Abstract
Background and objective
β-Lactam antibiotics are the recommended first-line treatment for acute bacterial sinusitis. Fluoroquinolones are recommended in patients with hypersensitivity reactions to penicillins, and macrolide antibiotics are no longer recommended. The objectives of this study were to understand whether outpatient antibiotic prescribing practices adhere to treatment guidelines and to describe rates of fluoroquinolone and macrolide antibiotic prescribing for the treatment of sinusitis.
Methods
This was a retrospective cross-sectional study using US National Ambulatory Medical Care Survey (NAMCS) data. The prevalence of antibiotic prescribing for sinusitis was estimated, and the antibiotic prescribing pattern was measured. Additionally, significant factors associated with various antibiotic prescribing during the visits related to sinusitis were identified.
Results
Among physician visits related to sinusitis from 2013 to 2016 (n = 2739), 66.4% involved antibiotic prescribing. Visits with antibiotic prescribing showed greater proportions of patients aged < 18 years (21.7 vs 11.1%, p < 0.001), patients reporting fever (79.8 vs 50.7%, p < 0.001), and patients seeing family physicians or internal medicine specialists (68.4 vs 44.8%, p < 0.001) than those without antibiotic prescribing. Penicillins, macrolides, cephalosporins, and fluoroquinolones were prescribed in 42.2%, 30.6%, 15.2%, and 9.5% of the visits involving antibiotic prescribing for sinusitis, respectively. The odds of fluoroquinolone/macrolide prescribing were reduced by 73% if patients visited pediatricians and by 59% with otolaryngologists.
Conclusions
Macrolides were the most common inappropriate antibiotic class prescribed for sinusitis. This study identifies a need for more focused attention to improve prescribing for sinusitis and adherence to the treatment guidelines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The need for enhanced antimicrobial stewardship efforts nationwide was highlighted in the 2013 Centers for Disease Control and Prevention (CDC) report Antibiotic Resistance Threats in the United States, which explained the negative impacts that antimicrobial resistance has on human health, including an estimated 23,000 deaths annually due to antibiotic-resistant infections [1]. The CDC later published the Core Elements of Hospital Antibiotic Stewardship Programs, and the Joint Commission implemented a requirement for stewardship programs in all hospitals and nursing care centers [2, 3]. While antimicrobial stewardship efforts have now become well-established in the acute care setting, more focused attention is being placed on the ambulatory care setting, which is where ≈ 47 million unnecessary antibiotics are prescribed annually [4]. Although the CDC published Core Elements of Outpatient Antibiotic Stewardship in 2016 [5], further studies are needed to examine antibiotic prescribing practices in the ambulatory care setting.
Fleming-Dutra et al. [6] attempted to quantify the rate of inappropriate oral antibiotic prescriptions written at hospital outpatient and office-based visits in the USA. Using data from 2010 to 2011, this study concluded that ≈ 506 antibiotic prescriptions per 1000 population were written annually, of which only 353 were appropriate. In other words, ≈ 30% of all outpatient antibiotic prescriptions were considered inappropriate. Sinusitis was the diagnosis associated with the highest number of prescriptions, at 56 per 1000 population in this study. Approximately 59 per 1000 patients aged 0–19 years, 27 per 1000 patients aged 20–64 years, and 37 per 1000 patients aged ≥ 65 years were deemed to receive antibiotics appropriately [6].
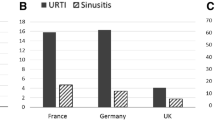
Sharma et al. [7] examined the use of antibiotics for management of acute sinusitis in Canada. More than 13 million cases of acute sinusitis were diagnosed in this study. From 2007 to 2013, antibiotic prescribing decreased from 517 to 388 per 10,000 patient population because of a decrease in diagnosis rates. However, the percentage of patients with a diagnosis of acute sinusitis who received an antibiotic decreased by only 3.7% during this 5-year period. Interestingly, the most prescribed antibiotics changed from macrolide antibiotics to extended-spectrum penicillins in patients aged > 10 years, likely due to updated national treatment guideline recommendations [7].
