Abstract
Dopamine agonists (DAs) represent an excellent treatment option for patients with Parkinson’s disease, in both the early and advanced stages of the disease, improving motor symptoms, lowering the incidence of motor complications, and addressing several non-motor symptoms. Indeed, each of these compounds have different pharmacokinetic and pharmacodynamic properties, resulting in a unique efficacy and safety profile. Comorbidities, prominent non-motor symptoms and individual subjects’ clinical characteristics should guide the choice of a specific DA, allowing better management of the patient by optimizing the DA benefit/risk ratio. In this article we discuss brain distribution of dopamine receptors and their role in each of the dopaminergic pathways, the pharmacological profile of non-ergoline DAs and class-related adverse effects, as reported from post-marketing studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
All dopamine agonists improve motor symptoms in patients with early Parkinson’s disease (PD), as well as motor fluctuations in the advanced stages of the disease. |
Dopamine agonists may address several bothersome non-motor symptoms, including gastro-intestinal and urinary dysfunction, sleep abnormalities and mood disorders. |
Dopamine agonists are generally well tolerated but impulse control disorders, dopamine agonist withdrawal syndrome, and heart failure have emerged as class-related adverse effects. |
Dopamine agonists should be prescribed according to their different pharmacologic and pharmacokinetic profiles in different PD subpopulations. |
1 Introduction
Dopamine agonists (DAs) are compounds that mimic the action of dopamine in stimulating striatal post-synaptic receptors and are usually classified as ergot derived (e.g. bromocriptine, pergolide, cabergoline, lisuride, α-dihydroergocryptine) and non-ergot derived (e.g. apomorphine, piribedil, ropinirole, pramipexole, and rotigotine). DAs were initially developed as an adjunctive therapy to levodopa (L-dopa) for patients with advanced Parkinson’s disease (PD) with motor complications [1,2,3]. DAs are also used both as monotherapy in mild-to-moderate PD and as first choice in younger patients with the goal of delaying L-dopa therapy and the related risk of motor complications [4, 5].
The newer DAs have the advantage of a longer half-life, which can simplify the schedule of administration, due to a once-daily dosing, ensuring better compliance and tolerability. However, post-marketing studies of DAs have highlighted the occurrence of important long-term adverse effects, such as impulse control disorders (ICDs), that have significantly limited their use in clinical practice.
Several factors, including pharmacokinetic and pharmacodynamic properties, patient’s clinical characteristics and concomitant morbidities, need to be considered when choosing a DA to optimize the benefit/risk ratio.
Currently, ergot-derived DAs are rarely utilized due to significant safety concerns, including heart valve fibrosis, vasospasm, erythromelalgia, pleuro-pulmonary and retroperitoneal fibrosis [6,7,8]. This article will focus on non-ergot DAs, which are well known to provide clinical benefits for both early and advanced PD [9, 10]. In particular, the advantages and disadvantages for each molecule will be discussed, with the aim of advising a more patient-tailored therapeutic choice.
1.1 Distribution and Role of Dopamine Receptors
Dopamine receptors are widely represented in the central nervous system (CNS) and in the periphery. Dopamine receptors can be divided in two families, D1 and D2: the D1 family includes D1 and D5 while the D2 family includes D2, D3 and D4.
There are four dopaminergic pathways in the brain. The Nigro-Striatal pathway is responsible for locomotor activity and is mediated by D1, D2 and D3 receptors. D1 and D2 receptors are present in high concentrations in the caudate and the putamen while D1 receptors are found exclusively in the internal globus pallidus (GPi) and substantia nigra pars reticulata (SNr) (direct pathway) and D2 receptors are mainly expressed in the striatal projections to external globus pallidus (GPe) (indirect pathway) [11, 12]. The Meso-Limbic pathway projects from the ventral tegmental area (VTA) of the midbrain to the nucleus accumbens and to the olfactory tubercle and expresses preferentially D3 receptors. Executive functions are mediated by the Meso-Cortical pathway that connects the VTA to the prefrontal cortex, which contains the highest expression of D4 receptors.
Both the Meso-Limbic and the Meso-Cortical pathways have a crucial role in learning and memory mechanisms implicated in reinforcement and reward-related behaviors [13, 14]. Recent studies demonstrated that changes in dopaminergic neurotransmission in the mesolimbic pathway are associated with modification of reward-related behaviors and are therefore closely associated with addiction-type behavior [15, 16]. The extensive representation of D3 receptors within the limbic system, frontal cortex and thalamus, reveals the crucial role of hyper-stimulation of this receptor in modifying behavior [17].
The Tubular-Infundibular pathway originates in the hypothalamus, projects to the hypophysis and is involved in neuroendocrine regulation and wake-sleep cycle generation. At this level, dopamine acts by inhibiting prolactin release, with a subsequent negative effect on heart rate and vascular tone [18].
Outside the CNS, dopamine receptors can be found in kidneys, blood vessels, postganglionic sympathetic nerves and sympathetic ganglia. In kidneys, stimulation of D1 receptors is associated with renal vasodilation and an increase in electrolyte excretion, determining increase in renal flow, diuresis, natriuresis and subsequent hypotension. D2 receptors mediate bradycardia, decrease in afterload and vasodilatation in certain vascular beds, also determining hypotension [19, 20].
Basal ganglia seem to be involved in autonomic mechanisms, regulating heart rate and blood pressure. Stimulation of D2/D3 receptors has been found to positively correlate with heart rate variability and negatively affect supine systolic blood pressure plus heart rate [21]. The vasodilatation and subsequent lowering of blood pressure can also result from the activation of post-synaptic dopamine receptors located on the vascular smooth muscle of blood vessels [22,23,24], while the activation of D2 receptors in the heart reduce heart rate and left ventricular contractility [25].
Dopaminergic mechanisms are also important in regulation of gastrointestinal motility. Dopamine exerts a direct relaxant effect by activating muscular D2 receptors in the lower esophageal sphincter and stomach. Furthermore, dopamine exerts an indirect inhibitory effect on the musculature by inhibiting acetylcholine release from the intrinsic cholinergic motor neurones via the activation of pre-junctional D2 receptors [26].
