Abstract
Background
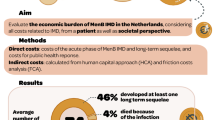
Invasive meningococcal disease remains a public health concern because of its rapid onset and significant risk of death and long-term disability. New meningococcal serogroup B and combination serogroup ACWY vaccines are being considered for publicly funded immunization programs in many countries. Contemporary costing data associated with invasive meningococcal disease are required to inform cost-effectiveness analyses.
Objective
The objective of this study was to estimate costs and resource utilization associated with acute infection and the long-term care of invasive meningococcal disease.
Data Sources and Methods
PubMed, EMBASE, The Cochrane Library, health economic databases, and electronically available conference abstracts were searched. Studies reporting any costs associated with acute infection and long-term sequelae of invasive meningococcal disease in English were included. All costs were converted into purchasing power parity-adjusted estimates [international dollars (I$)] using the Campbell and Cochrane Economics Methods Group and the Evidence for Policy and Practice Information and Coordinating Centre cost converter.
Results
Fourteen studies met our eligibility criteria and were included. The mean costs of acute admission ranged from I$1629 to I$50,796, with an incremental cost of I$16,378. The mean length of hospital stay was reported to be 6–18 days in multiple studies. The average costs reported for readmissions ranged from I$7905 to I$15,908. Key variables such as the presence of sequelae were associated with higher hospitalization costs and longer inpatient stay. No studies estimated direct non-healthcare costs and productivity loss. Ten studies reported only unadjusted mean values without using appropriate statistical methods for adjustment.
Conclusions
Invasive meningococcal disease can result in substantial costs to healthcare systems. However, costing data on long-term follow-up and indirect costs used to populate health economic models are lacking.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Invasive meningococcal disease (IMD) is a public health concern worldwide. Assumption and expert opinions have been commonly used in health economic evaluations to estimate unit costs associated with acute admission and long-term care of IMD. |
We systematically reviewed and synthesized published evidence of costs and resource utilization relevant to acute infection and long-term sequelae of IMD. The average healthcare costs of acute infection ranged from I$1629 in Colombia to I$50,796 in USA with an incremental cost of I$16,378. |
The public health burden of the disease is substantial with significant increases in healthcare costs and resource use for meningococcal patients with sequelae. |
1 Introduction
Although the incidence of invasive meningococcal disease (IMD) is relatively low in high-income countries, the disease still causes public health concern and anxiety because of its rapid onset, an increased risk of mortality in adolescents, and high rates of severe sequelae in children [1,2,3,4]. Results from retrospective and prospective studies show almost 40% of children had sequelae following IMD infection [2, 5]. Major disabling deficits including amputation, deafness, epilepsy, and learning difficulties were identified in around 10% of pediatric survivors [2]. Among 13 known serogroups, serogroups A, B, C, W, and Y are responsible for most cases of IMD with serogroup X mainly causing disease in Africa [6]. Vaccines against serogroup B disease (MenB), which causes around 40–85% of cases in Australia [7, 8], 64% of cases in Europe [9], and almost 50% in USA [10], have recently been developed. However, the MenB vaccination is publicly funded in a limited number of countries. The recommendation of funding the MenB vaccine under the National Immunisation Program Schedule in Australia has been rejected three times by the Pharmaceutical Benefits Advisory Committee, mainly owing to uncertainty around evidence on the effectiveness of the vaccine and potential for herd immunity response [11,12,13]. Although initially rejected in the UK [14], the Joint Committee on Vaccination and Immunisation (JCVI) finally recommended inclusion of the MenB vaccine into the UK immunization schedule at a ‘cost-effective’ price, which was significantly lower than the list price for the MenB vaccine [15]. Changes such as adding litigation costs to the final analysis supported the cost effectiveness of a MenB vaccination program in infants. The JCVI also noted that a similar model with key differences in a number of important parameters including healthcare resources could reach different conclusions on cost effectiveness when comparing an independent study with another unpublished cost-effectiveness study [14]. Because direct and indirect costs associated with acute treatment and long-term care in patients with IMD are important inputs into cost-effectiveness models, detailed costing data are required to inform cost-effectiveness analyses. The paucity of costing data and its potential impact on cost-effectiveness analyses have been acknowledged in recent economic evaluations of the MenB vaccine [16, 17].
By assessing the direct and indirect costs of a particular condition, the results of cost-of-illness (COI) studies can be used to inform public funding decisions such as estimating the magnitude of costs that can potentially be saved by preventative programs (e.g., MenB vaccination). Cost-of-illness studies have also been frequently cited to attract public attention to specific health problems by describing their impact on healthcare resources and productivity loss [18].
To our knowledge, no systematic reviews have been performed to estimate the financial impact associated with acute treatment and long-term follow up of IMD. Anonychuk et al. systematically reviewed the costs related to containment strategies for IMD outbreaks and concluded that the outbreaks result in substantial disruption and costs to society [19]. In a review article, Martinón-Torres delineated the extensive clinical and economic burden of IMD including the overlooked family burden, legal costs, and adaptive measures required for IMD survivors with disabilities [20]. However, this narrative review was based mainly on the author’s experience and knowledge, without a description of the literature searching methodology. This review article also used several costing studies related to all-cause bacterial meningitis including pneumococcal and other causes of meningitis to outline the financial burden of IMD.
The aim of the present study is to provide a systematic review of the global evidence on direct or indirect costs of IMD published since 2000. In addition, we compared methodologies used in each study and summarized the key factors affecting healthcare costs.
