Abstract
A fixed-dose combination tablet comprising the hepatitis C virus (HCV) NS5A inhibitor elbasvir and the HCV NS3/4A protease inhibitor grazoprevir (elbasvir/grazoprevir; Zepatier™) was recently approved for the treatment of chronic HCV genotype 1 and 4 infection in the EU and the USA. In phase III trials, 12 or 16 weeks of treatment with once-daily elbasvir/grazoprevir (fixed-dose tablet or as individual agents), taken with or without ribavirin, generally provided high rates of sustained virological response at 12 weeks (SVR12) in treatment-naive and -experienced adult patients with chronic HCV genotype 1a, 1b or 4 infection, including those with or without compensated cirrhosis, HIV co-infection, inherited blood disorders or chronic kidney disease or patients receiving opioid agonist therapy or of Japanese origin. Elbasvir/grazoprevir was generally well tolerated. Thus, elbasvir/grazoprevir, with or without ribavirin, represents an effective new option for the treatment of adults with chronic HCV genotype 1 and 4 infection, including a number of difficult-to-treat populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A fixed-dose combination of the HCV NS5A inhibitor elbasvir and the HCV NS3/4A protease inhibitor grazoprevir |
Provides high SVR12 rates when used ± ribavirin for 12 or 16 weeks in treatment-naive or treatment-experienced patients with HCV genotype 1a, 1b or 4 infection, including difficult-to-treat patients |
Regimen selection and treatment duration requires consideration of various factors, including genotype 1a NS5A polymorphisms |
Generally well tolerated |
1 Introduction
The development of direct-acting antiviral (DAA) agents has revolutionized the treatment of chronic hepatitis C, offering improved efficacy and tolerability and allowing for interferon (IFN)-free regimens [1]. A fixed-dose combination tablet of the hepatitis C virus (HCV) NS5A inhibitor elbasvir and the HCV NS3/4A protease inhibitor grazoprevir (elbasvir/grazoprevir; Zepatier™) is approved in the EU [2], the USA [3], Canada, Japan, Australia, Saudi Arabia, Israel and Switzerland [4] for the treatment of chronic HCV genotype 1 and 4 infections. This narrative review discusses pharmacological, therapeutic efficacy and tolerability data relevant to the use of elbasvir/grazoprevir in this indication.
2 Pharmacodynamic Properties
Elbasvir is a potent inhibitor of the HCV NS5A protein, which is important for viral RNA replication and viral assembly [5]. Grazoprevir is a potent, reversible, macrocyclic inhibitor of the NS3/4A protease that is essential for the processes of proteolytic cleavage of the HCV-encoded polyprotein and viral replication [6]. The elbasvir/grazoprevir combination demonstrated additive inhibitory effects on HCV RNA replication [6], with no antagonistic effects in reducing HCV RNA levels when elbasvir was combined with grazoprevir or ribavirin, or when grazoprevir was combined with ribavirin [3]. Supratherapeutic doses of elbasvir (700 mg) or grazoprevir (1600 mg) did not prolong the corrected QT interval to a clinically relevant extent, according to results of thorough QT studies [3].
2.1 Antiviral Activity
In HCV replicons containing NS5A sequences, elbasvir had potent antiviral activity against HCV genotypes 1a, 1b and 4a, with low mean 50% effective concentration (EC50) values of 0.004, 0.003 and 0.003 nmol/L, respectively [5]; grazoprevir had mean EC50 values of 0.4, 0.5 and 0.3 nmol/L against HCV genotypes 1a, 1b and 4a, respectively [6]. Potent activity was also seen with each of the drugs against HCV chimeric replicons encoding NS5A or NS3/4A sequences from clinical isolates [5, 7]. In vitro, grazoprevir is active against HCV with many of the key NS3 substitutions (genotype 1a and 1b) that confer resistance to other NS3/4A inhibitors [7] and, as expected, the activity of grazoprevir or elbasvir is not impacted by HCV amino acid substitutions that confer resistance to NS5B inhibitors [5, 7].
