Abstract
Background
The Patient Protection and Affordable Care Act (ACA) mandates the release of publicly available consumer reports to highlight differences in quality of care and reduce healthcare disparities. However, little is known about patient perceptions of the value of such reports.
Objective
This study aims to identify whether vulnerable populations with type 2 diabetes perceive consumer reports as helpful in making decisions about diabetes care.
Methods
We conducted a brief demographic survey and qualitative study of 18 focus groups: six each of African American, Hispanic, and non-Hispanic White consumers diagnosed with type 2 diabetes (n = 92). We analysed focus group transcripts to identify recurring themes, which were summarized and compared across population groups.
Results
Participants expressed minimal interest in currently available consumer reports. They instead listed personal referrals and interpersonal interactions among the most important factors when choosing a physician. Further, in place of information to aid in physician selection, participants articulated strong desires for more basic, straightforward disease-specific information that would promote diabetes self-management.
Conclusions
This study’s results call into question the value of consumer reports as defined by the ACA. Participants reported little interest in comparative provider performance data. Instead, they were more interested in information to assist in diabetes self-management. This suggests that consumer reports may not be as important a tool to improve outcomes and reduce health disparities as policy makers imagine them to be.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Patients, regardless of race and ethnicity, are far more interested in learning about diabetes self-management such as diet from public reports than in using public reports to select a physician. |
Many diabetes patients learn about physicians from friends and relatives rather than public reports. |
Developers of public reports must seek the input of vulnerable populations in order to reflect their values and perceptions about what should be included in these reports. |
Public reports may not be as important a tool in reducing health inequity as policy makers have imagined them to be. |
1 Introduction
For decades, the quality of care and healthcare service utilization has varied tremendously, with disparities experienced by vulnerable populations such as the poor, certain minorities, and other priority populations [1]. The Agency for Healthcare Research and Quality (AHRQ), the Institute of Medicine, and the Patient Protection and Affordable Care Act (ACA) have identified public reporting as one method of overcoming disparities. It is hoped that, by informing consumers through documented comparisons of provider group performance, the healthcare marketplace will influence change and encourage improvement [2–5].
One form of public reporting, the consumer report, has been developed with the explicit intention of assisting consumers in their healthcare decision-making processes. However, the authors of a Cochrane Collaboration review [6] concluded that there is “no evidence that public release of performance data changes consumer behavior or improves care.” A more recent review by Berger et al. [7] came to similar conclusions. Even with the growing investments of public funds in such reporting, consumer awareness and use of these reports remains extremely low [6, 8–13]. In part, this may be related to inadequate dissemination efforts. However, it may also be that policy makers lack an understanding of what information patients want. Despite the ACA’s emphasis on consumer empowerment and patient-centered care, few developers consult with consumers on what they would like to see in the reports.
If consumer reports are viewed as a potential avenue to reducing health disparities, it is important to learn how members of target vulnerable populations view them and what information they find most useful. This study focuses on a particular ‘vulnerable population of consumers’, minority and low-income individuals with type 2 diabetes, consistent with the AHRQ definition of vulnerable populations [14]. Diabetes is an increasingly prevalent public health problem, affecting 25.8 million people (8.3 %) in the USA in 2011 [15]. Certain populations, such as African Americans and Hispanics, are disproportionately affected. The prevalence of diagnosed diabetes was 66 % higher among Hispanics and 77 % higher among African Americans than among non-Hispanic White adults [15].
This study elicited reactions of vulnerable patients with type 2 diabetes to prototypical consumer reports. The aim was to determine whether scores on diabetes performance metrics satisfy the healthcare information needs of minority and low-income populations. The study’s overall aims were to determine (1) how public reports can be designed to address the varying information needs of vulnerable populations, including selection of healthcare providers, and (2) how the content of public reports can best reflect meaningful information that vulnerable consumers would actually use.
