Abstract
Aim
Triclofos sodium (TFS) has been used for many years in children as a sedative for painless medical procedures. It is physiologically and pharmacologically similar to chloral hydrate, which has been censured for use in children with neurocognitive disorders. The aim of this study was to investigate the safety and efficacy of TFS sedation in a pediatric population with a high rate of neurocognitive disability.
Methods
The database of the neurodiagnostic institute of a tertiary academic pediatric medical center was retrospectively reviewed for all children who underwent sedation with TFS in 2014. Data were collected on demographics, comorbidities, neurologic symptoms, sedation-related variables, and outcome.
Results
The study population consisted of 869 children (58.2% male) of median age 25 months (range 5–200 months); 364 (41.2%) had neurocognitive diagnoses, mainly seizures/epilepsy, hypotonia, or developmental delay. TFS was used for routine electroencephalography in 486 (53.8%) patients and audiometry in 401 (46.2%). Mean (± SD) dose of TFS was 50.2 ± 4.9 mg/kg. Median time to sedation was 45 min (range 5–245), and median duration of sedation was 35 min (range 5–190). Adequate sedation depth was achieved in 769 cases (88.5%). Rates of sedation-related adverse events were low: apnea, 0; desaturation ≤ 90%, 0.2% (two patients); and emesis, 0.35% (three patients). None of the children had hemodynamic instability or signs of poor perfusion. There was no association between desaturations and the presence of hypotonia or developmental delay.
Conclusion
TFS, when administered in a controlled and monitored environment, may be safe for use in children, including those with underlying neurocognitive disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Triclofos sodium, which has served as a mild sedative for many years, is physiologically and pharmacologically similar to chloral hydrate. |
Concerns have been raised regarding the safety of chloral hydrate use in children with neurocognitive disability. |
Our analysis of a pediatric population with a high rate of neurocognitive disability undergoing non-interventional neurodiagnostic examinations yielded a good safety profile for carefully monitored triclofos sodium sedation. |
Only a few, mild, adverse effects were documented. |
1 Introduction
Neurodiagnostic studies such as routine electroencephalography (rEEG) and brainstem evoked response audiometry (BERA) may be challenging in the pediatric population, especially in young and neurologically impaired children. Procedural sedation may offer a convenient means of obtaining technically adequate data from these studies. Benzodiazepines and other anesthetic agents are inappropriate for use in this setting, as they could potentially affect the background activity by inducing excessive beta activity and decrease epileptiform activity on the EEG. However, chloral hydrate at typical doses required for sedation does not tend to affect the EEG [1].
The use of chloral hydrate for sedation in children has been investigated in depth. Several studies, including a recent meta-analysis by the Cochrane collaboration, demonstrated relatively good sedation with a single dose of 50–100 mg/kg (maximal dose 2 g) [2,3,4,5,6,7,8]. Adverse events included nausea and vomiting, and respiratory depression that can progress to apnea, hypotension, and bradycardia [4, 7,8,9,10,11]. Although there are some reports of a rare risk of cardiac arrhythmia culminating in torsades de pointes, even with appropriate dosing [12, 13], two studies of children with congenital heart disease found chloral hydrate sedation to be effective and safe, with no cases of sedation-related arrhythmia [9, 14].
However, concerns regarding the use of chloral hydrate were raised following several reports of its potential lethality [2, 15, 16]. Most of the deaths occurred when the drug was administered at home by a parent under conditions that failed to meet the American Academy of Pediatrics (AAP) guidelines for monitoring and management before, during, and after sedation [17]. Nevertheless, Nordt et al. recommended that chloral hydrate not be used in children older than 4 years or in children of any age with neurodevelopmental disorders due to the increased risks of both adverse events and treatment failure [2].
