Abstract
Hypercholesterolaemia is frequently observed in patients with cardiovascular diseases (CVD) and is associated with increased mortality. Statin treatment has been the standard of care for reducing low-density lipoprotein cholesterol (LDL-C) to improve cardiovascular outcomes. However, statins have limited effects in some patients and may be discontinued due to adverse effects resulting in LDL-C above target levels. The proprotein convertase subtilisin kexin type 9 (PCSK9) is a pivotal regulator in the LDL-C metabolism by degrading the LDL-C receptor on hepatocytes. Inhibition of PCSK9 by monoclonal antibodies (mAb) significantly lowers LDL-C levels and is considered to reduce the likelihood of adverse cardiac events. However, such treatment regimens are not cost-effective, and require frequent administrations at high doses that may be associated with side effects and poor drug adherence. Furthermore, it has been shown that these PCSK9 medicines may trigger the formation of antidrug antibodies followed by a significant attenuation of the LDL-C-lowering effect. Active vaccination inducing high-affinity antibodies against PCSK9 with less frequent administration intervals may be a novel promising therapeutic approach to overcome the drawback of passive immunization with PCSK9 mAb. However there is a paucity of available clinical safety and efficacy data. This article discusses challenges in the development of PCSK9 vaccines and their potential therapeutic benefits by reviewing clinical studies that evaluated the safety and efficacy of PCSK9 mAb.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Increased low-density lipoprotein cholesterol (LDL-C) levels are associated with a greater likelihood of death in patients with cardiovascular diseases (CVD). |
Inhibition of proprotein convertase subtilisin kexin type 9 (PCSK9) using monoclonal antibodies has been shown to be highly efficient in lowering LDL-C and reducing the risk for CVD. |
Vaccines against PCSK9 may overcome drawbacks of passive immunization such as frequent administrations, but first candidates have just entered clinical studies and are not yet commercially available. |
1 Introduction
Cardiovascular disease (CVD) is associated with significant mortality and is the leading cause of death. Risk factors for CVD include, among others, smoking, physical inactivity and clinical conditions such as diabetes mellitus type 2, obesity, arterial hypertension or hyperlipidaemia. In particular, elevated low-density lipoprotein cholesterol (LDL-C) levels are recognized to be a major risk in CVD [1]. Numerous studies have shown that pharmacological interventions for lowering LDL-C prevent the progression of atherosclerosis and improve survival of patients with CVD. Treatment with 3-hydoxy-3-methyglutaryl-coenzyme A (HMG-CoA) inhibitors (statins) is currently the standard of care for primary or secondary prevention in patients with hypercholesterolaemia and these medicines are also used to treat familial hypercholesterolaemia (FH) [2,3,4,5,6]. Statins are considered to be a cost-effective therapeutic approach and are generally well tolerated [7]. However, statin therapy may be insufficient, in particular in patients with FH who do not respond adequately [8,9,10]. Further, up to 10% of patients exposed to statins experience muscle-related symptoms or more serious adverse effects, which may attenuate the LDL-C-lowering effect due do dose adjustment. Intolerance to HMG-CoA inhibitor treatment may also limit achievement of LDL-C target levels. Other disadvantages comprise drug-drug interactions, in particular with cardiovascular medicines, and the need for daily intake, which frequently results in poor adherence to statin treatment [11,12,13,14,15,16]. For patients requiring cholesterol-lowering therapy and who are not suitable for statins, alternative therapeutic approaches need to be provided to avoid cardiovascular events as non-statin therapies such as bile acid sequestrants, fibric acid derivatives, niacin or ezetimibe have been shown to reduce LDL-C less sufficiently [17].
The proprotein convertase subtilisin kexin type 9 (PCSK 9) has been shown to affect the LDL-C supply and has been identified to be a promising target in the treatment of hypercholesterolaemia. This article reviews preclinical data of PCSK9 vaccine candidates and presents potential clinical benefits and challenges in the development of PCSK9 vaccines extrapolated from experience with PCSK9 monoclonal antibodies (mAb).
2 Targeting Proprotein Convertase Subtilisin Kexin Type 9 (PCSK 9) in Hypercholesterolaemia
Circulating LDL-C gets primarily cleared by binding at the LDL receptor (LDLR) followed by hepatic internalization and subsequent LDL-C degradation (Fig. 1). After intracellular delivery of LDL-C particles, the LDLR recycles and returns to the cell surface with a physiological lifespan of up to 150 endocytosis series. PCSK 9, which is a key regulator of the LDLR supply in the cholesterol pathway, is a circulating serine protease synthesized in hepatocytes, enterocytes or kidney cells, and it has been shown that the majority of the secreted protease originates from liver tissue. Autocatalytic cleavage of a prodomain from its N-terminus prior to secretion induces activation of the protease. Active PCSK9 interacts with the extracellular LDLR domain and binding of PCSK9 induces endocytosis of the LDLR-PCSK9 complex followed by lysosomal degradation of both PCSK9 and the LDLR. This process results in decreased availability of LDLR on the extracellular surface of hepatocytes with attenuated hepatic LDL-C clearance and increased circulating plasma LDL-C [18,19,20,21,22,23,24]. Various genetic studies have shown that PCSK9 mutations affect LDL-C levels. Loss of function of PCSK9 lowers both LDL-C concentrations and the risk for CVD. Likewise, gain of function mutations in the PCSK9 gene are present in patients with familial hypercholesterolaemia (FH) who have a premature risk for cardiovascular events [25,26,27,28,29]. These observations have suggested that PCSK9 is a promising drug target for development of novel lipid-lowering medicines. Currently, there are two different therapeutic approaches under investigation to prevent PCSK9-mediated LDLR degradation: passive immunization by administration of mAb neutralizing PCSK9 and the formation of antibodies against PCSK9 by active vaccination with antigens with a homology to PCSK9.
