Abstract
Background
Previously developed models in ophthalmology have generally used a Markovian structure. There are a number of limitations with this approach, most notably the ability to base patient outcomes on best-corrected visual acuity (BCVA) in both eyes, which may be overcome using a different modelling structure. Simulation modelling allows for this to be modelled more precisely, and therefore may provide more accurate and relevant estimates of the cost effectiveness of ophthalmology interventions.
Objective
This study aimed to explore the appropriateness of simulation modelling in ophthalmology, using the disease area of wet age-related macular degeneration (wAMD) as an example.
Methods
A de novo economic model was built using a patient-level simulation, which compared ranibizumab with aflibercept in wAMD. Disease progression was measured using BCVA. Health-related quality of life (HRQoL) was estimated using a regression analysis linking BCVA in each eye to utility. The analysis was from the perspective of the National Health Service in the UK. Five different regression models were explored and were based on BCVA in either one eye or both eyes.
Results
The model outputs provide some evidence to support the hypothesis that the analyses using the two-eye models for estimating HRQoL generate a more accurate estimation of incremental quality-adjusted life-years (QALYs) associated with the positive treatment effect for ranibizumab versus aflibercept. Second-order analysis broadly supported these findings, and showed that the variation in incremental costs was slightly lower than in incremental QALYs. The second-order analysis estimated similar incremental costs and a greater overall variation in incremental QALYs than the first-order analysis, suggesting important non-linearities within the model.
Conclusions
This analysis suggests that patient-level simulation models may be well suited to representing the real-world patient pathway in wAMD, particularly when aspects of disease progression cannot be adequately captured using a Markov structure. The benefits of a simulation approach can be demonstrated in the modelling of HRQoL as a function of BCVA in both eyes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Patient-level simulation modelling may be a technique well-suited to representing the patient pathway and disease progression in ophthalmology. |
An analysis of two NICE-approved treatments for wet age-related macular degeneration provides an example of the benefits of simulation modelling over cohort (Markov) modelling in this disease area. |
1 Introduction
1.1 Background
To date, many economic models for evaluating interventions in ophthalmology conditions, such as wet age-related macular degeneration (wAMD), retinal vein occlusion, diabetic macular oedema (DMO) and pathologic myopia, have followed a Markov structure, in which patients or populations can move between defined health states over successive time periods or cycles. Reviews of cost-effectiveness evidence are undertaken as part of National Institute for Health and Care Excellence (NICE) technology appraisals, which demonstrate that the majority of previously conducted analyses used a cohort framework [1–7]. In ophthalmology, health states are typically based on best corrected visual acuity (BCVA), as measured in clinical trials, with improvement of BCVA a key goal of treatment. BCVA differs in both eyes at different time points, and has further been shown to be a determinant of health-related quality of life (HRQoL), with severe visual impairment associated with excess mortality [23]. Current cohort modelling methods may restrict the ability to reflect the BCVA change in both eyes at different time points. This is related to the memoryless nature of Markov modelling, and to the necessity to construct discrete health states for each event or combination of events. Markov models do not have the ability to retain memory of a patient’s previous health states without the introduction of additional health states or tunnel states, and so lack the ability to effectively incorporate the development of bilateral involvement. Moreover, incorporating treatment switch or treatment discontinuation without the addition of more health states limits the applicability of the cohort models. Models which attempt to model both eyes explicitly are typically associated with a large number of health states, even without the incorporation of any tunnel states to capture these aspects of the treatment pathway [1, 2].
Due to these limitations of a cohort model, a patient-level simulation approach may be considered a suitable alternative. This allows for modelling a single patient at a time, generating clinical events and treatment switches according to the treatment status in both the eyes independently, and the time from the start of treatment. It also allows for the occurrence of any number of events such as changes in BCVA over time in each eye, fellow-eye involvement, and improvement in HRQoL as a function of BCVA in both eyes. Recurrence could also be modelled based on a known prognostic variable a priori due to the ability of a simulation model to capture patient history. The major difference compared with cohort models is the absence of defined health states and the ability to model both eyes explicitly.
1.2 Study Objectives
In this study, wAMD has been used as an example to illustrate the points highlighted above. There are two intravitreal VEGF inhibitors currently licensed in Europe and approved by NICE for the treatment of wAMD in the UK: ranibizumab (Lucentis®, Genentech Inc./Novartis) and aflibercept (Eylea®, Bayer plc) [8, 9]. When conceptualising the economic analysis, previous technology appraisals undertaken by NICE were evaluated, specifically considering the modelling methods used and the critique by the Evidence Review Group (ERG) [1–3]. Historically, manufacturer models have explicitly assumed that only the better-seeing eye (BSE) was treated, even though the clinical data on which the model was based were drawn predominately from people whose worse-seeing eye (WSE) had been treated. Subsequent models attempted to incorporate WSE data in a limited capacity. Analyses based on either the BSE or WSE alone have been demonstrated to produce different model outcomes (such as quality-adjusted life-year [QALY] gains), partly because HRQoL of people with visual impairment is associated primarily with vision in the BSE [10, 11]. This is a major limitation in ophthalmology models, as improvements in patients’ vision function and HRQoL are recognised as the most important outcomes of any ophthalmology treatment. It can be expected that models based on one eye only will systematically underestimate the potential QALY gains associated with treatment. Disease activity can manifest in either the BSE or the WSE (or indeed both), and an analysis linking HRQoL to visual acuity (VA) in only one of these eyes will only capture the QALY gains associated with improvement in VA if the utility model corresponds to the eye that is being treated.