Current guidelines recommend a β-lactam antibiotic, amoxicillin ± clavulanate (a β-lactamase inhibitor), as first-line therapy for acute bacterial sinusitis in patients without allergies to this antibiotic class [8,9,10]. Fluoroquinolone antibiotics are only recommended initially in patients with type 1 hypersensitivity reactions to penicillins. Macrolide antibiotics are no longer recommended for treatment of acute sinusitis because of increased resistance (≈ 30%) to Streptococcus pneumoniae [8,9,10,11]. Inappropriate overuse of broad-spectrum antibiotics may further increase the societal burden of antibiotic-resistant infections, so adherence to current treatment guidelines is of utmost importance. The purpose of this study is to understand whether current outpatient antibiotic prescribing practices adhere to treatment guidelines and, more specifically, to describe the rates of inappropriate fluoroquinolone and macrolide antibiotic prescriptions for acute sinusitis and identify factors associated with antibiotic prescribing during sinusitis-related visits.
Methods
Data source
This retrospective cross-sectional study used the most recent National Ambulatory Medical Care Survey (NAMCS) data files (2013–2016) in the USA. NAMCS is one component of the National Health Care Surveys conducted and administered by US National Center for Health Statistics, CDC. This survey provides a stratified multistage probability sample to measure office-based physician visits at the US population level. Physicians reported all daily patient visits during the randomly assigned reporting week. Since 2012, NAMCS has collected data electronically for all sampled visits, including patient demographics, clinical characteristics, such as reason for the visit, diagnoses and procedures received, chronic comorbidities, treatments, and medication prescribed, as well as practice site information, such as physician specialty and geographic region. A patient weight is assigned by NAMCS to each visit in the sample data to help obtain the national estimates of the visits from the survey. The weighted response rates were 40.4% (2013), 39.0% (2014), 29.6% (2015), and 32.7% (2016), respectively.
This study was approved by the Institutional Review Board of Presbyterian College.
Study sample
All office-based physician visits for sinusitis during 2013–2016 were identified using International Statistical Classification of Diseases and Related Health Problems, Ninth Edition (ICD-9) codes (461: acute sinusitis and 473: chronic sinusitis), Tenth Edition (ICD-10) codes (J01), or reason for visit (i.e., sinusitis problems). The visits with an additional diagnosis of a disease almost always or maybe indicating antibiotic use were excluded from the study sample, including pneumonia, urinary tract infection, acne, gastrointestinal infection, pharyngitis, skin, cutaneous and mucosal infections, suppurative otitis media, and other bacterial infections [5]. Antibiotics prescribed during the eligible visits were identified using therapeutic classes defined by the Multum Lexicon Plus system, including fluoroquinolone, macrolide, penicillin, and cephalosporin. Antibiotics not included in these pharmacologic classes were categorized as “other”. The study sample visits were divided into antibiotic and no antibiotic groups. Subgroup analyses were conducted to further explore the antibiotic prescribing patterns. First, we divided all visits with penicillins, cephalosporins, fluoroquinolones, or macrolides into two groups (fluoroquinolones/macrolides vs penicillins/cephalosporins) to estimate potential inappropriate antibiotic prescribing for sinusitis. These distinctions were made because penicillins and cephalosporins are preferred as first-line and alternative antibiotics based on the current treatment guidelines. Fluoroquinolone antibiotics should rarely be used (i.e., in certain cases of type 1 hypersensitivity reactions to penicillins and/or cephalosporins or in cases of treatment failure), and macrolides are not recommended for the treatment of acute sinusitis [8,9,10]. Next, the visits were further divided into three groups for additional analysis: penicillins/cephalosporins, fluoroquinolones, and macrolides.
Outcome measures
The survey data were combined to measure the study outcomes. The outcomes for this study were (1) the prevalence of antibiotics prescribed during sinusitis-related visits, (2) prescribing patterns measured by distribution of antibiotics classified by therapeutic class and prescribed during sinusitis-related visits, (3) potential inappropriate antibiotic prescribing (i.e., fluoroquinolones/macrolides vs penicillins/cephalosporins) for sinusitis.
