Abstract
Background
Spending on new healthcare technologies increases net population health when the benefits of a new technology are greater than their opportunity costs—the benefits of the best alternative use of the additional resources required to fund a new technology.
Objective
The objective of this study was to estimate the expected incremental cost per quality-adjusted life-year (QALY) gained of increased government health expenditure as an empirical estimate of the average opportunity costs of decisions to fund new health technologies. The estimated incremental cost-effectiveness ratio (ICER) is proposed as a reference ICER to inform value-based decision making in Australia.
Methods
Empirical top-down approaches were used to estimate the QALY effects of government health expenditure with respect to reduced mortality and morbidity. Instrumental variable two-stage least-squares regression was used to estimate the elasticity of mortality-related QALY losses to a marginal change in government health expenditure. Regression analysis of longitudinal survey data representative of the general population was used to isolate the effects of increased government health expenditure on morbidity-related, QALY gains. Clinical judgement informed the duration of health-related quality-of-life improvement from the annual increase in government health expenditure.
Results
The base-case reference ICER was estimated at AUD28,033 per QALY gained. Parametric uncertainty associated with the estimation of mortality- and morbidity-related QALYs generated a 95% confidence interval AUD20,758–37,667.
Conclusion
Recent public summary documents suggest new technologies with ICERs above AUD40,000 per QALY gained are recommended for public funding. The empirical reference ICER reported in this article suggests more QALYs could be gained if resources were allocated to other forms of health spending.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Economic evaluation has a long and established history as an input to funding decisions for new technologies and medical services in Australia, but there remains uncertainty around the opportunity costs of such funding decisions and hence the interpretation of cost-effectiveness data. |
Alternative approaches to identifying and estimating opportunity costs have been discussed and proposed. The estimation of the expected quality-adjusted life-year (QALY) gains from additional health expenditure is the only approach through which empirical estimates of opportunity costs have been generated. |
This article describes the estimation of the expected QALY gains from additional government health expenditure in Australia by adapting and adding to methods used to estimate opportunity costs in England and Spain. The base-case results suggest opportunity costs of 1 QALY for every additional AUD28,033 of government health expenditure. The QALY may not capture all factors that may be considered by decision makers, but this estimate of opportunity costs provides a reference point for the assessment of value across the Australian healthcare system. |
1 Introduction
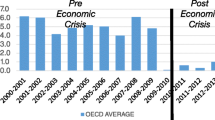
Government health expenditure in Australia increased from AUD71 billion to AUD108 billion between 2004/2005 and 2014/2015 [1]. Constraining this expanding budget without a negative impact on population health is a key policy priority. An important area of government health expenditure is in funding new healthcare technologies. For example, Commonwealth government expenditure on patented pharmaceuticals increased by 27.2% from 2013/2014 to 2015/2016 (AUD3.3 billion to AUD4.3 billion), whilst the script volume processed declined by 13.6% (35.5 million to 30.6 million script volume [2, 3]). The increased prices paid for these new drugs may represent good value for money to the Australian taxpayer, but the current basis for assessing value is limited by the lack of empirical information on the opportunity costs of decisions to fund new health technologies.
The incremental cost-effectiveness ratio [ICER; ∆costs/∆quality-adjusted life-years (QALYs)] provides one input to the assessment of the value of a new technology along with additional factors such as the availability of other treatment options and the characteristics of the eligible population. The utility of the ICER of a new health technology is constrained by limited evidence regarding what is an acceptable and an unacceptable price to pay per additional QALY. Approaches to estimating a threshold or reference ICER to inform the acceptability of ICERs for new technologies can be broadly classified into demand- and supply-side estimates that represent distinct theoretical bases.
Demand-side approaches consider the societal value of a QALY from the consumer perspective, relative to individual consumption [4]. Stated or revealed preferences may be used to estimate the value of a QALY, though we know of no relevant revealed preferences study. Various stated preference studies have elicited the willingness to pay for a QALY from representative samples of the general population [5]. Demand-side estimates of the value of a QALY may inform the value of decisions involving the expansion of the health budget, for example, if taxes are to be increased to fund additional healthcare. However, where the resources required to fund new technologies could be used to provide alternative forms of healthcare, willingness to pay does not provide a relevant basis for assessing value. In such cases, the benefits of new technologies should be compared with benefits forgone from not providing the best alternative forms of healthcare—the opportunity costs of a decision to fund a new technology.