Conceivably, dopamine receptors are involved in the regulation of a variety of functions including locomotor activity, cognition, memory, pleasure, reward, addiction, pain, modulation of neuroendocrine pathways, and learning. Clinically, dopaminergic modulation of all frontal-subcortical circuits provides the anatomic basis not only for the complex effect of dopaminergic agents, but also for their adverse reactions.
2 D1/D2 Family Agonists
2.1 Apomorphine
Apomorphine is a highly potent, short half-life D1/D2 agonist showing greater affinity for D1 compared with D2 receptors, resembling the receptor profile of dopamine. Apomorphine hydrochloride is derived by heating morphine with concentrated hydrochloric acid. However, it has completely different pharmacological properties to morphine: apomorphine has no opiate properties and no direct pain-killing properties [27]. In addition, apomorphine acts as an antagonist for adreno- and histamine-receptors [28].
It has been demonstrated that apomorphine has an efficacy profile comparable with levodopa [29]. The use of intermittent apomorphine injections represents an extremely efficacious rescue therapy for OFF related to delayed ON and NO-ON phenomena [30].
A sublingual formulation of apomorphine for the fast remission of OFF episodes is currently being evaluated in Phase III clinical trials [31].
Treatment with subcutaneous continuous infusion is indicated for advanced Parkinsonian patients suffering from drug-resistant OFF periods and peak dose dyskinesia uncontrolled by oral treatment. However, this therapy is available only in few European countries. Phase III studies for the development of apomorphine infusion are currently ongoing in Austria, Denmark, France, Germany, The Netherlands, Spain and the USA. Clinical trials have reported only mild adverse effects, the most common being site injection nodules, yawning, drowsiness, nausea, somnolence and dizziness [32,33,34].
Apomorphine is effective on non-motor symptoms (NMS) including mood/apathy, perceptual problems/hallucinations, attention/memory, gastro-intestinal and urinary domains [35]. Studies conducted with diagnostic instrumental tests found that apomorphine was able to correct anorectal dysfunction, improve swallowing abnormalities, total swallowing time and urinary function by ameliorating voiding efficiency [36,37,38]. Several case reports have highlighted the efficacy of apomorphine on treating OFF-related pain, in particular that of visceral presentation such as acute genital, pelvic and thoracic pain [39,40,41]. Therefore, when OFF is associated with intractable pain, apomorphine should be considered as an important option to relieve the patients’ discomfort.
2.2 Rotigotine
Rotigotine is the only DA manufactured as a transdermal patch, which offers several key advantages over oral therapy, including elimination of variables influencing gut absorption, such as impaired gastro-intestinal motility and food effects. It has affinity for both D2/D3 receptor as well as D1, suggesting that it closely resembles endogenous dopamine [42].
A recent meta-analysis demonstrated that rotigotine was associated with significant improvements in PD symptoms, as evidenced by reductions in Unified Parkinson’s Disease Rating Scale (UPDRS) motor and activity of daily living (ADL) scores in patients with both early and advanced PD. The most common adverse events (AEs) were application site reactions, nausea, and somnolence [43].
Several studies have investigated the long-term effect of rotigotine on motor complications and found that the incidence of dyskinesias was low with dyskinesia being generally “not disabling” or “mildly disabling” [44,45,46].
Among NMS, rotigotine has demonstrated its efficacy in improving nocturnal sleep disturbances, painful dystonia in the morning and nocturnal painful muscle cramps or spasms through amelioration of nocturnal OFF and early morning OFF [47,48,49]. Rotigotine has been shown to be effective for swallowing dysfunction, improving both the oral and pharyngeal phase of swallowing [50] and to ameliorate gastric emptying, in two small open-label studies in patients with early and advanced PD, based on video-fluoroscopy and breath test with 13C-octanoic acid results [51]. This beneficial effect on gastro-intestinal motility seems to be ascribable to the reduced inhibition of the myenteric plexus (D2 mediated) and the ability to bring about the central dopaminergic augmentation on gastro-intestinal motility mediated by D1 receptor. In a small study performed on patients with de novo PD, the administration of rotigotine was not associated with modification of cardiovascular parameters, such as orthostatic and cardiac response to Valsalva maneuver [52].
3 D2 Family Agonists
3.1 Pramipexole
Pramipexole has a high selectivity for D2, D3 and D4 receptors but higher affinity for D3 receptors [53]. The dopamine receptor-binding properties of pramipexole is similar to ropinirole: both have a C100-fold higher affinity for D3 over D2 receptors and no demonstrable affinity for dopamine D1 subfamily receptors [54, 55].
Both formulations of pramipexole [immediate release (IR) and extended release (ER)] are effective in improving motor disability and activities of daily living as measured by UPDRS part III and II in early PD patients and reducing the daily total ‘OFF-time’ in advanced Parkinsonian patients [56, 57].
The safety profile did not differ between pramipexole IR and ER, with somnolence, nausea, constipation, dizziness and hallucinations recognized as the most common treatment-emergent AEs in early PD [58] and dyskinesias in advanced PD [59]. Daily somnolence is frequently associated with pramipexole since sudden onset of sleep and sleep attacks have been reported with higher frequency in treated groups compared with placebo [60].
Pramipexole IR has been shown to have beneficial effects on depression [61, 62] and is considered to be efficacious for treating PD depressive symptoms according to Movement Disorders Society (MDS) guidelines [63].
3.2 Ropinirole
Ropinirole stimulates both D2 and D3 striatal dopamine receptors. It is 20-fold more selective for D3 than D2 receptors and 50-fold more selective for D3 than D4 receptors. It has almost no affinity for D1, β-adrenoceptors, adrenergic, serotoninergic and g-aminobutyric acid receptors [64].