2 Methods
2.1 Participant Enrollment
For this qualitative study, patients with type 2 diabetes were recruited to join one of several focus groups aimed at addressing the two specific aims above. This study was approved by the Virginia Commonwealth University (VCU) and Rutgers Biomedical and Health Sciences’ Institutional Review Boards. Written informed consent was obtained, and participant confidentiality was strictly guarded. VCU researchers designed the project, recruited for and conducted the focus groups, and performed the quantitative survey analysis. Rutgers researchers provided input into project design and conducted the qualitative analysis. The co-authors from the other institutions provided valuable critique and input at each stage of the study and for this paper.
We used two different approaches to recruit participants: (1) through the VCU Health System ambulatory care clinics and (2) through local community churches. Eligible VCU participants were identified using the electronic medical record database. Inclusion criteria were previous diagnosis of type 2 diabetes, ability to speak and understand English or Spanish, and age 18–85 years. All potential VCU clinic participants identified were mailed an opt-out letter signed by the appropriate practice’s medical director, allowing them to decline participation prior to being contacted by researchers. To confirm eligibility, research staff reviewed the medical records of those who did not opt out. Eligible individuals were contacted by phone using a recruitment script. However, this method did not yield sufficient Hispanic participants, so additional recruitment was conducted at primarily Hispanic churches. The same eligibility criteria applied.
2.2 Data Collection
Focus groups were conducted from February to May 2013. The approach was consistent with standard recommendations for a minimum of three to four focus groups per population group [16]. The African American groups were conducted by a female African American moderator. The Hispanic groups were conducted in Spanish as requested by participants by a non-Hispanic White male who was fluent in Spanish. The non-Hispanic White groups were conducted by another non-Hispanic White male. Sessions lasted approximately 1 h.
Moderators used a semi-structured interview guide consisting of six open-ended (grand tour) questions as described by Crabtree and Miller [17] (see Fig. 1). Main questions in the semi-structured interview guide related to report information, report seeking and use, report content, comparative data and format, and dissemination. The main questions were followed by probes. The focus group guide is provided in the Electronic Supplementary Material. At the beginning of sessions, participants were shown examples of current consumer reports on diabetes and provided individual copies of three publicly available consumer reports from the 2012 quality initiatives of the following US states: Wisconsin (Wisconsin Collaborative for Healthcare Quality), Ohio (Health Collaborative), and California (Office of the Patient Advocate). These reports were randomly chosen from a list of the six existing diabetes consumer reports available at the time and identified by Virginia Health Information’s co-investigator (ML) since the work of the organizations that produce the reports are known through the Health Data National Organization. They were further selected to show various types of reports. All used the Health Effectiveness Data and Information Set (HEDIS) measures, and some included patient satisfaction. They compared performance on several measures, such as percentage of patients with a yearly retinal examination, percentage of patients with an hemoglobin A1c (within various ranges), percentage of patients tested for cholesterol, and percentage of patients with a yearly foot exam. All subjects completed a one-page paper demographic survey at the end of each session.
2.3 Analysis
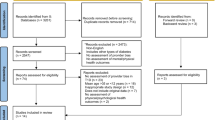
All focus groups were digitally recorded, translated (where appropriate), and transcribed prior to analysis. The qualitative team (BFC, MBP, and JH) used an ‘editing’ [18] approach based on grounded theory to analyze focus group data. This strategy was used because there was relatively little in the published literature on our study topic about how public reports are designed and how they are used by vulnerable populations; the editing approach allows for analysts to remain open to interpretation and theme generation. Transcripts were read for meaningful segments of text, which were then cut, pasted, and rearranged to create summaries of each focus group that highlighted recurring themes. All members of the qualitative team then read and discussed these segments in order to reach a final interpretation. The group was treated as the unit of analysis, with each focus group analyzed separately. Figure 2 depicts the overall analysis strategy.
