Abstract
This review discusses the available evidence in the current evaluation and treatment of nocturia in frail older adults. No evidence specifically evaluates the use of behavioral interventions in the treatment of the frail older adult with nocturia, but their use is supported in other cohorts. Behavioral modifications and optimal management of comorbidities remain the first-line treatment for all age groups and should be emphasized in the frail due to their favorable safety profile. No studies specific to the frail older adult support the use of pharmacotherapy. Some evidence exists for the efficacy of several agents in the older adult; however, this is difficult to extrapolate to the frail, and safety concerns abound. Desmopressin may be effective in the older adult, but a high risk of hyponatremia raises concerns for its safety, and therefore it is not recommended in the frail. α-Antagonists may have limited efficacy in men with known benign prostatic hyperplasia (BPH); they are relatively well tolerated, although the risk of orthostatic hypotension in the frail should be considered. β3-agonist trials suggest limited clinical utility. Antimuscarinics are not found to be useful in this cohort and are contraindicated in the frail older adult given the ability of antimuscarinics to cause cognitive impairment, delirium, and falls. No data examine the use of nonsteroidal anti-inflammatory drugs (NSAIDs) in the frail older adult. Additionally, the American Geriatrics Society Beers Criteria recommends against the use of muscarinics in those over the age of 75 years and therefore their use is not supported.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Behavioral modification and optimization of comorbidities are first-line treatment for nocturia in the frail older adult. |
Sparse evidence for pharmacotherapy directly addresses this cohort. |
Desmopressin is relatively contraindicated due to safety concerns. |
α-Blockers may have limited utility in men with benign prostatic hyperplasia. |
Antimuscarinics, β3 agonists, and nonsteroidal anti-inflammatory drugs do not have evidence supporting their use. |
1 Introduction
1.1 Epidemiology and Pathophysiology
Nocturia, the act of awakening from sleep to void urine, is a common and complex urological complaint. Although just one component of the broader category of lower urinary tract symptoms (LUTS), its multifactorial etiology and variable responsiveness to existing therapies makes nocturia a complicated symptom to understand and treat. Nocturia is defined by the International Continence Society (ICS) as awakening to void one or more times per night [1]; however it has been found that only two or more voids per night are associated with impaired health-related quality of life (HRQoL) [2]. Because we felt it to be more clinically relevant, this latter definition will be used throughout this review [3].
Patients typically seek treatment when the burden of nocturia begins to significantly impact their quality of life (QoL), and is infrequently brought to the attention of physicians prior to this impact as it is commonly believed to be a natural part of aging [4]. Waking from sleep numerous times per night increases the difficulty of returning to restful sleep, and diminishing sleep quality negatively impacts both physical and mental health [5,6,7,8,9]. Nocturia is associated with an increased risk for falls, fractures, and depression [10,11,12,13], and nocturia has been found to be an independent risk factor for mortality [7, 11, 14,15,16,17]. These associations should prompt an evaluation for nocturia in all frail older adults. Studies examining methods of decreasing nocturia have demonstrated an improvement in patient QoL with decreased nighttime voiding [7]. More work is still needed to evaluate the impact that existing treatments may have on patient mortality.
It is axiomatic that the prevalence of nocturia increases with age, and that age itself is a risk factor for developing nocturia. A 2019 study using National Health and Nutrition Exam Survey (NHANES) data found that 51.5% of men and 45% of women 60 years of age or older woke at least two times per night to void [18]. Numerous insults to the aging body contribute to the pathophysiology of nocturia in the older adult. One hypothesis is that the aging bladder loses smooth muscle cell content and accumulates depositions of collagen and fibrosis [19,20,21]; these changes contribute to detrusor instability and decreased bladder capacity [21,22,23]. It is also hypothesized that age-related changes to the central nervous system, increased sensitivity to neurotransmitters, and increased density of acetylcholinergic receptors may all contribute to bladder hypersensitivity or the sensation of urgency [21, 24].
Aging patients also experience atherosclerosis and peripheral vascular disease, which can cause reductions in renal blood flow and decreased glomerular filtration rate (GFR) [25]. Vascular disease risk factors may also contribute to generalized pelvic ischemia, which is strongly correlated with LUTS and nocturia [26, 27]. In addition to reduced renal function, nocturnal urine output is increased in the older adult. Arginine vasopressin (AVP) is an antidiuretic hormone that follows a circadian rhythm of release, with higher serum levels detected during the early hours of sleep. AVP functions to increase urine osmolality and decrease urine volume during the sleep cycle hours. This combination prevents the sleeper from reaching maximum bladder capacity, thereby minimizing the likelihood of awakening during the sleep cycle. There is a hypothesized reduction in the amplitude of this circadian rhythm that is associated with aging, leading to a decreased ability to concentrate urine during sleep [28]. Younger patients are known to have less nocturnal urine production: adults 21–35 years of age excrete approximately 14% of their total urine volume in 8 h of sleep, while adults > 65 years of age excrete approximately 34% [29, 30]. Thus, the combination of dysregulation of AVP and diminished renal concentrating ability results in a global increase in urine production that is exacerbated during sleeping hours. Consequently, nocturnal polyuria (NP) is a primary causative factor of nocturia in the older adult [7, 31]. Additionally, diseases that are more common in older adults, such as obstructive sleep apnea (OSA), benign prostatic hyperplasia (BPH), hypertension, renal failure, poorly controlled diabetes mellitus, and congestive heart disease, may put these adults at risk for overactive bladder (OAB) symptoms as well as NP [7, 32]. Multiple pathologies that coincide with nocturia, such as OSA, may also exacerbate the dysregulation of serum AVP levels [33].
Special attention must be paid when treating nocturia in older adults. The definition of ‘older adult’, commonly referred to as ‘elderly’, is nebulous and is inconsistently used across guidelines. There is no clear age cut-off, and the definition may reflect health status, independence, and culture. For the purpose of this review, ‘older adult’ refers to those over 65 years of age, as is common for research purposes, and we refer to studies as specifically addressing older adults if they recruit participants > 65 years of age [34]. With this in mind, we recognize that this definition is arbitrary. Many studies will have mean ages just above or below 65 years, and their clinical relevance is likely similar in this range. ‘The 60s’ is a young age range for older adults. Advancing age is a known risk factor for adverse drug-related events, however the pharmacodynamic and pharmacokinetic changes related to the decades beyond the 60s are poorly understood [35]. Limitations in our knowledge should be kept in mind when prescribing medications.
While clinicians are often aware of a patient’s chronological age, they may be less attuned to frailty as an important factor in the efficacy, tolerability, and safety of nocturia treatment. Frailty is best defined as a state of reduced physiologic functioning across multiple domains that is associated with an increased vulnerability to a wide range of stressors [36,37,38]. There are two primary approaches to characterizing frailty. The frailty phenotype, reported by Fried et al., lists criteria such as weakness, slow gait speed, low physical activity, exhaustion, and unintentional weight loss; those who fulfill at least three of these criteria are classified as ‘frail’ [39]. The Canadian Index model is based on accumulated deficits, wherein the number of counted deficits indicates the likelihood of existing frailty [40]. It is important to note that frailty is not part of the normal aging process and carries an increased risk of morbidity and mortality [36].
The relationship between nocturia and frailty is incompletely understood. In patients over 65 years of age, those with OAB symptoms have been shown to perform worse on proxy testing for frailty [24, 38]. Unfortunately, frail geriatric patients are often excluded from major studies, as their multiple comorbidities and impairments may impede their participation and confound results [24]. It remains unclear whether the frailty syndrome precipitates one to develop nocturia, or if nocturia and its associated risks (i.e. falls, fractures) precipitates the frailty syndrome [41]. The relationship between frailty and polypharmacy has been more clearly established, and polypharmacy remains a prominent barrier to effectively treating nocturia in the frail cohort.
1.2 Evaluation of Nocturia
Nocturia is a symptom that may be caused by a multitude of factors; therefore, any treatments that target the symptom of nocturia must understand and target the underlying causes. The evaluation of the nocturia patient is well-defined in the general population. Few suggested changes have been made specifically for the frail adult, and thus a general discussion follows. Full evaluation begins with a thorough history and physical examination. Understanding a patient’s comorbidities and functional capacity is critical. For example, an understanding of a patient’s functional limitations with a Timed Up and Go Test will inform their mobility and functional status, and is a sensitive screening test for those who may be frail [42]. Identifying patients with postural hypotension will guide treatment and inform which medications may be contraindicated. Blood glucose level measurement may reveal uncontrolled diabetics and glucosuria as causes of global polyuria. A 24-h frequency-volume chart (FVC) is recommended in the evaluation of all patients, and some disagreement exists about whether the FVC should extend to a 3-day diary [43]. In contrast to the 24-h FVC, ‘bladder diaries’ include measurements such as incontinence episodes, fluid intake, and pad use, which may be useful in some cases but may increase the burden placed on patients. While they are different, sometime patients refer to FVCs as a ‘bladder diary’. To ensure an accurate FVC, the patient must measure and record the volume and timing of each urinary void. Collecting the timing and volume of all fluid intake in a 24-h time period also aids in understanding the timing of the patient’s fluid intake. This is a valuable quantitative tool that enables the provider to personalize his/her recommendations, to understand behavioral causes that may be contributing to the patient’s symptoms, and to establish what type of nocturia the patient has. This evaluation requires simple calculations and effective instruction on how to properly use the FVC.
