Abstract
Background
There is a growing interest in incorporating informal care in cost-of-illness studies as a relevant part of the economic impact of some diseases.
Objective
The aim of this paper was to review the recent literature valuating the costs of informal care in a group of selected diseases from 2005 to 2015.
Methods
We carried out a systematic review on the economic impact of informal care, focusing on six selected diseases: arthritis or osteoarthritis, cancer, dementia, mental diseases, multiple sclerosis and stroke.
Results
We selected 91 cost-of-illness articles. The average weight attributed to the informal care cost over the total cost was highly relevant for dementia, stroke, mental diseases, cancer and multiple sclerosis. The most frequent valuation method applied was the opportunity cost method, followed by the proxy good method. The annual cost of informal care presented a high variability depending on the disease and geographic location. Distinguishing by type of illness, the disease with the highest annual value of informal caregiving was dementia, followed by mental illness and multiple sclerosis. The average hourly unit cost was €11.43 (2015 values), varying noticeably depending on the geographic location.
Conclusion
This paper identifies several aspects that should be enhanced to promote comparability between studies and countries, and it sends key messages for incorporating informal care costs to adequately measure the economic impact of diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The significant weight of informal care on the total cost of the selected diseases indicates that the non-consideration of informal care represents an underestimation of the social cost of certain diseases. |
The diseases that have a greater presence in estimating the costs of informal care are dementias, particularly Alzheimer’s disease, followed by other conditions that cause significant limitations on personal autonomy and therefore a strong demand for care. |
Several methodological aspects need to be improved to promote comparability among studies that focus on the estimation of the cost of illness from a social perspective or that valuate informal caregiving. |
1 Introduction
Population ageing is a triumph and a challenge [1]. On one hand, it requires public authorities and society itself to invest in policies and interventions focused on healthy and active ageing [2–6]. On the other hand, it will create an added element of tension for public services hitherto considered basic services, such as pensions, health care and long-term care [7, 8]. In precise terms, and focusing on this last point, there is great heterogeneity in the organisation of long-term care (LTC) among OECD countries. Despite substantial variations across countries, family carers are the backbone of LTC systems in OECD countries, especially in countries with strong family traditions. In fact, the number of informal care users is expected to rise significantly in the coming years, especially in certain European countries. For instance, countries such as Spain are expected to experience an increase of 140%, from approximately 1.2 million in 2010 to more than 2.8 million in 2060. In Germany, a 51% rise is expected, from approximately 2.7 million in 2010 to 4.1 million in 2060. In the Netherlands, a 66% increase, from 93,000 in 2010 to 154,000 in 2060, is envisaged [9].
Due to its heterogeneity, defining informal care is not straightforward [10]. This heterogeneity is related to differences in time investment per day or per week, the duration of care (in years), the type of care tasks provided and the intensity thereof. Informal care is provided by non-professional people, normally by family, close relatives, friends or neighbours. In many cases, caregivers have not received previous training despite the complexity of the tasks related to the specific health problems and diseases involved, i.e., personal care for people with limited autonomy to carry out their daily living activities, household work, administrative and supervision tasks, companionship and emotional support. Informal caregivers usually have no limits on their time spent providing care and are often not paid for their services. Although there may be specific benefits, training and support programmes for carers in some countries [11], the non-professional character of caregiving and the emotional relationship between the person being cared for and the caregiver are the most distinctive features of informal care. By contrast, formal care is defined as services that are provided by trained and qualified professionals. These care services are publicly or privately controlled and involve contracts specifying care-based responsibilities and working regulations. Care services are specified according to professional qualifications, and care workers have a precise time schedule [12].
Informal care has been an invisible resource until recently [13]. While informal care may be free of charge to public administrations, it has its own ‘hidden costs’, including detrimental health and psychological effects on carers, a decrease in labour supply and the deterioration of household finances and even being a risk factor for mortality [14–17]. By contrast, some studies show several positive aspects of informal caregiving [18, 19]. In fact, the provision of informal care can have simultaneously positive (companionship, satisfaction or enjoyment of caring) and negative effects on the wellbeing of the carer [19–21]. In this sense, LTC systems are evolving into mixed models of care in which care is considered to be a shared responsibility, as opposed to models in which care is considered the responsibility of either the welfare state or, conversely, individuals or families [12].
Cost-of-illness studies try to identify, measure and assess healthcare and non-healthcare resources and productivity losses that result from premature death, morbidity, disability or injury due to the corresponding disease and/or its co-morbidities [22]. This information can be useful as the basis for economic evaluation or in helping decision makers prioritise healthcare policies and interventions when considering efficiency. Currently, most cost-of-illness studies of diseases include healthcare costs. However, there is a growing interest in incorporating informal care as part of non-healthcare costs [23–30]. Moreover, in countries that have adopted a social perspective in the economic evaluation of health interventions, the costs associated with informal care can be very relevant. Even among those that have adopted the perspective of healthcare funders (healthcare costs only), if circumstances warrant it, they can also consider non-healthcare costs in economic evaluations [31]. The reason is that for certain diseases and injuries, non-consideration of non-healthcare costs might cause an impoverished and biased view of their real economic and social impacts. Thus, empirical studies can support the risk of suboptimal decisions based on a restricted view of benefits [32]. For instance, in the field of economic evaluation, the inclusion of productivity and informal care costs can have a strong impact on cost-effectiveness outcomes. Krol et al. [33] compared how incremental cost-effectiveness ratios (ICERs) varied with the inclusion and exclusion of productivity costs. The results showed that ICERs increased due to the inclusion of productivity costs in six out of 36 cases and decreased in 30 cases; in six of the latter, the incremental costs changed from positive to negative (the new treatment became a cost-saving alternative). In the case of informal care studies, the majority of economic evaluations ignore this type of social resource. However, its inclusion can have a relevant impact on cost-effectiveness studies [34]. The consequence is that ignoring informal care will lead to underinvestment in interventions that benefit people with limitations in their autonomy, and their caregivers [35]. In the framework of cost-of-illness studies, the exclusion of informal care leads to an underestimation of the true social impact of a disease, especially in the case of health problems that limit the personal autonomy of patients.