Low-density lipoprotein (LDL) interaction with the LDL receptor (LDLR) and their trafficking in the absence (a) and the presence (b) of antibodies that neutralize proprotein convertase subtilisin kexin type 9 (PCSK 9). PCSK9 inhibitors prevent the LDLR from its lysosomal degradation. After Krähenbühl et al. [82]
3 Efficacy, Safety and Tolerability of PCSK9 Inhibitors
Table 1 summarizes agents against PCSK 9 for treatment of hypercholesterolaemia that are approved or are currently being evaluated in clinical trials. In 2015, alirocumab (Praluent®, Sanofi/ Regeneron) and evolocumab (Repatha®, Amgen), both fully human mAb that bind circulating PCSK9, received approval as adjunct therapy in combination with diet and maximally tolerated statin therapy by the European Commission (EC) and the US Food and Drug Administration (FDA) [30,31,32,33]. Another anti-PCSK9 agent (LY3015014, Lilly) and two PCSK9 candidate vaccines (AFFITOPE® AT04A and AT06A, AFFiRiS) are currently being evaluated in human trials. The global clinical development program for the humanized mAb bococizumab (Pfizer) was discontinued in 2016 due to its poor safety and efficacy profile in phase III trials [34,35,36,37].
3.1 Alirocumab
The half-life of subcutaneous (SC) alirocumab has been shown to be 14–21 days with maximum serum concentrations after 3–7 days. Its peak inhibitory effect on free PCSK9 is achieved within 4–8 h [38].
Alirocumab has been evaluated in numerous randomized controlled trials (RCTs) including adults with heterozygous FH and patients with CVD and/or intolerance to statins. The “Long-term Safety and Tolerability of Alirocumab in High Cardiovascular Risk Patients with Hypercholesterolemia Not Adequately Controlled with Their Lipid Modifying Therapy” (ODYSSEY LONG TERM) trial [39] was a key study for the efficacy and safety evaluation of alirocumab. This placebo-controlled randomized study evaluated the effect of 150 mg SC alirocumab every 2 weeks (Q2 W) on top of maximum tolerated statin therapy for 78 weeks in a population at high risk for CVD (n = 2341 patients). The primary efficacy endpoint, percentage change in calculated LDL-C levels at week 24, showed a 62% decrease versus placebo with a mean absolute LDL-C of 48 mg/dl (alirocumab) and 119 mg/dl (placebo), respectively. The treatment effect remained consistent over a period of 78 weeks, and approximately 80% of those receiving alirocumab achieved LDL-C target levels below 70 mg/dl (placebo: 8%). The anti-PCSK9 drug was well tolerated but higher numbers of specific adverse events (AEs) were reported in the alirocumab group than during placebo treatment with more injection site reactions (5.9 vs. 0.5%), myalgia (5.4 vs. 2.9%), neurocognitive impairment (1.2 vs. 0.5%) and ophthalmological events (2.9 vs. 1.9%).
Zhang et al. [40] pooled in a meta-analysis 13 trials (n = 5593 patients) that investigated alirocumab SC for 12 weeks at different doses compared to placebo or ezetimibe. Alirocumab 50–150 mg significantly reduced LDL-C levels versus placebo with greater mean reductions during bi-weekly dosing (− 53.6%; 95% confidence interval [CI] − 47.0 to − 58.2) than with 150–300 mg alirocumab every 4 weeks (Q4 W), which lowered LDL-C only by 32.2% (95% CI 15.6–48.7). Compared with ezetimibe (10 mg once daily), Q2 W dosing of 75–150 mg alirocumab reduced LDL-C by 29.9% (95% CI 26.9–32.9). Pooled safety data of these trials suggest that the rate of AEs was similar during alirocumab, placebo or ezetimibe treatment except for greater numbers of injection site reactions following alirocumab versus placebo (6.0 vs. 3.7%; P = 0.02). Importantly, the number of deaths was lower during alirocumab treatment compared to placebo (relative risk [RR] = 0.43; 95% CI 0.19–0.96; P = 0.04) but similar to that of observed with ezetimibe-treated patients (RR = 0.48; 95% CI 0.16–1.45; P = 0.19).
Post-hoc analysis of ODYSSEY LONG TERM data suggest that alirocumab compared with placebo may have beneficial effects on major cardiovascular events (MACE) due to a lower incidence in the composite of death from coronary heart disease, myocardial infarction, ischaemic stroke and unstable angina requiring hospitalization (1.7 vs. 3.3%, hazard ratio [HR]: 0.52, 95% CI 0.31–0.60, P = 0.02) [39]. A recent meta-analysis has suggested that alirocumab may reduce cardiac mortality (n = 4057 patients; RR = 0.36; 95% CI 0.14–0.93; P = 0.035) without positive effects on other cardiovascular events [41]. Cardiovascular benefits have also been suggested by a pooled post hoc analysis of ten ODYSSEY trials (n = 4974 patients) indicating that alirocumab may prevent MACE in a LDL-C concentration-dependent manner [42]. These findings could be confirmed in the recently completed ODYSSEY OUTCOMES trial that evaluated the effect of alirocumab on cardiovascular events over a period of 5 years in 18,924 patients. Alirocumab in addition to of maximally tolerated statin therapy reduced MACE by 15% (HR = 0.85; 95% CI 0.78–0.93; P = 0.0003) as compared to placebo, with a greater impact in patients with LDL-C ≥ 100 mg/dl at baseline (HR = 0.76; 95% CI 0.65–0.87). Anti-PCSK9 treatment also reduced all-cause mortality by 15% (HR = 0.85; 95% CI 0.73–0.98; P = 0.026) and post hoc analysis of subjects with higher baseline LDL-C showed a 29% risk reduction in death from any cause (HR = 0.71; 95% CI 0.56–0.90) [43, 44].
3.2 Evolocumab
Evolocumab SC exerts a half-life of 11–17 day and achieves peak plasma levels at day 3–4 after administration [45].