In a randomized clinical trial performed in early PD, IR and prolonged released (PR) ropinirole demonstrated similar efficacy on the UPDRS motor score [65]; in subjects sub-optimally controlled by levodopa, ropinirole PR was found to significantly delay the onset of dyskinesia [66]. In advanced PD, a statistically significant reduction in daily OFF time compared with placebo group was observed with ropinirole PR [67], which was also significantly superior to ropinirole IR in maintaining an improvement in daily OFF time [68].
The most common adverse effects, for both formulations, were nausea and somnolence of mild-to-moderate severity, which occur more frequently during the titration phase [65]. Excessive somnolence and sudden onset of sleep (sleep attack) were also observed in randomized clinical trials, even though in one study ropinirole PR improved subjective quality of sleep, reduced daytime sleepiness and led to disappearance of sleep attacks compared with ropinirole IR, possibly due to a more stable plasma concentration of ropinirole [69].
Data on ropinirole and NMS from post hoc analysis of randomized clinical trials and post-marketing studies suggest that ropinirole may have beneficial effects on sleep, nocturnal disturbances, anxiety and depression [70, 71].
3.3 Piribedil
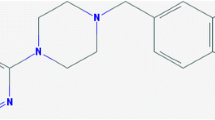
Piribedil is a dopamine agonist marketed in South and Central America, in a few European countries, and in Asia. It is a piperazine derivative that acts as a partial agonist for D2/D3 receptors; it also has α2-adrenergic antagonist properties, low affinity for serotonin 5-HT receptors, and slight affinity for the histaminergic and cholinergic receptors. Piribedil is formulated as an ER formulation that is administered three times a day [72, 73].
This drug has been proven to be efficacious as monotherapy and as adjunct to levodopa in early, non-fluctuating PD patients [74].
For NMS, piribedil has been found to be effective for apathy, perhaps in relation to its α2-antagonistic properties, and on daytime sleepiness as evidenced by randomized controlled trials [74].
In conclusion, piribedil can be considered a useful alternative to standard DAs in subjects with apathy and excessive daytime sleepiness.
4 Class-Related Adverse Effects
4.1 Impulse Control Disorders (ICDs)
ICD symptoms most commonly include pathological gambling, excessive spending and hypersexuality, and have been reported in association with the use of IR DAs [75,76,77]. ICD risk factors are well known and include younger age, male gender, premorbid personality, treatment with levodopa, monoamine oxidase-B (MAO-B) inhibitors and particularly DAs [78, 79].
The relatively recent marketing of the new ER DAs has not yet shown conclusive data on the incidence of ICD during their use. However, a recent study [80] clarified the incidence of ICD in PD patients treated with different DAs. This was a retrospective and prospective survey based on medical charts of 425 subjects enrolled from eight Movement Disorders Centers across Europe. The overall incidence of clinically relevant ICD was 13.4%; the rate of ICD was significantly lower with rotigotine compared with ropinirole (ER plus IR), pramipexole IR and pramipexole (IR plus ER). There was no significant difference between rotigotine and pramipexole ER, having the respective incidence rates of 4.9% and 6.6%, respectively [80].
These data have been confirmed by an earlier multicenter transversal study performed in Spain [81], suggesting that oral treatment with DA was found to be strongly associated with risk of ICD compared with transdermal rotigotine (42% vs 19%). No significant difference was found between standard versus ER DAs [81].
The different incidence detected between oral ER DAs and transdermal rotigotine might be related to the different route of administration and to the resulting stability of plasma concentrations [80, 81].
Treatment with subcutaneous apomorphine infusion has been associated with a lower rate of risk of developing ICDs according to several reports and confirmed by results of a large multicenter national study on advanced patients [82].
The occurrence of ICDs in patients treated with DA therapy has led many neurologists to switch to piribedil, which was rarely associated with this disorder. Nevertheless, in the last few years, several cases of ICD have been reported in subjects on piribedil [83], so caution is warranted when this drug is prescribed to subjects with a past history of ICD.
Current clinical practice has shown that ICDs can be successfully controlled by reducing the dose of the DA or by its discontinuation. A compensatory increase in levodopa dosage, the adjunct of catechol-O-methyl transferase (COMT) inhibitors, or MAO-B inhibitors is usually required to maintain an optimal clinical control.
Switching from one agonist to another, even with different pharmacological properties, does not always result in a disappearance of the ICD. There is no established treatment for ICD; small clinical trials have tested the efficacy of several drugs [e.g. atypical antipsychotics, mood stabilizers, selective serotonin reuptake inhibitors (SSRIs), amantadine, naltrexone] with insufficient evidence of efficacy [84].
4.2 Dopamine Agonist Withdrawal Syndrome (DAWS)
Dopamine agonist withdrawal syndrome (DAWS) was clinically defined in 2010 and includes a stereotyped cluster of physical and psychological disturbances such as panic attacks, depression, diaphoresis, agitation, fatigue, pain, orthostatic hypotension and drug craving. The development of DAWS seems to be related to higher DA dosage, cumulative DA exposure, higher levodopa equivalent daily doses (LEDD) and longer duration of DA treatment [85]. DAWS can occur immediately after the beginning or at the end of DA taper [86].
Interestingly, all subjects developing DAWS had to withdraw a DA because of an ICD and had a previous history of anxiety, depression and behavioral addiction disorders, which can therefore be identified as risk factors for developing both ICD and DAWS [85, 86].
DAWS has been observed after tapering of pergolide, pramipexole and ropinirole without statistically significant difference amongst DAs. Nowadays it is generally recognized that DAWS is a class effect since its occurrence has been noted after discontinuation of the majority of DAs.
No specific treatment for this syndrome has proven to be efficacious among those tested (e.g. SSRIs, mirtazapine, benzodiazepines, opiates, gabapentin, or cognitive behavioral therapy). Increasing levodopa following the taper of the DA does not usually ameliorate DAWS symptomatology even though there are some minor cases that can benefit from higher levodopa dosages [87].