The objective of this study was to develop a patient-level simulation model to address the limitations mentioned above, with the purpose of informing the optimal approach to modelling cost effectiveness in ophthalmology submissions to Health Technology Assessment (HTA) bodies such as NICE.
2 Methods
2.1 Overview
The analysis assessed the cost effectiveness of two treatments for wAMD (ranibizumab and aflibercept), which were both assumed to be administered via a pro re nata (PRN) dosing schedule. Outcomes were assessed in a population representative of those with wAMD, with baseline characteristics based on patients in the Extremity Constraint Induced Therapy Evaluation (EXCITE) clinical trial [12]. Costs were assessed from the perspective of the National Healthcare Service (NHS) and personal social services (PSS) in the UK. The model was designed to capture both first-order (individual patient) and second-order (parameter) uncertainty [37].
Disease progression in wAMD can be characterised by deterioration in vision in the affected eye. A proportion of patients will experience the disease in both their eyes. Within the model, BCVA (as assessed by number of letters read on an Early Treatment Diabetic Retinopathy Study [ETDRS] visual acuity chart) was used as a marker of disease progression. This measure ranges from 0 to 100, with 0 being completely blind and 100 being perfect vision. Change in BCVA was modelled independently in each eye, including when the patient had bilateral disease and was treated in both eyes.
The response to treatment and ongoing impact on disease activity can be characterised by an initial response to treatment, followed by a period of disease stabilisation. After this, vision has been demonstrated to deteriorate gradually over time. As such, disease progression was modelled in several stages. Discontinuation of active treatment can occur in a small proportion of patients due to persistent deterioration in visual acuity, or an inadequate response to treatment.
2.2 Modelling Approach
Within this analysis, a patient-level simulation model was developed. A decision-analytic model was developed in Microsoft Excel 2010®. Figure 1a, b present a diagrammatical representation of the model flow.
Model schematic—disease progression in affected eye(s) and impact of BCVA on patient outcomes. a A diagrammatical representation of the flow of a patient through the model. b A representation of how the patient’s disease pathway (as measured by BCVA) is linked to other model outcomes (including discontinuation, mortality, costs and quality of life). BCVA best-corrected visual acuity, FE fellow eye, QALY quality-adjusted life year, SE study eye
The procedure by which the model run was performed is as follows: (1) a patient was drawn at random from a pool of patient-level baseline characteristics; (2) the change in BCVA for this patient was evaluated in each model arm at each monthly cycle; (3) costs and QALYs were assigned to the patient; (4) a new patient was drawn from the original pool and the process from (1) to (3) repeated; (5) the mean costs and QALYs were estimated for the cohort. Patients with an unaffected fellow eye were assumed to have a probability of the fellow eye becoming affected [13]. The presence of bilateral disease was identified at the start of the cycle, and then BCVA change was estimated for the fellow eye based on presence of disease. Costs and QALYs were assigned as a patient entered the health state. Half-cycle correction was not applied to model outcomes: given the short cycle length, this was felt to have a negligible impact on the results.
Patients were assumed to receive either ranibizumab or aflibercept over a maximum of 5 years, although the model continued to assess outcomes over the patient’s lifetime.
Outcomes were modelled over a remaining-lifetime time horizon. Following NICE recommendations, future costs and health outcomes were discounted at 3.5% per annum.
Whilst the focus of the study was not specifically to establish the relative cost effectiveness of each intervention, efforts were made to ensure that all model inputs and assumptions were suitable and clinically justifiable.
2.3 Patient Population
Baseline patient characteristics were based on patients in the EXCITE phase III study, a trial comparing two regimens of ranibizumab [12]. This study was considered reflective of the wAMD patient population and was one of the few studies with available data on BCVA in both eyes, rather than just the study eye. The starting characteristics of each patient being entered into the model simulation were assigned by randomly selecting actual individual patient records of baseline characteristics from EXCITE, in order to preserve realistic correlation between characteristics. In the trial, the mean starting age of patients was 76 years and the likelihood of bilateral disease at the start of the trial was 18.54%. Mean BCVA in the study eye and fellow eye were 56 and 55, respectively.