RCTs evaluating evolocumab comprised similar populations at risk to studies with alirocumab but also included subjects with homozygous FH [46, 47]. A major trial for the efficacy and safety of evolocumab was the Open-Label Study of Long-Term Evaluation Against LDL-cholesterol (OSLER) [48] that pooled data of 4,465 patients who participated previously in at least one of five phase 2 trials [49,50,51,52,53] (OSLER-1) or one of seven phase 3 studies [54,55,56,57,58,59] investigating evolocumab (OSLER-2). Subjects received SC either 140 mg Q2 W or 420 mg Q4 W of evolocumab combined with standard therapy or standard therapy alone over a median period of 11 months. Additive treatment with evolocumab lowered LDL-C levels from baseline concentrations of 120 mg/dl to 48 mg/dl at week 12 indicating a 61% relative and an absolute reduction of -73 mg/dl in LDL-C, respectively. Approximately 90% of patients during combined therapy achieved LDL-C levels of ≤ 100 mg/dl (standard care: 26%) and in 74% LDL-C levels of 70 mg/dl or less (standard therapy: 4%) were observed. Similar to alirocumab, the treatment effect was consistent over the follow-up period of 11 months. Rates of AEs or serious AEs were similar in both study cohorts. However, neurocognitive AEs, although rare (< 1%), were more frequent during evolocumab treatment [48]. In a smaller open-label OSLER-1 extension study (n = 1324 patients), evolocumab has been shown to be safe with sustained reductions in LDL-C over 4 years similar to levels observed in previous short-term studies. In addition, no neutralizing antibodies developed during the follow-up period [60]. However, two ongoing studies (NCT03080935, NCT02867813) including more than 6,600 patients and with a follow-up of 5 years have to be completed to provide more long-term safety and efficacy data.
A meta-analysis involving 12 trials with evolocumab versus placebo or ezetimibe (10 mg once daily) showed that all tested doses (420 mg Q4 W, 350 mg Q4 W, 280 mg Q4 W, 140 mg Q2 W, 105 mg Q2 W, 70 mg Q2 W) markedly reduced LDL-C levels after 3 months of administration [40]. Evolocumab 420 mg monthly or 140 mg bi-weekly compared to placebo induced the greatest reductions in LDL-C with − 54.6% (95% CI − 50.5 to 58.7 for 420 mg Q4 W) and − 60.4% (95% CI − 52.9 to − 68.8 for 140 mg Q2 W). Absolute LDL-C levels changed by approximately -80 mg/dl in both treatment regimens. As expected, compared to ezetimibe this effect was less pronounced with reductions of − 36.3% (95% CI − 33.9 to − 38.8) and − 38.2% (95% CI − 34.5 to − 41.5%) for evolocumab 420 mg monthly and 140 mg bi-weekly, respectively. Safety analyses of pooled data suggest that AEs and abnormal laboratory findings do not differ between evolocumab, ezetimibe or placebo.
A recently published network meta-analysis that directly compared evolocumab with alirocumab showed a greater LDL-C reduction in patients receiving evolocumab [61]. After 12 weeks and bi-weekly administration of 140 mg evolocumab or 75 mg alirocumab LDL-C differed by 20.0% (Credible interval [CrI]: 13.0–27.3). These differences were also detectable when compared with 150 mg alirocumab Q2 W (− 13.6%; CrI − 5.3 to − 22.4). After monthly dosing of evolocumab (420 mg) or alirocumab (300 mg), LDL-C levels were 19.2% (CrI 10.4–28.5) lower when evolocumab was administered. However, this has to be interpreted cautiously due to the limited quantity of data available. Further, no prospective studies have been performed comparing evolocumab with alirocumab. Likewise, a systematic review showed that most PCSK9 trials use lipid-lowering medicines (statins, ezetimibe) as background medication and that there is a lack of high-quality data for non-placebo comparators. Only seven RCTs were identified with other LDL-C reducing drugs as an active comparator. In these studies PCSK9 mAb appeared to be more efficient in preventing CVD (HR = 0.45; 95% CI 0.27–0.75) than in placebo-controlled trials. It has been suggested that this effect is likely due to the very low quality of statin/ezetimibe-controlled trials (small event numbers, short follow-up, lack of blinding) [62].
Exploratory prospective analysis of the composite of all cardiovascular events (death, myocardial infarction, hospitalization for unstable angina or heart failure, coronary vascularization, stroke or transient ischaemic attack) in the OSLER population at 1-year follow-up showed lower event numbers in patients receiving evolocumab + standard therapy as compared to standard care alone (0.95 vs. 2.18%; hazard ratio [HR]: 0.47; 95% CI 0.28–0.78; P = 0.003). A similar effect could also be detected in a post hoc analysis of MACE in this population [48]. The “Further Cardiovascular Outcome Research with PCSK9 Inhibition in Subjects with Elevated Risk” (FOURIER) trial included 27,456 patients receiving evolocumab (140 mg Q2 W or 420 mg Q4 W) with a follow-up period of 26 months [63]. FOURIER could confirm the cardiovascular benefit observed in the shorter term OSLER trial with a significantly reduced risk in both the primary composite of cardiovascular events defined as cardiovascular death, myocardial infarction, stroke, hospitalization for unstable angina or coronary intervention (HR: 0.85; 95% CI 0.79–0.92; P < 0.001) and the key secondary endpoint of cardiovascular death, myocardial infarction or stroke (HR: 0.80; 95% CI 0.73–0.88; P < 0.001). A prespecified secondary analysis of FOURIER data suggests an association between LDL-C levels achieved and the incidence of cardiovascular events [64].
The finding of a potential cardiovascular benefit of PCSK9 inhibition is supported by assessment of pooled data of more than 28,000 patients (including PCSK9 inhibitor-treated patients of FOURIER) from RCTs involving evolocumab [41]. This meta-analysis reported a positive effect of evolocumab on cardiovascular events as a composite of all-cause mortality, cardiac death, myocardial infarction, stroke, coronary revascularization or hospitalization due to unstable angina (RR = 0.86; 95% CI 0.80–0.92; P = 0.000). This was driven by a lower risk of myocardial infarction, coronary revascularization and stroke. However, due to a paucity of long-term data of PCSK9 inhibitors further clinical trials are needed to evaluate the impact of those agents on safety and efficacy.
