Abstract
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by a new species of β-coronavirus genus named severe acute respiratory syndrome coronavirus 2. The COVID-19 pandemic, which started in late 2019 and continues as at mid-2021, has caused enormous damage to health and lives globally. The urgent public health need has led to the development of vaccines against COVID-19 in record-breaking time. The COVID-19 vaccines have been widely rolled out for the masses by many countries following approval for emergency use by the World Health Organization and regulatory agencies in many countries. In addition, several COVID-19 vaccine candidates are undergoing clinical trials. However, myths, fears, rumors, and misconceptions persist, particularly in regard to adverse events. In this commentary, we describe the adverse events associated with COVID-19 vaccines and discuss why it is essential to have a functional adverse event monitoring system in this context.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A small number of vaccines against COVID-19 have been authorized since 2020. |
Pharmacovigilance systems are imperative to ensure the safety of COVID-19 vaccines. |
Active pharmacovigilance monitoring involving all stakeholders of COVID-19 vaccination is needed to prevent and document possible adverse events related to COVID-19 vaccines. |
Background
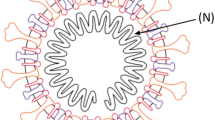
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by a new species of β-coronavirus named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1, 2]. It is a single-stranded RNA β-coronavirus whose genome encodes structural proteins, nonstructural proteins, and accessory proteins [3, 4]. Since its outbreak in late 2019, the virus has spread globally, creating global health, socioeconomic, and humanitarian crises [5,6,7]. Globally, as of 19 June 2021, more than 183 million confirmed cases of COVID-19 and almost 4 million deaths have been recorded [8, 9]. The high transmission rate of the virus means the numbers of confirmed cases are increasing exponentially, with new mutational variants also contributing. In addition, the mortality rate is higher in elderly patients and those with preexisting health conditions [10,11,12].
Thus far, the lack of effective treatment means vaccination, alongside other public health mitigation measures such as hand hygiene and social distancing, remains the only pathway to suppression of the virus and release from the pandemic. As a result, many governments have approved the rollout of some vaccines through emergency approval procedures, and several clinical trials are ongoing worldwide to find specific treatments and vaccines for COVID-19 [13,14,15]. However, fears, rumors, and misconceptions persist, particularly regarding COVID-19 vaccines. This article aims to provide information about the currently approved vaccines and the adverse events reported thus far and to discuss why excellent adverse event monitoring systems are vital.
Approved Vaccines and Ongoing Trials
As of 19 June 2021, 78 vaccine candidates are in development in 201 different ongoing trials. Among them, 12 vaccines were approved by the US FDA, the World Health Organization (WHO) and the European Medicines Agency (Table 1) [16].
As the virus is spreading widely in the population and causing infections, many new variants are emerging. Researchers believe that COVID-19 vaccines currently in development or already approved induce a broad immune response, so they are expected to give at least some protection against future viral strains. However, data are being collected to analyze the effectiveness of COVID-19 vaccines on new variants [27]. For example, in Qatar, a study was conducted to assess the effectiveness of the Pfizer–Biotech COVID-19 vaccine against the variants of concern, such as B.1.1.7 (α variant; WHO classification) and the B.1.351 (β variant; WHO classification), found that people who received two doses of the Pfizer–BioNTech vaccine were 75% less likely to develop a case of COVID-19 caused by B.1.351 (β) than were unvaccinated people [28].
Adverse Events with COVID Vaccines
Almost all vaccines for COVID-19 cause common side effects such as pain and swelling at the injection site, fever, chills, fatigue, joint pain, nausea, muscle soreness, and headache. In addition, some adverse events observed throughout the clinical trials are unique to specific vaccines, such as neutropenia with the AstraZeneca/Oxford vaccine [29], heart palpitations with Sputnik V, and vomiting with the CanSino vaccine [30]. Nevertheless, the findings from various clinical trials of COVID-19 vaccines concluded that the vaccines were well-tolerated and had a favorable safety profile. That has supported the large-scale evaluation of COVID-19 vaccines in the ongoing phase III trials and emergency use authorization by regulatory bodies in most countries [18, 26]. Table 2 summarizes the common adverse events from approved vaccines reported in clinical trials.