2 Methods
2.1 Literature Search
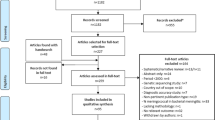
A search of the literature was conducted using the electronic databases: PubMed, EMBASE, The Cochrane Database of Systematic Reviews, The Cochrane Central Register of Controlled Trials, and the Database of Abstracts of Reviews of Effectiveness. The search terms included combinations of Medical Subject Headings/Emtree and text words contained in the title and abstract. Details on search strategies are presented in Table 1 of the Electronic Supplementary Material (ESM). Only studies reporting costing results are included in this review (Fig. 1). Health economic databases were also searched, including the Health Economic Evaluation Database, Cost-effectiveness Analysis Registry, Health Technology Assessment Database, and the Paediatric Economic Database Evaluation. Gray literature available online was searched for relevant abstracts and/or posters from the following organizations: Meningitis Research Foundation, Infectious Diseases Society of America, International Pathogenic Neisseria Conference, European Society for Paediatric Infectious Diseases, International Congress on Infectious Diseases, World Society for Pediatric Infectious Diseases, and the Australian Society for Infectious Diseases. If conference abstracts were eligible at the title and abstract screen, the first authors were contacted by e-mail and detailed study information was sought. The reference lists of eligible articles and other relevant review articles [19, 20] were searched for additional studies. The search was conducted by one reviewer (BW) from August 2016 to September 2017.
2.2 Inclusion and Exclusion Criteria
The article selection process occurred in two phases: (1) citation screen: titles and abstracts of articles identified from the electronic databases and from Internet searches were reviewed; and (2) full-text screen: the full text of articles selected at the citation screen were obtained and reviewed for eligibility. One reviewer (BW) completed the screening process according to a predefined protocol.
Studies were eligible if direct and/or indirect costs associated with acute infection and long-term complications/sequelae of IMD were reported through primary data collection. We excluded studies only recruiting patients with IMD as part of a larger population but not presenting outcomes for the IMD group separately. Comments, letters, editorials, case reports (fewer than ten patients with IMD), and reviews were excluded. Because the first national meningococcal vaccination (meningococcal C vaccines) program was implemented in the UK in 1999, we expected the vaccination could make significant changes to the epidemiology of IMD. Therefore, the search was restricted to studies published after January 2000. Studies reported in languages other than English were excluded.
Reporting and performing this review was guided by the Preferred Reporting Items for Systematic Reviews and Meta-analyses 2009 statement [21]. The inclusion and exclusion processes were documented.
2.3 Data Extraction and Quality Assessment
Data were independently extracted by two reviewers (BW and RS) using predefined data fields. Data extracted were: direct and indirect costs, and healthcare resource utilization [e.g., length of hospital stay (LOS), frequency of outpatient services and readmissions], study design, funding, study location, study population (e.g., sample size, serogroup, and age at illness), perspective, data sources, cost items, model type, time horizon, discount rates, cost adjustment approaches, sensitivity analysis, statistical methods, and limitations considered by authors.
As there are no consensus agreement or validated guidelines explicitly designed to perform critical appraisal for the COI studies, the quality of included studies was assessed using a checklist (Table 2 of the ESM), which was developed on the basis of the Drummond 10-point Checklist [22], the International Society For Pharmacoeconomics and Outcomes Research checklist for retrospective database studies [23], and criteria used in previous COI systematic reviews [24,25,26,27,28]. Two independent reviewers (BW and RS) assessed the quality of the studies and any divergences between reviewers were resolved by discussion.
No studies fulfilled all criteria, as most studies were only conducted from the healthcare system or third-party payer perspective without covering all relevant perspectives, used national hospital discharge or insurance claim databases with no description of data reliability and validity, or reported mean values with no adjustment for confounding variables.
2.4 Data Synthesis
To compare costing data across heterogeneous studies, all cost estimates were converted into international dollars using purchasing power parity according to the recommended guideline [22] and similar studies in the literature [29,30,31]. Henceforth, all cost estimates are presented with the sign of I$. The purchasing power parity-adjusted estimates were calculated using the Campbell and Cochrane Economics Methods Group and the Evidence for Policy and Practice Information and Coordinating Centre cost converter [32]. Because the Campbell and Cochrane Economics Methods Group and the Evidence for Policy and Practice Information and Coordinating Centre cost converter requires cost estimates reported in the original study’s local currency for inflation adjustment, the cost estimates were converted back into the local currency for studies not reporting their results in the study country’s local currency but in US$. If the exchange rate was not presented in the article, the average exchange rate (according to OANDA historical exchange rates [33]) for the reported year was used. If the price year was not specified in the publication, the last year of the study period was utilized. All costs were adjusted to the year 2014, as that was the last price year reported in the included studies.
A meta-analysis was performed using the metaan ado package [34] in STATA 14.2 (StataCorp LLC., College Station, TX, USA) [35]. Owing to marked variation in data sources, age group, follow-up period, cost items, statistical methods, and confounder adjustment across studies, a significantly high level of heterogeneity (I2 = 96.61%, τ2 = 4.6 × 108) was found in the pooled estimate of unadjusted acute admission costs. Owing to the considerable heterogeneity demonstrated in the meta-analysis, only descriptive results are presented here.
3 Results
3.1 Overview of Studies
The search strategy identified 2370 studies that met the inclusion criteria (Fig. 1). After title and abstract screening, full manuscripts of 326 articles were reviewed so as to exclude additional articles. Among 115 articles retained to assess the clinical and financial burden of IMD, 14 articles reported costing results (Table 1). The majority of the studies were conducted in high-income countries, including six studies in USA, two in Spain, one in Belgium, one in Italy, and another study in Australia. Three studies reported costs associated with IMD outbreaks in the UK, Colombia, and Brazil.
