Abstract
Background
The anaplastic lymphoma kinase (ALK) inhibitor treatment landscape is rapidly evolving, providing patients with ALK-positive (+) non-small cell lung cancer (NSCLC) with multiple therapy options, multiple lines of treatments, and prolonged survival. However, these recent treatment advances have resulted in additional increases in treatment costs. The objective of this article is to review the economic evidence of ALK inhibitors in patients with ALK+ NSCLC.
Methods
The systematic review was conducted in accordance with the Joanna Briggs Institute (JBI) systematic reviews of economic evaluation. The population included adult patients with locally advanced (stage IIIb/c) or metastatic (stage IV) NSCLC cancer with confirmed ALK fusions. The interventions included the ALK inhibitors alectinib, brigatinib, ceritinib, crizotinib, ensartinib, or lorlatinib. The comparators included the listed ALK inhibitors, chemotherapy, or best supportive care. The review considered cost-effectiveness analysis studies (CEAs) that reported incremental cost-effectiveness ratio in quality-adjusted life years and/or in life years gained. Published literature was searched in Medline (via Ovid) by 4 January 2023, in Embase (via Ovid) by 4 January 2023, in International Pharmaceutical Abstracts (via Ovid) by 4 January 2023, and in Cochrane library (via Wiley) by 11 January 2023. Preliminary screening of titles and abstracts was conducted against the inclusion criteria by two independent researchers followed by a full text of selected citations. Search results are presented in a Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flow diagram. Critical appraisal was conducted using the validated Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS) tool as well as the Phillips et al. 2004 appraisal tool to assess the reporting and quality of the economic evaluations. Data were extracted from the final set of articles and presented in a table of characteristics of included studies, an overview of study methods of included studies, and a summarization of outcomes of included studies.
Results
A total of 19 studies met all inclusion criteria. The majority of the studies were in the first-line treatment setting (n = 15). Included CEAs varied in the interventions and comparators being evaluated and were conducted from different country perspectives, limiting their comparability. Outcomes from the included CEAs showed that ALK inhibitors may be considered a cost-effective treatment option for patients with ALK+ NSCLC in the first-line and subsequent lines of treatment setting. However, the probability of cost effectiveness of ALK inhibitors ranged from 46 to 100% and were mostly achieved at willingness-to-pay thresholds of $100,000 USD or higher (> $30,000 or higher in China) in the first-line treatment setting and at thresholds of $50,000 USD or higher in subsequent lines of treatment setting. The number of published full-text CEAs is low and the studies represent a handful of country perspectives. The source of survival data was dependent on data from randomized controlled trials (RCTs). Where RCT data were not available, indirect treatment comparisons or matched adjusted indirect comparisons were performed using efficacy data from different clinical studies. Real world evidence was rarely used for efficacy and costing data inputs.
Conclusion
The findings summarized available evidence on cost effectiveness of ALK inhibitors for the treatment of patients with locally advanced or metastatic ALK+ NSCLC across lines of treatment settings and generated a valuable overview of analytical approaches utilized to support future economic analyses. To help further inform treatment and policy decisions, this review emphasizes the need for comparative cost effectiveness of multiple ALK inhibitors simultaneously using real-world data sources with broad representation of settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
There is a limited number of available full text cost-effectiveness analysis study (CEAs) publications examining the cost effectiveness of ALK inhibitors for the treatment of patients with ALK+ NSCLC. |
From the available full-text CEA publications, the majority are in the first-line treatment setting and represent very few country perspectives. |
Included CEAs varied in the interventions and comparators being evaluated and were conducted from different country perspectives, limiting their comparability. |
Outcomes from the included CEAs showed that ALK inhibitors may be considered a cost-effective treatment option for patients with ALK+ NSCLC in the first line and subsequent lines of treatment setting. However, the probability of cost effectiveness of ALK inhibitors ranged from 46% to 100% and were mostly achieved at willingness-to-pay thresholds of $100,000 USD or higher (> $30,000 or higher in China) in the first-line treatment setting and at thresholds of $50,000 USD or higher in the subsequent lines of treatment setting. |
Although data from randomized controlled trials were limited, real-world evidence was rarely used to support the objectives of the CEAs. |
1 Introduction
Lung cancer is the second most commonly diagnosed cancer worldwide (~ 2.2 million lung cancer cases per year) and results in the largest total number of cancer deaths (~ 25% of all cancer deaths) [1,2,3,4,5]. Non-small cell lung cancer (NSCLC) accounts for approximately 85% of lung cancers [5]. A percentage of the cancer of patients with NSCLC (~ 3–5%) expresses the anaplastic lymphoma kinase (ALK) gene alteration [6]. Globally, it is estimated that 75,000 individuals are diagnosed with ALK-positive (ALK+) NSCLC every year, 64,000 die from it, and the 5-year survival rate is ~ 25% [5,6,7]. The standard of care for patients with locally advanced or metastatic ALK+ NSCLC is targeted therapies known as tyrosine kinase inhibitors of the ALK or ALK inhibitors [8]. ALK inhibitors specifically target the proteins transcribed from the genomic alteration, inhibiting proliferation pathways that lead to cancer growth and survival [9]. The ALK inhibitor treatment landscape is rapidly evolving, providing patients with locally advanced or metastatic ALK+ NSCLC with multiple therapy options, multiple lines of treatments and prolonged survival [9, 10]. However, these advances have also resulted in significant evidence gaps on optimal treatment choice and pressure on healthcare systems due to increasing treatment costs [11, 12]. In 2011, crizotinib was the first ALK inhibitor to be approved for the treatment of patients with locally advanced or metastatic ALK+ NSCLC [9]. Crizotinib showed dramatic and prolonged responses compared with chemotherapy, although resistance and intracranial disease progression eventually occurred [10]. Additional ALK inhibitors were then developed. Ceritinib, alectinib, brigatinib, and lorlatinib have all received regulatory approval for the treatment of patients with locally advanced or metastatic ALK+ NSCLC in the first and subsequent lines of treatment setting (defined as >/= second line of treatment settings) from 2011 to present [13]. More recently, a phase 3 clinical trial demonstrated the efficacy and safety of ensartinib, a next-generation ALK inhibitor, compared with crizotinib in the first-line treatment setting [14]. Ensartinib received regulatory approval in China in 2022 for the treatment of patients with locally advanced or metastatic ALK+ NSCLC [15]. According to the National Comprehensive Cancer Network (NCCN) NSCLC panel September 2022 [16], five agents are recommended for the treatment of patients with locally advanced or metastatic ALK+ NSCLC on the basis of clinical trial data and FDA approval; alectinib, brigatinib, ceritinib, crizotinib, or lorlatinib. In the first-line treatment setting, alectinib, brigatinib, or lorlatinib are all preferred therapy options for patients with ALK+ NSCLC. Alectinib, brigatinib, or ceritinib are recommended in the subsequent line of treatment setting for patients who receive and progress on crizotinib. Lorlatinib is recommended as a subsequent therapy option after treatment with other ALK inhibitors, followed by platinum-based chemotherapy. Although ALK inhibitors are regulatory approved and recommended in guidelines, only a proportion of these therapies have received funding in healthcare systems around the world [17]. Economic analyses submitted to payer groups relied heavily on clinical trial data for model inputs and indirect treatment comparisons from single-arm studies or where the clinical trial comparator arms were no longer the standard of care. Some of the key noted concerns observed by reimbursement review committees included uncertainty in net clinical benefit compared with other available ALK inhibitors, lack of robust comparative direct/indirect data on outcomes important for decision making, limited real-world data demonstrating comparative effectiveness of ALK inhibitors, and incremental cost-effectiveness ratios (ICERs) much greater than acceptable willingness-to-pay (WTP) thresholds driven by high drug costs [18,19,20].
A number of studies examining the cost effectiveness of ALK inhibitors were conducted in different regions and used a multitude of analytical approaches, settings, WTP thresholds, and perspectives. However, a systematic review of these cost-effectiveness analysis studies (CEAs) has not yet been performed. The objective of this study is to systematically review published CEAs of ALK inhibitors for the treatment of patients with ALK+ NSCLC in first and subsequent lines of treatment settings. The findings will summarize available evidence on the cost effectiveness of ALK inhibitors across lines of treatment settings and will generate valuable insights on factors impacting cost effectiveness of ALK inhibitors, which may be useful for future economic analysis studies.
2 Methods
2.1 Search Strategy
The systematic review was conducted in accordance with the Joanna Briggs Institute (JBI) systematic reviews of economic evaluation [21, 22]. The protocol was submitted for registration on 3 February 2022 and automatically published by PROSPERO on 8 March 2022, with registration no. CRD42022308680. Search strategies were developed by the main author (LC) in collaboration with a health sciences librarian and were peer reviewed as per the Peer Review of Electronic Search Strategy tool by two independent reviewers (LC and NK) for each database [23].
The population, intervention, comparator, and outcomes (PICO) were defined prior to the literature search. The population included adult patients with locally advanced (stage IIIb/c) or metastatic (stage IV) NSCLC cancer with confirmed ALK genomic alterations. Advanced disease has been chosen since ALK inhibitors are approved in stages IIIb/c or stage IV NSCLC. The intervention included any ALK inhibitor with a marketing authorization and/or being studied in clinical trials for the treatment of patients with locally advanced or metastatic ALK+ NSCLC in the first-line treatment setting or subsequent lines of treatment setting including alectinib, brigatinib, ceritinib, crizotinib, ensartinib, or lorlatinib. The comparator included the previously described ALK inhibitors, chemotherapy, or best supportive care (BSC). Chemotherapy was defined as monotherapy or doublet therapy of cisplatin, carboplatin, paclitaxel, albumin-bound paclitaxel, docetaxel, gemcitabine, vinorelbine, etoposide, and/or pemetrexed. Best supportive care was defined as no systemic treatment or any supportive treatment provided to reduce symptoms of the disease (e.g., pain management) without systemic therapy. The review considered CEAs that reported an ICER in quality-adjusted life years (QALY) and/or in life years gained (LYG).