4.3 Cardiological Adverse Effects
Few studies have investigated the association between heart failure (HF) and DAs. None of these have provided a definite explanation of the association between use of DAs and increased risk of HF. This risk is not a class effect for DAs and is not related to ergoline structure. Pramipexole, which most of all has been found to be related to an increased risk of HF, has high affinity for D2, D3, D4 receptors but it is also an α2-adrenergic receptor agonist; its probable role in increasing the risk of HF could be related to the activation of these auto-receptors, thus reducing adrenergic tone and myocardial contractility [88]. Pramipexole could also unmask a subclinical HF or negatively influence preexisting cardiovascular comorbidities [89].
Conceivably, a careful cardiological assessment is recommended before prescribing and throughout the treatment with pramipexole. Other cardiological AEs associated with DA treatment are sinus node dysfunction with ropinirole [90] and first-degree AV block with rotigotine [91]. In Phase III studies and during post-marketing surveillance, apomorphine has been associated with QT prolongation and cardiac arrest [92, 93] even though animal studies [94] and a formal study performed with sublingual formulation (data not published) have not confirmed these data.
Further clinical and instrumental studies, targeted to a physio-pathological definition of the causes of HF, are needed to improve therapeutic management of PD patients.
5 Summary
DA agonists are definitely powerful drugs in the management of PD and have shown equal evidence of being clinically useful both as monotherapy or adjunct to L-dopa in early and mid-stage/advanced PD patients. DA agonists improve motor symptoms and also ameliorate some NMS (Table 1, Fig. 1). Moreover, no other antiparkinsonian drugs have shown a similar positive effect in improving motor fluctuations. The power of a DA becomes clear to physicians and patients when for any reason the dose of the agonist needs to be reduced or withdrawn. The worsening of motor and non-motor symptoms is abrupt and can be hardly compensated for by a significant increase of L-dopa.
Indeed, in the past years, some clinical problems have emerged with the use of DAs. ICDs and DAWS are clinical syndromes that physicians have to take into consideration when using DAs and learn how to deal with them. Moreover, cumulative knowledge about these drugs gives us the opportunity to recognize specific adverse effects, allowing the opportunity of an early intervention.
DAs are not all the same. On top of some class-related AEs there are differences in expression and frequency of AEs across DA agonists. This is due to the different dopamine receptor affinity, pharmacokinetic and pharmacodynamic properties. It has also been reported that the symptomatic effect can significantly increase by combining two DAs with different pharmacological profiles [95]. We reported in this article how the AE profile and the presence of prominent NMSs plus concomitant morbidities characterize each DA and need to be considered before prescribing a DA.
6 Recommendations
The clinical response to a DA is different for each subject and switching from one DA to another is recommended in case of a lack of benefit or bothersome adverse effects.
Treatment with DAs should begin with a low dose and be increased until a meaningful clinical benefit occurs.
The elderly are at greater risk of developing AEs during treatment with DAs, and a risk–benefit analysis should be performed before initiating treatment, based on presence of motor complications, comorbidities and cognitive impairment [96]. Patient’s preference and lifestyle habits should also guide neurologists to choose between oral medications (i.e. pramipexole and ropinirole), or rotigotine, which is administered by the transdermal route.
6.1 Motor Symptoms
Pramipexole, ropinirole and rotigotine have shown equal evidence of being clinically efficacious both as monotherapy and as add-on to L-dopa [9]. Treatment with apomorphine in subcutaneous infusion is approved for advanced Parkinsonian patients suffering from OFF periods and peak dose dyskinesia uncontrolled by oral treatment [30].
Apomorphine administered by subcutaneous injection (bolus) is a rescue therapy that offers very rapid relief of early morning akinesia, drug-resistant OFF and unpredictable OFF periods as well as OFF-related pains, with a dramatic impact on patients’ quality of life [30, 31, 39, 40].
6.2 Non-motor Symptoms
6.2.1 Neuropsychiatric Symptoms
Parkinsonian patients with depression may benefit from DA treatment and, in particular, pramipexole [62, 63]. Within this category of patients, particular attention should be paid to young, male patients who are known to be at greater risk for developing ICDs. Increased risk of ICD has also been found in subjects with baseline personality characterized by impulsivity, altered executive function, greater novelty seeking, and premorbid ICDs. Therefore, in this population, the use of a DA should be minimized or a DA with higher affinity for D1 receptors such as rotigotine or apomorphine should be preferred [78].
Piribedil is the only DA that has been found to be effective for apathy and can be considered when this symptom is present [74]. The presence of cognitive decline should discourage the use of DAs since they can trigger or exacerbate confusion and other psychotic symptoms. The occurrence of confusion, hallucination and delirium requires a temporary or permanent discontinuation of a DA accompanied by a compensatory increased in L-dopa daily dosage [63].
6.2.2 Autonomic Dysfunction
Apomorphine or rotigotine, because of their alternative route of administration and enhanced gastro-intestinal activity mediated by D1 receptors, should be preferred in subjects with drooling, dysphagia, or prominent gastrointestinal dysfunction, as well as in presence of delayed ON and NO-ON phenomena due to slow gastric emptying [36, 37, 50, 51].
Since apomorphine injection may cause an acute lowering of blood pressure values, it should be used with caution in patients suffering from post-prandial hypotension. Subjects with orthostatic hypotension (OH) should be preferentially treated with L-dopa because DAs are well known to exacerbate OH through vasodilatation in peripheral vascular beds [23]. Excessive sweating is a common NMS that can cause poor adhesiveness and reduce the effectiveness of treatment with rotigotine [97].
6.2.3 Sleep Disorders
Rotigotine and ropinirole have been shown to be efficacious in improving sleep with a significant effect on sleep quality and maintenance, nocturnal akinesia as well as early morning dystonia [69, 70, 98]. Daily somnolence, sudden onset of sleep and sleep attacks have been frequently associated with pramipexole and, to lesser extent, ropinirole. Since these episodes tend to occur without notice, even in non-demented subjects, close monitoring with specific scales measuring daily sleepiness is needed [60, 67].
