Abstract
Pemafibrate (Parmodia®) is a novel, highly selective peroxisome proliferator-activated receptor (PPAR)-α modulator (SPPARM). It acts by binding to PPAR-α and regulating the expression of target genes that modulate lipid metabolism, thereby decreasing plasma triglyceride levels and increasing high-density lipoprotein cholesterol levels. Developed by Kowa Company, Ltd., oral pemafibrate has been approved in Japan for the treatment of hyperlipidaemia (including familial hyperlipidaemia). This article summarizes the milestones in the development of pemafibrate leading to this first global approval for hyperlipidaemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
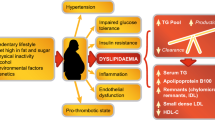
Pemafibrate (Parmodia®) is an oral peroxisome proliferator-activated receptor (PPAR)-α agonist developed by Kowa Company, Ltd. for the treatment of hyperlipidaemia [1]. PPAR-α, a transcription factor belonging to the nuclear receptor superfamily, controls hepatic lipid flux and improves plasma lipid profiles [2]. PPAR-α is predominantly expressed in the liver, and serves as a molecular target for hypolipidaemic fibrate drugs. Fibrates such as bezafibrate, fenofibrate and gemfibrozil are relatively weak PPAR-α agonists with poor substrate selectivity. Pemafibrate is a novel, highly selective PPAR-α modulator (SPPARM) with potent PPAR-α agonist activity [2].
On 3 July 2017, pemafibrate received its first global approval, in Japan, for the treatment of hyperlipidaemia (including familial hyperlipidaemia) [1, 3]. The recommended dosage of oral pemafibrate is 0.1 mg twice daily (administered in the morning and evening); this dosage can be adjusted according to age and symptoms to a maximum dosage of 0.2 mg twice daily [1].
Pemafibrate is undergoing phase III development in a number of countries for the treatment of dyslipidaemias and is also in phase III development for the treatment of hypertriglyceridaemia.
2 Scientific Summary
2.1 Pharmacodynamics
Selective binding of pemafibrate to PPAR-α regulates the expression of target genes, thereby decreasing plasma triglyceride levels and increasing high-density lipoprotein (HDL) cholesterol levels [1]. In cell-based transactivation assays, pemafibrate activated PPAR-α dose-dependently and more effectively than fenofibrate and pirinixic acid (Wy14643) [2, 4]. Pemafibrate was > 2000-fold more selective for PPAR-α than for PPAR-γ and PPAR-δ [4]. In primary human hepatocytes and the mouse liver, pemafibrate regulated the expression of several target genes that code for proteins involved in carbohydrate and lipid metabolism [4].
Studies in rat models showed that pemafibrate suppressed triglyceride synthesis in the liver, reduced the triglyceride secretion rate, increased lipoprotein lipase (LPL) activity, increased plasma triglyceride clearance and increased plasma levels of fibroblast growth factor (FGF)-21 [1]. Pemafibrate dose-dependently reduced plasma triglyceride levels and increased plasma HDL cholesterol and apolipoprotein (Apo) A-I levels [1]. Low doses of pemafibrate were associated with greater lipid-lowering effects than 200-fold higher doses of fenofibrate [2]. Pemafibrate also decreased plasma concentrations of ApoC-III and angiopoietin-like protein-3, both of which negatively regulate LPL activity [1].

Clinical development of pemafibrate for the treatment of dyslipidaemia
In mice, pemafibrate significantly reduced plasma triglyceride and total cholesterol levels, increased plasma HDL cholesterol levels, regulated gene expression related to triglyceride and HDL cholesterol metabolism in the liver, and regulated cholesterol and triglyceride metabolic gene expression in the small intestine [5]. Pemafibrate also promoted cholesterol efflux and reverse cholesterol transport, exerted anti-inflammatory activity, and decreased atherosclerotic lesions [6]. Pemafibrate was more effective than fenofibrate at suppressing the postprandial increase of chylomicrons and the accumulation of chylomicron remnants, thereby attenuating postprandial hypertriglyceridaemia [7].
