Abstract
Background
Consideration of patient preferences regarding delivery of mental health services within primary care may greatly improve access and quality of care for the many who could benefit from those services.
Objectives
This project evaluated the feasibility and usefulness of adding a consumer-products design method to qualitative methods implemented within a community-based participatory research (CBPR) framework.
Research Design
Discrete-choice conjoint experiment (DCE) added to systematic focus group data collection and analysis.
Subjects
Focus group data were collected from 64 patients of a Federally-Qualified Health Center (FQHC) serving a predominantly low-income Hispanic population. A total of 604 patients in the waiting rooms of the FQHC responded to the DCE.
Measures
The DCE contained 15 choice tasks that each asked respondents to choose between three mental health services options described by the levels of two (of eight) attributes based on themes that emerged from focus group data.
Results
The addition of the DCE was found to be feasible and useful in providing distinct information on relative patient preferences compared with the focus group analyses alone. According to market simulations, the package of mental health services guided by the results of the DCE was preferred by patients.
Conclusions
Unique patterns of patient preferences were uncovered by the DCE and these findings were useful in identifying pragmatic solutions to better address the mental health service needs of this population. However, for this resource-intensive method to be adopted more broadly, the scale of the primary care setting and/or scope of the issue addressed have to be relatively large.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Patient preferences are important to consider in the delivery design of mental health services. |
Use of the discrete-choice conjoint experiment (DCE) is feasible for use in an academic/federally-qualified health center partnership within a community-based participatory research framework, and provides useful additional and different information compared with focus groups alone. |
However, the additional resources required for a DCE may only be justified for a larger care design effort or in a larger health system. |
1 Introduction
Primary care systems have a critical role in addressing major gaps in the delivery of mental health services in the US. Persons with mental health problems most typically engage their primary care providers (if any health professional) [1, 2]. Although this creates a burden for primary care systems generally, clinics serving low-income, minority populations, where mental health problems are prevalent and resources are limited, are especially challenged [3]. Poverty and minority status have been found to be associated with an increased likelihood for psychological stress (e.g. from discrimination, fear of unemployment or underemployment), and mental health problems [3–5] and decreased likelihood of receiving treatment [6–8].
Federally-qualified health centers (FQHCs) provide an essential safety net for many underserved populations in the US [9]; they also face a number of challenges in providing primary care, mental health, and public health services responsive to their patients, i.e. patient-centered care. In the broader healthcare system, patient-centeredness has been identified as a key dimension of quality care [10]. However, most of what has been written about patient-centered care focuses on the patient–provider relationship, which is developed after the patient has made and kept an appointment, and is in the clinic sitting with the provider [10, 11]. This focus ignores much about what patient-centeredness could do outside this relationship to help healthcare systems improve patient access, satisfaction, and outcomes [12]. For example, before a patient–provider visit occurs, clinics need to inform patients about the availability, confidentiality, and quality of services. Once in the clinic, staff must help patients obtain the services they need, and assist them with treatment regimens, referrals, and recommendations.
The link between patient-centered care and quality is tightened further for the delivery of mental health services. In order to address the mental health needs of a population, patients’ (or clients’) needs must be identified and appropriate treatment offered and accepted. Patient preferences (e.g. language, cultural competency, less-stigmatizing locations) strongly affect whether patients see the providers who can identify them as having a need for mental health services [3, 4], and their preferences influence whether they get the care they need, both in terms of access and adherence [2–4, 13, 14].
There are a number of methodologies used to elicit patient preferences. One powerful set of methods—conjoint analytic (CA) methods—have been used extensively in the consumer-products industries to design products consumers want and will buy. These methods are also used in economics and, more recently, they have been applied to healthcare [15–19] and to patient preferences regarding mental health treatment [20–24], access [20–22, 24], messages [25], and outcomes [26].
