Abstract
Brigatinib (ALUNBRIG™) is a small molecule antineoplastic anaplastic lymphoma kinase (ALK) inhibitor being developed by ARIAD Pharmaceuticals (a wholly-owned subsidiary of Takeda Pharmaceutical Company). In April 2017 brigatinib received accelerated approval in the USA for the treatment of patients with ALK-positive metastatic non-small cell lung cancer (NSCLC) who have progressed on or are intolerant to crizotinib. The development of resistance to crizotinib is a therapeutic challenge that has led to the development of second-generation ALK-inhibitors such as brigatinib, which have activity against treatment-resistant ALK mutants. This article summarizes the milestones in the development of brigatinib leading to this first global approval for the treatment of patients with ALK-positive metastatic NSCLC who have progressed on or are intolerant to crizotinib.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
ARIAD Pharmaceuticals (a wholly-owned subsidiary of Takeda Pharmaceutical Company) are developing brigatinib (ALUNBRIG™), a small molecule anaplastic lymphoma kinase (ALK) inhibitor, for the treatment of ALK-positive metastatic non-small cell lung cancer (NSCLC) [1]. The development of resistance to anticancer treatment with current ALK-inhibitors such as crizotinib is a therapeutic challenge that has led to the development of second-generation ALK-inhibitors, including brigatinib, which have activity against crizotinib-resistant ALK mutants [2]. On the 28th of April 2017, brigatinib received accelerated approval in the USA for the treatment of patients with metastatic ALK-positive NSCLC who have progressed on or are intolerant to crizotinib. The recommended dosage of brigatinib is 90 mg orally once daily for the first 7 days then increasing to 180 mg once daily if tolerated [3]. A marketing authorization application for brigatinib as treatment for patients with ALK-positive NSCLC who have previously treated with crizotinib is under regulatory review in the EU [4].
1.1 Company Information
In July 2015 ARIAD Pharmaceuticals announced it had entered into a royalty agreement with PDL BioPharma Inc. (PDL). ARIAD agreed to pay PDL a mid-single digit royalty on sales of ponatinib (Iclusig®) in return for $US100 million up front and an additional $US50 million 1 year later. ARIAD stated these funds would be used to conduct a front line trial of brigatinib and to ensure launch readiness as early as possible [5].
On the 10th of January 2017 Takeda Pharmaceutical Company and ARIAD Pharmaceuticals announced they had entered into an agreement under which Takeda would acquire all outstanding shares in ARIAD for $US24 per share in cash [6]. Takeda announced the completion of its acquisition of ARIAD on the 16th February 2017 [7].

Clinical development of brigatinib in metastatic ALK-positive NSCLC. Est estimated date of completion, MAA Marketing authorisation application
2 Scientific Summary
2.1 Pharmacodynamics
Brigatinib is a tyrosine kinase inhibitor with in vitro activity against a number of kinases, including ALK, ROS1, insulin-like growth factor-1 receptor (IGF-1R), FLT-3, and also epidermal growth factor receptor (EGFR) deletion and point mutations [8, 9]. Autophosphorylation of ALK and ALK-mediated phosphorylation of the downstream signalling proteins STAT3, AKT, ERK1/2, and S6 is inhibited by brigatinib in vitro and in vivo [8].
In in vitro kinase assays, brigatinib had potent activity against ALK (IC50 0.6 nmol/L), including the mutant variants C1156Y (0.6 nmol/L), F1174L (1.4 nmol/L), L1196M (1.7 nmol/L), G1202R (4.9 nmol/L) and R1275Q (6.6 nmol/L). The drug also demonstrated activity against ROS1, FLT3, mutant variants of FLT3 (D835Y) and EGFR (L858R; IC50 1.5–2.1 nmol/L) and to a lesser extent EGFR with a T790M resistance mutation (L858R/T790M), native EGFR, IGF-R1, and INSR (IC50 values 29–160 nmol/L) [9].
Brigatinib inhibited growth of various anaplastic large cell lymphoma (ALCL) and NSCLC cell lines expressing NPM-ALK or EML4-ALK fusions [growth inhibition of 50% of cells (GI50) 4–31 nmol/L]; the ALK phosphorylation IC50 of the drug in these cell lines was 1.5–12 nmol/L. GI50 values for brigatinib ranged between 503 and 2387 nmol/L in 3 ALK-negative ALCL and NSCLC cell lines [9].
Brigatinib had substantial in vitro activity against a panel of 17 ALK mutants that confer resistance to crizotinib, ceritinib, and alectinib (IC50 of brigatinib 9–184 nmol/L). Brigatinib had 2.2- to 77-fold more potency than crizotinib (IC50 170–1109 nmol/L) against all but the L1198F mutant, was ≥3-fold more potent than ceritinib against L1152R/P, C1156Y, L1198F, and G1269A and ≥3-fold more potent than alectinib against L1152R, I1171N, V1180L, L1196M, G1202R, and G1269A [9].