Triclofos sodium (TFS) has long been used in our medical center as a sedative in children undergoing neurodiagnostic tests. TFS is the phosphate ester of trichloroethanol, the pharmacologically active metabolite of chloral hydrate, and it shares pharmacologic and physiologic properties with chloral hydrate, with the advantage of less gastric irritation [18,19,20]. Both agents seem to achieve comparable success rates of sedation for EEG [21]. TFS, however, has not been studied in depth and the incidence of TFS sedation adverse events has not been described [18,19,20, 22,23,24]. The present study was conducted in a pediatric population with a high prevalence of neurocognitive disorders. The aim of the study was to investigate the efficacy and safety of TFS for pediatric sedation, while evaluating predictive factors for both.
2 Methods
2.1 Population and Setting
The database of the neurodiagnostic institute of a tertiary university-affiliated pediatric medical center was searched for all children who underwent TFS sedation from January to December 2014 for purposes of EEG or BERA. Data were collected by chart review.
2.2 Institutional Protocol for Triclofos Sodium (TFS) Sedation
According to our departmental policy, TFS may be administered to children aged 3 months to 18 years by nurses (trained in pediatric acute life support, and pediatric sedation) under a continuous observation and monitoring protocol, as stipulated in the AAP safe sedation guidelines [17]. A pediatrician experienced and certified in pediatric sedation is available in immediate proximity to support the nursing staff in the management of significant adverse events, should they be encountered. Children must be in a fasting state of 4 h from food and 2 h from clear liquids, prior to the examination. Those who have fever or respiratory disease are rescheduled. The assessment of sedation risk is based on existing comorbid conditions and chronic diseases (history of prematurity, known genetic aberration, neuro-cognitive disorder, congenital heart disease, chronic respiratory disorder). Children with chronic diseases are further classified using the American Society of Anesthesia Physical Status (ASA-PS) system [25]. Those with an ASA-PS score of 3 or more (high-risk group) or otherwise identified by the nurse to have risk factors for sedation, namely, history of adverse events during prior sedation, abnormal vital signs, or a clinically significant abnormality on physical examination, are evaluated by a physician with expertise in pediatric sedation and at his discretion, can continue with the nurse-driven protocol, or be redirected to an alternative sedative pathway. Sedation is withheld if the child falls into a deep sleep prior to onset of the procedure, or if the parents withhold consent for administration of a sedative drug.
Prior to TFS administration, vital signs, including heart rate, blood pressure, oxygen saturation, and weight, are recorded. TFS is administered orally at an initial dose of 50 mg/kg. The child is then placed in a darkened sedation room and, once calm, connected to a pulse oximeter (Philips Intellivue MP20 Patient Monitor, Philips, Boeblingen, Germany) and overseen by a nurse. Cardiac leads and monitoring are added for children with cardiac risk factors or suspected irregularity on pulse oximetry. Oxygen saturation and heart rate continue to be monitored from the time of drug administration until the child is fully awake, and recorded to flow sheet every 10 min. Blood pressure measurement is repeated once in the sedate state and again after recovery. Children who do not fall asleep within 30 min of the initial dose or who have a history of difficulty with sedation may receive an additional 25 mg/kg dose of TFS. Oxygen is not routinely supplemented unless desaturation occurs and a trial of head repositioning fails to correct the problem. Maximal sedation depth is scored by the nurse using the University of Michigan Sedation Scale (UMSS) of 0–4, with 3 and above representing deep sleep [26]. Children are discharged home by the nurse after achieving full recovery with a return to their baseline physical status and demonstration of tolerance of food and drink by the oral route [27]. Contact telephone numbers are provided to the parents in case of concerns after discharge.