Supply-side approaches to estimating a reference ICER aim to reflect the opportunity costs of decisions to fund a new technology. Proposed supply-side approaches include the use of league tables [6] where the reference ICER is the least cost-effective currently funded technology [7], the estimation of the ICER of services that are displaced to fund a new technology [8] and the estimation of the ICER of current services that would further improve population health if expanded [9]. There are limitations to each of these methods including inadequate data on all currently funded health technologies and difficulties in identifying and analysing displaced services [8, 10] or selecting and analysing services with the potential for expansion.
Another approach to estimating a supply-side reference ICER is based on the expected incremental cost per QALY gained from marginal increases in health expenditure [11]. This approach is based on estimating the empirical relationship between health expenditure and health outcomes [11,12,13] and is limited again by data availability on health costs and outcomes. However, Martin et al. [12, 13] were able to use an estimate of the elasticity of life-years (LYs) lost to health expenditure to calculate the cost per LY and a cost per QALY within disease areas. Claxton et al. [11] estimated the elasticity of QALYs lost across disease areas and assumed a corresponding expenditure effect in disease areas with limited mortality effects, returning a central cost-effectiveness threshold of £12,936 (AUD22,573) per QALY gained across the National Health Service in England [11]. In Spain, estimates of opportunity cost were derived by dividing life expectancies (LEs) by the marginal effect of increased spending on quality-adjusted LEs returning estimates ranging from €21,000 (AUD32,628) based on the average estimate across different age groups to €24,000 (AUD37,289) based on the average population model [14].
In Australia, funding for new technologies comes from within the health budget. Therefore, to maximise health from this constrained budget, an appropriate reference ICER should represent opportunity costs with respect to the best alternative use of resources within the healthcare system. This article reports the first supply-side estimate of opportunity costs in the Australian healthcare system based on the expected incremental cost per QALY gained from marginal increases in government health expenditure. We estimate the relationship between government health expenditure and mortality outcomes and use nationally representative health-related quality-of-life (HRQoL) information to enable direct estimation of the impact of health spending on QALYs. This represents a new method to estimate and incorporate HRQoL gains independent of mortality effects from increased health expenditure.
2 Methodology
This analysis uses national data from 2011/2012 capturing government health expenditure, healthcare need and QALYs lost for small geographical areas across Australia and individual-level, nationally representative longitudinal data on HRQoL, demographics, and social and economic information. In Sects. 2 and 3, we outline the methodology and results and present these in three parts: (1) mortality-related QALY gains, (2) morbidity-related QALY gains and (3) the reference ICER. For part 1, the expenditure elasticity of QALYs lost was estimated controlling for demographics, socioeconomics and healthcare need and applied to the change in per capita government health expenditure between 2010/2011 and 2011/2012 to derive an estimate of the per capita mortality-related QALY gain. In part 2, we estimate the time trend on HRQoL using a fixed-effects regression model controlling for differences in demographics and social and economic conditions. To estimate morbidity-related QALY gains associated with annual increases in health expenditure, estimated annual improvements in HRQoL must be adjusted to account for sustained improvements from previous years and the expected duration of improvements in the year of interest. In part 3, change in total government health expenditure per capita from 2010/2011 to 2011/2012 was divided by the sum of estimated mortality- and morbidity-related QALY gains to estimate the expected incremental cost per QALY gained from increased government health expenditure, or the reference ICER. Parameter and structural uncertainty around the base-case estimate of the reference ICER was then assessed.
2.1 Mortality-Related Quality-Adjusted Life-Year Gains
2.1.1 Data
Government health expenditure data included public hospital data from the National Hospital Cost Data Collection, data on veterans through the Department of Veterans’ Affairs, and data on medical services through the Medical Benefits Schedule and on pharmaceuticals through the Pharmaceutical Benefits Scheme. All data were aggregated to the Statistical Local Area (SLA) based on the SLA of usual residence of the recipients of healthcare rather than the SLA in which healthcare was provided.
Years of life lost (YLL) in each SLA were estimated using the Cause of Death Unit Record File and were age and sex standardised to the Australian standard population. For each death at an age below the LE of the 2012 Australian population, YLL was calculated as the difference between LE and age at death. For each death at or above LE, one YLL was applied. This is a conservative assumption, i.e. that reducing mortality in persons aged over LE gains only one additional year of life. The YLL were summed for all deaths observed in each SLA. The estimated YLL were then weighted by age- and sex-specific utility scores using 36-Item Short Form Survey (SF-36) data from the 2015 South Australian Health Omnibus Survey and the Short-Form Six-Dimension (SF-6D) algorithm to generate QALYs lost for each SLA [15]. The South Australian Health Omnibus Survey is an annual cross-sectional survey administered face to face by trained interviewers to persons aged over 15 years with households identified from a clustered, multi-staged, self-weighted area design of metropolitan areas and towns over 1000 people.
