Abstract
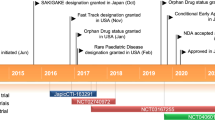
Golodirsen (Vyondys 53™), an antisense oligonucleotide of the phophorodiamidate morpholino oligomer (PMO) subclass designed to induce exon 53 skipping, has been developed by Sarepta Therapeutics for the treatment of Duchenne muscular dystrophy (DMD). In December 2019, intravenous golodirsen received its first global approval in the USA for the treatment of DMD in patients with a confirmed mutation of the DMD gene that is amenable to exon 53 skipping, based on positive results from a phase I/II clinical trial. Golodirsen is in phase III clinical development for the treatment of DMD worldwide. This article summarizes the milestones in the development of golodirsen leading to this first approval for DMD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
An antisense oligonucleotide of the PMO subclass designed to induce exon 53 skipping being developed by Sarepta Therapeutics for the treatment of DMD |
Received its first approval on 12 December 2019 in the USA |
Approved for use in DMD patients with a confirmed mutation of the DMD gene that is amenable to exon 53 skipping |
1 Introduction
Dunchenne muscular dystrophy (DMD), a rare, lethal, X-linked recessive genetic disorder, is caused by mutations in the dystrophin-encoding DMD gene and primarily affects males, with a prevalence of ≈ 1 in 5000 newborn boys [1]. DMD is characterized by progressive muscle deterioration that eventually leads to loss of ambulation in most affected patients by ≈ 12 years of age. Most of DMD patients have a deletion mutation of one or more exons (typically in exons 43–55) [1], which disrupt the open-reading frame and prevent the translation of dystrophin, an essential structural protein for muscle fibre integrity [1, 2]. At present, there is no cure for DMD and the goal of treatment is to delay disease progression and improve quality of life. A potential therapeutic approach for DMD is exon-skipping therapy, which aims to restore the function or expression of dystrophin by using antisense oligonucleotides to ‘skip-over’ the mutant exons from premessenger RNA (mRNA) reading frame, thereby producing truncated but functional dystrophin [1, 2].
Golodirsen (Vyondys 53™), an antisense oligonucleotide of the phosphorodiamidate morpholino oligomer (PMO) subclass designed to induce exon 53 skipping, has been developed by Sarepta Therapeutics for the treatment of DMD [3]. Following a New Drug Application (NDA) for golodirsen, the US FDA initially issued a Complete Response Letter in August 2019, raising concerns over the risk of infections related to intravenous infusion ports and renal toxicity observed in pre-clinical studies at doses that were 10-fold higher than therapeutic doses [4]. Subsequently, Sarepta Therapeutics made a formal dispute resolution request and after the review, the US FDA granted the company’s appeal [3]. On 12 December 2019, golodirsen received the US FDA accelerated approval for the treatment of DMD in patients with a confirmed mutation of the DMD gene amenable to exon 53 skipping, which represents ≈ 8% of all DMD patients [5, 6]. The approval was based on an increase in dystrophin production in skeletal muscle observed in golodirsen-treated patients; continued approval for this indication is contingent upon the verification of its clinical benefit in confirmatory trials [5, 6]. Golodirsen has been granted orphan drug designation and rare paediatric disease designation in the USA for DMD.

In the USA, golodirsen is available as single-dose vials containing 100 mg/2 mL golodirsen. The approved dosage of intravenous golodirsen is 30 mg/kg infused over 35–60 min once weekly [6]. Based on animal data, golodirsen may cause renal toxicity and therefore renal function should be monitored in patients taking golodirsen. Measurement of glomerular filtration rate (GFR) prior to treatment initiation and monitoring for renal toxicity during the treatment is recommended. Of note, creatinine may not be a reliable measure of renal function in DMD patients [6].
Golodirsen is in phase III clinical development for the treatment of DMD worldwide.
