Abstract
Large registries and epidemiologic studies have demonstrated that elderly patients (≥ 75 years old) represent a growing proportion of the acute coronary syndrome (ACS) population and are exposed to a high risk of both bleeding and ischemic events. In this setting, most of the randomized trials excluded elderly patients while evaluating therapeutic strategies in ACS and only few trials specifically dedicated their design to the elderly population, leading to a paucity of data. Elderly patients are less likely to be treated with an invasive strategy or potent antithrombotic drugs compared with younger patients, while they are exposed to a greater risk of mortality. Nevertheless, the benefit of an invasive approach in ST-segment elevation myocardial infarction (STEMI) has been consistently demonstrated in non-dedicated large percutaneous coronary intervention randomized trials, regardless of the patient’s age. European clinical practice guidelines recommend that STEMI in elderly patients should not be treated differently than in younger patients. However, the therapeutic decision should be based on a combined evaluation of both (1) the patient’s frailty, including functional or cognitive impairment, and (2) the balance between bleeding and ischemic risks. This review outlines the evidence on the optimal reperfusion and antithrombotic strategies among STEMI elderly patients, suggesting a patient-centered approach to apprehend the balanced therapeutic decision in the very old patient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Despite frequent atypical ST-segment elevation myocardial infarction (STEMI) presentation and more comorbidities among elderly patients, age should not be a limit with respect to receiving the optimal recommended treatment. |
An invasive strategy should be the default strategy after assessment of the benefit/risk ratio including cognitive status prior to the decision. |
A multidisciplinary patient-centered approach should be proposed to guide the global management of elderly patients. |
1 Introduction
Large registries and epidemiologic studies have demonstrated that elderly patients (≥ 75 years old) represent a growing proportion of the acute coronary syndrome (ACS) population and are exposed to a high risk of both bleeding and ischemic events. In this setting, the optimal strategy is a conundrum, in which the benefit of an invasive strategy on ischemic outcomes should be balanced with the iatrogenic risk inherent to antithrombotic therapies but also to the percutaneous coronary intervention (PCI). Indeed, intensive antiplatelet therapies can be a double-edged sword that decreases the risk of ischemic events while exposing elderly or frail patients to an increased risk of major bleeding.
Only a few dedicated studies have evaluated the recommended treatment strategies among this high-risk population. The lack of evidence from interventional or antithrombotic randomized controlled trials because of the selection of low-bleeding-risk patients and the exclusion of elderly patients results in a low representation of elderly patients (10%) in clinical trials and a higher representation in registries (35%) [1,2,3].
As a result, physicians are conservative in their strategy, and they are less likely to treat elderly patients with the same intensity as younger patients, exposing them to a lower potential benefit of proven therapies despite higher inherent risk of mortality. European clinical practice guidelines recommend that elderly patients with ST-segment elevation myocardial infarction (STEMI) should not be treated differently than younger patients [4]. However, in daily practice, the therapeutic decision is usually based on a patient-centered approach combining evaluation of both (1) the patient’s frailty, including functional or cognitive impairment and end-of-life wishes, and (2) the balance between bleeding and ischemic risks.
This review summarizes the evidence on therapeutic strategies and underlines the unmet needs among elderly patients with STEMI.
2 A High-Risk Population Less Likely to Receive Efficient Therapies
Although life expectancy is increasing, elderly patients with ACS are still less likely to be treated with PCI and evidence-based secondary prevention medicines than younger patients [5, 6]. In the England and Wales national registry, including more than 150,000 patients, age > 85 years was associated with a lower rate of coronary reperfusion compared with patients aged < 65 years (55% vs 85%, respectively; odds ratio [OR] 0.22, 95% confidence interval [CI] 0.21–0.24; p < 0.001), whereas medical treatment alone was associated with increased mortality among patients over the age of 85 years (OR 1.36, 95% CI 1.27–1.47; p < 0.001) [7]. These results are consistent with an analysis of 8578 STEMI patients enrolled in the Can Rapid risk stratification of Unstable angina patients Suppress Adverse outcomes with Early implementation of the American College of Cardiology/American Heart Association guidelines (CRUSADE) registry, demonstrating a reverse association between age and the decision to attempt an invasive reperfusion (hazard ratio [HR] 1.13, 95% CI 1.09–1.16) [8].