2.1.2 Analysis
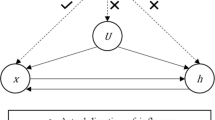
It is commonly suggested that health expenditure and outcomes are endogenous, i.e. expenditure improves outcomes, but poorer outcomes lead to more expenditure [11]. To control for the potential endogeneity of government health expenditure, the following equation was estimated using instrumental variable (IV) two-stage least-squares regression:
where \(h_{i}\) denotes healthcare outcomes measured as QALYs lost in SLA i, x i denotes government health expenditure in SLA i, and n i denotes the vector of covariates in SLA i including demographic factors, geographical variables, and the need for healthcare derived from socioeconomic and health status information. In the first stage, health expenditure is regressed on the IV and all covariates:
The predicted health expenditure from this stage then replaces health expenditure in the second stage, Eq. (1). The Hausman and the Durbin–Wu–Hausman tests were used to confirm the endogeneity of x i in Eq. (1). A relevant and valid instrument, Z in SLA i, should be a strong predictor of the endogenous regressor in the first stage (government health expenditure) and appropriately excluded from the vector of covariates n i in Eq. (1), i.e. the impact of the instrument on QALYs lost occurs solely through the endogenous regressor.
Following prior work [11], we used the proportion of the population providing unpaid care in each SLA as the sole instrument for health expenditure. The first-stage coefficient on expenditure and the Kleibergen–Paap LM and F-statistics are used to assess the relevance of the instrument. We expect a positive relationship between the two based on the rationale that provision of unpaid care leads to higher need-adjusted health expenditure owing to increased identification of the need for services by carers and increased access to health services through removing physical barriers to access, such as transport. Recent estimates for Australia suggest that 88.7 and 84.5% of people who needed support because of a disability received informal support for mobility and transport, respectively [16]. In contrast, Claxton et al. [11] hypothesised a negative relationship between unpaid care and expenditure as a result of substitution effects. Such substitution effects are less likely in Australia compared with England owing to the type of health expenditure included here (i.e. hospital services, Medical Benefits Schedule, Pharmaceutical Benefits Scheme, Department of Veterans’ Affairs), compared with the English analysis that incorporated spending on community and social care. It could be argued that substitution effects between unpaid care and expenditure might be more likely in remote areas of Australia because of the substitution between unpaid care and hospitalisations for example; however, such effects are accounted for here through inclusion of remoteness as a model covariate.
Assessing the validity of the instrument is less straightforward. Whilst there is limited evidence to suggest that the quantity of unpaid care provided has a direct effect on mortality-related QALYs lost, indirect effects through other channels cannot be completely discounted. There are two key potential indirect channels: healthcare need and remoteness. Areas with a high need for healthcare are more likely to have higher levels of unpaid care and higher rates of QALYs lost and, in remote areas, substitution effects between unpaid care and hospitalisations are more likely because of limited appropriate alternative care options such as aged care facilities. Healthcare need and remoteness are both accounted for in n i , Eq. (1), thus supporting the validity of our exclusion criterion. Although we have accounted for the key covariates in n i , Eq. (1), we cannot completely discount that unobserved covariates may be systematically related to the IV. In the Electronic Supplementary Material (ESM), we further discuss issues of instrument validity by examining IV balance on observed covariates. We also assess the sensitivity of our IV estimates to potential violation of the validity assumption using the Union of Confidence Intervals approach. Our sensitivity analyses show that our IV estimates are robust to large deviations from a perfectly valid IV.
The coefficient on expenditure (β 1) is used to calculate the change in QALYs lost from a 1% increase in expenditure. The incremental cost per mortality-related QALY is estimated as:
where x i denotes aggregate government health expenditure and h i denotes total mortality-related QALYs lost.
The annual per capita mortality-related QALY gain is then estimated as:
where the numerator represents the per capita increase in government expenditure on health between the financial years 2010/2011 and 2011/2012 and the denominator represents the incremental cost per mortality-related QALY gained calculated in Eq. (3).
2.2 Morbidity-Related Quality-Adjusted Life-Year Gains
2.2.1 Data
The Household, Income and Labour Dynamics in Australia (HILDA) survey is a longitudinal nationally representative survey of private Australian households conducted since 2001 based on a national probability sample [17]. We use data from 12 waves (2002–2013) for 68,873 observations from a balanced panel that includes the SF-36 survey, which can be converted to preference-based utility scores using the SF-6D [18].