2.2 Resistance
In cell culture, reductions in the antiviral activity of elbasvir were associated with the emergence of certain single NS5A amino acid substitutions including M28A/G/T, Q30D/E/H/K/R, L31M/V, H58D and Y93C/H/N in HCV genotype 1a replicons (1.5- to 2000-fold reductions), L28M, L31F and Y93H in genotype 1b replicons (2- to 17-fold) and L30S, M31V and Y93H in genotype 4 replicons (3- to 23-fold) [3]. Reductions in the antiviral activity of grazoprevir in cell culture were also associated with the emergence of single NS3 amino acid substitutions, which included Y56H, R155K, A156G/T/V and D168A/E/G/N/S/V/Y in genotype 1a replicons (2- to 81-fold reductions), F43S, Y56F, V107I, A156S/T/V and D168A/G/V in genotype 1b replicons (1.5- to 375-fold) and D168A/V in genotype 4 replicons (110- to 320-fold). In HCV genotype 1a, 1b or 4 replicons, further reductions in the antiviral activity of elbasvir or grazoprevir were generally observed with combinations of elbasvir or grazoprevir resistance-associated substitutions [3].
Resistance-associated substitutions also emerged in HCV-infected patients who received elbasvir/grazoprevir, with or without ribavirin, and experienced virological failure in phase II and III trials (pooled analysis; 50 patients evaluable) [2]. Treatment-emergent amino acid substitutions in the NS5A target were detected in 81, 88 and 100% of patients with HCV genotype 1a, 1b and 4 infection, respectively; treatment-emergent substitutions in the NS3 target were detected in 78, 25 and 40% of patients with HCV genotype 1a, 1b and 4 infection, respectively [2].
Pooled analyses of phase II and III trials evaluated whether baseline polymorphisms in NS5A (L/M28T/A, R/Q30E/H/R/G/K/L/D, L31M/V/F, H58D and Y93C/H/N) and NS3 (substitutions at positions 36, 54, 55, 56, 80, 107, 122, 132, 155, 156, 158, 168, 170 and 175), known to reduce the in vitro antiviral activity of elbasvir and grazoprevir more than fivefold, impact treatment responses to the drugs in combination [2]. Elbasvir/grazoprevir for 12 weeks in patients infected with HCV genotype 1a or 1b with baseline NS5A polymorphisms was associated with SVR12 rates of 53 and 92% (vs. 97 and 99% in patients without baseline NS5A polymorphisms); 16 weeks’ treatment with elbasvir/grazoprevir plus ribavirin was associated with SVR12 rates of 100% in patients infected with HCV genotype 1a, with or without NS5A polymorphisms [2]. Findings from individual phase II and III trials (discussed in Sect. 4) were generally consistent in patients with HCV genotype 1 infection [8,9,10,11,12,13,14]. In patients with HCV genotype 4 infection, elbasvir/grazoprevir treatment for 12 weeks demonstrated SVR12 rates of 100 and 86% in patients with or without baseline NS3 polymorphisms [2]. Overall, 55 of 825 (7%) HCV genotype 1a-infected patients and 75 of 540 (14%) genotype 1b-infected patients had baseline NS5A polymorphisms; 7 of 36 patients (19%) infected with HCV genotype 4 had baseline NS3 polymorphisms.
Despite commonly detected baseline NS3 resistance-associated variants (RAVs) in patients with HCV genotype 1a and 1b infection in phase II/III trials, elbasvir/grazoprevir was generally associated with high rates of SVR12 in these patients [8,9,10,11,12, 14, 15]. For example, baseline NS3 RAVs were detected in 57 and 19% of patients with genotype 1a and 1b infection in the C-EDGE TN trial, and SVR12 was achieved in 97 and 96% of these patients (vs. 89 and 100% of patients with genotype 1a and 1b infection without baseline NS3 RAVs) [11].
The combination of grazoprevir and elbasvir demonstrated a high genetic barrier to resistance in HCV genotype 1a replicons [16]. Although cross-resistance is possible within the NS3/4A and NS5A inhibitor classes [3], elbasvir and grazoprevir demonstrated activity against HCV genotype 1a replicons with RAVs commonly associated with grazoprevir and elbasvir resistance, respectively, indicating no cross-resistance [16]. Elbasvir and grazoprevir are fully active against HCV with amino acid substitutions associated with resistance to NS5B inhibitors [3].