As all focus groups were completed before analysis started, a strategy was designed in which the six transcripts from each racial/ethnic population were clustered into two groups of three. Analysts wrote a short summary for each of the first three focus groups in each population and then compiled a combined summary for each of the initial triads. This process was repeated for the second triad in each population using what was learned from the first triad to confirm or disconfirm emerging patterns. The analysts then met as a team to review each triad summary and distill the significant patterns and themes reflected in each. Thereafter, they looked across patterns and themes from the two triads for each race/ethnicity and extracted a coherent pattern within each. There was remarkable consistency between the two sets of triads, thus confirming saturation. Finally, the team identified similarities and differences across the patterns and themes of the three population groups and discussed these with the larger team for confirmation.
Although the editing method and thematic summaries constituted the bulk of the analytic work, the team also coded the transcripts in Atlas.ti 7.5.4 (2015, Cleverbridge, Inc., Chicago, IL, USA) to assist in data organization and facilitate quotation identification. The codebook was created on the basis of themes that emerged from the group summaries [18]. Rutgers researchers (BC, MBP, JH) coded two transcripts together, and then two analysts (MBP, JH) divided up the remaining transcripts to code individually. Uncertainties in coding and proposed new codes were discussed with the team.
3 Results
3.1 Population Characteristics
Table 1 shows participant characteristics by race and ethnicity. Participants (n = 92) (range of three to eight per group) were organized into 18 focus groups. Hispanic participants were significantly younger per group than African Americans and non-Hispanic Whites. Overall, there were significantly more female than male participants. More participants reported having their diabetes under control (51 %) than not (20 %) or not knowing (29 %). Nearly all participants reported low ($US25,000/year) to modest ($US25,000–49,999/year) income, but non-Hispanic White participants had significantly higher incomes than other groups, with none reporting $US25,000/year.
3.2 Qualitative Results
Themes reported below include those that were most closely aligned to the original research question (the usefulness of consumer reports) and those we did not anticipate but for which participants expressed a great deal of passion.
3.2.1 Comparative Information on Physician Quality Indicators is Not Desired
The vast majority of participants agreed that the information in consumer reports was not helpful in making healthcare decisions. Of all groups, non-Hispanic White participants were most familiar with consumer reports; however, they repeatedly questioned their utility. The technical nature of the information presented therein was a common concern. One African American participant said the report,
“…seemed to talk in a very high level. I was looking for more specifics that would affect me and different things that would help me. But it seemed to be very general what was there and no depth of information that I was looking for.”
This concern was echoed in a second African American group:
Woman 1: “This is not enough because your average person—what is LDL? You know? What is that? What is A1c?”
Woman 2: “When you get into all these little teeny types and percentages and stuff and words all over, I would just get lost in that.”
Woman 1: “The average person, they’re not gonna use it.”
The above quotes illustrate how a discussion of the reports pushed patients to ask for disease management information. In a third African American group, a woman who had only been diagnosed with diabetes a short time emphasized that, especially for a new patient, the reports were “confusing” and she questioned the usefulness of such information, “I mean how does it affect me that different healthcare providers…, they’re comparing…. You know, how is that useful? That doesn’t seem to be useful to me.”
Minority groups seemed less familiar with consumer reports. Many admitted they had not seen them. Even when repeatedly redirected to the reports, participants consistently discussed other information they would use either in selecting a physician or in self-managing diabetes. The following conversation took place in one non-Hispanic White group when the moderator asked if the participants had seen the consumer reports at hand.
Woman: “And when I was first diagnosed, I was given literature. So any time I’m anywhere and I see something on it, I pick it up anyway. So that’s how I get all my information.”
Moderator: “Okay. So have any of you ever seen these reports that—things like the ones what you have in your hands?”
Woman: “I haven’t. I’ve never seen it.”
Aside from being too technical, the comparative performance data in consumer reports may lack value because participants’ choice of physician is inevitably limited by the acceptance of their insurance. Non-Hispanic White participants often cited health insurance requirements to explain why they saw little need for information they might use in physician selection. For example, one man explained: “This is another one because when you don’t have good insurance you have to go where they tell you for people with low income, when you can’t pay for the costs.”