To properly utilize the FVC, calculations of urine volumes must be made, and further definitions categorized (see Table 1). Once computed, these calculations help define the four broad, causal categories of nocturia: 24-h polyuria, NP, sleep disorders, and reduced bladder capacity. These broad categories each have various known contributing factors and may overlap in any individual patient. Indeed, many patients will have a mixed clinical picture. Sleep disorders that interrupt normal sleep patterns, such as insomnia and restless leg syndrome, may cause patients to urinate more frequently during ‘sleeping’ hours even though the patient is not actually asleep; in this case, nocturnal voiding may be considered as incidental to the sleep disorder and not true nocturia [3, 44, 45]. Problems with restful sleep are common in older adults, affecting up to one-third of these patients [46], and include increased nocturnal awakenings, earlier bedtime and awakenings, and increased movement during sleep (dream-enacting behavior). Chronic pain, heart failure, and adverse effects from common medications may contribute to awakenings and nighttime voiding [47]. In practice it is difficult to separate nocturnal voiding due to primary insomnia from true nocturia. A practical way to do so is to have the patient grade each void in accordance with an urgency perception grade (UPG). Those who void at night with no desire or with a UPG of zero do so as convenience voids [3].
Mention must be made that, while ideal, FVCs are not easily recorded by all patients. Frail older adults have multiple difficulties to contend with in awakening at night, such as gait aids, appropriate footwear, or glasses or other visual aids that require their concentration, distract from accurate recordings or make the use of diaries difficult. Cognitive impairments add a further layer of difficulty in the accurate recording or evaluation of FVCs. Additionally, any concomitant incontinence may prevent accurate recordings of voided volumes. An understanding of a patient’s functional capacity is key. When a full diary is not possible or is assumed to be inaccurate, a tabulation of the number of voids, episodes of urgency or incontinence, and number of drinks may be useful [48]. Any further information beyond a verbal history can be helpful in identifying the frequency of nocturnal voids and timing of fluid intake, which helps to understand the cause of nocturia and potential interventions.
While the topic of nocturia treatment has been covered in prior reviews [43, 49], the specific treatment difficulties concerning the frail, geriatric cohort have not been discussed elsewhere. The aims of the present review are twofold: first, to discuss evidence for treatment and pharmacotherapeutics of nocturia in the frail geriatric population, and, second, to clarify the risks of pharmacotherapy when managing nocturia in the frail older adult, with special attention paid to the efficacy and tolerability of various medications and the risks of polypharmacy.
To inform this review, we utilized all relevant studies known to the authors. Additionally, we performed a full literature search in PubMed and Google Scholar using terms such as ‘nocturia’, ‘frail’, ‘frailty’, ‘elderly’, and ‘geriatrics’, as well as the specific treatment modalities to be discussed. Emphasis was placed on studies examining the frail older adult with nocturia as a primary endpoint. However, as evidence specific to nocturia and the frail older adult is sparse, papers in which nocturia was discussed but was not a primary endpoint were included, as were papers examining the older adult, and papers with cohorts that had a mean age of 65 years or older.
2 The Evidence for Nocturia Treatments
2.1 Behavior and Lifestyle Modifications
The safest interventions for nocturia are lifestyle and behavioral modifications, as well as therapeutic optimization of comorbidities [3]. Behavioral interventions are safe, cheap, and, in some cases, simple to implement; however, no trials have evaluated the efficacy of any behavioral intervention on nocturia in the frail older adult. Thus, recommendations are based on extrapolations from healthier and/or younger cohorts, along with the logical rationale that they are unlikely to be harmful if performed with a frail patients’ comorbidities and limitations in mind.
It is known that lower extremity edema in the older adult is correlated with NP [50], and that increased fluid redistribution from edema is correlated with earlier awakening due to nocturia, likely due to redistribution of fluid from lower extremity interstitial space back to the vasculature [51]. This has led to the recommendation to utilize compression stockings throughout the day and elevation of the legs several hours before bed in patients with edema. This has not been evaluated in either older adults or frail older adults. A prospective, non-controlled, observational study found that compressive leg stockings are effective in reducing nocturia and NP in young wheelchair-bound patients with spinal cord injuries [52]. No studies evaluating solely leg elevation as an intervention were identified. The majority of fluid distribution when transitioning to the supine position appears to take place within 30–60 min in healthy subjects [53]. Such interventions are unlikely to have adverse effects on patients. Therefore, 30–60 min of leg elevation in the evening before bed, and/or compressive leg stockings, are reasonable interventions to attempt, as tolerated by patients. In those with compressive stockings, the region should be inspected to ensure that no skin breakdown or wounds occur.
Management of fluid intake, including distributing fluid consumption more equally throughout the day, refraining from fluid intake 3–4 h before sleeping, and global fluid restriction may be effective [3, 54,55,56]. A single arm, non-controlled, prospective trial evaluating 65 healthy male patients (mean age 72 years) with NP-related nocturia attempted to examine global fluid restriction. The authors of that study evaluated patient’s total urine output divided by their bodyweight. They instructed patients to reduce their total fluid intake until their urine output was < 30 mL/kg (mean decrease 402 ± 522 mL/day), while continuing to drink whenever they felt thirsty. One month after this intervention, they found that patients had decreased their average nocturnal voids from 4.1 to 3.1, a mean reduction of 1 ± 1.2 voids (p < 0.001). Multivariate analysis found that a decrease in 24-h fluid restriction and daytime fluid restriction were associated with clinical effects, but not evening fluid restriction. The patients had no change in their serum osmolality or electrolyte concentrations and experienced no adverse events [57]. This evidence lends support to fluid restriction in patients with high fluid intake and global urine output > 30 mL/kg. However, the exact intervention of how patients decreased their fluid intake is unclear, making specific recommendations difficult. Furthermore, these patients cannot be considered to be frail, which makes full confidence in the validity of our proposed cohort difficult. The fact that the frail cohort is more susceptible to electrolyte and volume disturbances should be considered, as should the potential consequences of constipation, dry mucous membranes, and thirst should fluid intake be undertaken [58].
Pelvic floor muscle (PFM) exercises, known as ‘Kegel exercises’, have also been found to be effective in generally healthy patients, but have not been studied specifically in the frail cohort. With these exercises, the patient is instructed to relax the abdominal muscles while contracting the pelvic floor for 2–10 s, alternating with rest for 2–10 s, for a total of 45 sessions per day, 3 days per week. Often, the patient breaks these into multiple sessions throughout the day (i.e. 3 sessions of 15 sets per day) and should be instructed to slowly increase the duration of the contractions over time. These exercises, along with practiced delayed voiding throughout the day and timed convenience voids at night, help to strengthen the pelvic musculature and decrease nocturnal voiding symptoms. It is critical that patients are properly instructed on how to contract the PFMs without contracting their large abdominal muscles. This is often done through feedback while a clinician palpates the perineal body and abdomen for contraction. Sessions with physical therapists with expertise in this area may be beneficial. One two-site, randomized controlled trial, the Male Overactive Bladder Treatment in Veterans (MOTIVE) trial, randomized 143 men (mean age 64 years) with OAB taking α-blockers to receive pharmaceutical treatment with dose-titrated oxybutynin or behavioral treatment (including PFM exercises and urge suppression techniques) for 8 weeks. The behavioral group had a greater decrease in mean nocturia episodes than the drug group (0.70 vs. 0.32, p = 0.05) [55]. Secondary analysis of another three-arm, randomized, placebo-controlled trial that evaluated 131 women (mean age 67.9 years) with nocturia and predominantly urgency incontinence who underwent 8 weeks of treatment with biweekly behavioral coaching, including PFM exercises, drug treatment with oxybutynin, or placebo, found that behavioral treatment was the most effective arm, with a mean decrease in 0.5 voids per night, compared with drug treatment (0.3 voids per night; p < 0.02) and placebo (0 voids per night; p < 0.001) [59]. While statistically significant, these results may not be clinically significant, as the total decrease was small. These trials lend some support to the use of PFM exercises for the treatment of nocturia associated with OAB symptoms or incontinence. While no trials have evaluated whether PFM exercises are effective in isolated nocturia, or in the frail older adult, they are commonly recommended due to their safety when compared with surgical or pharmacologic interventions. Intuitively, they are likely efficacious and unlikely to have adverse effects in frail older adults [60].
Interventions aimed at improving sleep quality may also be beneficial. A randomized trial in 60 patients over the age of 60 years (mean age 72 years) found that a brief behavioral insomnia treatment decreased the total number of nocturnal voiding episodes by 31% over a 2-week period (p < 0.01), whereas the control group had no change. These patients also had improvements in sleep quality, and this is likely a clinically significant difference.