2.3 Data Collection
Data for the present study were extracted from the patient charts and entered into a computerized database established for the study. Patient demographics, history relevant to sedation practice, and potential risk factors were recorded, in addition to sedation-related variables. Risk factors included premature birth and known genetic abnormality, developmental delay, severe hypotonia, and convulsive disorder. Sedation-related factors included vital signs when awake and during sedation, drug dose, time to effective sedation, duration of sedation, and time to discharge. We also recorded adverse events of apnea, desaturation, hypotension, bradycardia, and vomiting. Hypotension and bradycardia were further classified as mild, moderate, or severe according to the percent of deviation from the normal lower limit [28, 29]: mild, 10% deviation or less; moderate, 11–20%; severe, > 20% or signs of hemodynamic compromise. Oxygen desaturation was defined as sustained saturation of ≤ 90% for at least 30 s, in accordance with the Pediatric Sedation Research Consortium [30]. Adverse events were considered minor if they could be managed by conservative means: clearing or suctioning of secretions, upper airway repositioning, tactile stimulation, and oxygen administration via mask, nasal cannula, or blow-by technique were categorized as minor. Events that required any additional respiratory, circulatory, or other support were categorized as major. The associations of the risk factors and sedation-related factors with the incidence of adverse events were determined.
2.4 Statistical Analysis
The data were analyzed using BMDP Statistical Software (Dixon WJ, ed. Los Angeles: University of California Press; 1993). Pearson’s chi-square test or Fisher’s exact test (two-tailed) was used to analyze between-group differences in categorical variables, and analysis of variance (ANOVA) was used for continuous variables. ANOVA with repeated measures was used to determine changes over time. Correlations between variables were analyzed using Pearson’s correlation. A p value of ≤ 0.05 was considered significant.
3 Results
3.1 Demographic Characteristics
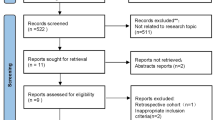
Between January and December 2014, 944 children were scheduled for a neurodiagnostic study under sedation in our medical center. Seventy-five children were ultimately not sedated and were excluded from the study: of these, 51 slept spontaneously without need for sedation; 20 were considered by the examining physician to be at excessively high risk for sedation; and two were sedated with nitrous oxide only; in two cases, the parents refused consent.
The remaining 869 children comprised the study population. They included 787 children who underwent sedation according to the nursing protocol and 82 who were authorized to undergo sedation following additional physician assessment. Median patient age was 25 months (range 5–200 months), and mean (± SD) weight was 13.4 ± 5.9 kg. TFS sedation was used for EEG examination in 468 patients (53.8%) and BERA in 401 (46.2%). The patients’ background factors are summarized in Table 1.
3.2 Comorbidities
Assessment of comorbid conditions known to harbor a risk for sedation yielded 123 patients (14.2%) with premature birth, 22 (2.6%) with a known genetic abnormality, 154 (17.7%) with developmental delay, and 61 (7.0%) with severe hypotonia. In addition, 249 patients (28.9%) had previously diagnosed epilepsy. Together, severe hypotonia or developmental delay affected 177 children (20.4%), and the addition of children with epilepsy increased the neurological disability subgroup to 364 (41.2%). The distribution of the ASA-PS scores was as follows: 496 patients (57.1%) ASA-PS 1, 348 (40%) ASA-PS 2, and 25 (2.9%) ASA-PS 3. An ASA-PS score of 1 or 2 (low-risk group) was found in 844 children (97.1%). The risk factor data are summarized in Table 2.
3.3 Efficacy and Safety
3.3.1 Sedation Dose and Effect
The mean (± SD) dose of TFS was 50.2 ± 4.9 (range 39–87) mg/kg. The median time from drug dosing to sleep was 45 min (IQR 30–75), and from onset of sleep to the first signs of awakening, 35 min (IQR 25–45). Time to sedation was affected by age, older children taking longer to fall asleep (R = 0.22, p < 0.001), and was significantly shorter in children < 3 years of age than in older children (51.7 ± 31 vs 70 ± 43; p < 0.001). The time from drug administration to hospital discharge was 133 ± 53 min. Figure 1 demonstrates the time to sedation and duration of sedation by age.