3.3 Bococizumab
The humanized IgG2Δa mAb bococizumab was another anti-PCSK9 agent for treatment of hyperlipidaemia in clinical development. In four phase 1 studies (single dosing [n = 3], multiple dosing [n = 1]) in subjects with hypercholesterolaemia bococizumab intravenously (IV) and/ or SC administered at ascending doses was safe and well tolerated. Bococizumab showed a similar safety and tolerability profile to placebo and most AEs were mild and not related to the study drug. LDL-C reductions were dose-dependent and ranged from − 33 to − 84% with a more sustained LDL-C-lowering effect after IV administration as compared to equivalent SC doses [65].
A phase IIb trial over 24 weeks with 351 patients on stable statin therapy who were exposed to bococizumab SC (50 mg, 100 mg or 150 mg Q2 W; 200 mg or 300 mgQ4 W) or placebo confirmed safety and efficacy data from short-term phase I studies [66].
The “Studies of PCSK9 Inhibition and the Reduction of Vascular Events” (SPIRE) development program comprised more than 30.000 patients and consisted of six lipid-lowering studies (SPIRE-HR, SPIRE-LDL, SPIRE-FH, SPIRE-LL, SPIRE-SI, SPIRE-AI) and two large-scale trials to address potential cardiovascular benefits (SPIRE-1, SPIRE-2) of 150 mg bococizumab SC Q2 W [37]. Data from the six lipid-lowering trials showed bococizumab lowered LDL-C levels at 12 weeks by − 55% (95% CI − 53 to − 58, P < 0.001) versus placebo. However, at the 52-week follow-up visit the lipid-lowering effect was substantially attenuated − 45%; 95% CI − 38 to − 47) with inhomogeneous individual responses to bococizumab, and 48% of those who received anti-PCSK9 treatment developed antidrug antibodies (ADAs). Comparison of ADA titres and LDL-C suggest that the treatment response and plasma bococizumab concentrations changed titre-dependently. Further, MACE were similar in patients receiving bococizumab and placebo, respectively (HR = 0.96; CI 0.66–1.39; P = 0.83) [35]. In addition, no benefit of anti-PCSK9 treatment on clinical outcomes was observed in the assessment of the combined SPIRE-1 and SPIRE-2 data in patients at low and high risk, respectively. Subjects treated with bococizumab or placebo had a similar risk for MACE (HR = 0.88; 95% CI 0.76–1.02; P = 0.08) during 7 months (SPIRE-1) or 12 months (SPIRE-2) of follow-up. However, these non-significant findings should be interpreted with caution as neither of the two SPIRE trials had continued long enough to reach the prespecified number of MACE [36]. Although there was a significant clinical effect in the longer duration SPIRE-2 trial including patients at high-risk (HR for MACE = 0.79; 95% CI: 0.65–0.97; P = 0.02), the sponsor of the SPIRE trials terminated the program early due to an increased rate of immunogenicity of bococizumab and its high variability in lowering LDL-C [34,35,36,37].
3.4 Ly3015014
In preclinical studies the humanized IgG4 mAb LY3015014 (LY) has demonstrated a more sustained LDL-C lowering effect, which has been attributed to its binding site at PCSK9, which differs from other anti-PCSK9 agents. LY allows cleavage of active PCSK9 and thus prevents excessive accumulation of PCSK9 followed by a decreased LY clearance. It has been suggested that these properties might result in a more potent anti-PCSK9 agent requiring lower doses and/or extended dosing intervals, which may be of particular clinical interest [67, 68].
LY has been clinically evaluated in phase I and II trials in healthy subjects and in patients with hypercholesterolaemia [69, 70]. A double-blinded, randomized, placebo-controlled trial including 527 patients with hypercholesterolaemia with or without statin therapy assessed SC administered LY at different doses (20 mg, 120 mg or 300 mg) Q4 W, or 100 mg or 300 mg every 8 weeks (Q8 W) alternating with placebo Q4 W [70]. LDL-C levels changed dose dependently with maximum reductions at LY 300 mg Q4 W and Q8 W, respectively. Monthly dosing of LY 300 mg as compared with placebo reduced LDL-C at week 16 by − 62.8% (95% CI − 57.3 to − 68.3), while Q8 W administration caused a decrease by − 62.3% (95% CI − 57.4 to − 67.3). The short-term safety profile of LY was similar to other PCSK9 mAb. Injection site reactions and erythema were more frequent in LY treated patients than during placebo administration. The incidence of ADA was low in this short-term trial but if LY ADA play a pivotal role for clinical efficacy needs to be assessed in further trials [70].
4 Rationale for Active Immunization against PCSK9
The approved anti-PCSK9 mAbs alirocumab and evolocumab have shown a substantial reduction in LDL-C. Although results of longer-term studies suggest a decrease in mortality during combined statin treatment, it remains unclear if the observed LDL-C-lowering effect also translates into a protective cardiovascular effect during more extended follow-up periods in major clinical endpoint trials. The shortcomings of PCSK9 mAb such as high costs of approximately $14,000/year [71] or the possibility of ADA formation require efforts in the development of alternative, more efficient therapeutic strategies targeting the PCSK9 pathway that are different from passive immunization with mAb.
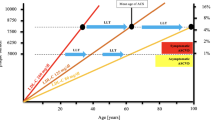
Due to a lack of prospective economic analysis in large RCTs available data on the cost-effectiveness of PCSK9 inhibitors are based on simulations. Hlatky et al. reviewed seven studies that involved different economic models for the assessment of PCSK9 mAb [71]. All evaluations reported independent from their assumptions a major increase in lifetime costs using PCSK9 mAb and projected only small savings due to prevention of cardiovascular events resulting in a lifetime incremental cost-effectiveness ratio (ICER) ranging from $141,700 to $450,000 per quality-adjusted life-year (QALY) compared to statins. Even with the most optimistic assumptions, the projected cost-effectiveness is approximately threefold higher than the threshold of an ICER/QALY (< $50.000) that is considered to provide a highly cost-effective drug [72]. Also we can only speculate on a price for PCSK9 vaccines; an active immunization followed by induction of antibodies against PCSK9 may be a promising alternative approach to overcome poor cost-effectiveness as vaccines are designed to achieve a similar response to administration of mAb but with less frequent applications.