1.1 Company Agreements
In November 2012, Sarepta Therapeutics entered into a collaboration with University College of London, the Dubowitz Neuromuscular Centre and the Institute of Child Health to develop golodirsen for the treatment of DMD [7]. In April 2013, Sarepta Therapeutics and University of Western Australia (UWA) entered into an exclusive worldwide license agreement under which the former was granted the rights to access UWA’s extensive patent portfolio in DMD to support the development of new exon-skipping drug candidates, including golodirsen, based on its proprietary PMO technology [8]. Under the terms of the agreement, UWA is entitled to receive an upfront payment up to $7.1 million, as well as development milestone payments and a low single-digit royalty on net sales [8]. In June 2016, Sarepta Therapeutics entered into the first amendment of the license agreement with UWA under which the latter waived rights to certain royalties and amended the timing of certain other royalty payments [9]. As per the amended agreement, Sarepta remained obligated to make up to $20 million in payments to UWA upon achievement of certain sales milestones [9].
1.2 Patent Information
The US Patent and Trademark Office (USPTO) granted composition of matter and method of use patent protection for golodirsen in the USA until 2021–2025. The drug is also protected by a European patent in the EU.
In September 2016, the Patent Trial and Appeal Board (PTAB) of the USPTO issued two favorable decisions for Sarepta Therapeutics, refusing all the exon 51 and exon 53 composition of matter patent interferences claims made by BioMarin Pharmaceuticals, which if granted could have formed a basis for a claim of infringement against eteplirsen and golodirsen [10]. In July 2017, Sarepta Therapeutics and BioMarin Pharmaceutical executed a settlement agreement, resolving the ongoing worldwide patent proceeding regarding the use of eteplirsen and future exon-skipping products for the treatment. Under the terms of the license and settlement agreements, Sarepta will make a one-time payment of $35 million to BioMarin and additional certain regulatory and commercial milestone payments for exon 51, 45, 53 and possibly future exon-skipping products [11].
2 Scientific Summary
2.1 Pharmacodynamics
Golodirsen is an antisense oligonucleotide of the PMO subclass that binds and skips exon 53 during dystrophin mRNA processing, allowing the production of an internally truncated but functional dystrophin in patients with DMD mutations that are amenable to exon 53 skipping [6, 12]. In the pivotal 2-part, multicentre phase I/II trial (NCT02310906), all of golodirsen-treated patients demonstrated a significant (p < 0.001) increase in exon 53 skipping over baseline levels at week 48, which were confirmed by reverse transcription polymerase chain reaction (RT-PCR) [6, 12].
2.2 Pharmacokinetics
In DMD patients, golodirsen exposure increased in a dose-proportional manner after multiple weekly intravenous administrations of golodirsen (4–30 mg/kg/week); minimal accumulation was seen with once-weekly dosing [6]. The inter-subject variability of the peak plasma concentration (Cmax) and the area under the concentration–time curve of golodirsen ranged from 38–72% and 34–44%, respectively. Following intravenous infusion of golodirsen 30 mg/kg, the mean steady-state volume of distribution was 668 mL/kg and plasma protein binding of golodirsen was 33–39%, which was concentration-independent. Golodirsen appeared to be metabolically stable and no metabolites were detected in plasma or urine. Golodirsen was mostly excreted unchanged in the urine, with an elimination half-life of 3.4 h. After intravenous administration of golodirsen 30 mg/kg, the plasma clearance of golodirsen was 346 mL/h/kg [6].
A reduced renal clearance of golodirsen was seen in non-DMD adults with renal impairment (based on estimated GFR) [6]. However, due to the effect of reduced skeletal muscle mass on creatinine measurements, no specific dosage adjustment of golodirsen can be made for DMD patients with renal impairment based on estimated GFR. DMD patients with known renal impairment should be closely monitored during golodirsen treatment [6].
The drug-drug interaction potential of golodirsen is low, according to in vitro studies. In vitro, golodirsen is not an inhibitor of CYP450 isoenzymes (CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19 or CYP3A4/5) [13], nor a substrate or inhibitor of key transporter proteins (OAT1, OAT3, OCT2, OATP1B1, OATP1B3, MATE1, MATE2-K, P-gp and BCRP) [6]. Golodirsen is not an inducer of CYP2B6 or CYP3A4, but a weak inducer of CYP1A2 [6].