However, it would be unfair to label ‘age’ as the main driver of whether revascularization is attempted or not. Many cofounders may explain the lower rate of PCI among elderly patients. First, the delay between elderly patients experiencing symptoms and reporting to an emergency room is usually increased [2, 9, 10]. This is mainly due to the frequent atypical presentation (dyspnea, nausea, abdominal pain) of elderly patients, setting back the diagnosis of STEMI. Since the benefit of PCI is inversely associated with the symptoms-to-balloon time, they are more likely to be treated medically and thus exposed to an increased risk of mortality [5, 6]. Second, the subjective assessment of frailty, including functional and cognitive status, may also influence the decision to conservatively treat elderly patients or to limit access to the intensive care unit. Frailty is diagnosed among approximately 25% of STEMI patients over the age of 85 years and is strongly associated with mortality [11]. It should be noted, however, that the lack of standardized criteria to define frailty remains a major issue with respect to adequately guiding the decision of revascularization [12]. Third, elderly patients have a higher risk of bleeding and a higher rate of chronic kidney disease compared with younger patients [13]. These factors are closely associated with two acute PCI complications: hematoma and contrast-induced nephropathy, both associated with an increased risk of mortality [14,15,16]. Finally, the greater prevalence of multivessel coronary disease, cardiogenic shock, and malignant ventricular arrhythmias among elderly patients, leading to a higher total number of events, explains also the greater absolute reduction in mortality among elderly and very elderly patients compared to younger primary PCI patients [17, 18]. Despite these cofounders, age is less associated with mortality than heart failure or diabetes at presentation. Thus, elderly patients, even after 90 years of age, treated with primary PCI have still a two- to threefold lower rate of in-hospital and 12-month mortality compared to those treated medically [19,20,21,22,23]. Moreover, although elderly patients carry an important and increasing medical cost burden, financial dimensions should not be considered in therapeutic management and emergency care, which should be provided independently of age and rather with regard to frailty in order to avoid futile interventions.
These findings advocate for a first-line invasive approach for elderly patients with STEMI.
3 Specificities of the Reperfusion Strategy in Elderly Patients
Over the last decades, primary PCI combined with evidence-based therapies and reduction of transfer times have dramatically improved the prognosis of STEMI patients, regardless of the age, including patients over the age of 85 years [24, 25].
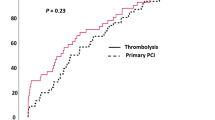
Few dedicated studies have compared PCI with fibrinolytic reperfusion strategy among elderly patients, a subgroup representing less than 10% of the population when not systematically excluded [26,27,28]. Of interest, primary PCI and fibrinolytic therapy among elderly patients were associated with consistent rates of major bleeding events (3–5%) and intracranial hemorrhages (about 0.5%), while the impact on ischemic events was controversial [28,29,30,31]. Only three small sample size randomized trials compared PCI with fibrinolytic therapy among elderly subjects: the Zwolle trial (n = 87) [32], the TRatamiento del Infarto Agudo de miocardio eN Ancianos (TRIANA) trial [33] (n = 266), and the unpublished PAMI Senior (Primary Angioplasty Versus Thrombolytic Therapy for Acute Myocardial Infarction in the Elderly) (n = 481) trial. The PAMI Senior and TRIANA trials were prematurely interrupted because of recruitment issues, illustrating the difficulties of conducting large trials in this population. In both trials, there was no difference between the two strategies on the primary endpoint, a composite of all-cause mortality, re-infarction, or disabling stroke at 30 days. However, a pooled analysis [33] demonstrated that primary PCI was associated with a reduced rate of the primary composite endpoint compared with fibrinolytic therapy (14.9% vs 21.5%, respectively; OR 0.64, 95% CI 0.45–0.91; p = 0.013). Despite limited data, these analyses suggest a benefit of primary PCI among elderly patients, supporting an invasive approach as a first-line therapy in STEMI, regardless of age [4]. Following this recommendation, the proportion of older patients undergoing PCI increased from 30 to 80–90% over the last 15 years [21, 34, 35]. Moreover, it was followed by a reduction of in-hospital and long-term mortality [21, 36].
Finally, the transradial approach should be the preferred approach among elderly patients, since it is associated with a reduction in mortality and bleeding events compared with the transfemoral approach. This approach is widely feasible in elderly patients, as demonstrated in 95% of the patients prospectively enrolled in an observational study [37]. Other technical aspects of reperfusions strategies should be similar, regardless of age, such as the use of drug-eluting stents (DES) in the first line [4].
Among elderly patients, bare-metal stents (BMS) were historically implanted to reduce the duration of dual antiplatelet therapy, decreasing the risk of bleeding. Nevertheless, the latest generation of DES allows a similar duration of dual antiplatelet therapy. The Short Duration of Dual antiplatElet Therapy With SyNergy II Stent in Patients Older Than 75 Years Undergoing Percutaneous Coronary Revascularization (SENIOR) trial randomized 1200 patients aged ≥ 75 years requiring PCI to either BMS or DES in stable angina or ACS settings. The primary composite endpoint (all-cause mortality, myocardial infarction (MI), stroke, or ischemia-driven target lesion revascularization) occurred less frequently in patients treated with DES than BMS [12% vs 16%; Relative Risk (RR) 0.71, 95% CI 0.52–0.94; p = 0.02]. This study demonstrates that DES implantation among all-comer elderly patients, regardless of their clinical presentation, is safe and is associated with fewer ischemic events, with a benefit mainly related to a reduction in repeated revascularizations [38].