3.2.2 Participants Rely on Other Means of Selecting Physicians that Cannot be Expressed in Consumer Reports
When asked by moderators how they would select another doctor if theirs were to relocate, participants across all groups cited referrals from friends, family, or their current physician as their preferred method. One non-Hispanic White man shared his experience:
“Well, I have a friend that had diabetes. He had gone to this clinic that I went to when I first was diagnosed. I knew that he had, and I asked him did he like it and was it informative and did he get anything out of it? Did he feel like it was beneficial to his care? He recommended it, and that’s why I went.”
When asked how he chose his doctors, one Hispanic man expressed a similar experience that was common in that group: “Asking people. I mean like asking the people we know near where we live. I mean like asking what doctors they go to, and then you choose one.”
Aside from referrals, participants’ choices to use particular physicians were based on characteristics that were less about performance measures and more about how care is provided. Non-Hispanic White and African American participants commonly expressed that good rapport is the most important factor in selecting a physician. One woman elaborated:
“When you go to a doctor or any place, if you go across the door and that person makes you think that you’re the only person in the world, and not all these other people in your waiting room, then I can relate to that person because I figure they care they’re there to help me.”
Another African American participant further emphasized the importance of personality, saying she would meet with multiple physicians before selecting one:
“I would like to meet with both of them, to see what type of manner they are, how comfortable I feel with them. If I feel rushed or I feel like they really are interested in hearing what my story is. And that would help me to decide.”
The time factor was valued by many participants; they want doctors who, as one phrased it, would “really take time with me” and “take time with my personal individual need.”
These physician characteristics, which are obviously important to participants across all groups, are beyond the scope of a consumer report. Several, in fact, would be difficult to derive from any report and instead require personal interaction.
3.2.3 Although Consumers Saw Little Value in a Consumer Report, They Did Express the Desire for Basic Information in Lay Language About Various Aspects of Diabetes Care, Especially Diet
While participants did not feel that reports containing comparative physician quality indicators would improve their care, they consistently expressed a desire for basic information about diabetes care, particularly related to diet. Although not directly related to consumer reports, this theme is reported on because of the great interest and enthusiasm expressed by participants and the amount of time they spent discussing the desire for information for self-management. Concern and confusion with issues around diet generated the most conversation and energy within all groups. The following was typical when participants were asked what they would like to know more about:
Man: “The nutrition because the doctors tell us we can eat rice, not too much rice; you can eat bananas, one banana or half a banana [but if] the banana is large, half of that is the same as a small one. I mean what portions….”
Similar conversations took place in the other groups, each highlighting different aspects of diet that were perceived as confusing or challenging. An excerpt from an African American group is illustrative:
Woman 1: “Nutritional information is like the utmost important.”
Woman 2: “It is.”
Woman 1: “Because that’s the main thing we’ve got to do….”
Woman 2: “Well, nutrition is important, but the fresh fruits and vegetables that you actually need, and like salmon and the fresh fish, it’s so hard, even if you want to do it, you can’t do it all the time. Unless you’re in that income bracket.”
Moderator: “So would information about eating healthy on a budget be something….”
Woman 1: “Mm-hm. Exactly.”
Woman 2: “Yes.”
Non-Hispanic White participants also indicated that information about diet was their top priority. For example, a female respondent said: “The whole total thing is your diet. …what I should eat and what I shouldn’t eat…. I think that’s my big thing is just I really need to know more about the diets.” Another woman from a different non-Hispanic White group said: “I just want enough for me to learn what to eat and what not to eat.”
A number of respondents noted that this basic health information should be provided in understandable language. For example, a non-Hispanic White female respondent said, “And use everyday language instead of big old words.” Similarly, an African American male respondent noted, “[Present it in a way] that anyone can understand. Bring it down to earth so we can understand. Bring it all the way down cause if you don’t, we’re lost.”