2.4 Model Parameters
2.4.1 Clinical Effectiveness
Disease progression was incorporated within the model as the mean change in BCVA per month. The use of a simulation model allowed for BCVA to be estimated directly as a continuous variable, rather than artificially dividing into a number of mutually exclusive health states (as would be the case if a cohort model, such as a Markov model, was adopted). This adds to the precision and granularity of change in BCVA compared with the Markov approach, where it is recommended to limit the number of health states used [14]. With a cohort model with discrete health states, in order to be able to include all viable study data, it would have been necessary to transform the data so that it measured the probability of achieving each health state in the model. This would require making assumptions about the data and would introduce additional uncertainty and potential errors. It would also diminish the viability of incorporating synthesised evidence from a network meta-analysis (NMA) with the same level of accuracy, due to additional assumptions needing to be made and not having access to patient-level data sets for all relevant comparators. The present approach circumvents this need by using the outcome from an NMA directly.
Disease progression was modelled in several stages. Monthly BCVA change for each comparator was estimated by a random draw from a normal distribution with a mean and standard deviation. The assumption of normality is supported by evidence from the clinical trials comparing ranibizumab with aflibercept [16]. For example, mean change in BCVA at 52 weeks in the ranibizumab arm of the VIEW 1 study (Vascular Endothelial Growth Factor [VEGF] Trap-Eye: Investigation of Efficacy and Safety in Wet Age-Related Macular Degeneration) is 8.1 letters with a standard deviation of 15.3 letters. If response was normally distributed, this would suggest that 32.6% of patients would experience an increase of 15 or more letters and 6.6% would experience a decline of more than 15 letters. These figures are in line with those reported in the study which reports that 30.9% of patients experienced an increase of 15 or more letters and 5.6% a decline of more than 15 letters. In the initial period up to 24 months, treatment response to ranibizumab was based on data from the IVAN study (Inhibition of VEGF in Age-Related Choroidal Neovascularisation; the discontinuous treatment arm) [15]. Patients in the IVAN trial had similar baseline characteristics to those used in the EXCITE study (mean age of 77.7 years); however, the mean BCVA in the study was slightly higher than that used in this analysis (mean BCVA of 61.4). The relative effectiveness of ranibizumab versus aflibercept was modelled using data from an NMA of randomised controlled trials [17] and was estimated for every month for 24 months using methods outlined in Ding and Fu [18]. The studies used to inform the NMA are provided in the electronic supplementary material (ESM) (Table S1). Details of the clinical effectiveness parameters are provided in the ESM (Table S2).
The model assumed that treatment response was independent over time, that is, treatment response in a given month was not correlated with treatment response in previous months. Where both eyes were affected, treatment response in each eye was modelled independently. It was assumed patients could discontinue treatment at any time in the 5-year period. Probabilities of discontinuation were based on a naïve comparison of the rate of withdrawal not due to death in the IVAN trial [15] for ranibizumab and the VIEW trial [19] for aflibercept.
Beyond 24 months and up to 60 months, BCVA was assumed to remain constant, an assumption validated and implemented within a previous NICE appraisal [1]. After this period or after treatment discontinuation, BCVA was modelled using natural history data for wAMD patients [20]. Vision loss in an unaffected eye was modelled using data on normal vision loss taken from a meta-analysis of data [21, 22].
Adverse events relating to treatment were excluded from the analysis. These were considered to be equivalent between treatment arms, and the VIEW trials found there to be no meaningful differences in adverse event rates [16, 19].
2.4.2 Quality of Life
HRQoL may be influenced by VA for a number of reasons. It may be related to the vision in one eye only (either the WSE or the BSE). It is more likely to be a function of visual acuity in both eyes, with the relative differences between the eyes being a possible influence. Becoming legally blind may also impact upon the patient’s wellbeing due to the psychological significance of the event, as well as more pragmatic factors (e.g. moving to a care home, loss of freedom due to not being able to drive). These factors are difficult to capture in a one-eye model, which has been used in many previous Markov models.
Quality of life was estimated using a de novo regression analysis of a real-world dataset obtained from Czoski-Murray et al. [23], a study that used contact lenses to simulate the effect of visual impairment. Within the regression analysis, a number of models were considered, whereby quality of life was a function of VA in the BSE alone, WSE alone, VA in both eyes separately, VA in both eyes with interaction term, VA in both eyes with an interaction term and a blindness threshold (ESM, Table S3). The blindness threshold was implemented, where an additional utility decrement was applied, when patients had a BCVA of <35 in both eyes. The impact of using each of the five regression models was explored in the analysis. Further details of the regression methods are provided in Appendix 1 of the ESM.
2.4.3 Costs and Resource Use
A summary of unit costs and resource use in the model is provided in the ESM (Table S4 for unit costs, Table S5 for treatment and monitoring schedule). Costs from earlier years were inflated to 2014 prices using the Hospital and Community Services Inflation Index [24]. Costs were based on a UK healthcare provider (NHS and PSS) perspective. The key costs considered in the analysis included drug costs, costs of administering treatment and monitoring costs. Costs were also applied as patients entered the blindness health state.
Patients were treated and monitored using a PRN schedule, and were based on previously published estimates of mean number of visits per year over the 5-year treatment period [25–27]. The mean treatment and monitoring cost per cycle was estimated for each year of treatment, and applied to patients while on treatment.