2.2.2 Analysis
Temporal change in HRQoL was estimated using fixed-effects regression with cluster robust standard errors to account for unobserved omitted variable bias arising from intra-individual differences affecting SF-6D scores. To interpret the estimated coefficient for temporal change as a result of the effects of increased government health expenditure, we controlled for an extensive range of demographic, social and economic covariates that might otherwise have led to changes in HRQoL over time in the following model:
where Y it is the SF-6D utility score for the i-th individual in the t-th year, W t is the year trend variable representing the average year-on-year change in HRQoL from 2002 to 2013, and individual-level factors including the year × age interaction, relationship status (married, de facto, separated, divorces, widowed and not married/de facto), highest level of education achieved (postgraduate, graduate diploma/certificate, bachelor/honours degree, advanced diploma/diploma, certificate, year 12, and year 11 or below) and 21 life events such as separation from a spouse in the prior 12 months (see Table 2). X it denotes social covariates including self-reported satisfaction with personal safety, local community, neighbourhood, amount of free time and life in general, and Z it denotes economic covariates including currently weekly gross wages and salary, employment status (employed, not employed, not in the labour force), self-reported prosperity given current needs and financial responsibilities, self-reported satisfaction with financial situation, perceived difficulty in raising money for an emergency, ability to pay utility bills or mortgage/rent on time, whether pawned or sold something, whether went without meals or were unable to heat their home, and whether asked for financial help from friends/family or welfare/community organisations, and a binary measure of income insecurity [19]. Only statistically significant covariates were retained in the final model.
This time trend represents the average annual change in HRQoL. The reference ICER should capture all HRQoL improvement from a single year of health expenditure. Thus, (1) ongoing effects of expenditure in years prior to 2011 should be excluded from the estimated impact of increased expenditure in 2011 on HRQoL and (2) ongoing effects of 2011 expenditure on HRQoL in subsequent years should be incorporated.
Clinician input was used to classify alternative categories of health expenditure that improve HRQoL for 1 year, or across the remainder of the individuals’ lifetime. The aggregate improvement in HRQoL over the 11-year time horizon of the observed data was then estimated as:
where \(x_{i}\) is the improvement in HRQoL in the year of increased expenditure i, which is weighted by the increase in expenditure in each year relative to increased expenditure in 2011 (at 2011 prices). \({\text{Agg}}.{\text{pr}}({\text{maintained HRQoL}})\) is the proportion of improved HRQoL that is maintained over patients’ remaining lifetime (estimated from Eq. (4) in the ESM). The HRQoL improvement in 2011 (x 10) was fitted so that \({\text{Agg}}.{\text{HRQoL improve}}\) from Eq. (6) matched the sum of the year trend coefficient from 2002 to 2013. The morbidity-related QALY gains associated with increased expenditure in 2011 were estimated by multiplying the HRQoL improvement in 2011 (x 10) by the weighted average duration of HRQoL improvements (estimated from Eq. (2) in the ESM).
2.3 Reference Incremental Cost-Effectiveness Ratio
Equation (7) describes the estimation of the expected incremental cost per QALY gained from increased government health expenditure in 2011/2012. The reported increase in total per capita government health expenditure in 2010/2011 to 2011/2012 is divided by the combined per capita mortality- and morbidity-related QALY gains:
To represent uncertainty, deterministic sensitivity analyses were undertaken around the two key input parameters: the elasticity that informs the mortality-related QALY gains and the year trend that informs the morbidity-related QALY gains. Scenario analyses were undertaken using the alternative estimates of the expected duration of HRQoL improvements without ongoing expenditure. A probabilistic sensitivity analysis was informed by the repeated drawing of 10,000 values from the sampling distributions of the elasticity and year trend parameters. A log-normal distribution was assumed for the elasticity of mortality-related QALYs to expenditure, and a normal distribution for the estimated change in morbidity-related QALYs from expenditure.