A reduction in salt intake has been found to be effective, while also being beneficial for overall cardiovascular health outcomes. One retrospective review of 74 older adults (mean age 67 years) who underwent comprehensive salt reduction counselling by their cardiologists and followed this regimen found a mean reduction in nocturnal voids from 2.5 to 1.0 (p < 0.01), whereas those who were not adherent to the regimen had no change in nocturnal voids [61]. Furthermore, a prospective cohort study of 321 patients (mean age 64.3 years) with single nightly void nocturia and elevated salt intake were chosen to undergo salt reduction counselling every 4 weeks for 12 weeks. They found that those who reduced their salt intake had a reduction from 1.9 to 1.3 voids per night (p < 0.001), as well as improvement in the QoL index [62]. These are both small contributions that may not be clinically significant. Such interventions should be undertaken with full consideration of a patient’s comorbidities. For instance, they should be avoided in patients with orthostatic hypotension or those at risk of falls. Conversely, they may be beneficial in patients with ascites or heart failure.
A three-arm, randomized trial of 72 men > 40 years of age (mean age 65.8 years) with nocturia examined behavioral treatments (leg elevation, PFM exercises, fluid management, and sleep hygiene behaviors, including avoidance of alcohol and caffeine in the afternoon; minimization of noise, light, and temperature extremes in the bedroom; and avoidance of strenuous exercise or large meals before bed) compared with tamsulosin 0.4 mg or combined treatment with both for 12 weeks. The trial found that the behavioral treatment-alone group had a reduction of 1.39 voiding episodes per night (p < 0.001), along with improvements in sleep quality, QoL, and nocturia bother. These results were not statistically different from the tamsulosin or combined treatment arms [63]. In contrast to the trials examining PFM exercises alone, these results are likely clinically significant and support that comprehensive behavioral interventions are effective when undertaken, although the ability for community-dwelling frail adults to effectively implement them is unknown. While individual behavioral adjustments may lead to only small improvements, they likely have additive effects.
Optimizing a patient’s existing medications is a crucial step in addressing nocturia. Careful review of prescriptions may reveal the use of pharmacotherapeutics that have been found to be independent risk factors for nocturia. These include calcium channel blockers, diuretics, selective serotonin reuptake inhibitors (SSRIs), and lithium [3, 64]. Therefore, the elimination or substitution of these medications for others may be beneficial. Physicians may also find it effective to use existing treatments for comorbidities to benefit nocturia. For example, optimal management of patients with diabetes may alleviate glucosuria as a cause of polyuria. In patients with OSA, the use of continuous positive airway pressure (CPAP) has been shown to be highly effective at reducing nocturia, although this has not been studied specifically in frail older adults [65]. Adjustments in medication timing may also be beneficial in improving nocturia symptoms and may prevent the need for increased medication burden. For instance, the nighttime administration of diuretics may actually exacerbate nocturia, while administration in the afternoon has shown a beneficial impact on symptoms [8].
Non-dipping hypertension is one proposed mechanism of nocturia [66,67,68,69]. To that end, a clinical trial is currently underway to examine whether the nighttime administration of antihypertensives, given to decrease nocturnal blood pressure, has efficacy in treating nocturia symptoms [70]. This will be the first trial to provide data on whether such an approach is effective beyond theoretical means but has been found to be safe and to improve cardiovascular mortality outcomes [71, 72].
If behavioral and lifestyle interventions do not yield adequate improvement in nocturia, pharmacotherapy may be considered. Because frail older adults are largely underrepresented in clinical trials, we lack data concerning the efficacy of pharmacologic treatment of nocturia in this cohort. Therefore, evidence pertaining to frail older adults must be extrapolated from studies of healthier older adults, while keeping in mind the increased potential for medication safety hazards in the frail population. It is of the utmost importance that treatment for nocturia be based on objective improvements in the patient’s QoL, and the clinician should avoid continued treatment if it yields little benefit in this domain.
2.2 Arginine-Vasopressin Agonists (Desmopressin)
NP is a major contributing cause of nocturia in older adults [7, 43]. Desmopressin acetate, an antidiuretic, has long been considered the first-line pharmacologic treatment for NP [43]. Desmopressin is an AVP analog that acts as an agonist at V2 receptors, thereby facilitating urine concentration and decreasing urine volume via the reabsorption of water in the collecting ducts and ascending loop of Henle without effects on coagulation seen at higher dosing [73]. Despite the epidemiology of this pathology, few studies evaluate arginine-vasopressin agonists specifically in the older adult, and none have done so in the frail older adult. The majority of randomized controlled trials studying desmopressin recruit patients >18 years of age [74,75,76,77]. Even those trials that title themselves as studying the ‘older adult’ recruit patients >50 [78, 79] or > 60 years of age [80, 81]. One trial recruited patients >65 years of age—a randomized, double-blinded, placebo-controlled trial with 115 men with BPH (mean age 74 years) who received 0.1 mg of desmopressin tablets. The trial found that 61.4% of patients treated with desmopressin reduced their nightly voids by two or more over 12 months of treatment, versus 13.8% in the placebo group (p < 0.001). This likely represents a clinically meaningful response. The treatment group also had lower overnight urine production, longer first period of sleep prior to voiding, and improved QoL compared with the placebo group. A single patient dropped from the treatment arm due to symptomatic hyponatremia. There was no difference in episodes of asymptomatic hyponatremia (10 and 9, respectively) or other adverse events (17 and 19, respectively) between the treatment and placebo arms. Kaminetsky et al. pooled two double-blind, randomized controlled trials of patients >50 years of age (54% of their patients were > 65 years of age), and found that both low and high doses of desmopressin nasal spray (SER120, i.e. Noctiva©) showed significant reductions in mean nocturnal voids (− 1.4 with 0.83 μg and − 1.5 with 1.66 μg) compared with placebo [78]. Additionally, both treatment arms had a significant number of patients who achieved > 50% reduction in mean nocturnal voids compared with placebo. Significant findings were also noted in the following secondary endpoints: time from bedtime to first nocturnal void, percentage of nights with fewer than one nocturnal void episodes, percentage of patients with remission of nocturia symptoms (0 voids per night), and reduction in nocturnal urine volume. Hyponatremia occurred at higher rates in the treatment groups than in the placebo groups (11.2% vs. 4.4%, 2% vs. 0, and 1.1 vs. 0.2% in 135–130, 130–125, and < 125 mmol/L, respectively, in the high-dose versus placebo groups). Higher rates of hyponatremia were also noted in the low-dose treatment group than the placebo group. This treatment was specifically studied in older adults and is marketed as such, however less data are available and the risk of hyponatremia is still highly concerning. It is worth noting that these trials excluded patients with numerous comorbidities and contraindicated conditions, including uncontrolled hypertension, diabetes, and heart failure, among others. The patient population studied is likely healthier than the average older adult and is almost certainly not frail. Adverse effects of desmopressin include headache, nausea, diarrhea, lower extremity edema, dizziness, and hyponatremia. Symptomatic hyponatremia is the most dangerous adverse reaction, carrying a black-box warning on sublingual and nasal spray preparations [82, 83]; standard tablet preparations may carry up to a 6% incidence of hyponatremia in patients aged > 65 years, and can result in falls, severe morbidity and even mortality, especially in the frail cohort [77]. Of note, there is a sex-specific difference in desmopressin efficacy and responsiveness. Women require a lower dosage for symptomatic relief and have a higher risk of hyponatremia than men. This may be attributed to the location of the vasopressin V2 receptor gene on the X chromosome; because it is present in an area of relatively decreased inactivation, women express higher levels of the receptor than men, which increases their sensitivity to desmopressin [84, 85].
The American Geriatrics Society (AGS) Beers Criteria has classified desmopressin as a potentially inappropriate medication [86]. Additionally, frailty is a contraindication for desmopressin use per the ICS and should only be utilized if deemed necessary and all other treatment options have been exhausted [43]. Numerous contraindications exist (see Table 2) and no further trials of desmopressin treatment in older adults have been performed since these recommendations were made.
As this cohort carries the highest risk of adverse outcomes from desmopressin treatment, the risks of mortality and severe adverse effects must be balanced against the expected QoL improvement that comes from a potential decrease of one to two nocturnal voids. If lifestyle adjustments and management of comorbidities have failed, the use of desmopressin has been deemed necessary, and the patient has been adequately informed of the risks, it is recommended to start older adults at the lowest therapeutic dose in order to avoid adverse effects reported with higher doses [87].
Patients should be screened before a trial of desmopressin to check for hyponatremia, and all older adult patients should have routine monitoring of serum sodium levels. While ICS recommendations state that a sodium level of 130–135 mEq/L is a relative contraindication only, one trial found that those over 65 years of age with initial hyponatremia had a 75% absolute risk of experiencing symptomatic hyponatremia [88], and another found that a baseline sodium level of < 135 mEq/L was the highest risk factor for clinically significant hyponatremia (hazard ratio 16.5, p < 0.001) [89].