3.2.3.1 Means of Dissemination of Such Basic Diabetes Information is Particularly Important When Trying to Reach Minority Groups
The modes of disseminating information, especially that aimed at minority groups, is equally important to the nature of the information. Electronic distribution is not ideal. While non-Hispanic White participants commonly described the Internet as a preferred source of diabetes information, Hispanic and African American respondents reported low Internet usage. A comment by this Hispanic woman was characteristic: “…not all of us have Internet access to look for that information, or some of us do have computers but we don’t know how to use it….” A similar message was prominent in African American groups; one woman said, “We were talking about the Internet and stuff, but a lot of us don’t have access to computers or we’re not computer literate enough to know exactly how to go in and research and get information.”
Focusing solely on electronic formats of the information these groups desire and need may neglect these target populations. Instead, it seems that clinicians and diabetes educators may be preferable disseminators.
Participants in both the Hispanic and African American groups felt strongly that doctors were their most trusted source for information about diabetes. This was not the case for non-Hispanic White groups. This woman’s statement reflects a common perspective in Hispanic groups:
“Personally, the word doctor for a Hispanic person is like saying a priest. For us the doctors have a very important position, and they can solve anything. So many times in our culture we don’t look for the doctor’s résumé or to know if he knows something about diabetes.”
A woman from another Hispanic group said: “We don’t really look for information because we are only guided by the doctor.” Similar opinions were expressed in all three African American groups.
Moderator (group 1): “If you have questions about diabetes care, what’s your first step to seek information?”
Woman (group 1): “[My] doctor.”
Man (group 2): “My doctor; basically that’s my source for everything.”
Woman (group 3): “My first source of information when it comes to my health, period, is I go to my doctor.”
Non-Hispanic White participants indicated much less reliance on physicians as a source of diabetes information, but they did consistently express that they sought information from other sources, including the Internet. Therefore, doctors may not be as important a source of information for non-Hispanic White patients as they are for minority groups.
4 Discussion
We found that, by and large, consumers did not feel that provider quality measures could be useful to them in selecting a provider. This is consistent with previous literature on consumer use of provider quality measures. For example, regardless of race/ethnicity, participants had minimal interest in the provider performance information from consumer reports. This is consistent with the review by Totten et al. [19] of articles between 1980 and 2011, which found that, among other things, “public reporting is more likely to be associated with changes in health care provider behaviors than with selection of health services providers by patients or families.” In our study, this may at least partially be because participants in all three populations indicated they had little choice in selecting their physicians. Most indicated that insurance dictated limited choice in physician selection. This may be different in other insurance markets with wide choice in provider selection.
If the option to choose a physician presented itself, all groups strongly valued personal referrals from friends and other doctors as a means of identifying candidates. This is consistent with the study by Kolstad and Chernew [20], which reports “consumers obtain information on [health] plan quality from a litany of sources. These include informal sources such as friends, coworkers or families.” When choosing one doctor over another, our participants cited rapport and time spent with patients as factors that were much more important than the specialized metrics in consumer reports. A number of studies have found that measures such as provider communication skills and courtesy are valuable to consumers [20]. However, the sample reports to which we had access did not include such measures. This has clear implications for those promoting, developing, and distributing consumer reports, and measures of patient experience may have greater salience for helping patients choose providers than the performance measures used in the reports we presented to patients.
Our participants felt instead that diabetes care could be improved not by comparative information on physician metrics, but by better health education and disease-specific resources that promote self-management. Due to the complexities of living with diabetes, vulnerable populations have unmet needs for quite basic information about the disease and its management. Comparative data regarding physician performance might be a desire only after basic information needs regarding diabetes are met [21], but our study cannot directly address that possibility. In the meantime, clinicians need to meet the challenge of providing these patients with what several participants referred to as “plain language” information that can best assist them with diabetes self-management. Interestingly, Hibbard et al. [22] also reported the positive effect of using what they also refer to as “plain language” information for consumers.