While the strengths and weaknesses of the methods used to valuate labour losses caused by diseases and injuries have been widely discussed [36–44], the available evidence in the case of informal care is less extensive [10, 45, 46], and many of the methods used are constantly being tested [47–56]. There are two recent systematic literature reviews on the inclusion of informal care, focused on economic evaluations [34, 35]. Nevertheless, the objectives of economic evaluation studies differ from those of cost-of-illness studies. Therefore, the aim of this paper is to review the recent literature on the costs of informal care in two dimensions: the disclosure and the valuation of caregiving times. To do this, a systematic review of cost-of-illness studies on six selected diseases (arthritis/osteoarthritis, cancer, dementia, mental disease, multiple sclerosis and stroke) was carried out for the period 2005–2015. These diseases were selected due to their high prevalence and the limitations they place on personal autonomy, therefore generating need for personal care. As a result, this study will identify several aspects for enhancement to promote comparability among studies focused on valuating informal caregiving.
2 Methods
The systematic literature review used three databases: PubMed, the National Health Service Economic Evaluation Database (NHS EED) and EconLit. The articles were searched in these databases by title and abstract using two different groups of keywords. In order to select the search terms, we considered two recent systematic literature reviews on the inclusion of informal care in economic studies [34, 35]. Goodrich et al. [35] did use the terms ‘caregive*’, ‘carer family’, ‘carer home’, ‘carer informal’, ‘care*’, ‘informal caregive*’ and ‘unpaid care*’ equivalent to the ‘care’ or ‘informal’ terms we have used, whereas Krol et al. [34] used ‘cost’ and ‘costs’ which are equivalent to our ‘cost*’ search term. The Health Information Research Unit at McMaster University (Hamilton, ON, Canada) specifies the search filters for MEDLINE in Ovid syntax and the PubMed translation. In addition, the NHS Centre for Reviews and Dissemination also specifies the recommended search terms to use in a systematic search. Therefore, a mix of those search terms was used. The systematic review followed the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines on reporting systematic reviews [57]. More details about the systematic review strategy can be found in Annex 1 of the electronic supplementary material.
Papers in English measuring the cost or value of time of informal care were included. Exclusion criteria comprised studies that were not cost-of-illness analyses, were economic evaluations, were reviews, were not focused on a disease of interest, did not distinguish informal care from other costs, were not original papers, did not evaluate informal care, were methodological papers or were not written in English.
A data extraction form included questions on the studies’ context (e.g. geographical study location), sampling and sample characteristics (e.g. disease), methods and results (e.g. method to valuate informal care, perspective) and conclusions (e.g. results summary, study funding). The first screening was conducted by the researcher most experienced in systematic revisions among the authors (MTB). Then, each abstract and paper selected was reviewed by two investigators (LPL and RPR), and data extraction was performed independently. The decision for inclusion in the review was made by two investigators (LPL and MTB). Whenever there was a disagreement, the papers were reviewed by a third investigator (JOM). Microsoft Excel was used to summarise the results from the systematic literature review.
After all articles that satisfied the inclusion criteria were collected, summary descriptive statistics were used to describe the methodological characteristics and the type of informal care costs analysed. A quantitative analysis was performed based on papers reporting informal time and its monetary value. The mean, median, standard deviation, maximum and minimum values were calculated using STATA 14 to summarise time and cost information among the studies included.
To aid the comparative quantitative analysis, the mean unit and annual costs were converted to 2015 euros (€) using country-specific or country-group-specific inflation on average consumer prices [58]. The annual costs and mean unit values were adjusted by the interannual inflation rate from the price year to 2015. If required, the unit and annual costs from 2015 were multiplied by the European Central Bank’s 2015 exchange rates. For papers not reporting the year in which the costs were calculated, the publication year was used.
To simplify the reporting of the results, the authors created different country groups, as follows: Nordic Europe, Central Europe, Eastern Europe, Southern Europe, British Isles, Europe, North America, Asia-Oceania, low-middle-income countries (including Africa, India, Latin America, Sri Lanka, low-income countries, and lower-middle-income countries), and other countries (including high-income countries, worldwide, and upper-middle-income countries).
3 Results
The search identified a total of 1705 studies of interest. Of those, 157 studies were not included because they were duplicates. Of the rest of the papers (n = 1548), 1277 were excluded because they were not cost-of-illness analyses; were economic evaluations or reviews; or were not focused on the disease of interest. A total of 271 articles that met the initial inclusion criteria were included in the full-text review. Finally, we selected 91 cost-of-illness studies (Fig. 1).
Of the 91 cost-of-illness articles included, 29 used a retrospective analysis, and 44 used a prospective analysis (Table 1). They used samples ranging from 57 to 3440 individuals. Regarding illness, dementia was the most prevalent disease in which informal care costs were analysed (37 articles), followed by multiple sclerosis (18), cancer (14), stroke and mental illness (9 each) and arthritis/arthrosis (4). The US was the country with the highest number of papers (14). However, once European studies were aggregated, this continent had more estimations of caregiving (with a total of 67 articles), with Spain occupying first place, followed by the UK, Sweden, Germany and Italy. Of the 91 papers selected, the most were published in 2006 (20 published articles), followed by 2013 and the first eight months of 2015 (12 articles).
The majority of the studies (87%) included several types of costs (healthcare and non-healthcare costs). The remaining 13% focused on estimating only the cost of informal care. In almost 70% of the studies, informal care was valuated without indicating whether caring time corresponded to the primary caregiver or primary and other secondary caregivers. Among the studies carried out, 27% used the recall method with a structured questionnaire, 14% used direct questions, and 4% used other methods. Approximately 53% did not detail the method used to measure care time. Only eight articles showed the time spent by caregivers in each activity, and 17 applied time restrictions in caregiving hours (most applying a maximum of 16 daily hours, assuming 8 h of rest). Thus, the most frequent valuation method found was the opportunity cost method (54 studies), followed by the proxy good method (24). Seven articles applied several methods. Finally, more than 50% of the studies included were funded by private sectors/companies (Table 1; interested readers may find more detail by geographical area in the electronic supplementary material). In 51% of the studies, the hourly unit cost applied to valuate caregiving appeared explicitly. In the remaining 49%, either it was not expressly indicated or there was no unique shadow price (that is, an imputed valuation of a service for which no market price exists [59]), making it impossible to obtain the unique unit value. The presence of multiple values for care time mainly occurred in studies where the opportunity cost method was applied, with different shadow prices based on the activity given up (leisure or working time), or in studies where the proxy good method was applied, with prices differentiated depending on the activity (personal care, administrative activities, domestic work, etc.).