ICS and US FDA recommendations for serum sodium concentration monitoring in those > 65 years of age state that levels should be taken within 3–7 days of initiating treatment and 1 month following initiation. No guidance on sodium monitoring is given specifically for the frail population. Patients found to have a serum sodium level < 130 mEq/L, regardless of symptoms, should discontinue desmopressin. If the patient has symptoms consistent with hyponatremia and a serum sodium level between 130 and 135 mEq/L, desmopressin treatment should be stopped. Asymptomatic patients with a serum sodium level of 130–135 mEq/L should be monitored for persistence of hyponatremia and should not increase their dosage [43]. Retrospective analysis of 1443 patients (mean age 61 years) across three randomized controlled trials found that all cases of clinically significant hyponatremia would have been averted with such a screening program [89]. Nocturnal fluid restriction is advised to help avoid hyponatremia, which should already be part of an effective behavioral treatment of nocturia and should continue if prescribed desmopressin. Additionally, FDA prescribing information suggests ‘more frequent sodium monitoring’ in patients taking medications that increase the risk of fluid overload or hyponatremia, including tricyclic antidepressants (TCAs), SSRIs, chlorpromazine, lamotrigine, carbamazepine, opiate analgesics, and nonsteroidal anti-inflammatory drugs (NSAIDS) [82, 83, 90]. Follow-up and subsequent laboratory work should take place with any medication changes, and patients should be advised to watch closely for symptoms that could indicate hyponatremia. The development of clinically significant hyponatremia can occur even several months after starting medication, therefore older adults taking desmopressin should be carefully monitored every 6 months [43]. This surveillance is costly and onerous to both physicians and patients and should be considered and discussed at length with the patient prior to institution of desmopressin as a treatment modality.
2.3 α-Blockers
α1-Adrenoceptor (AR) antagonists are commonly used in the treatment of men with LUTS associated with BPH and bladder outlet obstruction (BOO). Relief of symptoms caused by BOO is achieved via relaxation of the bladder neck or reduction of the outlet obstruction. This class of drugs also modifies afferent pathways of micturition which decreases voiding frequency [91, 92].
To our knowledge, no studies exist that specifically examine α-blockers as a treatment for nocturia in the frail, older adult, nor do any studies exist that specifically target patients who are solely > 65 years of age; however, we identified a single study that included patients > 50 years of age and performed a subgroup analysis of patients aged > 70 years of age. Furthermore, we identified several studies examining the treatment of nocturia with α-blockers that included a population with a mean age of > 65 years.
A single double-blind, randomized controlled trial of 2583 men compared four treatment arms, comprised of doxazosin, finasteride, and finasteride + doxazosin, with placebo in the treatment of LUTS and included nocturia as an outcome. The trial subgrouped patients by age above and below 70 years. Those aged >70 years (mean age 73.7 ± 3.1) had a decrease of 0.46 and 0.59 voids per night compared with baseline at 1 and 4 years of treatment, respectively (p < 0.05). There was no apparent benefit to combination therapy with finasteride [93]. These results are likely clinically insignificant.
One study pooled the results from three double-blind, randomized, placebo-controlled trials with a total of 1479 men > 50 years of age (mean age 65 years) randomized to silodosin versus placebo and found a decrease of 0.2 voids per night (p < 0.0001), and 61% versus 48% had a decrease of more than one void per night (p = 0.0003) after 12 weeks [94]. These results are likely clinically insignificant. An international randomized, double-blind, placebo-controlled study of silodosin and tamsulosin use in men > 50 years of age with LUTS/BPH (mean age of 65.8 years; 44% aged 65–74 years and 14% aged > 75 years) found that, for the treatment of LUTS with nocturia as a secondary endpoint only, silodosin was effective (− 0.9 voids from baseline, p = 0.013), while tamsulosin was not [95]. This result may be clinically significant, however whether it extends to the frail cohort is unknown. Although α-blockers have not been widely studied in women, a single prospective observational study evaluating the use of tamsulosin in 296 women >20 years of age (mean age 58.3 ± 11.2) found a significant decrease in the number of nocturnal voids (− 1.12), as well as improvements in sleep quality, International Prostate Symptom Scores, and other clinical markers [91]. It is unknown if these results are translatable to older adults, especially the frail. More evidence is needed before recommendations for their use in women can be given.
These medications are largely well-tolerated with few adverse effects among the general population. With respect to the aging population, this class of medication carries a notable risk of orthostatic hypotension secondary to vasodilation, which is compounded if the patient is taking nitrates. The prevalence of orthostatic hypotension in ambulatory patients over 65 years of age is estimated to be 10–30% [96], which can lead to lightheadedness, falls, and syncope. Fall-associated injuries have a significant impact on older adults [97]. A population-based study of 147,084 men over the age of 66 years first prescribed α-blockers, compared with an equal size group of men not prescribed α-blockers, found a small but significantly increased risk of an emergency room visit or hospital admission for falls (odds ratio [OR] 1.14), fracture (OR 1.16), hypotension (OR 1.8), and head trauma (OR 1.15) within 90 days of initiating treatment [98]. Frail individuals have larger reductions in systolic arterial pressure upon orthostatic changes, and are known to be at a high risk of falls at baseline than the non-frail older adult [99].
Recently, there has been concern that the use of α-blockers, specifically tamsulosin, in men with LUTS/BPH may be associated with an increased risk of developing dementia [100, 101]. However, while Duan et al. found a significantly higher risk of dementia in older men taking tamsulosin in a large-scale study in the US, a 2019 large-scale study of Korean adults by Tae et al. in response, which addressed proposed methodological flaws in the prior study, failed to find any significant association between α-blocker use and incidence of dementia [101, 102]. More research is required before definitive conclusions may be drawn, and it is noted that this association lacks mechanistic plausibility [103]. Regardless, clinicians should be observant of changes in their patients. Given the vulnerability of frail, older adults to orthostatic hypotension and the risk of fall-related morbidity and mortality, the potentially small benefits of α-blockers alone for the treatment of nocturia in this population should be weighed against the risks in men. The evidence does not support their use in women.
2.4 Antimuscarinics
Antimuscarinics have long been the gold standard for the treatment of daytime OAB, and the efficacy of this drug class extends to the sensation of nocturnal urgency in younger patients, although their efficacy in treating a number of nocturnal micturitions is potentially clinically insignificant [104,105,106,107,108,109,110]. The micturition reflex is mediated via parasympathetic efferent pathways to the detrusor muscle and bladder neck. Acetylcholine is released and binds to M3 muscarinic receptors, facilitating the contraction of the detrusor muscle [111,112,113]. Antimuscarinic agents preferentially antagonize M2 and M3 receptors, thereby blocking the micturition reflex and decreasing contractility and instability of the detrusor.
Despite their wide use, there is a paucity of data examining antimuscarinic use for the treatment of nocturia in those over the age of 65 years. A single study examining frail older adults was identified. A randomized, flexible dose, placebo-controlled trial by DuBeau et al. evaluated fesoterodine in a medically complex, community-dwelling population of 582 older adults (aged > 65 years; mean age 75 years, 50% > 75 years) with urgency urinary incontinence, and tracked nocturnal urgency episodes [114]. These adults had high rates of polypharmacy and comorbidities, and the treatment group was assigned to 12 weeks of fesoterodine 4 mg, which could be escalated to 8 mg at any point. Ultimately, the study found that treatment with fesoterodine did not significantly affect the number of nocturnal micturitions in this cohort. Therefore, there is no evidence for the use of antimuscarinic medications for the treatment of nocturia in frail older adults.
As further evidence against their use, muscarinic receptors predominate across the body and mediate numerous physiologic effects. Therefore, antimuscarinic agents carry a number of potential adverse effects, many of which are magnified in the older adult and frail populations. These include, but are not limited to, dry eyes, dry mouth, urinary retention, constipation, risk of falls, and cognitive impairment [113, 115, 116]. These adverse effects can be especially detrimental to older and frail older adults, and can influence medication adherence, as well as overall health. Constipation is known to be very bothersome to patients [117] and, more seriously, can cause urinary retention, fecal impaction, obstruction, rectal prolapse, and increased risk of cerebrovascular disease or myocardial infarction due to straining [118, 119]. In contrast to α-blockers, the association of antimuscarinics with cognitive changes is well-supported and should not be underestimated [103]. The AGS Beers Criteria has recommended avoiding these drugs in patients with constipation, delirium, dementia, or cognitive impairment. Additionally they recommend avoiding coadministration of medications with anticholinergic properties due to possible additive effects [86]. Therefore, the lack of evidence for efficacy, in conjunction with their relative contraindication for use in older adults due to the high risk of adverse effects, indicates that antimuscarinics should not be utilized to treat nocturia in frail older adults.
2.5 β3-Adrenergic Agonists
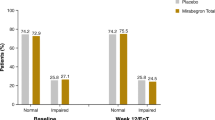
β3-agonists target β3 receptors in the bladder, which induces bladder smooth muscle relaxation during the filling phase, and predominantly reduces urinary urgency with minimal effects on voided volume [120, 121]. Mirabegron (Myrbetriq) is currently the only approved β3-agonist for OAB symptoms, with another formulation, vibegron, now undergoing phase III trials [122]. Mirabegron has been studied for the treatment of OAB, with nocturia as a secondary endpoint. No trials exist that study mirabegron specifically in the frail older adult. One prospective observational trial examining patients with numerous comorbidities grouped 217 patients into a 40- to 60-year age group (62 patients) and an 80+ age group (155 patients), and were administered mirabegron 25 mg for 12 weeks. These patients had a statistically significant reduction in the number of nocturia episodes of −0.18 from baseline (p = 0.005) [123]. Furthermore, a recent meta-analysis of eight trials and 10,248 adults with OAB treated with mirabegron found a decrease in nocturia episodes of − 0.13 to − 0.16 (from lowest to the highest dose administered) [124]. While statistically significant, these results are likely clinically insignificant; therefore, the evidence does not support the use of mirabegron in the treatment of nocturia in frail adults.
