appl Sport Sci. 1992;17:129–34.
Lake M, Cavanagh P. Six weeks of training does not change running mechanics or improve running economy. Med Sci Sports Exerc. 1996;28:860–9.
de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother. 2009;55:129–33.
Oxford Centre for Evidence-based Medicine. Levels of evidence. Univ Oxford. 4–5, 2009.
Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83:713–21.
Baz-Valle E, Fontes-Villalba M, Santos-Concejero J. Total number of sets as a training volumen quantification method for muscle hypertrophy: a systematic review. J Strength Cond Res. Post Acceptance: July 30, 2018.
Schoenfeld BJ, Grgic J, Ogborn D, Krieger JW. Strength and hypertrophy adaptations between low-vs. high-load resistance training: a systematic review and meta-analysis. J Strength Cond Res. 2017;31(2):3508–3523.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1000100.
Hopkins WG, Marshall SW, Batterham AM, Hanin J. Progressive statistics for studies in sports medicine and exercise science. Med Sci Sports Exerc. 2009;41:3–12.
Pugliese L, Porcelli S, Vezzoli A, La Torre A, Serpiello FR, Pavei G, et al. Different training modalities improve energy cost and performance in master runners. Front Physiol. 2018;9:21.
Gunnarsson TP, Bangsbo J. The 10-20-30 training concept improves performance and health profile in moderately trained runners. J Appl Physiol. 2012;113(1):16–24.
Gliemann L, Gunnarsson TP, Hellsten Y, Bangsbo J. 10–20-30 training increases performance and lowers blood pressure and VEGF in runners. Scand J Med Sci Sports. 2015;25(5):e479–89.
Schaun GZ, Pinto SS, Silva MR, Dolinski DB, Alberton CL. Whole-body high-intensity interval training induce similar cardiorespiratory adaptations compared with traditional high-intensity interval training and moderate-intensity continuous training in healthy men. J Strength Cond Res. 2018;32(10):2730–42.
Saunders PU, Cox AJ, Hopkins WG, Pyne DB. Physiological measures tracking seasonal changes in peak running speed. Int J Sports Physiol. 2010;5:230–8.
Jones AM, Carter H. The effect of endurance training on parameters of aerobic fitness. Sports Med. 2000;29: 373–386.
Smith TP, Coombes JS, Geraghty DP. Optimising high-intensity treadmill training using the running speed at maximal O(2) uptake and the time for which this can be maintained. Eur J Appl Physiol. 2003;89(3–4):337–43.
Denadai BS, Ortiz MJ, Greco CC, de Mello MT. Interval training at 95% and 100% of the velocity at VO2max: effects on aerobic physiological indexes and running performance. Appl Physiol Nutr Metab. 2006;31:737–43.
Bassett DR, Howley ET. Maximal oxygen uptake: “classical” versus “contemporary” viewpoints. Med Sci Sports Exerc. 1997;29:591–603.
Daniels J, Daniels N. Running economy of elite male and elite female runners. Med Sci Sports Exerc. 1992;24:483–9.
Morgan DW, Daniels JT. Relationship between VO2max and the aerobic demand of running in elite distance runners. Int J Sports Med. 1994;15:426–9.
Lucía A, Hoyos J, Pérez M, Santalla A, Chicharro JL. Inverse relationship between VO2max and economy/efficiency in world-class cyclists. Med Sci Sports Exerc. 2002;34(12):2079–84.
Shaw AJ, Ingham SA, Atkinson G, Folland JP. The correlation between running economy and maximal oxygen uptake: cross-sectional and longitudinal relationships in highly trained distance runners. Plos One. 2015;10(4):e0123101.
Midgley AW, McNaughton LR, Jones AM. Training to enhance the physiological determinants of long-distance running performance. Sports Med. 2007;37(10):857–80.
Denadai BS, de Aguiar RA, de Lima LCR, Greco CC, Caputo F. Explosive training and heavy weight training are effective for improving running economy in endurance athletes: a systematic review and meta-analysis. Sports Med. 2017;47(3):545–54.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used in the preparation of this article.
Conflict of interest
Fernando González-Mohíno, Jordan Santos-Concejero, Inmaculada Yustres and José María González-Ravé declare that they have no conflicts of interest relevant to the content of this review.
Rights and permissions
About this article
Cite this article
González-Mohíno, F., Santos-Concejero, J., Yustres, I. et al. The Effects of Interval and Continuous Training on the Oxygen Cost of Running in Recreational Runners: A Systematic Review and Meta-analysis. Sports Med 50, 283–294 (2020). https://doi.org/10.1007/s40279-019-01201-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-019-01201-x