3.2 Methodological Heterogeneity
Although all studies were conducted from the perspective of the healthcare system or third-party payers with a bottom-up approach, the range of cost items included in each study varied considerably (Table 2). Except for three outbreak studies, all other studies used retrospective insurance claim or hospital discharge databases. Five studies did not provide detailed cost breakdowns with three of them reporting costs based on Diagnosis Related Group codes [36, 38, 41, 45, 48]. Five studies provided a breakdown of healthcare costs by age groups. The main cost item reported was inpatient costs. Some studies also included other cost components such as emergency department, hospital outpatient services, physician office visits, nursing home services and rehabilitation facilities, pharmacy claims, and associated costs. Cost adjustment was not documented in three studies [36, 41, 45]. One study compared costing data and resource utilization between cases and controls [38]. Four studies reported healthcare costs relevant to medical follow-up after hospital discharge [39, 40, 43, 49]. The follow-up period varied between 0 and 3659 days. Serogroup information was only available for six studies.
Only four studies used statistical models to adjust cost and resource utilization data [38, 39, 43, 49]. Among those, a generalized linear model was commonly used for costing data adjustment, with three studies fitting a generalized linear model with a log link function and a gamma distribution. Resource utilization was analyzed using negative binomial regression, Cox proportional hazard, or Poisson regression models. Two studies chose the same set of confounding variables [39, 43]. There is considerable variability in selecting confounding variables between the aforementioned two studies and other studies. Both unadjusted and adjusted analyses were presented in three studies [39, 43, 49]. Except for patients without sequelae in two US studies, all adjusted costs were reported to be lower than unadjusted costs. For those performing only unadjusted analyses, four of them presented mean and/or median values with no variability measures (e.g., range, interquartile range, 95% confidence interval or standard deviation) [40, 41, 45, 46].
3.3 Direct Medical Cost Estimates and Healthcare Resource Utilization
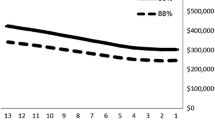
The unadjusted acute admission costs per patient ranged from I$1629 in Colombia [47] to I$50,796 in USA [39] (Tables 3, 4). The unadjusted mean cost of follow-up care during 1-year post-admission was reported as I$23,565 in USA including readmission costs and other healthcare expenses [40]. The unadjusted total healthcare cost for initial admission, readmissions, and other healthcare services was around I$60,000 on average in USA during 1-year post-admission [39, 40, 43]. Readmissions resulted in I$15,908 in USA [40] and I$7905 in Australia [49] in unadjusted analyses with varied follow-up periods. The adjusted mean costs associated with acute admission were reported in four studies ranging from I$8571 in Australia [49] to I$23,792 in USA [38]. The adjusted mean cost relevant to IMD readmissions was estimated to be I$935 in Australian pediatric patients with sequelae [49]. Both unadjusted and adjusted healthcare costs including inpatient costs almost doubled in patients with sequelae compared with patients without sequelae [38, 43, 49]. The incremental cost and LOS of acute admission (I$16,378, 4.3 days) could only be inferred from a case-control study [38].
Of the 14 included studies, ten reported an estimated hospital resource use. The mean LOS during acute admission was reported from 8 to 18 days in unadjusted analyses with around 1 week in adjusted analyses. Approximately 40% of patients with IMD had sequelae after discharging from hospital. Those patients were 1.5–3 times more likely to stay in hospital longer and visit outpatient clinics during the acute admission and/or in the year following admission [39, 43, 49].
The total cost associated with an outbreak was reported as I$55,778 in Brazil and I$7873 in Colombia [37] (Table 4). As MenB vaccines were not available for the outbreak in Colombia, the cost of managing the outbreak was lower in Colombia than the one in Brazil. It was reported in the UK study that the incremental cost of managing a second case of IMD was I$7815 [44].
3.4 Direct Non-medical Costs and Indirect Costs
We have not found any studies reporting direct non-medical costs and indirect costs relevant to IMD. We excluded studies that estimated productivity loss based on assumption or expert opinions without any primary data collection.
3.5 Factors Impacting Healthcare Costs
Studies in USA and Australia suggested sequelae/complications, serogroup B infection, male sex, and previous medical history were significantly associated with higher healthcare costs and resource use compared with their counterparts [5, 38, 39, 43]. Infants aged less than 1 year had the highest healthcare costs and LOS in pediatric patients and young patients aged < 21 years [38, 49]. However, unadjusted mean costs or LOS reported in other studies did not show a similar trend. In contrast, adolescents or adults were reported as having higher costs and longer LOS than other age groups [41, 42, 45, 46, 48].
4 Discussion
This systematic review included 14 studies that reported costs associated with acute infection and/or long-term care of patients with IMD, and descriptively described and compared study results and methodologies. To our knowledge, this is the first study to systematically review and investigate the financial impact of IMD.
The results show a considerable impact of IMD on healthcare resources, which reflects severe outcomes associated with the disease requiring resource-intensive treatments. The costs of acute treatment and readmissions were the most important components of total healthcare costs. The national costs per year were estimated to be around €5 million in Spain [41, 45] and US$50 million in USA [40, 46]. Although total costs of controlling IMD outbreaks are not significant in Brazil and Colombia, the management of outbreaks cost 2.7 times more than the annual gross domestic product per capita in Brazil including vaccination costs and 9.5% of Colombia’s annual gross domestic product per capita without using any vaccination [37].