Oral brigatinib 10, 25 or 50 mg/kg administered once daily inhibited tumour growth dose dependently in ALK-positive Karpas-299 (ALCL) and H2228 (NSCLC) xenograft mouse models [9].
In a murine orthotopic brain tumour model in which ALK-positive H2228 (NSCLC) cells were injected intracranially to form tumours in the brain, daily oral administration of brigatinib 25 and 50 mg/kg prolonged median survival to 62 and >64 days, respectively, compared to crizotinib 100 mg/kg/day (median survival 47.5 days) and vehicle (median survival 28 days) [9].

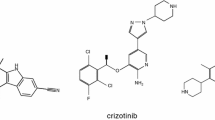
Chemical structure of brigatinib
2.2 Pharmacokinetics
Steady-state geometric mean maximum concentrations (Cmax) of 552 and 1452 ng/mL were seen after administration of brigatinib 90 and 180 mg once daily, respectively. Area under the concentration-time curve during the dosage interval (AUC τ ) was 8165 and 20,276 ng·h/mL, respectively. Systemic exposure to the drug was dose proportional, with a mean accumulation ratio after repeat dosing of 1.9–2.4. The median time to Cmax ranged between 1 and 4 h after single oral doses of brigatinib 30–240 mg. Administration of brigatinib after a high fat meal to volunteers was associated with a 13% reduction in Cmax and no effect on AUC compared to values after overnight fasting [8].
Brigatinib is 66% bound to human plasma proteins and this binding is not concentration-dependent in vitro. The blood-to-plasma concentration ratio is 0.69. The mean apparent steady-state volume of distribution was 153 L after oral administration of 180 mg brigatinib once daily. The mean apparent oral clearance of brigatinib at steady-state was 12.7 L/h and the mean plasma elimination half-life was 25 h [8].
The primary metabolic pathway for brigatinib in vitro is via CYP2C8 and CYP3A4. N-demethylation and cysteine conjugation were the major metabolic pathways after oral administration of a single 180 mg dose of radiolabelled brigatinib to volunteers. Unchanged brigatinib and the primary metabolite AP26123 accounted for 92 and 3.5% of circulating radioactivity, and 65 and 25% of the administered dose was recovered in faeces and urine, respectively [8].
Exposure to brigatinib was similar in 49 subjects with mild hepatic impairment compared to 377 subjects with normal hepatic function in a population pharmacokinetic analysis. Age, race, sex, body weight, albumin concentration and mild-to-moderate renal impairment had no clinically meaningful effect on the pharmacokinetic properties of brigatinib. The pharmacokinetic properties of brigatinib in patients with moderate-to-severe hepatic impairment, or severe renal impairment has not been studied [8].
2.2.1 Drug Interactions
Coadministration of itraconazole 200 mg twice daily and a single 90 mg dose of brigatinib was associated with a 21 and 101% increase in brigatinib Cmax and AUC from zero to infinity (AUC∞), respectively, relative to brigatinib 90 mg alone. On this basis concomitant use of brigatinib with strong CYP3A inhibitors should be avoided. Coadministration of rifampin 600 mg twice daily and a single 180 mg dose of brigatinib decreased brigatinib Cmax and AUC∞ by 60 and 80%, compared to brigatinib 180 mg alone. Because of this concomitant use of brigatinib with strong CYP3A inducers should be avoided. Brigatinib induces CYP3A in vitro and thus may decrease concentrations of CYP3A substrates, potentially leading to loss of efficacy [8].