Published literature was searched in Medline (via Ovid) by 4 January 2023, Embase (via Ovid) by 4 January 2023, International Pharmaceutical Abstracts (via Ovid) by 4 January 2023, and Cochrane library (via Wiley) by 11 January 2023. Key search words used for the search strategy included NSCLC (e.g., Carcinoma, Non-Small-Cell Lung/), ALK inhibitors (e.g., Anaplastic Lymphoma Kinase/) and cost effectiveness (e.g., Economics/). Each concept was entered one at a time using subject headings and text words (with tools and mechanics of the searched database and combined using Boolean logic). The search strategy was adapted for each database. Full search strategies for each database are included in Supplementary Information and the exact export date for each is reported. The inclusion criteria consisted of the PICO elements and the exclusion criteria included abstracts, editorials, reviews, duplicates, publications not in English language, non-CEAs, and grey literature due to language limitations and redactions of confidential information. No date restrictions were incorporated. The number of records were recorded using the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flow diagram [26].
2.2 Data Extraction and Synthesis
Data extraction was conducted by two researchers independently (LC and NK). Any disagreements between the researchers were resolved through discussion and a third reviewer was not needed. An expert oncologist (NL) and health economist (WW) were consulted to ensure the most appropriate variables and terminology were used for data extraction. The extracted data were presented in tables that provide an overview of the characteristics of included CEA, an overview of the study methods of included CEAs, and an overview of the outcomes of included CEAs. All extracted variables were presented as stated in the published papers and no conversion to common currency was applied to any of the costing data. Data synthesis included a detailed description and discussion on the comparability of the study population and treatments across included CEAs, on the suitability of the analytical approaches undertaken by the included CEAs, and on the comparability of outcomes across included CEAs by intervention, by region, and by source of funding in the first-line treatment setting and in subsequent lines of treatment setting.
2.3 Quality Assessments
Eligible studies were critically appraised by two independent researchers (LC and NK) using standardized critical appraisal instruments for economic evaluations. CHEERS 2022 was used to assess the comprehensiveness of the reporting and Phillips et al. was used to assess the quality of the model-based evaluations [24, 25]. Any disagreements between the researchers were resolved through discussion. All studies, regardless of the results of their comprehensiveness of reporting and/or their methodological quality, underwent data extraction and synthesis (where possible).
3 Results
3.1 Literature Search
The PRISMA diagram [26] demonstrating the flow of studies that were selected for data extraction on the basis of inclusion criteria is shown in Fig. 1. The search strategy yielded a total of 4885 potentially relevant records excluding duplicates. Title and abstracts were screened by the two researchers, yielding 231 unique records for full-text review. Full-text screening was then conducted by the same two researchers and records were excluded for various reasons detailed in Fig. 1. A final set of 19 publications were included for analysis [27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45].
PRISMA [26] diagram of flow of studies that were selected for data extraction based on inclusion criteria. IPA International Pharmaceutical Abstracts
3.2 Overview of the Characteristics of Included CEAs
Table 1 provides an overview of the study population(s), line(s) of treatment setting, intervention(s), comparator(s), and study objectives of the included CEAs. The majority of the included CEAs were in the first-line treatment setting (n = 15) [27, 29, 31,32,33,34,35,36,37,38, 40,41,42, 44, 45], while a few of the included CEAs were in subsequent lines of treatment setting (n = 4) [29, 30, 39, 43].
In the first-line treatment setting, the study population was similar in all included CEAs and included patients with advanced NSCLC who did not previously receive systemic therapy in the advanced disease stage. The interventions included alectinib, brigatinib, ceritinib, crizotinib, ensartinib, or lorlatinib. The dose and duration of ALK inhibitors assumed in the models of included CEAs were based on the referenced clinical trial data for efficacy outcomes. For example, the dose and duration of alectinib was assumed at 600 mg BID (twice a day) every 28 days [29, 30, 32, 34, 36, 37, 42, 44], which is aligned with the RCTs referenced by the publications, including ALEX [46, 47], ALESIA [48, 49], and ALUR [50, 51]. Similarly, brigatinib was assumed at 180 mg OD (once per day) every 28 days with a 7-day lead-in period at 90 mg OD [42, 44], which is also aligned with the ALTA-1L RCT referenced by the publications [52, 53]. Moreover, ceritinib was assumed either at 750 mg OD every 28 days [28,29,30,31, 35, 44] or 450 mg OD every 28 days [36, 40], which is aligned with the ASCEND RCTs referenced by the included CEAs [54,55,56,57,58,59,60,61]. Additionally, crizotinib was assumed at 250 mg BID every 28 days [27, 29, 31,32,33,34, 36,37,38, 40,41,42, 44, 45], which is aligned with the referenced PROFILE RCTs [62,63,64,65,66,67], ensartinib was assumed at 225 mg OD every 28 days [44, 45], which is aligned with the referenced eXALT 3 RCT [14, 68], and lorlatinib was assumed at 100 mg OD every 28 days [39, 41, 43, 44], which is aligned with the referenced CROWN RCT [69, 70]. All ALK inhibitors were administered until progression, toxicity, or death as presented in Table 1. The comparators included platinum-based doublet chemotherapy, alectinib, brigatinib, ceritinib, crizotinib, or ensartinib. Platinum-based chemotherapy regimens were given up to four cycles [27, 31, 35] or up to 6 cycles [33] in the first-line treatment setting and the regimens consisted of a combination of pemetrexed plus cisplatin or carboplatin [27, 31, 33] or a combination of pemetrexed, paclitaxel, or etoposide plus platinum chemotherapy [35].
In subsequent lines of treatment setting, the study population differed between included CEAs and included patients who received prior crizotinib and/or chemotherapy [29, 30] or included patients with at least one ALK inhibitor and/or chemotherapy [39, 43]. For example, in Hurry et al. [28] and Carlson et al. [30], the cost effectiveness of ceritinib versus BSC/historical control/pemetrexed and alectinib versus ceritinib, respectively, were being compared in patients who have discontinued crizotinib. Therefore, both studies included patients who received prior crizotinib and/or chemotherapy. However, in Nilsson et al. [39] and in Gourzoulidis et al. [43], the objective of both studies was to determine the cost effectiveness of lorlatinib as second- or third-line treatment compared with chemotherapy. Therefore, both studies included patients with at least one other ALK inhibitor (since alectinib, crizotinib, and/or ceritinib may have been available for patients as part of standard of care) and/or chemotherapy. The interventions included alectinib [30], ceritinib [28], or lorlatinib [39, 43] at the same dose and duration as discussed in the first-line treatment setting above and presented in Table 1. The comparators included chemotherapy (monotherapy with pemetrexed or docetaxel) [28, 39, 43], ceritinib [30], or BSC (defined as no active treatment) [28]. The chemotherapy regimen consisted of pemetrexed 500 mg/m2 or docetaxel 75 mg/m2 IV every 21 days [28, 39, 43] with duration not specified [28] or until disease progression, toxicity, or death [39, 43].
The objective of all included CEAs was to evaluate the cost effectiveness of the intervention(s) compared with the comparator(s) using a model-based evaluation of cost effectiveness.
3.3 Overview of the Study Methods of Included CEAs
Table 2 provides an overview of study methods of included CEAs. Of the included CEAs, the year of publication ranged from 2014 to 2022. Only a few regions were represented, including China (n = 9 [29, 33,34,35,36, 38, 40, 44, 45]), the USA (n = 5 [20, 31, 41, 42]), Canada (n = 2 [27, 28]), France (n = 1 [37]), Greece (n = 1 [43]) and Sweden (n = 1 [39]). The majority of studies were funded by industry (n = 12 [28, 30,31,32,33, 35, 37,38,39,40, 42, 43]) with a few receiving no funding or funded by non-profit organizations (n = 7 [27, 29, 34, 36, 41, 44, 45]). Included CEAs used state-transition Markov models (n = 9 [27, 29, 30, 32,33,34,35,36, 44]) or partitioned survival models (n = 9 [28, 31, 39,40,41,42,43, 45]) and applied either QALY (n = 7 [29, 33, 35, 37, 38, 44, 45]) or both QALY and LYG (n = 12 [27, 28, 30,31,32, 34, 37, 39,40,41,42,43]) as outcomes. Time horizon varied across studies and ranged from 3 years to 30 years to extrapolate costs and outcomes. The cycle lengths were 2 months or less in all studies and the discount rate ranged from 3% to 5%. The majority of studies were conducted from a healthcare system perspective (n = 12 [27,28,29,30, 32,33,34,35,36, 38, 44, 45]) or a payer perspective (n = 6 [31, 37, 40,41,42,43]) with one study presented from a societal perspective [39] and a few studies presenting additional societal/patient perspectives [30, 37]. Sensitivity analyses were performed in all studies. Two studies conducted deterministic sensitivity analysis (DSA) only [27, 40], while the remainder of the studies conducted both DSA and probabilistic sensitivity analyses (PSA).
3.4 Overview of Outcomes of Included CEAs
Table 3 provides an overview of outcomes of included CEAs. The findings are summarized by intervention, by region, and by source of funding below for the first-line treatment setting and for subsequent lines of treatment setting.
3.5 Findings by Intervention
3.5.1 Alectinib
In the first-line setting, six CEAs examined the cost effectiveness of alectinib compared with crizotinib, ceritinib, or ensartinib. Compared with crizotinib, alectinib use was not considered cost effective in three CEAs conducted from a Chinese healthcare system perspective at a WTP threshold ranging from ~ $29,000–$50,000 United States dollars (USD) [29, 34, 36]. However, alectinib use was considered cost effective compared with crizotinib in two CEAs [32, 37], where alectinib had a 64% probability of being cost effective at a WTP threshold of $100,000 USD compared with crizotinib from a US healthcare system perspective and alectinib had a 50–70% probability of being cost effective at a WTP threshold of €110,000–162,000 EUR from a French public/private insurance and patient perspective, respectively [32, 37]. Multiple RCT study data are available directly comparing alectinib and crizotinib in a head-to-head clinical trial setting. As a result, the CEAs utilized efficacy data of direct treatment comparisons from the phase 3 ALEX [46, 47] or ALESIA [48, 49] RCTs and/or direct and indirect treatment comparisons from a network meta-analysis (NMA) of various RCTs [36]. Compared with ceritinib, alectinib use was not cost effective in one CEA conducted from a Chinese healthcare system perspective at a WTP threshold of $29,306 USD [29]. There are no head-to-head trials comparing alectinib with ceritinib. In the absence of a direct comparison, the CEA [29] utilized an indirect unadjusted comparison of treatment arms from two different RCTs, the ALEX [46, 47] and ASCEND-4 [58, 59] RCTs, for efficacy outcomes. Compared with ensartinib, alectinib use was not cost effective in one CEA conducted from a Chinese healthcare system perspective at a WTP threshold of $37,654 USD or lower [44]. There are no head-to-head clinical trials conducted that directly compare alectinib with ensartinib. In the absence of a direct comparison, the CEA [44] utilized an indirect adjusted treatment comparison of PROFILE 1029 [66, 67] and a published NMA [71] for efficacy outcomes.