3.3.2 Sedation Quality
Sedation depth was rated according to the UMSS. Good sedation (i.e., a score of 3 or above), designating deep sleep, was found in 769 patients (88.5%), UMSS 2 (moderate sedation) in 52 (6%), and suboptimal (UMSS 0–1: awake or minimally sedated) in 48 (5.5%). Age was found to be a significant factor affecting sedation quality, with a significantly lower mean age in the good sedation group (UMSS 3 or above), compared with those suboptimally sedated (scored UMSS 0–1), (32 ± 26.8 vs 60.8 ± 38.3 months; p < 0.001). Using 5 years of age as a cutoff, good sedation was achieved significantly more often in those aged < 5 years compared with the rest of the cohort (680/749, 90.8% vs 89/120, 74.2%; p < 0.001), whereas suboptimal sedation was rated significantly more often in those older than 5 years of age (24/749, 3.2% vs 24/120, 20%; p < 0.001). Figure 2 demonstrates sedation quality following TFS treatment by age.
3.4 Adverse Events
3.4.1 Respiratory Events
Significant oxygen desaturation (≤ 90% for 30 s) occurred in two children (0.2%), and mild oxygen desaturation (≤ 94% for 30 s), in 21 children (2.4%). In all cases, oxygen saturation normalized after the head was repositioned and the airway was stabilized, with no need for oxygen supplementation. Mild desaturation was significantly associated with a history of prematurity (p < 0.001) and an ASA-PS of 3 (5.6% vs 13.6%; p = 0.003), but not with hypotonia (p = 0.067) or developmental delay (p = 0.56). No apnea events were documented throughout the study period. Concomitant apnea was not documented as the cause in any of the children demonstrating oxygen desaturation.
3.4.2 Hemodynamic Events
No arrhythmias were documented throughout the study period. Age-corrected bradycardia was found in 24 children (2.9%) during sedation, mild in 14 and moderate in 10. There were no cases of severe or symptomatic bradycardia, and none of the patients required intervention for hemodynamic stabilization. Analysis of the hemodynamic events by investigated risk factors revealed that bradycardia was associated with a known genetic abnormality (p = 0.008) and developmental delay (p = 0.05), but not with hypotonia. Age-corrected hypotension was found in four children (0.5%) during sedation, mild in three and moderate in one. None of them demonstrated concurrent tachycardia, poor perfusion, or other evidence of hemodynamic instability, and all cases resolved spontaneously without intervention. Hypotension was not found to be associated with any of the risk factors for sedation investigated. None of the hemodynamic events was associated with the ASA-PS score.
3.4.3 Other Adverse Events
Vomiting episodes, found in three children (0.35%), occurred immediately after or in close proximity to drug administration, while the child was still fully conscious. None of the children in the cohort was hospitalized for associated adverse events or presented to the emergency department for evaluation of adverse events. The contact number provided to the parents was not utilized.
3.4.4 Age as a Risk Factor for Adverse Events
Age was assessed as a risk factor for adverse events, as described in Table 3. Age was not found in correlation with any adverse events for the whole cohort. However, for the subgroup of children who developed mild desaturation ≤ 94%, a statistical significance could be demonstrated for those younger than 2 years of age when compared with those aged 2 years and above (15/393 [3.8%] vs 6/476 [1.2%]; p = 0.03).
4 Discussion
To our knowledge, this is the largest study investigating the safety and efficacy of TFS sedation for neurodiagnostic examinations in children. Our cohort of 869 patients constituted 92% of the children originally scheduled for sedation at our center during the study period. Only 20 patients (2.3%) were denied sedation because of the severity or complexity of their background illness or acute illness at the time of examination. This low non-sedation rate supports the ability to extrapolate our findings to similar pediatric populations, mitigating the risk of a selection bias.
Our study population is unique for the high proportion of neurologically disabled children, previously tagged as being at risk for chloral hydrate sedation. Indeed, approximately 20% of the cohort had significant hypotonia or severe developmental delay, and when children with epilepsy were included, the rate rose to 41%.