Data on the persistence of resistance-associated substitutions remain limited but generally indicate that treatment-emergent NS5A resistance-associated substitutions persist for longer periods than NS3 resistance-associated substitutions [6]. In pooled analyses of patients with chronic HCV genotype 1 infection in phase II and III trials, detectable levels of NS5A resistance-associated substitutions persisted at follow-up week 12 and week 24 in 95 and 100% of genotype 1a-infected patients, and in 100% of patients at follow-up week 12 and 24 in genotype 1b-infected patients [2]. By contrast, NS3 resistance-associated substitutions persisted at follow-up week 24 in 31 and 50% of genotype 1a- and 1b-infected patients; trends in genotype 4-infected patients could not be established.
3 Pharmacokinetic Profile
Following administration of elbasvir/grazoprevir to patients with HCV, peak plasma concentrations of elbasvir and grazoprevir were reached at a median of 3 and 2 h; steady-state pharmacokinetics were reached within approximately 6 days with once-daily administration [2, 3]. Elbasvir exposure is approximately dose proportional over dosages of 50–100 mg once daily and grazoprevir exposure is greater than dose-proportional over dosages of 10–800 mg once daily. Food has no clinically relevant impact on elbasvir or grazoprevir exposure; therefore, elbasvir/grazoprevir may be administered without regard to food [2, 3]. Plasma protein binding of elbasvir and grazoprevir was >99.9 and 98.8% [2, 3], and the estimated apparent volumes of distribution were ≈680 and 1250 L [3]. Both elbasvir and grazoprevir undergo partial elimination by oxidative metabolism, predominantly by CYP3A [2, 3]. Following administration of a radiolabelled dose, elbasvir and grazoprevir were mainly excreted in the faeces (>90%), with <1% recovered in the urine. In patients with HCV infection, the geometric mean apparent terminal half-lives of elbasvir (50 mg) and grazoprevir (100 mg) were ≈24 and ≈31 h [2, 3].
The elbasvir/grazoprevir dosage does not need to be adjusted in patients with any degree of renal impairment (including patients receiving haemodialysis [2, 3] or peritoneal dialysis [2]) or in patients with mild hepatic impairment (Child-Pugh A) [2, 3]. Although the magnitude of change in exposure to elbasvir in patients with moderate or severe hepatic impairment did not appear to be clinically relevant, grazoprevir exposure is significantly increased in these patients and may increase the risk of alanine aminotransferase (ALT) elevation [17]; therefore, elbasvir/grazoprevir is contraindicated in patients with moderate or severe hepatic impairment (Child-Pugh B or C) [2, 3]. Dosage adjustments of elbasvir/grazoprevir are not recommended on the basis of age, gender, race/ethnicity [2, 3] or weight/BMI [2].
Elbasvir and grazoprevir are substrates of CYP3A [2, 3]. Thus, coadministration of elbasvir/grazoprevir with CYP3A inducers (specifically strong inducers, including efavirenz [3]) is contraindicated in the EU [2] and the USA [3], as plasma concentrations of elbasvir and grazoprevir may be reduced. Similarly, concomitant use of elbasvir/grazoprevir with strong CYP3A inhibitors is not recommended, due to the potential for increased elbasvir and grazoprevir plasma concentrations [2, 3]. Elbasvir and grazoprevir are also substrates of P-gp [2, 3], although the role of intestinal P-gp in elbasvir/grazoprevir absorption appears to be minimal [3]; in the EU, coadministering P-gp inducers with elbasvir/grazoprevir is contraindicated [2]. Moreover, given that grazoprevir is a substrate of OATP1B1/3, coadministration of elbasvir/grazoprevir with inhibitors of OATP1B1/3 [some HIV antivirals (e.g. atazanavir, darunavir, lopinavir, saquinavir, tipranavir) and some immunosuppressants (e.g. ciclosporin)] is contraindicated due to the potential for increased grazoprevir plasma concentrations [2, 3], which may increase the risk of ALT elevations [3].
At the intestinal level in humans, elbasvir and grazoprevir are inhibitors of the drug transporter BCRP, and coadministration of elbasvir/grazoprevir with substrates of this transporter may cause an increase in exposure to such drugs; consequently, the dosages of some statins require consideration [2, 3]. There is also potential for tacrolimus levels to increase upon coadministration with elbasvir/grazoprevir, as grazoprevir weakly inhibits CYP3A; thus clinical monitoring is recommended.
