Abstract
Background
Low-load resistance training (< 50% of one-repetition maximum [1RM]) associated with blood-flow restriction (BFR-RT) has been thought to promote increases in muscle strength and mass. However, it remains unclear if the magnitude of these adaptations is similar to conventional high-load resistance training (> 65% 1RM; HL-RT).
Objective
To compare the effects of HL- versus BFR-RT on muscle adaptations using a systematic review and meta-analysis procedure.
Methods
Studies were identified via electronic databases based on the following inclusion criteria: (a) pre- and post-training assessment of muscular strength; (b) pre- and post-training assessment of muscle hypertrophy; (c) comparison of HL-RT vs. BFR-RT; (d) score ≥ 4 on PEDro scale; (e) means and standard deviations (or standard errors) are reported from absolute values or allow estimation from graphs. If this last criterion was not met, data were directly requested from the authors.
Results
The main results showed higher increases in muscle strength for HL- as compared with BFR-RT, even when considering test specificity, absolute occlusion pressure, cuff width, and occlusion pressure prescription. Regarding the hypertrophic response, results revealed similar effects between HL- and BFR-RT, regardless of the absolute occlusion pressure, cuff width, and occlusion pressure prescription.
Conclusions
Based on the present data, maximum muscle strength may be optimized by specific training methods (i.e., HL-RT) while both HL- and BFR-RT seem equally effective in increasing muscle mass. Importantly, BFR-RT is a valid and effective approach for increasing muscle strength in a wide spectrum of ages and physical capacity, although it may seem particularly of interest for those individuals with physical limitations to engage in HL-RT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The results from the present systematic review and meta-analysis demonstrate superior muscle strength gains for high-load (HL-RT) as compared with low-load resistance training associated with blood-flow restriction (BFR-RT), even when adjusting for potential moderators (i.e., test specificity, absolute occlusion pressure, cuff width, and occlusion pressure prescription method). |
Regarding the hypertrophic response, HL-RT was shown to induce comparable increases in muscle mass when compared to BFR-RT, regardless of absolute occlusion pressure, cuff width, and occlusion pressure prescription method. |
From a practical viewpoint, individuals with a special interest in increasing maximum muscle strength may benefit from a more specific training method (i.e., HL-RT); however, when considering muscle mass accrual, both HL- and BFR-RT seem equally effective. |
1 Introduction
The strength-endurance continuum hypothesis dictates that increases in muscle strength and mass are dependent upon proper resistance training (RT) load manipulation [1]. Accordingly, for many years high-load RT (HL-RT; i.e., > 65% of one-repetition maximum [1RM]) has been indicated to maximize both functional (i.e., strength) and morphological (i.e., hypertrophy) adaptations [2,3,4,5]. However, recent evidence has shown otherwise. Specifically, low-load resistance training (20–50% 1RM) associated with blood-flow restriction (BFR-RT) has been demonstrated to be effective in promoting increases in muscle strength and mass in different populations, from athletes to severely diseased individuals [6,7,8,9].
Recently, a meta-analysis demonstrated the superiority of BFR-RT when compared with an equivalent low-load RT without blood flow restriction on gains in muscle strength and mass [10]. Although relevant, it seems imperative to understand the effects of BFR- as compared to HL-RT, an allegedly “gold standard” protocol to increase muscle strength and mass. In this regard, the literature is controversial regarding the magnitude of these adaptations across protocols. For instance, while some studies have suggested greater increases in muscle strength for HL- as compared with BFR-RT [7, 11,12,13,14], others have demonstrated similar gains between training protocols [15,16,17,18,19]. With respect to muscle mass accrual, results are somewhat more consistent, pointing toward similar effects between HL- and BFR-RT [6, 7, 11, 13, 16,17,18,19,20].
Current literature allows the speculation that discrepancies between studies may be, at least partially, explained by differences in testing procedures. Testing specificity may affect the results, as dynamic muscle strength assessment via a 1RM test may undermine the potential of BFR-RT. In short, HL-RT implies exercising with heavy loads, which are similar to a 1RM test, whereas during BFR-RT subjects are never exposed to high loads [21]. Therefore, it has been suggested that nonspecific strength assessment, such as in isometric or isokinetic testing, may more precisely reflect the response to different training protocols [21]. Dissonant findings may also be attributed to differences in BFR-RT characteristics, such as absolute occlusion pressure, cuff width and prescription method (i.e., individualized or not) between studies. In this regard, higher occlusion pressures may be related to greater muscle activation [22], which could theoretically lead to greater long-term adaptations. Importantly, occlusion pressure is heavily affected by cuff width, as wider cuffs require lower absolute pressures to similarly reduce blood flow as compared with narrow ones [23]. Also, it has been suggested that individualized occlusion pressure determination may be a more appropriate approach in BFR-RT, preventing under- or overestimation of occlusion pressure, and thus allowing a more accurate exercise prescription when compared to generalized and non-individualized protocols [24]. Finally, differences may also be related to the small samples within each study, which could increase the chance for a type II error, warranting a meta-analytic approach.
Thus, the aim of the present article was to perform a systematic review and meta-analysis of the effects of HL- versus BFR-RT on muscle strength and mass adaptations. A secondary purpose was to explore the muscle strength and hypertrophy responses between these protocols taking into account potential moderators such as test specificity (i.e., dynamic 1RM and isometric or isokinetic test), absolute occlusion pressure, cuff width, and occlusion pressure prescription method.