In the 91 studies, 98 estimations of weekly caregiving time and 107 values of unit costs were obtained. Regarding care time, the average caregiving time was 32.4 h per week (standard deviation [SD] 23.8), ranging from 2 to 120 h, depending on the disease (Table 2). Among the diseases considered, dementia, mental illness and multiple sclerosis required the most care time (36, 32 and 30 weekly hours, respectively). Depending on the country or geographic location, the amount of caregiving time varied significantly. Dementia was the disease analysed most frequently. Focusing on this illness, we can carry out a more homogeneous comparison of the results by groups of countries. Focusing on dementia, studies carried out in Southern European countries and the British Isles show that those countries spent on average 67 and 57 h per week on caring, respectively, followed by Eastern Europe, with 42 h. Asian countries invested on average 19 h a week.
The average hourly unit cost used to valuate informal caregiving in the included studies was €11.43 (SD 6.32). Nevertheless, this unit cost varied noticeably among the different geographic locations (Table 3). The highest values were found in studies conducted in North America, Central Europe, the British Isles and the Nordic countries, with €14.97, €14.68, €13.92 and €13.58 per hour, respectively. By contrast, low-middle-income countries and Eastern Europe had average hourly unit costs of informal care of €5.40 and €3.68, respectively. In dementia studies, the figures were slightly higher. Again, Central Europe, the Nordic countries and North America were those with the highest hourly unit costs (€15.85, €14.63 and €14.32, respectively), with the average for all countries being €10.78, while low-middle-income countries and Eastern Europe were those with the lowest (€5.40 and €3.29, respectively).
Taking into account the technique applied, we observed differences in the unit cost considered (Table 4). Among studies that used the opportunity cost method, the hourly average unit cost was €10.14 (SD 4.78), with values ranging from €3.71 (in Eastern Europe) to €15.95 (in North America). Meanwhile, the average unit cost used under the proxy good method was €14.86 (SD 7.89), fluctuating between €4.56 (in Eastern countries) and €21.77 (in Nordic countries).
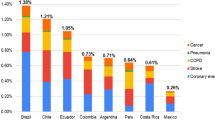
Regarding costs, the average weight attributed to informal care of the total cost was 50.0% for dementia, 28.0% for stroke, 27.7% for mental illnesses, 24.3% for cancer, 22.9% for multiple sclerosis and 9.3% for arthritis or osteoarthritis. Considering all studies included, the annual cost of informal care was €17,049 (SD 19,550) (year 2015), with values ranging from €26 to €160,970 (Table 5). When differentiating by type of illness, the illness with the highest annual value of informal caregiving was dementia, followed by mental illness and multiple sclerosis, with €21,065 (SD 21,793), €15,416 (SD 16,311) and €12,709 (SD 16,763), respectively. Needless to say, the value of this cost might vary significantly depending on the country or geographic location. The highest annual cost of informal care was obtained in the British Isles, with an average of €42,956 (SD 44,514), followed by the Southern and Nordic countries with €27,966 (SD 17,152) and €27,283 (SD 25,749), respectively (Table 5).
4 Discussion and Conclusion
This study conducted a review of the inclusion of informal care in cost-of-illness studies during the period 2005–2015. Several patterns of interest were observed from this analysis. First, the significant weight of informal care as a percentage of the total cost of the diseases selected indicated that the non-consideration of informal care represented an underestimation of the social cost of certain diseases. In fact, jointly with the 91 cost-of-illness studies analysed, four studies were identified that estimated the aggregated impact of the value of informal care (that is, without differentiating between any disease at an aggregate/national level). These studies were conducted in the US, Canada, France and Spain [60–63]. The results of these studies confirmed that informal caregiving has a highly significant economic impact at an aggregated level. A US paper [60] estimated a total value of informal care of US$221 billion to US$642 billion (with the proxy good method) and $522 billion (with the opportunity cost method) in 2012. These figures are equivalent to 1.4–4.0% of US GDP in 2012. Paraponaris et al. [61], using the proxy good approach, valuated informal care in France at €6.6 billion in 1999 (equivalent to 0.5% of French GDP in 1999). Hollander et al. [62], also using the proxy good method, estimated the value of informal caregiving in Canada to be CAN$17 billion in 2007 (equivalent to 1.1% of Canadian GDP). Oliva-Moreno et al. [63], using the opportunity cost, proxy good and contingent valuation methods, estimated the monetary value of informal care in Spain to range from €18.9 billion to €53.3 billion in 2008 (equivalent to 1.7–4.9% of Spanish GDP). The differences in the results of these four studies may be due to methodological issues and the different development of formal LTC systems among countries. In any case, even in those countries with more conservative figures, the monetary value of informal care reaches very high figures.
Second, the diseases that have a greater presence in estimating the costs of informal care are dementias, particularly Alzheimer’s disease, followed by other conditions that cause significant limitations on personal autonomy and thus a significant demand for care. It is interesting to note how important the presence of cancer is. Although we have no previous works for comparison, our impression is that its presence has clearly grown in recent years. By contrast, arthritis/osteoarthritis, a disease that by its very nature and its high prevalence limits the autonomy of a large number of people, is weakly represented.
While the US is the country with the most studies included in the review, Europe is the continent where the most studies on the cost of informal care have been carried out. Nevertheless, in Europe, there is no unique LTC model. While we can speak generically about different models (Nordic, Central European, Anglo-Saxon, Mediterranean) [64, 65], each country has its own cultural peculiarities, family traditions, levels of income per capita, etc., which means that LTC systems can present notable differences. This is reflected indirectly in the differences between countries in the time of care reported by carers and in the annual cost of informal care. The intensity of informal care (weekly hours of care) is probably inversely associated with the development of the LTC system of each country. Additionally, differences found in the unit costs among countries could be explained by the differences in income per capita and salaries, which determine the shadow price applied in each country, and by the social consideration of informal care among the countries.