6.3 Comorbidities and Concomitant Medication
It is of outmost importance to carefully evaluate patients’ comorbidities and concomitant medication before prescribing a specific DA since all DAs are extensively metabolized by the liver, except for pramipexole, which is primarily excreted unaltered in the urine by active renal tubular secretion (Table 2). The major route of elimination of the remaining DA is via the liver through the cytochrome P450 (CYP) enzyme system; thus, particular attention needs to be given to patients treated with other CYP inhibitors.
Pramipexole can be particularly useful for patients receiving multiple drugs to minimize drug–drug interactions. In contrast, pramipexole should not be used in patients with advanced renal impairment, and dosage must be adjusted in patients with mild or moderate renal insufficiency [55]. The link between pramipexole and HF needs still to be fully elucidated, but a risk–benefit analysis should be performed before starting pramipexole in a population at risk due to older age, male gender, history of hypertension or other cardiovascular disturbances, cigarette smoking, diabetes and physical inactivity [89].
7 Conclusion
DAs represent an excellent treatment option for patients with PD, both as monotherapy in early disease and as an add-on to L-dopa in later disease. However, it is very important that these medications are prescribed at the right time, at the right doses and in the right combinations with other antiparkinsonian drugs in order to optimize benefits and minimize AEs. Finally, we are still not close to the ideal DA agonist, which should mirror the clinical and pharmacologic profile of L-dopa, with a rapid-onset and long duration of action, a manageable route of administration but without the adverse effects. Fostering the development of new dopaminergic compounds that would prove clearly superior to those currently used, should be considered as one of the priorities in PD.
References
Quinn N. Drug treatment of Parkinson’s disease. Br Med J. 1995;310:575–9.
Calne DB, Teychenne PF, Leigh PN, Bamji AN, Greenacre JK. Treatment of parkinsonism with bromocriptine. Lancet. 1974;2(7893):1355–6.
Hoehn MM, Elton RL. Low dosages of bromocriptine added to levodopa in Parkinson’s disease. Neurology. 1985;35(2):199–206.
Stocchi F. Continuous dopaminergic stimulation and novel formulation of dopamine agonists. J Neurol. 2011;258(2):S316–22.
Nutt JG, Obeso JA, Stocchi F. Continuous dopamine receptor stimulation in advanced Parkinson’s disease. Trends Neurosci. 2000;23:109–15.
Antonini A, Poewe W. Fibrotic heart-valve reactions to dopamine-agonist treatment in Parkinson’s disease. Lancet Neurol. 2007;6(9):826–9.
Goetz CG, Diederich NJ. Dopaminergic agonists in the treatment of Parkinson’s disease. Neurol Clin. 1992;10(2):527–40.
Uitti RJ, Ahlskog JE. Comparative review of dopamine receptor agonists in Parkinson’s disease. CNS Drugs. 1996;5(5):369–88.
Fox SH, Katzenschlager R, Lim SY, Ravina B, Seppi K, Coelho M, et al. The movement disorder society evidence-based medicine review update: treatments for the motor symptoms of Parkinson’s disease. Mov Disord. 2011;26(Suppl 3):S2–41.
Yamamoto M, Schapira AH. Dopamine agonist in Parkinson’s disease. Expert Rev Neurother. 2008;8(4):671–7.
Kvernmo T, Hartter S, Burger E. A review of the receptor binding and pharmacokinetic properties of dopamine agonists. Clin Ther. 2006;28(8):1065–78.
Jenner P. Pharmacology of dopamine agonists in the treatment of Parkinson’s disease. Neurology. 2002;58(1):S1–8.
Beninger RJ. The role of dopamine in locomotor activity and learning. Brain Res. 1983;287(2):173–96.
Pignatelli M, Bonci A. Role of dopamine neurons in reward and aversion: a synaptic plasticity perspective. Neuron. 2015;86(5):1145–57.
Nestler EJ, Carlezon WA. The mesolimbic dopamine reward circuit in depression. Biol Psychiatry. 2006;59:1151–9.
Steketee JD, Kalivas PW. Drug wanting: behavioral sensitization and relapse to drug-seeking behavior. Pharmacol Rev. 2011;63:348–65.
Seeman P. Parkinson’s Disease treatment may cause impulse–control disorder via dopamine D3 receptors. Synapse. 2015;69:183–9.
Manku MS, Horrobin DF, Zinner H, Karmazyn M, Morgan RO, Ally AI, et al. Dopamine enhances the action of prolactin on rat blood vessels. Implication for dopamine effects on plasma prolactin. Endocrinology. 1977;101:1343–5.
Jose PA, Raymond JR, Bates MD, Aperia A, Felder RA, Carey RM. The renal dopamine receptors. J Am Soc Nephrol. 1992;2(8):1265–78.
Contreras F, Fouillioux C, Bolívar A, Simonovis N, Hernández-Hernández R, Armas-Hernandez MJ, et al. Dopamine, hypertension and obesity. J Hum Hypertens. 2002;16(Suppl 1):S13–7.
Yeh TL, Yang YK, Chiu NT, Yao WJ, Yeh SJ, Wu JS, et al. Correlation between striatal dopamine D2/D3 receptor binding and cardiovascular activity in healthy subjects. Am J Hypertens. 2006;19:964–9.
Goldberg LI. Cardiovascular and renal actions of dopamine: potential clinical applications. Pharmacol Rev. 1972;24(1):1–29.
Pendleton RG, Setler PE. Peripheral cardiovascular dopamine receptors. Gen Pharmacol. 1977;8(1):1–5.
Lokhandwala MF, Jandhyala BS. The role of sympathetic nervous system in the vascular actions of dopamine. J Pharmacol Exp Ther. 1979;210(1):120–6.
Polakoski JS, Segreti JA, Cox BF, Hsieh GC, Kolasa T, Moreland RB, et al. Effects of selective dopamine receptors subtype agonists on cardiac contractility and regional hemodynamics in rats. Clin Exp Pharmacol Phisiol. 2004;31:837–41.