3 Results
3.1 Mortality-Related Quality-Adjusted Life-Years
Our analysis of the expenditure model in Eq. (1) indicated that the null hypothesis that expenditure was exogenous was rejected (Hausman; 26.138, p < 0.01). A significant Durbin–Wu–Hausman test [20] supported this conclusion, with the estimated coefficient on the residuals being significantly different from zero (F(1,1004) = 25.94, p < 0.001) [see Table 1 in the ESM). The instrument was relevant, indicated by its significant prediction of health expenditure in the first stage (β = 0.193, p < 0.001), the Kleibergen–Paap LM statistic (10.826, p < 0.05) and the Kleibergen–Paap F-statistic greater than the rule-of thumb of 10 (F-statistic = 12.36). Regression estimates are presented in Table 1. The estimated coefficient on government health expenditure indicates that a 1% increase in government health expenditure is associated with a reduction of 1.6% in QALYs lost. Applying the estimated outcome elasticity to estimate mortality-related QALY gains associated with increased health expenditure in 2011/2012 (Eq. 3) generates a per capita mortality-related QALY gain of 0.0013 [95% confidence interval (CI) 0.0003–0.0023].
3.2 Morbidity-Related Quality-Adjusted Life-Years
From the fixed-effects regression predicting SF-6D scores (F(72,6729) = 33.63, p < 0.001), the estimated coefficient on the time trend indicated that HRQoL improved on average by 0.0026 per year (t = 7.17, p < 0.001; 95% CI 0.0019–0.0033), controlling for an extensive set of demographic, societal and economic variables as shown in Table 2. Estimates of the weighted average length for ongoing HRQoL were 2.6 years for unreferred medical services (see Table 3 in the ESM) and across the three options used to classify hospital services, ranged from 3.3 (see Table 4 in the ESM) to 14 years. The aggregate weighted duration of HRQoL effects ranged from 2.0 to 4.1 years across the three scenarios (see Table 6 in the ESM). These are associated with corresponding estimates of the proportion of total health services that provide a lifetime HRQoL effect of 10.2–23.5% (calculated from Eq. (4) in the ESM). In the base case, we take the central estimates of a duration of continued HRQoL improvement of 2.54 years from a single year of expenditure, and the proportion of lifetime HRQoL effects of 11.7%. Our base-case estimate suggests an annual per capita improvement of 0.0066 morbidity-related QALYs owing to increased health expenditure in 2011/2012. Table 3 describes the alternative scenarios used to estimate morbidity-related QALY gains.
3.3 Reference Incremental Cost-Effectiveness Ratio
Government health expenditure across all areas increased by AUD229 per capita in 2011/2012. The base-case estimate of the combined mortality- and morbidity-related QALY gain per capita from increased expenditure in 2011/2012 is 0.0078. The resulting reference ICER, representing the expected incremental cost per QALY gained from increased health expenditure calculated from Eq. (7) is AUD28,033. Figure 1 shows that the value of the reference ICER is not sensitive to the alternate scenarios around the duration of the estimated HRQoL improvement in 2011/2012. Deterministic sensitivity analyses in Table 4 indicate the base-case estimate is more sensitive to uncertainty around the estimated morbidity-related QALY gains than mortality-related QALY gains, ranging from AUD22,815 to AUD36,349 for the upper and lower bounds of the estimated HRQoL improvement. The probabilistic sensitivity analysis generated a 95% CI of AUD20,758–37,667, and Fig. 2 indicates the high probability (0.94) that the reference ICER is less than AUD35,000 per QALY.
4 Discussion
Economic evaluation has been a key component of public funding decisions for new technologies in Australia since 1993 [21]. However, there is a lack of clarity and transparency in how decision makers interpret and use such evidence. To ensure a net gain in QALYs across the health system, decision makers should be aware of the benefits that will be forgone (the opportunity costs) if a new technology is funded. To date, empirical estimates of opportunity costs have been a missing element of the decision-making process. Seminal work by Claxton and colleagues at the University of York described an empirical approach to estimating opportunity costs as the expected shadow price of the healthcare budget in the English National Health Service [11]. Adapting these methods, we have estimated the reference ICER as AUD28,033 for the Australian healthcare system. It is expected that the funding of a new technology with an ICER greater than the reference ICER results in a net decrease in population health, as represented by net QALY losses. Uncertainty analysis around the base-case estimate indicates the high probability that the reference ICER of AUD28,033 (bootstrapped 95% CI AUD20,758–37,667) is less than AUD35,000 per QALY.
There are no prior estimates of the opportunity costs of healthcare funding decisions in Australia, but similar analyses have been undertaken in England and Spain. In England, Claxton et al. [11] employed several cross-sectional datasets capturing national and regional spending and YLL across disease categories to estimate YLL elasticities also using IV two-stage least-squares approaches. YLL were then translated to QALYs by weighting YLL by utility scores from the UK population. QALY gains associated with improvements in HRQoL were assumed to be generated at the same rate as QALY gains derived from reduced mortality [11]. In Spain, Vallejo-Torres et al. [14] used a fixed-effects model with 5-year data from the 17 regional health service areas to assess the impact of health spending on quality-adjusted LE estimated using the healthy LE approach [22]. Spanish life tables by region and year were used to adjust LE for HRQoL by multiplying the number of years lived within sex and age categories by corresponding average EQ-5D utilities.