2.6 Nonsteroidal Anti-Inflammatory Drugs
Although several studies have examined the use of NSAIDs in the treatment of OAB (93-95), as of yet no studies have examined the use of NSAIDs for treatment of nocturia specifically in the older adult or frail older adult populations. Clinicians should nevertheless be aware of specific guidelines for NSAID use in geriatric patients along with standard contraindications. Patients with gastrointestinal symptoms or disease, renal dysfunction, or bleeding and coagulation disorders should not use NSAIDs [125]. Additionally, the AGS 2015 Beers Criteria recommends against the chronic use of all NSAIDs due to the risk of gastrointestinal bleeding in high-risk groups, which includes those over the age of 75 years [86]. Therefore, although some evidence supports the clinical utility of using NSAIDs in the armamentarium of nocturia treatment, concern about these contraindications and the adverse effects currently prevents them from being used as first- or second-line agents.
2.7 Upcoming/In-Trial Pharmacologic Agents
Several trials are currently underway to develop agents that treat NP while decreasing the likelihood of hyponatremic events. This may be achieved by novel medications that are similar to desmopressin but have different pharmacological activity at the V2 receptor [126,127,128]. Fedovapagon, SK-1404, and FE 201836 are three such novel compounds that have progressed to clinical trials [129,130,131]; results from these trials are still pending. None of these trials are specific to the frail or older adult cohorts, and it remains to be seen if results will include subgroup analyses or will enable the clinician to elucidate the role of these novel compounds in treating the frail older adult patient.
3 Discussion on American Geriatrics Society Beers Criteria and Polypharmacy
When discussing the implementation of pharmacotherapy in the older adult and frail cohorts, we must address the issue of polypharmacy. Polypharmacy is the concomitant use of multiple medications in a single patient. While the numerical cut-off for polypharmacy is not well-defined, the most commonly cited number in the literature is the use of five or more medications; however, this is not by a clear majority, and an actual range of ≥ 2 to ≥ 11 medications has been utilized [132]. It is more important to define ‘appropriate’ versus ‘inappropriate’ polypharmacy, although disagreement also exists in how to apply these terms [41, 132, 133]. This leaves ample room for confusion among practitioners and may contribute to the prevalence of polypharmacy [132]. Regardless of definition, it is important to recognize that the simultaneous use of multiple medications carries several negative consequences, including, but not limited to, increased financial cost, reduced medication adherence, increased risk of adverse medication interactions, increased risk of drug toxicity, and increased risk of geriatric syndromes, including falls, cognitive impairment, and malnutrition [41, 133].
Polypharmacy is commonplace in the older adult, given this cohort’s tendency for multiple comorbid conditions requiring pharmacologic treatment. It is difficult for physicians to balance the pharmacologic treatment of comorbidities with the known risks of polypharmacy. In the frail geriatric patient, polypharmacy poses an even greater danger in terms of adverse outcomes and mortality [41]. There is evidence supporting a bidirectional, multifactorial relationship between polypharmacy and frailty. Frailty has been associated with changes in drug pharmacokinetics, which may result in an enhancing effect on drug–drug interactions and toxicity, thereby worsening the frail state [41, 134]. Moreover, the prevalence of comorbid conditions in the frail adult may warrant multiple prescriptions and, likewise, the prescription of multiple medications may carry adverse effects that contribute to developing frailty. In their systematic review of literature describing the relationship between frailty and polypharmacy, Gutiérrez-Valencia et al. noted that the studies examined made no definitive conclusions about a causal relationship between frailty and polypharmacy [41]. Therefore, the intertwined nature of polypharmacy and frailty presents a unique challenge and merits future research.
Clinicians treating nocturia should take several steps to address polypharmacy. As discussed, the effective treatment of nocturia often requires optimization of current medications, including the elimination or substitution of possible contributors to nocturia, and alterations in medication timing that may improve nocturia symptoms. These steps should be taken before considering prescribing an additional medication, especially in patients already under a heavy pill burden. When additional medications are considered, their potential interactions, harms, and likely expected benefit should be weighed before prescribing.
4 Conclusion
Nocturia is a prevalent and bothersome complaint that lies at the intersection of a variety of common and serious health conditions. Behavioral and lifestyle adjustments are the cornerstone of any effective treatment for nocturia. In addition to behavioral modifications, the appropriate optimization of patients’ other comorbidities and consideration of currently prescribed medications are a crucial element in treating nocturia. When these fail, pharmacologic agents may be considered to be added to the treatment regimen only after serious deliberation. Given the increased prevalence of polypharmacy in geriatric and frail cohorts, clinicians must weigh the risks and benefits of nocturia pharmacotherapy in these patients.
Many drug trials that use a cohort of older adults are limited by recruiting predominantly healthy older adult participants; therefore, although some pharmacologic nocturia treatments may be efficacious in these older adult cohorts, it is difficult to generalize the results of these trials to the frail older adult population. What is known is that many medications used to treat nocturia have pronounced adverse effects in the older adult and frail cohorts. The goal should be avoidance of these potentially harmful agents, as well as those that may induce or worsen nocturia. Clinicians should be aware of available criteria that outline relatively contraindicated medications for the frail and older adult populations. After these steps have been taken, two medication classes (α-blockers and AVP agonists) may be used judiciously if the benefits in patient QoL outweigh the risks of serious adverse effects, some of which include delirium, cognitive changes, electrolyte abnormalities, falls, and death.
Older adults and frail patients should be monitored closely and routinely after starting medications for the treatment of nocturia. Patients and their caregivers should be involved in discussions surrounding treatment. QoL, patient-specific goals, and individualized consideration of risk factors should always be a priority, and shared decision making is paramount to treatment success. Importantly, patients should have accurate expectations for their clinical response, and the expected and real improvement in QoL should be balanced against the risks associated with each treatment, as well as the global risk polypharmacy poses to the older adult. The patient should be re-engaged in these discussions over time to reassess their response to treatment, their goals of care, and the need for treatment. Therefore, we conclude that the optimal evaluation of nocturia in an older adult or frail older adult should be centered on (1) the optimization of comorbidities and reduction of polypharmacy; (2) behavioral and lifestyle adjustments; (3) the assessment of drug–disease interaction; and (4) the judicious consolidation of goals. In this way, the treatment of nocturia can act as a nidus for holistic improvement in patient care.
References
Hashim H, Blanker MH, Drake MJ, Djurhuus JC, Meijlink J, Morris V, et al. International Continence Society (ICS) report on the terminology for nocturia and nocturnal lower urinary tract function. Neurourol Urodyn. 2019;38(2):499–508.
Tikkinen KAO, Johnson TM, Tammela TLJ, Sintonen H, Haukka J, Huhtala H, et al. Nocturia frequency, bother, and quality of life: how often is too often? A population-based study in Finland. Eur Urol. 2010;57(3):488–98.
Weiss J, Marshall S. Nocturia. In: Wein A, Kavoussi L, Partin A, Peters C, editors. Campbell Walsh Urology. 11th ed. Elsevier: Amsterdam; 2016. p. 1821–35.
Bing MH, Moller LA, Jennum P, Mortensen S, Skovgaard LT, Lose G. Prevalence and bother of nocturia, and causes of sleep interruption in a Danish population of men and women aged 60–80 years. BJU Int. 2006;98(3):599–604.
Kupelian V, Wei JT, O’Leary MP, Norgaard JP, Rosen RC, McKinlay JB. Nocturia and quality of life: results from the Boston Area Community Health Survey. Eur Urol. 2012;61(1):78–84.
Endeshaw YW, Schwartz AV, Stone K, Caserotti P, Harris T, Smagula S, et al. Nocturia, insomnia symptoms and mortality among older men: the health, aging and body composition study. J Clin Sleep Med. 2016;12(6):789–96.
Weiss JP, Monaghan TF, Epstein MR, Lazar JM. Future considerations in nocturia and nocturnal polyuria. Urology. 2019;133:34–42.
Oelke M, De Wachter S, Drake MJ, Giannantoni A, Kirby M, Orme S, et al. A practical approach to the management of nocturia. Int J Clin Pract. 2017;71(11):e13027.
Hafner M, Andersson FL, Burtea T, van Stolk C, Whitmore M, Yerushalmi E, et al. Assessing the burden of nocturia in the workplace: the associations between nocturnal voiding, subjective well-being, work engagement and productivity. J Med Econ. 2020;23(9):994–1003.
Asplund R. Nocturia in relation to sleep, somatic diseases and medical treatment in the elderly. BJU Int. 2002;90(6):533–6.
Bliwise DL, Howard LE, Moreira DM, Andriole GL, Hopp ML, Freedland SJ. Nocturia and associated mortality: observational data from the REDUCE trial. Prostate Cancer Prostatic Dis. 2019;22(1):77–83.
Coyne KS, Zhou Z, Bhattacharyya SK, Thompson CL, Dhawan R, Versi E. The prevalence of nocturia and its effect on health-related quality of life and sleep in a community sample in the USA. BJU Int. 2003;92(9):948–54.
Parsons JK, Mougey J, Lambert L, Wilt TJ, Fink HA, Garzotto M, et al. Lower urinary tract symptoms increase the risk of falls in older men. BJU Int. 2009;104(1):63–8.