Tonini M, Cipollina L, Poluzzi E, Crema F, Corazza GR, De Ponti F. Review article: clinical implications of enteric and central D2 receptor blockade by antidopaminergic gastrointestinal prokinetics. Aliment Pharmacol Ther. 2004;19:379–90.
Menon R, Stacy M. Apomorphine in the treatment of Parkinson’s disease. Expert Opin. Phamachother. 2007;8(12):1941–50.
Boyle A, Ondo W. Role of apomorphine in the treatment of Parkinson’s disease. CNS Drugs. 2015;29:83–9.
Deleu D, Hanssens Y, Northway MG. Subcutaneous apomorphine: an evidence-based review of its use in Parkinson’s disease. Drugs Aging. 2004;21:687–709.
Trenkwalder C, Ray Chadury K, Garcia Riuz PJ, LeWitt P, Katzenschlager R, Sixel-Döring F, et al. Expert consensus group report on the use of apomorphine in the treatment of Parkinson’s disease—clinical practice recommendations. Parkinson Relat Disord. 2015;21(9):1023–30.
Hauser RA, Olanow CW, Dzyngel B, Bilbault T, Shill H, Isaacson S, et al. Sublingual apomorphine (APL-130277) for the acute conversion of OFF to ON in Parkinson’s disease. Mov Disord. 2016;31(9):1366–72.
Hughes AJ, Bishop S, Kleedorfer B, Turjanski N, Fernandez W, Lees AJ, et al. Subcutaneous apomorphine in Parkinson’s disease: response to chronic administration for up to five years. Mov Disord. 1993;8(2):165–70.
Dewey RB, Hutton JT, LeWitt PA, Factor SA. A randomized, double-blind, placebo-controlled trial of subcutaneously injected apomorphine for parkinsonian off-state events. Arch Neurol. 2001;58:1385–92.
Pfeiffer RF, Gutmann L, Hull KL, Bottini PB, Sherry JH, APO302 Study Investigators. Continued efficacy and safety of subcutaneous apomorphine in patients with advanced Parkinson’s disease. Parkinsonism Relat Disord. 2007;13(2):93–100.
Martinez-Martin P, Reddy P, Antonini A, Henriksen T, Katzenschlager R, Odin P, et al. Chronic subcutaneous infusion therapy with apomorphine in advanced Parkinson’s disease compared to conventional therapy: a real-life study of non-motor effect. J Parkininson’s Dis. 2011;1:197–203.
Edwards LL, Quigley EM, Harned RK, Hofman R, Pfeiffer RF. Defecatory function in Parkinson’s disease: response to apomorphine. Ann Neurol. 1993;33:490–3.
Tison F, Wiart L, Guatterie M, Fouillet N, Lozano V, Henry P, et al. Effects of central dopaminergic stimulation by apomorphine on swallowing disorders in Parkinson’s disease. Mov Disord. 1996;11:729–32.
Christmas TJ, Kempster PA, Chapple CR, Frankel JP, Lees AJ, Stern GM, et al. Role of subcutaneous apomorphine in parkinsonian voiding dysfunction. Lancet. 1988;2:1451–3.
Lefaucheur R, Berthelot L, Senant J, Borden A, Maltête D. Acute genital pain during non-motor fluctuations improved by Apomorphine. Mov Disord. 2013;28:5687–8.
Factor SA, Brown DL, Molho ES. Subcutaneous apomorphine injections as a treatment for intractable pain in Parkinson’s disease. Mov Disord. 2000;15:167–9.
Frankel JP, Lees AJ, Kempster PA, Stern GM. Subcutaneous apomorphine in the treatment of Parkinson’s disease. J Neurol Neurosurg Psychiatry. 1990;53:96–101.
Elshoff JP, Cawello W, Andreas JO, Mathy FX, Braun M. Update on pharmacological, pharmacokinetic properties and drug-drug interactions of rotigotine transdermal system in Parkinson’s Disease and Restless Legs Syndrome. Drugs. 2015;75:487–501.
Zhou CQ, Li SS, Chen ZM, Li FQ, Lei P, Peng GG. Rotigotine transdermal patch in Parkinson’s disease: a systematic review and meta-analysis. PLoS One. 2013;8(7):e69738.
Elmer LW, Surmann E, Boroojerdi B, Jankovic J. Long-term safety and tolerability of rotigotine transdermal system in patients with early-stage idiopathic Parkinson’s disease: a prospective, open label extension study. Parkinson Relat Disord. 2012;18:488–93.
Giladi N, Boroojerdi B, Surmann E. The safety and tolerability of rotigotine transdermal system over a 6-year period in patients with early-stage Parkinson’s disease. J Neural Transm (Vienna). 2013;120(9):1321–9.
Giladi N, Ghys L, Surmann E, Boroojerdi B, Jankovic J. Effects of long-term treatment with rotigotine transdermal system on dyskinesia in patients with early-stage Parkinson’s disease. Parkinsonism Relat Disord. 2014;20(12):1345–51.
Trenkwalder C, Kies B, Rudzinska M, Fine J, Nikl J, Honczarenko K, Recover Study Group, et al. Rotigotine effects on early morning motor function and sleep in Parkinson’s disease: a double-blind, randomized, placebo-controlled study (RECOVER). Mov Disord. 2011;26(1):90–9.
Ghys L, Surmann E, Whitesides J, Boroojerdi B. Effect of rotigotine on sleep and quality of life in Parkinson’s disease patients: post hoc analysis of RECOVER patients who were symptomatic at baseline. Expert Opin Pharmacother. 2011;12:1985–98.
Kassubek J, Ray Chadury K, Zesiewicz T, Surmann E, Boroojerdi B, Moran K, et al. Rotigotine transdermal system and evaluation of pain in patients with Parkinson’s disease: a post hoc analysis of the RECOVER study. BMC Neurol. 2014;14:42.