2 Methods
2.1 Search Strategy and Study Selection
The articles were identified through the databases PubMed and ISI Web of Knowledge from the earliest record up to January 2017. The search strategy combined the terms “Kaatsu training”, “practical Kaatsu training”, “practical blood flow restriction training”, “practical blood flow strength training”, “blood flow restriction training” “resistance training associated with blood flow restriction”, “strength training associated with blood flow restriction”, “low-load resistance training associated with blood flow restriction”, “low-intensity associated with blood flow restriction”, “muscle strength”, “muscle force”, “hypertrophic response”, “hypertrophy”, and “muscle mass”. Titles and abstracts for the retrieved articles were evaluated by two reviewers (ML and RB) to assess their eligibility for the meta-analysis. In case of disagreements, a consensus was adopted or, if necessary, a third reviewer evaluated the article (FCV). If the abstract did not provide sufficient information regarding the inclusion criteria, the reviewers read the full text.
2.2 Eligibility Criteria
Articles were eligible for inclusion if they met the following criteria: (a) pre- and post-training assessment of muscular strength (i.e., dynamic, isometric, or isokinetic test); (b) pre- and post-training assessment of muscle hypertrophy (i.e., magnetic resonance imaging, computerized tomography, or ultrasonography); (c) compared HL-RT (i.e., > 65% 1RM) vs. BFR-RT (i.e., < 50% 1RM); (d) score ≥ 4 on the Physiotherapy Evidence Database (PEDro) scale; (e) means and standard deviations (or standard errors) were reported from absolute values or allow estimation from graphs. If this last criterion was not met, data were directly requested from the authors.
2.3 Study Quality
The study quality was assessed with the PEDro scale, based on the list of Delphi [25]. The scale is composed of 11 questions of which only 10 can be scored. The non-rated question influences external validity, but not the internal or statistical validity of the trial. To be included in the present meta-analysis, the study must have met at least 4 points on the PEDro scale (see Electronic Supplementary Material (ESM), Table S1). Two reviewers (ML and RB) scored the studies according to the proposed scale. In case of disagreements, a consensus was adopted or, if necessary, a third reviewer evaluated the article (FCV).
2.4 Data Extraction
Two reviewers (ML and RB) separately and independently evaluated all articles and extracted data. Relevant data regarding participant characteristics (i.e., age and sex), study characteristics (i.e., training frequency, exercise, sets, repetitions, exercise load, absolute occlusion pressure, occlusion pressure prescription, cuff type and intervention period), muscular strength testing (i.e., dynamic, isometric, and isokinetic) and muscle mass (magnetic resonance imaging or ultrasound) were extracted. Importantly, when multiple time points for muscle strength and muscle mass were assessed, the latter/last time point available was considered as the post-training value for analysis. In order to assess potential coder drift, two reviewers (ML and RB) independently recorded 100% of the articles. Afterwards, all of the studies were cross-checked to confirm accuracy. In case of disagreement, a consensus was adopted or, if necessary, was solved by a third researcher (FCV). Data extracted are available in Tables 1 and 2.
2.5 Statistical Analyses
All analyses were conducted using Comprehensive Meta-analysis version 2.2 software (Biostat Inc., Englewwod, NJ, USA). Between-group comparisons (HL- vs. BFR-RT) were calculated as the effect size difference (ESdiff) using pre- and post-intervention (muscle strength and mass), pre-intervention standard deviation, sample size and pre- to post-correlation for each group. Provided that none of the studies included in the meta-analysis presented pre- to post-correlation, this was estimated with the following formula: \( r = \left( {S_{\text{pre}}^{2} + S_{\text{post}}^{2} {-}S_{\text{D}}^{2} } \right)/ 2\times \left( {S_{\text{pre}} \times S_{\text{post}} } \right) \). S is the standard deviation, and S D is the standard deviation of the difference score (pre- to post-intervention), defined by: S D = root square \( \left[ {\left( {S_{\text{pre}}^{2} /n} \right) + \left( {S_{\text{post}}^{2} /n} \right)} \right] \). All ESdiff were corrected for small sample size bias with the following formula: [1 − (3/(4 × (n 1 + n 2 − 2) − 1)]. Heterogeneity for between-study variability was verified with the I2 statistics, with thresholds set as I 2 = 25% (low), I 2 = 50% (moderate), and I 2 = 75% (high) [26]. Based on the results, data were then analyzed using fixed-effect models. Despite the low between-study heterogeneity, the present meta-analysis further explored potential moderators that could influence the results, expanding the knowledge on whether BFR characteristics could affect training responses.