Potential variables associated with antibiotic prescribing
Patient demographics, including age, race, sex, and primary payer, were collected for each visit. Collected patient clinical characteristics included comorbid asthma and chronic obstructive pulmonary disease (COPD), total number of chronic conditions, and whether fever was reported. NAMCS measured 17 of 20 chronic conditions defined by the Office of the Assistant Secretary for Health, US Department of Health and Human Services [12]. Physician specialty, location, and geographic region were also collected. Physician specialty was separated into four categories: family practice and internal medicine, pediatrics, otolaryngology, and other specialties. Physician location was defined as metropolitan or non-metropolitan. The geographic region represents the location where most visit records were sampled, including northeast, midwest, south, and west.
Data analysis
Chi squared tests were used to compare the characteristics of the office visits between antibiotic and non-antibiotic groups and between penicillin/cephalosporin and fluoroquinolone/macrolide groups. Multivariate logistic regression was performed to identify significant factors associated with antibiotic prescribing (vs no antibiotics) during sinusitis-related visits and factors associated with potential inappropriate antibiotic prescribing (i.e., fluoroquinolones/macrolides vs penicillins/cephalosporins) during sinusitis-related visits. Multinomial logistic regression was used to identify factors associated with fluoroquinolone prescribing (vs penicillins/cephalosporins) or macrolide prescribing (vs penicillins/cephalosporins) during sinusitis-related visits. Statistical significance was set at p < 0.05. NAMCS assigned an inflation factor called patient weight to each visit in the sample data. By aggregating the patient weights in the analysis, the national estimates of the visits made in the USA can be obtained from the survey data. Given the complex survey design, the patient weights were applied to all analyses as recommended by NAMCS. All analyses were performed using SAS 9.4 (2013).
Results
Figure 1 shows that 66.4% (n = 1631) of all eligible sinusitis-related physician office visits from 2013 to 2016 (n = 2739, representing 17.9 million visits in the USA) involved antibiotic prescribing, representing more than 11.9 million visits in the USA during the 3-year period. Table 1 shows the characteristics of sinusitis-related visits with antibiotic prescribing versus no antibiotic prescribing. Visits with antibiotic prescribing had more patients aged < 18 years (21.7 vs 11.1%, p < 0.001), reporting fever (79.8 vs 50.7%, p < 0.001), and visiting family physicians or internal medicine specialists (68.4 vs 44.8%, p < 0.001) than visits without antibiotic prescribing. Table 1 also displays the significant factors associated with antibiotic prescribing during sinusitis-related visits. Patients aged ≥ 65 years and those aged 45–64 years were 45% [odds ratio (OR) 0.55; 95% confidence interval (CI) 0.31–0.98] and 41% (OR 0.59; 95% CI 0.37–0.94) less likely to be prescribed antibiotics during sinusitis-related visits than those aged < 18 years. In general, African American patients were 53% less likely to be prescribed an antibiotic than white patients (OR 0.47; 95% CI 0.25–0.88). If fever was reported during the sinusitis-related visits, the odds of antibiotic prescribing increased by 109% (OR 2.09; 95% CI 1.52–2.89). Otolaryngology specialists were 72% less likely than family physicians and internal medicine specialists to prescribe antibiotics (OR 0.28; 95% CI 0.19–0.42).
Table 2 presents the characteristics of sinusitis-related visits with penicillin/cephalosporin versus fluoroquinolone/macrolide prescribing. The distributions of age, race, comorbid COPD, number of chronic conditions, and physician specialty differed significantly between the two groups. Overall, visits with fluoroquinolone/macrolide prescribing showed higher proportions of patients aged 18–64 years (71.8 vs 58.3%, p < 0.001), African Americans (10.9 vs 4.3%, p = 0.009), patients reporting comorbid COPD (11.6 vs 3.7%, p = 0.002) or more than one chronic condition (37.7 vs 23.3%, p = 0.002), and those seeing family or internal medicine physicians (79.4 vs 60.8%, p < 0.001) than those with penicillin/cephalosporin prescribing. Table 2 also shows the factors associated with potential inappropriate antibiotic prescribing (fluoroquinolone/macrolide vs penicillin/cephalosporin prescribing). The odds of fluoroquinolone/macrolide prescribing reduced by 73% (OR 0.27; 95% CI 0.11–0.69) if patients visited pediatricians and by 59% (OR 0.4; 95% CI 0.22–0.75) if patients visited otolaryngologists compared with visiting family or internal medicine physicians.