Hirano M, Isono C, Sakamaoto H, Ueno S, Kusunoki S, Nakamura Y. Rotigotine Transdermal Patch Improves Swallowing in Dysphagic Patients with Parkinson’s Disease. Dysphagia. 2015;30(4):452–6.
Tateno H, Sakakibara R, Shiina S, Doi H, Tateno F, Sato M, et al. Transdermal dopamine agonist ameliorates gastric emptying in Parkinson’s disease. Am Geriatr Soc. 2015;63(11):2416–8.
Rocchi C, Pierantozzi M, Pisani V, Marfia GA, Di Giorgio A, Stanzione P, et al. The impact of rotigotine on cardiovascular autonomic function in early Parkinson’s disease. Eur Neurol. 2012;68:187–92.
Piercey MF. Pharmacology of pramipexole, a dopamine D3-preferring agonist useful in treating Parkinson’s disease. Clin Neuropharmacol. 1998;21(3):141–51.
Hisahara S, Shimohama S. Dopamine receptors and Parkinson’s disease. Int J Med Chem. 2011;11:1–16.
Jenner P, Konen-Bergmann M, Schepers C, Haertter S. Pharmacokinetics of a Once-Daily extended-release formulation of pramipexole in healthy male volunteers: three studies. Clin Ther. 2009;31(11):2698–711.
Poewe W, Rascol O, Barone P, Hauser RA, Mizuno Y, Haaksma M, Pramipexole ER Studies Group, et al. Extended-release pramipexole in early Parkinson disease: a 33-week randomized controlled trial. Neurology. 2011;77(8):759–66.
Schapira AHV, Barone P, Hauser RA, Mizuno Y, Rascol O, Busse M, Pramipexole ER Studies Group, et al. Extended-release pramipexole in advanced Parkinson disease: a randomized controlled trial. Neurology. 2011;77(8):767–74.
European Medicines Agency. Assessment report for Mirapexin. International non-proprietary name: pramipexole. Procedure no.: EMEA/H/C/000134/X/0059, 2009. Accessed 29 Jun 2018.
Bergmann K. Center for Drug Evaluation and Research. Application number: 22-514. Medicalreview(s). 2010.http://www.accessdata.fda.gov/drugsatfda_docs/nda/2010/022514s000MedR. Accessed 29 Jun 2018.
Boehringer Ingelheim Pharmaceuticals Inc. Mirapex ER (pramipexole dihydrochloride) extended-release tablets: US prescribing information. 2013. Accessed 29 Jun 2018.
Antonini A, Barone P, Ceravolo R, Fabbrini G, Tinazzi M, Abbruzzese G. Role of pramipexole in the management of Parkinson’s disease. CNS Drugs. 2010;24(10):829–41.
Barone P, Poewe W, Albrecht S, Debieuvre C, Massey D, Rascol O, et al. Pramipexole for the treatment of depressive symptoms in patients with Parkinson’s disease: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2010;9(6):573–80.
Seppi K, Weintraub D, Coelho M, Perez-Lloret S, Fox SH, Katzenschlager R, et al. The Movement Disorder Society evidence-based Medicine review update: treatments for the non-motor symptoms of Parkinson’s disease. Mov Disord. 2011;26(Suppl 3):S42–80.
Kaye CM, Nicholls B. Clinical pharmacokinetics of ropinirole. Clin Pharmacokinet. 2000;39(4):243–54.
Stocchi F, Hersh BP, Scott B, Nausieda PA, Giorgi L, Ease-PD Monotherapy study investigators. Ropinirole 24-hour prolonged release and ropinirole immediate release in early Parkinson disease: a randomized, double blind, non-inferiority crossover study. Curr Med Res Opin. 2008;24:2883–95.
Watts RL, Lyons KE, Pahwa R, Sethi K, Stern M, Hauser RA, 228 Study Investigators, et al. Onset of dyskinesia with adjunct ropinirole prolonged-release or additional levodopa in early Parkinson’s disease. Mov Disord. 2010;25:858–66.
Pahwa R, Stacy MA, Factor SA, Stocchi F, Hersh BP, Elmer LW, EASE-PD Adjunct Study Investigators, et al. Ropinirole 24-hour prolonged release: randomized, controlled study in advanced Parkinson disease. Neurology. 2007;68:1108–15.
Stocchi F, Giorgi L, Hunter B, Schapira AH. PREPARED: comparison of prolonged and immediate release ropinirole in advanced Parkinson’s disease. Mov Disord. 2011;26:1259–65.
Dusek P, Buskova J, Ruzicka E, Majerová V, Srp A, Jech R, et al. Effects of ropinirole prolonged-release on sleep disturbances and daytime sleepiness in Parkinson’s disease. Clin Neuropharmacol. 2010;33:186–90.
Rektorova I, Balaz M, Svatova J, Zarubova K, Honig I, Dostal V, et al. Effects of ropinirole on non motor symptoms of Parkinson’s disease: a prospective multicenter study. Clin Neuropharmacol. 2008;31:261–6.
Buchwald B, Angersbach D, Jost WH. Improvements in motor and non-motor symptoms in Parkinson’s patients under ropinirole therapy. Fortschr Neurol Psychiatr. 2007;75(4):236–41.
Dourish CT. Piribedil: behavioural, neurochemical and clinical profile of a dopamine agonist. Prog Neuropsychopharmacol Biol Psychiatry. 1983;7:3–27.
Servier Laboratories. Trivastal 50 mg LP Summary of Product Characteristics. http://www.servier.com/sites/default/files/SPC_TRIVASTAL_50mg.pdf. Accessed 09 Feb 2019.
Perez-Lloret S, Rascol O. Piribedil for the treatment of motor and non-motor symptoms of Parkinson disease. CNS Drugs. 2016;30:703–17.
Weintraub D, Koester J, Potenza M, Siderowf AD, Stacy M, Voon V, et al. Impulse control disorders in Parkinson disease: a cross-sectional study of 3090 patients. Arch Neurol. 2010;67:589–95.
Bastiaens J, Dorfman BJ, Christos PJ, Nirenberg MJ. Prospective cohort study of impulse control disorders in Parkinson’s disease. Mov Disord. 2013;28:327–30.