CA methods evaluate patient choices and the associated tradeoffs made between bundles of care, i.e. sets of multilevel attributes relating to how they would receive such care [27]. Although CA methods depend on patient report about behavior in a future-choice situation, they are considered more valid than other self-report methods [19, 28]. Capturing patient report through complex, multi-attribute choice tasks reduces halo effects and social desirability biases [29]. The requirement that respondents evaluate competing options conjointly, and the resulting evocation of simplifying cognitive heuristics [30], both of which mimic real-world decisions, result in better predictions of future behavior than rating scales [28, 29, 31]. In fact, while newer to health contexts, this method has been used for decades by large corporations to make multimillion-dollar product design decisions [27]. Finally, CA can be used to evaluate interventions that do not currently exist (i.e. hypothetical treatments), allowing evaluation, including acceptability to patients, to commence before a program/intervention is implemented or even designed/developed [32, 33]. This allows for efficient program design, which is essential when resources are limited.
The current investigation sought to test the feasibility and usefulness of CA methods to improve the delivery of patient-centered mental health services in an FQHC serving a low-income Hispanic population. In this study, CA methods were tested as an add-on to qualitative methods (systematic focus group data collection and analysis) within a community-based participatory research (CBPR) framework. The specific research questions were as follows. (1) Is it feasible for a primary care-focused organization, in this case with the support of an academic partner in a participatory framework, to apply conjoint methods to design mental health services their patients want and will use? (2) Are the results from the conjoint analysis useful to the health center? Specifically, do conjoint methods result in a different package of mental health services than would be recommended using qualitative methods alone, and is the CA-informed package of mental health services likely to be more attractive to patients? (3) Are the extra effort and resources required of the health center and research-community partnership to utilize conjoint methods worth the additional information gained?
2 Methods
The setting for this study was a federally-qualified migrant health center (FQHC) serving a community of predominantly low-income Hispanics in the US–Mexican border region. The academic partner has a long-standing (20-year) relationship with this FQHC, including work on various projects using the CBPR approach. The FQHC and academic partner were the primary partners in this study, although additional methodological expertise was provided by collaborators at two other research-intensive institutions.
2.1 Community-Based Participatory Research
CBPR brings together researchers and community members to collaboratively ensure that the issues under study are relevant and that knowledge gained from the research effort benefits the community [34]. The FQHC’s leadership had specifically identified the incorporation of mental health services into primary care as a research topic for which they needed pragmatic and feasible solutions. The involvement of clinic staff and patients in identifying these solutions is intrinsic to the CBPR approach. As a first step, the FQHC convened a 12-member stakeholder group (including FQHC leadership, staff, and patients) to clarify their present level of mental health services, to facilitate ongoing and active participation of clinic stakeholders, and to ensure that study findings would be integrated into new feasible models of mental health care. Community health workers (CHWs), who have been part of the FQHC’s healthcare team since 1998, were central to all aspects of this CBPR project [35].
2.2 Qualitative Data Collection and Analysis
A team of four bilingual and bicultural FQHC CHWs, who underwent human subjects protection and focus group facilitation training, conducted eight focus groups onsite at the FQHC to elicit qualitative data on the community’s preferences for mental health services (64 patients in total; between 6 and 12 patients per group) [36]. Focus groups are a common data collection method used in CBPR [37]. Participants were recruited to ensure a range of patient perspectives—two groups each of patients (1) 20–45 years of age; (2) 65 years of age and older; (3) diagnosed with chronic disease; and (4) general patient population. All participants were consented. The focus groups were recorded and transcribed, and the research team coded and analyzed the data based on an adaptation of a conceptual map of dimensions and attributes of patient-centered care developed by Cheraghi-Sohi and colleagues [38]. The team presented findings regarding patients’ perceptions of mental health and their preferences for mental health-related services to the stakeholder group. Additional detail on the procedures and findings of these qualitative components are available in two recently published papers [35, 36].