At an average TFS dose of 50.2 mg/kg, 88.5% of our patients achieved good sedation, and only 5.5% had unsatisfactory sedation. The median time to sedation from drug administration was 45 min, and sedation lasted 35 min. These results are in line with a recent prospective observational study of 160 children sedated with TFS for routine sleep EEGs, which demonstrated a single dose of 50 mg/kg to have an 82.5% success rate, median sleep onset of 30 min, and sleep duration of 90 min [31]. Similar results were obtained in an older study of 71 children, comparing success rates of EEG sedation with chloral hydrate versus TFS [21], and are consistent with a published chloral hydrate-based institutional protocol for EEG sedation demonstrating a 92% success rate using similar doses in children younger than 6 years [32].
Our study finds age to be a significant factor affecting both time to sedation and sedation quality. Younger children were faster to achieve the sedate state, and demonstrated significantly better sedation quality scores. Five years of age was found to be a significant cut-off point, with a 90.8% sedation success rate prior, decreasing to 75% in those aged 5 years and above.
With regard to adverse events, a previously published conference paper [23] performed a systematic review regarding adverse events of TFS for procedural sedation in children. Of 17 identified articles, 12 evaluated painless procedural sedation (170 patients) and 5 (780 patients) evaluated sedation for painful procedures. Vomiting was the most common adverse event at 7.1%. Most were not severe, nor warranted medical intervention. The second most frequently reported adverse event was hypoxia at 6.9%, but was reported only in children undergoing painful procedural sedation. All cases of hypoxia were mild (oxygen saturation of 90–95%) and did not require medical intervention. Adverse events were much higher for painful procedures compared with painless procedures (14.1% vs 1.5%, respectively). The authors state the size of included studies and lack of reporting uniformity as major limitations.
In our study, children were closely monitored for adverse events, which were few and mild. There were no cases of apnea, and none of the children required urgent respiratory or hemodynamic support apart from oxygen supplementation or airway repositioning. Vital signs returned to baseline in all cases, and none of the children needed hospitalization or a referral to the emergency department. Events of age-corrected bradycardia and hypotension were mostly mild. Hypotension was not accompanied by compensatory tachycardia, and peripheral perfusion was maintained in all children without signs of hemodynamic instability. Arrhythmia was not noted in any of our patients. The rate of emesis at 0.34% was lower than that reported for chloral hydrate (0.4–15%) [2, 9, 11, 14], perhaps because of the lesser gastric mucosal irritation associated with TFS. All cases of emesis occurred in close proximity to drug administration, while the child was still awake and the airway-protective reflexes intact, minimizing the risk of emesis-induced aspiration.
Desaturation, defined as a prolonged decline in oxygen saturation to 90% or less [30], was found in only two children (0.2%). When we broadened the definition to 94% or less, the incidence rose to 2.4%. Although mild desaturation was easily resolved by repositioning the head and stabilizing the airway, this finding serves as a reminder of the potential risks of sedation. Without constant monitoring, an alert nursing staff, and appropriate action when necessary, mild, transient desaturation could have progressed to significant life-threatening events. Risk factors for mild desaturation included a history of prematurity and low ASA-PS. However, hypotonia and developmental delay were not found to pose a risk for oxygen desaturation in our study.
The mild physiologic effects of TFS sedation together with the overall paucity of adverse events support its use for pediatric non-painful neurodiagnostic procedures in children and confirm its relatively safe profile when used in a monitored and controlled environment. This finding was also true for the children with a neurologic disability and should help clarify its suitability for this patient subgroup.
While chloral hydrate has often been used in the past for non-painful sedation, this drug is often unavailable in its commercial liquid formulation, necessitating local formulation from reconstituted crystals. In addition to the added demand on pharmacy resources, concerns have been raised regarding sedation efficacy of the locally formulated drugs [33]. TFS is not only readily available in a commercial formulation, but is also more palatable and causes less gastric irritation than chloral hydrate, and therefore may serve as an appropriate alternative.