4 Timing and Dosage of Fibrinolytic Therapy Among Elderly Patients
When primary PCI cannot be performed within 120 min, fibrinolytic therapy is the recommended reperfusion strategy within 12 h of symptom onset, regardless of age [4]. However, elderly patients are more likely to have both absolute (e.g., uncontrolled hypertension, recent stroke, history of intracranial hemorrhage) and relative (e.g., prior stroke, dementia, chronic anticoagulation) contraindications to fibrinolytic therapy. In addition, the intracranial hemorrhage rate increases from 0.75% in patients aged < 70 years to 2% among patients aged > 70 years [39]. Therefore, the evaluation of the benefit/risk ratio is critical to guide the decision regarding fibrinolytic administration.
The recent multicentric randomized Strategic Reperfusion Early after Myocardial Infarction (STREAM) trial demonstrated that half-dose tenecteplase yields a favorable risk/benefit ratio among elderly patients [26]. The study protocol was amended to halve the dose of tenecteplase because of an excess of intracranial hemorrhage in patients older than 75 years with the standard dose. After amendment, the composite primary endpoint (death, shock, congestive heart failure or reinfarction) at 30 days occurred among 24.7% of subjects in the fibrinolysis group and 28.4% in the primary PCI group, while major bleedings occurred, respectively, in 14.0% and 11.2% (no direct statistical comparison available), without any intracranial hemorrhage [40]. The ongoing STREAM2 trial (NCT02777580) should provide additional data, comparing early half-dose tenecteplase fibrinolytic therapy with primary PCI among patients ≥ 70 years.
5 Should Antiplatelet Therapy be Different in Elderly Patients?
Dual antiplatelet therapy with aspirin plus a P2Y12 inhibitor is the cornerstone treatment of ACS patients undergoing PCI. In the STEMI setting, early administration of P2Y12 inhibition, before coronary angiogram, is not still debated and is recommended in international guidelines [4]. Although no trial has yet specifically included elderly patients in this setting, a recent meta-analysis, including 9648 patients from seven randomized clinical trials, confirmed that early P2Y12 inhibition is associated with a reduction in major cardiac adverse events without an increase of major bleeding in comparison to a delayed treatment on arrival in the catheterization laboratory [41].
Prasugrel and ticagrelor demonstrated superiority in reducing the ischemic endpoints compared to clopidogrel in large randomized trials [42, 43] but the benefit/risk ratio of intense platelet inhibition in elderly patients remains debated, and clopidogrel is still widely used [44]. However, international guidelines recommend ticagrelor as first-line therapy regardless of age [4]. There was, indeed, no interaction between ticagrelor effect and age on the reduction of all-cause and cardiovascular mortality in the pivotal PLATelet inhibition and patient Outcomes (PLATO) trial. There was also no effect modification of age on the occurrence of major bleeding [45]. In STEMI, the use of ticagrelor has not been specifically evaluated among elderly patients. However, patients ≥ 75 years of age represented one sixth of the subjects randomized in the A 30 Day Study to Evaluate Efficacy and Safety of Pre-hospital vs In-hospital Initiation of Ticagrelor Therapy in STEMI Patients Planned for Percutaneous Coronary Intervention (ATLANTIC) trial [46, 47] that evaluated the optimal timing of ticagrelor administration. There was no interaction between time of ticagrelor administration (pre-hospital vs in cathlab) and age on ischemic or bleeding outcomes, suggesting the safety of the ticagrelor loading dose in STEMI elderly patients.
In contrast, administration of prasugrel 10 mg is not recommended among patients ≥ 75 years of age, since it was not associated with improved net clinical benefit [48]. Even if a reduced dose (5 mg) is recommended in elderly patients [4, 49], the question regarding the efficacy and safety of this dose in comparison to clopidogrel remains debated. The Elderly ACS2 trial [50] comparing prasugrel 5 mg with clopidogrel 75 mg among ACS patients ≥ 75 years of age undergoing PCI was prematurely stopped. However, 1443 patients were enrolled, including 40% of STEMI patients with a median follow-up of 12 months. It demonstrated a similar rate of the primary endpoint (mortality, MI, disabling stroke, and rehospitalization for cardiovascular causes or bleeding) between the two treatment arms (17% vs 16.6%; HR 1.01, 95% CI 0.78–1.30; p = 0.95). Reduced-dose prasugrel was associated with a numerically lower rate of definite/probable stent thrombosis (0.7% vs 1.9%; OR 0.36, 95% CI 0.13–1.00; p = 0.06) and a numerically higher rate of bleeding (4.1% vs 2.7%; OR 1.52, 95% CI 0.85–3.16; p = 0.18) compared with clopidogrel. Thus, there was no net clinical benefit of prasugrel compared with clopidogrel in elderly patients.