Post-authorization Experience
As at 14 June 2021, the Centers for Disease Control and Prevention (CDC) have recorded more than 3500 reports of side effects from people in the USA who have received COVID-19 vaccines. The CDC data also revealed hospitalizations of those receiving COVID-19 vaccines [44]. Summaries of their symptoms include heart palpitations, severe abdominal pain, seizures, and “almost stroke-like symptoms.” Several people have also reported that they could not breathe after receiving the shot [46].
According to the CDC report from 14–23 December 2020, 21 cases of anaphylactic reaction out of 1,893,360 first doses of the Pfizer vaccines were detected in the USA [46]. In addition, from 21 December 2020 to 10 January 2021, ten cases of anaphylactic reaction out of 4,041,396 first doses of Moderna vaccines were detected in the USA [47]. Anaphylactic reactions were treated with epinephrine and recovered fully [46]. Additionally, few people who received the Moderna vaccine were diagnosed with Bell’s palsy (facial nerve paralysis) [48]. At the same time, it is important to remember that COVID-19 caused such palsy before vaccinations started [49]. In Estonia, vaccination with Pfizer and Moderna vaccines began around December 2020 [50]. A total of 158 side effects have been reported to the medicines agency, two of which were severe. One person developed a hypersensitivity reaction 10 minutes after receiving the dose. Another vaccinated person developed a visual impairment; speech disorder; malaise; numbness of the nose, nasopharynx, and lips; and limb tenderness 2 days after receiving the second dose. Treatment was required, and the person recovered fully [50]. However, researchers are still figuring out whether these reactions are related to the core ingredients of the vaccine.
Several rare but serious adverse reactions have been reported in the postmarketing surveillance of COVID-19 vaccines. For instance, according to a retrospective descriptive study using spontaneous reports submitted to the EudraVigilance database from 17 February to 12 March 2021, of the 54,571 adverse reactions to the AstraZeneca vaccine, 28 were thrombotic events [51]. In addition, during postauthorization use of the Janssen COVID-19 vaccine, thrombosis involving large blood vessels, including the cerebral venous sinuses, portal vein, lower extremity veins, and pulmonary artery, combined with thrombocytopenia, have all been reported [52].
According to the CDC, since April 2021, more than 1000 cases of myocarditis and pericarditis have been reported to the Vaccine Adverse Event Reporting System after messenger RNA COVID-19 vaccination (i.e., Pfizer–BioNTech, Moderna) in the USA [53]. Moreover, on 25 June 2021, the FDA revised the patient and provider fact sheets regarding the suggested increased risks of myocarditis and pericarditis following vaccination [54]. However, data on postmarketing surveillance of other COVID vaccines are limited.
Monitoring and Reporting of Adverse Events
Monitoring the safety of vaccines is essential to improve safety profiles and enhance public trust. In Canada, the vaccine-associated adverse events surveillance program is involved in the Division of Immunization’s spontaneous voluntary reporting system for adverse reactions to vaccines. Individual case reports and standardized causality assessment by the multidisciplinary expert team are critical [55]. The WHO Programme for International Drug Monitoring provides a safety surveillance manual for COVID-19 vaccines that mandates several requirements for the safety of COVID-19 vaccines to be met [56]. In addition, regional and national pharmacovigilance centers within different countries can manage the pharmacovigilance of COVID-19 vaccines [56]. A study by Soldatos et al. [57] showed that pharmacovigilance played a considerable role in improving vaccine safety [57].