4 Therapeutic Efficacy of Elbasvir/Grazoprevir
This section focusses on the efficacy of once-daily elbasvir/grazoprevir 50/100 mg in patients with chronic HCV infection, with or without compensated cirrhosis, as evaluated in several double-blind [10, 11, 13, 15, 18, 19] or open-label [8, 9, 12] trials, the majority of which are phase III and are part of the C-EDGE trial programme. However, the C-EDGE HEAD-TO-HEAD trial [20] which showed that elbasvir/grazoprevir was more effective than sofosbuvir/pegylated IFN (pegIFN)/ribavirin in treatment-naive or pegIFN-ribavirin-experienced adults with HCV genotype 1 or 4 infection is not discussed, as pegIFN-ribavirin regimens are no longer recommended in US [21] or EU [22] guidelines (unless DAAs are unavailable/unaffordable); key data for the study are tabulated for completeness (Table 1).
Studies included patients infected with HCV genotype 1, 4 or 6, although the genotypes for which elbasvir/grazoprevir is approved (i.e. 1 and 4) are the focus of discussion. Patients were required to be aged ≥18 years and have a baseline HCV RNA level of ≥10,000 IU/mL (including in C-CORAL [23]) [8,9,10,11,12, 14, 18, 24] or ≥100,000 IU/mL [15] where specified. Compensated cirrhosis was permitted in all trials, with some studies also permitting HIV co-infection [8,9,10, 14]. Where specified, patients co-infected with HIV could be HIV-antiretroviral therapy (ART)-naive or -experienced [8,9,10], although one study enrolled only ART-experienced patients [14]; all ART regimens were required to be stable. Patients with hepatitis B virus co-infection and decompensated liver disease were generally among those excluded.
Among trials that contained a placebo arm [10, 11, 13,14,15, 18], eligible patients were randomly assigned to receive elbasvir/grazoprevir for 12 weeks (i.e. immediate treatment) or placebo for 12 weeks, with treatment allocation unblinded 4 weeks later and the placebo group then treated with open-label elbasvir/grazoprevir for 12 weeks (i.e. deferred treatment). The primary efficacy endpoint was the proportion of patients achieving unquantifiable HCV RNA (<15 IU/mL) 12 weeks post-treatment (SVR12) [8,9,10,11,12,13,14,15, 18], specifically in the immediate-treatment group of each placebo-controlled trial [10, 11, 13,14,15] [a group which was combined with a pharmacokinetic (PK) cohort in one study [18]; Sect. 4.4]. The majority of enrolled patients were infected with HCV genotype 1a (50–76%) [8,9,10,11, 18] or 1b (62–98%) [12, 13, 15] and had a baseline HCV RNA level of >800,000 IU/mL (57–78%) [9,10,11, 13, 15, 18] and a non-CC IL28B genotype (65–97.5%) [8,9,10,11,12, 18].
Across trials, the efficacy of elbasvir/grazoprevir regimens (as measured by SVR12 rates) was generally not impacted to any meaningful extent by factors such as patient age, sex, race, IL28B genotype, cirrhosis status or baseline viral load [8,9,10,11,12,13,14, 18]; however, some subgroups contained only a small number of patients (n = 1–7) [12,13,14,15]. Some data discussed in this section are from abstracts/posters/conference reports [13, 25,26,27,28].
4.1 Treatment-Naive Patients
Four trials (C-EDGE TN, COSTAR, CO-INFECTION and C-CORAL) assessed the efficacy of elbasvir/grazoprevir specifically in treatment-naive adults with HCV genotype 1, 4 or 6 infection, who were or were not co-infected with HIV, or were receiving opioid agonist therapy (OAT) [Table 1]. In C-EDGE TN and COSTAR, enrolment of patients with cirrhosis was prespecified to 20% [10, 11] and in C-CORAL, the majority of patients (59%) were Asian [13].