The first analysis compared the effects of HL-and BFR-RT on muscle strength and mass response. Subsequently, a subgroup analysis was performed to investigate the effects of test specificity (specific [1RM] and nonspecific [isometric or isokinetic]), absolute occlusion pressure (≤ 110 or ≥ 111 mmHg), cuff width (≤ 139 or ≥ 140 mm) and occlusion pressure prescription (individualized or non-individualized) on muscle strength response. Similarly, additional analyses were performed to investigate the effects of absolute occlusion pressure value, cuff width, and occlusion pressure prescription (i.e., individualized or non-individualized) on muscle hypertrophy outcomes. Given the inconsistency of absolute occlusion pressure and cuff width among studies and the inherent relationship between these parameters [23] we opted to cluster studies according to the median values of these variables. That is, studies were separated with values below or above the median values for absolute occlusion pressure (≤ 110 or ≥ 111 mmHg) or cuff width (≤ 139 or ≥ 140 mm). Importantly, after the clustering procedure, all studies classified as “narrow cuff” were the same as those classified as “higher absolute occlusion pressure” and vice-versa. Furthermore, relative changes pre- to post-intervention were calculated (post-intervention × 100/pre-intervention − 100) for both HL- and BFR-RT. A sensitivity analysis was carried out to identify the presence of highly influential studies, which might bias the analyses. Thus, an analysis removing one study at a time was performed, and then examining its effect on between-group comparisons. Studies were considered as influential if removal resulted in a change of the ESdiff from significant (P ≤ 0.05) to non-significant (P > 0.05) or if removal caused a large change in the magnitude of the coefficient. This procedure has been adopted elsewhere [27]. Furthermore, publication bias was verified via funnel plot analysis. The significance level adopted was P < 0.05. All data are presented as mean ± standard error.
3 Results
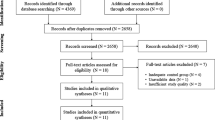
The initial search process returned 708 studies. After that, 504 duplicated studies were excluded. Then, titles and abstracts of the remaining studies were read, from which 190 were excluded. The remaining 14 articles were fully read and 13 studies were considered eligible according to our previously set criteria. After multiple unsuccessful attempts to contact the authors, hypertrophy and strength data from one study could not be included [28]. The search process is depicted in Fig. 1.
Twelve studies investigating muscle strength gains between HL- vs. BFR-RT were included in the present meta-analysis, resulting in 24 treatment outcome measures in 460 participants. Mean ES across all studies was 0.74 ± 0.07 (95% confidence interval (CI) 0.60–0.88). Mean muscle strength percentage gain was 14.36 ± 1.53% (95% CI 11.37–17.35). Between-group comparisons showed significantly higher gains in muscle strength for HL-RT as compared with BFR-RT (ESdiff: 0.63 ± 0.09; 95% CI 0.43–0.80) (Fig. 2). This was equivalent to a percentage gain difference of 7.36%, favoring HL-RT. A similar pattern was observed when considering test specificity, with ESdiff favoring HL-RT in either specific (i.e., 1RM; ESdiff: 0.63 ± 0.11; 95% CI 0.41– 0.85) or nonspecific (i.e., isometric and isokinetic; ESdiff: 0.58 ± 0.17; 95% CI 0.25–0.92) muscle strength assessment (Fig. 3). Importantly, BFR-RT was still less effective when compared with HL-RT even when accounting for absolute occlusion pressure and cuff width. Results from our cluster analysis revealed that narrower cuffs at higher-absolute occlusion pressure or wider cuffs at lower-absolute occlusion pressures resulted in smaller strength gains when compared with HL-RT (ESdiff: 0.52 ± 0.15; 95% CI 0.23–0.81 and (ESdiff: 0.68 ± 0.12; 95% CI 0.45–0.92, respectively) (Fig. 4). Finally, occlusion pressure prescription method did not affect the results, as either individualized or non-individualized methods resulted in smaller muscle strength gains as compared with HL-RT (ESdiff: 0.73 ± 0.18; 95% CI 0.39–1.07 and ESdiff: 0.57 ± 0.11; 95% CI 0.36–0.79, respectively) (Fig. 5). Sensitivity analysis (i.e., removing one study at a time and re-analyzing the data) revealed that muscle strength results were not highly affected by any single study (data not shown). Furthermore, funnel plot analysis revealed the presence of an influential study (Fig. 6). The study outside the funnel limit, on the left side of Fig. 6, introduced a minor publication bias with Kendall’s tau with continuity correction equal to 0.18 (P = 0.20), and Egger’s regression intercept equal to 5.66 (P = 0.051). Removing this study from the analysis resulted in Kendall’s tau with continuity correction value equal to 0.11 (P = 0.46), and Egger’s regression intercept equal to 2.69 (P = 0.36), minimizing publication bias. The fill and trim procedure did not affect the effect size estimates. As the influence of the aforementioned study on the ES was trivial, we retained it in the analysis.