Pharmacovigilance, which relates to the systematic detection, reporting, assessment, understanding, and prevention of adverse reactions [58, 59], is an essential aspect of surveillance to ensure the safety of COVID-19 vaccines. Scientists around the globe are working collaboratively to develop safe and effective vaccines to end the pandemic. However, the rapid development of COVID-19 vaccines has raised concerns about their safety, contributing to vaccine hesitancy [60]. For example, in a scoping review conducted to assess healthcare workers' hesitancy to receive COVID-19 vaccines, concerns about vaccine safety, efficacy, and potential side effects were the main reasons for COVID-19 vaccination hesitancy [61]. Therefore, it is essential to address such concerns by providing evidence-based information through established public health and regulatory bodies.
Effective communication practices, positive framing of mild side effects, and addressing misinformation related to vaccine adverse effects can reduce concerns over adverse effects of vaccines [62]. Furthermore, healthcare professionals must be at the forefront, listening to the public's concerns regarding vaccination programs and responding accordingly. In addition, monitoring of vaccine safety should occur out of the media spotlight to avoid reporting exaggerated information that can decrease vaccine acceptance [63].
Summary
To date, 12 different vaccines against COVID-19 have been approved for emergency use by many countries. As there is a lack of rigorous data from long-term trials on the safety of COVID-19 vaccines, there is an urgent need to strengthen postmarketing surveillance of adverse event data, particularly in low- and middle-income countries. This will require the continuous monitoring of vaccinated patients for possible adverse reactions to COVID-19 vaccines. Adoption of safety measures, systematic strategies, and timely assessment of any adverse incidents is crucial. Active pharmacovigilance monitoring involving all stakeholders of COVID-19 vaccination is needed to prevent and document possible adverse reactions related to COVID-19 vaccines.
References
Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–33.
Dhama K, Patel SK, Sharun K, et al. SARS-CoV-2 jumping the species barrier: zoonotic lessons from SARS, MERS and recent advances to combat this pandemic virus. Travel Med Infect Dis. 2020;37:101830.
Mousavizadeh L, Ghasemi S. Genotype and phenotype of COVID-19: their roles in pathogenesis. J Microbiol Immunol Infect. 2020;S1684–182(20):30082–7.
Malik YS, Kumar N, Sircar S, et al. Coronavirus disease pandemic (COVID-19): challenges and a global perspective. Pathogens. 2020;9(7):519.
Shadmi E, Chen Y, Dourado I, et al. Health equity and COVID-19: global perspectives. Int J Equity Health. 2020;19(1):1–16.
Paniz-Mondolfi AE, Sordillo EM, Marquez-Colmenarez MC, et al. The arrival of SARS-CoV-2 in venezuela. Lancet. 2020;395(10):e85–6.
Bonilla-Aldana DK, Villamil-Gómez WE, Rabaan AA, et al. Una nueva zoonosis viral de preocupación global: COVID-19, enfermedad por coronavirus 2019. Iatreia. 2020;33(2):107–10.
World Health Organization. WHO coronavirus disease (COVID-19) Dashboard. 2021. https://covid19.who.int/. Accessed 3 Jul 2021.
Choudhary OP, Priyanka Singh I, Rodriguez-Morales AJ. Second wave of COVID-19 in India: dissection of the causes and lessons learnt. Travel Med Infect Dis. 2021;43:102126.
Shahid Z, Kalayanamitra R, McClafferty B, et al. COVID-19 and older adults: what we know. J Am Geriatr Soc. 2020;68(5):926–9.
Rodriguez-Morales AJ, Cardona-Ospina JA, Gutierrez-Ocampo E, et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med Infect Dis. 2020;34:101623.
Patel SK, Singh R, Rana J, et al. The kidney and COVID-19 patients—important considerations. Travel Med Infect Dis. 2020;37:101831.
Wang J, Peng Y, Xu H, et al. The COVID-19 vaccine race: challenges and opportunities in vaccine formulation. AAPS PharmSciTech. 2020;21(6):225.
Patel SK, Pathak M, Tiwari R, et al. A vaccine is not too far for COVID-19. J Infect Dev Ctries. 2020;14(5):450–3.
Rabaan AA, Al-Ahmed SH, Sah R, et al. SARS-CoV-2/COVID-19 and advances in developing potential therapeutics and vaccines to counter this emerging pandemic. Ann Clin Microbiol Antimicrob. 2020;19(1):40.