Features and properties of brigatinib
Alternative names | ALUNBRIG™, AP26113 |
Class | Antineoplastics, diamines, piperazines, piperidines, pyrimidines, small molecules |
Mechanism of action | Anaplastic lymphoma kinase inhibitors; epidermal growth factor receptor antagonists; ROS1-protein-inhibitors |
Route of administration | Oral |
Pharmacodynamics | ALK IC50 0.6 nmol/L |
Pharmacokinetics | Steady state Cmax 1452 ng/mL, AUC τ 20,276 ng·h/mL, apparent clearance 12.7 L/h and t½ 25 h (180 mg oral once daily regimen) |
Adverse events | |
Most frequent | Nausea, diarrhoea, fatigue, cough, headache, CPK elevation, pancreatic enzyme elevation, hyperglycaemia |
Occasional | Hypertension, visual disturbance |
Rare | ILD/pneumonitis, bradycardia |
ATC codes | |
WHO ATC code | L01X-E (Protein kinase inhibitors) |
EphMRA ATC code | L1H (Protein Kinase Inhibitor Antineoplastics) |
Chemical Name | 5-chloro-N4 -[2-(dimethylphosphoryl)phenyl]-N2 -{2-methoxy-4 [4-(4-methylpiperazin-1-yl)piperidin-1-yl]phenyl}pyrimidine-2,4-diamine |
2.3 Therapeutic Trials
2.3.1 Phase I/II
Brigatinib has demonstrated promising clinical activity in patients with crizotinib-treated and crizotinib-naïve ALK-rearranged NSCLC, including substantial activity against brain metastases, in an ongoing phase I/II, single-arm, open-label, multicentre study (NCT01449461) [2]. In phase I, patients received escalating total daily doses of brigatinib 30–300 mg with the objective of establishing the recommended phase II dose. Phase II evaluated three once daily dosage regimens; 90 mg, 180 mg, and 180 mg with a 7 day lead in at 90 mg. A total of 137 patients were enrolled into phase I and II between September 2011 and July 2014 [2].
In phase II of the study confirmed objective response was observed in 66% of patients with ALK-rearranged NSCLC (n = 79), including 72% of patients previously treated with crizotinib (n = 71) and 100% of crizotinib-naïve patients (n = 8). Objective response was observed in all patients with ALK inhibitor-naive ALK-rearranged NSCLC (n = 4), 74% of patients with ALK-rearranged NSCLC previously treated with crizotinib (n = 42), no patients with EGFR T790M-positive NSCLC and resistance to one previous EGFR tyrosine kinase inhibitor (n = 1), 17% of patients with other cancers with abnormalities in brigatinib targets (n = 18) and 83% of crizotinib-naïve or crizotinib-treated patients with ALK-rearranged NSCLC and active, measurable, intracranial CNS metastases (n = 6) [2].
Key clinical trials of brigatinib (ARIAD Pharmaceuticals)
Drug(s) | Indication | Phase | Status | Location(s) | Identifier |
|---|---|---|---|---|---|
Brigatinib | NSCLC | I/II | Ongoing | USA, Spain | NCT01449461 |
Brigatinib | NSCLC | II | Ongoing | Multinational | NCT02094573 (ALTA) |
Brigatinib | NSCLC | II (investigator-sponsored) | Recruiting | USA | NCT02706626 |
Brigatinib, crizotinib | NSCLC | III | Recruiting | Multinational | NCT02737501 (ALTA-1L) |
Brigatinib | NSCLC | Expanded access | Available | USA | NCT02784158 |
As response and adverse event profiles varied with the starting dose of brigatinib in NCT01449461, two regimens are under evaluation in the phase II ALTA trial (NCT02094573), both of which were associated with substantial responses and prolonged progression-free survival. Patients with advanced NSCLC with a documented ALK rearrangement (according to an FDA-approved test or a different test with adequate archival tissue to confirm ALK arrangement by the Vysis® ALK Break-Apart fluorescence in situ hybridization Probe Kit test [3, 8]) who had progressed on treatment with crizotinib and had not received any other ALK tyrosine kinase inhibitor were randomised to brigatinib 90 mg once daily (n = 112) or 180 mg once daily with a 7-day lead-in (n = 110). 74% of patients in each arm had previously received chemotherapy and 71 and 67%, respectively, had brain metastases; 63 and 66% had had a complete or partial response to prior crizotinib therapy. After ≈8 months’ median follow up the investigator-assessed confirmed overall response rate was 45 and 54% in the 90 mg/day and 180 mg/day with lead-in arms, respectively. Median progression-free survival was 9.2 and 12.9 months, respectively. The independent review committee-assessed intracranial overall response rate in patients with measurable brain metastases at baseline was 42% in the 90 mg/day arm (n = 26) and 67% in the 180 mg/day with lead-in arm (n = 18) [10].
2.4 Adverse Events
In the ALTA trial, adverse events (all grades) occurring in ≥10% of patients treated with brigatinib 90 mg once daily (n = 109) or 90 then 180 mg once daily (n = 110) included nausea (in 33 and 40% of patients, respectively), diarrhoea (19 and 38%), vomiting (24 and 23%), constipation (19 and 15%), abdominal pain (17 and 10%), fatigue (29 and 36%), pyrexia (14 and 6.4%), cough (18 and 34%), dyspnoea (27 and 21%), interstitial lung disease (ILD)/pneumonitis (3.7 and 9.1%), hypoxia (0.9 and 2.7%), headache (28 and 27%), peripheral neuropathy (13% in each), rash (15 and 24%), hypertension (11 and 21%), muscle spasms (12 and 17%), back pain (10 and 15%), myalgia (9.2 and 15%), arthralgia (14% in each), pain in extremity (11 and 3.6%), decreased appetite (22 and 15%), visual disturbance (7.3 and 10%), pneumonia (4.6 and 10%) and insomnia (11 and 7.3%) [8].