The main difference between the reported studies is in the estimation of expenditure effects on HRQoL. The English study did not use empirical HRQoL data, whilst the Spanish and Australian studies used alternative methods to generate yearly HRQoL effects. The Spanish study mapped utility values to a set of health and socioeconomic indicators for which repeat observations were available. Nationally representative EQ-5D utilities were only available for 2011/2012 from the Spanish Health Survey; therefore, information from the Spanish Health Survey in 2006/2007 and the European Health Interview Survey in 2009/2010 were used to model year-specific EQ-5D utilities based on health indicators and socioeconomic variables stratified by age and sex. The Australian study analysed longitudinal data that included SF-6D derived utility values and a comprehensive range of sociodemographic and social and economic condition variables aimed at isolating the effects of health expenditure on HRQoL. The similarity of the estimated opportunity costs in relation to current ICER thresholds, despite divergent healthcare systems and methodological approaches, provides some support for the cross-validity of these studies (see Table 5).
4.1 Limitations and Assumptions
Estimating Eq. (1) via ordinary least squares regression results in biased coefficients on expenditure because of the endogeneity to health outcomes. Instrumental variable two-stage least-squares regression generates unbiased estimates under such conditions; however, the robustness of these estimates centres on the relevance and validity of the instrument. To account for the endogeneity of health expenditure to health outcomes in Eq. (1), we instrumented the endogenous regressor with the proportion of the population providing unpaid care. Evidence was provided for the relevance of the instrument, and its validity was established theoretically and supported empirically with sensitivity analyses indicating only large deviations from the exclusion criterion would alter the qualitative conclusions drawn (see ESM for full details).
Table 6 lists the assumptions incorporated in the presented analysis, noting the expected directions of each assumption on the base-case reference ICER. The qualitative interpretation from these assumptions is that the reference ICER does not significantly over- or underestimate the true opportunity cost: of 10 key assumptions made in the analysis, five are argued to have no directional impact on the estimated reference ICER, three represent an overestimate of the reference ICER and two represent an underestimate of the reference ICER. As the central estimate of the reference ICER suggests the current implied decision-making threshold should be reduced, from a change management perspective it may be more important to focus on assumptions (5) and (8), which are predicted to underestimate the reference ICER.
For assumption (5), the mortality-related QALY gains calculated from Eq. (3) assume that averted YLL are lived in the same utility as the general population matched by age and sex. This may overestimate differences in QALYs lost, as YLL are more likely to occur in clinical populations with lower HRQoL than the general population.
A sensitivity analysis using utility values derived from EQ-5D-3L data [23], which were on average 6% higher than our base-case values, had minimal impact on the reference ICER: the reference ICER reduced by AUD237 to AUD27,796. Thus, the base-case reference ICER is likely to be robust to the potential overestimation of utility values to estimate mortality-related QALY gains.
For assumption (8), in the estimation of morbidity-related QALY gains, the time trend variable may represent the effects of factors other than government health expenditure on population-level changes in HRQoL. The wide range of socioeconomic covariates is assumed to control for the effects of private health insurance and individual health spending and the ‘assistance from welfare or community organisations’ covariate controls for non-government organisation expenditure. Variation in social determinants of health may also explain improvements in HRQoL over time. Determinants of health and illness are broadly classified as biological, psychological and social [24, 25], with government health expenditure largely directed toward the biological and psychological determinants. Social determinants of health include social and community networks and the general socioeconomic, cultural and environmental conditions such as education, work conditions, unemployment and housing [26]. Our fixed-effects regression model included a wide range of covariates such as community engagement measures, employment, perceived prosperity and difficulty in meeting utility payments, to control for changes in such social determinants of health over time to provide the best current estimate of the impact of government health expenditure on population HRQoL. In addition, it is not clear whether social determinants of health improved or declined over the study period. A related factor likely to have underestimated the reference ICER to some degree is the omission of covariates representing improvements in safety (e.g. occupational and transport safety) that are likely to have contributed to improvements in HRQoL over the time period.