McGill COVID19 Vaccine Tracker Team. 2021. Vaccines Candidates by Trial Phase. https://covid19.trackvaccines.org/vaccines/?fbclid=IwAR0rJdUx1T1j9TalYCJzwvnqm6MWluN2wwWtnuDP0GW6YvKLh3nW-Ex0ZKU. Accessed 27 June 2021.
Bloomberg News. China’s CanSino covid vaccine shows 65.7% efficacy. https://www.bloomberg.com/news/articles/2021-02-08/pakistan-says-cansino-s-covid-vaccine-shows-65-7-efficacy. Accessed 3 Jul 2021.
Voysey M, Clemens SAC, Madhi SA, et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. The Lancet. 2021;397(10269):99–111.
Reuters. UAE says Sinopharm vaccine has 86% efficacy against COVID-19. 2021. https://www.reuters.com/article/health-coronavirus-emirates-idUSKBN28J0G4. Accessed 27 Jun 2021.
Mahase E. Covid-19: Pfizer vaccine efficacy was 52% after first dose and 95% after second dose, paper shows. BMJ. 2020;371:m4826.
Al-Tawfiq JA, Gautret P. Asymptomatic middle east respiratory syndrome coronavirus (MERS-CoV) infection: extent and implications for infection control: a systematic review. Travel Med Infect Dis. 2019;27:27–32.
HindustanTimes. Covaxin efficacy 78% in phase 3 analysis. https://www.hindustantimes.com/india-news/covaxin-efficacy-78-in-phase-3-analysis-101622227104005.html. Accessed 3 Jul 2021.
World Health Organization. WHO lists additional COVID-19 vaccine for emergency use and issues interim policy recommendations. 2021. https://www.who.int/news/item/07-05-2021-who-lists-additional-covid-19-vaccine-for-emergency-use-and-issues-interim-policy-recommendations#:~:text=The%20Sinopharm%20product%20is%20an,2%20Vaccine%20(Vero%20C. Accessed 27 Jun 2021.
Baden LR, El Sahly HM, Essink B, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2020;384(5):403–16.
Sadoff J, Gray G, Vandebosch A, et al. Safety and efficacy of single-dose Ad26.COV2.S vaccine against Covid-19. N Engl J Med. 2021;384(23):2187–201.
Logunov DY, Dolzhikova IV, Shcheblyakov DV, et al. Safety and efficacy of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine: an interim analysis of a randomised controlled phase 3 trial in Russia. Lancet. 2021;397(10275):671–81.
World Health Organization. The effects of virus variants on COVID-19 vaccines. 2021. https://www.who.int/news-room/feature-stories/detail/the-effects-of-virus-variants-on-covid-19-vaccines. Accessed 3 Jul 2021.
Abu-Raddad LJ, Chemaitelly H, Butt AA. Effectiveness of the BNT162b2 Covid-19 vaccine against the B.1.1.7 and B.1.351 variants. N Engl J Med. 2021;385:187–9.
Bhopal S, Olabi B, Bhopal R. Vaccines for COVID-19: learning from ten phase II trials to inform clinical and public health vaccination programmes. Public Health. 2021;193:57–60.
Zhu F-C, Guan X-H, Li Y-H, et al. Immunogenicity and safety of a recombinant adenovirus type-5-vectored COVID-19 vaccine in healthy adults aged 18 years or older: a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet. 2020;396(10249):479–88.
Polack FP, Thomas SJ, Kitchin N, et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N Engl J Med. 2020;383(27):2603–15.
World Health Organization. mRNA vaccines against COVID-19: Pfizer-BioNTech COVID-19 vaccine BNT162b2 2021. https://apps.who.int/iris/bitstream/handle/10665/338096/WHO-2019-nCoV-vaccines-SAGE_evaluation-BNT162b2-2020.1-eng.pdf?sequence=1&isAllowed=y. Accessed 5 July 2021
AAP News. CDC confirms 226 cases of myocarditis after COVID-19 vaccination in people 30 and under. 2021. https://www.aappublications.org/news/2021/06/10/covid-vaccine-myocarditis-rates-061021. Accessed 19 Jun 2021.