Penicillins and macrolides were prescribed during 42.2% and 30.6%, respectively, of sinusitis-related visits involving antibiotic prescribing (n = 1631; Table 3). Cephalosporin and fluoroquinolone prescribing accounted for 15.2% and 9.5% of the visits, respectively, and visits in which more than one antibiotic was prescribed accounted for 7.5% of the total sinusitis-related visits.
Characteristics of sinusitis-related visits with penicillin/cephalosporin, fluoroquinolone, or macrolide prescribing are shown in Table S1 in the Electronic Supplementary Material (ESM). Table 4 shows the factors associated with fluoroquinolone (vs penicillin/cephalosporin) and macrolide (vs penicillin/cephalosporin) prescribing. Older patients were more likely to be prescribed fluoroquinolones (vs penicillins/cephalosporins). Pediatricians and otolaryngologists were 74% less likely than family/internal medicine physicians to prescribe macrolides (vs penicillins/cephalosporins).
Discussion
This study sample of eligible visits represents ≈ 17.9 million ambulatory care visits addressing sinusitis in the USA (2013–2016). Overall, 66.4% of these visits resulted in at least one antibiotic being prescribed. Previous data suggest that ≈ 2% of sinusitis cases are caused by bacterial pathogens, so many of these antibiotics may have been inappropriately prescribed [13]. Penicillin antibiotics were the most commonly prescribed antibiotics, demonstrating adherence to current guidelines for treatment of sinusitis in ≈ 40% of office visits in which antibiotics were prescribed [8,9,10]. However, potentially inappropriate prescribing of fluoroquinolones and, more commonly, macrolides was present in ≈ 40% of office visits involving antibiotic prescribing. Macrolide antibiotics are no longer recommended to treat sinusitis, and fluoroquinolones are only recommended initially in patients with type 1 hypersensitivity reactions to penicillins [8,9,10]. Studies have shown that ≈ 10–15% of patients self-report a penicillin allergy [14,15,16,17]. Based on the results of this study, fluoroquinolones were prescribed in 9.5% of outpatient visits, which could theoretically account for patients who reported a penicillin allergy. Even if every patient who received a fluoroquinolone in this study had a reported penicillin allergy, evidence suggests that only 1–10% of those who report an allergy have a type 1 hypersensitivity reaction to penicillins [14,15,16,17]. More detailed and comprehensive allergy reconciliation measures are needed in the outpatient setting to ensure that optimal antibiotics are being prescribed for patients with sinusitis. Based on the outcomes of this study, macrolides and fluoroquinolones were likely overused and inappropriately prescribed in the majority of cases.
Differences in age distributions between penicillin/cephalosporin and fluoroquinolone/macrolide prescribing were observed in the study. During visits involving patients aged < 18 years, the rate of penicillin/cephalosporin prescribing was nearly 20% higher than that of fluoroquinolone/macrolide prescribing. However, during visits involving patients aged 18–64 years, the rate of penicillin/cephalosporin prescribing was 13% lower than that of fluoroquinolone/macrolide prescribing.
Several factors may contribute to the differences in prescribing of antibiotics for treatment of sinusitis. Adverse effects associated with fluoroquinolones in younger patients likely account for the minimal use identified in this study. The use of broad-spectrum antibiotics in elderly patients (aged ≥ 65 years) may be due to the higher risk of morbidity and mortality with certain infections [18]. In addition, older patients may have more comorbid conditions than younger patients, which may lead to prescribing of broad-spectrum antibiotics, as identified in our results.