We acknowledge that QALY maximisation is not always the sole goal of public funding decisions [27]. QALY gains do not represent the full societal valuation of individual health benefits nor do they capture external factors such as the perceived need to support and incentivise the pharmaceutical industry. Despite the limitations of the QALY as a measure of benefit and the extraneous factors that may influence funding decisions, the estimation of opportunity costs with respect to forgone QALYs is a useful input to the decision-making process. If a new technology is estimated to gain fewer QALYs than are being forgone, then the decision maker can trade off the QALY losses with other aspects or dimensions of value that might be provided by the new health technology under evaluation. Alternatively, a new technology may be estimated to gain more QALYs than are expected to be forgone, but other factors such as the overall size of the eligible population may require the ICER of the new technology to be lower than the reference ICER. The reference ICER reflects the effects of marginal increases in government health expenditure, which likely underestimate the opportunity costs of technologies with large budget impacts.
5 Conclusion
Australian decision-making committees do not have explicit cost-effectiveness thresholds. However, public summary documents show that medical services with ICERs over AUD40,000 per QALY gained have been recommended for funding [28], whilst summary documents from the Pharmaceutical Benefits Advisory Committee have referred to the need to bring prices down so that ICERs are reduced to a value between AUD45,000 and AUD75,000 [29]. This article presents the first empirical estimate of the opportunity costs of decisions to publicly fund new health technologies in Australia of AUD28,033 per QALY gained, which suggests a net loss in population health associated with funding a proportion of new pharmaceuticals and medical services.
Australia was an early adopter of economic evaluation to inform funding decisions for new health technologies [30]. We encourage the early adoption of these first empirical estimates of the opportunity costs in Australia to better inform value-based decision making and to better improve population health from the public funds allocated to healthcare.
References
AIHW. National health expenditure data cube, 1985–86 to 2014–15. Canberra: AIHW; 2016.
Pharmaceutical Benefits Scheme Information Management Section Pharmaceutical Policy Branch. Expenditure and prescriptions twelve months to 30 June 2015.
Pharmaceutical Benefits Scheme Information Management Section Pharmaceutical Policy Branch. Expenditure and prescriptions twelve months to 30 June 2016.
Woods B, Revill P, Sculpher M, Claxton K. Country-level cost-effectiveness thresholds: initial estimates and the need for further research. Value Health. 2016;19:929–35.
Shiroiwa T, Sung Y, Fukuda T, Lang H, Bae S, Tsutani K. International survey on willingness-to-pay (WTP) for one additional QALY gained: what is the threshold of cost effectiveness? Health Econ. 2010;19:422–37.
Weinstein M, Zeckhauser R. Critical ratios and efficient allocation. J Public Econ. 1973;2:147–57.
Eichler H-G, Kong SX, Gerth WC, Mavros P, Jönsson B. Use of cost-effectiveness analysis in health-care resource allocation decision-making: how are cost-effectiveness thresholds expected to emerge? Value Health. 2004;7:518–28.
Appleby J, Devlin N, Parkin D, Buxton M, Chalkidou K. Searching for cost effectiveness thresholds in the NHS. Health Policy. 2009;91:239–45.
O’Mahony JF, Coughlan D. The Irish cost-effectiveness threshold: does it support rational rationing or might it lead to unintended harm to Ireland’s health system? Pharmacoeconomics. 2016;34:5–11.
Schaffer SK, Sussex J, Devlin N, Walker A. Local health care expenditure plans and their opportunity costs. Health Policy. 2015;119:1237–44.
Claxton K, Martin S, Soares M, Rice N, Spackman E, Hinde S, et al. Methods for the estimation of the National Institute for Health and Care Excellence cost-effectiveness threshold. Health Technol Assess. 2015;19:1–503.
Martin S, Rice N, Smith PC. Does health care spending improve health outcomes? Evidence from English programme budgeting data. J Health Econ. 2008;27:826–42.
Martin S, Rice N, Smith PC. Comparing costs and outcomes across programmes of health care. Health Econ. 2012;21:316–37.
Vallejo-Torres L, García-Lorenzo B, Serrano-Aguilar P. Estimating a cost-effectiveness threshold for the Spanish NHS. Spanish Health Economics Study Group Meeting, Gran Canaria. 2016.
Taylor A, Dal Grande E, Wilson D. The South Australian Health Omnibus Survey 15 years on: has public health benefited. Public Health Bull. 2006;3:30–2.
Australian Bureau of Statistics. Disability, ageing and carers, Australia: summary of findings, 2015. Cat No. 44300 2016.
Watson N, Wooden MP. The HILDA survey: a case study in the design and development of a successful household panel survey. Longit Life Course Stud. 2012;3:369–81.