In dyslipidaemic patients with high fasting triglyceride levels (150 to < 400 mg/dL) and low HDL cholesterol levels (< 50 mg/dL in males, < 55 mg/dL in females), pemafibrate was associated with significant (p < 0.01) reductions in fasting and postprandial levels of triglycerides, total cholesterol, ApoB-48, remnant lipoprotein cholesterol and free fatty acids compared with placebo [8]. Before treatment, peak concentration time of triglycerides, ApoB-48 and remnant lipoprotein cholesterol was delayed and observed at 4.5 h post-food loading, with suppression of peak concentration time after pemafibrate treatment. Compared with placebo, pemafibrate significantly (p < 0.01) increased fasting and postprandial FGF-21 levels [8]. Pemafibrate stimulated cholesterol efflux capacity to a significantly (p = 0.049) greater extent than placebo, accompanied by significant (p < 0.01) increases in Apo-AI, HDL3 cholesterol and preβ1-HDL cholesterol [9].
2.2 Pharmacokinetics
When a single dose of pemafibrate 0.1 mg was administered to healthy subjects with food or in the fasting state, the geometric mean ratios of maximum plasma concentration and area under the concentration–time curve from time zero to time τ were 0.873 ng/mL (90% CI 0.803–0.950) and 0.911 ng · h/mL (90% CI 0.863–0.961) [1]. Steady state concentrations were reached on day 2 of repeated administration, and the absolute oral bioavailability was 61.5%. Pemafibrate is highly (≥ 99%) bound to plasma proteins. Pemafibrate is metabolized to benzyl oxidized oxidant and a mixture of glucuronic acid conjugate and N-dealkylated dicarboxylic acid. Following the administration of radiolabelled pemafibrate in healthy subjects, 14.5% of the radioactivity was recovered in the urine and 73.3% was recovered in the faeces within 216 h [1].

Chemical structure of pemafibrate
In vitro, pemafibrate was a substrate of CYP2C8, CYP2C9, CYP3A4, CYP3A7, UGT1A1, UGT1A3 and UGT1A8 [1]. In addition, pemafibrate was a substrate of several efflux and uptake transporters (e.g. P-glycoprotein, BCRP, OATP1A2, OATP1B1, OATP1B3, OCT2 and NTCP). Coadministration of pemafibrate with ciclosporin or rifampicin is contraindicated. Caution is advised when pemafibrate is co-administered with cholestyramine, colestimide, clopidogrel, clarithromycin, HIV protease inhibitors (e.g. ritonavir), fluconazole or strong inducers of CYP3A (e.g. carbamazepine, phenobarbital, phenytoin, St. John’s Wort) [1].
Exposure to pemafibrate increased in patients with mild (Child–Pugh classification A) or moderate (Child–Pugh classification B) cirrhosis and in patients with fatty liver, relative to patients with normal liver function [1]. Similarly, relative to subjects with normal renal function, exposure to pemafibrate increased in subjects with mild [creatinine clearance (CLCR) 50 to < 80 mL/min], moderate (CLCR 30 to < 50 mL/min) or high-grade (CLCR < 30 mL/min) renal dysfunction or end-stage renal failure. However, the increase was not dependent on the extent of renal dysfunction [1].