Some relevant methodological aspects are not considered in many of the articles reviewed. For instance, it would be useful to disaggregate the time spent according to the valuation method used (time of paid work, domestic work and leisure, in the case of the opportunity cost approach, and care tasks, in the case of the proxy good method) and explicitly show the shadow price used in each of the disaggregated categories and the final unit cost of a standard hour of care. Another aspect to consider is whether the care time includes some sort of censorship (the carer’s maximum hours of care per day or per week) and, if so, what that censorship is and how it is applied. For example, it can be determined that a carer must have a minimum rest period per day (i.e. 8 h) [66–69]. Once the care tasks have been differentiated, if the number of hours of daily care exceeds 16 h (24 h minus 8 h of rest), then the excess care time can be detracted from the supervision task time because this is the type of task that occurs most often in situations of conjoint production [70]. In any case, to facilitate comparability among studies, it is recommended to show disaggregated time before and after applying care limits on daily, weekly or monthly bases.
Another interesting aspect found during the review was the nonexistence of the use of the diary method to reveal care time. Despite its potential advantages [10, 45], the diary method is time intensive and requires a high degree of motivation among carers to ensure good compliance. These elements may be why researchers opt for simpler methods without having to face sampling losses, such as the recall method or even direct questions about care time. In this sense, there is an important field of research to develop for analysing whether the valuation method chosen influences the care times declared. For instance, van den Berg and Spauwen [47] compared the application of the opportunity cost and proxy good methods to determine a monetary value of informal care. The authors concluded that the two methods did not differ greatly with respect to the valuation step; the differences were small or explained by the relatively low cost of housework in the case of the proxy good method. However, the measurement step seemed to be more problematic; the opportunity cost and proxy good methods yielded considerably different results in terms of care-time estimations.
Considering the valuation methods, the opportunity cost method (69%) and the proxy good method (27%) were the most frequently used approaches (with 8% of studies combining several methods in the main analysis). In general, determining the value of care time is a complex task, from both theoretical and applied perspectives. Our work aims to be a snapshot of the methods and variations observed in cost-of-illness studies carried out over the last decade. There are other relevant works that have not focused on estimating the cost of informal care for a particular disease, and they have therefore not been included in our review. However, they have studied different methodological approaches in assessing the care time, in valuating different tasks and in assessing the care time spent by different agents (caregivers, non-caregivers, care recipients). These papers have analysed the feasibility of using contingent valuation (CV) [50] and well-being methods to valuate informal care [51], the differences between willingness to pay (WTP) and willingness to accept (WTA) values in caregivers and care recipients [52], the application of the conjoint measurement method to determine a monetary value of informal care [53, 54], the use of a discrete choice experiment to valuate informal care tasks [55] and the feasibility of deriving a monetary valuation for informal care from the preferences of non-carers [56].
In our review, we also found studies that applied more than one valuation technique in the main analysis [68, 71–76]. These works are relevant because performing different estimations is interesting not only from a methodological point of view but also for decision makers. For all articles reviewed, the hourly unit costs used under the opportunity cost method were lower compared with those used under the proxy good method (on average €10.14 vs €14.86). In principle, it could be expected that the unit cost of the time of informal care was greater when applying the opportunity cost method than when applying the replacement cost method. However, it should be noted that applying the opportunity cost approach led to several shadow prices: assessment of lost work time (high), time valuation of domestic work (low) and assessment of leisure time (low and in many studies the same value as for domestic work). Instead, the proxy good method often used a weighted average value corresponding to personal services and domestic tasks. Some studies distinguished between different tasks, and it was possible to impute a different value per task, but usually, the same value was used for all time spent providing care.
As noted in the introduction, most OECD countries are moving towards a model of shared responsibility in caring for people with limited autonomy. Thus, the identification, measurement and valuation of informal care are very relevant but do not necessarily imply that informal care will be completely replaced by formal care. In fact, although the literature on the relationship between formal and informal care is growing, the number of works that explore this relationship is still limited. There are different hypotheses to explain the relationship between formal and informal care [15]. According to the compensatory model, caregivers turn to formal care as a last resort once other possibilities have been exhausted. The substitution effect model supports the idea that informal and formal care are substitute goods in most cases. The complementary model proposes that professional formal care supports informal care without actually replacing it. Task-specific models note that the nature of a task determines the type of care provision (formal care is used for more complex tasks or those that require more specialised attention, while informal care is more focused on affective support, supervision and day-to-day care). Recently published papers suggest that there is not a dominant model [15, 77–87]. Thus, substituting formal for informal care when needs are growing does not entail fewer interventions from informal carers (in terms of frequency) than previously. For instance, Lee and Kim [82] found that family health care has a large substitute effect for diabetics and there is also weak evidence that informal family health care has substitute effects for high blood pressure and mental illnesses. Therefore, the nature of the relationship between formal and informal care will be determined by the disease that instigates the need for care, the disease severity, the type of care and tasks that the dependent person requires, the level of training of the carer, the family relationship with the carer, family income, and sociocultural elements.
As Arno et al. noted in their paper, “Imputing an economic value to the extraordinary level of caregiving described in this study does not detract from the emotional, cultural, and societal values expressed through informal caregiving. On the contrary, it enhances their importance by providing a tangible measure of the vast but vulnerable base upon which our chronic care system rests” [88]. Family support and informal care should be regarded as a fundamental part of the LTC system [89]. Informal care in the future will remain a cornerstone in the care of dependents and, therefore, an important part of the social costs associated with certain diseases [90]. The challenge is to improve the coordination among health systems, social care systems and households, with the aim of attaining an efficient and equitable allocation of resources to improve citizens’ well-being [91]. As Nolte and Pitchforth noted, “the rising burden of chronic disease and of the number of people with complex care needs require the development of delivery systems that bring together a range of professionals and skills from both the cure (health care) and care (long-term and social-care) sectors” [92]. In this context, it is expected that public authorities will adopt or expand specific strategies and measures for the support of informal carers, such as information, training, education, housing adaptation, technical supplies, respite care, psychological support, flexible working arrangements, benefits, and a higher provision of formal care [11, 93]. However, we need many more valuations of these types of programmes as well as evidence of the economic and social impacts of integrated care.