The financial impact of long-term sequelae on the healthcare system has not been well investigated. The included studies consistently reported that the presence of sequelae is an important predictor of high healthcare costs and resource use. Clinical data show that around 10% of patients with IMD had severe long-term sequelae such as amputation, skin scarring, or neurological disabilities [1, 2, 5]. However, most patients were only followed up until discharge, and costs for other healthcare services such as rehabilitation associated with long-term care were not included. Studies in USA followed patients up to 12 months post-discharge [39, 43] and one study in Australia assessed readmission costs in one tertiary pediatric hospital [49]. Including costs relevant to care and clinical management of long-term sequelae may lead to substantially higher cost estimates. A few case studies show that the discounted lifetime cost associated with severe long-term sequelae could be more than €1 million. However, those severe IMD cases were developed on the basis of expert opinions and interviews with patients and their families [50,51,52]. Future studies are warranted to investigate the longer term financial burden imposed on the healthcare system, patients, their families, and society as well as the negative effect on economically meaningful health outcomes (e.g., quality of life) [53, 54]. The cost and quality of life are key inputs into health economic evaluation, and therefore reliable data on the costs of long-term care would be valuable in reducing parameter uncertainty.
Undertaking studies to follow patients with IMD over a long period of time (e.g., lifetime) could be time and resource consuming. It might be problematic to link different administrative, costing, and clinical databases, as researchers would need to follow ethics, privacy, and legal guidelines and fulfill local and national requirements. Because the incidence rate of IMD peaks in infants [55], those infant survivors with neurological sequelae and motor deficits would need multiple hospital readmissions, special education, and long-term carers. The time frame of follow-up is a critical point to consider. For example, following adult patients until their conditions stabilize may only take 2 years. It may take at least 3–5 years to confirm diagnoses of permanent neurological and psychological sequelae in infant survivors. Given the previous literature indicating that around 20–40% of IMD survivors had multiple sequelae following IMD [1, 56], determining the long-term effect of each single sequela separately could be very difficult. The cost associated with individual sequela has been used to develop decision analytical models to assess the cost effectiveness of meningococcal vaccines. Those parameters were determined mainly on the basis of data collected for similar medical conditions, assumptions, or expert opinions [42, 48, 57, 58].
The impact of the disease on individuals and the community has been widely discussed and considered substantial [19, 20], but we have not found any studies reporting data associated with direct non-healthcare costs and indirect costs. The financial burden of the disease estimated in our review was relatively conservative, as third-party payers were the only perspective taken by the included studies. The measurement of reduced employment, absenteeism, presenteeism, and productivity loss associated with informal carers is controversial [59]. In a small number of cost-effectiveness studies taking the societal perspective, the productivity costs were based on assumptions or average national employment data [57, 58, 60].
Our review found that around one third of included studies reported costing results by serogroup [37, 42, 44, 47, 49]. One study compared serogroup B with non-B and reported serogroup B disease was likely to result in the highest costs to the healthcare system in pediatric patients [49]. Clinical literature indicated serogroup C disease was associated with high rates of morbidity and mortality [1, 61]. The serogroup may be an important factor in predicting the disease severity and hence healthcare expenditures. Cost-of-illness analyses should reflect the epidemiology of the disease and variations in serogroup distribution in relation to time period and geographical region. Serogroup comparison may be necessary to consider in COI analyses to support cost-effectiveness evaluations assessing vaccines against certain serogroups. Because of the limited number of COI studies examining the effect of serogroups on healthcare costs, some cost-effectiveness studies used the average acute admission cost for all IMD cases derived from International Classification of Diseases codes [48, 62]. Several studies estimated the average acute hospitalization cost based on Diagnosis Related Group costs associated with meningococcal diagnosis [57, 58].
Although the new MenB vaccines are protein based, the preliminary results obtained from studies evaluating the impact of meningococcal vaccines on disease carriage prevalence show that MenB vaccines could potentially offer a certain level of protection against non-B serogroup disease [63]. All MenB vaccines are licensed to provide protection against serogroup B disease only. Serogroup-specific COI analyses may still be warranted to provide useful information on disease burden for cost-effectiveness evaluations. Pentavalent vaccines that protect against five serogroups (A, B, C, W, and Y) causing the majority of IMD are currently in phase III clinical trials. It may be less important to compare and evaluate healthcare resource use by serogroup in a decade.
Invasive meningococcal disease has become uncommon especially in industrialized countries, which may be owing to vaccine pressure, a reduction in smoking, or natural fluctuations of disease incidence [55]. However, outbreaks of IMD continue to occur in schools and universities [64, 65]. Surveillance networks have closely monitored capsule switching and capsule replacement after implementing meningococcal vaccination programs. The impact of the new protein-based MenB vaccines on clearing carriage and interrupting transmission in adolescents remains unclear. It is too early to envisage eradication of the meningococcus bacteria at the current stage, when most developing countries have not implemented meningococcal vaccine programs because of the high costs of vaccines [66]. Although inclusion of the MenB vaccine on the government-funded National Immunisation Program was rejected by the Pharmaceutical Benefits Advisory Committee in Australia, the Australian Technical Advisory Group on Immunisation provided clinical advice to the Pharmaceutical Benefits Advisory Committee and recommended routine MenB vaccination of infants, young children, and adolescents owing to their higher risk of MenB infection [11, 67]. The COI analyses would still be required to inform a cost-effectiveness review of a new submission or resubmission to national decision-making bodies for publicly funding new meningococcal vaccines. However, we acknowledge that the evaluation of the true costs of IMD may be more challenging in the future because of a reduced number of patients infected with IMD.