Dexmedetomidine, an agonist of the α-2 receptor, belongs to a new generation of drugs appropriate for use in neurodiagnostic studies, as it minimally effects EEG interpretation. Dexmedetomidine has been successfully delivered by intravenous, oral, intranasal, and intramuscular routes with > 90% success rates [34,35,36,37]. While reported adverse events are mostly mild, one study reported a 10.7% rate of hypotension, and 3.5% rate of desaturation ≤ 90% [36]. A comparison study of oral dexmedetomidine and chloral hydrate at two different doses of each, demonstrated a trend towards improved success rates with dexmedetomidine, and increased adverse events only in the subgroup treated with 100 mg/kg of chloral hydrate (albeit mostly nausea and vomiting of limited clinical significance) [37]. Our study, on a much larger population, with high risk, neurologically debilitated children, demonstrates a much lower risk of significant desaturation at 0.2%, questioning the overall benefit from dexmedetomidine use. Furthermore, dexmedetomidine is much more costly, and in resource-limited health systems, may be chosen to be used in reserve, for those who have failed prior attempts at sedation with drugs of the older generation.
Nevertheless, despite its good safety profile, some limitations of TFS were demonstrated in our study. Although highly efficient for non-painful sedation in young children, the efficacy of TFS was decreased in the older children, who required a longer time to achieve sedation, and attained a lesser quality of sedation. For children aged up to 5 years, our results are very supportive for continued use of TFS sedation. For children older than 5 years, TFS may be insufficient, and an additional drug or different medication may be indicated.
Besides the retrospective design, our study has several limitations that may affect the interpretation of the results. First, most of the children in the cohort were younger than 3 years, and as such, do not represent the entire pediatric spectrum. Our population was almost entirely composed of children with ASA-PS scores of 1 or 2, limiting the generalizability of our results to sicker children. Finally, the paucity of adverse events in our study, albeit a welcome finding, prevented us from completing a more in-depth analysis of associated subgroups and sedation risk factors.
5 Conclusion
Our study showed that TFS may serve as a safe and effective agent for sedation of children < 5 years old for non-painful procedures, including those with neurologic disabilities, when used under close observation in a monitored environment. For older children, TFS alone may be insufficient, and an additional drug or alternative medication is warranted.
References
Thoresen M, Henriksen O, Wannag E, Laegreid L. Does a sedative dose of chloral hydrate modify the EEG of children with epilepsy? Electroencephalogr Clin Neurophysiol. 1997;102(2):152–7.
Nordt SP, Rangan C, Hardmaslani M, Clark RF, Wendler C, Valente M. Pediatric chloral hydrate poisonings and death following outpatient procedural sedation. J Med Toxicol. 2014;10(2):219–22. https://doi.org/10.1007/s13181-013-0358-z.
Pershad J, Palmisano P, Nichols M. Chloral hydrate: the good and the bad. Pediatr Emerg Care. 1999;15(6):432–5.
Chloral hydrate. Drug facts and comparisons. Efacts. Philadelphia: Wolters Kluwer Health, Inc; 2006.
Martí-Bonmatí L, Ronchera-Oms CL, Casillas C, Poyatos C, Torrijo C, Jiménez NV. Randomised double-blind clinical trial of intermediate- versus high-dose chloral hydrate for neuroimaging of children. Neuroradiology. 1995;37(8):687–91.
Fong CY, Tay CG, Ong LC, Lai NM. Chloral hydrate as a sedating agent for neurodiagnostic procedures in children. Cochrane Database Syst Rev. 2017;11:CD011786. https://doi.org/10.1002/14651858.cd011786.pub2.
Buck ML. Chloral hydrate use during infancy. Neonatal Pharmacol Quart. 1992;1:31–7.
Twite MD, Rashid A, Zuk J, Friesen RH. Sedation, analgesia, and neuromuscular blockade in the pediatric intensive care unit: survey of fellowship training program. Pediatr Crit Care Med. 2004;5(6):521–32. https://doi.org/10.1097/01.PCC.0000144710.13710.2E.