Some of the results of our review are comparable with those obtained in the reviews of economic valuations performed by Goodrich et al. [35] and Krol et al. [34]. Informal care is not consistently included in the economic studies, and there is a need for greater transparency and clarity in their methods and results. From our point of view, this involves minimal recommendations for authors of studies that include informal care costs in their analyses. (1) Clearly indicate whether the collection of information is prospective or retrospective; (2) clearly indicate how time of care is revealed (collection method); (3) provide more detailed information on the different tasks of care; (4) explicitly state the time of care (total and for each task); (5) explicitly state the unit value of time of care (for each task and the weighted shadow price for total care); (6) differentiate whether time of care refers to the primary caregiver or includes others caregivers (display the time of care performing tasks for main and other caregivers); (7) if there were a censorship in time of care, clearly indicate the maximum time of daily care considered; (8) if possible, differentiate by the degree of severity of illness or disability/dependence of the sample considered. We cannot indicate which valuation method is the most appropriate. Each of the three main methods (opportunity cost, proxy good and contingent valuation) has advantages and limitations. Additionally, there are new methods that have been applied experimentally [50, 55] but in the future may have greater empirical applications. We can suggest that, where feasible, (9) researchers should use more than one method of valuation to facilitate comparability of studies and increase the usefulness of the analysis for decision makers.
Our systematic literature review used three databases: MEDLINE (PubMed), NHS EED and Econlit [94]. MEDLINE was selected as one of the main major biomedical databases used in this field to conduct systematic literature reviews. Although we are conscious that EMBASE is also another main database, because of resource restrictions and recommendations for using MEDLINE instead of EMBASE [95, 96], we ended up using MEDLINE. Other previous work [97] has shown that very few additional-costs studies are found in EMBASE compared with a search of MEDLINE, while a number of papers may in fact be lost if EMBASE were to be substituted for MEDLINE. The NHS EED database was used because of claims that it complements main search engines such as MEDLINE [98]. We have tried to adopt a reasonably broad coverage of grey literature and have examined a number of different databases. For these reasons we are confident in that we have incorporated the most relevant studies on the topic.
Because of flaws in the design and execution of this systematic literature review, there is a risk of a systematic deviation from the truth (i.e. overestimating or underestimating the true treatment effect). In this case, there is a risk of overestimating the results knowing that researchers will only publish those informal care costs that show a relevant monetary magnitude, and those informal care costs that are not relevant or significant will not be published. We cannot really assess the risk of individual bias because no study has been studying those. However, most studies have been using primary data for the cost calculation and reporting uncertainty information such as the standard deviation of the 95% confidence interval. So, even though there is a risk of bias for overestimating the results, we have reported uncertainty measures to try to inform the reader on the magnitude of this bias.
It should be noted that our review focused on the valuation of informal care time. However, there are other non-monetary costs related to informal caregiving that were not included in the articles selected, such as the excessive burden suffered by caregivers, represented in terms of health, professional or social problems, and the monetary cost associated with the activities of carers (including travelling, parking, meals, accommodation, housing adaptations, costs of prostheses and devices, etc.) that are very rarely referred to in studies on informal care [99].
Our results suggest that any program, strategy or policy of health promotion and care for people with limited autonomy cannot overlook the importance of informal support networks. Taking into consideration that informal caregiving has a very significant economic impact on total costs, identifying and evaluating the relevance of informal care in the economic impact of some chronic diseases should be considered as a fundamental priority for policy makers and for society as a whole. Theoretical and empirical advances should be applied for better identification of informal care time, for revealing different care tasks and for the proper assessment of caregiving time. Additionally, bearing in mind that the value of informal caregiving can be reflected not only by monetary valuations (as shown this review) but also by the burden of care caused by excessive intensity in the care provided, there is a latent need for surveys performed at national and international levels. Thus, enhancing the method of collecting information, in terms of the time devoted to care, the burden of care, caregivers’ problems in different dimensions (health, work, social) and positive aspects of care for both care recipients and carers [19–21, 100–102], would help reveal the real value associated with informal care. All in all, improvements in the data and methods applied in cost-of-illness studies and greater transparency in the methodology and results of these analyses will, first, promote the comparability of informal care value among different countries and different chronic diseases and, second, help in the design and valuation of social and healthcare policies.
An integral approach to the care of chronic patients should include the role and the needs of caregivers, reveal their value and promote their social recognition. These are necessary steps to improve coordination between the healthcare system, LTC system and households to attain an efficient and equitable allocation of available resources. The final aim is to contribute to the sustainability of the healthcare and LTC systems while improving citizens’ well-being.
References
World Health Organization. Health and ageing: a discussion paper. Geneva: World Health Organization, Department of Health Promotion, Non-Communicable Disease Prevention and Surveillance; 2001.
Commission European. Healthy ageing: keystone for a sustainable Europe. Brussels: European Commission; 2007.
Kendig H, Phillipson C. Building age-friendly communities: new approaches to challenging health and social inequalities. “If you could do one thing” Nine local actions to reduce health inequalities. London: The British Academy; 2014. p. 102–11.
Iezzoni LI. Policy concerns raised by the growing U.S. population aging with disability. Disabil Health J. 2014;7(1 Suppl):S64–8.
Midtsundstad T, Bogen H. Active Aging policies between individual needs and collective goods. A study of active aging policies and practices in Norway. Nordic J Work Life Stud. 2014;4(2):139–58.
Buffel T, McGarry P, Phillipson C, De Donder L, Dury S, De Witte N, et al. Developing age-friendly cities: case studies from Brussels and Manchester and implications for policy and practice. J Aging Soc Policy. 2014;26(1–2):52–72.
Commission European. The 2015 Ageing Report. Directorate-General for Economic and Financial Affairs: Underlying Assumptions and Projection Methodologies. European Commission; 2014.
Lafortune G, Balestat G. Trends in Severe Disability Among Elderly People: Assessing the Evidence in 12 OECD Countries and the Future Implications. Paris: OECD Publishing; 2007. OECD Health Working Papers, No. 26.
Pickard L, King D. Informal care supply and demand in Europe. In: Geerts. J, Willeme P, Mot E, editors. Long-term care use and supply in Europe: projections for Germany, the Netherlands, Spain and Poland. Brussels: European Network of Economic Policy Research Institutes (ENEPRI) Research Report 116; 2012. p. 114–23.
van den Berg B, Brouwer WB, Koopmanschap MA. Economic valuation of informal care. An overview of methods and applications. Eur J Health Econ. 2004;5(1):36–45.
Courtin E, Jemiai N, Mossialos E. Mapping support policies for informal carers across the European Union. Health Policy. 2014;118(1):84–94.