Patients, in general, should expect their physicians to thoroughly educate them about diabetes, either directly or by pointing them toward good sources of information. Our African American participants, contrary to findings in other studies that report mistrust of physicians and the healthcare system [23], reported trust in their existing clinicians. Literature on Hispanic culture is consistent with our finding that, given the respect reported by Hispanics for their physicians, some patients may neither ask for clarification nor express inability to understand information provided [24]. The trust placed in doctors by these minority groups, combined with lower Internet usage than non-Hispanic White counterparts, suggests that educational efforts for Latinos and African Americans may be more effective if the physician is directly involved as an information source.
This study has a number of limitations. First, all participants had established primary care providers. Perhaps when a patient is searching for a new provider, comparative performance information could be more relevant. However, participants’ comments about the overriding importance of providers’ interpersonal skills and referrals from friends as well as limited choice due to insurance restrictions suggest that comparative performance reports may have limited relevance even when searching for a new provider.
Second, we were unable to recruit Hispanic participants from the VCU clinic because very few seek care there as a result of their immigration status. This is a long-standing problem in the Richmond area. Consequently, our Hispanic sample came from local churches. This population seeks care from free clinics where questions about immigration status are not asked. We did not acquire insurance or employment information from participants, so we do not know the extent to which this recruitment issue may have systematically affected our sampling.
Our sampling may have also influenced our finding that African American participants trust their physicians. This is not consistent with the literature, which suggests that this population tends to have low trust of the medical system. In our focus groups, African Americans expressed great loyalty to their personal physicians and hence felt no need for a consumer report that would help them change physicians. These results stand in marked contrast to the vast majority of literature that documents African Americans’ mistrust of the “healthcare system,” starting with the exposure of the Tuskegee experiments [25, 26] and including the mistrust of “clinical trials” or “experiments” [27–29] and concerns about an HIV vaccine [30, 31]. Our findings are consistent with the work of Sinaiko and Rosenthal [32], in which study participants expressed feelings about their personal physician as opposed to the healthcare system. Thus, one must take care in drawing conclusions about loyalty to and trust in one’s personal physician in contrast with healthcare system loyalty. Because our African American sample was recruited from the clinic setting and therefore had primary care physicians, perhaps they displayed trust of their particular doctor, not necessarily the medical system in general.
Unfortunately, we did not collect data on education or literacy, which would be helpful in exploring other conclusions to be drawn about minority groups. However, such studies must take into account the consumer choice may be more about ‘activation’ than it is about literacy or comprehension [33]. Future studies should collect and analyze such data.
Another potential limitation is that there was no racial/ethnic concordance between moderator and participants in the Hispanic focus groups, while there was in the other groups. However, our moderator was fluent in Spanish, and nothing in the transcripts suggested this was a barrier to free expression of participants’ viewpoints.
Finally, we cannot estimate the extent to which our findings generalize to other geographic regions, health conditions, or populations. Importantly, we cannot generalize our findings to higher-income populations. Further study in other populations is clearly needed.
Despite its limitations, our research suggests that consumer reports may not be as important a tool in reducing health equity as policy makers have imagined them to be. Patients such as those who participated in this study may instead use other means when selecting a provider. Our study employs an hypothesis-generating methodology. Thus, it is clearly appropriate to conclude that there is a signal from this study that warrants further work to test the hypothesis—are consumer reports a reliable means of reducing disparities?
References
Agency for Healthcare Research and Quality. 2013 national healthcare quality report. http://www.ahrq.gov/research/findings/nhqrdr/nhqr13/index.html. Accessed 4 Aug 2014.
Agency for Healthcare Research and Quality. Consumer assessment of healthcare providers and systems. https://www.cahps.ahrq.gov. Accessed 30 Jan 2012.
Agency for Healthcare Research and Quality. Public reports on provider performance for consumers. http://www.ahrq.gov/path/publicreporting.htm. Accessed 30 Jan 2012.
Agency for Healthcare Research and Quality. Quality indicators. http://www.qualityindicators.ahrq.gov/. Accessed 7 Jan 2012.