A systematic review comparing potent P2Y12 inhibitors with clopidogrel among 7860 elderly and 37,857 non-elderly ACS patients demonstrated that a similar risk of bleeding events between elderly (RR 1.19 [0.95–1.49]) and nonelderly patients (RR 1.16 [0.95–1.41]. Since the effect of novel P2Y12 inhibitors is consistent among elderly versus younger patients, potent antiplatelet therapy should not be discontinued because of advanced age [51] (Fig. 1).

(adapted from Tarantini et al. meta-analysis [51]). The meta-analysis was performed from six studies with a total of 7394 elderly patients (3657 patients treated with potent P2Y12 inhibitors, 3737 patients treated with clopidogrel) for efficacy endpoints and five studies with a total of 7436 elderly patients (3497 patients treated with potent P2Y12 inhibitors, 3939 patients treated with clopidogrel) for safety endpoints. Potent P2Y12 inhibitors included ticagrelor, prasugrel 5 mg and prasugrel 10 mg. CI confidence interval, CV cardiovascular, MI myocardial infarction
Efficacy and safety of potent P2Y12 inhibitors in elderly and non-elderly patients
Age is not a key criterion to evaluate duration of dual antiplatelet therapy after STEMI, which is usually recommended within 12 months [4]. In case of additional bleeding risk factors such as chronic kidney disease, low body weight, concomitant oral anticoagulant, or prior bleeding events, dual antiplatelet therapy should be reduced to a minimal duration of 1 month. Of importance, routine use of proton-pump inhibitors is systematically recommended to reduce the risk of gastrointestinal bleeding [52].
Cangrelor is the only available intravenous P2Y12 inhibitor. The CHAMPION PHOENIX trial demonstrated a reduction in the prevalence of ischemic events in patients undergoing PCI and treated with cangrelor compared with clopidogrel [53]. The population of patients aged ≥ 75 years represented only 18% out of the 11,145 included subjects. A sub-analysis regarding the impact of age on the clinical outcomes reported that the effects of cangrelor were consistent both in patients aged < 75 years and those ≥ 75 years (interaction p = 0.55). There was no significant difference in the occurrence of GUSTO severe bleeding with cangrelor or clopidogrel in patients aged ≥ 75 years (0.3% vs 0.5%; OR 0.58, 95% CI 0.14–2.44; p = 0.45). The net clinical endpoint (death, MI, ischemia-driven revascularization, stent thrombosis, or GUSTO severe bleeding) was reduced in patients treated by cangrelor irrespective of age (≥ 75 years: OR 0.71, 95% CI 0.50–1.01; and < 75 years: OR 0.82, 95% CI 0.68–0.99; interaction p = 0.48) [54]. As a result, cangrelor may be considered at the time of PCI in ACS elderly patients not pre-treated with oral P2Y12 inhibitors or in those who are considered unable to absorb oral agents [4].
Finally, in the acute phase, despite the absence of specific data regarding elderly patients, there is no evidence for glycoprotein (GP) IIb/IIIa inhibitors pre-hospital administration, and this should be considered only for bailout if there is evidence of no-reflow or a thrombotic complication, irrespective of age [4].
Recommended antithrombotic drugs and doses in elderly patients are summarized in Table 1.
6 Added Value of Platelet Function Testing in Elderly
Platelet function testing offers the possibility to adjust antithrombotic treatment to a prespecified target. Several pharmacodynamic studies demonstrated that high on-treatment platelet reactivity is more frequent in elderly patients, exposing them to an increased risk of ischemic events, particularly for patients treated with clopidogrel [55]. In contrast, elderly patients receiving more potent P2Y12 inhibitors have a higher rate of low on-treatment platelet reactivity, increasing the risk of bleeding [2, 56].
The Assessment of a Normal Versus Tailored Dose of Prasugrel After Stenting in Patients Aged > 75 Years to Reduce the Composite of Bleeding, Stent Thrombosis and Ischemic Complications (ANTARCTIC) trial [57] randomized patients aged ≥ 75 years to oral prasugrel 5 mg daily, with dose or drug adjustment in the case of inadequate response, or oral prasugrel 5 mg daily with no monitoring. This individualized approach failed to demonstrate a benefit of platelet function testing on the clinical endpoint among elderly ACS patients. The pre-specified analysis of the randomized TROPICAL ACS trial [58, 59] aimed to assess the impact of age on clinical outcomes following guided de-escalation of antiplatelet treatment in ACS patients. Patients were randomly assigned to either standard treatment with prasugrel for 12 months or to a guided de-escalation maintenance therapy with clopidogrel or prasugrel. In comparison to that in younger patients, the absolute risk of the composite of cardiovascular death, MI, stroke, or bleeding ≥ Bleeding Academic Research Consortium (BARC) grade 2 was higher in patients aged > 70 years, without significant difference between the two strategies (HR 1.17, 95% CI 0.69–2.01; p = 0.56). Therefore, routine use of platelet function testing in elderly patients is not recommended to adjust antithrombotic treatment [60].