Triantafillou J, Naiditch M, Repkova K, Stiehr K, Carretero S, Emilsson T, et al. Informal care in the long-term care system. European Overview Paper. Athens: Health systems and long-term care for older people in Europe—INTERLINKS Project; 2010.
van Exel J, Bobinac A, Koopmanschap M, Brouwer W. The invisible hands made visible: recognizing the value of informal care in healthcare decision-making. Expert Rev Pharmacoecon Outcomes Res. 2008;8(6):557–61.
van Exel NJ, Brouwer WB, van den Berg B, Koopmanschap M, van den Bos GA. What really matters: an inquiry into the relative importance of dimensions of informal caregiver burden. Clin Rehabil. 2004;18(6):683–93.
Jimenez-Martin S, Prieto CV. The trade-off between formal and informal care in Spain. Eur J Health Econ. 2012;13(4):461–90.
Bauer JM, Sousa-Poza A. Impacts of Informal Caregiving on Caregiver Employment, Health, and Family. J Popul Ageing. 2015;8(3):113–45.
Schulz R, Beach SR. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA. 1999;282(23):2215–9.
Cohen CA, Colantonio A, Vernich L. Positive aspects of caregiving: rounding out the caregiver experience. Int J Geriatr Psychiatry. 2002;17:184–8.
Brouwer W, Van Exel J, Van Den Berg B, et al. Process utility from providing informal care: the benefit of caring. Health Policy. 2005;74:85–99.
Beach S, Schulz R, Yee J, Jackson S. Negative and positive health effects of caring for a disabled spouse: longitudinal findings from the caregiver health effects study. Psychol Aging. 2000;15:259–71.
Al-Janabi H, Coast J, Flynn T. What do people value when they provide unpaid care to an older person? A meta-ethnography with interview follow-up. Soc Sci Med. 2008;67:111–21.
Michael F. Drummond, Mark J. Sculpher, Karl Claxton, Greg L. Stoddart, and George W. Torrance. Methods for the economic evaluation of health care programmes. Fourth Edition. Oxford University Press. 2015.
Costa N, Ferlicoq L, Derumeaux-Burel H, Rapp T, Garnault V, Gillette-Guyonnet S, et al. Comparison of informal care time and costs in different age-related dementias: a review. Biomed Res Int. 2013;2013:852368.
Joo H, George MG, Fang J, Wang G. A literature review of indirect costs associated with stroke. J Stroke Cerebrovasc Dis. 2014;23(7):1753–63.
Pares-Badell O, Barbaglia G, Jerinic P, Gustavsson A, Salvador-Carulla L, Alonso J. Cost of disorders of the brain in Spain. PLoS One. 2014;9(8):e105471.
Phillipson L, Magee C, Jones SC. Why carers of people with dementia do not utilise out-of-home respite services. Health Soc Care Community. 2013;21(4):411–22.
Quentin W, Riedel-Heller SG, Luppa M, Rudolph A, Konig HH. Cost-of-illness studies of dementia: a systematic review focusing on stage dependency of costs. Acta Psychiatr Scand. 2010;121(4):243–59.
Russell LB. Completing costs: patients’ time. Med Care. 2009;47(7 Suppl 1):S89–93.
Schaller S, Mauskopf J, Kriza C, Wahlster P, Kolominsky-Rabas PL. The main cost drivers in dementia: a systematic review. Int J Geriatr Psychiatry. 2015;30(2):111–29.
Wineland AM, Stack BC Jr. Modern methods to predict costs for the treatment and management of head and neck cancer patients: examples of methods used in the current literature. Curr Opin Otolaryngol Head Neck Surg. 2008;16(2):113–6.
Heintz E, Gerber-Grote A, Ghabri S, Hamers FF, Rupel VP, Slabe-Erker R, et al. Is there a European view on health economic evaluations? Results from a synopsis of methodological guidelines used in the EUnetHTA partner countries. Pharmacoeconomics. 2016;34(1):59–76.
Jonsson B. Ten arguments for a societal perspective in the economic evaluation of medical innovations. Eur J Health Econ. 2009;10(4):357–9.
Krol M, Papenburg J, Tan SS, Brouwer W, Hakkaart L. A noticeable difference? Productivity costs related to paid and unpaid work in economic evaluations on expensive drugs. Eur J Health Econ. 2016;17(4):391–402.
Krol M, Papenburg J, van Exel J. Does including informal care in economic evaluations matter? A systematic review of inclusion and impact of informal care in cost-effectiveness studies. Pharmacoeconomics. 2015;33(2):123–35.
Goodrich K, Kaambwa B, Al-Janabi H. The inclusion of informal care in applied economic evaluation: a review. Value Health. 2012;15(6):975–81.
Koopmanschap MA, van Ineveld BM. Towards a new approach for estimating indirect costs of disease. Soc Sci Med. 1992;34(9):1005–10.
Liljas B. How to calculate indirect costs in economic evaluations. Pharmacoeconomics. 1998;13(1 Pt 1):1–7.
Krol M, Brouwer W, Rutten F. Productivity costs in economic evaluations: past, present, future. Pharmacoeconomics. 2013;31(7):537–49.
Lensberg BR, Drummond MF, Danchenko N, Despiegel N, Francois C. Challenges in measuring and valuing productivity costs, and their relevance in mood disorders. Clinicoecon Outcomes Res. 2013;5:565–73.
Oliva J, Lobo F, Lopez-Bastida J, Zozaya N, Romay R. Indirect costs of cervical and breast cancers in Spain. Eur J Health Econ. 2005;6(4):309–13.
Lofland JH, Locklear JC, Frick KD. Different approaches to valuing the lost productivity of patients with migraine. Pharmacoeconomics. 2001;19(9):917–25.
Nicholson S, Pauly MV, Polsky D, Sharda C, Szrek H, Berger ML. Measuring the effects of work loss on productivity with team production. Health Econ. 2006;15(2):111–23.
Tilling C, Krol M, Tsuchiya A, Brazier J, Brouwer W. In or out? Income losses in health state valuations: a review. Value Health. 2010;13(2):298–305.
Nyman JA. Productivity costs revisited: toward a new US policy. Health Econ. 2012;21(12):1387–401.
Hoefman RJ, van Exel J, Brouwer W. How to include informal care in economic evaluations. Pharmacoeconomics. 2013;31(12):1105–19.