In subsequent lines of treatment settings, only one CEA was published evaluating the cost effectiveness of alectinib compared with ceritinib from a US healthcare system and societal perspective [30]. In the absence of a direct comparison between alectinib and ceritinib, the CEA [30] utilized an indirect unadjusted comparison using efficacy data from pooled analysis of single-arm phase 1/2 studies, NP28761 [72, 73] and NP28673 [73, 74], for alectinib and efficacy data from pooled analysis of another single-arm phase 1/2 studies, ASCEND-1 [54, 55] and ASCEND-2 [56, 57], for ceritinib. At a WTP threshold of $100,000 USD, alectinib use had a 96% probability of being considered a cost-effective treatment option compared with ceritinib for the treatment of patients with ALK+ NSCLC in the second- or third-line treatment setting.
3.5.2 Brigatinib
In the first-line treatment setting, only one CEA has been published that examined the cost effectiveness of brigatinib compared with crizotinib and alectinib from a US payer perspective [42]. Compared with crizotinib, brigatinib use was considered a cost-effective option in the treatment of patients with ALK+ NSCLC in the first-line setting at a WTP threshold of $236,000 USD or higher (with probability, %, of being cost effective not reported) [42]. Compared with alectinib, the CEA concluded that brigatinib use provides a cost-saving option (with probability, %, of being cost saving not reported). The CEA [42] utilized data from the phase 3 ALTA-1L RCT [52, 53] for efficacy outcomes that directly compared brigatinib with crizotinib in a head-to-head trial in the first-line treatment setting. There are no head-to-head clinical trials comparing brigatinib with alectinib. In the absence of a direct comparison, the CEA [42] conducted a cost comparison only while assuming comparable efficacy measures and used an indirect adjusted MAIC of efficacy data from the phase 3 ALEX [46, 47] RCT for alectinib and the phase 3 ALTA-1L [52, 53] RCT for brigatinib.
In subsequent treatment settings, there were no CEAs published as full journal articles that examined the cost effectiveness of brigatinib for the treatment of patients with ALK+ NSCLC at the time of the literature search.
3.5.3 Ceritinib
In the first-line treatment setting, four CEAs examined the cost effectiveness of ceritinib compared with crizotinib or chemotherapy (pemetrexed and cisplatin or pemetrexed and carboplatin) [31, 35, 36, 40]. Compared with chemotherapy, ceritinib use was not considered a cost-effective treatment option in one CEA conducted from a Chinese healthcare system perspective with WTP thresholds of $27,143 USD [35]. However, ceritinib had an 84.3% probability of being a cost-effective treatment option in another CEA conducted from a US third-party payer perspective at a WTP threshold of $150,000 USD [31] compared with chemotherapy. Both CEAs [31, 35] utilized data from the phase 3 ASCEND-4 [58, 59] RCT, which directly compared ceritinib with chemotherapy. Compared with crizotinib, ceritinib use was considered a cost-effective treatment option in three CEAs [31, 36, 40]. In Zhou et al. [31], ceritinib had a 76% probability of being cost effective at a WTP threshold of $150,000 USD conducted from a US third-party perspective. In Li et al. [36], ceritinib use had a greater than 95% probability of being cost effective at a WTP threshold of $28,410 USD conducted from a Chinese healthcare system perspective. In Loong et al. [40], ceritinib use was considered a cost-effective treatment option at a WTP threshold of $119,274 USD conducted from a Hong Kong healthcare service or government perspective (PSA not performed). There are no head-to-head clinical trials available that directly compare ceritinib and crizotinib. As a result, the CEAs [31, 35, 40] conducted indirect adjusted treatment comparisons through MAIC or a NMA using multiple clinical trials as efficacy data sources for inputs including ASCEND-4 [58, 59], PROFILE 1014 [64, 65], and/or ALEX [46, 47].
In subsequent treatment settings, only one CEA was published comparing cost effectiveness of ceritinib with BSC, chemotherapy, or a historical control arm from a Canadian healthcare system perspective [28]. Ceritinib use had a 46.3%, 94%, and 99% probability of being cost effective at a WTP threshold of $150,000 Canadian Dollars (CAD) compared with BSC, pemetrexed, and the historical control arm, respectively. In the absence of head-to-head comparisons from a clinical trial setting at the time the CEA [28] was conducted, indirect unadjusted treatment comparisons were performed using efficacy data inputs from a pooled analysis of single-arm phase 1/2 studies, ASCEND-1 [54, 55] and ASCEND-2 [56, 57], for ceritinib and efficacy data inputs from a retrospective study of administrative claims data for the comparators [28].
3.5.4 Crizotinib
In the first-line treatment setting, crizotinib was compared with chemotherapy (platinum-doublet chemotherapy) in three CEAs [27, 33, 38]. Given that crizotinib was the first ALK inhibitor to be approved and ALK inhibitors are only indicated for patients whose cancers express the ALK gene fusion, cost of testing for the gene was also being evaluated in some CEAs. As a result, two of the three CEAs, Djalalov et al. [27] and Lu et al. [33], evaluated the cost effectiveness of testing for all patients with locally advanced or metastatic NSCLC and treatment with crizotinib for patients whose cancers express the ALK gene fusion compared with chemotherapy. Huang et al. [38] evaluated the cost of treatment only without incorporating the cost of testing.
In Djalalov et al. [27], testing and crizotinib use were not a cost-effective treatment option compared with no testing and chemotherapy for the treatment of patients with ALK+ NSCLC from a Canadian healthcare system perspective (WTP threshold not reported) with key drivers of the ICER being treatment-related utility with crizotinib and the cost of crizotinib. The CEA [27] utilized data from a phase 1 PROFILE 1001 [62, 63] single-arm study and data from a retrospective Canadian study [75] and performed an indirect unadjusted treatment comparison for efficacy outcomes into the model. In Lu et al. [33], testing and crizotinib use was also not a cost-effective treatment option compared with no testing and chemotherapy for the treatment of patients with ALK+ NSCLC from a Chinese healthcare system perspective at a WTP threshold of $32,000 USD, with key drivers of the ICER being utility of PFS and cost of treatments. The CEA [33] utilized data from the phase 3 PROFILE 1029 [66, 67] RCT as well as direct and indirect treatment comparisons from a published systematic literature review [76]. In Huang et al. [38], crizotinib use was not a cost-effective treatment option compared with chemotherapy from a Chinese healthcare system perspective and at a WTP threshold of $6,607 USD, with key drivers of the ICER not reported. Furthermore, Lu et al. [33] and Huang et al. [38] showed that when cost of crizotinib was covered by a patient assistance program or by medical insurance, testing and crizotinib use or crizotinib use became a cost-effective treatment option at a probability of cost effectiveness of 82% and 99%, respectively.
In subsequent lines of treatment settings, there were no CEAs published as full journal articles that examined the cost effectiveness of crizotinib for the treatment of patients with ALK+ NSCLC at the time of the literature search.
3.5.5 Ensartinib
In the first-line treatment setting, two CEAs, Luo et al. [44] and Zhang et al. [45], were published comparing the cost effectiveness of ensartinib compared with crizotinib, ceritinib, or brigatinib from a Chinese healthcare system perspective. Compared with crizotinib, Zhang et al. [45] showed that ensartinib use had a 100% probability of being a cost-effective treatment option for patients with ALK+ NSCLC at a WTP threshold of $38,163 USD. The CEA [45] utilized data from the eXALT3 RCT [14, 68], which directly compared ensartinib with crizotinib in a head-to-head trial in the first-line treatment setting. Similarly, Luo et al. [44] showed that ensartinib use was considered a cost-effective treatment option for patients with ALK+ NSCLC at a WTP threshold of $37,654 USD compared with crizotinib (PSA not reported). Compared with ceritinib and brigatinib, this CEA [44] also showed that ensartinib use was considered a dominant alternative option for patients with ALK+ NSCLC. Since there are no head-to-head clinical trials available that directly compare ensartinib with ceritinib or with brigatinib, the CEA [44] utilized indirect adjusted treatment comparisons of PROFILE 1029 [66, 67] and a published NMA [71] for efficacy data inputs into the model.
In subsequent treatment settings, there were no CEAs published as full journal articles that examined the cost effectiveness of ensartinib for the treatment of patients with ALK+ NSCLC at the time of the literature search.
3.5.6 Lorlatinib
In the first-line treatment setting, two CEAs were published comparing the cost effectiveness of lorlatinib compared with crizotinib or ensartinib [41, 44]. Compared with crizotinib, lorlatinib use was not considered a cost-effective treatment option for patients with ALK+ NSCLC from a US payer perspective at a WTP threshold of $200,000 USD [41]. The CEA [41] utilized efficacy data from the CROWN RCT [69, 70], which directly compared lorlatinib with crizotinib in a head-to-head trial in the first-line treatment setting. Compared with ensartinib, lorlatinib use was also not considered a cost-effective treatment option from a Chinese healthcare perspective and at a WTP threshold of $37,654 USD or lower [44]. Due to the lack of head-to-head studies comparing lorlatinib with ensartinib, the CEA [44] utilized a published NMA [71] for efficacy data inputs into the model.
In subsequent treatment settings, two CEAs, Nilsson et al. [39] and Gourzoulidis et al. [43], were published comparing lorlatinib with doublet chemotherapy from a Swedish societal perspective and from a Greek payer perspective, respectively. Both CEAs [39, 43] showed that lorlatinib use had approximately 100% and greater than 75% probability of being a cost-effective treatment option in the second- or third-line treatment setting at a WTP threshold of 1 million Swedish Krona Equals (SEK) and at a WTP threshold of €54,000 EUR, respectively. Due to the lack of head-to-head studies directly comparing lorlatinib with chemotherapy, the CEAs [39, 43] utilized an indirect adjusted MAIC from a phase two single-arm lorlatinib clinical study [83] for the lorlatinib efficacy outcomes and phase 3 ASCEND-5 [60, 61] and ALUR [50, 51] RCTs for the chemotherapy efficacy outcomes.