Kupelian V, Fitzgerald MP, Kaplan SA, Norgaard JP, Chiu GR, Rosen RC. Association of nocturia and mortality: results from the third national health and nutrition examination survey. J Urol. 2011;185(2):571–7.
Funada S, Tabara Y, Setoh K, Negoro H, Akamatsu S, Yoshino T, et al. Impact of nocturia on mortality: the Nagahama Study. J Urol. 2020;204(5):996–1002.
Fan Y, Wei F, Lang Y, Qi W. Meta-analysis of nocturia and risk of all-cause mortality in adult population. Int J Cardiol. 2015;195:120–2.
Pesonen JS, Cartwright R, Vernooij RWM, Aoki Y, Agarwal A, Mangera A, et al. The impact of nocturia on mortality: a systematic review and meta-analysis. J Urol. 2020;203(3):486–95.
Soysal P, Cao C, Xu T, Yang L, Isik AT, Turan Kazancioglu R, et al. Trends and prevalence of nocturia among US adults, 2005–2016. Int Urol Nephrol. 2020;52(5):805–13.
Elbadawi A, Hailemariam S, Yalla SV, Resnick NM. Structural basis of geriatric voiding dysfunction. VII. Prospective ultrastructural/urodynamic evaluation of its natural evolution. J Urol. 1997;157(5):1814–22.
Lowalekar SK, Cristofaro V, Radisavljevic ZM, Yalla SV, Sullivan MP. Loss of bladder smooth muscle caveolae in the aging bladder. Neurourol Urodyn. 2012;31(4):586–92.
Siroky MB. The aging bladder. Rev Urol. 2004;6(Suppl 1):S3-7.
Dutoglu E, Soysal P, Smith L, Arik F, Kalan U, Kazancioglu RT, et al. Nocturia and its clinical implications in older women. Arch Gerontol Geriatr. 2019;85:103917.
Natalin R, Lorenzetti F, Dambros M. Management of OAB in those over age 65. Curr Urol Rep. 2013;14(5):379–85.
Suskind AM. The aging overactive bladder: a review of aging-related changes from the brain to the bladder. Curr Bladder Dysfunct Rep. 2017;12(1):42–7.
Hanlon JT, Aspinall SL, Semla TP, Weisbord SD, Fried LF, Good CB, et al. Consensus GUIDELINES FOR ORAL DOSING OF PRIMARILY RENALLY CLEARED MEDICATIONS IN OLDER ADULTS. J Am Geriatr Soc. 2009;57(2):335–40.
Pinggera G-M, Mitterberger M, Steiner E, Pallwein L, Frauscher F, Aigner F, et al. Association of lower urinary tract symptoms and chronic ischaemia of the lower urinary tract in elderly women and men: assessment using colour Doppler ultrasonography. BJU Int. 2008;102(4):470–4.
Kim S, Jeong JY, Choi YJ, Kim DH, Lee WK, Lee SKSH, et al. Association between lower urinary tract symptoms and vascular risk factors in aging men: the Hallym Aging Study. Korean J Urol. 2010;51(7):477.
Duffy JF, Scheuermaier K, Loughlin KR. Age-related sleep disruption and reduction in the circadian rhythm of urine output: contribution to nocturia? Curr Aging Sci. 2015;9(1):34–43.
Van Kerrebroeck P, Andersson K-E. Terminology, epidemiology, etiology, and pathophysiology of nocturia. Neurourol Urodyn. 2014;33(Suppl 1):S2-5.
Van Kerrebroeck P, Hashim H, Holm-Larsen T, Robinson D, Stanley N. Thinking beyond the bladder: antidiuretic treatment of nocturia. Int J Clin Pract. 2010;64(6):807–16.
Tani M, Hirayama A, Fujimoto K, Torimoto K, Akiyama T, Hirao Y. Increase in 24-hour urine production/weight causes nocturnal polyuria due to impaired function of antidiuretic hormone in elderly men. Int J Urol. 2008;15(2):151–4.
Chen J-L, Chen S-F, Jiang Y-H, Kuo H-C. Practical points in the medical treatment of overactive bladder and nocturia in the elderly. Tzu Chi Med J. 2016;28(1):1–5.
Hoshiyama F, Hirayama A, Tanaka M, Taniguchi M, Ohi M, Momose H, et al. The impact of obstructive sleep apnea syndrome on nocturnal urine production in older men with nocturia. Urology. 2014;84(4):892–7.
Singh S, Bajorek B. Defining, “elderly” in clinical practice guidelines for pharmacotherapy. Pharm Pract. 2014;12(4):489.
Hilmer SN, McLachlan AJ, Le Couteur DG. Clinical pharmacology in the geriatric patient. Fundam Clin Pharmacol. 2007;21(3):217–30.
Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet. 2019;394(10206):1365–75.
Khan KT, Hemati K, Donovan AL. Geriatric physiology and the frailty syndrome. Anesthesiol Clin. 2019;37(3):453–74.
Monaghan TF, Wagg AS, Bliwise DL, Agudelo CW, Michelson KP, Rahman SN, et al. Association between nocturia and frailty among elderly males in a veterans administration population. Aging Clin Exp Res. 2020;32(10):1993–2000.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol Ser A Biol Sci Med Sci. 2001;56(3):M146–57.
Mitnitski AB, Mogilner AJ, Rockwood K. Accumulation of deficits as a proxy measure of aging. Sci World J. 2001;1:323–36.
Gutiérrez-Valencia M, Izquierdo M, Cesari M, Casas-Herrero Á, Inzitari M, Martínez-Velilla N. The relationship between frailty and polypharmacy in older people: a systematic review. Br J Clin Pharmacol. 2018;84(7):1432–44.
Clegg A, Rogers L, Young J. Diagnostic test accuracy of simple instruments for identifying frailty in community-dwelling older people: a systematic review. Age Ageing. 2015;44(1):148–52.
Everaert K, Hervé F, Bosch R, Dmochowski R, Drake M, Hashim H, et al. International Continence Society consensus on the diagnosis and treatment of nocturia. Neurourol Urodyn. 2019;38(2):478–98.
Feldstein CA. Nocturia in arterial hypertension: a prevalent, underreported, and sometimes underestimated association. J Am Soc Hypertens. 2013;7(1):75–84.
Cornu J-N, Abrams P, Chapple CR, Dmochowski RR, Lemack GE, Michel MC, et al. A contemporary assessment of nocturia: definition, epidemiology, pathophysiology, and management–a systematic review and meta-analysis. Eur Urol. 2012;62(5):877–90.
Lubetkin EI, Jia H. Burden of disease due to sleep duration and sleep problems in the elderly. Sleep Heal. 2018;4(2):182–7.
Feinsilver SH, Hernandez AB. Sleep in the elderly. Clin Geriatr Med. 2017;33(4):579–96.
Alexander L, Shakespeare K, Barradell V, Orme S. Management of urinary incontinence in frail elderly women. Obstet Gynaecol Reprod Med. 2015;25(3):75–82.
Gordon DJ, Emeruwa CJ, Weiss JP. Management strategies for nocturia. Curr Urol Rep. 2019;20(11):75.
Torimoto K, Hirayama A, Samma S, Yoshida K, Fujimoto K, Hirao Y. The relationship between nocturnal polyuria and the distribution of body fluid: assessment by bioelectric impedance analysis. J Urol. 2009;181(1):219–24.
Kiba K, Hirayama A, Yoshikawa M, Yamamoto Y, Torimoto K, Shimizu N, et al. Increased urine production due to leg fluid displacement reduces hours of undisturbed sleep. Low Urin Tract Symptoms. 2018;10(3):253–8.
Viaene A, Roggeman S, Goessaert A-S, Kessler TM, Mehnert U, Van BV, et al. Conservative treatment for leg oedema and the effect on nocturnal polyuria in patients with spinal cord injury. BJU Int. 2019;123(5A):E43-50.
Berg HE, Tedner B, Tesch PA. Changes in lower limb muscle cross-sectional area and tissue fluid volume after transition from standing to supine. Acta Physiol Scand. 1993;148(4):379–85.
Burgio KL, Kraus SR, Johnson TM, Markland AD, Vaughan CP, Li P, et al. Effectiveness of combined behavioral and drug therapy for overactive bladder symptoms in men. JAMA Intern Med. 2020;180(3):411.
Burgio KL, Goode PS, Johnson TM, Hammontree L, Ouslander JG, Markland AD, et al. Behavioral versus drug treatment for overactive bladder in men: the male overactive bladder treatment in veterans (MOTIVE) Trial. J Am Geriatr Soc. 2011;59(12):2209–16.
Johnson TM, Sattin RW, Parmelee P, Fultz NH, Ouslander JG. Evaluating potentially modifiable risk factors for prevalent and incident nocturia in older adults. J Am Geriatr Soc. 2005;53(6):1011–6.
Tani M, Hirayama A, Torimoto K, Matsushita C, Yamada A, Fujimoto K. Guidance on water intake effectively improves urinary frequency in patients with nocturia. Int J Urol. 2014;21(6):595–600.
Asplund R. Pharmacotherapy for nocturia in the elderly patient. Drugs Aging. 2007;24(4):325–43.