7 Medical Treatment Features in Elderly
During the acute phase, age, by itself, should not limit the administration of the recommended drugs. However, morphine should be carefully used, to reduce the risk of confusion. Of importance, education on the benefit of statins is essential to improve patient adherence. Indeed, while STEMI patients often achieve better medical adherence than non-ST-segment myocardial infarction (NSTEMI) patients (60% vs 40%), a progressive rate of discontinuation of evidence-based medicine is usually observed among elderly patients, including for antithrombotic drugs and statins [61]. Finally, age is usually associated with longer hospitalization duration, that however, should be individualized and shortened following PCI, based on the patient’s cardiac risk, comorbidities, functional status and social support [62, 63].
8 Conclusion
Despite frequent atypical symptoms, electrocardiogram findings and delayed presentation, the diagnosis of STEMI should always be suspected among elderly patients. When it is confirmed, they should receive the same recommended treatment as younger patients. An invasive strategy should be the default strategy, although it is essential to assess functional and cognitive status prior to the decision. Specific strategies to reduce the risk of bleeding should be preferred such as a radial approach and adjusted dose of antithrombotic therapies. (See Fig. 2 for an overview of the management of STEMI in elderly patients.) Finally, a multidisciplinary patient-centered approach, designed by both cardiologist and gerontologist, should be proposed to guide the global management of the frailest patients.
References
Lee PY, Alexander KP, Hammill BG, Pasquali SK, Peterson ED. Representation of elderly persons and women in published randomized trials of acute coronary syndromes. JAMA. 2001;286(6):708–13.
Alexander KP, Newby LK, Armstrong PW, et al. Acute coronary care in the elderly, part II: ST-segment-elevation myocardial infarction: a scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology: in collaboration with the Society of Geriatric Cardiology. Circulation. 2007;115(19):2570–89.
Hordijk-Trion M, Lenzen M, Wijns W, et al. Patients enrolled in coronary intervention trials are not representative of patients in clinical practice: results from the Euro Heart Survey on Coronary Revascularization. Eur Heart J. 2006;27(6):671–8.
Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–77.
Toleva O, Ibrahim Q, Brass N, Sookram S, Welsh R. Treatment choices in elderly patients with ST: elevation myocardial infarction-insights from the Vital Heart Response registry. Open Heart. 2015;2(1):e000235. https://doi.org/10.1136/openhrt-2014-000235.
Avezum A, Makdisse M, Spencer F, et al. Impact of age on management and outcome of acute coronary syndrome: observations from the Global Registry of Acute Coronary Events (GRACE). Am Heart J. 2005;149(1):67–73.
Zaman MJ, Stirling S, Shepstone L, et al. The association between older age and receipt of care and outcomes in patients with acute coronary syndromes: a cohort study of the Myocardial Ischaemia National Audit Project (MINAP). Eur Heart J. 2014;35(23):1551–8.
Gharacholou SM, Alexander KP, Chen AY, et al. Implications and reasons for the lack of use of reperfusion therapy in patients with ST-segment elevation myocardial infarction: findings from the CRUSADE initiative. Am Heart J. 2010;159(5):757–63.
Assali AR, Moustapha A, Sdringola S, et al. The dilemma of success: percutaneous coronary interventions in patients > or = 75 years of age-successful but associated with higher vascular complications and cardiac mortality. Catheter Cardiovasc Interv. 2003;59(2):195–9.
Bagur R, Bertrand OF, Rodés-Cabau J, et al. Comparison of outcomes in patients > or = 70 years versus < 70 years after transradial coronary stenting with maximal antiplatelet therapy for acute coronary syndrome. Am J Cardiol. 2009;104(5):624–9.
Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol. 2001;56(3):M146–56.
Afilalo J, Alexander KP, Mack MJ, et al. Frailty assessment in the cardiovascular care of older adults. J Am Coll Cardiol. 2014;63(8):747–62.
Jomaa W, Hamdi S, Ben Ali I, et al. Risk profile and in-hospital prognosis in elderly patients presenting for acute ST-elevation myocardial infarction in the Tunisian context. Indian Heart J. 2016;68(6):760–5.
Alexander KP, Chen AY, Roe MT, et al. Excess dosing of antiplatelet and antithrombin agents in the treatment of non-ST-segment elevation acute coronary syndromes. JAMA. 2005;294(24):3108–16.