2.3 Conjoint Analytic Methods
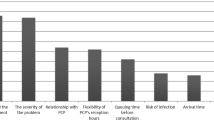
Following best practices for conjoint methods (including building on prior qualitative work), we collected data on patient preferences for mental health services using a survey-based discrete-choice conjoint experiment (DCE) with 15 choice tasks [32]. Each task asked respondents to choose between three mental health services options described by the levels of two (of eight) attributes (Fig. 1) [17, 39]. We used the themes that emerged from the analysis of the focus group data and the recommendations of the stakeholder group to identify eight attributes of mental health services likely to influence patients’ service utilization decisions [39, 40]. Since cost did not come up as an issue in the focus groups and since the clinic’s intent was to provide no-cost services to all patients, cost is not included as an attribute. For each attribute we composed three to four levels that were easily understood, salient to respondents, and plausible when combined in choice tasks (see Table 2) [39, 40]. Current care was one of the levels offered, and suggested improvements comprised the others. The description of each attribute level was finalized through an iterative process that included review by conjoint and DCE experts, review by the CHWs and FQHC leadership, by English to Spanish translation and Spanish to English back-translations, and by a pilot test. Our experimental design algorithm maximized variability in the choice tasks across respondents and generated 999 unique versions of the survey [39]. Each respondent was randomly assigned one version. The internet-based survey was programmed using Sawtooth Software’s SSI web version 8.2.4 (Orem, UT, USA).
Between March and August 2014, the CHWs approached adult patients in the waiting rooms of the FQHC’s three clinics. The CHWs administered the survey on laptop computers in English or Spanish. Before beginning the survey, participants were consented via a screen that assured confidentiality, and explained the study, the option to refuse participation, and their ability to withdraw without consequence.
Data were analyzed using Hierarchical Bayes (CBC/HB) analysis [39, 41–43]. This technique leverages choice data from all respondents to estimate part-worth utility coefficients (indicators of relative preference) for each respondent for each attribute level. Higher values of these coefficients reflect stronger preferences and they were standardized (zero centered) for comparability [44]. Importance scores, which indicate the relative influence of each attribute on participant choices, were computed by calculating the percentage of the total of the utility value ranges across all attributes that is each attribute’s utility value range [27].
Randomized first-choice simulations were used to examine various packages of care to determine those likely to be most attractive to patients. These simulations predicted the percentage of patients who would choose various hypothetical mental health services package options by assuming that, in general, each patient would choose the option that has the highest total utility but allowing for the fact that patients (like all of us) do not always make perfect choices [27, 45, 46]. More detail on the conjoint methods can be found in Herman et al. [47].
2.4 Evaluation of the Research Questions
Whether the application of CA methods was feasible in this FQHC (question 1) was determined by whether the FQHC provided ongoing support for the project and worked together with academic partner staff to successfully design the survey, field it, collect adequate data, and analyze the results.
Whether CA methods were useful (question 2) was evaluated using two criteria. First, we compared the components of the package of mental health services resulting from the qualitative analysis and the package of mental health services identified as most preferred from the conjoint results to see if they were different. To determine whether conjoint methods helped design a better (more attractive, more likely to be used) package of care, we simulated the proportion of patients who would likely choose each package of mental health services.
Finally, in order to determine whether the use of CA methods (beyond qualitative methods) was ‘worth it’ to the FQHC (question 3) we used feedback obtained from interviews with the FQHC’s leadership after they were presented with study results, and an accounting of the time and effort expended in the process. Throughout the study, staff time spent in all activities was captured, but this question focused on staff time involved in developing the DCE survey, recruiting for and fielding that survey, and analyzing its results. We asked FQHC leadership to consider whether the benefits from this approach were worth the effort and whether they would likely use conjoint methods again.
3 Results
CHWs administered the DCE survey to 604 adult patients across the three FQHC clinics waiting rooms. The participation rate was extremely high (over 99 %), with only five individuals refusing to take the survey, which is consistent with other studies using CHWs in this population [48]. Respondent characteristics are shown in Table 1. As can be seen, this is a mostly immigrant (24.8 % US born), Hispanic (98.3 %), and Spanish language-preferring (95.4 %) population. Although the clinic had few statistics on the characteristics of their patients, informal review of study demographics by clinic staff and the large sample size validate this sample as representative of the FQHC’s population. The average time to complete the survey was 13.5 min (standard deviation 4.8; median 12.3 min).
Table 2 shows the results of the conjoint analysis compared with current care and the focus group results. The level of each attribute that received the highest utility coefficient was the one indicated as being recommended according to the CA. As can be seen, the packages of care are different; thus, the conjoint methods were useful in those terms (first part of question 2). The attributes are shown in descending order of their importance scores, i.e. each attribute’s influence on patient choice (see Herman et al. [47]). As can be seen, where patients receive these services and the language spoken, as well as cultural awareness of the provider who screens them for these services, exerted the largest influence on mental health service choices in this population.