Lee JY, Kim JM, Kim JW, Cho J, Lee WY, Kim HJ, et al. Association between the dose of dopaminergic medication and the behavioral disturbances in Parkinson’s disease. Parkinsonism Relat Disord. 2010;16:202–7.
Perez-Lloret S, Rey MV, Fabre N, Ory F, Spampinato U, Brefel-Courbon C, et al. Prevalence and pharmacological factors associated with impulse-control disorder symptoms in patients with Parkinson disease. Clin Neuropharmacol. 2012;35:261–5.
Ondo WG, Lai D. Predictors of impulsivity and reward seeking behavior with dopamine agonists. Parkinsonism Relat Disord. 2008;14:28–32.
Rizos A, Sauerbier A, Antonini A, Weintraub D, Martinez-Martin P, Kessel B, et al. A European multicentre survey of impulse control behaviours in Parkinson’s disease patients treated with short- and long-acting dopamine agonists. Eur J Neurol. 2016;23(8):1255–61.
Garcia-Ruiz PJ, Martinez Castrillo JC, Alonso-Canovas A, Herranz Barcenas A, Vela L, Sanchez Alonso P, et al. Impulse control disorder in patients with Parkinson’s disease under dopamine agonist therapy: a multicentre study. J Neurol Neurosurg Psychiatry. 2014;85(8):840–4.
Garcia Ruiz PJ, Sesar Ignacio A, Ares Pensado B, Castro García A, Alonso Frech F, Alvarez López M, et al. Efficacy of long term continuous subcutaneous apomorphine infusion in advanced Parkinson’s disease with motor fluctuations: a multicenter study. Mov Disord. 2008;23:1130–6.
Micheli F, Giugni J, De Arco Espinosa M, Calvo DS, Raina GB. Piribedil and pathological gambling in six parkinsonian patients. Arq Neuropsiquiatr. 2015;73(2):115–8.
Samuel M, Rodriguez-Oroz M, Antonini A, Brotchie JM, Ray Chaudhuri K, Brown RG, et al. Management of impulse control disorders in Parkinson’s disease: controversies and future approaches. Mov Disord. 2015;30(2):150–9.
Rabinak AC, Niremberg JM. Dopamine agonist withdrawal syndrome in Parkinson’s disease. Arch Neurol. 2010;67(1):58–63.
Niremberg MJ. Dopamine agonist withdrawal syndrome: implications for patient care. Drugs Aging. 2013;30:587–92.
Yu XX, Fernandez HH. Dopamine agonist withdrawal syndrome: a comprehensive review. J Neurol Sci. 2017;374:53–5.
Apraxine M, Pasuqet A, Jeanjean A. Pramipexole-induced reversible heart failure. Mov Disord Clin Pract. 2014;1(4):381–2.
Perez-Lloret S, Rey MV, Crispo J, Krewski D, Lapeyre-Mestre M, Montastruc JL, et al. Risk of heart failure following treatment with dopamine agonists in Parkinson’s disease patients. Expert Opin Drug Saf. 2014;13(3):351–60.
Szymanski C, Boey S, Hermida JS. Ropinirole-induced symptomatic sinus node dysfunction. Pacing Clin Electrophysiol. 2008;31(8):1079–82.
Product Information. Neupro (rotigotine). Schwarz Pharma, Mequon.
Food and Drug Administration, FDA Approved Labeling Text forNDA 021264. http://www.accessdata.fda.gov/drugsatfda_docs/label/2010/021264s009lbl.pdf. Accessed on 15 Sept 2018.
PharmaPendium, Post-marketing reports (AERS) for apomorphinehydrochloride and cardiac disorders. https://www.pharmapendium.com/postmarket.do?initial.drug%5B0%5D=Apomorphine+Hydrochloride&structure=false&multiView.statEntityType=EFFECT&chemistry=false&initial.effect%5B0%5D=Cardiac+disorders&multiView.entityType=DRUG. Accessed 15 Sept 2018.
Watanabe Y, Nakamura Y, Cao X, Ohara H, Yamazaki Y, Murayama N, et al. Intravenous administration of apomorphine does NOT induce long QT syndrome: experimental evidence from in vivo canine models. Basic Clin Pharmacol Toxicol. 2015;116(6):468–75.
Stocchi F, Vacca L, Berardelli A, Onofrj M, Manfredi M, Ruggieri S. Dual dopamine agonist treatment in Parkinson’s disease. J Neurol. 2003;250(7):822–6.
Latt MD, Lewis S, Zekry O, Fung VSC. Factors to consider in the selection of dopamine agonists for older persons with Parkinson’s disease. Drugs Aging. 2019;36(3):189–202.
Elshoff JP, Bauer L, Goldammer N, Oortgiesen M, Pesch H, Timmermann L. Randomized, double-blind, crossover study of the adhesiveness of two formulations of rotigotine transdermal patch in patients with Parkinson’s disease. Curr Med Res Opin. 2018;34(7):1293–9.
Seppi K, Ray Chaudhuri K, Coelho M, Fox SH, Katzenschlager R, Perez Lloret S, et al. Update on treatments for nonmotor symptoms of Parkinson’s disease-an evidence-based medicine review. Mov Disord. 2019;34(2):180–98.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No specific funding was received for this work by the authors.
Conflicts of interest
F. Stocchi has received honoraria as a consultant for Zambon, UCB, Chiesi Pharma, Lundbeck, Sunovion, Bial, SynAgile, Biogen, Kiowa. D. Bravi is an employee of Lundbeck, Research and Development department. M. Torti and L. Vacca have received honoraria from Chiesi Pharma, UCB and Zambon.
Rights and permissions
About this article
Cite this article
Torti, M., Bravi, D., Vacca, L. et al. Are All Dopamine Agonists Essentially the Same?. Drugs 79, 693–703 (2019). https://doi.org/10.1007/s40265-019-01103-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-019-01103-2