Costs of blindness were applied when both eyes had a BCVA below 35 letters. Treatment was terminated if the treated eye reached a BCVA below 35 letters. Resource utilisation in patients who were blind was based on data in a published study, a systematic review and economic evaluation of photodynamic therapy for the treatment of wAMD [28]. Each resource associated with treating patients with blindness was applied to a varying proportion of patients [29]. Blind registration was applied as a one-off cost when patients entered the blindness state for the first time.
2.4.4 Mortality
Age-specific all-cause mortality for the general population was estimated from UK life tables [30]. To reflect the increased mortality risk in patients who have some degree of impaired vision, a relative risk (RR) was applied to the background mortality rate [31]. For individuals with severe visual impairment, defined as BCVA lower than 35 in both eyes, an RR of 1.54 was applied. For individuals with some visual impairment (defined as either eye having BCVA lower than 55), an RR of 1.23 was applied. For the impact on mortality associated with visual impairment to be modelled adequately, the BCVA in both eyes should be estimated explicitly.
2.5 Validation
BCVA change in the model was validated by comparing the mean BCVA change in each arm with the BCVA change observed in the original source (the IVAN trial [15] for BCVA progression in patients on ranibizumab, and the NMA [17] for the difference in BCVA between aflibercept and ranibizumab patients), over the first 24 months of treatment.
2.6 Analysis
The primary outcome of the analysis was the mean cost and the mean number of QALYs for each intervention.
The base-case analysis incorporated individual patient, or first-order, uncertainty. The probabilistic sensitivity analysis incorporated parameter, or second-order uncertainty in addition to first-order uncertainty [14].
Results of the first-order (base-case) analysis were based on 200,000 simulated patients over a lifetime time horizon, to ensure stability. A number of scenarios were undertaken, based on different methods of estimating HRQoL. The different analyses included (1) Model 1: HRQoL as a function of BCVA in the BSE; (2) Model 2: HRQoL as a function of BCVA in the WSE; (3) Model 3: HRQoL as a function of BCVA in both eyes (no interaction); (4) Model 4: HRQoL as a function of BCVA in both eyes (with interaction); and (5) Model 5: HRQoL as a function of BCVA in both eyes (with interaction and a blindness threshold). In this analysis, parameters that were varied stochastically include baseline patient characteristics and response to treatment. Event occurrence (death, discontinuation, development of bilateral disease) was determined stochastically, based on the point estimate of the parameter. Monte Carlo error (MCE) was assessed at different numbers of iterations of the model [32].
Second-order uncertainty was assigned to the point estimate of key variables, including baseline characteristics, treatment response, the coefficients in the utility regression analysis, and the relative risk of mortality. A total of 100 probabilistic estimates of cost effectiveness were generated, each based on 10,000 simulations of the model. Each of the 100 probabilistic estimates was based on a randomly generated point estimate (mean value) of the key parameters. Details of the parameters included in the second-order analysis and their variation are provided in the ESM (Table S6).
3 Results
The results of this study demonstrate that a simulation modelling approach provides a feasible option for evaluating the cost effectiveness of ophthalmology interventions.
3.1 First-Order (Individual Patient) Uncertainty: Base-Case Analysis
Results of the base-case analysis are presented in Table 1.
The total costs and life-years gained were very similar in both treatment arms, with the small decrease for aflibercept reflecting the higher mortality rate in patients with lower BCVA.
Results for the three two-eye models were broadly similar. Total QALYs were highest in the model based on the BSE only (Model 1) for estimating HRQoL, and lowest in the model based on the WSE only (Model 2). The one-eye model based on BSE only (Model 1) resulted in the largest number of incremental QALYs.
3.2 Second-Order (Parameter) Uncertainty: Probabilistic Sensitivity Analysis
The mean incremental QALYs and the mean incremental costs in the second-order analysis were similar to those observed in the first-order analysis. There was slightly greater variation in incremental QALYs than incremental costs in the second-order analysis (Table 2). Figure 2 presents the scatterplot for the probabilistic results of Model 4. Ranibizumab had a >95% probability of cost effectiveness at all willingness-to-pay threshold values, in all five scenarios.
Scatterplot of second-order analysis (ranibizumab vs aflibercept). Results are presented for Model 4, the two-eye model with an interaction term. Each red dot represents one estimate of cost effectiveness (incremental QALYs and incremental costs for ranibizumab compared with aflibercept). The results show that ranibizumab was the dominant strategy (more effective and less costly) compared with aflibercept. AFL aflibercept, QALY quality-adjusted life-year, RBZ ranibizumab
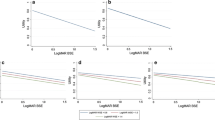
3.3 Visual Acuity
The simulation model can be demonstrated to model BCVA progression similarly to that observed in the studies on which the input parameters were based (Fig. 3a, b). Baseline BCVA in the model was consistent with that of the population on which they were modelled: the mean baseline BCVA of the EXCITE study was 56.93, compared with 56.90 in the model. Consistent with the results of the NMA, the model predicted a slight treatment benefit in favour of ranibizumab compared with aflibercept. Modelled BCVA in the ranibizumab arm was similar to that observed in the IVAN trial, although the modelled mean BCVA was lower towards the end of the 24-month period. Predicted differences in BCVA between the ranibizumab and aflibercept arms were broadly similar to those estimated in the NMA, although there was some observed variation towards the end of the study period.