Further, PCSK9 vaccines disperse the phenomenon of ADA induction that occurred during mAb treatment followed by a significant lack of responsiveness as observed in the majority of patients receiving bococizumab [35]. ADA may even occur when fully humanized mAb are administered as detected in a trial over 3 years involving adalimumab, a fully humanized TNF-α inhibitor. Patients who developed ADA had a poorer clinical response and a lower likelihood of clinical remission than patients without ADA [73]. In contrast, no neutralizing antibodies were reported during treatment with alirocumab or evolocumab, which are both fully human mAb [39, 63]. However, long-term immunogenicity studies with these medicines are not available yet and it remains uncertain if the development of ADA would not significantly affect the efficacy of these PCSK9 inhibitors during lifetime treatment, which is required in patients with hypercholesterolaemia.
To sum up, PCSK9 vaccines may circumvent the overt drawbacks of passive PCSK9 immunotherapy such frequent applications or development of ADA, and thus may result in improved efficacy.
5 PCSK9 Vaccines in Clinical Development and Pre-clinical Data
According to clinicaltrials.gov (search terms “PCSK9”, “vaccine”, “vaccination”) there is currently only one company (AFFiRiS, Austria) that is evaluating vaccines against peptides of PCSK9 in humans (NCT02508896). In this randomized, single-blind, placebo-controlled phase 1 study with 72 subjects (n = 24 per group), safety, immunogenicity and the LDL-C-lowering effect of one of two different PCSK9 vaccine candidates (AFFITOPE® AT04 or AT06) versus placebo was assessed. Subjects received three subcutaneous priming vaccinations at Q4 W intervals followed by a booster vaccination at 1 year after the last priming injection. The trial was completed in August 2017; however, results have not yet been published.
The candidate peptides AT04 and AT06 mimic structures of the N-terminus of the human mature PCSK9 and are similar to the target regions in rodents where these potential vaccines were pre-clinically assessed [74]. Primary immunization induced high-affine antibodies against both human and rodent PCSK9 with high titres reaching their peak levels at 6–10 weeks after the priming vaccination and remained significantly increased for up to 1 year. This indicates a sustained immunogenic effect with a half-life of approximately 4 months, which markedly exceeds the frequent dosing intervals of mAb against PCSK9. Likewise, LDL-C and total cholesterol decreased by − 50 and − 30%, respectively. A booster vaccination at 1 year after primary immunization reactivated PCSK9 antibody formation followed by the expected changes in lipid parameters. This study could also confirm the absence of a potential cross-reactivity of the candidate peptides against human structures, which would be a major limitation in the development of PCSK9 vaccines. To overcome cross-reactions with endogenous proteins other than the target structure, it is essential that the desired antigen for the development of a PCSK9 vaccine is almost identical to PCSK9 structures but differs to a small degree to induce an immunogenic response [75]. Another potential limitation of vaccines to self-antigens such as PCSK9 is the formation of autoreactive T cells against human tissue that have been shown to be potentially life threatening [76]. CD4+ T helper cells need to be presented to foreign epitopes for an effective activation and these stimulated T cells are required to assist B cells to induce an efficient antibody formation [77]. To prevent the induction of a target-specific T-cell response, the developer coupled their short peptide vaccine candidates to a foreign carrier protein (keyhole limpet haemocyanin; KLH, which acted as source for T-cell epitopes without accumulating autoreactive T cells [74].
Another approach for an active PCSK9 vaccination is the presentation of epitopes derived from PCSK9 on the surface of virus-like particles (VLP). Animal data suggest an effective lipid-lowering effect after VLP vaccination in mice and macaques [78]. However, a PCSK9-VLP vaccination has not been clinically evaluated. Table 2 summarizes pre-clinical studies involving active immunization against PCSK9.
In conclusion, the development of PCSK9 vaccines is in an early clinical stage and data from human trials are not yet available. However, pre-clinical data suggest an effective attenuation of plasma lipids with a decrease of atherosclerotic lesions, and a reduction of vascular and systemic inflammation [79]. Challenges in the development of effective and safe vaccines against PCSK9 include the identification of protein structures of the endogenous target with sufficient homology for the formation of highly specific antibodies at high titres. An increased half-life of vaccine-induced antibodies at a lower dose injected as compared to passive immunization of PCSK9 mAb would suggest PCSK9 vaccines as a cost-effective treatment alternative. Further, the induction of an autoreactive T-cell response needs to be prevented that such vaccines can be considered as a safe therapeutic approach for treatment of patients with hypercholesterolaemia.
References
Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133:e38–360.
Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet. 1994;344:1383–9.
Heart Protection Study Collaborative G. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360:7–22.
Athyros VG, Papageorgiou AA, Mercouris BR, et al. Treatment with atorvastatin to the National Cholesterol Educational Program goal versus ‘usual’ care in secondary coronary heart disease prevention. The GREek Atorvastatin and Coronary-heart-disease Evaluation (GREACE) study. Curr Med Res Opin. 2002;18:220–8.
Baigent C, Blackwell L, Emberson J, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376:1670–81.
Jacobson TA, Maki KC, Orringer CE, et al. National lipid association recommendations for patient—centered management of dyslipidemia: part 2. J Clin Lipidol. 2015;9(S1–122):e121.
Lin L, Teng M, Zhao YJ, et al. Long-term cost-effectiveness of statin treatment for primary prevention of cardiovascular disease in the elderly. Cardiovasc Drugs Ther. 2015;29:187–97.