4.1.1 Without HIV Co-infection
Elbasvir/grazoprevir therapy for 12 weeks in treatment-naive adults without HIV co-infection was associated with a high rate of SVR12 in the overall immediate-treatment group of the C-EDGE TN [11] and C-CORAL [13] studies, with rates of 89–100% being observed in patients with HCV genotype 1a, 1b and 4 infections (Table 1). In C-EDGE TN, SVR12 rates were not impacted to any meaningful extent by IFN treatment eligibility [11]. SVR12 rates were not impacted by baseline viral load in C-CORAL [13], although were 8% higher (with non-overlapping 95% CIs) in patients with a baseline HCV RNA of ≤800,000 IU/mL (n = 94) than of >800,000 IU/mL (n = 222) [100 vs. 92%] in the C-EDGE TN study [11]. The rate of virological failure was low in each of the trials (Table 1), and was mainly due to virological relapse [11, 13]. For instance, in C-EDGE TN, relapse occurred in 12 patients (nine of which had HCV genotype 1a infection) and virological breakthrough in one patient (HCV genotype 1a) [11].
Twenty-four weeks after treatment with elbasvir/grazoprevir in the C-EDGE TN trial, SVR rates (i.e. SVR24) were high in both the immediate- and deferred-treatment groups (94 and 91%) [28]. Moreover, in per-protocol analyses combining these two treatment arms (n = 414), high SVR24 rates were observed in patients with HCV genotype 1a (93%), 1b (99%) and 4 (100%) and regardless of sex, age, race, IL28B genotype, IFN eligibility, cirrhosis status and baseline HCV RNA load (92–100%).
4.1.2 With HIV Co-infection
The efficacy of elbasvir/grazoprevir therapy for 12 weeks in patients with HCV/HIV-1 co-infection was evaluated in the single-arm C-EDGE CO-INFECTION trial [9]. ART-stable patients were receiving tenofovir or abacavir, and either emtricitabine or lamivudine plus raltegravir, dolutegravir or rilpivirine, for ≥8 weeks before enrolment and were required to have CD3 or CD4 T-cell counts of >200 cells/μL and undetectable HIV RNA levels of <20 copies/mL; ART-naive patients had to have CD3 or CD4 counts of >500 cells/μL and an HIV viral load of <50,000 copies/mL. At baseline, the mean HCV RNA level was 6.03 log10 IU/mL, the mean CD3 or CD4 count was 613 cells/μL and 97% of patients were ART-stable [9].
Elbasvir/grazoprevir therapy for 12 weeks was associated with high rates of SVR12 in the overall population and across all assessed genotypes, including 1a, 1b and 4 (Table 1) [9]. SVR12 rates were consistently high across all other subgroups (≥94%), including some historically associated with poor response (i.e. Black/African American, presence of cirrhosis, IL28B non-CC genotype and baseline HCV viral load >800,000 IU/mL). Virological failure occurred in seven patients (all non-cirrhotic), five of whom experienced virological relapse (four with HCV genotype 1a infection and one with HCV genotype 4 infection) and two who had been re-infected with a different HCV genotype during follow-up [9]. There was no impact on CD3 or CD4 cell counts or percentages during this study.
4.1.3 Receiving Opioid Agonist Therapy
The C-EDGE COSTAR trial evaluated the efficacy of 12 weeks of treatment with elbasvir/grazoprevir in patients with chronic HCV who had been receiving OAT (methadone, buprenorphine or buprenorphine-naloxone) for ≥3 months with ≥80% adherence to OAT visits (Table 1); patients actively using drugs of potential abuse were included [10].
Elbasvir/grazoprevir treatment for 12 weeks was associated with high overall SVR12 rates in the immediate-treatment group, which were consistent across genotypes 1a, 1b and 4 (Table 1) [10]. Moreover, SVR12 rates of 90–95% were observed in subgroups defined by urine drug screen outcome (i.e. negative or positive) or race [White and African Americans, but not Asians (n = 9)] [10]. Virological failure occurred in 12 patients (6%) receiving elbasvir/grazoprevir (Table 1), with evidence of relapse in seven of these patients and probable reinfection present in five patients [10]. SVR24 rates (secondary endpoint) of >87% were achieved in the elbasvir/grazoprevir immediate-treatment group and across genotypes 1a, 1b and 4; two additional relapses were identified at 24 weeks [10]. Viral recurrence and probable reinfection did not occur in patients with HCV genotype 4 infections at either timepoint. Similar SVR12 and SVR24 rates were reported with elbasvir/grazoprevir in patients who participated in the active phase of the deferred-treatment group of the trial.