Anderson EJ, Rouphael NG, Widge AT, et al. Safety and immunogenicity of SARS-CoV-2 mRNA-1273 vaccine in older adults. N Engl J Med. 2020;383(25):2427–38.
Food and Drug Adminstration. Vaccines and related biological products advisory committee meeting December 17, 2020. https://www.fda.gov/media/144434/download#:~:text=The%20most%20common%20solicited%20adverse,in%200.2%25%20to%209.7%25%20of. Accessed 6 Feb 2021.
Folegatti PM, Ewer KJ, Aley PK, et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2: a preliminary report of a phase 1/2, single-blind, randomised controlled trial. Lancet. 2020;396(10249):467–78.
Sah R, Shrestha S, Mehta R, et al. AZD1222 (Covishield) vaccination for COVID-19: experiences, challenges, and solutions in Nepal. Travel Med Infect Dis. 2021;40:101989.
Logunov DY, Dolzhikova IV, Zubkova OV, et al. Safety and immunogenicity of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine in two formulations: two open, non-randomised phase 1/2 studies from Russia. Lancet. 2020;396(10255):887–97.
Ella R, Vadrevu KM, Jogdand H, et al. Safety and immunogenicity of an inactivated SARS-CoV-2 vaccine, BBV152: a double-blind, randomised, phase 1 trial. Lancet Infect Dis. 2021;21(5):637–46.
Xia S, Zhang Y, Wang Y, et al. Safety and immunogenicity of an inactivated SARS-CoV-2 vaccine, BBIBP-CorV: a randomised, double-blind, placebo-controlled, phase 1/2 trial. Lancet Infect Dis. 2021;21(1):39–51.
Zhang Y, Zeng G, Pan H, et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine in healthy adults aged 18–59 years: a randomised, double-blind, placebo-controlled, phase 1/2 clinical trial. Lancet Infect Dis. 2021;21(2):181–92.
Kaur RJ, Dutta S, Bhardwaj P, et al. Adverse events reported from COVID-19 vaccine trials: a systematic review. Indian J Clin Biochem. 2021:1–13.
Voysey M, Clemens SAC, Madhi SA, et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet. 2021;397(10269):99–111.
Centers for Disease Control and Prevention. COVID-19 vaccine breakthrough case investigation and reporting 2021. https://www.cdc.gov/vaccines/covid-19/health-departments/breakthrough-cases.html. Accessed 8 Jul 2021.
KHOU 11. A closer look at reported COVID-19 vaccine side effects. 2021. https://www.khou.com/article/news/health/coronavirus/vaccine/reported-covid-19-vaccine-side-effects/285-dcf5ca1e-9b87-4cca-bcb2-f8f943933518. Accessed 6 Feb 2021.
Centers for Disease Control and Prevention. Allergic reactions including anaphylaxis after receipt of the first dose of Pfizer-BioNTech COVID-19 vaccine—United States, December 14–23, 2020.https://www.cdc.gov/mmwr/volumes/70/wr/mm7002e1.htm. Accessed 6 Feb 2021.
Centers for Disease Control and Prevention. Allergic reactions including anaphylaxis after receipt of the first dose of moderna COVID-19 vaccine—United States, December 21, 2020–January 10, 2021. https://www.cdc.gov/mmwr/volumes/70/wr/mm7004e1.htm. Accessed 8 Jul 2021.
WebMD. FDA: Track Vaccine Recipients for Facial Paralysis. 2021. https://www.webmd.com/vaccines/covid-19-vaccine/news/20201217/fda-says-vaccine-recipients-should-be-monitored-for-facial-paralysis?fbclid=IwAR2Xg2YVJVZ5GubOuowvVhiLlkypOiRvaWO2_5oYXR5ESZmo23ezjWqTHfg. Accessed 3 July 2021.