3.6 Findings by Region
In the USA, the cost effectiveness of alectinib, brigatinib, ceritinib, and lorlatinib were compared with crizotinib in four different CEAs for the treatment of patients with ALK+ NSCLC in the first-line treatment setting [31, 32, 41, 42]. Alectinib had a 64% probability of being cost effective at a WTP threshold of $100,000 USD [32], brigatinib had a high probability (PSA not reported) of being cost effective at a WTP threshold of > $236,000 USD [42], and ceritinib had a 76% probability of being cost effective at a WTP threshold of $150,000 USD [31] compared with crizotinib [31, 32, 42]. Lorlatinib use was not a cost-effective treatment option compared with crizotinib at the target WTP threshold of $200,000 USD [41]. The acceptability curve further showed that lorlatinib had a 90% probability of cost effectiveness only when the WTP threshold was increased to $448,000/QALY [41].
In China, the cost effectiveness of alectinib, ceritinib, and ensartinib were compared with crizotinib in seven different CEAs for the treatment of patients with ALK+ NSCLC in the first-line treatment setting [29, 34, 36, 40, 44, 45]. Compared with crizotinib, alectinib was not a cost-effective treatment option in three CEAs [29, 34, 36] at a WTP threshold of $29,306.37 USD, $28,109 USD, and $28,410 USD, respectively. The acceptability curve in Guan et al. [34] further demonstrated that alectinib had a 43.7% probability of being cost effective only when the WTP threshold was increased to $50,000 USD/QALY [34]. Compared with crizotinib, three CEAs examined the cost effectiveness of ceritinib [29, 36, 40]. In Liu et al. [29], ceritinib use was not considered a cost-effective treatment option at a WTP threshold of $29,306 USD. However, in Li et al. [36], ceritinib had a > 95% probability of being cost effective at a WTP threshold of $28,109 USD [36] and in Loong et al. [40], ceritinib use was considered a cost-effective treatment option at a WTP threshold of $119,274 USD (PSA not performed). Compared with crizotinib, two CEAs also demonstrated that ensartinib use was considered a cost-effective treatment option [44, 45] at a WTP threshold of $37,654 USD (PSA not reported) and at a 100% probability of being cost effective at a WTP threshold of $38,163 USD, respectively.
There were two CEAs that were conducted in Canada, in which the treatment and comparator in the CEAs differed [27, 28]. Other regions only had one CEA published [37, 39, 43].
3.7 Findings by Source of Funding
Of the included CEAs that were funded by industry, 9 of 12 (75%) CEAs showed that the intervention was cost effective compared with the comparator on the basis of their predetermined WTP thresholds [28, 30,31,32, 37, 39, 40, 42, 43], while 3 of 12 (25%) CEAs showed that the intervention was not cost effective compared with its comparator [3, 33] or cost effective only if a portion of the costs were covered by medical insurance [38]. Of included CEAs that received no funding or were funded by non-profit organizations, two of seven CEAs (28.5%) showed that the intervention was cost effective compared with the comparator on the basis of their predetermined WTP thresholds [44, 45], while four of seven CEAs (57%) showed that the intervention was not cost effective compared with the comparator [27, 29, 34, 41], with one CEA demonstrating both results of cost effectiveness and lack of cost effectiveness in the included interventions as compared with the comparators [36].
3.8 Reporting and Quality Assessment Findings Using CHEERS and Phillips Checklists
Table 4 provides an overview of the 28-item CHEERS 2022 checklist [24] for each of the 19 publications. Most of the publications comprehensively reported on the context, background, and objectives, as well as the study methods and measures of effectiveness. However, a few publications did not comprehensively report on the characteristics of the study population and subgroups [27,28,29, 31,32,33,34,35,36, 39, 40, 44] and on how the results vary amongst subgroups [28, 29, 31,32,33,34,35,36, 38, 40, 43,44,45]. The characteristics of the study population, although incomplete in some publications, may still be retrieved on the basis of the referenced clinical studies. In all 19 publications, reporting was missing or incomplete on items that were recently incorporated in the updated version of the CHEERS checklist, which include an indication to the development and location of a health economic analysis plan, efforts to engage with patients and/or relevant stakeholders, and the impact of the engagement on study findings. Huang et al. [38] had the most incomplete items compared with the other publications, including the type of decision model used, model structure, time horizon, cycle length, base case values, ranges, and distributional effects. This may be due to publication length limitations, as Huang et al. [38] had two study objectives covered in the manuscript: the results from a real-world retrospective study as well as results from a cost effectiveness study.
Table 5 provides an overview of the assessment of the quality of model-based evaluations for each of the 19 publications using Phillips et al. [25]. The quality of the methodological approaches undertaken by the included CEAs was high, with the majority of the items justified by the studies. In all publications, the objective of the model-based evaluations as well as the model types specified (except for Huang et al. [38] where the model type was not specified) were consistent with the stated decision problem, the choice of model inputs, the health condition under evaluation, and with the stated assumptions. The key areas for improvement include definition and justification of included [27,28,29, 31,32,33,34,35,36, 38,39,40,41]/excluded [27,28,29, 32, 34,35,36,37,38,39,40,41,42,43,44,45] options under evaluation, lack of use of half-cycle corrections [27, 29,30,31,32,33,34,35,36, 38, 40,41,42, 44, 45], and consideration of subgroups and sources of heterogeneity, which may impact the generalizability of the results [31,32,33, 36, 40, 43,44,45].
The results of the reporting and quality assessment should be interpreted with caution due to the subjective nature accompanied with these types of assessment tools.
4 Discussion
4.1 Cost Effectiveness of ALK Inhibitors for the Treatment of Patients with ALK+ NSCLC
Only 19 full-text CEA publications are available examining the cost effectiveness of ALK inhibitors for the treatment of patients with ALK+ NSCLC. The availability of full-text CEA publication is limited given the number of available ALK inhibitors as well as the number of abstracts available on this topic. From the available full-text publications, the majority are in the first-line treatment setting and represent very few country perspectives. Included CEAs varied in the interventions and comparators being evaluated and were conducted from different country perspectives, limiting their comparability. When the outcomes of included CEAs were summarized by intervention, the results showed that ALK inhibitors may be considered a cost-effective treatment option for patients with ALK+ NSCLC in the first- and subsequent lines of treatment setting. However, the probability of cost effectiveness of ALK inhibitors ranged from 46% to 100% and was mostly achieved at WTP thresholds of $100,000 USD or higher (> $30,000 or higher in China) in the first-line treatment setting and at WTP thresholds of $50,000 USD or higher in the second-line treatment setting.
Alectinib use may be considered a cost-effective treatment option in the first and subsequent lines of treatment setting compared with crizotinib and/or ceritinib at WTP thresholds of $100,000 USD or higher. Brigatinib use may be a cost-effective treatment option in the first-line treatment setting at a WTP threshold of $236,000 USD or higher compared with crizotinib. Additionally, ceritinib use may be a cost-effective treatment option in the first-line treatment setting at a WTP threshold above $100,000 USD compared with chemotherapy, at a WTP threshold of $28,410 USD or higher compared with crizotinib, and in subsequent lines of treatment setting at a WTP threshold of $150,000 USD compared with BSC, pemetrexed, or a historical control. Lastly, ensartinib use may be a cost-effective option in the first-line treatment setting at a WTP threshold of $37,654 USD or higher compared with crizotinib, while lorlatinib use may be a cost-effective option in subsequent lines of treatment at WTP thresholds of ~ $90,000 USD and €54,000 EUR compared with doublet chemotherapy.
All available CEAs examining the cost effectiveness of crizotinib showed that crizotinib use was not a cost-effective treatment option in the first-line treatment setting or subsequent lines of treatments except when a portion of the costs were covered by a patient assistance program or by medical insurance. Of importance to note, crizotinib was the first ALK inhibitor to be approved, shifting the standard of care for patients with locally advanced or metastatic ALK+ NSCLC from chemotherapy to ALK inhibitor therapy. As ALK inhibitors are only indicated for patients whose cancers express the ALK gene fusion, testing for the gene had to be incorporated into clinical practice for all patients with advanced NSCLC. Therefore, the CEAs conducted during that time for crizotinib incorporated two new interventions, testing for all patients with advanced NSCLC and crizotinib treatment for patients with ALK+ NSCLC. The inclusion of two new interventions for a rare population may have increased the difficulty for crizotinib to show cost effectiveness with a test and treat strategy even with the added benefit that crizotinib provides compared with chemotherapy. All other next-generation ALK inhibitors did not need to incorporate the cost of testing in the CEAs, as testing became standard of care by then and was already incorporated into clinical practice. Having said that, the included CEAs for crizotinib that incorporated the test-and-treat strategy showed that the key drivers of the ICER were utility and cost of treatment, not the cost of testing. In addition, although crizotinib was not shown to be cost effective, it was used as a comparator to determine the cost effectiveness of newer ALK inhibitors that, in some cases, were shown to be more cost effective than crizotinib. Demonstrating cost effectiveness compared with a comparator that was not shown to be cost effective may be a point of consideration by decision makers and reflects the complexity associated with suitable selection of comparators in CEAs.
4.2 Other Systematic Reviews Covering Similar Topics
This study serves as the first comprehensive review of all published articles of CEAs examining the cost effectiveness of ALK inhibitors in patients with ALK+ NSCLC. There are no other systematic reviews summarizing evidence on cost effectiveness of ALK inhibitors for the treatment of patients with advanced ALK+ NSCLC in any country and time period available in the literature. Yu et al. [77] provides a comprehensive review of cost effectiveness of targeted therapies and immunotherapies for the treatment of advanced NSCLC only in the USA from 2017 to 2020. In the ALK inhibitor component of the review, three CEAs were included [30,31,32]. The summarized findings from these three studies were consistent with the summary provided in this review for the CEAs conducted in the USA where alectinib has been shown to be more cost effective than crizotinib and ceritinib, ceritinib has been shown to be more cost effective than crizotinib and doublet chemotherapy, and ALK inhibitors are cost effective at a minimum WTP threshold of $100,000 USD. In another systematic review by Haslam et al. [78], the characteristics of CEAs for all oncology drugs approved in the USA from 2015 to 2020 were examined. Only one CEA study (of 134 CEAs) examining the cost effectiveness of alectinib in patients with advanced ALK+ NSCLC was included. The review did not provide a summary of cost effectiveness as the focus was to summarize characteristics of the CEAs, including the impact of funding source and conflict of interest on cost effectiveness outcomes, which are topics not addressed in detail in this review.