More patients aged 45–64 years received prescriptions for fluoroquinolones than other antibiotic classes in this study. Interestingly, communication from the US FDA [19] indicated that patients aged 30–59 years experienced more serious adverse effects when taking oral fluoroquinolones for either acute bacterial sinusitis, acute bacterial exacerbation of chronic bronchitis, or uncomplicated urinary tract infections. This led to the FDA advising in 2016 that fluoroquinolones should be reserved for patients with no alternative options for the treatment of acute sinusitis. The fluoroquinolone prescribing patterns in this age group may have decreased after the FDA warning was released, but this would not be reflected in this study. Recently, the results of post-marketing surveillance led the FDA to require updates to fluoroquinolone labeling to strengthen warnings about the risk of hypoglycemia and mental health adverse effects [20]. The review of data from October 1987 through April 2017 found 13 deaths due to hypoglycemic coma, some of which occurred in patients taking fluoroquinolones for uncomplicated infections, including upper respiratory infections. Again, the changes in fluoroquinolone prescribing after 2016 would not be reflected in this study.
A higher proportion of adults aged 18–44 years were prescribed a macrolide relative to other antibiotics and age groups. The ease of administration and prescribing of macrolides, commonly azithromycin, in daily-dose packs may increase the utilization of these antibiotics in this group. However, macrolides are no longer recommended for treatment of sinusitis because of increased resistance patterns [8,9,10,11]. This finding highlights a potential area of focus for antimicrobial stewardship efforts in the outpatient setting to reduce the use of this inappropriate antibiotic class for treatment of sinusitis.
Physician specialty was also associated with differences in antibiotic prescribing. Specialists, including otolaryngologists, were less likely to prescribe an antibiotic for sinusitis, and pediatricians were more likely to prescribe penicillin or cephalosporin antibiotics. Family or internal medicine physicians were more likely not only to prescribe antibiotics in general for sinusitis-related visits but also to prescribe potentially inappropriate antibiotics, including both fluoroquinolones and macrolides. These prescribing patterns identify a need to focus stewardship efforts regarding the treatment of sinusitis on family and internal medicine practices. Interventions such as academic detailing may help improve these patterns.
The strengths of this study include the representation of the US physician office visits and the amount of data available in the database. However, several limitations exist. Information necessary to fully determine the appropriateness of antibiotic prescribing may not be available because of the data collected and the aggregate form, as the NAMCS only reflects a snapshot of antibiotic prescribing patterns. For instance, patients for whom treatment with preferred antibiotic therapy failed may have presented again and appropriately received a fluoroquinolone. However, it is not possible to identify this because the visits are neither linked to nor matched by individual patients. In addition, no data on allergies were available for evaluation. Some patients included in the data set may have a true penicillin allergy and, in such cases, a fluoroquinolone may be an appropriate treatment option. Additionally, the estimates of some variables in subgroup analysis might not be reliable because of the small number of visits (< 30).
The most recent data available in the NAMCS database is through 2016. More attention nationally has been paid to antibiotic stewardship, as rates of antibiotic-resistant organisms increase and more data become available about the adverse effects of antimicrobials [1,2,3,4]. Therefore, there may be a more recent trend towards decreased prescribing of inappropriate antibiotics that has not been identified in this study. Antibiotic choice is only one portion of determining the appropriateness of antibiotic use. Other areas include the dose and duration of antibiotics, neither of which this study captured, so no comment can be made on their appropriateness.
Conclusion
In the USA, 66.4% of sinusitis-related visits involved antibiotic prescribing; less than half of these included a prescription of a β-lactam antibiotic for the treatment of sinusitis. Although attention to antibiotic stewardship and the proper prescribing of antibiotics for the treatment of infectious diseases is increasing, this study identifies that more focused attention is needed for the appropriate treatment of sinusitis.
References
Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States. 2013. http://www.cdc.gov/drugresistance/threat-report-2013/. Accessed 19 Nov 2017.
Centers for Disease Control and Prevention. Core elements of hospital antibiotic stewardship programs. https://www.cdc.gov/antibiotic-use/healthcare/ implementation/core-elements.html. Accessed 19 Nov 2017.
The Joint Commission. Antimicrobial stewardship. https://www.jointcommission.org/antimicrobial_stewardship_faqs/. Accessed 19 Nov 2017.