4.1.4 Health-Related Quality of Life
General and disease-specific health-related quality of life (HR-QOL) measures improved or did not markedly worsen with elbasvir/grazoprevir in treatment-naive patients in the C-EDGE TN, COSTAR and CO-INFECTION trials [25,26,27]. For instance, in C-EDGE TN, elbasvir/grazoprevir recipients had mean improvements from baseline in general HR-QOL (as assessed by most SF-36v2® components and EQ-VAS), HCV-specific HR-QOL (assessed by Chronic Liver Disease Questionnaire-HCV), fatigue (on the FACIT-Fatigue scale) and activity/work productivity (as measured by Work Productivity and Activity Impairment scores) after 12 weeks of treatment and/or during follow-up, although only changes in general HR-QOL differed from those observed in placebo recipients [27].
4.2 Treatment-Experienced Patients
The C-EDGE TE trial evaluated the efficacy of elbasvir/grazoprevir with or without ribavirin for 12 or 16 weeks of therapy in treatment-experienced adults with chronic HCV infection who had failed prior treatment with pegIFN plus ribavirin (Table 1); patients who had received previous DAA treatment were excluded [8]. Randomization was stratified based on cirrhosis status and previous treatment response (i.e. relapse, partial or null response) [8], and the prespecified reference SVR12 rate was 58% [6].
In this study, elbasvir/grazoprevir treatment with or without ribavirin for 12 or 16 weeks was associated with high SVR12 rates in the overall patient population, with most regimens providing rates of ≥92% in patients with genotype 1 or 4 infections, with the exception of elbasvir/grazoprevir without ribavirin in genotype 4 infection (Table 1) [8]. High SVR12 rates (92–100%) were achieved in patients with prior relapse or partial or null response in a per-protocol analysis [8]. There were no occurrences of virological failure in recipients of elbasvir/grazoprevir plus ribavirin for 16 weeks, whereas 6–7% of patients in other treatment arms had virological failure (Table 1); the majority of these failures were due to relapse, which occurred predominantly in patients with HCV genotype 1a infection [8].
In another study (the phase II C-SALVAGE trial; n = 79), a similar benefit was seen with elbasvir plus grazoprevir treatment in patients with HCV genotype 1 infection who had already failed ≥4 weeks of triple therapy (i.e. pegIFN and ribavirin plus an earlier-generation protease inhibitor) [12]. Patients in this study had received an NS3/4A protease inhibitor (i.e. boceprevir, telaprevir or simeprevir) and most (84%) had a history of virological failure. After 12 weeks of once-daily elbasvir 50 mg plus grazoprevir 100 mg with ribavirin, the SVR12 rate was 97% [primary endpoint in the per-protocol population; n = 70] [12]. SVR12 rates were also high (91–100%) in patients with prior virological failure and in patients with signature NS3 RAVs at baseline and across various subgroups based on ethnicity and HCV genotype (1a or 1b); an SVR12 rate of 75% was observed in patients with signature NS5A RAVs at baseline (n = 8) [12]. Virological failure (all relapses) occurred in three patients, all of whom had experienced prior virological failure. High SVR rates (92–96%) were maintained at 24 weeks post treatment [24].
4.3 Patients with Inherited Blood Disorders
The C-EDGE IBLD trial (NCT02252016) evaluated the efficacy of elbasvir/grazoprevir in HCV-infected adults with various inherited blood disorders (IBLDs), including sickle cell anaemia (18% of patients), β-thalassaemia (38%) and von Willebrand disease/haemophilia A or B (43%) [14]. At baseline, HCV genotype 1a, 1b and 4 infections were reported in 41, 46 and 11% of patients, respectively, 50% of patients were treatment-experienced, 23% had IL28B CC genotype, 24% had cirrhosis and 6% were HIV co-infected [14].
Treatment with elbasvir/grazoprevir for 12 weeks was associated with high overall rates of SVR12 in the immediate-treatment group of this trial, including across genotypes 1a, 1b and 4 (Table 1) [14]. SVR12 rates of >86.5% were achieved across most other patient subgroups, including those defined by treatment history, HIV co-infection and type of IBLD [14]. The lowest SVR12 rates (both 83.3%) were evident in patients co-infected with HIV and those who were Asian; however, these subgroups contained only a small number of patients (both n = 6) [14]. The rate of virological failure was low (all relapses) [Table 1], occurring in six patients, all of whom were aged <65 years, treatment-naive and without cirrhosis [14]. These patients were generally white, male, infected with HCV genotype 1a and had a baseline viral count of >2,000,000 IU/mL and NS5A RAVs.