Johnson TM, Burgio KL, Redden DT, Wright KC, Goode PS. Effects of behavioral and drug therapy on nocturia in older incontinent women. J Am Geriatr Soc. 2005;53(5):846–50.
Niu S, Griebling TL, Kowalik CG. Impact of frailty on the treatment of pelvic floor disorders. Curr Bladder Dysfunct Rep. 2020;15:121–6.
Monaghan TF, Michelson KP, Wu ZD, Gong F, Agudelo CW, George CD, et al. Sodium restriction improves nocturia in patients at a cardiology clinic. J Clin Hypertens. 2020;22(4):633–8.
Matsuo T, Miyata Y, Sakai H. Effect of salt intake reduction on nocturia in patients with excessive salt intake. Neurourol Urodyn. 2019;38(3):927–33.
Johnson TM, Vaughan CP, Goode PS, Bliwise DL, Markland AD, Huisingh C, et al. Pilot results from a randomized trial in men comparing alpha-adrenergic antagonist versus behavior and exercise for nocturia and sleep. Clin Ther. 2016;38(11):2394-2406.e3.
Akhavizadegan H, Locke JA, Stothers L, Kavanagh A. A comprehensive review of adult enuresis. Can Urol Assoc J. 2018;13(8):282–7.
Wang T, Huang W, Zong H, Zhang Y. The efficacy of continuous positive airway pressure therapy on nocturia in patients with obstructive sleep apnea: a systematic review and meta-analysis. Int Neurourol J. 2015;19(3):178–84.
Lombardo R, Tubaro A, Burkhard F. Nocturia: the complex role of the heart, kidneys, and bladder. Eur Urol Focus. 2020;6(3):534–6.
Sugaya K, Nakada S, Simoji T, Odaguchi N, Nakamoto M, Nakazoto S. Relationship between blood pressure and nocturia in hypertensive patients. LUTS Low Urin Tract Symptoms. 2009;1(1):16–9.
Agarwal R, Light RP, Bills JE, Hummel LA. Nocturia, nocturnal activity, and nondipping. Hypertension. 2009;54(3):646–51.
Takayama M, Omori S, Iwasaki K, Shiomi E, Takata R, Sugimura J, et al. Relationship between nocturnal polyuria and non-dipping blood pressure in male patients with lower urinary tract symptoms. LUTS Low Urin Tract Symptoms. 2019;11(2):O98-102.
Cedars-Sinai Medical Center. Treating Nocturnal Hypertension and Nocturia in African American Men. ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT03319823?cond=nocturia+AND+%22Hypertension%22&draw=2&rank=2
Hermida RC, Crespo JJ, Domínguez-Sardiña M, Otero A, Moyá A, Ríos MT, et al. Bedtime hypertension treatment improves cardiovascular risk reduction: the Hygia Chronotherapy Trial. Eur Heart J. 2019. https://doi.org/10.1093/eurheartj/ehz754(Epub 22 Oct 2019).
Bowles NP, Thosar SS, Herzig MX, Shea SA. Chronotherapy for hypertension. Curr Hypertens Rep. 2018;20(11):97.
Chung E. Desmopressin and nocturnal voiding dysfunction: clinical evidence and safety profile in the treatment of nocturia. Expert Opin Pharmacother. 2018;19(3):291–8.
Lose G, Mattiason A, Walter S, Lalos O, Van Kerrebroeck P, Abrams P, et al. Clinical experiences with desmopressin for long-term treatment of nocturia. J Urol. 2004;172(3):1021–5.
Mattiasson A, Abrams P, Van Kerrebroeck P, Walter S, Weiss J. Efficacy of desmopressin in the treatment of nocturia: a double-blind placebo-controlled study in men. BJU Int. 2002;89(9):855–62.
Berges R, Höfner K, Gedamke M, Oelke M. Impact of desmopressin on nocturia due to nocturnal polyuria in men with lower urinary tract symptoms suggestive of benign prostatic hyperplasia (LUTS/BPH). World J Urol. 2014;32(5):1163–70.
Weiss JP, Zinner NR, Klein BM, Nørgaard JP. Desmopressin orally disintegrating tablet effectively reduces nocturia: results of a randomized, double-blind, placebo-controlled trial. Neurourol Urodyn. 2012;31(4):441–7.
Kaminetsky J, Fein S, Dmochowski R, MacDiarmid S, Abrams S, Cheng M, et al. Efficacy and safety of SER120 nasal spray in patients with nocturia: pooled analysis of 2 randomized, double-blind, placebo controlled, phase 3 trials. J Urol. 2018;200(3):604–11.
Rezakhaniha B, Arianpour N, Siroosbakhat S. Efficacy of desmopressin in treatment of nocturia in elderly men. J Res Med Sci. 2011;16(4):516–23.
Fu F-G, Lavery HJ, Wu D-L. Reducing nocturia in the elderly: a randomized placebo-controlled trial of staggered furosemide and desmopressin. Neurourol Urodyn. 2011;30(3):312–6.
Weinrebe W, Käbe-Frisch S, Füsgen I, Karaman M, Johannsdottir E, Rupp S. Do independent geriatric outpatients with nocturnal polyuria profit from desmopressin? Z Gerontol Geriatr. 2019;52(3):272–8.
NOCDURNA (desmopressin acetate) sublingual tablets prescribing information. 2018. http://www.ferringusa.com/wp-content/uploads/2018/06/NOCDURNA-Prescribing-Information.pdf
NOCTIVA (desmopressin acetate) prescribing information. 2017. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/201656lbl.pdf
Juul KV, Klein BM, Sandström R, Erichsen L, Nørgaard JP. Gender difference in antidiuretic response to desmopressin. Am J Physiol Physiol. 2011;300(5):F1116–22.
Yamaguchi O, Nishizawa O, Juul KV, Nørgaard JP. Gender difference in efficacy and dose response in Japanese patients with nocturia treated with four different doses of desmopressin orally disintegrating tablet in a randomized, placebo-controlled trial. BJU Int. 2013;111(3):474–84.
2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 Updated AGS Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2019;67(4):674–94.
Ebell MH, Radke T, Gardner J. A systematic review of the efficacy and safety of desmopressin for nocturia in adults. J Urol. 2014;192(3):829–35.
Rembratt A, Riis A, Norgaard JP. Desmopressin treatment in nocturia; an analysis of risk factors for hyponatremia. Neurourol Urodyn. 2006;25(2):105–9.
Juul KV, Malmberg A, van der Meulen E, Vande WJ, Nørgaard JP. Low-dose desmopressin combined with serum sodium monitoring can prevent clinically significant hyponatraemia in patients treated for nocturia. BJU Int. 2017;119(5):776–84.
Desmopressin Acetate 0.1mg and 0.2mg [package insert]. 2008. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2008/021795s000_Lbl.pdf
Kim S-O, Choi HS, Kwon D. The α1 adrenoceptor antagonist tamsulosin for the treatment of voiding symptoms improves nocturia and sleep quality in women. Urol J. 2014;11(3):1636–41.
Roehrborn CG, Cruz F, Fusco F. α1-blockers in men with lower urinary tract symptoms suggestive of benign prostatic obstruction: is silodosin different? Adv Ther. 2016;33(12):2110–21.
Johnson TM, Burrows PK, Kusek JW, Nyberg LM, Tenover JL, Lepor H, et al. The effect of doxazosin, finasteride and combination therapy on nocturia in men with benign prostatic hyperplasia. J Urol. 2007;178(5):2045–51.
Eisenhardt A, Schneider T, Cruz F, Oelke M. Consistent and significant improvement of nighttime voiding frequency (nocturia) with silodosin in men with LUTS suggestive of BPH: pooled analysis of three randomized, placebo-controlled, double-blind phase III studies. World J Urol. 2014;32(5):1119–25.
Chapple CR, Montorsi F, Tammela TLJ, Wirth M, Koldewijn E, Fernández FE. Silodosin therapy for lower urinary tract symptoms in men with suspected benign prostatic hyperplasia: results of an international, randomized, double-blind, placebo- and active-controlled clinical trial performed in Europe. Eur Urol. 2011;59(3):342–52.
Low PA. Prevalence of orthostatic hypotension. Clin Auton Res. 2008;18(Suppl 1):8–13.
Shaw BH, Claydon VE. The relationship between orthostatic hypotension and falling in older adults. Clin Auton Res. 2014;24(1):3–13.
Welk B, McArthur E, Fraser L-A, Hayward J, Dixon S, Hwang YJ, et al. The risk of fall and fracture with the initiation of a prostate-selective α antagonist: a population based cohort study. BMJ. 2015;351:h5398.
Shaw BH, Borrel D, Sabbaghan K, Kum C, Yang Y, Robinovitch SN, et al. Relationships between orthostatic hypotension, frailty, falling and mortality in elderly care home residents. BMC Geriatr. 2019;19(1):80.
Frankel JK, Duan Y, Albertsen PC. Is tamsulosin linked to dementia in the elderly? Curr Urol Rep. 2018;19(9):69.
Duan Y, Grady JJ, Albertsen PC, Helen WuZ. Tamsulosin and the risk of dementia in older men with benign prostatic hyperplasia. Pharmacoepidemiol Drug Saf. 2018;27(3):340–8.