2.3 Therapeutic Trials
The efficacy of golodirsen was evaluated in the pivotal, 2-part, multicenter phase I/II trial (NCT02310906) in DMD patients (aged 6–15 years) with a confirmed DMD gene mutation that is amenable to exon 53 skipping [12, 14]. Part 1 was a 12-week, double-blind, placebo-controlled, dose-titration phase I study where randomized patients received intravenous golodirsen (n = 8) in four escalating dose levels (from 4 mg/kg/week to 30 mg/kg/week for 2 weeks at each dose level) or matching placebo (n = 4) once weekly. Part 2 was a 168-week, open-label, phase 2 study assessing the long-term efficacy and safety of intravenous golodirsen 30 mg/kg once weekly in 12 patients who participated in part 1 plus 13 treatment-naïve patients [12, 14]. In the interim analysis at week 48 of part 2 (n = 25), all patients demonstrated a 100% exon 53 skipping response rate [12]. The mean dystrophin level (from muscle biopsies) assessed by western blot significantly (p < 0.001) increased from baseline (mean and median change from baseline of + 0.92% and + 0.88% of normal levels). Positive correlation was observed between de novo dystrophin protein production and exon 53 skipping (Spearman-r = 0.5; p = 0.011) [12]. Correct sarcolemmal localization of dystrophin in muscle fibers was also confirmed by immunofluorescence staining, suggesting that the produced dystrophin was functional [12, 15].
2.4 Adverse Events
In two double-blind, placebo-controlled clinical trials in DMD patients, the most common adverse events occurring in ≥ 20% of patients with a higher incidence in golodirsen (n = 41) than placebo (n = 21) recipients included headache (41% vs 10%), pyrexia (41% vs 14%), fall (29% vs 19%), abdominal pain (27% vs 10%), nasopharyngitis (27% vs 14%), cough (27% vs 19%), vomiting (27% vs 19%) and nausea (20% vs 10%) [6]. Hypersensitivity reactions, including rash, pyrexia, pruritus, urticaria, dermatitis and skin exfoliation, have been reported with golodirsen. In the event of hypersensitivity reactions, appropriate medical treatment and slowing or interrupting the infusion of golodirsen therapy should be considered. Renal toxicity with golodirsen was not observed in the clinical studies [6].
2.5 Ongoing Clinical Trials
An ongoing double-blind, placebo-controlled multicentre phase III trial (NCT02500381; ESSENCE) in DMD patients (aged 7–13 years) with mutations amenable to exon 45 or 53 skipping is evaluating the efficacy and safety of casimersen or golodirsen, respectively, versus placebo. Eligible patients will be randomized to receive active treatment (golodirsen or casimersen depending on the DMD gene mutation) or placebo for up to 96 weeks, after which all patients will receive open-label active treatment for 48 weeks. In addition, a 144-week, open-label, phase III extension study (NCT03532542) is underway to evaluate the long-term safety and tolerability of casimersen and golodirsen in DMD patients (aged 7–23 years) with mutations amenable to exon 45 or 53 skipping, respectively. The trial intends to enroll 260 patients who have completed a clinical trial evaluating casimersen or golodirsen by invitation. Sarepta Therapeutics is also planning to initiate a 48-week, open-label phase II clinical trial (NCT04179409) to evaluate the efficacy and safety of casimersen, eteplirsen or golodirsen for the treatment of DMD in patients (aged ≥ 6 months) carrying a single exon duplication of either exon 45, 51 or 53, respectively. A longitudinal evaluation of exon-skipping-amenable patients (LEAP) study is enrolling ambulatory and/or nonambulatory patients with DMD with a confirmed mutation of the DMD gene amenable to exon 51 or 53 skipping to evaluate longitudinal treatment outcomes of eteplirsen and golodirsen in a real-world setting [16].
3 Current Status
Intravenous golodirsen received its first global approval on 12 December 2019 in the USA for the treatment of DMD in patients with a confirmed mutation of the DMD gene amenable to exon 53 skipping [5].
References
Verhaart IEC, Aartsma-Rus A. Therapeutic developments for Duchenne muscular dystrophy. Nat Rev Neurol. 2019;15(7):373–86.
Messina S, Vita GL. Clinical management of Duchenne muscular dystrophy: the state of the art. Neurol Sci. 2018;39(11):1837–45.