Koopmanschap MA, van Exel JN, van den Berg B, Brouwer WB. An overview of methods and applications to value informal care in economic evaluations of healthcare. Pharmacoeconomics. 2008;26(4):269–80.
van den Berg B, Spauwen P. Measurement of informal care: an empirical study into the valid measurement of time spent on informal caregiving. Health Econ. 2006;15(5):447–60.
van den Berg B, Brouwer W, van Exel J, Koopmanschap M. Economic valuation of informal care: the contingent valuation method applied to informal caregiving. Health Econ. 2005;14(2):169–83.
van den Berg B, Brouwer W, van Exel J, Koopmanschap M, van den Bos GA, Rutten F. Economic valuation of informal care: lessons from the application of the opportunity costs and proxy good methods. Soc Sci Med. 2006;62(4):835–45.
van den Berg B, Bleichrodt H, Eeckhoudt L. The economic value of informal care: a study of informal caregivers’ and patients’ willingness to pay and willingness to accept for informal care. Health Econ. 2005;14(4):363–76.
van den Berg B, Ferrer ICA. Monetary valuation of informal care: the well-being valuation method. Health Econ. 2007;16(11):1227–44.
de Meijer C, Brouwer W, Koopmanschap M, van den Berg B, van Exel J. The value of informal care–a further investigation of the feasibility of contingent valuation in informal caregivers. Health Econ. 2010;19(7):755–71.
van den Berg B, Al M, Brouwer W, van Exel J, Koopmanschap M. Economic valuation of informal care: the conjoint measurement method applied to informal caregiving. Soc Sci Med. 2005;61(6):1342–55.
van den Berg B, Al M, van Exel J, Koopmanschap M, Brouwer W. Economic valuation of informal care: conjoint analysis applied in a heterogeneous population of informal caregivers. Value Health. 2008;11(7):1041–50.
Mentzakis E, Ryan M, McNamee P. Using discrete choice experiments to value informal care tasks: exploring preference heterogeneity. Health Econ. 2011;20(8):930–44.
Garrido-Garcia S, Sanchez-Martinez FI, Abellan-Perpinan JM, van Exel J. Monetary valuation of informal care based on carers’ and noncarers’ preferences. Value Health. 2015;18(6):832–40.
Moher D, Liberati A, Tetzlaff J, Altman DG. The PRISMA Group. preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
International Monetary Fund. World Economic Outlook Database [Internet] Washington: International Monetary Fund; 2015 [cited 2016 Jan Feb]. Available from: https://www.imf.org/external/pubs/ft/weo/2015/02/weodata/index.aspx.
Centers for Disease Control and Prevention. Division for Heart Disease and Stroke Prevention. Five-Part Webcast on Economic Evaluation. Glossary of terms. Available from: https://www.cdc.gov/dhdsp/programs/spha/economic_evaluation/docs/economic_evaluation_glossary.pdf.
Chari AV, Engberg J, Ray KN, Mehrotra A. The opportunity costs of informal elder-care in the United States: new estimates from the american time use survey. Health Serv Res. 2015;50(3):871–82.
Paraponaris A, Davin B, Verger P. Formal and informal care for disabled elderly living in the community: an appraisal of French care composition and costs. Eur J Health Econ. 2012;13(3):327–36.
Hollander MJ, Liu G, Chappell NL. Who cares and how much? The imputed economic contribution to the Canadian healthcare system of middle-aged and older unpaid caregivers providing care to the elderly. Healthc Q. 2009;12(2):42–9.
Oliva-Moreno J, Peña-Longobardo LM, Vilaplana-Prieto C. An estimation of the value of informal care provided to dependent people in Spain. Appl Health Econ Health Policy. 2015;13(2):223–31.
Carrera F, Pavolini E, Ranci C, Sabbatini A. Long-term care systems in comparative perspective: Care needs, informal and formal coverage, and social impacts in European countries. In: Pavolini E, Ranci C, editors. Reforms in long-term care policies in Europe: Investigating Institutional Change and Social Impacts. New York: Springer-Verlag New York; 2013. p. 23–52.
Costa-Font J, Zigante V. Long Term Care Coverage in Europe: A Case for ‘Implicit Insurance Partnerships’. London: The London School of Economics and Political Science; 2014. LSE Health Working Paper, No. 37.
Neubauer S, Holle R, Menn P, Grossfeld-Schmitz M, Graesel E. Measurement of informal care time in a study of patients with dementia. Int Psychogeriatr. 2008;20(6):1160–76.
Trepel D. Informal cost of dementia care- a proxy-good valuation in Ireland. Econ Soc Rev (Irel). 2011;42(4):479–503.
Peña-Longobardo LM, Oliva-Moreno J. Economic valuation and determinants of informal care to people with Alzheimer’s disease. Eur J Health Econ. 2015;16(5):507–15.
Yabroff KR, Kim Y. Time costs associated with informal caregiving for cancer survivors. Cancer. 2009;115(18 Suppl):4362–73.
Albrecht D, Wollensak T, Ernst C, Becker C, Hautzinger M, Pfeiffer K. Costs of informal care in a sample of German geriatric stroke survivors. Eur J Ageing. 2016;13(1):49–61.
Hanly P, Ceilleachair AO, Skally M, O’Leary E, Staines A, Kapur K, et al. Time costs associated with informal care for colorectal cancer: an investigation of the impact of alternative valuation methods. Appl Health Econ Health Policy. 2013;11(3):193–203.
Hurd MD, Martorell P, Delavande A, Mullen KJ, Langa KM. Monetary costs of dementia in the United States. N Engl J Med. 2013;368(14):1326–34.
Gerves C, Chauvin P, Bellanger MM. Evaluation of full costs of care for patients with Alzheimer’s disease in France: the predominant role of informal care. Health Policy. 2014;116(1):114–22.
Wimo A, Reed CC, Dodel R, Belger M, Jones RW, Happich M, et al. The GERAS Study: a prospective observational study of costs and resource use in community dwellers with Alzheimer’s disease in three European countries–study design and baseline findings. J Alzheimers Dis. 2013;36(2):385–99.
Wolff N, Perlick DA, Kaczynski R, Calabrese J, Nierenberg A, Miklowitz DJ. Modeling costs and burden of informal caregiving for persons with bipolar disorder. J Ment Health Policy Econ. 2006;9(2):99–110.