4.3 Suitability of Analytical Approaches Utilized in the CEAs
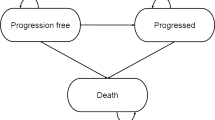
All CEAs used suitable model types and structures, Markov health state-transition models, or partitioned-survival models, to determine the cost effectiveness of ALK inhibitors in patients with ALK+ NSCLC [79]. This is because patients with locally advanced or metastatic NSCLC receive systematic treatment and stay on treatment until progression before moving into their next line of treatment setting(s) or until death. Once patients are in the advanced disease stage of ALK+ NSCLC, they do not get cured or move back into earlier lines of treatment. Model structures used in all included CEAs mimic the progression of advanced ALK+ NSCLC disease, where patients enter the model in the progression-free state then move into progressed disease state or into the death state. Transition probabilities are then applied to estimate the transition of individuals from state to state on the basis of survival data from clinical trials. Most of the included CEAs had a cycle length of 1 month, which is appropriate since patients are assessed for progression during ALK inhibitor treatment administration cycles (every 28 days) and median overall survival is ~ 35 months in the first-line treatment setting and ~ 20 months or less in subsequent lines of treatment settings [9, 10]. All CEAs assessed the comparative cost effectiveness using appropriate outcomes of LY gained, QALYs, incremental costs, and/or ICERs [79]. The time horizon varied amongst CEAs and the number of years increased over time, which is reflective of the prolonged survival of patients with locally advanced or metastatic ALK+ NSCLC with the availability of new and more effective ALK inhibitors over time [9, 10]. Perspectives were stated in all CEAs and included healthcare system, public or private payer, and societal and/or patient perspectives. However, the CEAs did not provide sufficient context on how healthcare was managed and funded within a country/region, who the decision makers were, and how various stakeholders (e.g., patients) may influence funding decisions. This lack of context made it difficult to interpret the impact of the CEA outcomes on the selected perspective.
4.4 Comparability of Study Population and Treatments Between Included CEAs
In the first-line treatment setting, the study population was comparable, as all CEAs included patients with advanced NSCLC who did not previously receive systemic therapy in the advanced disease stage. In subsequent line of treatment settings, the study population in the included CEAs was less comparable, as studies differed in their inclusion of historical treatments dependent on which treatments were available as part of the standard of care in the year of study and the intervention(s) and comparator(s) being compared [28, 30, 39, 43].
In the first-line treatment setting, the dose and duration of each ALK inhibitor examined across the various included CEAs were the same and based on their referenced clinical trials for efficacy outcomes. Ceritinib was the only ALK inhibitor that varied in dose across included CEAs. The variation of the ceritinib dose was due to a bioequivalence study, ASCEND-8 [80], which demonstrated similar efficacy and better tolerability of ceritinib at a dose of 450 mg OD compared with the dose used in earlier clinical trials of 750 mg OD. The CEAs that followed the ASCEND-8 findings incorporated the lower dose of ceritinib, which may have played a factor in the cost effectiveness of ceritinib compared with its comparators given the better tolerability and lower cost of treatment [36, 40]. The type and duration of doublet chemotherapy examined across included CEAs differed, which limits the comparability of the treatments used for the comparator arms across CEAs [27, 31, 33, 35].
In subsequent lines of treatment setting, the dose and duration of ALK inhibitors and chemotherapy was similar between the included CEAs [28, 30, 39, 43].
4.5 Source(s) of Survival Data
Source of survival data was dependent on data from head-to-head RCTs, where available. In many cases in which there is no clinical data from head-to-head RCTs for the treatment(s) and comparator(s), indirect treatment comparisons were performed, including unadjusted (naïve) treatment comparisons, matched adjusted indirect comparisons, or network metanalysis, using efficacy data from different RCT arms, single-arm studies, or from real-world studies. Comparing efficacy data from independent studies introduces heterogeneity and increases uncertainty of the results of the CEAs [81]. Even in cases in which the indirect comparisons adjust for observed differences in patient characteristics, there may be residual unobserved prognostic variables and effect modifiers that impact the results of the CEAs [81]. Moreover, with lack of guidelines in the assessment of cost effectiveness of technologies where there are no available head-to-head treatment comparisons from RCTs, variations in approach to clinical data inputs into the CEAs are high, as observed in this systematic review.
In the absence of head-to-head clinical trial evidence, real-world evidence may play an important role in generating evidence to support the comparative effectiveness of treatments from practice. However, real-world data was rarely used in included CEAs and its use was limited to historical comparator performance and mostly collected from a single institution data source. To enable more consistent approaches and relevant clinical data inputs in future CEAs with limited/no RCT data, guidelines should be established on the use of real-world evidence for both the intervention and the comparator. In addition, since ALK inhibitors are being used in clinical practice, re-conducting CEAs using real-world data would provide insights on the true effect of these therapies in practice and may pave the path for implementation considerations and maintaining/revising initial funding decisions.
4.6 Selection of Comparator(s)
The selection of comparator(s) in CEAs conducted during the earlier years were reflective of the standard of care at the time for patients with ALK+ NSCLC. For example, when crizotinib became the first ALK inhibitor to be approved in the first line of treatment setting, crizotinib was compared with chemotherapy in Djalalov et al. [27] and Lu et al. [33]. Ceritinib and alectinib subsequently emerged as next-generation ALK inhibitors and were appropriately compared with crizotinib or chemotherapy in Hurry et al. [28], Carlson et al. [30], Zhou et al. [31], Carlson et al. [32], Liu et al. [29], Guan et al. [34], and Peng et al. [35]. However, with the emergence of third- and fourth-generation ALK inhibitors, the CEAs should aim to compare the cost effectiveness of a new ALK inhibitor with multiple other available ALK inhibitors to ensure appropriate representation of the newer ALK inhibitors available for patients with locally advanced or metastatic ALK+ NSCLC, as well as representation of the recommended treatments in the guidelines [16], similar to the CEA conducted by Luo et al. [44]. Therefore, a few of the more recent CEAs should have selected more appropriate comparators on the basis of the year of reporting and the treatment guidelines being followed in the selected setting.
4.7 Key Model Drivers
In the first-line treatment setting, the key model drivers were drug and drug administrative cost for initial treatment, utilities in progression-free health state and costs associated with post-progression treatment. In subsequent lines of treatment setting, drug costs until treatment discontinuation were the key model driver as well as utilities in the subsequent therapy health state. With the emergence of multiple ALK inhibitors that prolong time to progression, the drug costs in the progression-free state increased. Similarly, with additional ALK inhibitors becoming available post-progression, the drug costs in the post-progression state increased as well. The additional drug costs in each disease state are offset to some extent by the clinical value (QALYs) that these new therapies are providing. However, even with the added clinical benefit, the key drivers of costs remain treatment related, which support opinion suggesting increased pressure on healthcare systems due to treatment costs.
4.8 Sponsor Bias in Included CEAs
Sponsor bias has been reported in cost-effectiveness analysis across a range of diseases and study designs [82]. Of the included CEAs in this study, a higher number of industry-funded CEAs showed that the intervention was cost effective compared with its comparator than non-industry funded CEAs on the basis of their predetermined WTP thresholds. However, since included CEAs differed in interventions and comparators, line of therapies, regions, and methods, it is difficult to draw any conclusion relating to sponsor bias, as the difference in the results between industry-funded and non-industry-funded CEAs may be dependent on a number of other factors. Moreover, due to the low number of published full-text CEAs on ALK inhibitors for the treatment of patients with ALK+ NSCLC, it limits the availability of a sufficient number of CEAs to be grouped on the basis of similar interventions, comparators, methods, regions, and funding.
4.9 Geographic Representation
Many high-income countries (e.g., the UK, France, Canada, and Australia) and middle-income countries (e.g., Turkey, China, and Brazil, etc.) rely on cost-effectiveness studies for health technology assessments to enable reimbursement decision making. However, the lack of broad geographic representation in published CEAs makes it difficult to establish rigorous conclusions on the most cost-effective treatment in each setting. A vast number of ALK inhibitor CEAs are available as Congress abstracts with broader geographic representation (n = 60 as shown in Fig. 1). Unfortunately, very few of these abstracts translate into full article publications.
4.10 Limitations of this Systematic Review
There are potential limitations to this review. First, caution should be taken when interpreting the summary of findings as variability in analytical approaches, settings, WTP thresholds, perspective, costs, healthcare administration, and availability of subsequent lines of treatments in the different countries impact the outcomes of each included study. Another key challenge of this systematic review is bias due to inclusion of full records only. There were 60 abstracts identified in the initial search examining the cost effectiveness of ALK inhibitors in patients with ALK+ NSCLC. The abstracts were excluded due to lack of ability to assess their quality and their lack of completeness for data extraction. Similarly, economic evaluation reports performed by payer groups and available in supplemental searches are valuable as they may provide another stakeholder opinion and approach to the assessment of new technologies. These reports were excluded as well due to language limitations and redactions of confidential information. Lastly, CEAs for newer ALK inhibitors, brigatinib, lorlatinib, and ensartinib, were limited and/or unavailable. As the treatment landscape continues to evolve with new ALK inhibitors and ALK inhibitor combinations, future CEAs should be conducted to assess CEAs that simultaneously compare various ALK inhibitors with each other.
5 Conclusion
The treatment landscape for patients with ALK+ NSCLC continues to rapidly evolve, leading to uncertainty in clinical and funding decisions. This study systematically reviewed published CEAs of ALK inhibitors for the treatment of patients with ALK+ NSCLC in first- and subsequent lines of treatment settings. The findings summarized available evidence on cost effectiveness of ALK inhibitors across lines of treatment settings and generated a valuable overview of analytical approaches utilized by published CEAs to support future economic analyses studies. The study also highlights the need for CEAs to be published as full-set articles, the need for sufficient representation from various countries that rely on CEAs for reimbursement decision making, and the need for real-world data to be used as a relevant source of evidence in the absence of direct treatment comparisons from clinical trials. Most importantly, as the use of ALK inhibitors is already established in practice and as the treatment landscape continues to evolve, CEAs need to assess the comparative cost effectiveness of multiple ALK inhibitors simultaneously using clinical and costing data that represent the real-world experience to enable insights that help validate and/or revise initial funding decisions. As a result, this study emphasizes the need for comparative cost-effectiveness efforts of multiple ALK inhibitors across lines of treatments using real-world data sources with broad representation of settings to enable conclusions on the most cost-effective ALK inhibitors for the treatment of patients with ALK+ NSCLC.