Forest plot displaying the overall ESdiff for muscle strength adaptations between high-load resistance training (HL-RT) vs. low-load resistance training associated with blood-flow restriction (BFR-RT). Different letters for the same study represent different protocols. The data are shown as ESdiff and 95% confidence interval. ES diff effect size difference
Forest plot displaying the ESdiff for muscle strength between high-load resistance training (HL-RT) vs. low-load resistance training associated with blood-flow restriction (BFR-RT) according to test specificity. Different letters for the same study represent different protocols. The data are shown as ESdiff and 95% confidence interval. ES diff effect size difference
Forest plot displaying the ESdiff for muscle strength between high-load resistance training (HL-RT) vs. low-load resistance training associated with blood-flow restriction (BFR-RT) according to absolute occlusion pressure and cuff width. Different letters for the same study represent different protocols. The data are shown as ESdiff and 95% confidence interval. ES diff effect size difference
Forest plot displaying the ESdiff for muscle strength between high-load resistance training (HL-RT) vs. low-load resistance training associated with blood-flow restriction (BFR-RT) according to occlusion pressure prescription method. Different letters for the same study represent different protocols. The data are shown as ESdiff and 95% confidence interval. ES diff effect size difference
Funnel plot of studies comparing muscle strength between high-load resistance training (HL-RT) vs. low-load resistance training associated with blood-flow restriction (BFR-RT). The diamond represents the Hedges’ g overall standard error. Removal of the study outside the funnel limit on the left side of the figure minimized publication bias
Regarding gains in muscle mass, ten studies were included resulting in 20 effect sizes for between-group comparisons and 368 total sample size. Mean ES across all studies was 0.48 ± 0.04 (95% CI 0.40–0.56). Mean percentage gain in muscle mass was 7.22 ± 0.58% (95% CI 6.08–8.37). Between-group comparisons showed similar gains in muscle hypertrophy for HL- as compared with BFR-RT (ESdiff: 0.10 ± 0.10; 95% CI −0.10 to 0.30) (Fig. 7), which corresponds to a non-clinically relevant 0.74% gain difference between protocols in favor of HL-RT. The magnitude of muscle hypertrophy was not affected by either absolute occlusion pressure or cuff width, as both wider cuffs at lower absolute occlusion pressure and narrow cuffs at higher absolute occlusion pressure resulted in similar gains in muscle mass when compared to HL-RT (ESdiff: 0.11 ± 0.12; 95% CI −0.14 to 0.35 and ESdiff: 0.09 ± 0.17; 95% CI −0.25 to 0.42, respectively) (Fig. 8). Finally, pooling studies according to the occlusion pressure prescription method revealed that both individualized and non-individualized prescription resulted in similar muscle mass accrual to that observed in HL-RT (ESdiff: 0.24 ± 0.17; 95% CI −0.09 to 0.57 and ESdiff: 0.02 ± 0.13; 95% CI −0.23 to 0.27, respectively) (Fig. 9). Sensitivity analyses showed that muscle hypertrophic response was not affected by any particular study (data not shown). Furthermore, funnel plot analysis revealed no influential study (Fig. 10), with a Kendall’s tau with continuity correction equal to −0.14 (P = 0.38), and Egger’s regression intercept equal to −3.20 (P = 0.17).
Forest plot displaying the overall ESdiff for muscle hypertrophy between high-load resistance training (HL-RT) vs. low-load resistance training associated with blood-flow restriction (BFR-RT). Different letters for the same study represent different protocols. 1Mean values for quadriceps cross-sectional area between the proximal and distal portions. The data are shown as ESdiff and 95% confidence interval. ES diff effect size difference
Forest plot displaying the ESdiff for muscle hypertrophy between high-load resistance training (HL-RT) vs. low-load resistance training associated with blood-flow restriction (BFR-RT) according to absolute occlusion pressure and cuff width. Different letters for the same study represent different protocols. 1Mean values for quadriceps cross-sectional area between the proximal and distal portions. The data are shown as ESdiff and 95% confidence interval. ES diff effect size difference
Forest plot displaying the ESdiff for muscle hypertrophy between high-load resistance training (HL-RT) vs. low-load resistance training associated with blood-flow restriction (BFR-RT) according to occlusion pressure prescription method. Different letters for the same study represent different protocols. 1Mean values for quadriceps cross-sectional area between the proximal and distal portions. The data are shown as ESdiff and 95% confidence interval. ES diff effect size difference
4 Discussion
The present meta-analysis aimed to compare the effects of HL- versus BFR-RT on muscle strength and mass. The main results showed higher increases in muscle strength for HL- as compared with BFR-RT, even when considering specificity of the muscle strength test (i.e., specific [1RM] or nonspecific [isometric and isokinetic] testing). Importantly, none of the BFR-RT characteristics investigated (i.e., absolute occlusion pressure value, cuff width, and occlusion pressure prescription) influenced the muscle strength response (i.e., higher muscle strength gains for HL- as compared with BFR-RT). Regarding hypertrophic response, the overall results revealed similar increases in muscle mass between HL- and BFR-RT. Muscle hypertrophy was not influenced by absolute occlusion pressure and cuff width, as both wider-cuff lower-pressure and narrow-cuff higher-pressure BFR-RT protocols showed similar increases in muscle mass as compared to HL-RT. Finally, despite occlusion pressure prescription (i.e., individualized or non-individualized), BRF-RT was shown to be effective in inducing similar muscle mass accrual to those observed in HL-RT.
4.1 Muscle Strength
The superior gains in muscle strength observed after the HL-RT protocols could be related to a motor unit (MU) recruitment level, which is typically estimated via surface electromyography (EMG). Cook et al. [29] showed higher EMG amplitude during an acute HL- as compared with a BFR-RT session. Similar results were observed in the long term, as 12 weeks of training significantly increased surface EMG amplitude in HL-RT, with no changes in BFR-RT [11]. Furthermore, the authors observed a trend toward greater increases in isometric maximum voluntary contraction (MVC) in the HL- as compared with BFR-RT group. Importantly, in this study, only HL-RT adjusted the training load throughout intervention, which might have influenced muscle strength results. Conversely, Takarada et al. [28] demonstrated similar surface EMG amplitude acutely between HL- versus BFR-RT and comparable isokinetic MVC gains between protocols after 16 training weeks. Although these results are difficult to reconcile, MU recruitment estimated via surface EMG has been shown to be problematic due to methodological limitations. Surface EMG is an indirect measure of MU recruitment, represented by the sum of recruitment, firing rate (discharge rate), and synchronization of all the active muscle fibers underneath the electrode area, with important implications when attempting to compare HL- versus BFR-RT. In this regard, differences between protocols may be related to possibly different behaviors in recruitment, firing rate, and MU synchronization. Thus, despite studies showing possibly lower EMG amplitude during BFR- as compared with HL-RT, MU recruitment cannot be properly measured with actual EMG methods, which are based only on signal amplitude. Future studies should more comprehensively investigate possible differences in MU recruitment between protocols.