Features and properties of pemafibrate
Alternative names | Parmodia; K877 |
Class | Antihyperlipidaemics; benzoxazoles; butyric acids |
Mechanism of action | PPAR-α agonist |
Route of administration | Oral |
Pharmacodynamics | Selectively binds to PPAR-α and regulates expression of target genes, thereby decreasing plasma TG levels and increasing HDL-C levels |
Pharmacokinetics | Steady state plasma concentrations reached on day 2 of repeated administration; absolute bioavailability 61.5%; human plasma protein binding ratio ≥ 99% |
Most common adverse events | Cholelithiasis, diabetes mellitus, increased creatine kinase |
ATC codes | |
WHO ATC code | C10 (lipid-modifying agents) |
EphMRA ATC code | C10 (lipid-regulating/anti-atheroma preparations) |
Chemical name | (2R)-2-[3-[[1,3-benzoxazol-2-yl-[3-(4-methoxyphenoxy)propyl]amino]methyl]phenoxy]butanoic acid |
2.3 Therapeutic Trials
2.3.1 Phase III
2.3.1.1 Monotherapy
In a randomized, double-blind trial (JapicCTI-142412), pemafibrate significantly improved dyslipidaemia in both fasting and postprandial states in 167 patients with high triglyceride levels (150 to < 1000 mg/dL) and type 2 diabetes mellitus [10]. Relative to placebo, treatment with pemafibrate 0.2 or 0.4 mg/day for 24 weeks significantly (p < 0.001) reduced fasting triglyceride levels (− 44.3 and − 45.1 vs. − 10.8%) and remnant lipoprotein cholesterol levels (− 49.1 and − 48.3 vs. + 1.1%). The proportion of patients with triglyceride levels of < 150 mg/dL was 81.5% in the pemafibrate 0.2 mg/day group and 70.9% in the 0.4 mg/day group, compared with 15.8% in the placebo group. Pemafibrate significantly (p < 0.001) ameliorated postprandial hyperlipidaemia without affecting postprandial plasma glucose and insulin [10].
In a long-term study (JapicCTI-142496), 189 patients with high triglyceride levels were treated with pemafibrate 0.2 mg/day for 52 weeks; the dosage could be increased to 0.4 mg/day after 12 weeks if the treatment goal had not been reached [1]. The change from baseline in fasting serum triglyceride level was − 48.8% at week 24 and − 45.9% at week 52. The low-density lipoprotein (LDL) cholesterol level was reduced from 119.3 mg/dL at baseline to 116.6 mg/dL at week 52 [1].
Two randomized, double-blind, multicentre trials compared the efficacy of pemafibrate with that of fenofibrate in dyslipidaemic patients with high triglyceride levels and low HDL cholesterol levels [1, 11]. In one trial (JapicCTI-121764), 526 patients with fasting hypertriglyceridaemia (200 to < 1000 mg/dL) received pemafibrate 0.1, 0.2 or 0.4 mg/day, fenofibrate 100 or 200 mg/day or placebo for 12 weeks [11]. The reductions in fasting triglyceride levels from baseline (primary endpoint) were significantly greater in the pemafibrate 0.1, 0.2 and 0.4 mg/day groups (− 46.3, − 46.7 and − 51.8%) compared with placebo (− 2.7%) and fenofibrate 100 mg/day (− 38.3%), but not fenofibrate 200 mg/day (– 51.5%). Pemafibrate improved HDL cholesterol, very low-density lipoprotein (VLDL) cholesterol, remnant lipoprotein cholesterol and ApoC-III levels [11]. Compared with fenofibrate, pemafibrate shifted the HDL composition to smaller and cholesterol-rich particles [12].
In the other trial (JapicCTI-142620), 223 patients received pemafibrate 0.2 or 0.4 mg/day or fenofibrate 106.6 mg/day for 24 weeks [1]. The change from baseline in fasting serum triglyceride levels at week 24 was − 46.3% in the pemafibrate 0.2 mg/day group, − 45.8% in the 0.4 mg/day group and − 39.7% in the fenofibrate group. Non-inferiority of pemafibrate to fenofibrate was demonstrated (non-inferiority margin of 10%) [1].
2.3.1.2 Add-on therapy
Two randomized, double-blind, multicentre trials demonstrated that when administered as add-on therapy to a statin, pemafibrate was associated with significantly greater reductions in fasting triglyceride levels than statin monotherapy (placebo) in patients with residual hypertriglyceridaemia [13]. The primary endpoint of both studies was the percent change in fasting triglycerides from baseline [13].