Braamskamp M, Langslet G, McCrindle BW, et al. Efficacy and safety of rosuvastatin therapy in children and adolescents with familial hypercholesterolemia: Results from the CHARON study. J Clin Lipidol. 2015;9:741–50.
Raal FJ, Pappu AS, Illingworth DR, et al. Inhibition of cholesterol synthesis by atorvastatin in homozygous familial hypercholesterolaemia. Atherosclerosis. 2000;150:421–8.
Langslet G, Breazna A, Drogari E. A 3-year study of atorvastatin in children and adolescents with heterozygous familial hypercholesterolemia. J Clin Lipidol. 2016;10(1153–1162):e1153.
Bruckert E, Hayem G, Dejager S, et al. Mild to moderate muscular symptoms with high-dosage statin therapy in hyperlipidemic patients—the PRIMO study. Cardiovasc Drugs Ther. 2005;19:403–14.
Silva M, Matthews ML, Jarvis C, et al. Meta-analysis of drug-induced adverse events associated with intensive-dose statin therapy. Clin Ther. 2007;29:253–60.
Cohen JD, Brinton EA, Ito MK, et al. Understanding Statin Use in America and Gaps in Patient Education (USAGE): an internet-based survey of 10,138 current and former statin users. J Clin Lipidol. 2012;6:208–15.
Cheetham TC, Niu F, Green K, et al. Primary nonadherence to statin medications in a managed care organization. J Manag Care Pharm. 2013;19:367–73.
Jackevicius CA, Mamdani M, Tu JV. Adherence with statin therapy in elderly patients with and without acute coronary syndromes. JAMA. 2002;288:462–7.
Bellosta S, Corsini A. Statin drug interactions and related adverse reactions: an update. Expert Opin Drug Saf. 2018;17:25–37.
Karr S. Epidemiology and management of hyperlipidemia. Am J Manag Care. 2017;23:S139–48.
Horton JD, Cohen JC, Hobbs HH. PCSK9: a convertase that coordinates LDL catabolism. J Lipid Res. 2009;50(Suppl):S172–7.
Peterson AS, Fong LG, Young SG. PCSK9 function and physiology. J Lipid Res. 2008;49:1595–9.
Rashid S, Curtis DE, Garuti R, et al. Decreased plasma cholesterol and hypersensitivity to statins in mice lacking Pcsk9. Proc Natl Acad Sci USA. 2005;102:5374–9.
Maxwell KN, Fisher EA, Breslow JL. Overexpression of PCSK9 accelerates the degradation of the LDLR in a post-endoplasmic reticulum compartment. Proc Natl Acad Sci USA. 2005;102:2069–74.
Luo Y, Warren L, Xia D, et al. Function and distribution of circulating human PCSK9 expressed extrahepatically in transgenic mice. J Lipid Res. 2009;50:1581–8.
Zaid A, Roubtsova A, Essalmani R, et al. Proprotein convertase subtilisin/kexin type 9 (PCSK9): hepatocyte-specific low-density lipoprotein receptor degradation and critical role in mouse liver regeneration. Hepatology. 2008;48:646–54.
Grefhorst A, McNutt MC, Lagace TA, et al. Plasma PCSK9 preferentially reduces liver LDL receptors in mice. J Lipid Res. 2008;49:1303–11.
Cohen JC, Boerwinkle E, Mosley TH Jr, et al. Sequence variations in PCSK9, low LDL, and protection against coronary heart disease. N Engl J Med. 2006;354:1264–72.
Kotowski IK, Pertsemlidis A, Luke A, et al. A spectrum of PCSK9 alleles contributes to plasma levels of low-density lipoprotein cholesterol. Am J Hum Genet. 2006;78:410–22.
Cohen J, Pertsemlidis A, Kotowski IK, et al. Low LDL cholesterol in individuals of African descent resulting from frequent nonsense mutations in PCSK9. Nat Genet. 2005;37:161–5.
Cunningham D, Danley DE, Geoghegan KF, et al. Structural and biophysical studies of PCSK9 and its mutants linked to familial hypercholesterolemia. Nat Struct Mol Biol. 2007;14:413–9.
Abifadel M, Varret M, Rabes JP, et al. Mutations in PCSK9 cause autosomal dominant hypercholesterolemia. Nat Genet. 2003;34:154–6.
Food and Drug Administration. Praluent Alirocumab. 2015.https://www.accessdata.fda.gov/drugsatfda_docs/nda/2015/125559Orig1s000TOC.cfm. Accessed 18 Jan 2018.
European Medicines Agency. Praluent Alirocumab. 2015. http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/003882/human_med_001915.jsp&mid=WC0b01ac058001d124. Accessed 18 Jan 2018.
Food and Drug Administration. Repatha Evolocumab. 2015. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/125522s000lbl.pdf. Accessed 18 Jan 2018.
European Medicines Agency. Repatha Alirocumab. 2015. http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/003766/human_med_001890.jsp&mid=WC0b01ac058001d124. Accessed 18 Jan 2018.
Pfizer. Pfizer discontinues global development of bococizumab, its investigational PCSK9 inhibitor. 2016. http://www.pfizer.com/news/press-release/press-release-detail/pfizer_discontinues_global_development_of_bococizumab_its_investigational_pcsk9_inhibitor. Accessed 14 Dec 2017.
Ridker PM, Tardif JC, Amarenco P, et al. Lipid-reduction variability and antidrug-antibody formation with bococizumab. N Engl J Med. 2017;376:1517–26.
Ridker PM, Revkin J, Amarenco P, et al. Cardiovascular efficacy and safety of bococizumab in high-risk patients. N Engl J Med. 2017;376:1527–39.
Ridker PM, Amarenco P, Brunell R, et al. Evaluating bococizumab, a monoclonal antibody to PCSK9, on lipid levels and clinical events in broad patient groups with and without prior cardiovascular events: Rationale and design of the Studies of PCSK9 Inhibition and the Reduction of vascular Events (SPIRE) Lipid Lowering and SPIRE Cardiovascular Outcomes Trials. Am Heart J. 2016;178:135–44.