Mehran R, Pocock SJ, Nikolsky E, et al. A risk score to predict bleeding in patients with acute coronary syndromes. J Am Coll Cardiol. 2010;55(23):2556–66.
Silvain J, Nguyen LS, Spagnoli V, et al. Contrast-induced acute kidney injury and mortality in ST elevation myocardial infarction treated with primary percutaneous coronary intervention. Heart. 2018;104(9):767–72.
Malkin CJ, Prakash R, Chew DP. The impact of increased age on outcome from a strategy of early invasive management and revascularisation in patients with acute coronary syndromes: retrospective analysis study from the ACACIA registry. BMJ Open. 2012;2(1):e000540. https://doi.org/10.1136/bmjopen-2011-000540.
Mehta RH, Sadiq I, Goldberg RJ, et al. Effectiveness of primary percutaneous coronary intervention compared with that of thrombolytic therapy in elderly patients with acute myocardial infarction. Am Heart J. 2004;147(2):253–9.
Helft G, Georges J-L, Mouranche X, et al. Outcomes of primary percutaneous coronary interventions in nonagenarians with acute myocardial infarction. Int J Cardiol. 2015;192:24–9.
de Boer SPM, Westerhout CM, Simes RJ, et al. Mortality and morbidity reduction by primary percutaneous coronary intervention is independent of the patient’s age. JACC Cardiovasc Interv. 2010;3(3):324–31.
Khera S, Kolte D, Palaniswamy C, et al. ST-elevation myocardial infarction in the elderly—temporal trends in incidence, utilization of percutaneous coronary intervention and outcomes in the United States. Int J Cardiol. 2013;168(4):3683–90.
Mandawat A, Mandawat A, Mandawat MK. Percutaneous coronary intervention after ST-segment elevation myocardial infarction in nonagenarians: use rates and in-hospital mortality. J Am Coll Cardiol. 2013;61(11):1207–8.
Yudi MB, Jones N, Fernando D, et al. Management of patients aged ≥ 85 years with ST-elevation myocardial infarction. Am J Cardiol. 2016;118(1):44–8.
Devlin G, Gore JM, Elliott J, et al. Management and 6-month outcomes in elderly and very elderly patients with high-risk non-ST-elevation acute coronary syndromes: the Global Registry of Acute Coronary Events. Eur Heart J. 2008;29(10):1275–82.
Skolnick AH, Alexander KP, Chen AY, et al. Characteristics, management, and outcomes of 5,557 patients age > or = 90 years with acute coronary syndromes: results from the CRUSADE initiative. J Am Coll Cardiol. 2007;49(17):1790–7.
Armstrong PW, Gershlick AH, Goldstein P, et al. Fibrinolysis or primary PCI in ST-segment elevation myocardial infarction. N Engl J Med. 2013;368(15):1379–87.
Bonnefoy E, Lapostolle F, Leizorovicz A, et al. Primary angioplasty versus prehospital fibrinolysis in acute myocardial infarction: a randomised study. Lancet. 2002;360(9336):825–9.
Peiyuan H, Jingang Y, Haiyan X, et al. The comparison of the outcomes between primary PCI, fibrinolysis, and no reperfusion in patients ≥ 75 years old with ST-segment elevation myocardial infarction: results from the Chinese Acute Myocardial Infarction (CAMI) Registry. PLoS ONE. 2016;11(11):e0165672. https://doi.org/10.1371/journal.pone.0165672.
Thiemann DR, Coresh J, Schulman SP, Gerstenblith G, Oetgen WJ, Powe NR. Lack of benefit for intravenous thrombolysis in patients with myocardial infarction who are older than 75 years. Circulation. 2000;101(19):2239–46.
Mehta RH, Granger CB, Alexander KP, Bossone E, White HD, Sketch MH. Reperfusion strategies for acute myocardial infarction in the elderly: benefits and risks. J Am Coll Cardiol. 2005;45(4):471–8.
Berger AK, Schulman KA, Gersh BJ, et al. Primary coronary angioplasty vs thrombolysis for the management of acute myocardial infarction in elderly patients. JAMA. 1999;282(4):341–8.
de Boer M-J, Ottervanger J-P, van ’t Hof AWJ, et al. Reperfusion therapy in elderly patients with acute myocardial infarction: a randomized comparison of primary angioplasty and thrombolytic therapy. J Am Coll Cardiol. 2002;39(11):1723–8.
Bueno H, Betriu A, Heras M, et al. Primary angioplasty vs. fibrinolysis in very old patients with acute myocardial infarction: TRIANA (TRatamiento del Infarto Agudo de miocardio eN Ancianos) randomized trial and pooled analysis with previous studies. Eur Heart J. 2011;32(1):51.