Laboratory abnormalities (all grades) occurring in ≥20% of patients treated with brigatinib 90 mg once daily or 90 then 180 mg once daily in ALTA included increased AST (38 and 65%, respectively), hyperglycaemia (38 and 49%), increased CPK (27 and 48%), increased lipase (21 and 45%), increased ALT (34 and 40%), increased amylase (27 and 39%), increased alkaline phosphatase (15 and 29%), decreased phosphorus (15 and 23%), prolonged activated partial thromboplastin time (22 and 20%), anaemia (23 and 40%) and lymphopenia (19 and 27%) [8].
Brigatinib carries warnings and precautions in relation to the potential for severe, potentially fatal pulmonary adverse reactions consistent with ILD/pneumonitis, hypertension, bradycardia, visual disturbance, CPK elevation, pancreatic enzyme elevation, hyperglycaemia and embryo-foetal toxicity [8].
2.5 Ongoing Clinical Trials
The ongoing phase III ALTA-1L trial (NCT02737501) is comparing brigatinib and crizotinib in patients with advanced NSCLC. A phase II ARIAD-funded, investigator-sponsored study evaluating the use of brigatinib in patients with advanced NSCLC who have progressed despite treatment with the second-generation ALK inhibitors ceritinib and alectinib is also underway (NCT02706626).
3 Current Status
Brigatinib received its first global approval on the 28th of April 2017 in the USA for the treatment of patients with metastatic ALK-positive NSCLC who have progressed on or are intolerant to crizotinib.
References
ARIAD Pharmaceuticals Inc. ARIAD announces issuance of key U.S. patent on brigatinib [media release] 22 Apr 2015. http://www.ariad.com.
Gettinger SN, Bazhenova LA, Langer CJ, et al. Activity and safety of brigatinib in ALK-rearranged non-small-cell lung cancer and other malignancies: a single-arm, open-label, phase 1/2 trial. Lancet Oncol. 2016;17(12):1683–96.
US FDA. Brigatinib [media release] 28 Apr 2017. http://www.fda.gov.
ARIAD Pharmaceuticals Inc. ARIAD announces submission of Marketing Authorization Application for brigatinib to the European Medicines Agency [media release] 6 Feb 2017. http://investor.ariad.com.
ARIAD Pharmaceuticals Inc. ARIAD to receive up to $200 million through Iclusig non-dilutive synthetic-royalty financing with PDL BioPharma [media release] 29 Jul 2015. http://www.ariad.com.
Takeda Pharmaceutical Company Limited. Takeda to acquire ARIAD Pharmaceuticals, Inc. [media release] 10 Jan 2017. https://www.takeda.com.
Takeda Pharmaceutical Company Limited. Takeda completes acquisition of ARIAD Pharmaceuticals, Inc. [media release] 17 Feb 2017. https://www.takeda.com.
ARIAD Pharmaceuticals Inc. ALUNBRIGTM (brigatinib): US prescribing information. 2017. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/208772lbl.pdf. Accessed 2 May 2017.
Zhang S, Anjum R, Squillace R, et al. The potent ALK inhibitor brigatinib (AP26113) overcomes mechanisms of resistance to first- and second-generation ALK inhibitors in preclinical models. Clin Cancer Res. 2016;22(22):5527–38.
Kim DW, Tiseo M, Ahn MJ, et al. Brigatinib in patients with crizotinib-refractory anaplastic lymphoma kinase-positive non-small-cell lung cancer: a randomized, multicenter phase II trial. J Clin Oncol. 2017. doi:10.1200/JCO.2016.71.5904.
Disclosure
The preparation of this review was not supported by any external funding. During the peer review process the manufacturer of the agent under review was offered an opportunity to comment on the article. Changes resulting from any comments received were made by the author on the basis of scientific completeness and accuracy. A. Markham is a contracted employee of Adis, Springer SBM.
Additional information about this Adis Drug Review can be found at http://www.medengine.com/Redeem/4B48F06066ACFC3C.
Author information
Authors and Affiliations
Corresponding author
Additional information
This profile has been extracted and modified from the AdisInsight database. AdisInsight tracks drug development worldwide through the entire development process, from discovery, through pre-clinical and clinical studies to market launch and beyond.
Rights and permissions
About this article
Cite this article
Markham, A. Brigatinib: First Global Approval. Drugs 77, 1131–1135 (2017). https://doi.org/10.1007/s40265-017-0776-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-017-0776-3