Manniello M, Pisano M. Alirocumab (Praluent): first in the new class of PCSK9 inhibitors. P T. 2016;41:28–53.
Robinson JG, Farnier M, Krempf M, et al. Efficacy and safety of alirocumab in reducing lipids and cardiovascular events. N Engl J Med. 2015;372:1489–99.
Zhang XL, Zhu QQ, Zhu L, et al. Safety and efficacy of anti-PCSK9 antibodies: a meta-analysis of 25 randomized, controlled trials. BMC Med. 2015;13:123.
Zhu Y, Shen X, Jiang Q, et al. Effects of monoclonal antibodies against PCSK9 on clinical cardiovascular events: a meta-analysis of randomized controlled trials. Herz. 2017. https://doi.org/10.1007/s00059-017-4640-8.
Ray KK, Ginsberg HN, Davidson MH, et al. Reductions in atherogenic lipids and major cardiovascular events: a pooled analysis of 10 odyssey trials comparing alirocumab with control. Circulation. 2016;134:1931–43.
Schwartz GG, Bessac L, Berdan LG, et al. Effect of alirocumab, a monoclonal antibody to PCSK9, on long-term cardiovascular outcomes following acute coronary syndromes: rationale and design of the ODYSSEY outcomes trial. Am Heart J. 2014;168:682–9.
Sanofi. Praluent® (alirocumab) significantly reduced risk of cardiovascular events in high-risk patients, and was associated with lower death rate 2018. http://mediaroom.sanofi.com/praluent-alirocumab-significantly-reduced-risk-of-cardiovascular-events-in-high-risk-patients-and-was-associated-with-lower-death-rate/. Accessed 29 Mar 2018.
European Medicines Agency. Product information—Repatha. 2015. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/003766/WC500191398.pdf. Accessed 18 Jan 2018.
Raal FJ, Honarpour N, Blom DJ, et al. Inhibition of PCSK9 with evolocumab in homozygous familial hypercholesterolaemia (TESLA Part B): a randomised, double-blind, placebo-controlled trial. Lancet. 2015;385:341–50.
Stein EA, Honarpour N, Wasserman SM, et al. Effect of the proprotein convertase subtilisin/kexin 9 monoclonal antibody, AMG 145, in homozygous familial hypercholesterolemia. Circulation. 2013;128:2113–20.
Sabatine MS, Giugliano RP, Wiviott SD, et al. Efficacy and safety of evolocumab in reducing lipids and cardiovascular events. N Engl J Med. 2015;372:1500–9.
Giugliano RP, Desai NR, Kohli P, et al. Efficacy, safety, and tolerability of a monoclonal antibody to proprotein convertase subtilisin/kexin type 9 in combination with a statin in patients with hypercholesterolaemia (LAPLACE-TIMI 57): a randomised, placebo-controlled, dose-ranging, phase 2 study. Lancet. 2012;380:2007–17.
Koren MJ, Scott R, Kim JB, et al. Efficacy, safety, and tolerability of a monoclonal antibody to proprotein convertase subtilisin/kexin type 9 as monotherapy in patients with hypercholesterolaemia (MENDEL): a randomised, double-blind, placebo-controlled, phase 2 study. Lancet. 2012;380:1995–2006.
Raal F, Scott R, Somaratne R, et al. Low-density lipoprotein cholesterol-lowering effects of AMG 145, a monoclonal antibody to proprotein convertase subtilisin/kexin type 9 serine protease in patients with heterozygous familial hypercholesterolemia: the Reduction of LDL-C with PCSK9 Inhibition in Heterozygous Familial Hypercholesterolemia Disorder (RUTHERFORD) randomized trial. Circulation. 2012;126:2408–17.
Sullivan D, Olsson AG, Scott R, et al. Effect of a monoclonal antibody to PCSK9 on low-density lipoprotein cholesterol levels in statin-intolerant patients: the GAUSS randomized trial. JAMA. 2012;308:2497–506.
Hirayama A, Honarpour N, Yoshida M, et al. Effects of evolocumab (AMG 145), a monoclonal antibody to PCSK9, in hypercholesterolemic, statin-treated Japanese patients at high cardiovascular risk–primary results from the phase 2 YUKAWA study. Circ J. 2014;78:1073–82.
Blom DJ, Hala T, Bolognese M, et al. A 52-week placebo-controlled trial of evolocumab in hyperlipidemia. N Engl J Med. 2014;370:1809–19.
Robinson JG, Nedergaard BS, Rogers WJ, et al. Effect of evolocumab or ezetimibe added to moderate- or high-intensity statin therapy on LDL-C lowering in patients with hypercholesterolemia: the LAPLACE-2 randomized clinical trial. JAMA. 2014;311:1870–82.
Koren MJ, Lundqvist P, Bolognese M, et al. Anti-PCSK9 monotherapy for hypercholesterolemia: the MENDEL-2 randomized, controlled phase III clinical trial of evolocumab. J Am Coll Cardiol. 2014;63:2531–40.
Stroes E, Colquhoun D, Sullivan D, et al. Anti-PCSK9 antibody effectively lowers cholesterol in patients with statin intolerance: the GAUSS-2 randomized, placebo-controlled phase 3 clinical trial of evolocumab. J Am Coll Cardiol. 2014;63:2541–8.
Raal FJ, Stein EA, Dufour R, et al. PCSK9 inhibition with evolocumab (AMG 145) in heterozygous familial hypercholesterolaemia (RUTHERFORD-2): a randomised, double-blind, placebo-controlled trial. Lancet. 2015;385:331–40.
Dent R, Joshi R, Stephen Djedjos C, et al. Evolocumab lowers LDL-C safely and effectively when self-administered in the at-home setting. Springerplus. 2016;5:300.