Napoli KL, Ingall CG, Martin GR. Safety and efficacy of chloral hydrate sedation in children undergoing echocardiography. J Pediatr. 1996;129(2):287–91.
Greenberg SB, Faerber EN, Aspinall CL. High dose chloral hydrate sedation for children undergoing CT. J Comput Assist Tomogr. 1991;15(3):467–9.
Kao SC, Adamson SD, Tatman LH, Berbaum KS. A survey of post-discharge side effects of conscious sedation using chloral hydrate in pediatric CT and MR imaging. Pediatr Radiol. 1999;29(4):287–90. https://doi.org/10.1007/s002470050590.
Coté CJ, Karl HW, Notterman DA, Weinberg JA, McCloskey C. Adverse sedation events in pediatrics: analysis of medications used for sedation. Pediatrics. 2000;106(4):633–44.
Rokicki W. Cardiac arrhythmia in a child after the usual dose of chloral hydrate. Pediatr Cardiol. 1996;17(6):419–20.
Heistein LC, Ramaciotti C, Scott WA, Coursey M, Sheeran PW, Lemler MS. Chloral hydrate sedation for pediatric echocardiography: pysiologic responses, adverse events, and risk factors. Pediatrics. 2006;117(3):e434–41.
Sing K, Erickson T, Amitai Y, Hryhorczuk D. Chloral hydrate toxicity from oral and intravenous administration. J Toxicol Clin Toxicol. 1996;34(1):101–6.
Hirsch IA, Zauder HI. Chloral hydrate: a potential cause of arrhythmias. Anesth Analg. 1986;65(6):691–2.
Coté CJ, Wilson S. Guidelines for monitoring and management of pediatric patients before, during, and after sedation for diagnostic and therapeutic procedures: update 2016. Pediatr Dent. 2016;38(4):13–39.
Sellers EM, Lang-Sellers M, Koch-Weser J. Comparative metabolism of chloral hydrate and triclofos. J Clin Pharmacol. 1978;18(10):457–61.
Jackson EA, Rabbette PS, Dezateux C, Hatch DJ, Stocks J. The effect of triclofos sodium sedation on respiratory rate, oxygen saturation, and heart rate in infants and young children. Pediatr Pulmonol. 1991;10(1):40–5.
Gozal D, Drenger B, Levin PD, Kadari A, Gozal Y. A pediatric sedation/anesthesia program with dedicated care by anesthesiologists and nurses for procedures outside the operating room. J Pediatr. 2004;145(1):47–52. https://doi.org/10.1016/j.jpeds.2004.01.044.
Millichap JG. Electroencephalographic evaluation of triclofos sodium sedation in children. Am J Dis Child. 1972;124(4):526–7.
Chaudhary S, Jindal R, Girotra G, Salhotra R, Rautela RS, Sethi AK. Is midozolam superior to triclofos and hydroxyzine as premedicant in children? J Anaesthesiol Clin Pharmacol. 2014;30(1):53–8. https://doi.org/10.4103/0970-9185.125704.
Sammons H, Choonara I, Alotaibi B. Safety and clinical effectiveness of triclofos for procedural sedation in children: a systemic review. Arch Dis Child. 2015;100(6):e1.
Bhatnagar S, Das UM, Bhatnagar G. Comparison of oral midazolam with oral tramadol, triclofos and zolpidem in the sedation of pediatric dental patients : an in vivo study. J Indian Soc Pedod Prev Dent. 2012;30(2):109–14. https://doi.org/10.4103/0970-4388.99980.
ASA Physical Status classification system (ASA PS): American Society of Anesthesiologists: October 15, 2014. https://www.asahq.org/resources/clinical-information/asa-physical-status-classification-system. Accessed 9 July 2019.