Table 3 shows the results of the market-share simulations. According to the choices patients made during the DCE, if they were given the choice of either current mental health services or a package including those attribute levels recommended by the qualitative data (see Table 2 for the attribute levels for each), 94 % would choose the focus-group-informed package. Thus, this new package of mental health services better matched patient preferences than what was currently available. However, when compared with the package of care composed of the levels of the attributes having the highest utility in the CA, the simulation shows that 77 % of patients would choose the conjoint package over that informed by the focus group results alone. Thus, in response to the second part of question 2, the package of mental health services resulting from the conjoint methods appears more attractive to patients.
To determine whether the results of the conjoint analysis were worth the effort, we presented the FQHC’s leadership with a summary of results and an accounting of the labor hours required to add conjoint analysis to the focus group methods. It was estimated that (leaving out initial learning time and assuming a sample size of 200, which should be sufficient to perform a similar analysis [27]), it would take approximately 122 h of FQHC staff time and 96 h of academic partner staff time to repeat the conjoint analysis. Benefits of the conjoint methods included determination of the attributes of mental health care that most influenced patient choices and the preferred level for each attribute, and the ability to simulate future choices in lieu of pilot/demonstration projects. FQHC leadership was mixed about whether the benefits of adding the conjoint analysis were worth it and whether they would do it again. They believed that the results generated were useful, e.g. ‘the information itself was extremely useful’. However, they thought that the extra time and effort required for the conjoint analysis would not likely be worth it for a ‘quick question’, but that it would possibly be useful for ‘a strategic long-term planning process’.
4 Discussion
This study examined the feasibility and usefulness of a rigorous consumer-preference product design method (conjoint analysis) to help an FQHC design mental health services that their patients would prefer and use. The application of these methods was feasible using an academic/health center partnership, and they generated a different and better-received (in terms of revealed patient choices) package of mental health services than current care or that informed by focus group results alone. However, while it can be concluded that the CA methods were useful in designing patient-centered mental health services, this same leadership also reported that the extra effort required to add the conjoint analysis would not likely be worth repeating for a brief question but might be for a larger strategic planning process.
There were some particularly unexpected and nuanced findings provided by the CA method. Given the enthusiasm the focus group participants had for various supportive services [35, 36] (e.g. talks on behavioral health, support groups, workshops), it was surprising that, on average, the preference was for none of these services to be offered. This could be because patients thought that these were a good idea in general but that when confronted with the actual option to attend they would not choose to participate. Another explanation may lie in the interactional nature of focus groups that may have either attracted different participants or had the effect of promoting these options through the group dynamic or social desirability biases [29, 49, 50]. Another difference seen was that the focus group participants frequently expressed their desire that the doctor take the time to ask how they were feeling [36]. This option did have the highest average utility across the screening levels tested; however, the low relative importance given this attribute (Table 2) suggested addressing it alone was not likely to substantially change patient receptivity, a result that was not obvious from the focus group results. Given these divergent findings, it is evident that different methodological approaches to addressing the preferences of primary care patients can yield results that lead to different recommendations for patient-centered care.
The usefulness of the conjoint methods was clearly illustrated in three ways: (1) it was possible to determine what was most important/what most influenced patient choices; (2) the preferred package of care that emerged from this method differed substantively from that which emerged through the rigorous qualitative data collection and analysis expected of well-conducted CBPR and patient-centered care research; and (3) the ability to simulate patient choices across hypothetical packages of care.
Regarding the first point, the importance scores calculated in conjoint analysis go beyond simple ranking; they indicate how much the levels of each attribute affect the package of mental health services a patient would choose when presented with options. From the importance scores, we learned that where services were located and the language/cultural awareness of the prescribing provider are not just ranked as important (see Herman et al. [47]), they are approximately equal in importance and have almost twice the influence on choices as the next most influential attribute. Knowing patient preferences across the levels available for each attribute also provides information. According to the estimated utilities (see Herman et al. [47]) the second most preferred level for the language/culture attribute was talking ‘to someone who speaks English but understands my culture’. This level was strongly preferred over talking ‘to someone who speaks Spanish, but does not understand my culture’, indicating that cultural understanding was more important to patient choice than having a Spanish-speaking provider. This was a surprise to FQHC leadership and not evident from the qualitative analysis.