In addition to surface EMG, neural adaptations to different RT protocols have been evaluated through twitch-interpolation technique, which estimates voluntary muscle activation level to a given task [30]. However, to the best of the authors’ knowledge, only two studies [11, 31] investigated voluntary activation levels after long-term periods of BFR-RT, and only one compared BFR- to a HL-RT protocol [11]. For instance, 12 weeks of training increased voluntary activation level by ~ 3% in HL-RT, with no significant changes in the BFR-RT group [11]. Although these results suggest a potentially greater effect of HL-RT on muscle activation, some concerns should be highlighted. As mentioned previously, in Kubo et al. [11], only the HL-RT group adjusted the load during the intervention (performing additional 1RM tests at weeks 4 and 8); hence, given that this group not only routinely practiced with the 1RM test but, also, and most importantly, progressively increased the load, the results may be misleading. Similarly, others have not observed significant increases in muscle activation levels after long-term periods of BFR-RT [31]; however, this study did not include a HL-RT group, precluding more definite conclusions. Nevertheless, in conjunction, these results suggest that BFR- protocols may be not as effective as HL-RT to increase voluntary muscle activation levels, which is in consonance with our findings regarding muscle strength.
Recently, it has been suggested that differences in muscle strength adaptations between RT protocols may be related to test specificity [21]. Indeed, HL-RT has been shown to induce greater gains in muscle strength than low-load RT when assessed by specific testing procedures (i.e., 1RM test); however, when muscle strength was evaluated through non-specific testing (i.e., isometric MVC), both RT protocols showed similar results [32]. These results are somewhat in accordance with the present meta-analysis, as we observed superior gains in muscle strength for HL-RT in specific tests. However, even when using non-specific tests, HL-RT was still shown to be more effective in increasing muscle strength than BFR-RT. Interestingly, it has been suggested that specificity deficit between different RT protocols could be mitigated by routinely practicing with 1RM [33]. According to the authors, adding testing sessions (i.e., 1RM tests) during the intervention resulted in similar increases in muscle strength between HL- and low-load RT, despite test specificity theoretically favoring the former. The literature, however, does not support this contention when considering BFR protocols, as others have still [6, 7, 12] found HL-RT to induce greater gains in muscle strength than BFR, even in studies that periodically adjusted training load, and thus provided multiple 1RM testing sessions throughout the intervention. It is important to emphasize that both Morton et al. [33] and Mitchell et al. [32] compared HL- with low-load-RT (and not with BFR-RT), with the latter encompassing far greater exercise volumes than typical BFR-RT, which could account for the dissonant results.
Occlusion pressure has been considered an important variable within BFR-RT, as it is thought to modulate muscle adaptation [22, 28, 34, 35]. Nevertheless, occlusion pressure is highly dependent on cuff width [23, 36]. Thus, in order to gain insight as to whether absolute occlusion pressure could affect muscle strength response, we conducted a sub-analysis dividing studies into clusters according to not only absolute occlusion pressure but also according to cuff width. Importantly, all studies within the lower absolute occlusion pressure cluster were also the ones classified within the wider cuff width cluster. The results demonstrated that neither absolute occlusion pressure nor cuff width affected muscle strength capacity, given that all BFR-RT protocols resulted in lower gains in muscle strength as compared with HL-RT. This seems in line with current literature, as previous studies demonstrated that neither occlusion pressure nor cuff width influence muscle strength adaptations to BFR-RT [6, 16, 37].
It is important to note that only a few studies within the present meta-analysis used individualized occlusion pressure prescriptions [6, 7, 16, 20]. This has important implications, as a given absolute pressure may impose different degrees of vascular restriction depending upon limb circumference, individual blood pressure, and cuff width [23, 36]. Thus, it has been suggested that individualized occlusion pressure determination, accounting for cuff width, may be a more appropriate approach in BFR-RT, preventing under- or overestimation of occlusion pressure, and thus allowing a more accurate exercise prescription when compared to generalized occlusion pressures [24]. Despite these suggestions, when considering the occlusion pressure prescription analysis (i.e., individualized or non-individualized), our results demonstrated that both methods produce lower gains in muscle strength as compared with HL-RT. Interestingly, previous studies have demonstrated that when considering cuff width and individualized prescription, pressures as low as 40% may be all that is necessary to improve muscle strength capacity [6, 37].
Collectively, these data suggest that HL-RT is superior to BFR-RT in inducing gains in muscle strength, even after accounting for possible moderators. Importantly, individuals engaged in BFR-RT can substantially increase muscle strength capacity; however, this training protocol might not be considered optimal. Interestingly, combining BFR-RT with occasional HL-RT sessions may optimize muscle strength adaptations and mitigate possible differences between protocols [13].
4.2 Muscle Hypertrophy
BFR-RT has been widely advocated as a valid strategy to induce gains in muscle mass, with allegedly comparable results to those of HL-RT. The present results corroborate with these assertions and add to the current literature by demonstrating similar efficacy between protocols by means of a robust meta-analytic procedure. Nevertheless, BFR-RT characteristics such as occlusion pressure, cuff width, and occlusion pressure prescription method have been thought to influence training adaptations. In this sense, the present meta-analysis aimed to further explore the possible effects of these moderators on muscle mass accrual.