Tisminetzky M, Erskine N, Chen H-Y, et al. Changing trends in, and characteristics associated with, not undergoing cardiac catheterization in elderly adults hospitalized with ST-segment elevation acute myocardial infarction. J Am Geriatr Soc. 2015;63(5):925–31.
Johnman C, Oldroyd KG, Mackay DF, et al. Percutaneous coronary intervention in the elderly: changes in case-mix and periprocedural outcomes in 31,758 patients treated between 2000 and 2007. Circ Cardiovasc Interv. 2010;3(4):341–5.
Fox KAA, Steg PG, Eagle KA, et al. Decline in rates of death and heart failure in acute coronary syndromes, 1999–2006. JAMA. 2007;297(17):1892–900.
Rodriguez-Leor O, Fernandez-Nofrerias E, Carrillo X, et al. Results of primary percutaneous coronary intervention in patients ≥ 75 years treated by the transradial approach. Am J Cardiol. 2014;113(3):452–6.
Varenne O, Cook S, Sideris G, et al. Drug-eluting stents in elderly patients with coronary artery disease (SENIOR): a randomised single-blind trial. Lancet. 2018;391(10115):41–50.
Van De Werf F, Adgey J, Ardissino D, et al. Single-bolus tenecteplase compared with front-loaded alteplase in acute myocardial infarction: the ASSENT-2 double-blind randomised trial. Lancet. 1999;354(9180):716–22.
Armstrong PW, Zheng Y, Westerhout CM, et al. Reduced dose tenecteplase and outcomes in elderly ST-segment elevation myocardial infarction patients: insights from the STrategic Reperfusion Early After Myocardial infarction trial. Am Heart J. 2015;169(6):890.e1–898.e1.
Bellemain-Appaix A, Bégué C, Bhatt DL, et al. The efficacy of early versus delayed P2Y12 inhibition in percutaneous coronary intervention for ST-elevation myocardial infarction: a systematic review and meta-analysis. EuroIntervention. 2018;14(1):78–85.
Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357(20):2001–15.
Wallentin L, Becker RC, Budaj A, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045–57.
Danchin N, Lettino M, Zeymer U, et al. Use, patient selection and outcomes of P2Y12 receptor inhibitor treatment in patients with STEMI based on contemporary European registries. Eur Heart J Cardiovasc Pharmacother. 2016;2(3):152–67.
Husted S, James S, Becker RC, et al. Ticagrelor versus clopidogrel in elderly patients with acute coronary syndromes: a substudy from the prospective randomized PLATelet inhibition and patient Outcomes (PLATO) trial. Circ Cardiovasc Qual Outcomes. 2012;5(5):680–8.
Collet J-P, Kerneis M, Lattuca B, et al. The effect of prehospital P2Y12 receptor inhibition in primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: the ATLANTIC-Elderly analysis. EuroIntervention. 2018;14(7):789–97.
Montalescot G, van ’t Hof AW, Lapostolle F, et al. Prehospital ticagrelor in ST-segment elevation myocardial infarction. N Engl J Med. 2014;371(11):1016–27.
Wiviott SD, Desai N, Murphy SA, et al. Efficacy and safety of intensive antiplatelet therapy with prasugrel from TRITON-TIMI 38 in a core clinical cohort defined by worldwide regulatory agencies. Am J Cardiol. 2011;108(7):905–11.
Roe MT, Armstrong PW, Fox KAA, et al. Prasugrel versus clopidogrel for acute coronary syndromes without revascularization. N Engl J Med. 2012;367(14):1297–309.
Savonitto S, Ferri LA, Piatti L, et al. A comparison of reduced-dose prasugrel and standard-dose clopidogrel in elderly patients with acute coronary syndromes undergoing early percutaneous revascularization. Circulation. 2018;137(23):2435–45.
Tarantini G, Ueshima D, D’Amico G, et al. Efficacy and safety of potent platelet P2Y12 receptor inhibitors in elderly versus nonelderly patients with acute coronary syndrome: a systematic review and meta-analysis. Am Heart J. 2018;195:78–85.
Agewall S, Cattaneo M, Collet JP, et al. Expert position paper on the use of proton pump inhibitors in patients with cardiovascular disease and antithrombotic therapy. Eur Heart J. 2013;34(23):1708–13 (1713a–1713b).
Bhatt DL, Stone GW, Mahaffey KW, et al. Effect of platelet inhibition with cangrelor during PCI on ischemic events. N Engl J Med. 2013;368(14):1303–13.
Cavender MA, Bhatt DL, Stone GW, et al. Cangrelor in older patients undergoing percutaneous coronary intervention: findings from CHAMPION PHOENIX. Circ Cardiovasc Interv. 2017;10(8):e005257.
Silvain J, Cayla G, Hulot J-S, et al. High on-thienopyridine platelet reactivity in elderly coronary patients: the SENIOR-PLATELET study. Eur Heart J. 2012;33(10):1241–9.