We also found that CA is not a panacea for addressing patient-centered research questions. In this study clinic, leadership was not enthusiastic about applying this method to address additional questions in patient-centered care delivery. Although we did not include these hours in our time estimates, and emphasized that the question was about using these methods again, it is possible that their experience was negatively affected by learning-curve challenges, e.g. ‘took too long’. The FQHC’s leadership also noted that they were not in a position to implement all the recommendations made and would have to take ‘baby steps’. So the method might provide more information than a health center of this size can digest and use in a timely fashion. Nevertheless, as a result of this study, the clinic recently acquired funds to hire an onsite behavioral health specialist and provide other supportive services. Finally, it is also possible that taking on something simpler and less costly than adding mental health services to primary care could make the process more acceptable.
This study was conducted in one FQHC and addressed one question of interest to that clinic—how to incorporate mental health services that their patient population (low-income, Hispanic, Spanish-speaking) would prefer and utilize. Although this setting and sample has considerable contextual validity for this health center, the transferability of these results to other FQHCs should not be assumed. While the utilization of CHWs in this research undoubtedly improved the CA/DCE survey response rate, their presence during this survey could have affected participants’ responses despite the CHWs’ research training. Also, even though patients were not being asked about their current care, and although DCE has been shown to minimize social desirability bias [29, 50], it is possible that being recruited while awaiting care at the FQHC may have introduced some of this bias. Substantial effort was made to clearly describe the options included in the choice tasks. However, it is possible that respondents interpreted the options in ways other than was intended. Within the project timeframe it was not feasible to implement and observe actual patient response to alternative mental health services packages; we were limited to simulations. However, this is also one benefit of these methods—the ability to determine preferences across options prior to resources being dedicated to their full design and implementation. Finally, this was a study of the feasibility and usefulness of an FQHC working with an academic partner to add a DCE. It is unlikely that most FQHCs would have the expertise needed to design and analyze a DCE on their own.
5 Conclusions
Market research and the consumer products industries have helped develop and refine a set of methods (conjoint analysis) to capture consumers’ preferences and design successful products—products consumers want and will buy. This study explored whether these methods would be applicable to the design of improved patient-centered mental health service offerings in a primary care health center. The method was found to be feasible and useful in terms of providing more information than common qualitative methods used in patient-centered research and CBPR, and resulted in a package of mental health services that, according to market simulation, more of the health center’s population would use. However, in the present case the conjoint methods may have provided more information than leadership could fully act upon, and were deemed as likely to be repeated only for larger strategic planning efforts. Thus, while successful in most research aims, the methods may have further utility in ongoing monitoring and improvement for larger-scale primary care and public health delivery systems.
References
Croghan TW, Brown JD. Integrating mental health treatment into the patient-centered medical home. Rockville (MD): Mathematical Policy Research; 2009.
Kessler R, Stafford D. Primary care is the de facto mental health system. New York: Springer; 2008.
Caldwell A, Couture A, Nowotny H. Closing the mental health gap: eliminating disparities in treatment for Latinos. Kansas City: Mattie Rhodes Center; 2008.
Arcury TA, Quandt SA. Delivery of health services to migrant and seasonal farmworkers. Annu Rev Public Health. 2007;28:345–63.
Surgeon General. Mental health: culture, race, ethnicity. A supplement to mental health: a report of the Surgeon General. Washington, DC: US Department of Health and Human Services; 2001.
Miranda J, Cooper LA. Disparities in care for depression among primary care patients. J Gen Intern Med. 2004;19(2):120–6.
Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):629–40.
González HM, Vega WA, Williams DR, Tarraf W, West BT, Neighbors HW. Depression care in the United States: too little for too few. Arch Gen Psychiatry. 2010;67(1):37–46.
Grant R. A bridge between public health and primary care. Am J Public Health. 2012;102(Suppl 3):S304.
Institute of Medicine. Crossing the quality chasm: a new health system for the twenty-first century. Washington, DC: National Academies Press; 2001.