The incremental cost-effectiveness ratios derived from the estimate of costs and quality-adjusted life-years are one of the key inputs to inform public funding decisions in countries such as the UK and Australia. An evaluation of IMD vaccines by national funding bodies in Australia and the UK found that the results of economic evaluations of meningococcal prevention strategies were, among others, highly sensitive to herd immunity and vaccine effectiveness [12, 15]. After considering new evidence in 2014, the JCVI recommended the MenB vaccine for inclusion on the UK national immunization program with a reduced dose schedule at a very low price of £7 per dose based on the revised analysis [16]. Including litigation costs associated with the disease, updating cost data relevant to long-term care, and using a quality-of-life adjustment factor affected the outcome of a cost-effectiveness analysis in the UK [15]. With very limited COI analyses conducted for this severe but uncommon disease, there may be a risk of underestimating the true disease burden. The results of model-based evaluations are subject to a significant level of parameter uncertainty as emphasized by the Global Meningococcal Initiative [68]. Because of considerable uncertainty around the duration of protection against IMD and potential for reduction in the carriage in adolescents, the JCVI rejected the inclusion of the routine MenB vaccine schedule in adolescents. If the true value of COI is ultimately shown to be high enough, for example, considering all important direct and societal costs, it may be argued that this could potentially offset the significance of indirect protective effects/herd immunity that play an important role in determining the cost effectiveness of new meningococcal vaccine programs.
Therefore, comprehensive COI analyses could provide important inputs into economic evaluations of meningococcal vaccines to better inform public funding decisions. It is worth noting that individuals, charity organizations, and clinicians strongly criticized the JCVI’s initial rejection and called for re-evaluation of the vaccine program. Subsequently, the JCVI reviewed and revised the analysis that included more favorable assumptions, optimized parameters, and additional costs associated with the disease, thereby amending its interim position [69]. Economic evidence is only one of several inputs into decision making. Guidelines developed by decision-making bodies in countries such as Australia and Canada recommend considering less-readily quantifiable factors for health technology funding decisions [70, 71]. In Australia, for example, national funding bodies consider factors such as severity and rapid onset of the condition under study, the age at which a person with the condition might die, and rarity of the condition. Such societal values are all relevant to IMD and hence should be considered in evaluating IMD-related vaccines. However, as reported by Drew et al., there is a lack of transparency and consistency in defining and integrating these values into decision making [72].
The quality and methodologies varied significantly between studies. Although we converted costs from original studies to international dollars, extremely high heterogeneity including differences in the treated population, study design, cost items, or data analysis hinders direct comparison between studies, which may also explain the conflicting results of inpatient costs and healthcare resource use in infants. The included studies used insurance claims, hospital charges, or payments to estimate costs that may not represent the same ‘market value’ between studies. Only four out of 14 studies reported adjusted mean values using a regression model to adjust for confounding factors including sociodemographic characteristics, disease outcomes, comorbidities, and/or medical history. Differences between unadjusted and adjusted mean values were apparent within the same study, reflecting the importance of consideration of potential confounders in any analyses.
It is of concern that overlooking the nature of highly skewed costing data and not using any appropriate statistical models to deal with skewness and adjusting for potential confounders could lead to biased results [18, 26, 73]. Among those studies presenting only unadjusted results, four studies reported average costs and/or LOS without any variability measures. Incremental costs are commonly recommended for health economic analyses and have been frequently reported in the COI studies of other diseases [26, 28, 74]. The incremental costs were only reported in one included study through a comparison of patients with IMD with matched controls.
We understand various methodologies are used to generate estimates in the COI studies to serve different purposes [75]. However, this variation in study conduct may also reflect a lack of guidelines to standardize COI study designs and methodologies [76]. A review of COI studies highlighted the need for standardized methods of cost calculation, mathematical modeling, choice of cost components, disease classification, and selection of study perspective [77]. The findings of COI studies are often used to support funding decisions and attract public attention. Developing and implementing best-practice recommendations will improve the comparability and generalizability of the costing studies.
As some studies enrolled patients with meningitis caused by a range of bacteria, including Haemophilus influenzae type B, Neisseria meningitides, and Streptococcus pneumoniae, we were unable to separate the costs for patients with meningococcal meningitis from those with other bacterial meningitis. We excluded studies describing the financial burden of meningitis during epidemics of serogroup A meningococcal disease in the meningitis belt of sub-Saharan Africa because those studies did not report costs associated with meningococcal meningitis specifically. Because the authors’ first language is English and not all languages were included, there may be important studies not included in this review, resulting in regional or English-language bias.
5 Conclusions
Despite the variability in estimates of medical costs and hospital resource use, all included studies concluded IMD resulted in substantial costs to healthcare systems or third-party payers. The public concerns and fears caused by IMD have been frequently reported. However, few have implemented appropriate research methods, for example, using micro-costing methodology and collecting primary data prospectively from the societal perspective [22], to investigate the true costs of the disease. This systematic review provides important information for the selection of an appropriate unit cost for future cost-effectiveness studies, identifying the financial burden of the disease in prioritizing healthcare policies, and estimating potential cost savings accrued from the introduction of new vaccines, and also reinforces the need to standardize methodology and improve the quality of the COI studies.
Data Availability Statement
The full dataset including data extracted from the full-text review and quality assessment results that support the findings of this study are available from the corresponding author upon request. The authors declare that all other data supporting the findings of this study are available within the article and its supplementary information files.
References
Bettinger JA, Scheifele DW, Le Saux N, Halperin SA, Vaudry W, Tsang R, et al. The disease burden of invasive meningococcal serogroup B disease in Canada. Pediatr Infect Dis J. 2013;32(1):e20–5.
Viner RM, Booy R, Johnson H, Edmunds WJ, Hudson L, Bedford H, et al. Outcomes of invasive meningococcal serogroup B disease in children and adolescents (MOSAIC): a case-control study. Lancet Neurol. 2012;11(9):774–83.
Edge C, Waight P, Ribeiro S, Borrow R, Ramsay M, Ladhani SN. Clinical diagnoses and outcomes of 4,619 hospitalised cases of laboratory-confirmed invasive meningococcal disease in England: linkage analysis of multiple national databases. J Infect. 2016;73(5):427–36.