Ranibizumab mean BCVA over time and aflibercept mean BCVA difference (relative to ranibizumab) over time. a The mean change in BCVA for ranibizumab patients in their treated eye over the first 24 months of starting treatment. The blue line represents the BCVA progression in the model, and the red line represents BCVA progression observed in the IVAN trial, on which the model was based. b The mean difference in BCVA for aflibercept patients in their treated eye compared with ranibizumab patients over the first 24 months of treatment. The blue line represents the difference in BCVA in the model, and the red line represents the difference as estimated in the NMA on which the model was based. BCVA best-corrected visual acuity, NMA network meta-analysis
A limitation of simulation modelling is the additional computational requirements to generate sufficient numbers of patients to estimate the mean model outcomes, and the resulting time for the model to run. A stabilisation test was undertaken: after very few (approximately 5000) iterations of the model, the variability in the mean result is reduced, and the mean result converges to within 1% of the base case result. The MCE was demonstrated to decrease with an increasing number of iterations. The MCE for each analysis is presented in the ESM (Table S7).
4 Discussion
4.1 Overview
The results of this economic evaluation suggest that simulation modelling is a suitable alternative for modelling in ophthalmology. The analysis provides some evidence to support the hypothesis that health economic models based on the two-eye regression models may generate a more accurate estimation of incremental QALYs for the comparison of ranibizumab versus aflibercept in wAMD. The model based on the BSE eye only provides a substantially higher estimate of total QALYs compared with the model based on the WSE only. A one-eye model is likely to misrepresent QALY gains, as it will only capture the benefit of treatment when the eye being treated is the eye used in the utility regression. A two-eye model is able to capture improvement in vision regardless of the eye it occurs in.
4.2 Limitations
There were some limitations associated with the dataset used to estimate the relationship between vision and HRQoL. Data was collected by Czoski-Murray et al. in a population of healthy subjects with no ocular pathology, with HRQoL elicited using the time trade off (TTO) technique [23]. Subjects were younger than those who typically present with wAMD, and more likely to be employed and educated to degree level than the general population. The utility estimate for patients with high BCVA is higher than one may expect for patients with wAMD of this age. It is unclear whether the Czoski-Murray dataset provides sufficient variation between BSEs and WSEs to clearly distinguish between the models, and therefore the difference between the BSEs and WSEs may be minimal compared with the differences seen in patients with AMD. Due to these factors, the study population was not considered to be representative of the wAMD population, and it may be that the resulting dataset does not capture the impact of HRQoL adequately. The Czoski-Murray dataset was the only HRQoL dataset that we had access to which collected BCVA data in both eyes. It has also been previously used in a number of NICE technology appraisals—while it was noted that there were limitations associated with the study, including issues around generalisability to the wAMD population, it was considered to be the most appropriate source of utility data [9]. A more appropriate dataset that has been collected from representative patients with ocular disease may show a more definitive impact of using different utility models. However, the authors of this study are unaware of any patient-level datasets where HRQoL and BCVA in both eyes were collected and are readily available, particularly in a format that is suitable for economic modelling purposes. The availability of such data would also allow further investigation of how vision in both eyes contributes to overall HRQoL, which would allow the advantages of a true two-eye model to be further leveraged. Previous studies undertaken in representative patients have established the link between BCVA in the BSE and HRQoL [33, 34]. A comparison of the utilities in these studies with those elicited in the Czoski-Murray et al. study found higher estimates of overall variation in HRQoL in the two studies of representative patients. We would welcome work to validate our utility analysis using a real-world dataset.
The MCE has been estimated for total costs and QALYs in the ranibizumab arm. It is normally recommended that MCE should be <5% of the mean value of the main outcome of interest; after 200,000 iterations, the MCE around total QALYs is 0.006, which is approximately 0.1% of the total QALY value and approximately 15% of the mean QALY difference between the two comparators. As a result, it is possible that at least some of the difference between the comparators could be attributable to MCE.
There is some evidence to suggest that contrast sensitivity (CS), rather than BCVA, is key to HRQoL in ophthalmology [35]. However, CS is usually a secondary outcome in clinical trials of wAMD and is often not reported in the appropriate manner to enable economic modelling. Further, without an explicit link between CS and blindness, it would be challenging to incorporate all relevant costs and resource use into an analysis.