Occlusion pressure has been suggested to influence muscle hypertrophic response to BFR-RT [6, 22, 34, 35]. However, our exploratory analysis clustering studies according to absolute occlusion pressure revealed no significant effect of this variable on muscle mass accrual. Namely, both the lower- and the higher-pressure BRF-RT protocols resulted in similar increases in muscle mass as compared to HL-RT. It is important to highlight that considering absolute occlusion pressure values irrespective of cuff width may be misleading, as occlusion pressure is highly influenced by cuff width [36, 38].
In this respect, all studies classified as “lower-pressure” were also those clustered as “wider-cuff” and vice versa. This analysis yielded similar results, as both variables (i.e., absolute occlusion pressure and cuff width) were shown not to influence muscle hypertrophic response. Our results corroborate previous studies demonstrating that neither occlusion pressure [6, 37] nor cuff width [38] affect the muscle mass response to BFR-RT. These results are of practical application as occlusion pressure was previously shown to be directly related to pain and rating of perceived exertion, suggesting that lower-pressure BFR-RT (hence perceived as more comfortable and less physically demanding) could be effectively employed, particularly in those individuals with lower tolerance to physical stress.
Additionally, the present meta-analysis explored the effects of the occlusion pressure prescription method (i.e., individualized vs. non-individualized) on muscle hypertrophy. Individualized prescription accounts for individual anatomical differences (e.g., limb circumference, fat and muscle cross-sectional area), as well as for cuff width, allowing a more robust approach by avoiding under- or overestimation of blood flow restriction to musculature [23]. Interestingly, both individualized and non-individualized protocols showed comparable hypertrophy to that with HL-RT. This suggests that both prescription methods provided sufficient blood flow restriction to the working muscle, directly affecting fatigue and MU recruitment, which are often described to underpin BFR-RT-related adaptations [39,40,41].
Despite the above, one may argue that the CIs for hypertrophy may show a trend towards greater response to HL-RT. Importantly, the ESdiff between RT protocols, regardless of moderators, translate to a difference lower than 1% for muscle hypertrophy. The clinical relevance of such a small difference is debatable and may be confined to specific populations. Finally, although speculative, these small differences may be related to fiber-type specificity. In fact, there is short-term evidence to suggest BFR-RT to preferentially stresses type-I fibers [42]; however, long-term studies suggest otherwise [43, 44]. Importantly, data on direct comparison in fiber-type-specific response between BFR- and HL-RT are still lacking.
4.3 Limitations
The present meta-analysis has some limitations. Absolute occlusion pressure values are highly influenced by cuff width. Given the discrepancies between studies for these variables, it is difficult to understand what a given absolute occlusion pressure for a wider cuff represents on a narrower one and how it affects vascular restriction. Therefore, results must be interpreted with caution. In addition, due to the sparse number of studies comparing BFR- with HL-RT, we could not perform additional analyses for other important potential moderators (e.g., volume, frequency, and sex). Studies included herein did not report pre- to post-correlation for muscle mass and strength, thus, we estimated these correlation parameters for all studies (see Sect. 2.5). Importantly, the estimated values were very similar to those obtained from our laboratory, allowing us to assume that our estimations were within the expected range. Finally, we were not able to include data from Takarada et al. [28]; however, according to our sensitivity analysis we observed that no single study was able to significantly change the magnitude of response between protocols. Thus, the lack of these data most likely would not have changed the present results and interpretations.
5 Conclusions
In conclusion, the results from the present meta-analysis demonstrate superior muscle strength gains for HL- as compared with BFR-RT, even when adjusting for potential moderators (i.e., test specificity, absolute occlusion pressure, cuff width, and occlusion pressure prescription method). Regarding the hypertrophic response, HL-RT was shown to induce comparable increases in muscle mass when compared to BFR-RT, regardless of absolute occlusion pressure, cuff width, and occlusion pressure prescription method, supporting its efficacy, despite differences in BFR-RT protocols across research groups.
From a practical standpoint, individuals with special interest in increasing maximum muscle strength may benefit from a more specific training method (i.e., HL-RT); however, when considering muscle mass accrual, both HL- and BFR-RT seem equally effective. Finally, it is important to highlight that BFR-RT is still a valid and effective approach for increasing muscle strength in a wide spectrum of age and physical capacity, although it may seem particularly beneficial for those individuals with physical limitations to engage in HL-RT.
References
Coffey TH. Delorme method of restoration of muscle power by heavy resistance exercises. Treat Serv Bull. 1946;1(2):8–11.
Campos GE, Luecke TJ, Wendeln HK, et al. Muscular adaptations in response to three different resistance-training regimens: specificity of repetition maximum training zones. Eur J Appl Physiol. 2002;88(1–2):50–60. doi:10.1007/s00421-002-0681-6.
Kraemer WJ, Ratamess NA. Fundamentals of resistance training: progression and exercise prescription. Med Sci Sports Exerc. 2004;36(4):674–88.
Schoenfeld BJ, Wilson JM, Lowery RP, et al. Muscular adaptations in low- versus high-load resistance training: a meta-analysis. Eur J Sport Sci. 2016;16(1):1–10. doi:10.1080/17461391.2014.989922.