Walters SJ, Brazier JE. What is the relationship between the minimally important difference and health state utility values? The case of the SF-6D. Health Qual Life Outcomes. 2003;1:4.
Rohde N, Tang KK, Osberg L, Rao P. The effect of economic insecurity on mental health: recent evidence from Australian panel data. Soc Sci Med. 2016;151:250–8.
Davidson R, MacKinnon JG. Estimation and inference in econometrics. New York: Oxford University Press; 1993.
Pharmaceutical Benefits Advisory Committee. Guidelines for preparing submissions to the Pharmaceutical Benefits Advisory Committee, Version 4.5; 2015.
Sullivan DF. A single index of mortality and morbidity. HSMHA Health Rep. 1971;86:347.
Clemens S, Begum N, Harper C, Whitty JA, Scuffham PA. A comparison of EQ-5D-3L population norms in Queensland, Australia, estimated using utility value sets from Australia, the UK and USA. Qual Life Res. 2014;23:2375–81.
Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196:129–36.
Havelka M, Despot Lučanin J, Lučanin D. Biopsychosocial model: the integrated approach to health and disease. Coll Antropol. 2009;33:303–10.
Dahlgren G, Whitehead M. Policies and strategies to promote social equity in health Background document to WHO — Strategy paper for Europe. Stockholm: Institute for Futures Studies; 1991.
Carter D, Vogan A, Afzali HHA. Governments need better guidance to maximise value for money: the case of Australia’s Pharmaceutical Benefits Advisory Committee. Appl Health Econ Health Policy. 2016;14:401–7.
Australian Government Department of Health. Application No. 1428: mechanical thrombectomy for acute ischaemic stroke. November 2016: public summary document.
Australian Government Department of Health. Idelalisib oral tablet, 100 mg, 150 mg Zydelig®, Gilead Sciences Pty Ltd. March 2016: public summary document.
Raftery JP. Paying for costly pharmaceuticals: regulation of new drugs in Australia, England and New Zealand. Med J Aust. 2008;188:26.
Acknowledgements
The authors gratefully acknowledge the cooperation and effort of the data providers (Independent Hospital Pricing Authority, Department of Human Services, Department of Veterans’ Affairs, Australian Coordinating Registry) in the health authorities of the States and Territories and the Australian Government; the Australian Bureau of Statistics for access to the Census of Population and Housing 2011 through Tablebuilder; and the Household, Income and Labour Dynamics in Australia (HILDA) survey. The HILDA Project was initiated and is funded by the Australian Government Department of Social Services and is managed by the Melbourne Institute of Applied Economic and Social Research (Melbourne Institute). The findings and views reported in this article, however, are those of the authors and should not be attributed to either the Department of Social Services or the Melbourne Institute. The authors thank Prof. Mark Sculpher for his conceptual input and Dr. James Lomas for useful comments on the statistical methods. The authors also acknowledge the members of their advisory group; Prof. Rosalie Viney, Prof. Robyn Ward, Prof. Catherine Cole, Prof. Jonathan Craig and Associate Prof. Rachael Moorin for their input to the overall research methodology.
Author information
Authors and Affiliations
Contributions
Jonathan Karnon, Hossein Haji Ali Afzali and Terence C. Cheng conceptualised the study, all authors contributed to the development of the methods used and approved the analyses. Laura C. Edney wrote the first draft of the manuscript. All authors contributed to subsequent drafts, responses to the peer reviewers and approved the final version.
Corresponding author
Ethics declarations
Funding
This study was funded by a National Health and Medical Research Council Project Grant (No. 108-4387).
Conflict of interest
Jonathan Karnon is a member of the Economic Sub-Committee of the Pharmaceutical Benefits Advisory Committee and Hossein Haji Ali Afzali is a member of the Evaluation Sub-Committee of the Medical Services Advisory Committee. Terence C. Cheng and Laura C. Edney have no conflicts of interest directly relevant to the contents of this article.
Ethics approval
Ethics approval was granted by the South Australian Health Human Research Ethics Committee (Ethics Reference No. HREC/14/SAH/159).
Data availability statement
The datasets generated and analysed during the current study are not publicly available owing to strict confidentiality requirements imposed by the data custodians.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Edney, L.C., Haji Ali Afzali, H., Cheng, T.C. et al. Estimating the Reference Incremental Cost-Effectiveness Ratio for the Australian Health System. PharmacoEconomics 36, 239–252 (2018). https://doi.org/10.1007/s40273-017-0585-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-017-0585-2