Bastola A, Sah R, Nepal G, et al. Bell’s palsy as a possible neurological complication of COVID-19: a case report. Clin Case Rep. 2021;9(2):747–50.
Eesti Rahvusringhääling. 71 COVID-19 vaccine side effects cases reported over last week. 2021. https://news.err.ee/1608086491/71-covid-19-vaccine-side-effects-cases-reported-over-last-week. Accessed 1 Feb 2021.
Tobaiqy M, Elkout H, MacLure K. Analysis of thrombotic adverse reactions of COVID-19 AstraZeneca vaccine reported to eudravigilance database. Vaccines. 2021;9(4):393.
Janssen. Clinical Data for the Janssen COVID-19 vaccine. 2021. https://www.janssencovid19vaccine.com/hcp/clinical-data.html. Accessed 3 Jul 2021.
Centers for Disease Control and Prevention. Myocarditis and pericarditis following mRNA COVID-19 vaccination. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/safety/myocarditis.html. Accessed 2 Jul 2021.
United States Food and Drug Adminstration. Pfizer-BioNTech COVID-19 vaccine. 2021. https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/pfizer-biontech-covid-19-vaccine. Accessed 3 Jul 2021.
Collet J-P, MacDonald N, Cashman N, et al. Monitoring signals for vaccine safety: the assessment of individual adverse event reports by an expert advisory committee. Bull World Health Organ. 2000;78:178–85.
World Health Organization. Covid-19 vaccines: safety surveillance manual. 2020. https://apps.who.int/iris/handle/10665/338400. Accessed 3 Jul 2021.
Soldatos TG, Taglang G, Jackson DB. In silico profiling of clinical phenotypes for human targets using adverse event data. High-Throughput. 2018;7(4):37.
Paudyal V, Al-Hamid A, Bowen M, et al. Interventions to improve spontaneous adverse drug reaction reporting by healthcare professionals and patients: systematic review and meta-analysis. Expert Opin Drug Saf. 2020;19(9):1173–91.
Shrestha S, Danekhu K, KC B, et al. Bibliometric analysis of adverse drug reactions and pharmacovigilance research activities in Nepal. Ther Adv Drug Saf. 2020;11:2042098620922480.
Ullah I, Khan KS, Tahir MJ, et al. Myths and conspiracy theories on vaccines and COVID-19: potential effect on global vaccine refusals. Vacunas. 2021;22(2):93–7.
Biswas N, Mustapha T, Khubchandani J, et al. The nature and extent of COVID-19 vaccination hesitancy in healthcare workers. J Community Health. 2021:1–8.
Rief W. Fear of adverse effects and COVID-19 vaccine hesitancy: recommendations of the treatment expectation expert group. JAMA Health Forum. 2021;2(4):210804.
Motta M, Sylvester S, Callaghan T, et al. Encouraging COVID-19 vaccine uptake through effective health communication. Front Polit Sci. 2021;3:1.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This research did not receive any funding from any agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
Sunil Shrestha (SSa), Januka Khatri (JK), Sujyoti Shakya (SSb), Krisha Danekhu (KD), Asmita Priyadarshini Khatiwada (APK), Ranjit Sah (RS), Bhuvan KC (BKC), Vibhu Paudyal (VP), Saval Khanal (SK), and Alfonso J. Rodriguez-Morales (AJM) have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Author contributions
SSa and JK conceptualized the idea of this manuscript, conducted the literature review and wrote the initial draft of the manuscript. SSb, KD and APK made substantial changes to the conception, conducted the literature review, and contributed to the critical review of the manuscript. BKC, VP, RS, AJRM and SK provided intellectual feedback to the concept of the study, conducted the literature review, and contributed to the critical review of the manuscript.
Rights and permissions
About this article
Cite this article
Shrestha, S., Khatri, J., Shakya, S. et al. Adverse events related to COVID-19 vaccines: the need to strengthen pharmacovigilance monitoring systems. Drugs Ther Perspect 37, 376–382 (2021). https://doi.org/10.1007/s40267-021-00852-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40267-021-00852-z