Nadel S. Prospects for eradication of meningococcal disease. Arch Dis Child. 2012;97(11):993–8.
Wang B, Clarke M, Thomas N, Howell S, Afzali HH, Marshall H. The clinical burden and predictors of sequelae following invasive meningococcal disease in Australian children. Pediatr Infect Dis J. 2014;33(3):316–8.
Harrison LH, Trotter CL, Ramsay ME. Global epidemiology of meningococcal disease. Vaccine. 2009;24(27 Suppl. 2):B51–63.
Department of Health Australian Government. Invasive meningococcal disease: national surveillance report, with a focus on MenW, December 2016 [updated 13 Oct 2017]. https://acpc.gov.au/internet/main/publishing.nsf/Content/5FEABC4B495BDEC1CA25807D001327FA/$File/IMD-Surveillance-report20161212.pdf. Accessed 31 May 2018.
Lahra MM, Enriquez RP. Australian meningococcal surveillance programme annual report, 2015. Commun Dis Intell Q Rep. 2016;40(4):E503–11.
European Centre for Disease Prevention and Control. Annual epidemiological report 2016: invasive meningococcal disease (2014 data). Stockholm: ECDC; 2016. https://ecdc.europa.eu/en/publications-data/invasive-meningococcal-disease-annual-epidemiological-report-2016-2014-data. Accessed 25 Jul 2017.
National Center for Immunization and Respiratory Diseases. Enhanced meningococcal disease surveillance report, 2015 [updated 9 June 2017]. https://www.cdc.gov/meningococcal/downloads/NCIRD-EMS-Report.pdf. Accessed 25 Jul 2017.
Pharmaceutical Benefits Advisory Committee. Multicomponent meningococcal group B vaccine, 0.5 mL, injection, prefilled syringe, Bexsero®: July 2015. Pharmaceutical Benefits Scheme; 2014. http://www.pbs.gov.au/pbs/industry/listing/elements/pbac-meetings/psd/2015-07/mulit-component-meningococcal-group-b-vaccine-psd-july-2015. Accessed 25 Jul 2017.
Pharmaceutical Benefits Advisory Committee. Multicomponent meningococcal group B vaccine, 0.5 mL, injection, prefilled syringe, Bexsero®: July 2014. Pharmaceutical Benefits Scheme; 2014. http://www.pbs.gov.au/pbs/industry/listing/elements/pbac-meetings/psd/2014-07/meningococcal-vaccine-psd-07-2014. Accessed 25 Jul 2017.
Pharmaceutical Benefits Advisory Committee. Multicomponent meningococcal group B vaccine, 0.5 mL, injection, prefilled syringe, Bexsero®: November 2013. Pharmaceutical Benefits Scheme; 2013. http://www.pbs.gov.au/info/industry/listing/elements/pbac-meetings/psd/2013-11/meningococcal-vaccine. Accessed 25 Jul 2017.
Joint Committee on Vaccination and Immunisation (JCVI). JCVI interim position statement on use of Bexsero® meningococcal B vaccine in the UK 2013 [updated July 2013]. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/224896/JCVI_interim_statement_on_meningococcal_B_vaccination_for_web.pdf. Accessed 25 Jul 2017.
Joint Committee on Vaccination and Immunisation (JCVI). JCVI position statement on use of Bexsero® meningococcal B vaccine in the UK 2014 [updated 21 March 2014]. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/252859/JCVI_MenB_Update.pdf. Accessed 5 Sep 2017.
Christensen H, Trotter CL, Hickman M, Edmunds WJ. Re-evaluating cost effectiveness of universal meningitis vaccination (Bexsero) in England: modelling study. BMJ. 2014;349:g5725.
Tu HA, Deeks SL, Morris SK, Strifler L, Crowcroft N, Jamieson FB, et al. Economic evaluation of meningococcal serogroup B childhood vaccination in Ontario, Canada. Vaccine. 2014;32(42):5436–46.
Larg A, Moss JR. Cost-of-illness studies: a guide to critical evaluation. Pharmacoeconomics. 2011;29(8):653–71.
Anonychuk A, Woo G, Vyse A, Demarteau N, Tricco AC. The cost and public health burden of invasive meningococcal disease outbreaks: a systematic review. Pharmacoeconomics. 2013;31(7):563–76.
Martinon-Torres F. Deciphering the burden of meningococcal disease: conventional and under-recognized elements. J Adolesc Health. 2016;59(2 Suppl.):S12–20.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;21(339):b2700.
Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 2015.
Motheral B, Brooks J, Clark MA, Crown WH, Davey P, Hutchins D, et al. A checklist for retrospective database studies: report of the ISPOR Task Force on Retrospective Databases. Value Health. 2003;6(2):90–7.
Kleine-Budde K, Touil E, Moock J, Bramesfeld A, Kawohl W, Rossler W. Cost of illness for bipolar disorder: a systematic review of the economic burden. Bipolar Disord. 2014;16(4):337–53.
Ernstsson O, Gyllensten H, Alexanderson K, Tinghog P, Friberg E, Norlund A. Cost of illness of multiple sclerosis: a systematic review. PLoS One. 2016;11(7):e0159129.
Kim DD, Basu A. Estimating the medical care costs of obesity in the United States: systematic review, meta-analysis, and empirical analysis. Value Health. 2016;19(5):602–13.
Jarbrink K, Ni G, Sonnergren H, Schmidtchen A, Pang C, Bajpai R, et al. The humanistic and economic burden of chronic wounds: a protocol for a systematic review. Syst Rev. 2017;6(1):15.
Budhia S, Mikyas Y, Tang M, Badamgarav E. Osteoporotic fractures: a systematic review of U.S. healthcare costs and resource utilization. Pharmacoeconomics. 2012;30(2):147–70.