Tae BS, Jeon BJ, Choi H, Cheon J, Park JY, Bae JH. α-Blocker and risk of dementia in patients with benign prostatic hyperplasia: a nationwide population based study using the National Health Insurance Service Database. J Urol. 2019;202(2):362–8.
Muderrisoglu AE, Becher KF, Madersbacher S, Michel MC. Cognitive and mood side effects of lower urinary tract medication. Expert Opin Drug Saf. 2019;18(10):915–23.
Weiss JP, Jumadilova Z, Johnson TM, FitzGerald MP, Carlsson M, Martire DL, et al. Efficacy and safety of flexible dose fesoterodine in men and women with overactive bladder symptoms including nocturnal urinary urgency. J Urol. 2013;189(4):1396–401.
Nitti VW, Dmochowski R, Sand PK, Forst H-T, Haag-Molkenteller C, Massow U, et al. Efficacy, safety and tolerability of fesoterodine for overactive bladder syndrome. J Urol. 2007;178(6):2488–94.
Yokoyama O, Yamaguchi O, Kakizaki H, Itoh N, Yokota T, Okada H, et al. Efficacy of solifenacin on nocturia in Japanese patients with overactive bladder: impact on sleep evaluated by bladder diary. J Urol. 2011;186(1):170–4.
Rudy D, Cline K, Harris R, Goldberg K, Dmochowski R. Multicenter phase III trial studying trospium chloride in patients with overactive bladder. Urology. 2006;67(2):275–80.
Dmochowski RR, Peters KM, Morrow JD, Guan Z, Gong J, Sun F, et al. Randomized, double-blind, placebo-controlled trial of flexible-dose fesoterodine in subjects with overactive bladder. Urology. 2010;75(1):62–8.
Herschorn S, Swift S, Guan Z, Carlsson M, Morrow JD, Brodsky M, et al. Comparison of fesoterodine and tolterodine extended release for the treatment of overactive bladder: a head-to-head placebo-controlled trial. BJU Int. 2010;105(1):58–66.
Rackley R, Weiss JP, Rovner ES, Wang JT, Guan Z. Nighttime dosing with tolterodine reduces overactive bladder-related nocturnal micturitions in patients with overactive bladder and nocturia. Urology. 2006;67(4):731–6.
Clemens JQ. Basic bladder neurophysiology. Urol Clin North Am. 2010;37(4):487–94.
Yamada S, Ito Y, Nishijima S, Kadekawa K, Sugaya K. Basic and clinical aspects of antimuscarinic agents used to treat overactive bladder. Pharmacol Ther. 2018;189:130–48.
Kay GG, Granville LJ. Antimuscarinic agents: Implications and concerns in themanagement of overactive bladder in the elderly. Clin Ther. 2005;27(1):127–38.
DuBeau CE, Kraus SR, Griebling TL, Newman DK, Wyman JF, Johnson TM, et al. Effect of fesoterodine in vulnerable elderly subjects with urgency incontinence: a double-blind. Placebo Controlled Trial. J Urol. 2014;191(2):395–404.
Peters NL. Snipping the thread of life. Antimuscarinic side effects of medications in the elderly. Arch Intern Med. 1989;149(11):2414–20.
Moga DC, Abner EL, Wu Q, Jicha GA. Bladder antimuscarinics and cognitive decline in elderly patients. Alzheimer’s Dement Transl Res Clin Interv. 2017;3(1):139–48.
Akino H, Namiki M, Suzuki K, Fuse H, Kitagawa Y, Miyazawa K, et al. Factors influencing patient satisfaction with antimuscarinic treatment of overactive bladder syndrome: results of a real-life clinical study. Int J Urol. 2014;21(4):389–94.
Zheng S, Yao J. Expert consensus on the assessment and treatment of chronic constipation in the elderly. Aging Med. 2018;1(1):8–17.
Gallagher P, O’Mahony D. Constipation in old age. Best Pract Res Clin Gastroenterol. 2009;23(6):875–87.
Nitti VW, Khullar V, van Kerrebroeck P, Herschorn S, Cambronero J, Angulo JC, et al. Mirabegron for the treatment of overactive bladder: a prespecified pooled efficacy analysis and pooled safety analysis of three randomised, double-blind, placebo-controlled, phase III studies. Int J Clin Pract. 2013;67(7):619–32.
Chapple CR, Dvorak V, Radziszewski P, Van Kerrebroeck P, Wyndaele JJ, Bosman B, et al. A phase II dose-ranging study of mirabegron in patients with overactive bladder. Int Urogynecol J. 2013;24(9):1447–58.
Makhani A, Thake M, Gibson W. Mirabegron in the treatment of overactive bladder: safety and efficacy in the very elderly patient. Clin Interv Aging. 2020;15:575–81.
Lee YK, Kuo H-C. Safety and therapeutic efficacy of mirabegron 25 mg in older patients with overactive bladder and multiple comorbidities. Geriatr Gerontol Int. 2018;18(9):1330–3.
Sebastianelli A, Russo GI, Kaplan SA, McVary KT, Moncada I, Gravas S, et al. Systematic review and meta-analysis on the efficacy and tolerability of mirabegron for the treatment of storage lower urinary tract symptoms/overactive bladder: comparison with placebo and tolterodine. Int J Urol. 2018;25(3):196–205.
Lee KC, Rauscher F, Kaminesky J, Ryndin I, Xie L, Zhao Y, et al. Novel immediate/sustained-release formulation of acetaminophen-ibuprofen combination (Paxerol®) for severe nocturia associated with overactive bladder: A multi-center, randomized, double blinded, placebo-controlled, 4-arm trial. Neurourol Urodyn. 2019;38(2):740–8.
Wiśniewski K, Qi S, Kraus J, Ly B, Srinivasan K, Tariga H, et al. Discovery of potent, selective, and short-acting peptidic V 2 receptor agonists. J Med Chem. 2019;62(10):4991–5005.
Tsukamoto I, Koshio H, Akamatsu S, Kuramochi T, Saitoh C, Yatsu T, et al. Preparation of (4,4-difluoro-1,2,3,4-tetrahydro-5H-1-benzazepin-5-ylidene)acetamide derivatives as novel arginine vasopressin V2 receptor agonists. Bioorg Med Chem. 2008;16(21):9524–35.
Yea CM, Allan CE, Ashworth DM, Barnett J, Baxter AJ, Broadbridge JD, et al. New benzylureas as a novel series of potent, nonpeptidic vasopressin V2 receptor agonists. J Med Chem. 2008;51(24):8124–34.
Sanwa Kagaku Kenkyusho Co., Ltd. Trial of SK-1404 for Nocturia Due to Nocturnal Polyuria in Japanese Subjects. ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT03116191
Ferring Pharmaceuticals. A Trial to Investigate Efficacy, Safety and Tolerability of FE 201836 for Nocturia Due to Nocturnal Polyuria in Adults (DAWN). ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT03201419
Vantia Ltd. Efficacy Study of Fedovapagon for Nocturia in Men With Benign Prostatic Hyperplasia (BPH) (EQUINOC). ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT02637960
Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17(1):230.
Levy HB. Polypharmacy reduction strategies. Clin Geriatr Med. 2017;33(2):177–87.
Ballew SH, Chen Y, Daya NR, Godino JG, Windham BG, McAdams-DeMarco M, et al. Frailty, kidney function, and polypharmacy: the atherosclerosis risk in communities (ARIC) Study. Am J Kidney Dis. 2017;69(2):228–36.
Van Haarst EP, Heldeweg EA, Newling DW, Schlatmann TJ. The 24-h frequency-volume chart in adults reporting no voiding complaints: defining reference values and analysing variables. BJU Int. 2004;93(9):1257–61.
Huang Foen Chung JWNC, van Mastrigt R. Age and volume dependent normal frequency volume charts for healthy males. J Urol. 2009;182(1):210–4.
Denys M-A, Decalf V, Kumps C, Petrovic M, Goessaert A-S, Everaert K. Pathophysiology of nocturnal lower urinary tract symptoms in older patients with urinary incontinence. Int J Urol. 2017;24(11):808–15.
Bing MH, Moller LA, Jennum P, Mortensen S, Lose G. Pathophysiological aspects of nocturia in a Danish population of men and women age 60 to 80 years. J Urol. 2007;178(2):552–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were sought or provided for this work.
Conflicts of interest
Jeffrey P. Weiss declares Ferring Pharmaceuticals and the Institute for Bladder and Prostate Research as potential conflicts of interest. Corey S. Weinstein, Kerry A. Adler, and Dylan T. Wolff have no financial declarations to declare.
Ethics Approval
Not applicable to a review.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data
All data were sourced from academic journals, are listed in the references, and are available to the public.
Code Availability
Not applicable.
Author contributions
All listed authors meet the common criteria for authorship; each contributed significantly to the intellectual creation of this project, as well as the writing and editing of this manuscript. The author order has been approved by all authors, and the final manuscript has been read and approved by all authors.
Rights and permissions
About this article
Cite this article
Wolff, D.T., Adler, K.A., Weinstein, C.S. et al. Managing Nocturia in Frail Older Adults. Drugs Aging 38, 95–109 (2021). https://doi.org/10.1007/s40266-020-00815-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-020-00815-5