ACSM. ACSM clinician profile. David T. Bernhardt, M.D. Curr Sports Med Rep. 2009;8(4):161. doi:10.1249/JSR.0b013e3181adff73.
Lixandrao ME, Ugrinowitsch C, Laurentino G, et al. Effects of exercise intensity and occlusion pressure after 12 weeks of resistance training with blood-flow restriction. Eur J Appl Physiol. 2015;115(12):2471–80. doi:10.1007/s00421-015-3253-2.
Vechin FC, Libardi CA, Conceicao MS, et al. Comparisons between low-intensity resistance training with blood flow restriction and high-intensity resistance training on quadriceps muscle mass and strength in elderly. J Strength Cond Res. 2015;29(4):1071–6. doi:10.1519/JSC.0000000000000703.
Manimmanakorn A, Hamlin MJ, Ross JJ, et al. Effects of low-load resistance training combined with blood flow restriction or hypoxia on muscle function and performance in netball athletes. J Sci Med Sport. 2013;16(4):337–42. doi:10.1016/j.jsams.2012.08.009.
Mattar MA, Gualano B, Perandini LA, et al. Safety and possible effects of low-intensity resistance training associated with partial blood flow restriction in polymyositis and dermatomyositis. Arthritis Res Ther. 2014;16(5):473. doi:10.1186/s13075-014-0473-5.
Slysz J, Stultz J, Burr JF. The efficacy of blood flow restricted exercise: a systematic review and meta-analysis. J Sci Med Sport. 2016;19(8):669–75. doi:10.1016/j.jsams.2015.09.005.
Kubo K, Komuro T, Ishiguro N, et al. Effects of low-load resistance training with vascular occlusion on the mechanical properties of muscle and tendon. J Appl Biomech. 2006;22(2):112–9.
Karabulut M, Abe T, Sato Y, et al. The effects of low-intensity resistance training with vascular restriction on leg muscle strength in older men. Eur J Appl Physiol. 2010;108(1):147–55. doi:10.1007/s00421-009-1204-5.
Yasuda T, Ogasawara R, Sakamaki M, et al. Combined effects of low-intensity blood flow restriction training and high-intensity resistance training on muscle strength and size. Eur J Appl Physiol. 2011;111(10):2525–33. doi:10.1007/s00421-011-1873-8.
Martin-Hernandez J, Marin PJ, Menendez H, et al. Muscular adaptations after two different volumes of blood flow-restricted training. Scand J Med Sci Sports. 2013;23(2):e114–20. doi:10.1111/sms.12036.
Clark BC, Manini TM, Hoffman RL, et al. Relative safety of 4 weeks of blood flow-restricted resistance exercise in young, healthy adults. Scand J Med Sci Sports. 2011;21(5):653–62. doi:10.1111/j.1600-0838.2010.01100.x.
Laurentino GC, Ugrinowitsch C, Roschel H, et al. Strength training with blood flow restriction diminishes myostatin gene expression. Med Sci Sports Exerc. 2012;44(3):406–12. doi:10.1249/MSS.0b013e318233b4bc.
Ozaki H, Yasuda T, Ogasawara R, et al. Effects of high-intensity and blood flow-restricted low-intensity resistance training on carotid arterial compliance: role of blood pressure during training sessions. Eur J Appl Physiol. 2013;113(1):167–74. doi:10.1007/s00421-012-2422-9.
Thiebaud RS, Loenneke JP, Fahs CA, et al. The effects of elastic band resistance training combined with blood flow restriction on strength, total bone-free lean body mass and muscle thickness in postmenopausal women. Clin Physiol Funct Imaging. 2013;33(5):344–52. doi:10.1111/cpf.12033.
Ellefsen S, Hammarstrom D, Strand TA, et al. Blood flow-restricted strength training displays high functional and biological efficacy in women: a within-subject comparison with high-load strength training. Am J Physiol Regul Integr Comp Physiol. 2015;309(7):R767–79. doi:10.1152/ajpregu.00497.2014.
Libardi CA, Chacon-Mikahil MP, Cavaglieri CR, et al. Effect of concurrent training with blood flow restriction in the elderly. Int J Sports Med. 2015;36(5):395–9. doi:10.1055/s-0034-1390496.
Buckner SL, Jessee MB, Mattocks KT, et al. Determining strength: a case for multiple methods of measurement. Sports Med. 2017;47(2):193–5. doi:10.1007/s40279-016-0580-3.
Loenneke JP, Kim D, Fahs CA, et al. Effects of exercise with and without different degrees of blood flow restriction on torque and muscle activation. Muscle Nerve. 2014;. doi:10.1002/mus.24448.
Loenneke JP, Fahs CA, Rossow LM, et al. Effects of cuff width on arterial occlusion: implications for blood flow restricted exercise. Eur J Appl Physiol. 2012;112(8):2903–12. doi:10.1007/s00421-011-2266-8.
Loenneke JP, Fahs CA, Rossow LM, et al. Blood flow restriction pressure recommendations: a tale of two cuffs. Front Physiol. 2013;4:249. doi:10.3389/fphys.2013.00249.
Verhagen AP, de Vet HC, de Bie RA, et al. The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidemiol. 1998;51(12):1235–41.
Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. doi:10.1136/bmj.327.7414.557.