A further important limitation of the model is that changes in BCVA are not correlated over time. In reality, one would expect BCVA progression to follow some form of autoregressive process rather than exhibiting random changes from month to month. This limitation would also be present in a Markov model in which transitions were fixed over time, and is not specific to simulation modelling. A possible extension to the model we present would be, therefore, to seek to model this process and for changes in BCVA to follow an autoregressive process whereby the change in BCVA at a particular time point is dependent upon changes at previous time points and possibly on baseline characteristics. If appropriate source data were available, this could potentially provide a further advantage of a simulation model over a Markov model as this would be very difficult to implement in a Markov model.
Similar conclusions to the first-order analysis were reached in the second-order analysis, although some variation was observed. The second-order analysis estimated similar incremental QALYs but lower incremental costs than the first-order analysis. A number of parameters were based on mean values in the first-order analysis but varied in the second-order analysis, thus suggesting that there are important non-linear relationships between variables contained within the model, including mortality associated with aging, and the treatment effect over time. When there is a non-linear relationship between patient characteristics and model outputs, the mean of the inputs cannot be used to evaluate the mean of the outputs. This is a further limitation of Markov models in this context, which are based on mean cohort characteristics.
4.3 Strengths
Individual-patient simulation models offer significant additional flexibility over Markov models allowing for the incorporation of two eyes into the model in an easy and transparent way, which results in a higher face validity of the model. Quality of life was estimated using a de novo regression analysis of a real-world dataset obtained from Czoski-Murray et al. [23]. Thus, HRQoL is based on the person as a whole rather than any individual components, and so is intuitively linked to the BCVA in both eyes. This is supported by the different outcomes of models based on the BSE or the WSE only. This ability to model both eyes independently is particularly important in wAMD where bilateral involvement is common, but is also relevant even where there is no bilateral involvement as it allows for incorporation of VA in an untreated eye. This is important as HRQoL is likely to be a function of vision in both eyes.
An individual-patient approach also offers a number of further advantages. Firstly, because it models events rather than states, discontinuation and blindness can be modelled more naturally. Patient history can be captured more readily, allowing for aspects like one-off costs (blindness registration) to be incorporated in a more transparent manner. This aspect of the treatment pathway is difficult to capture in a Markov model given its memoryless properties (patients newly entering the blindness state are indistinguishable from those who have been there for at least one cycle). Secondly, because the model does not use health states, it allows BCVA to be modelled on a continuous scale rather than being split into discrete health states in which patients are assumed to have the same HRQoL. This allows the potential benefits of interventions to be more accurately modelled and allows for effectiveness data to be incorporated in a more transparent way, including estimates derived from indirect evidence via an NMA. It also allows for non-linear relationships between VA and both benefits and costs to be incorporated more accurately, increasing both precision and the accuracy of predicted benefits and costs. Further, these gains in the precision and accuracy of predicted benefits and costs can be obtained without a significant increase in model complexity and therefore the transparency of the model is maintained.
The analysis has been demonstrated to capture BCVA progression relatively precisely over the study period (Fig. 3). While there is some degree of divergence towards the end of the study period, this may be due to factors such as the incorporation of discontinuation in the model and the resulting impact on BCVA, and the cumulative impact of Monte Carlo error. The model structure would also allow for the correlation between baseline characteristics and treatment response throughout the study period, using the method of multivariate normality, although the authors did not have access to the appropriate data (the covariance between each pair of parameters) at the time of the study in order to implement this method.
4.4 Previous Economic Analyses in Ophthalmology
To our knowledge, this study is the first economic evaluation for ophthalmology that has been developed using an individual simulation modelling approach rather than a Markov model. Previous economic evaluations using Markov models have been subject to criticism when reviewed by NICE, and were considered to accurately reflect vision in a single eye only. The NICE submission for aflibercept in wAMD was considered to inadequately model two eyes, leading to NICE rejecting this part of the analysis, using it as single-eye model only [2]. A Markov model was developed for the aflibercept submission for the treatment of DMO [6]. The analysis attempted to model both eyes explicitly, and as such the model included a large number of unique health states to allow for all combinations of BCVA in the study and fellow eye. Given the large amount of data that would be required to estimate transition probabilities between each health state, the model estimated probabilities whereby movement between health states was restricted and these were constant across all health states. While this is likely the most practical approach to modelling two eyes in a Markov model, there are a number of limitations of modelling in this way. Firstly, the lack of granularity by using discrete health states to represent BCVA progression; secondly, the ceiling effect experienced through use of constant probabilities across health states (whereby patients in the highest health states would be ‘unable’ to improve, even though the data suggest that a given proportion will do so, resulting in improvement in patients with a high BCVA being underestimated and the average VA score over time gradually falling below the observed value); and finally, the complexities of using a large number of health states (difficulty in assessing and error-checking the model). The impact of the ceiling effect is likely to be more pronounced where there are few health states. Increasing the number of health states, however, can rapidly increase model complexity and place heavy demands on input data such that the number of observations on which transition probabilities are estimated from becomes very small.