References
Blackadar CB. Historical review of the causes of cancer. World J Clin Oncol. 2016;7(1):54–86. https://doi.org/10.5306/wjco.v7.i1.54.
Sadikovic B, Al-Romaih K, Squire JA, Zielenska M. Cause and consequences of genetic and epigenetic alterations in human cancer. Curr Genom. 2008;9(6):394–408. https://doi.org/10.2174/138920208785699580.
Minamoto T, Mai M, Ronai Z. Environmental factors as regulators and effectors of multistep carcinogenesis. Carcinogenesis. 1999;20(4):519–27. https://doi.org/10.1093/carcin/20.4.519.
Schwaederle M, Kurzrock R. Actionability and precision oncology. Oncoscience. 2015;2(10):779–80.
Cancer.Net. Lung cancer—non-small cell—statistics. June 25, 2012. https://www.cancer.net/cancer-types/lung-cancer-non-small-cell/statistics.
Zhu QG, Zhang SM, Ding XX, He B, Zhang HQ. Driver genes in non-small cell lung cancer: characteristics, detection methods, and targeted therapies. Oncotarget. 2017;8(34):57680–92. https://doi.org/10.18632/oncotarget.17016.
Griesinger F, Roeper J, Pöttgen C, Willborn KC, Eberhardt WEE. Brain metastases in alk-positive nsclc—time to adjust current treatment algorithms. Oncotarget. 2018;9(80):35181–94. https://doi.org/10.18632/oncotarget.26073.
Melosky B. Rapidly changing treatment algorithms for metastatic nonsquamous non-small-cell lung cancer. Curr Oncol. 2018;25(Suppl 1):S68-76. https://doi.org/10.3747/co.25.3839.
Khan M, Lin J, Liao G, Tian Y, Liang Y, Li R, Liu M, Yuan Y. ALK inhibitors in the treatment of ALK positive NSCLC. Front Oncol. 2019;8:557. https://doi.org/10.3389/fonc.2018.00557.
Barrows SM, Wright K, Copley-Merriman C, Kaye JA, Chioda M, Wiltshire R, Torgersen KM, Masters ET. Systematic review of sequencing of ALK inhibitors in ALK-positive non-small-cell lung cancer. Lung Cancer Targ Ther. 2019;10:11–20. https://doi.org/10.2147/LCTT.S179349.
Migliorino MR, Santo A, Romano G, Cortinovis D, Galetta D, Alabiso O, Cartenì G, et al. Economic burden of patients affected by non-small cell lung cancer (nsclc): the life study. J Cancer Res Clin Oncol. 2017;143(5):783–91. https://doi.org/10.1007/s00432-016-2326-x.
Evans WK, Will BP, Berthelot J-M, Wolfson MC. The economics of lung cancer management in Canada. Lung Cancer. 1996;14(1):19–29. https://doi.org/10.1016/0169-5002(95)00510-2.
Elliott J, Bai Z, Hsieh S-C, Kelly SE, Chen L, Skidmore B, Yousef S, Zheng C, Stewart DJ, Wells GA. ALK inhibitors for non-small cell lung cancer: a systematic review and network meta-analysis. PLoS ONE. 2020;15(2): e0229179. https://doi.org/10.1371/journal.pone.0229179.
Horn L, Wang Z, Wu G, Poddubskaya E, Mok T, Reck M, Wakelee H, et al. Ensartinib vs crizotinib for patients with anaplastic lymphoma kinase-positive non-small cell lung cancer: a randomized clinical trial. JAMA Oncol. 2021;7(11):1617–25. https://doi.org/10.1001/jamaoncol.2021.3523.
NMPA (China) approves ensartinib to treat first line ALK positive NSCLC. https://www.medthority.com/news/2022/3/nmpachina-approves-ensartinib-to-treat-first-line-alk-positive-nsclc.--xcovery-holdings--betta-pharma-/. Accessed 27 Apr 2023.
NCCN. Guidelines detail. https://www.nccn.org/guidelines/guidelines-detail. Accessed 2 Nov 2022.
IASLC. The rising cost of lung cancer therapies: what are the global implications? https://www.iaslc.org/iaslc-news/ilcn/rising-cost-lung-cancer-therapies-what-are-global-implications. Accessed 19 July 2021.
Cancer Care Ontario. “Crizotinib.” https://www.cancercareontario.ca/en/drugformulary/drugs/crizotinib. Accessed 24 Oct 2021.
Cancer Care Ontario. “Ceritinib”. https://www.cancercareontario.ca/en/drugformulary/drugs/ceritinib. Accessed 24 Oct 2021.
Cancer Care Ontario. “Alectinib.” https://www.cancercareontario.ca/en/drugformulary/drugs/alectinib. Accessed 24 Oct 2021.
Aromataris E, Munn Z, Editors. JBI Manual for evidence synthesis. JBI, 2020. https://synthesismanual.jbi.global. https://doi.org/10.46658/JBIMES-20-01. Accessed 19 July 2021.
Gomersall JS, Jadotte YT, Xue Y, Lockwood S, Riddle D, Preda A. Conducting systematic reviews of economic evaluations. JBI Evid Implement. 2015;13(3):170–8. https://doi.org/10.1097/XEB.0000000000000063.
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–6. https://doi.org/10.1016/j.jclinepi.2016.01.021.
Husereau D, Drummond M, Augustovski F, et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) explanation and elaboration: a report of the ISPOR CHEERS II Good Practices Task Force. Value Health. 2022;25(1):10–31.
Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, et al. Review of guidelines for good practice in decision-analytic modelling in health technology assessment. Health Technol Assess. 2004;8(36). https://doi.org/10.3310/hta8360.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, et al. The PRISMA 2020 Statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89. https://doi.org/10.1186/s13643-021-01626-4.
Djalalov S, Beca J, Hoch JS, Krahn M, Tsao M-S, Cutz J-C, Leighl NB. Cost effectiveness of EML4-ALK fusion testing and first-line crizotinib treatment for patients with advanced ALK-positive non-small-cell lung cancer. J Clin Oncol. 2014;32(10):1012–9. https://doi.org/10.1200/JCO.2013.53.1186.
Hurry M, Zhou Z-Y, Zhang J, Zhang C, Fan L, Rebeira M, Xie J. Cost-effectiveness of ceritinib in patients previously treated with crizotinib in anaplastic lymphoma kinase positive (ALK+) non-small cell lung cancer in Canada. J Med Econ. 2016;19(10):936–44. https://doi.org/10.1080/13696998.2016.1187151.
Liu M, Zhang L, Huang Q, Li Na, Zheng B, Cai H. Cost-effectiveness analysis of ceritinib and alectinib versus crizotinib in the treatment of anaplastic lymphoma kinase-positive advanced non-small cell lung cancer. Cancer Manag Res. 2019;11(101512700):9195–202. https://doi.org/10.2147/CMAR.S223441.
Carlson JJ, Canestaro W, Ravelo A, Wong W. The cost-effectiveness of alectinib in anaplastic lymphoma kinase-positive (ALK+) advanced NSCLC previously treated with crizotinib. J Med Econ. 2017;20(7):671–7. https://doi.org/10.1080/13696998.2017.1302453.
Zhou Z-Y, Mutebi A, Han S, Bensimon AG, Ricculli ML, Xie J, Dalal A, Culver K. Cost-effectiveness of ceritinib in previously untreated anaplastic lymphoma kinase-positive metastatic non-small cell lung cancer in the United States. J Med Econ. 2018;21(6):577–86. https://doi.org/10.1080/13696998.2018.1443111.
Carlson JJ, Suh K, Orfanos P, Wong W. Cost effectiveness of alectinib vs crizotinib in first-line anaplastic lymphoma kinase-positive advanced non-small-cell lung cancer. Pharmacoeconomics. 2018;36(4):495–504. https://doi.org/10.1007/s40273-018-0625-6.
Lu S, Yu Y, Fu S, Ren H. Cost-effectiveness of ALK testing and first-line crizotinib therapy for non-small-cell lung cancer in China. PLoS ONE. 2018;13(10): e0205827. https://doi.org/10.1371/journal.pone.0205827.
Guan H, Sheng Y, Guo W, Han S, Shi L. Cost-effectiveness of alectinib for patients with untreated ALK-positive non-small cell lung cancer in China. Adv Ther. 2019;36(5):1114–25. https://doi.org/10.1007/s12325-019-00908-7.
Peng Ye, Ma F, Tan C, Wan X, Yi L, Peng L, Zeng X. Model-based economic evaluation of ceritinib and platinum-based chemotherapy as first-line treatments for advanced non-small cell lung cancer in China. Adv Ther. 2019;36(11):3047–58. https://doi.org/10.1007/s12325-019-01103-4.
Li H, Lai L, Bin Wu. Cost effectiveness of ceritinib and alectinib versus crizotinib in first-line anaplastic lymphoma kinase-positive advanced non-small-cell lung cancer. Clin Drug Investig. 2020;40(2):183–9. https://doi.org/10.1007/s40261-019-00880-8.
Savignon M, Monnier R, Tehard B, Roze S. Cost-effectiveness of alectinib compared to crizotinib for the treatment of first-line ALK+ advanced non-small-cell lung cancer in France. PLoS ONE. 2020;15(1): e0226196. https://doi.org/10.1371/journal.pone.0226196.
Huang M, Tian Y, He M, Liu J, Ren L, Gong Y, Peng F, et al. Crizotinib versus chemotherapy: a real-world cost-effectiveness study in China. J Compar Effect Res. 2020;9(2):93–102. https://doi.org/10.2217/cer-2019-0075.