The first trial (JapicCTI-121837) enrolled 188 dyslipidaemic patients with fasting triglyceride levels of ≥ 200 mg/dL and non-HDL cholesterol levels of ≥ 150 mg/dL [13]. They received placebo or pemafibrate 0.1, 0.2 or 0.4 mg/day, each in combination with pitavastatin. The reductions in fasting triglyceride levels from baseline to week 12 were significantly (p < 0.001) greater with pemafibrate 0.1, 0.2 and 0.4 mg/day plus pitavastatin (− 46.1, − 53.4 and − 52.0%) than with pitavastatin alone (− 6.9%). Reductions in remnant lipoprotein cholesterol, triglycerides/HDL cholesterol, ApoB-48 and ApoC-III were also significantly (p < 0.001) greater in the pemafibrate groups than in the placebo group. Increases in HDL cholesterol, ApoA-II and FGF-21 were significantly (p < 0.05) greater with pemafibrate compared with placebo [13].
In the second trial (JapicCTI-132067), 423 dyslipidaemic patients with fasting triglyceride levels of ≥ 200 mg/dL received placebo or pemafibrate 0.2 mg/day (either as a fixed dose, or up-titrated to 0.4 mg/day after week 12 if fasting triglyceride levels were ≥ 150 mg/dL at week 8) [13]. All patients received a statin (most commonly atorvastatin, pitavastatin or rosuvastatin). At week 24, fasting triglyceride levels were reduced from baseline to a significantly (p < 0.001) greater extent in both pemafibrate plus statin groups (− 46.8 and − 50.8%) compared with a statin alone (− 0.8%). Reductions in non-HDL cholesterol, triglycerides/HDL cholesterol, ApoB, ApoC-III and ApoB/A-I were also significantly (p < 0.05) greater with pemafibrate than with placebo. Increases in HDL cholesterol, ApoA-I and ApoA-II were significantly (p < 0.001) greater in the pemafibrate groups than in the placebo group [13].
2.3.2 Phase II
Pemafibrate significantly reduced triglyceride levels in patients with dyslipidaemia whose LDL cholesterol levels were adequately controlled with atorvastatin, rosuvastatin or simvastatin (EudraCT2013-001517-32) [14]. This randomized, double-blind, multicentre trial enrolled 408 patients with baseline triglyceride levels of 175–500 mg/dL and low HDL cholesterol levels (≤ 50 mg/dL in males, ≤ 55 mg/dL in females). They received pemafibrate 0.05 mg twice daily, 0.1 mg twice daily, 0.2 mg twice daily, 0.1 mg once daily, 0.2 mg once daily or 0.4 mg once daily or placebo for 12 weeks. Pemafibrate significantly reduced triglyceride levels by 34.0–54.4% and non-HDL cholesterol levels by 7.8–9.1% (primary endpoints; p-values not stated). Pemafibrate also significantly reduced remnant cholesterol and ApoC-III levels. HDL cholesterol was significantly increased in all pemafibrate groups except 0.1 mg once daily [14]. Similar results were seen in a post hoc subgroup analysis of patients with type 2 diabetes mellitus (n = 161) [15]. In these patients, pemafibrate significantly reduced triglyceride levels by 44.7–67.4% and non-HDL cholesterol levels by 5.4–17.3% compared with placebo [15].
In a randomized, double-blind, placebo-controlled trial (JapicCTI-101331), pemafibrate was significantly more effective than placebo, but not fenofibrate, at reducing triglyceride levels and increasing HDL cholesterol levels in 224 patients with dyslipidaemia [16]. In this study, patients with triglyceride levels of ≥ 200 mg/dL and low HDL cholesterol levels (< 50 mg/dL in males, < 55 mg/dL in females) received pemafibrate 0.05, 0.1, 0.2 or 0.4 mg/day, fenofibrate 100 mg/day or placebo for 12 weeks. All treatments except placebo were associated with significant (p < 0.001) reductions from baseline in triglyceride levels at the end of the treatment period (primary endpoint). Pemafibrate decreased triglyceride levels in a dose-dependent manner (− 30.9, − 36.4, − 42.6 and − 42.7% in the 0.05, 0.1, 0.2 and 0.4 mg/day groups, respectively). Although triglyceride levels were reduced to a numerically greater extent with pemafibrate than with fenofibrate (− 29.7%), the differences were not statistically significant. All dosages of pemafibrate were also associated with improvements from baseline in other lipid variables, including a significant (p < 0.001) increase in HDL cholesterol and significant (p < 0.05) reductions in non-HDL cholesterol, VLDL cholesterol, remnant lipoprotein cholesterol, ApoB, ApoB-48 and ApoC-III [16].