A previous study comparing the outcomes of a Markov model and a simulation model for wAMD suggested that the incremental costs as estimated by a Markov model are lower, and the incremental QALYs are higher, than those estimated by a simulation model [36]. Since there is no gold standard for modelling in ophthalmology, it is difficult to ascertain which of the two model structures provides a more accurate estimate of the costs and QALYs that would be accrued in reality. It is likely that a simulation model is more accurate at estimating clinical and model outcomes, given its dynamic nature and ability to capture certain elements of the patient pathway.
The benefits of simulation modelling are not restricted to ophthalmology. Simulation modelling has been demonstrated to be relevant in chronic and degenerative diseases where patient history is often more important, such as in rheumatoid arthritis and cardiovascular disease. These benefit from being modelled with a structure that allows for sequences of treatments to be incorporated, and time-since-event probabilities to be incorporated.
4.5 Conclusions
The advantages of individual patient simulations outlined in the previous sections may mean that the results of this analysis are more accurately estimated than in previously developed models. Additional studies comparing and verifying the results of a Markov model and a simulation model for the same decision problem, using the same data inputs, could be a useful direction for further research. The collection of bilateral utility outcomes from a representative population would allow the benefits of a patient simulation to be further exploited.
References
Bayer. Aflibercept solution for injection for treating wet age-related macular degeneration—Single Technology Appraisal [TA294]. Manufacturer’s Submission, 2013.
Cummins E, Fielding S, Johnston R, Rothnie K, Stewart F, Lois N, Burr J, Brazzelli M. Aflibercept solution for injection for the treatment of wet age-related macular degeneration. Aberdeen HTA Group; 2013.
Colquitt JL, Jones J, Tan SC, Takeda A, Clegg AJ, Price A. Ranibizumab and pegaptanib for the treatment of age-related macular degeneration: a systematic review and economic evaluation. Southampton Health Technology Assessments Centre; 2006.
Edwards SJ, Barton S, Trevor N, Lois N, Nherera L, Hamilton V. Ranibizumab for the treatment of macular oedema caused by retinal vein occlusion (RVO): A Single Technology Appraisal. London: BMJ Technology Assessment Group; 2011.
Shyangdan DS, Cummins E, Clar C, Ford J, Court R, Lois N, Waugh N. Aflibercept for treating visual impairment caused by macular oedema secondary to central retinal vein occlusion—a single technology assessment. Warwick Evidence 2013.
Fielding S, Cummins E, Cruickshank M, Fraser C, Lois N, Brazzelli M. Aflibercept for treating diabetic macular oedema. Aberdeen HTA group; 2014.
Cummins E, Fielding S, Cruickshank M, Fraser C, Lois N, Brazzelli M. Ranibizumab for the treatment of choroidal neovascularisation associated with pathological myopia. Aberdeen HTA Group; 2013.
National Institute for Health and Care Excellence. Aflibercept solution for injection for treating wet age-related macular degeneration. NICE technology appraisal guidance [TA294], 2013.
National Institute for Health and Care Excellence. Ranibizumab and pegaptanib for the treatment of wet age-related macular degeneration. NICE technology appraisal guidance [TA155], 2008.
Brown GC, Brown MM, Sharma S, Brown HC. Patient perceptions of quality-of-life associated with bilateral vision loss. Int Ophthalmol. 1998;22(5):307–12.
Butt T, Patient PJ, Tufail A, Rubin GS. Modelling cost effectiveness in neovascular age-related macular degeneration the impact of using contrast sensitivity vs visual acuity. Appl Health Econ Health Policy. 2014;12(3):289–97.
Schmidt-Erfurth U, Eldem B, Guymer R, Korobelnik JF, Schlingemann RO, Axer-Siegel R, et al. Efficacy and safety of monthly versus quarterly ranibizumab treatment in neovascular age-related macular degeneration: the EXCITE study. Ophthalmology. 2011;118(5):831–9.
Submacular Surgery Trials Research Group, Solomon SD, Jefferys JL, Hawkins BS, Bressler NM. Incident choroidal neovascularization in fellow eyes of patients with unilateral subfoveal choroidal neovascularization secondary to age-related macular degeneration: SST report No. 20 from the Submacular Surgery Trials Research Group. Arch Ophthalmol. 2007;125(10):1323–30.
Davis S, Stevenson M, Tappenden P, Wailoo A. NICE DSU Technical Support Document 15: cost-effectiveness modelling using patient-level simulation. 2014.
Chakravarthy U, Harding SP, Rogers CA, Downes SM, Lotery AJ, et al. Alternative treatments to inhibit VEGF in age-related choroidal neovascularisation: 2-year findings of the IVAN randomized trial. Lancet. 2013;382(9900):1258–67.
Heier JS, Brown DM, Chong V, et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology. 2012;119(12):2537–48.
Malcolm WA, Hodgson R, Glanville J, et al. Indirect treatment comparison of interventions for neovascular (wet) age-related macular degeneration (wet AMD) [Code PSS2]. ISPOR 20th Annual International Meeting. Philadelphia, PA, USA, 2015.
Ding Y, Fu H. Bayesian indirect and mixed treatment comparisons across longitudinal time points. Stat Med. 2013;32(15):2613–28.