Seuring T, Archangelidi O, Suhrcke M. The economic costs of type 2 diabetes: a global systematic review. Pharmacoeconomics. 2015;33(8):811–31.
Wodchis WP, Bhatia RS, Leblanc K, Meshkat N, Morra D. A review of the cost of atrial fibrillation. Value Health. 2012;15(2):240–8.
Bahia L, Toscano CM, Takemoto ML, Araujo DV. Systematic review of pneumococcal disease costs and productivity loss studies in Latin America and the Caribbean. Vaccine. 2013;2(31 Suppl. 3):C33–44.
Shemilt I, Thomas J, Morciano M. A web-based tool for adjusting costs to a specific target currency and price year. Evid Policy. 2010;6(1):51–9.
OANDA. Historical exchange rates 2018 [cited 23 April 2018]. https://www.oanda.com/fx-for-business/historical-rates. Accessed 31 May 2018.
Kontopantelis E, Reeves D. metaan: random-effects meta-analysis. Stata J. 2010;10(3):395.
StataCorp. Stata statistical software: release 14. College Station: StataCorp LP; 2015.
Clarke C, Mallonee S. State-based surveillance to determine trends in meningococcal disease. Public Health Rep. 2009;124(2):280–7.
Constenla D, Carvalho A, Alvis Guzman N. Economic impact of meningococcal outbreaks in Brazil and Colombia. Open Forum Infect Dis. 2015;2(4):ofv167.
Davis KL, Bell TJ, Miller JM, Misurski DA, Bapat B. Hospital costs, length of stay and mortality associated with childhood, adolescent and young adult meningococcal disease in the US. Appl Health Econ Health Policy. 2011;9(3):197–207.
Davis KL, Misurski D, Miller J, Karve S. Cost impact of complications in meningococcal disease: evidence from a United States managed care population. Hum Vaccin. 2011;7(4):458–65.
Davis KL, Misurski D, Miller JM, Bell TJ, Bapat B. Cost of acute hospitalization and post-discharge follow-up care for meningococcal disease in the US. Hum Vaccin. 2011;7(1):96–101.
Gil-Prieto R, Garcia-Garcia L, Alvaro-Meca A, Gonzalez-Escalada A, Viguera Ester P, Gil De Miguel A. The burden of hospitalizations for meningococcal infection in Spain (1997–2008). Vaccine. 2011;29(34):5765–70.
Hanquet GC, Agnew E, Trotter CL, Robays J, Dubois, Devriese S, et al. A quadrivalent vaccine against serogroup B meningococcal disease: a cost-effectiveness study. Health technology assessment (HTA). 2014; KCE reports 231.
Karve S, Misurski D, Miller J, Davis KL. Costs of sequelae associated with invasive meningococcal disease: findings from a US managed care population. Health Outcomes Res Med. 2011;2(4):e215–26.
Letouze D, Yao G, Clarke SC. The costs associated with the public health management of a cluster of meningococcal infection in England. Vaccine. 2014;32(43):5549–51.
Montero JM, Prieto RG, Alejandre CG, Meca LA, Portugal P, de Miguel AG. Hospital admissions for meningococcal infection in Spain (1997–2005). J Infect. 2009;58(1):15–20.
O’Brien JA, Caro JJ, Getsios D. Managing meningococcal disease in the United States: hospital case characteristics and costs by age. Value Health. 2006;9(4):236–43.
Pinzon-Redondo H, Coronell-Rodriguez W, Diaz-Martinez I, Guzman-Corena A, Constenla D, Alvis-Guzman N. Estimating costs associated with a community outbreak of meningococcal disease in a colombian Caribbean city. J Health Popul Nutr. 2014;32(3):539–48.
Tirani M, Meregaglia M, Melegaro A. Health and economic outcomes of introducing the new MenB vaccine (Bexsero) into the Italian routine infant immunisation programme. PLoS One. 2015;10(4):e0123383.
Wang B, Haji Ali Afzali H, Marshall H. The inpatient costs and hospital service use associated with invasive meningococcal disease in South Australian children. Vaccine. 2014;32(37):4791–8.
Benard S, Wright C, Voisine J, Olivier CW, Gaudelus J. Lifetime cost of meningococcal disease in France: scenarios of severe meningitis and septicemia with purpura fulminans. J Infect Public Health. 2016;9(3):339–47.
Darba J, Kaskens L, Hark M, Wright C. Costs of surviving meningococcal disease in Spain: evaluation for two cases of severe meningitis and septicaemia. Vaccine. 2014;32(39):5006–12.
Wright C, Wordsworth R, Glennie L. Counting the cost of meningococcal disease: scenarios of severe meningitis and septicemia. Paediatr Drugs. 2013;15(1):49–58.
Kennedy ITR, van Hoek AJ, Ribeiro S, Christensen H, Edmunds WJ, Ramsay ME, et al. Short-term changes in the health state of children with group B meningococcal disease: a prospective, national cohort study. PLoS One. 2017;12(5):e0177082.
Vyse A, Anonychuk A, Jakel A, Wieffer H, Nadel S. The burden and impact of severe and long-term sequelae of meningococcal disease. Expert Rev Anti Infect Ther. 2013;11(6):597–604.
Pelton SI. The global evolution of meningococcal epidemiology following the introduction of meningococcal vaccines. J Adolesc Health. 2016;59(2 Suppl.):S3–11.
Sadarangani M, Scheifele DW, Halperin SA, Vaudry W, Le Saux N, Tsang R, et al. Outcomes of invasive meningococcal disease in adults and children in Canada between 2002 and 2011: a prospective cohort study. Clin Infect Dis. 2015;60(8):e27–35.