Centers for Disease Control and Prevention. Antibiotic use in the United States, 2017: Progress and opportunities. US Department of Health and Human Services, CDC. 2017. https://www.cdc.gov/antibiotic-use/stewardship-report/pdf/stewardship-report.pdf. Accessed 19 Nov 2017.
Sanchez GV, Fleming-Dutra KE, Roberts RM, et al. Core elements of outpatient antibiotic stewardship. MMWR Recomm Rep. 2016;65(6):1–12.
Fleming-Dutra KE, Hersh AL, Shapiro DJ, et al. Prevalence of inappropriate antibiotic prescriptions among US ambulatory care visits, 2010–2011. JAMA. 2016;315(17):1864–73.
Sharma P, Finley R, Weese S, et al. Antibiotic prescriptions for outpatient acute rhinosinusitis in Canada, 2007–2013. PLoS One. 2017;12(7):e0181957. https://doi.org/10.1371/journal.pone.0181957.
Wald E, Applegate K, Bordley C, et al. Clinical practice guideline for the diagnosis and management of acute bacterial sinusitis in children aged 1 to 18 years. Pediatrics. 2013;132(1):e262–80.
Chow AW, Benninger MS, Brook I, et al. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012;54(8):e72–112.
Rosenfeld R, Piccirillo J, Chandrasekhar S, et al. Clinical practice guideline (update): adult sinusitis. Otolaryngol Head Neck Surg. 2015;152(2 Suppl):S1–39.
Harrison CJ, Woods C, Stout G, et al. Susceptibilities of Haemophilus influenzae, Streptococcus pneumoniae, including serotype 19A, and Moraxella catarrhalis paediatric isolates from 2005 to 2007 to commonly used antibiotics. J Antimicrob Chemother. 2009;63(3):511–9.
Goodman RA, Posner SF, Huang ES, et al. Defining and measuring chronic conditions: imperatives for research, policy, program, and practice. Prev Chronic Dis. 2013;10:E66. https://doi.org/10.5888/pcd10.120239.
Meltzer EO, Hamilos DL. Rhinosinusitis diagnosis and management for the clinician: a synopsis of recent consensus guidelines. Mayo Clin Proc. 2011;86(5):427–43.
Zhou L, Dhopeshwarkar N, Blumenthal KG, et al. Drug allergies documented in electronic health records of a large healthcare system. Allergy. 2016;71(9):1305–13.
Lee CE, Zembower TR, Fotis MA, et al. The incidence of antimicrobial allergies in hospitalized patients: implications regarding prescribing patterns and emerging bacterial resistance. Arch Intern Med. 2000;160(18):2819–22.
Macy E, Ngor EW. Safely diagnosing clinically significant penicillin allergy using only penicilloyl-poly-lysine, penicillin, and oral amoxicillin. J Allergy Clin Immunol Pract. 2013;1(3):258–63.
Sagar PS, Katelaris CH. Utility of penicillin allergy testing in patients presenting with a history of penicillin allergy. Asia Pac Allergy. 2013;3(2):115–9.
Beckett CL, Harbarth S, Huttner B. Special considerations of antibiotic prescription in the geriatric population. Clin Microbiol Infect. 2015;21(1):3–9.
U.S. Food & Drug Administration. FDA drug safety communication: FDA updates warnings for oral and injectable fluoroquinolone antibiotics due to disabling side effects. https://www.fda.gov/Drugs/DrugSafety/ucm511530.htm. Accessed 19 Nov 2017.
U.S. Food & Drug Administration. FDA drug safety communication: FDA reinforces safety information about serious low blood sugar levels and mental health side effects with fluoroquinolone antibiotics; requires label changes. https://www.fda.gov/Drugs/DrugSafety/ucm611032.htm/ Accessed 30 July 2018.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No source of funding was used for this study.
Conflicts of Interest
The authors have no conflicts of interest that are directly relevant to the content of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Giles, A.B., Wu, J. & Shealy, K.M. The use of fluoroquinolones and macrolides for sinusitis: a retrospective cross-sectional study. Drugs Ther Perspect 35, 518–526 (2019). https://doi.org/10.1007/s40267-019-00652-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40267-019-00652-6