Wubker A, Zwakhalen SM, Challis D, Suhonen R, Karlsson S, Zabalegui A, et al. Costs of care for people with dementia just before and after nursing home placement: primary data from eight European countries. Eur J Health Econ. 2015;16(7):689–707.
Bolin K, Lindgren B, Lundborg P. Informal and formal care among single-living elderly in Europe. Health Econ. 2008;17(3):393–409.
Chappell N, Blandford A. Informal and formal care: exploring the complementarity. Ageing Soc. 1991;11(03):299–317.
Denton M. The linkages between informal and formal care of the elderly. Can J Aging. 1997;16(01):30–50.
Greene VL. Substitution between formally and informally provided care for the impaired elderly in the community. Med Care. 1983:609–19.
Kehusmaa S, Autti-Ramo I, Helenius H, Rissanen P. Does informal care reduce public care expenditure on elderly care? Estimates based on Finland’s Age Study. BMC Health Serv Res. 2013;13:317.
Lee MJ, Kim YS. Zero-inflated endogenous count in censored model: effects of informal family care on formal health care. Health Econ. 2012;21(9):1119–33.
Litwak E. Helping the elderly: the complementary roles of informal networks & formal systems. New York: The Guilford Press; 1985.
Mentzakis E, McNamee P, Ryan M. Who cares and how much: exploring the determinants of co-residential informal care. Rev Econ Househ. 2009;7(3):283–303.
Moscovice I, Davidson G, McCaffrey D. Substitution of formal and informal care for the community-based elderly. Med Care. 1988;26(10):971–81.
Muramatsu N, Campbell RT. State expenditures on home and community based services and use of formal and informal personal assistance: a multilevel analysis. J Health Soc Behav. 2002;43(1):107–24.
Van Houtven CH, Norton EC. Informal care and health care use of older adults. J Health Econ. 2004;23(6):1159–80.
Arno PS, Levine C, Memmott MM. The economic value of informal caregiving. Health Aff (Millwood). 1999;18(2):182–8.
Saltman RB, Dubois HF, Chawla M. The impact of aging on long-term care in Europe and some potential policy responses. Int J Health Serv. 2006;36(4):719–46.
Fujisawa R, Colombo F. The Long-Term Care Workforce: overview and strategies to adapt supply to a growing demand. Paris: OECD Publishing; 2009. OECD Health Working Papers, No. 44.
Fernandez JL, Forder J, Trukeschitz B, Rokasova M, McDaid D. How can European states design efficient, equitable and sustainable funding systems for long-term care for older people? Copenhagen: WHO Regional Office for Europe; 2009. European Observatory on Health Systems and Policies. Policy Brief, No. 11.
Nolte H, Pitchforth E. What is the evidence on the economic impacts of integrated care? Copenhagen: WHO Regional Office for Europe; 2014. European Observatory on Health Systems and Policies. Policy Summary, No. 11.
Viitanen TK. Informal and Formal Care in Europe. Bonn: IZA, Institute for the Study of Labor; 2007. Discussion Paper Series, No. 2648.
Glanville J, Paisley S. Searching for evidence on resource use, costs, effects and cost-effectiveness. In: Shemilt I et al (editors) Evidence based economics. Oxford: Wiley-Blackwell;2010.
McKinlay RJ, Wilczynski NL, Haynes RB, the Hedges Team. Optimal search strategies for detecting cost and economic studies in EMBASE. BMC Health Serv Res 2006;6:67.
Coyle KB, Trochlil K, Iversen P. MEDLINE and EMBASE for health economic literature reviews [abstract]. Value Health. 2012;15(4):A162.
Sassi F, Archard L. McDaid d. Searching literature databases for health care economic evaluations: how systematic can we afford to be? Med Care. 2002;40(5):387–94.
Shemilt I, Mugford M, Vale L, Craig D. Searching NHS EED and HEED to inform development of economic commentary for Cochrane intervention reviews. Oxford: Cochrane Collaboration; 2011.
Hanly P, Ceilleachair AO, Skally M, O’Leary E, Kapur K, Fitzpatrick P, et al. How much does it cost to care for survivors of colorectal cancer? Caregiver’s time, travel and out-of-pocket costs. Support Care Cancer. 2013;21(9):2583–92.
Boyd KJ, Murray SA, Kendall M, Worth A, Frederick Benton T, Clausen H. Living with advanced heart failure: a prospective, community based study of patients and their carers. Eur J Heart Fail. 2004;6(5):585–91.
Hamalainen H, Smith R, Puukka P, Lind J, Kallio V, Kuttila K, et al. Social support and physical and psychological recovery one year after myocardial infarction or coronary artery bypass surgery. Scand J Public Health. 2000;28(1):62–70.
Haley WE, Allen JY, Grant JS, Clay OJ, Perkins M, Roth DL. Problems and benefits reported by stroke family caregivers: results from a prospective epidemiological study. Stroke. 2009;40(6):2129–33.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This work was funded by the Spanish Ministry of Economy and Competitiveness under the “Programa Estatal de Investigación, Desarrollo e Innovación Orientada a los Retos de la Sociedad, Plan Estatal de Investigación Científica Técnica y de Innovación 2013–2016” programme. Research project references: ECO2013-48217-C2-1 and ECON2013-48217-C2-2-R (http://invesfeps.ulpgc.es/en). The funder had no influence over the conducting of this study or the drafting of this manuscript. No conflicts exist for Juan Oliva-Moreno, Marta Trapero-Bertran, Luz Maria Peña-Longobardo and Raúl del Pozo-Rubio. We are also grateful to the two anonymous reviewers and the editor for their helpful comments.
Author Contributions
JOM designed and managed the study. MTB carried out the systematic literature review. All authors (JOM, MTB, LPL and RPR) have reviewed, summarised and extracted information articles included in the review. JOM, MTB and LPL have contributed in writing the first draft of the manuscript. All the authors have provided input on multiple drafts of the manuscript and approval of the final version.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Oliva-Moreno, J., Trapero-Bertran, M., Peña-Longobardo, L.M. et al. The Valuation of Informal Care in Cost-of-Illness Studies: A Systematic Review. PharmacoEconomics 35, 331–345 (2017). https://doi.org/10.1007/s40273-016-0468-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-016-0468-y