Nilsson FOL, Asanin ST, Masters ET, Iadeluca L, Almond C, Cooper M, Smith S. The cost-effectiveness of lorlatinib versus chemotherapy as a second- or third-line treatment in anaplastic lymphoma kinase (ALK)-positive non-small-cell lung cancer in Sweden. Pharmacoeconomics. 2021;39(8):941–52. https://doi.org/10.1007/s40273-021-01015-8.
Loong HH, Wong CKH, Leung LKS, Chan CPK, Chang A, Zhou Z-Y, Xie J, Gibbs M. Cost-effectiveness analysis of ceritinib vs. crizotinib in previously untreated anaplastic lymphoma kinase (ALK)-positive non-small cell lung cancer (NSCLC) in Hong Kong. Cost Effect Resour Alloc C/E. 2020;18(1):50. https://doi.org/10.1186/s12962-020-00244-6.
Li S, Li JH, Peng LB, Li YM, Wan XM. Cost-effectiveness of lorlatinib as a first-line therapy for untreated advanced anaplastic lymphoma kinase-positive non-small cell lung cancer. Front Oncol. 2021;11(101568867): 684073. https://doi.org/10.3389/fonc.2021.684073.
Cranmer H, Kearns I, Young M, Humphries MJ, Trueman D. The cost-effectiveness of brigatinib in adult patients with ALK inhibitor-naive ALK-positive non-small cell lung cancer from a US perspective. J Manag Care Spec Pharm. 2022;28(9):970–9. https://doi.org/10.18553/jmcp.2022.28.9.970.
Gourzoulidis G, Zisimopoulou O, Boubouchairopoulou N, Michailidi C, Lowry C, Tzanetakos C, Kourlaba G. Cost-effectiveness analysis of lorlatinib in patients previously treated with anaplastic lymphoma kinase inhibitors for non-small cell lung cancer in Greece. J Health Econ Outcomes Res. 2022;9(1):50–7. https://doi.org/10.36469/jheor.2022.32983.
Luo X, Zhou Z, Zeng X, Peng L, Liu Q. Cost-effectiveness of ensartinib, crizotinib, ceritinib, alectinib, brigatinib and lorlatinib in patients with anaplastic lymphoma kinase-positive non-small cell lung cancer in China. Front Public Health. 2022;10: 985834. https://doi.org/10.3389/fpubh.2022.985834.
Zhang X, Fang P, Guangquan Su, Gui S, Shen A. Cost-effectiveness of ensartinib for patients with anaplastic lymphoma kinase-positive non-small-cell lung cancer in China. J Compar Effect Res. 2022;11(12):871–8. https://doi.org/10.2217/cer-2022-0066.
Roche HL. Randomized, Multicenter, Phase III, Open-label study of alectinib versus crizotinib in treatment-naive anaplastic lymphoma kinase-positive advanced non-small cell lung cancer. Clinical trial registration. clinicaltrials.gov, March 1, 2023. https://clinicaltrials.gov/ct2/show/NCT02075840.
Camidge DR, Dziadziuszko R, Peters S, Mok T, Noe J, Nowicka M, Gadgeel SM, et al. Updated efficacy and safety data and impact of the eml4-alk fusion variant on the efficacy of alectinib in untreated ALK-positive advanced non–small cell lung cancer in the global phase III ALEX study. J Thorac Oncol. 2019;14(7):1233–43. https://doi.org/10.1016/j.jtho.2019.03.007.
Roche H-L. Randomized, multicenter, phase III, open-label study of alectinib versus crizotinib in Asian patients with treatment-naive anaplastic lymphoma kinase-positive advanced non-small cell lung cancer. Clinical trial registration. clinicaltrials.gov, September 6, 2019. https://clinicaltrials.gov/ct2/show/NCT02838420.
Zhou C, Kim S-W, Reungwetwattana T, Zhou J, Zhang Y, He J, Yang J-J, et al. Alectinib versus crizotinib in untreated Asian patients with anaplastic lymphoma kinase-positive non-small-cell lung cancer (ALESIA): a randomised phase 3 study. Lancet Respir Med. 2019;7(5):437–46. https://doi.org/10.1016/S2213-2600(19)30053-0.
Roche H-L. Randomized, Multicenter, Phase III, Open-label study of alectinib versus pemetrexed or docetaxel in anaplastic lymphoma kinase-positive advanced non small cell lung cancer patients previously treated with platinum-based chemotherapy and crizotinib. Clinical trial registration. clinicaltrials.gov, October 7, 2019. https://clinicaltrials.gov/ct2/show/NCT02604342.
Signorovitch JE, Sikirica V, Erder MH, Xie J, Lu M, Hodgkins PS, et al. Matching-adjusted indirect comparisons: a new tool for timely comparative effectiveness research. Value Health. 2012;15(6):940–7.
Ariad Pharmaceuticals. “A phase 3 multicenter open-label study of brigatinib (AP26113) versus crizotinib in patients with ALK-positive advanced lung cancer.” Clinical trial registration. Clinicaltrials.gov, July 27, 2021. https://clinicaltrials.gov/ct2/show/NCT02737501.
Camidge, D. Ross, Hye Ryun Kim, Myung-Ju Ahn, James C.H. Yang, Ji-Youn Han, Maximilian J. Hochmair, Ki Hyeong Lee, et al. “Brigatinib versus crizotinib in ALK inhibitor–naive advanced ALK-positive NSCLC: final results of phase 3 ALTA-1L trial.” Journal of Thoracic Oncology 16, no. 12 (December 2021): 2091–2108. https://doi.org/10.1016/j.jtho.2021.07.035.
Novartis Pharmaceuticals. “A phase I, multi-center, open label dose escalation study of LDK378, administered orally in adult patients with tumors characterized by genetic abnormalities in anaplastic lymphoma kinase (ALK).” Clinical trial registration. Clinicaltrials.gov, November 28, 2018. https://clinicaltrials.gov/ct2/show/NCT01283516.
Kim, Dong-Wan, Ranee Mehra, Daniel S W Tan, Enriqueta Felip, Laura Q M Chow, D Ross Camidge, Johan Vansteenkiste, et al. “Intracranial and whole-body response of ceritinib in ALK inhibitor-naïve and previously ALK inhibitor-treated patients with ALK-rearranged non-small-cell lung cancer (NSCLC): updated results from the phase 1, multicentre, open-label ASCEND-1 trial.” The Lancet. Oncology 17, no. 4 (April 2016): 452–63. https://doi.org/10.1016/S1470-2045(15)00614-2.
Novartis Pharmaceuticals. “A phase II, multicenter, single-arm study of oral LDK378 in adult patients with ALK-activated non-small cell lung cancer previously treated with chemotherapy and crizotinib.” Clinical trial registration. Clinicaltrials.gov, May 25, 2017. https://clinicaltrials.gov/ct2/show/NCT01685060.
“Multicenter phase II study of whole-body and intracranial activity with ceritinib in patients with ALK-rearranged non–small-cell lung cancer previously treated with chemotherapy and crizotinib: results from ASCEND-2.” Journal of Clinical Oncology. Accessed November 5, 2021. http://ascopubs.org/doi/pdf/https://doi.org/10.1200/JCO.2015.65.5936.
Novartis Pharmaceuticals. “A Phase III Multicenter, Randomized Study of Oral LDK378 Versus Standard Chemotherapy in Previously Untreated Adult Patients With ALK Rearranged (ALK-Positive), Stage IIIB or IV, Non-Squamous Non-Small Cell Lung Cancer.” Clinical trial registration. clinicaltrials.gov, March 30, 2023. https://clinicaltrials.gov/ct2/show/NCT01828099.
Soria, Jean-Charles, Daniel S W Tan, Rita Chiari, Yi-Long Wu, Luis Paz-Ares, Juergen Wolf, Sarayut L Geater, et al. “First-line ceritinib versus platinum-based chemotherapy in advanced ALK -rearranged non-small-cell lung cancer (ASCEND-4): a randomised, open-label, phase 3 study.” The Lancet 389, no. 10072 (March 2017): 917–29. https://doi.org/10.1016/S0140-6736(17)30123-X.
Novartis Pharmaceuticals. A phase III, multicenter, randomized, open-label study of oral LDK378 versus standard chemotherapy in adult patients with ALK-rearranged (ALK-positive) advanced non-small cell lung cancer who have been treated previously with chemotherapy (platinum doublet) and crizotinib. Clinical trial registration. Clinicaltrials.gov, March 30, 2023. https://clinicaltrials.gov/ct2/show/NCT01828112.
Smith S, Albuquerque de Almeida F, Ines M, Iadeluca L, Cooper M. Matching-adjusted indirect treatment comparisons of the efect of lorlatinib versus chemotherapy on overall survival and progression-free survival for patients with second-line or later anaplastic lymphoma kinase-positive non-small-cell lung cancer. Presented at the International Society for Pharmacoeconomics and Outcomes Research—23rd Annual European Congress. 16–19 November 2020.
Pfizer. Phase 1 safety, pharmacokinetic and pharmacodynamic study of PF-02341066, a MET/HGFR selective tyrosine kinase inhibitor, administered orally to patients with advanced cancer. Clinical trial registration. Clinicaltrials.gov, January 10, 2023. https://clinicaltrials.gov/ct2/show/NCT00585195.
Drilon AE, Camidge DR, Ou S-HI, Clark JW, Socinski MA, Weiss J, Riely GJ, et al. Efficacy and safety of crizotinib in patients (pts) with advanced met exon 14-altered non-small cell lung cancer (NSCLC). J Clin Oncol. 2016;34(15):108–108. https://doi.org/10.1200/JCO.2016.34.15_suppl.108.
Pfizer. Phase 3, randomized, open-label study of the efficacy and safety of crizotinib versus pemetrexed/cisplatin or pemetrexed/carboplatin in previously untreated patients with non-squamous carcinoma of the lung harboring a translocation or inversion event involving the anaplastic lymphoma kinase (Alk) gene locus. Clinical trial registration. Clinicaltrials.gov, September 29, 2017. https://clinicaltrials.gov/ct2/show/NCT01154140.
Solomon, Benjamin J., Tony Mok, Dong-Wan Kim, Yi-Long Wu, Kazuhiko Nakagawa, Tarek Mekhail, Enriqueta Felip, et al. “First-Line Crizotinib versus Chemotherapy in ALK-Positive Lung Cancer.” New England Journal of Medicine 371, no. 23 (December 4, 2014): 2167–77. https://doi.org/10.1056/NEJMoa1408440.