Schoenfeld BJ, Ogborn D, Krieger JW. Dose-response relationship between weekly resistance training volume and increases in muscle mass: a systematic review and meta-analysis. J Sports Sci. 2016. doi:10.1080/02640414.2016.1210197.
Takarada Y, Takazawa H, Sato Y, et al. Effects of resistance exercise combined with moderate vascular occlusion on muscular function in humans. J Appl Physiol (1985). 2000;88(6):2097–106.
Cook SB, Murphy BG, Labarbera KE. Neuromuscular function after a bout of low-load blood flow-restricted exercise. Med Sci Sports Exerc. 2013;45(1):67–74. doi:10.1249/MSS.0b013e31826c6fa8.
Becker R, Awiszus F. Physiological alterations of maximal voluntary quadriceps activation by changes of knee joint angle. Muscle Nerve. 2001;24(5):667–72.
Moore DR, Burgomaster KA, Schofield LM, et al. Neuromuscular adaptations in human muscle following low intensity resistance training with vascular occlusion. Eur J Appl Physiol. 2004;92(4–5):399–406. doi:10.1007/s00421-004-1072-y.
Mitchell CJ, Churchward-Venne TA, West DW, et al. Resistance exercise load does not determine training-mediated hypertrophic gains in young men. J Appl Physiol (1985). 2012;113(1):71–7. doi:10.1152/japplphysiol.00307.2012.
Morton RW, Oikawa SY, Wavell CG, et al. Neither load nor systemic hormones determine resistance training-mediated hypertrophy or strength gains in resistance-trained young men. J Appl Physiol (1985). 2016;121(1):129–38. doi:10.1152/japplphysiol.00154.2016.
Sugaya M, Yasuda T, Suga T, et al. Change in intramuscular inorganic phosphate during multiple sets of blood flow-restricted low-intensity exercise. Clin Physiol Funct Imaging. 2011;31(5):411–3. doi:10.1111/j.1475-097X.2011.01033.x.
Yasuda T, Brechue WF, Fujita T, et al. Muscle activation during low-intensity muscle contractions with restricted blood flow. J Sports Sci. 2009;27(5):479–89. doi:10.1080/02640410802626567.
Crenshaw AG, Hargens AR, Gershuni DH, et al. Wide tourniquet cuffs more effective at lower inflation pressures. Acta Orthop Scand. 1988;59(4):447–51.
Counts BR, Dankel SJ, Barnett BE, et al. Influence of relative blood flow restriction pressure on muscle activation and muscle adaptation. Muscle Nerve. 2016;53(3):438–45. doi:10.1002/mus.24756.
Laurentino GC, Loenneke JP, Teixeira EL, et al. The effect of cuff cidth on cuscle adaptations after blood blow restriction training. Med Sci Sports Exerc. 2016;48(5):920–5. doi:10.1249/MSS.0000000000000833.
Loenneke JP, Fahs CA, Wilson JM, et al. Blood flow restriction: the metabolite/volume threshold theory. Med Hypotheses. 2011;77(5):748–52. doi:10.1016/j.mehy.2011.07.029.
McCall GE, Byrnes WC, Dickinson A, et al. Muscle fiber hypertrophy, hyperplasia, and capillary density in college men after resistance training. J Appl Physiol (1985). 1996;81(5):2004–12.
Takada S, Okita K, Suga T, et al. Low-intensity exercise can increase muscle mass and strength proportionally to enhanced metabolic stress under ischemic conditions. J Appl Physiol (1985). 2012;113(2):199–205. doi:10.1152/japplphysiol.00149.2012.
Cumming KT, Paulsen G, Wernbom M, et al. Acute response and subcellular movement of HSP27, alphaB-crystallin and HSP70 in human skeletal muscle after blood-flow-restricted low-load resistance exercise. Acta Physiol (Oxf). 2014;211(4):634–46. doi:10.1111/apha.12305.
Nielsen JL, Aagaard P, Bech RD, et al. Proliferation of myogenic stem cells in human skeletal muscle in response to low-load resistance training with blood flow restriction. J Physiol. 2012;590(Pt 17):4351–61. doi:10.1113/jphysiol.2012.237008.
Yasuda T, Abe T, Sato Y, et al. Muscle fiber cross-section area is increased after two weeks of twice daily KAATSU-resistance training. Int J Kaatsu Train Res. 2005;1:65–70.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The authors are grateful to Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) for financial support and Fundação de Amparo à Pesquisa (FAPESP). Manoel Lixandrão is supported by CNPq and FAPESP (141733/2016-0 and 2016/22635-6, respectively). Hamilton Roschel is supported by CNPq and FAPESP (307023/2014-1 and 2016/10993-5, respectively). Carlos Ugrinowitsch is supported by CNPq (304205/2011-7 and 2016/09759-8, respectively).
Conflict of interest
Manoel Lixandrão, Carlos Ugrinowitsch, Ricardo Berton, Felipe Vechin, Miguel Conceição, Felipe Damas, Cleiton Libardi, and Hamilton Roschel declare that they have no conflicts of interest relevant to the content of this review.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lixandrão, M.E., Ugrinowitsch, C., Berton, R. et al. Magnitude of Muscle Strength and Mass Adaptations Between High-Load Resistance Training Versus Low-Load Resistance Training Associated with Blood-Flow Restriction: A Systematic Review and Meta-Analysis. Sports Med 48, 361–378 (2018). https://doi.org/10.1007/s40279-017-0795-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-017-0795-y