Agency for Healthcare Research and Quality. Chapter 5. Patient centeredness: national healthcare disparities report, 2010. Rockville : Agency for Healthcare Research and Quality; 2014.
Berry LL, Beckham D, Dettman A, Mead R. Toward a strategy of patient-centered access to primary care. Mayo Clin Proc. 2014;89(10):1406–15.
Sorel E, Everett A. Psychiatry and primary care integration: challenges and opportunities. Int Rev Psychiatry. 2011;23(1):28–30.
Lin P, Campbell DG, Chaney EF, Liu C-F, Heagerty P, Felker BL, et al. The influence of patient preference on depression treatment in primary care. Ann Behav Med. 2005;30(2):164–73.
Cunningham CE, Deal K, Rimas H, Campbell H, Russell A, Henderson J, et al. Using conjoint analysis to model the preferences of different patient segments for attributes of patient-centered care. Patient. 2008;1(4):317–30.
Fraenkel L, Gulanski B, Wittink D. Patient treatment preferences for osteoporosis. Arthritis Care Res. 2006;55(5):729–35.
Marshall D, Bridges JF, Hauber B, Cameron R, Donnalley L, Fyie K, et al. Conjoint analysis applications in health: how are studies being designed and reported? Patient. 2010;3(4):249–56.
Osman L, McKenzie L, Cairns J, Friend J, Godden D, Legge J, et al. Patient weighting of importance of asthma symptoms. Thorax. 2001;56(2):138–42.
Ryan M, Farrar S. Using conjoint analysis to elicit preferences for health care. BMJ. 2000;320(7248):1530.
Dwight-Johnson M, Lagomasino IT, Aisenberg E, Hay J. Using conjoint analysis to assess depression treatment preferences among low-income Latinos. Psychiatric Serv. 2004;55(8):934–6.
Dwight-Johnson M, Lagomasino IT, Hay J, Zhang L, Tang LQ, Green JM, et al. Effectiveness of collaborative care in addressing depression treatment preferences among low-income Latinos. Psychiatric Serv. 2010;61(11):1112–8.
Okumura Y, Sakamoto S. Depression treatment preferences among Japanese undergraduates: using conjoint analysis. Int J Soc Psychiatry. 2012;58(2):195–203.
Wittink MN, Cary M, TenHave T, Baron J, Gallo JJ. Towards patient-centered care for depression. Patient. 2010;3(3):145–57.
Wittink MN, Morales KH, Cary M, Gallo JJ, Bartels SJ. Towards personalizing treatment for depression. Patient. 2013;6(1):35–43.
Bell RA, Paterniti DA, Azari R, Duberstein PR, Epstein RM, Rochlen AB, et al. Encouraging patients with depressive symptoms to seek care: a mixed methods approach to message development. Patient Educ Couns. 2010;78(2):198–205.
Zimmermann TM, Clouth J, Elosge M, Heurich M, Schneider E, Wilhelm S, et al. Patient preferences for outcomes of depression treatment in Germany: a choice-based conjoint analysis study. J Affect Disord. 2013;148(2):210–9.
Orme BK. Getting started with conjoint analysis: strategies for product design and pricing research. 2nd ed. Madison: Research Publishers; 2010.
Ryan M, Scott D, Reeves C, Bate A, Van Teijlingen E, Russell E, et al. Eliciting public preferences for healthcare: a systematic review of techniques. Health Technol Assess. 2001;5:1–186.
Phillips KA, Johnson FR, Maddala T. Measuring what people value: a comparison of “attitude” and “preference” surveys. Health Serv Res. 2002;37(6):1659–79.
Payne J, Bettman J, Johnson E. The adaptive decision maker. Cambridge: Cambridge University Press; 1993.
Hsee CK, Loewenstein GF, Blount S, Bazerman MH. Preference reversals between joint and separate evaluations of options: a review and theoretical analysis. Psychol Bull. 1999;125(5):576.
Bridges J, Onukwugha E, Johnson F, Hauber A. Patient preference methods: a patient centered evaluation paradigm. ISPOR Connect. 2007;13(6):4–7.
Bridges J. Stated preference methods in health care evaluation: an emerging methodological paradigm in health economics. Appl Health Econ Health Policy. 2003;2(4):213–24.
Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19(1):173–202.
Ingram M, Murrietta L, de Zapien JG, Herman PM, Carvajal SC. Community health workers as focus group facilitators: A participatory action research method to improve behavioral health services for farmworkers in a primary care setting. Action Res. 2015;13(1):48–64.
Ingram M, Schachter KA, Guernsey de Zapien J, Herman PM, Carvajal SC. Using participatory methods to enhance patient-centred mental health care in a federally qualified community health center serving a Mexican American farmworker community. Health Expect. doi:10.1111/hex.12284 (Epub 10 Oct 2014).
Bergold J, Thomas S. Participatory research methods: a methodological approach in motion. FORUM: Qual Soc Res. 2012;13(1):30.
Cheraghi-Sohi S, Bower P, Mead N, McDonald R, Whalley D, Roland M. What are the key attributes of primary care for patients? Building a conceptual ‘map’of patient preferences. Health Expect. 2006;9(3):275–84.
Bridges JF, Hauber AB, Marshall D, Lloyd A, Prosser LA, Regier DA, et al. Conjoint analysis applications in health—a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health. 2011;14(4):403–13.
Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making. Pharmacoeconomics. 2008;26(8):661–77.
Lenk PJ, DeSarbo WS, Green PE, Young MR. Hierarchical Bayes conjoint analysis: recovery of partworth heterogeneity from reduced experimental designs. Mark Sci. 1996;15(2):173–91.
Sawtooth Software I. The CBC/HB system for hierarchical Bayes estimation version 5.0 technical paper. Sequim: Sawtooth Software, Inc.; 2009.
Halme M, Kallio M. Estimation methods for choice-based conjoint analysis of consumer preferences. Eur J Oper Res. 2011;214(1):160–7.
Orme BK. SSI Web V6.6 software for web interviewing and conjoint analysis. Sequim: Sawtooth Software, Inc.; 2009.
Orme B, Huber J. Improving the value of conjoint simulations. Mark Res. 2000;12(4):12–20.
Huber J, Orme BK, Miller R. Dealing with product similarity in conjoint simulations. In: Gustafsson A, Herrmann A, Huber F, editors. Conjoint measurement: methods and applications. 4th ed. New York: Springer; 2007. p. 347–62.
Herman PM, Ingram M, Rimas H, Carvajal S, Cunningham CE. Patient preferences of a low-income Hispanic population for mental health services in primary care. Adm Policy Ment Health (Epub 26 Sep 2015).
Carvajal SC, Rosales C, Rubio-Goldsmith R, Sabo S, Ingram M, McClelland DJ, et al. The border community and immigration stress scale: a preliminary examination of a community responsive measure in two southwest samples. J Immigr Minor Health. 2013;15(2):427–36.
Wilkinson S. Focus groups in health research exploring the meanings of health and illness. J Health Psychol. 1998;3(3):329–48.
Caruso EM, Rahnev DA, Banaji MR. Using conjoint analysis to detect discrimination: revealing covert preferences from overt choices. Soc Cogn. 2009;27(1):128–37.
Acknowledgments
The authors would like to acknowledge the partnership of the Sunset Community Health Center in carrying out this research, and the Sunset Community Health Workers who participated in research activities.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This work was supported through a Patient-Centered Outcomes Research Institute (PCORI) Pilot Project Program award (1IP2PI000275-01). The participation of Dr. Cunningham and Ms. Rimas was supported by the Jack Laidlaw Chair in Patient-Centered Health Care. Lucy Murrieta is an employee of the FQHC that was the subject of this research. With the exception of Ms. Murrieta’s employment status, all authors declare that they have no conflicts of interest, financial or otherwise, with respect to this research. Our study received exempt approval from the University of Arizona Institutional Review Board. Informed consent was obtained from all individual participants included in this study.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Herman, P.M., Ingram, M., Cunningham, C.E. et al. A Comparison of Methods for Capturing Patient Preferences for Delivery of Mental Health Services to Low-Income Hispanics Engaged in Primary Care. Patient 9, 293–301 (2016). https://doi.org/10.1007/s40271-015-0155-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-015-0155-7