Schmidt-Erfurth U, Kaiser PK, Korobelnik JF, Brown DM, Chong V, Nguyen QD, et al. Intravitreal aflibercept injection for neovascular age-related macular degeneration: ninety-six-week results of the VIEW studies. Ophthalmology. 2014;121(1):193–201.
Wong T, Chakravarthy U, Klein R, Mitchell P, Zlateva G, Buggage R, et al. The natural history and prognosis of neovascular age-related macular degeneration. Ophthalmology. 2008;115(1):116–26.
Frisen L, Frisen M. How good is normal visual acuity? A study of letter acuity thresholds as a function of age. Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1981;215(3):149–57.
Elliott DB, Yang KCH, Whitaker D. Visual acuity changes throughout adulthood in normal, health eyes: seeing beyond 6/6. Optom Vis Sci. 1995;72(3):186–91.
Czoski-Murray C, Carlton J, Brazier J, Young T, Papo NL, Kang HK. Valuing condition-specific health states using simulation contact lenses. Value Health. 2009;12(5):793–9.
PSSRU. Personal Social Services Research Unit. Unit costs of Health and Social Care 2014. http://www.pssru.ac.uk/project-pages/unit-costs/2014/. Accessed Dec 2015.
Writing Committee for the UKA-RMDEMRUG. The neovascular age-related macular degeneration database: multicenter study of 92,976 ranibizumab injections: report 1: visual acuity. Ophthalmology. 2014;121(5):1092–101.
Novartis Pharmaceuticals UK Limited. LUCENTIS summary of product characteristics.
Technology Appraisal TA294. Aflibercept solution for injection for treating wet age-related macular degeneration. Assumptions based on expert opinion and used within NICE costing template.
Meads C, Salas C, Roberts T, Moor D, Fry-Smith A, Hyde C. Clinical effectiveness and cost-utility of photodynamic therapy for wet age-related macular degenerations: a systematic review and economic evaluation. Health Technol Assess. 2003;7(9):v–vi, 1–98.
Shyangdan D CE, Lois N, Royle P, Waugh N. Dexamethasone implants in the treatment of macular oedema due to retinal vein occlusion: a single technology appraisal. Aberdeen HTA group; 2010.
National Life Tables, United Kingdom, 2012-2014: Office for National Statistics; 2015. http://www.ons.gov.uk/ons/rel/lifetables/national-life-tables/2012-2014/index.html. Accessed Dec 2015.
Christ SL, Lee DJ, Lam BL, Zheng DD, Arheart KL. Assessment of the effect of visual impairment on mortality through multiple health pathways: structural equation modeling. Investig Ophthalmol Vis Sci. 2008;49(8):3318–23.
Koehler E, Brown E, Haneuse SJ. On the assessment of Monte Carlo error in simulation-based statistical analyses. Am Stat. 2009;63(2):155–62.
Brown GC. Vision and quality-of-life. Trans Am Ophthalmol Soc. 1999;97:473–511.
Sharma S, Brown GC, Brown MM, et al. Converting visual acuity to utilities. Can J Ophthalmol. 2000;35(5):267–72.
Bansback N, Czoski-Murray C, Carlton J, Lewis G, Hughes L, Espallargues M, et al. Determinants of health related quality of life and health state utility in patients with age related macular degeneration: the association of contrast sensitivity and visual acuity. Qual Life Res. 2007;16(3):533–43.
Claxton L, Hodgson R, Malcolm W. A comparison of modelling techniques: Patient simulation vs Markov modelling in ophthalmology. International Society for Pharmacoeconomics and Outcomes Research 17th Annual European Congress, Amsterdam, The Netherlands, 2014.
Acknowledgements
The original regression analysis of the Czoski-Murray quality of life dataset was undertaken by David Trueman and Tim Reason at Abacus International, and was funded by Novartis.
The authors would like to thank the IVAN trial investigators for providing the dataset for modelling ranibizumab BCVA progression.
Author contributions
All authors were involved in the conceptualisation of the analysis. LC and RH developed the economic analysis. LC, RH and RPJ contributed equally towards the drafting of the manuscript. All authors provided feedback on each draft of the manuscript. LC will act as the overall guarantor.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was funded and initiated by Novartis Pharmaceuticals UK Ltd. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Ruth Pulikottil-Jacob is an employee of Novartis and Bill Malcolm is an ex-employee of Novartis. Lindsay Claxton and Matthew Taylor are employees of York Health Economics Consortium, which was commissioned by Novartis to develop the study. Robert Hodgson is an ex-employee of York Health Economics Consortium.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Claxton, L., Hodgson, R., Taylor, M. et al. Simulation Modelling in Ophthalmology: Application to Cost Effectiveness of Ranibizumab and Aflibercept for the Treatment of Wet Age-Related Macular Degeneration in the United Kingdom. PharmacoEconomics 35, 237–248 (2017). https://doi.org/10.1007/s40273-016-0459-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-016-0459-z