Christensen H, Irving T, Koch J, Trotter CL, Ultsch B, Weidemann F, et al. Epidemiological impact and cost-effectiveness of universal vaccination with Bexsero® to reduce meningococcal group B disease in Germany. Vaccine. 2016;34(29):3412–9.
Gasparini R, Landa P, Amicizia D, Icardi G, Ricciardi W, de Waure C, et al. Vaccinating Italian infants with a new multicomponent vaccine (Bexsero®) against meningococcal B disease: a cost-effectiveness analysis. Hum Vaccin Immunother. 2016;12(8):2148–61.
Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 2015. p. 245–50.
Hepkema H, Pouwels KB, van der Ende A, Westra TA, Postma MJ. Meningococcal serogroup A, C, W(1)(3)(5) and Y conjugated vaccine: a cost-effectiveness analysis in the Netherlands. PLoS One. 2013;8(5):e65036.
Erickson L, De Wals P. Complications and sequelae of meningococcal disease in Quebec, Canada, 1990–1994. Rev Infect Dis. 1998;26(5):1159–64.
Lecocq H, Parent du Chatelet I, Taha MK, Levy-Bruhl D, Dervaux B. Epidemiological impact and cost-effectiveness of introducing vaccination against serogroup B meningococcal disease in France. Vaccine. 2016;34(19):2240–50.
Balmer P, Burman C, Serra L, York LJ. Impact of meningococcal vaccination on carriage and disease transmission: a review of the literature. Hum Vaccin Immunother. 2018. https://doi.org/10.1080/21645515.2018.1454570 (Epub ahead of print).
Breakwell L, Whaley M, Khan UI, Bandy U, Alexander-Scott N, Dupont L, et al. Meningococcal carriage among a university student population: United States, 2015. Vaccine. 2018;36(1):29–35.
McNamara LA, Thomas JD, MacNeil J, Chang HY, Day M, Fisher E, et al. Meningococcal carriage following a vaccination campaign with MenB-4C and MenB-FHbp in response to a university serogroup B meningococcal disease outbreak: Oregon, 2015–2016. J Infect Dis. 2017;216(9):1130–40.
Shaker R, Fayad D, Dbaibo G. Challenges and opportunities for meningococcal vaccination in the developing world. Hum Vaccin Immunother. 2018. https://doi.org/10.1080/21645515.2018.1434463 (Epub ahead of print).
Australian Technical Advisory Group on Immunisation. The Australian immunisation handbook. 10th ed. Canberra: Australian Government Department of Health; 2015 (2015 update).
Borrow R, Alarcon P, Carlos J, Caugant DA, Christensen H, Debbag R, et al. The Global Meningococcal Initiative: global epidemiology, the impact of vaccines on meningococcal disease and the importance of herd protection. Expert Rev Vaccines. 2017;16(4):313–28.
Timmis JK, Black S, Rappuoli R. Improving accountability in vaccine decision-making. Expert Rev Vaccines. 2017;16(11):1057–66.
Committee Pharmaceutical Benefits Advisory. Guidelines for preparing submissions to the Pharmaceutical Benefits Advisory Committee (version 5.0). Canberra: Australian Government Department of Health and Ageing; 2016.
Erickson LJ, De Wals P, Farand L. An analytical framework for immunization programs in Canada. Vaccine. 2005;23(19):2470–6.
Carter D, Vogan A, Haji Ali Afzali H. Governments need better guidance to maximise value for money: the case of Australia’s Pharmaceutical Benefits Advisory Committee. Appl Health Econ Health Policy. 2016;14(4):401–7.
Mihaylova B, Briggs A, O’Hagan A, Thompson SG. Review of statistical methods for analysing healthcare resources and costs. Health Econ. 2011;20(8):897–916.
Desmedt M, Vertriest S, Hellings J, Bergs J, Dessers E, Vankrunkelsven P, et al. Economic impact of integrated care models for patients with chronic diseases: a systematic review. Value Health. 2016;19(6):892–902.
Jo C. Cost-of-illness studies: concepts, scopes, and methods. Clin Mol Hepatol. 2014;20(4):327–37.
Jacobs P, Ohinmaa A, Brady B. Providing systematic guidance in pharmacoeconomic guidelines for analysing costs. Pharmacoeconomics. 2005;23(2):143–53.
Onukwugha E, McRae J, Kravetz A, Varga S, Khairnar R, Mullins CD. Cost-of-illness studies: an updated review of current methods. Pharmacoeconomics. 2016;34(1):43–58.
Acknowledgements
Helen Marshall acknowledges support from the National Health and Medical Research Council of Australia: Career Development Fellowship (1084951).
Author information
Authors and Affiliations
Contributions
BW, HM, LG, and HA conceived and designed the study. BW conducted the database searches, extracted, analyzed, and interpreted the data, performed a quality assessment, and produced the draft of the manuscript. RS extracted data and performed a quality assessment. HM, RS, LG, and HA contributed to, reviewed, and edited the manuscript. HM acts as the overall guarantor.
Corresponding author
Ethics declarations
Conflict of interest
Helen Marshall is an independent investigator on clinical trials of investigational vaccines manufactured by pharmaceutical companies including GlaxoSmithKline, Novavax, and Pfizer. Her institution has received funding for investigator-led research from GlaxoSmithKline, Sanofi-Pasteur, Pfizer, and Novartis Vaccines. Bing Wang, Renee Santoreneos, Hossein Afzali, and Lynne Giles have no conflicts of interest directly relevant to the content of this article.
Funding
No funding was received for the preparation of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, B., Santoreneos, R., Afzali, H. et al. Costs of Invasive Meningococcal Disease: A Global Systematic Review. PharmacoEconomics 36, 1201–1222 (2018). https://doi.org/10.1007/s40273-018-0679-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-018-0679-5