Cuisset T, Cayla G, Frere C, et al. Predictive value of post-treatment platelet reactivity for occurrence of post-discharge bleeding after non-ST elevation acute coronary syndrome. Shifting from antiplatelet resistance to bleeding risk assessment? EuroIntervention. 2009;5(3):325–9.
Cayla G, Cuisset T, Silvain J, et al. Platelet function monitoring to adjust antiplatelet therapy in elderly patients stented for an acute coronary syndrome (ANTARCTIC): an open-label, blinded-endpoint, randomised controlled superiority trial. Lancet. 2016;388(10055):2015–22.
Sibbing D, Aradi D, Jacobshagen C, et al. Guided de-escalation of antiplatelet treatment in patients with acute coronary syndrome undergoing percutaneous coronary intervention (TROPICAL-ACS): a randomised, open-label, multicentre trial. Lancet. 2017;390(10104):1747–57.
Sibbing D, Gross L, Trenk D, et al. Age and outcomes following guided de-escalation of antiplatelet treatment in acute coronary syndrome patients undergoing percutaneous coronary intervention: results from the randomized TROPICAL-ACS trial. Eur Heart J. 2018;39(29):2749–58.
Valgimigli M, Bueno H, Byrne RA, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: the task force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2018;39(3):213–60.
Eindhoven DC, Hilt AD, Zwaan TC, Schalij MJ, Borleffs CJW. Age and gender differences in medical adherence after myocardial infarction: women do not receive optimal treatment—the Netherlands claims database. Eur J Prev Cardiol. 2018;25(2):181–9.
Melberg T, Jørgensen M, Ørn S, Solli T, Edland U, Dickstein K. Safety and health status following early discharge in patients with acute myocardial infarction treated with primary PCI: a randomized trial. Eur J Prev Cardiol. 2015;22(11):1427–34.
Azzalini L, Solé E, Sans J, et al. Feasibility and safety of an early discharge strategy after low-risk acute myocardial infarction treated with primary percutaneous coronary intervention: the EDAMI pilot trial. Cardiology. 2015;130(2):120–9.
Andreotti F, Rocca B, Husted S, et al. Antithrombotic therapy in the elderly: expert position paper of the European Society of Cardiology Working Group on Thrombosis. Eur Heart J. 2015;36(46):3238–49.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used in the preparation of this article.
Conflict of interest
B. Lattuca has received research grants from Biotronik, Daiichi-Sankyo and Fédération Française de Cardiologie; consultant fees from Daiichi-Sankyo and Eli Lilly; and lecture fees from AstraZeneca and Novartis. M. Kerneis has received research grants from Sanofi, Institut Servier and Fédération Française de Cardiologie; consultant fees from Bayer and AstraZeneca. M. Zeitouni has received research grants from Institut Servier and Federation Française de Cardiologie. G. Cayla has received consulting and lecture fees from Abbott Vascular, AstraZeneca, Bayer, BMS, Boehringer-Ingelheim, Boston Scientific, CLS Behring, Daiichi-Sankyo, Eli Lilly, Iroko Cardio, Novartis and Pfizer. P. Guedeney reports no financial relationships or conflicts of interest. J.P. Collet has received research grants or honorarium from AstraZeneca, Bayer, Bristol-Myers Squibb, Daiichi-Sankyo, Eli-Lilly, Fédération Française de Cardiologie, Lead-Up, Medtronic, MSD, Sanofi-Aventis, and WebMD. G. Montalescot has received research grants or honorarium from Abbott, Amgen, Actelion, AstraZeneca, Bayer, Boehringer-Ingelheim, Boston-Scientific, Bristol-Myers Squibb, Beth Israel Deaconess Medical, Brigham Women’s Hospital, Cardiovascular Research Foundation, Daiichi-Sankyo, Idorsia, Lilly, Europa, Elsevier, Fédération Française de Cardiologie, ICAN, Medtronic, Journal of the American College of Cardiology, Lead-Up, Menarini, MSD, Novo-Nordisk, Pfizer, Sanofi, Servier, the Mount Sinai School, TIMI Study Group, and WebMD. J. Silvain has received consulting fees from AstraZeneca, Bayer, Boehringer-Ingelheim, Gilead Science and Sanofi-Aventis; speaker honorariums from AstraZeneca, Amgen, Bayer, Algorythm and Sanofi-Aventis; and travel support from Amgen, AstraZeneca, Bayer and Bristol-Myer Squibb.
Rights and permissions
About this article
Cite this article
Lattuca, B., Kerneis, M., Zeitouni, M. et al. Elderly Patients with ST-Segment Elevation Myocardial Infarction: A Patient-Centered Approach. Drugs Aging 36, 531–539 (2019). https://doi.org/10.1007/s40266-019-00663-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-019-00663-y