Key clinical trials of pemafibrate (Kowa Company, Ltd.)
Drug(s) | Indication | Phase | Status | Location(s) | Identifier(s) |
|---|---|---|---|---|---|
Pemafibrate, fenofibrate, placebo | Dyslipidaemia | II | Complete | Japan | JapicCTI-101331 |
Pemafibrate, placebo | Dyslipidaemia | II | Complete | Multinational | EudraCT2013-001517-32 |
Pemafibrate, fenofibrate, placebo | Dyslipidaemia | II/III | Complete | Japan | JapicCTI-121764 |
Pemafibrate + pitavastatin | Dyslipidaemia | III | Complete | Japan | JapicCTI-121837 |
Pemafibrate + any statin | Dyslipidaemia | III | Complete | Japan | JapicCTI-132067 |
Pemafibrate, placebo | Dyslipidaemia in patients with type 2 diabetes mellitus | III | Complete | Japan | JapicCTI-142412 |
Pemafibrate | Dyslipidaemia | III | Complete | Japan | JapicCTI-142496 |
Pemafibrate, fenofibrate | Dyslipidaemia | III | Complete | Japan | JapicCTI-142620 |
Pemafibrate, placebo | Severe hypertriglyceridaemia | III | Ongoing | USA | NCT03011450, EudraCT2016-001518-39 |
Pemafibrate, fenofibrate, placebo | Severe hypertriglyceridaemia | III | Ongoing | USA | NCT03001817, EudraCT2015-003511-37 |
Pemafibrate, fenofibrate, placebo | Dyslipidaemia in patients with type 2 diabetes mellitus | III | Ongoing | Multinational | PROMINENT; NCT03071692, EudraCT2016-003818-26 |
2.4 Adverse Events
Currently available data indicate that oral pemafibrate is generally well tolerated in patients with dyslipidaemia. In clinical trials, the incidence of adverse events (AEs) was generally similar between the pemafibrate and placebo groups [10, 11, 13, 14, 16]. In clinical trials conducted prior to the approval of pemafibrate, the most commonly reported AEs were cholelithiasis, diabetes mellitus and elevated creatine kinase levels [1]. Rhabdomyolysis with muscle pain, weakness, elevated creatine kinase, elevated blood and urinary myoglobin and severe kidney disorder may occur [1]. Cases of rhabdomyolysis with pemafibrate have not been reported in clinical trials. Longer-term data (including from post-marketing surveillance) will be required to more fully establish the safety and tolerability of the agent.
In the phase II active comparator trial, the incidence of AEs in the pemafibrate 0.05, 0.1, 0.2 and 0.4 mg/day groups (56.8, 32.4, 47.4 and 41.0%) was similar to that in the fenofibrate 100 mg/day group (56.8%) [16]. The most commonly reported AEs were seasonal allergy and nasopharyngitis. Only two pemafibrate recipients experienced serious AEs, and no pemafibrate recipients discontinued treatment due to AEs. Adverse drug reactions occurred in 2.7–5.4% of pemafibrate recipients, compared with 10.8% of patients in the fenofibrate group. Pemafibrate did not increase plasma creatinine levels. Plasma homocysteine levels were significantly (p < 0.001) increased in the fenofibrate and pemafibrate 0.4 mg/day groups, but not in the pemafibrate 0.05, 0.1 or 0.2 mg/day groups. Pemafibrate significantly (p < 0.01) decreased plasma concentrations of ALT and γ-glutamyltransferase, while fenofibrate did not. Elevated AST levels (higher than the upper limit of normal) were seen in 5.4 and 7.9% of patients in the pemafibrate 0.1 and 0.2 mg/day groups, compared with 8.3% of placebo recipients and 24.3% of fenofibrate recipients. Elevated ALT levels (higher than the upper limit of normal) were seen in 5.4, 10.5 and 2.6% of patients in the pemafibrate 0.05, 0.2 and 0.4 mg/day groups, respectively, compared with 13.9% of placebo recipients and 13.5% of fenofibrate recipients [16].