Koren MJ, Sabatine MS, Giugliano RP, et al. Long-term Low-Density Lipoprotein Cholesterol-Lowering Efficacy, Persistence, and Safety of Evolocumab in Treatment of Hypercholesterolemia: Results Up to 4 Years From the Open-Label OSLER-1 Extension Study. JAMA Cardiol. 2017;2:598–607.
Toth PP, Worthy G, Gandra SR, et al. Systematic review and network meta-analysis on the efficacy of evolocumab and other therapies for the management of lipid levels in hyperlipidemia. J Am Heart Assoc 2017;6(10). https://doi.org/10.1161/JAHA.116.005367.
Schmidt AF, Pearce LS, Wilkins JT, et al. Cochrane corner: PCSK9 monoclonal antibodies for the primary and secondary prevention of cardiovascular disease. Heart. 2018. https://doi.org/10.1136/heartjnl-2017-312858.
Sabatine MS, Giugliano RP, Pedersen TR. Evolocumab in patients with cardiovascular disease. N Engl J Med. 2017;377:787–8.
Giugliano RP, Pedersen TR, Park JG, et al. Clinical efficacy and safety of achieving very low LDL-cholesterol concentrations with the PCSK9 inhibitor evolocumab: a prespecified secondary analysis of the FOURIER trial. Lancet. 2017;390:1962–71.
Gumbiner B, Joh T, Liang H, et al. The effects of single- and multiple-dose administration of bococizumab (RN316/PF-04950615), a humanized IgG2Deltaa monoclonal antibody binding proprotein convertase subtilisin/kexin type 9, in hypercholesterolemic subjects treated with and without atorvastatin: Results from four phase I studies. Cardiovasc Ther. 2018. https://doi.org/10.1111/1755-5922.12309.
Ballantyne CM, Neutel J, Cropp A, et al. Results of bococizumab, a monoclonal antibody against proprotein convertase subtilisin/kexin type 9, from a randomized, placebo-controlled, dose-ranging study in statin-treated subjects with hypercholesterolemia. Am J Cardiol. 2015;115:1212–21.
Schroeder KM, Beyer TP, Hansen RJ, et al. Proteolytic cleavage of antigen extends the durability of an anti-PCSK9 monoclonal antibody. J Lipid Res. 2015;56:2124–32.
Hansen RJ, Berna MJ, Sperry AE, et al. Quantitative characterization of the mechanism of action and impact of a ‘proteolysis-permitting’ anti-PCSK9 antibody. MAbs. 2017;9:285–96.
Shen T, James DE, Krueger KA. Population Pharmacokinetics (PK) and Pharmacodynamics (PD) Analysis of LY3015014, a Monoclonal Antibody to Protein Convertase Subtilisin/Kexin Type 9 (PCSK9) in Healthy Subjects and Hypercholesterolemia Patients. Pharm Res. 2017;34:185–92.
Kastelein JJ, Nissen SE, Rader DJ, et al. Safety and efficacy of LY3015014, a monoclonal antibody to proprotein convertase subtilisin/kexin type 9 (PCSK9): a randomized, placebo-controlled Phase 2 study. Eur Heart J. 2016;37:1360–9.
Hlatky MA, Kazi DS. PCSK9 inhibitors: economics and policy. J Am Coll Cardiol. 2017;70:2677–87.
Anderson JL, Heidenreich PA, Barnett PG, et al. ACC/AHA statement on cost/value methodology in clinical practice guidelines and performance measures: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures and Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2304–22.
Bartelds GM, Krieckaert CL, Nurmohamed MT, et al. Development of antidrug antibodies against adalimumab and association with disease activity and treatment failure during long-term follow-up. JAMA. 2011;305:1460–8.
Galabova G, Brunner S, Winsauer G, et al. Peptide-based anti-PCSK9 vaccines—an approach for long-term LDLc management. PLoS One. 2014;9:e114469.
Schneeberger A, Mandler M, Otawa O, et al. Development of AFFITOPE vaccines for Alzheimer’s disease (AD)—from concept to clinical testing. J Nutr Health Aging. 2009;13:264–7.
Ferrer I, Boada Rovira M, Sanchez Guerra ML, et al. Neuropathology and pathogenesis of encephalitis following amyloid-beta immunization in Alzheimer’s disease. Brain Pathol. 2004;14:11–20.
Chackerian B, Durfee MR, Schiller JT. Virus-like display of a neo-self antigen reverses B cell anergy in a B cell receptor transgenic mouse model. J Immunol. 2008;180:5816–25.
Crossey E, Amar MJ, Sampson M, et al. A cholesterol-lowering VLP vaccine that targets PCSK9. Vaccine. 2015;33:5747–55.
Landlinger C, Pouwer MG, Juno C, et al. The AT04A vaccine against proprotein convertase subtilisin/kexin type 9 reduces total cholesterol, vascular inflammation, and atherosclerosis in APOE*3Leiden.CETP mice. Eur Heart J. 2017;38:2499–507.
Pan Y, Zhou Y, Wu H, et al. A therapeutic peptide vaccine against PCSK9. Sci Rep. 2017;7:12534.
Kawakami R, Nozato Y, Nakagami H, et al. Development of vaccine for dyslipidemia targeted to a proprotein convertase subtilisin/kexin type 9 (PCSK9) epitope in mice. PLoS One. 2018;13:e0191895.
Krähenbühl S, Pavik-Mezzour I, von Eckardstein A. Unmet needs in LDL-C lowering: when statins won’t do! Drugs. 2016;76:1175–90.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this manuscript.
Conflict of interest
Stefan Weisshaar and Markus Zeitlinger declare that they have no conflicts of interest that might be relevant to the contents of this manuscript.
Rights and permissions
About this article
Cite this article
Weisshaar, S., Zeitlinger, M. Vaccines Targeting PCSK9: A Promising Alternative to Passive Immunization with Monoclonal Antibodies in the Management of Hyperlipidaemia?. Drugs 78, 799–808 (2018). https://doi.org/10.1007/s40265-018-0915-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-018-0915-5