Sarepta Therapeutics. Sarepta Therapeutics announces FDA approval of Vyondys 53™ (golodirsen) injection for the treatment of Duchenne muscular dystrophy (DMD) in patients amenable to skipping exon 53 [media release]. 12 Dec 2019.
Sarepta Therapeutics. Sarepta Therapeutics receives Complete Response Letter from the US Food and Drug administration for golodirsen new drug application [media release]. 19 Aug 2019.
US Food & Drug Administration. FDA grants accelerated approval to first targeted treatment for rare Duchenne muscular dystrophy mutation [media release]. Dec 12 2019.
Sarepta Therapeutics. Vyondys 53™ (golodirsen) injection, for intravenous use. 2019. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/211970s000lbl.pdf. Accessed 12 Dec 2019.
Sarepta Therapeutics. Sarepta Therapeutics enters into collaboration for the development of additional exon-skipping product for Duchenne muscular dystrophy [media release]. 26 Nov 2012.
Sarepta Therapeutics, University of Western Australia. Sarepta therapeutics and University of Western Australia announce exclusive worldwide licensing agreement for exon-skipping program in duchenne muscular dystrophy [media release]. 11 Apr 2013.
US Securities and Exchange commission. First amendement to license agreement 2016. https://www.sec.gov/. Accessed 9 Jan 2020.
Sarepta Therapeutics. Sarepta Therapeutics announces favorable USPTO decisions in exon 51 and exon 53 composition of matter patent interference cases against BioMarin Pharmaceutical [media release]. 20 Sep 2016.
Sarepta Therapeutics. Sarepta Therapeutics and BioMarin Pharmaceutical Inc. announce execution of a global settlement and a license agreement resolving exon skipping patent litigation [media release]. 18 Jul 2017.
Muntoni F, Frank DE, Morgan J, et al. Golodirsen induces dystrophin expression [abstract no. S-5 and presentation]. J Clin Neuromuscul Dis. 2018;19(3):173.
Sazani P, Charleston JS, Shanks C, et al. Pharmacokinetic evaluation of eteplirsen, SRP-4045, and SRP-4053; three phosphorodiamidate morpholino oligomers (PMOs) for the treatment of patients with Duchenne muscular dystrophy (DMD) [abstract no. PP09.5-2350]. Eur J Paediatr Neurol. 2015;19(Suppl 1):S66.
Frank DE, Mercuri E, Servais L, et al. Golodirsen treatment induces dystrophin expression and is well-tolerated in eligible patients with Duchenne muscular dystrophy [abstract no. 8]. Muscle Nerve. 2019;60(Suppl 2):S7.
Scaglioni D, Catapano F, Ellis M, et al. Novel high-throughput digital analysis to quantify the amount of functional sarcolemmal dystrophin and myofibre regeneration in Duchenne muscular dystrophy clinical trial samples (exon 53 skipping with golodirsen) [abstract no. P.146]. Neuromuscul Disord. 2019;29(Suppl 1):S91.
Tsai K, McSherry C, Leffler M, et al. Physical function of eteplirsen- and golodirsen-treated Duchenne muscular dystrophy patients: methodology of the longitudinal evaluation of exon-skipping–amenable patients (LEAP) sudy [poster presentation]. In: Muscular Dystrophy Association Clinical and Scientific Conference 2019.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Conflict of interest
During the peer review process the manufacturer of the agent under review was offered an opportunity to comment on the article. Changes resulting from any comments received were made by the authors on the basis of scientific completeness and accuracy. Young-A Heo is a salaried employee of Adis International Ltd/Springer Nature, is responsible for the article content and declares no relevant conflicts of interest.
Additional information
Enhanced material for this AdisInsight Report can be found at https://doi.org/10.6084/m9.figshare.11788788.
This profile has been extracted and modified from the AdisInsight database. AdisInsight tracks drug development worldwide through the entire development process, from discovery, through pre-clinical and clinical studies to market launch and beyond.
Rights and permissions
About this article
Cite this article
Heo, YA. Golodirsen: First Approval. Drugs 80, 329–333 (2020). https://doi.org/10.1007/s40265-020-01267-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-020-01267-2