Clinical data from two studies suggest that pemafibrate is also generally well tolerated when administered as add-on therapy to a statin [13]. The most frequently (incidence ≥ 5%) reported AEs were nasopharyngitis, diabetes mellitus, seasonal allergy, increased creatine kinase, increased uric acid and abnormal liver function tests. There were no deaths and no reports of rhabdomyolysis [13].
2.5 Ongoing Clinical Trials
In March 2017, Kowa Research Institute initiated a randomized, multicentre, phase III trial (PROMINENT; NCT03071692) to evaluate the effects of triglyceride reduction with pemafibrate on cardiovascular outcomes in type 2 diabetic patients with high fasting triglyceride levels (200 to < 500 mg/dL) and low HDL cholesterol levels (≤ 40 mg/dL) who are already receiving statins. The trial plans to recruit an estimated 10,000 patients worldwide. The primary endpoint is the first occurrence of non-fatal myocardial infarction, non-fatal ischaemic stroke, hospitalization for unstable angina requiring unplanned revascularization, or cardiovascular death. The study has an estimated completion date of May 2022.
Pemafibrate is also being investigated in the treatment of adult patients with severe hypertriglyceridaemia (fasting triglyceride levels 500 to < 2000 mg/dL) in two randomized, placebo-controlled phase III trials. One trial (NCT03001817) is being conducted in patients with normal renal function [estimated glomerular filtration rate (eGFR) ≥ 90 mL/min/1.73 m2] and the other (NCT03011450) in patients with mild or moderate renal impairment (eGFR 30 to < 90 mL/min/1.73 m2).
3 Current Status
Pemafibrate received its first global approval on 3 July 2017 for the treatment of hyperlipidaemia (including familial hyperlipidaemia) in Japan [3].
References
Kowa Co. PARMODIA® tab. 0.1 mg: prescribing information. 2017. www.kowa-souyaku.co.jp. Accessed 16 Aug 2017.
Takei K, Han SI, Murayama Y, et al. Selective peroxisome proliferator-activated receptor-alpha modulator K-877 efficiently activates the peroxisome proliferator-activated receptor-alpha pathway and improves lipid metabolism in mice. J Diabetes Investig. 2017;8(4):446–52.
Kowa Co Ltd. [The treatment of hyperlipidemia “Parmodia® tablets 0.1 mg” about acquiring manufacturing and marketing approval in Japan. First time high active and highly selective PPARα modulator in the world]. 2017. http://www.kowa.co.jp. Accessed 16 Aug 2017.
Raza-Iqbal S, Tanaka T, Anai M, et al. Transcriptome analysis of K-877 (a novel selective PPARα modulator (SPPARMα))-regulated genes in primary human hepatocytes and the mouse liver. J Atheroscler Thromb. 2015;22(8):754–72.
Takei K, Nakagawa Y, Wang Y, et al. Effects of K-877, a novel selective PPARα modulator, on small intestine contribute to the amelioration of hyperlipidemia in low-density lipoprotein receptor knockout mice. J Pharmacol Sci. 2017;133(4):214–22.
Hennuyer N, Duplan I, Paquet C, et al. The novel selective PPARα modulator (SPPARMα) pemafibrate improves dyslipidemia, enhances reverse cholesterol transport and decreases inflammation and atherosclerosis. Atherosclerosis. 2016;249:200–8.