Patient Protection and Affordable Care Act, 2010. H.R. 3590, 111th Congress of the United States of America.
Ketelaar NA, Faber MJ, Flottorp S, Rygh LH, Deane KH, Eccles MP. Public release of performance data in changing the behaviour of healthcare consumers, professionals or organisations. Cochrane Database Syst Rev. 2011;11:CD004538.
Berger ZD, Joy SM, Hutfless S, Bridges JF. Can public reporting impact patient outcomes and disparities? A systematic review. Patient Educ Couns. 2013;93:480–7.
Fung CH, Lim Y, Mattke S, Damberg C, Shekelle PG. Systematic review: the evidence that publishing patient care performance data improves quality of care. Ann Intern Med. 2008;148:111–23.
Hannan EL, Cozzens K, King SB 3rd, Walford G, Shah NR. The New York state cardiac registries: history, contributions, limitations and lessons for future efforts to assess and publicly report health care outcomes. J Am Coll Cardiol. 2012;59:2309–16.
Anonymous. Public reporting as a quality improvement strategy: a systematic review of the multiple pathways public reporting may influence quality of health care. http://www.effectivehealthcare.ahrq.gov/ehc/products/343/763/CQG-Public-Reporting_Protocol_20110817.pdf Accessed 30 Jan 2012.
Elixhauser A, Parker J, Pine M, Andrews R. Improving administrative data for public reporting. Agency for Healthcare Research and Quality (AHRQ) Annual Conference: Promoting Quality. Partnering for Change, Bethesda, 9 September 2008.
Bardach NS, Hibbard JH, Dudley RA. Users of public reports of hospital quality: who, what, why and how? An aggregate analysis of 16 online public reporting web sites and users’ and experts’ suggestions for improvement. http://archive.ahrq.gov/professionals/quality-patient-safety/quality-resources/value/pubreportusers/index.html. Accessed 30 Jan 2012.
Schauffler H, Mordavsky J. Consumer reports in health care: do they make a difference? Annu Rev Public Health. 2001;22:69–89.
Dorsey CJ, Murdaugh CL. The theory of self-care management for vulnerable populations. J Theor Constr Test. 2003;7:43–9.
Centers for Disease Control and Prevention. National diabetes fact sheet: National estimates and general information on diabetes and prediabetes in the United States; 2011. http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf. Accessed 12 Mar 2012.
Krueger RA, Casey MA. Focus groups: a practical guide for applied research. 4th ed. London: SAGE; 2009.
Crabtree BF, Miller WL. Doing qualitative research. 2nd ed. Thousand Oaks: Sage Publications; 2000.
Addison RB. A grounded hermeneutic editing approach. In: Crabtree BF, Miller WL, editors. Doing qualitative research. Thousand Oaks: Sage Publications; 1999. p. 145–61.
Totten AM, Wagner J, Tiwari A, O’Haire C, Griffin J, Walker M. Closing the quality gap: revisiting the state of the science (vol. 5: Public reporting as a quality improvement strategy). Evid Rep Technol Assess (Full Rep). 2012;(208.5):1–645.
Kolstad JE, Chernew ME. Quality and consumer decision making in the market for health insurance and health care services. Med Care Res Rev. 2009;66(1 Suppl):28S.
Longo DR, Woolf SH. Rethinking the information priorities of patients. JAMA. 2014;311:1857–8.
Hibbard JH, Greene J, Daniel D. What is quality anyway? Performance reports that clearly communicate to consumers the meaning of quality of care. Med Care Res Rev. 2010;67:275–93.
Halbert CH, Armstrong K, Gandy OH Jr, Shaker L. Racial differences in trust in health care providers. Arch Intern Med. 2006;166:896–901.
Hispanic health in the United States. Council on scientific affairs. JAMA. 1991;265:248–52.