Malviya S, Voepel-Lewis T, Tait AR, Merkel S, Tremper K, Naughton N. Depth of sedation in children undergoing computed tomography: validity and reliability of the University of Michigan Sedation Scale (UMSS). Br J Anaesth. 2002;88(2):241–5.
Aldrete JA. The post-anesthesia recovery score revisited. J Clin Anesth. 1995;7(1):89–91.
Kliegman RM, Stanton B, St Geme J, Schor NF, Behrman RE. Nelson textbook of pediatrics. 20th ed. New York: Elsevier; 2016.
Ralston M. Pediatric advanced life support provider manual. Dallas: American Heart Association; 2006.
Cravero JP, Beach ML, Blike GT, Gallagher SM, Hertzog JH, Pediatric Sedation Research Consortium. The incidence and nature of adverse events during pediatric sedation/anesthesia with propofol for procedures outside the operating room: a report from the Pediatric Sedation Research Consortium. Anesth Analg. 2009;108(3):795–804. https://doi.org/10.1213/ane.0b013e31818fc334.
Jain P, Sharma S, Sharma A, Goel S, Jose A, Aneja S. Efficacy and safety of oral triclofos as sedative for children undergoing sleep electroencephalogram: an observational study. J Pediatr Neurosci. 2016;11(2):105–8. https://doi.org/10.4103/1817-1745.187622.
Keidan I, Ben-Menachem E, Tzadok M, Ben-Zeev B, Berkenstadt H. Electroencephalography for children with autistic spectrum disorder: a sedation protocol. Paediatr Anaesth. 2015;25(2):200–5. https://doi.org/10.1111/pan.12510.
Hill GD, Walbergh DB, Frommelt PC. Efficacy of reconstituted oral chloral hydrate from crystals for echocardiography sedation. J Am Soc Echocardiogr. 2016;29(4):337–40. https://doi.org/10.1016/j.echo.2015.11.014.
Mason KP, Lubisch N, Robinson F, Roskos R, Epstein MA. Intramuscular dexmedetomidine: an effective route of sedation preserves background activity for pediatric electroencephalograms. J Pediatr. 2012;161(5):927–32. https://doi.org/10.1016/j.jpeds.2012.05.011.
Liu H, Sun M, Zhang J, Tian Q, Yu Q, Liu Y, Yang F, Li S, Tu S. Determination of the 90% effective dose of intranasal dexmedetomidine for sedation during electroencephalography in children. Acta Anaesthesiol Scand. 2019. https://doi.org/10.1111/aas.13372.
Baier NM, Mendez SS, Kimm D, Velazquez AE, Schroeder AR. Intranasal dexmedetomidine: an effective sedative agent for electroencephalogram and auditory brain response testing. Paediatr Anaesth. 2016;26(3):280–5. https://doi.org/10.1111/pan.12851.
Gumus H, Bayram AK, Poyrazoglu HG, Canpolat DG, Per H, Canpolat M, Yildiz K, Kumandas S. Comparison of effects of different dexmedetomidine and chloral hydrate doses used in sedation on electroencephalography in pediatric patients. J Child Neurol. 2015;30(8):983–8. https://doi.org/10.1177/0883073814549582.
Acknowledgements
We thank Mrs Pnina Lilos for her insights regarding the study design and assistance in the data analysis and interpretation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors including EK, AD, AW, DK, GK, RM, and EN have no conflicts of interest to disclose.
Funding source
No funding was secured for this study.
Ethical approval and informed consent
The study was approved by the Institutional Review Board of Schneider Children’s Medical Center of Israel with a waiver of parental consent owing to the retrospective study design (RMC-0010-15).
Rights and permissions
About this article
Cite this article
Kaplan, E., Daka, A., Weissbach, A. et al. Triclofos Sodium for Pediatric Sedation in Non-Painful Neurodiagnostic Studies. Pediatr Drugs 21, 371–378 (2019). https://doi.org/10.1007/s40272-019-00346-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-019-00346-6