Pfizer. Phase 3, randomized, open-label study of the efficacy and safety of crizotinib versus pemetrexed/cisplatin or pemetrexed/carboplatin in previously untreated east Asian patients with non-squamous carcinoma of the lung harboring a translocation or inversion event involving the anaplastic lymphoma kinase (ALK) gene locus. Clinical trial registration. Clinicaltrials.gov, November 16, 2020. https://clinicaltrials.gov/ct2/show/NCT01639001.
Wu Y-L, Lu S, Lu Y, Zhou J, Y-k Shi V, Sriuranpong JCMH, et al. Results of PROFILE 1029, a phase III comparison of first-line crizotinib versus chemotherapy in East Asian patients with ALK-positive advanced non-small cell lung cancer. J Thorac Oncol. 2018;13(10):1539–48. https://doi.org/10.1016/j.jtho.2018.06.012.
Xcovery Holding Company, LLC. Phase 3 randomized study comparing X-396 (ensartinib) to crizotinib in anaplastic lymphoma kinase (ALK) positive non-small cell lung cancer (NSCLC) patients. Clinical trial registration. Clinicaltrials.gov, February 7, 2023. https://clinicaltrials.gov/ct2/show/NCT02767804.
Pfizer. A phase 3, randomized, open-label study of lorlatinib (PF-06463922) monotherapy versus crizotinib monotherapy in the first-line treatment of patients with advanced ALK-positive non-small cell lung cancer. Clinical trial registration. clinicaltrials.gov, May 27, 2022. https://clinicaltrials.gov/ct2/show/NCT03052608.
Shaw AT, Bauer TM, de Marinis F, Felip E, Goto Y, Liu G, Mazieres J, et al. First-line lorlatinib or crizotinib in advanced ALK -positive lung cancer. N Engl J Med. 2020;383(21):2018–29. https://doi.org/10.1056/NEJMoa2027187.
Ma H-c, Liu Y-h, Ding K-l, Liu Y-f, Zhao W-j, Zhu Y-j, Chang X-s, et al. Comparative efficacy and safety of first-line treatments for advanced non-small cell lung cancer with ALK-rearranged: a meta-analysis of clinical trials. BMC Cancer. 2021;21:1278. https://doi.org/10.1186/s12885-021-08977-0.
Roche H-L. An open-label, non-randomized, multicenter phase I/II trial of RO5424802 given orally to non-small cell lung cancer patients who have ALK mutation and who have failed crizotinib treatment. Clinical trial registration. Clinicaltrials.gov, October 31, 2018. https://clinicaltrials.gov/ct2/show/NCT01801111.
Shaw AT, Gandhi L, Gadgeel S, Riely GJ, Cetnar J, West H, RossCamidge D, et al. Phase 2 prospective analysis of alectinib in ALK-positive, crizotinib-resistant non-small-cell lung cancer. Lancet Oncol. 2016;17(2):234–42. https://doi.org/10.1016/S1470-2045(15)00488-X.
Roche H-L. A phase I/II study of the ALK inhibitor CH5424802/RO5424802 in patients with ALK-rearranged non-small cell lung cancer previously treated with crizotinib. Clinical trial registration. Clinicaltrials.gov, July 23, 2018. https://clinicaltrials.gov/ct2/show/NCT01871805.
Sacher AG, Le LW, Lau A, Earle CC, Leighl NB. Real-world chemotherapy treatment patterns in metastatic non–small cell lung cancer: are patients undertreated? Cancer. 2015;121(15):2562–9. https://doi.org/10.1002/cncr.29386.
Chemotherapy in addition to supportive care improves survival in advanced non–small-cell lung cancer: a systematic review and meta-analysis of individual patient data from 16 randomized controlled trials. J Clin Oncol. 2008;26(28):4617–25. https://doi.org/10.1200/JCO.2008.17.7162.
Yu A, Huang E, Abe M, An K, Park S-K, Park C. Cost-effectiveness analyses of targeted therapy and immunotherapy for advanced non-small cell lung cancer in the United States: a systematic review. Expert Rev Pharmacoecon Outcomes Res. 2021;21(3):381–93. https://doi.org/10.1080/14737167.2021.1886928.
Haslam A, Lythgoe MP, Greenstreet Akman E, Prasad V. Characteristics of cost-effectiveness studies for oncology drugs approved in the United States from 2015–2020. JAMA Netw Open. 2021;4(11): e2135123. https://doi.org/10.1001/jamanetworkopen.2021.35123.
Roberts M, Russell LB, Paltiel AD, Chambers M, McEwan P, Krahn M. Conceptualizing a model: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force-2. Value Health. 2012;15(62012):804–11. https://doi.org/10.1016/j.jval.2012.06.016.
Novartis Pharmaceuticals. A multi-center, randomized open label study to assess the systemic exposure, efficacy, and safety of 450 mg ceritinib taken with a low-fat meal and 600 mg ceritinib taken with a low-fat meal as compared with that of 750 mg ceritinib taken in the fasted state in adult patients with ALK rearranged (ALK-positive) metastatic non-small cell lung cancer (NSCLC). Clinical trial registration. clinicaltrials.gov, February 7, 2022. https://clinicaltrials.gov/ct2/show/NCT02299505.
Kiefer C, Sturtz S, Bender R. Indirect comparisons and network meta-analyses. Dtsch Arztebl Int. 2015;112(47):803–8. https://doi.org/10.3238/arztebl.2015.0803.
Xie F, Zhou T. Industry sponsorship bias in cost effectiveness analysis: registry based analysis. BMJ. 2022;377: e069573. https://doi.org/10.1136/bmj-2021-069573.
Solomon, Benjamin J., Benjamin Besse, Todd M. Bauer, Enriqueta Felip, Ross A. Soo, D. Ross Camidge, Rita Chiari, et al. “Lorlatinib in Patients with ALK-Positive Non-Small-Cell Lung Cancer: Results from a Global Phase 2 Study.” The Lancet. Oncology 19, no. 12 (December 2018): 1654–67. https://doi.org/10.1016/S1470-2045(18)30649-1https://doi.org/10.1016/S1470-2045(18)30649-1.
Acknowledgements
The authors would like to thank the liaison and education librarian Ms. Glyneva Bradley-Ridout at the University of Toronto for her help and contribution to the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
LC is an employee of Hoffmann La-Roche, a pharmaceutical and diagnostics company. This systematic review is being conducted independent of LC’s place of employment. MT received consulting fees from CADTH and Green Shield Canada. NBL has received institutional grant funding from Amgen, Array, AstraZeneca, Bayer, BMS, Eli Lilly, EMD Serono, Guardant Health, Inivata, MSD, Novartis, Pfizer, Roche, and Takeda as well as honoraria for independent CME lectures from Amgen, BMS, EMD Serono, MSD, Novartis, Sanofi Genzyme, and Takeda.
Author contributions
Author 1: Lara Chayab: Conceived and designed the systematic review protocol (objective, research question, PICO, inclusion/exclusion criteria, and methodology); Conducted the systematic review including the search strategy, study selection, assessment of methodological quality, data extraction, analysis, synthesis, and presentation; Drafted the manuscript and revised manuscript on the basis of editor and reviewer comments; Approver of the final manuscript version to be published; Accountable to all aspects of the systematic review conduct and reporting. Author 2: Natalia Konstantelos: Provided substantial intellectual contribution to the systematic review methodology design and conduct; Conducted the systematic review alongside author 1 in the capacity of independent reviewer, including study selection, assessment of methodological quality, and data extraction; Provided critical revisions to the results section of the manuscript including data analysis and presentation as well as to the full manuscript, ensuring overall accuracy, consistency, and rigor; Assisted in addressing reviewer comments and helped revise manuscript prior to resubmission; Approver of the final manuscript version to be published; Accountable to all aspects of the systematic review conduct and reporting. Author 3: Natasha B. Leighl: Provided substantial intellectual contribution to the conception and design of the systematic review objective, research question, PICO, and inclusion/exclusion criteria from a clinical (medical oncologist) expert perspective; Provided critical revisions to the background, result interpretation, discussion, and relevance/conclusion of the manuscript; Assisted in addressing reviewer comments and provided input to revised manuscript prior to resubmission; Approver of the final manuscript version to be published; Accountable to all aspects of the systematic review conduct and reporting. Author 4: Mina Tadrous: Provided substantial intellectual contribution to the conception and design of the systematic review protocol (objective, research question, PICO, inclusion/exclusion criteria, and methodology) from a health services and outcomes research expert perspective; Provided critical revisions to the results’ presentation and interpretation, to the discussion, and to the conclusion sections of the manuscript, as well as to the full manuscript, ensuring overall accuracy, consistency, and rigor; Assisted in addressing reviewer comments and provided input to revised manuscript prior to resubmission; Approver of the final manuscript version to be published; Accountable to all aspects of the systematic review conduct and reporting. Author 5: In supervision, William W.L. Wong: Provided co-leadership (and oversight to) the conception and design of the systematic review protocol and study conduct together with author 1; Conducted the systematic review alongside author 1 and author 2 in the capacity of third reviewer, which required oversight of the study selection, assessment of methodological quality, and data extraction processes; Provided critical and intellectual revisions to the full manuscript, ensuring relevance, rigor, and integrity throughout with special focus on the abstract, methodology description, the results’ analysis, presentation, and interpretation, and the key points for decision makers; Assisted in addressing reviewer comments and helped revise manuscript prior to resubmission; Approver of the final manuscript version to be published; Accountable to all aspects of the systematic review conduct and reporting.
Funding
The team received no external funding for this study.
Data availability
The systematic review protocol is available in the International Prospective Register of systematic review, PROSPERO, under registration code CRD42022308680; https://www.crd.york.ac.uk/prospero/. Results of the search strategy are included in this published article (and its supplementary information files).
Code availability
Not applicable.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chayab, L., Konstantelos, N., Leighl, N.B. et al. A Systematic Review of the Cost-Effectiveness Analyses of Anaplastic Lymphoma Kinase (ALK) Inhibitors in Patients with Locally Advanced or Metastatic Non-small Cell Lung Cancer (NSCLC). PharmacoEconomics 41, 945–980 (2023). https://doi.org/10.1007/s40273-023-01279-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-023-01279-2