Sairyo M, Kobayashi T, Masuda D, et al. A novel selective PPARα modulator (SPPARMα), K-877 (pemafibrate), attenuates postprandial hypertriglyceridemia in mice. J Atheroscler Thromb. 2017. doi:10.5551/jat.39693.
Yamashita S, Ishibashi S, Arai H, et al. Effect of K-877, a potent and selective PPAR alpha modulator (SPPARM alpha), on postprandial hyperlipidemia in dyslipidemic patients: a randomized cross-over study [abstract no. P5891]. Eur Heart J. 2016;37(Suppl 1):1204.
Yamashita S, Ishibashi S, Arai H, et al. Effect of K-877, a potent and selective PPAR alpha modulator (SPPARM alpha), on cholesterol efflux from macrophages in dyslipidemic patients [abstract no. P5982]. Eur Heart J. 2015;36(Suppl. 1):1047–8.
Araki E, Yamashita S, Arai H, et al. Effects of K-877, a novel selective PPARα modulator (SPPARMα), on lipid and glucose metabolism in fasting and postprandial states in type 2 diabetic patients with dyslipidaemia [abstract no. 1112]. Diabetologia. 2016;59(Suppl. 1):S531.
Ishibashi S, Yamashita S, Arai H, et al. Efficacy and safety of K-877, a potent and selective PPAR-α agonist, in Japanese patients with dyslipidemia [abstract no. 10718]. Circulation. 2013;128(22 Suppl. 1).
Yamashita S, Ishibashi S, Arai H, et al. Comparison of the novel peroxisome proliferator-activated receptor alpha agonist K-877 and fenofibrate on high-density lipoprotein subclass distribution determined by high-performance liquid chromatography in patients with dyslipidemia [abstract no. 15652]. Circulation. 2013;128(22 Suppl. 1).
Arai H, Yamashita S, Yokote K, et al. Efficacy and safety of K-877, a novel selective peroxisome proliferator-activated receptor α modulator (SPPARMα), in combination with statin treatment: two randomised, double-blind, placebo-controlled clinical trials in patients with dyslipidaemia. Atherosclerosis. 2017;261:144–52.
Kastelein JJP, Senko Y, Hounslow N, et al. K-877, a selective PPAR alpha modulator (SPPARM alpha), ameliorates dyslipidaemia in patients with well-controlled LDL cholesterol levels on statin therapy, without increases in serum creatinine [abstract no. P5983]. Eur Heart J. 2015;36(Suppl. 1):1048.
Kastelein JJP, Senko Y, Hounslow N, et al. K-877, a selective PPAR alpha modulator (SPPARM alpha), improves dyslipidaemia in statin-treated patients with type 2 diabetes mellitus [abstract no. P5985]. Eur Heart J. 2015;36(Suppl. 1):1048.
Ishibashi S, Yamashita S, Arai H, et al. Effects of K-877, a novel selective PPARα modulator (SPPARMα), in dyslipidaemic patients: a randomized, double blind, active- and placebo-controlled, phase 2 trial. Atherosclerosis. 2016;249:36–43.
Disclosure
The preparation of this review was not supported by any external funding. During the peer review process the manufacturer of the agent under review was offered an opportunity to comment on the article. Changes resulting from any comments received were made by the author on the basis of scientific completeness and accuracy. H. A. Blair is a salaried employee of Adis, Springer SBM.
Additional information about this Adis Drug Review can be found at http://www.medengine.com/Redeem/B8FBF0603C57D013.
Author information
Authors and Affiliations
Corresponding author
Additional information
This profile has been extracted and modified from the AdisInsight database. AdisInsight tracks drug development worldwide through the entire development process, from discovery, through preclinical and clinical studies to market launch and beyond.
Rights and permissions
About this article
Cite this article
Blair, H.A. Pemafibrate: First Global Approval. Drugs 77, 1805–1810 (2017). https://doi.org/10.1007/s40265-017-0818-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-017-0818-x