Brandon DT, Isaac LA, LaVeist TA. The legacy of Tuskegee and trust in medical care: is Tuskegee responsible for race differences in mistrust of medical care? J Natl Med Assoc. 2005;97:951–6.
Kennedy BR, Mathis CC, Woods AK. African Americans and their distrust of the health care system: healthcare for diverse populations. J Cult Divers. 2007;14:56–60.
Lagnado L. When racial sensitivities clash with research. Wall St J (East Ed). 1997;B1:B5.
Harris Y, Gorelick PB, Samuels P, Bempong I. Why African Americans may not be participating in clinical trials. J Natl Med Assoc. 1996;88:630–4.
Scharff DP, Mathews KJ, Jackson P, Hoffsuemmer J, Martin E, Edwards D. More than Tuskegee: understanding mistrust about research participation. J Health Care Poor Underserved. 2010;21:879–97.
Katz RV, Kegeles SS, Kressin NR, Green BL, James SA, Wang MQ, et al. Awareness of the Tuskegee syphilis study and the US presidential apology and their influence on minority participation in biomedical research. Am J Public Health. 2008;98:1137–42.
Westergaard RP, Beach MC, Saha S, Jacobs EA. Racial/ethnic differences in trust in health care: HIV conspiracy beliefs and vaccine research participation. J Gen Intern Med. 2014;29:140–6.
Sinaiko AD, Rosenthal MB. The impact of tiered physician networks on patient choices. Health Serv Res. 2014;49:1348–63.
Hibbard JH, Peters E, Dixon A, Tusler M. Consumer competencies and the use of comparative quality information: it isn’t just about literacy. Med Care Res Rev. 2007;64:379–94.
Acknowledgments
Shannon D. Jones moderated the African American focus groups, Melissa Hayes and Justin Lee recruited participants for the focus groups, and Dr. Mark Ryan and Dr. Carmen Zorrilla provided support to Dr. Lee with regard to the Hispanic focus groups. Heather Longo provided editorial services.
Author contributions
Drs. Longo and Crabtree had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Longo, Lundberg, Hannan. Acquisition of data: Longo and Lee. Analysis and interpretation of data: Longo, Crabtree, Pellerano, Howard, Sabo. Critical revision of the manuscript for important intellectual content: Longo, Crabtree, Pellerano, Howard, Saver, Hannan, Lundberg, Sabo. Qualitative analysis: Crabtree, Pellerano, Howard, Longo. Administrative, technical, and material support: Longo and Lee. Study supervision: Longo and Crabtree.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the appropriate Institutional Review Boards and has been performed in accordance with the ethical standards of the Declaration of Helsinki.
Informed consent was obtained from all individual participants included in the study.
Conflict of interest disclosures
The authors (Longo, Crabtree, Pellerano, Howard, Saver, Hannan, Lee, Lundberg, and Sabo) have completed and submitted the Adis Form for Disclosure of Potential Conflicts of Interest, and none were reported.
Funding/support
Funding by the Agency for Healthcare Research and Policy (AHRQ) grant number 1R21 HS021902-01.
Role of the sponsor
The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Prior presentations
Longo DR, Wright B, Lee J. Public reporting as a communication tool to aid vulnerable consumers in healthcare decisions: what do we know? AcademyHealth; Annual Research Meeting, Baltimore, MD, USA; 23 June 2013.
Lee J, Longo DR, Crabtree B, Howard J, Pellerano M. What do patients who are vulnerable want in publicly available health care consumer reports? AcademyHealth; Annual Research Meeting, San Diego, CA, USA; 10 June 2014.
Longo DR. Engaging vulnerable consumers in developing useful public health reports. AHRQ Building the Science of Public Reporting: Grantee Meeting at Academy Health; 10 June 2014.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Longo, D.R., Crabtree, B.F., Pellerano, M.B. et al. A Qualitative Study of Vulnerable Patient Views of Type 2 Diabetes Consumer Reports. Patient 9, 231–240 (2016). https://doi.org/10.1007/s40271-015-0146-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-015-0146-8