4.4 Patients with Chronic Kidney Disease
The C-SURFER trial examined the use of elbasvir/grazoprevir in patients with HCV genotype 1 infection and stage 4 or 5 chronic kidney disease (CKD), with or without haemodialysis dependence (Table 1) [18]. The trial included patients who were HCV treatment-naive or had previously received IFN-based therapy and excluded those requiring peritoneal dialysis or likely to receive a renal transplant during the study. In addition to the patients randomized to receive elbasvir and grazoprevir (immediate-treatment group) or placebo (deferred-treatment group) in a double-blind fashion in this study, a cohort of 11 patients received open-label elbasvir plus grazoprevir and underwent intensive PK sampling [18]. Patients in the immediate-treatment and PK cohort received elbasvir and grazoprevir as separate entities, whereas patients in the deferred-treatment arm received the fixed-dose combination. At baseline, most patients were treatment-naive (80%), not cirrhotic (94%), had CKD stage 5 (81%) and were on haemodialysis (76%). The primary efficacy endpoint was a non-randomized comparison of SVR12 for the combined immediate-treatment group and PK population at the end of therapy versus an historical control SVR12 of 45% [18].
In this study, elbasvir/grazoprevir was associated with a high SVR12 rate that was significantly better than the historical control (p < 0.001), with a very low rate of virological failure (one relapse) [Table 1] [18]. In subgroup analyses, SVR12 rates were high (98–100%), regardless of CKD severity, HCV genotype (1a or 1b; Table 1), haemodialysis status and diabetes status [18].
4.5 Japanese Patients
The phase III portion of a phase II/III Japanese study evaluated the efficacy of elbasvir (50 mg) plus grazoprevir (100 mg) in treatment-naive and -experienced (IFN-based therapy without DAAs) Japanese patients (20–80 years old) infected with HCV genotype 1, with or without cirrhosis [15]. Patients without cirrhosis were randomized to receive elbasvir/grazoprevir (n = 227) or placebo (n = 74) for 12 weeks, and patients with compensated cirrhosis received open-label elbasvir/grazoprevir for 12 weeks (n = 35). At baseline, the majority of patients were treatment-naive (65%) and had an IL28B CC genotype (59%) [15].
Treatment with elbasvir plus grazoprevir was associated with high SVR12 rates in non-cirrhotic patients (Table 1) [15]. SVR12 rates of 91–100% were observed consistently across subgroups including those defined by HCV genotype, prior treatment history, meal condition (with or without meals), estimated glomerular filtration rate (eGFR) and baseline ALT levels, although it should be noted that subgroups of HCV genotype 1a infection and those receiving treatment without meals contained a small number of patients (n = 4–7) [15]. The rate of virological failure (all relapses) was low (Table 1), with no on-treatment virological breakthroughs [15]. In cirrhotic patients, SVR12 rates were 97%, with low rates of virological failure (one relapse).
5 Tolerability of Elbasvir/Grazoprevir
Elbasvir/grazoprevir was generally well tolerated in patients with chronic HCV genotype 1a, 1b or 4 infections in phase II/III studies (Sect. 4), regardless of whether the patients were treatment-naive or -experienced (including those who had failed prior triple therapy), had HIV co-infection, IBLD or advanced CKD, or were Japanese or receiving OAT (Sect. 4).
In a pooled analysis of three of these studies (C-EDGE TN, TE and CO-INFECTION) [6], drug-related adverse events (AEs) during the 12-week treatment phase plus 14 days of follow up occurred in 64 and 36% of patients who received elbasvir/grazoprevir with (n = 104) or without (n = 639) ribavirin versus 39% of patients who received placebo (n = 105), and led to discontinuations in ≤1% of patients in these treatment groups. The majority of drug-related AEs were of mild or moderate severity. Serious drug-related AEs occurred in 1% of elbasvir/grazoprevir plus ribavirin recipients and led to no discontinuations in these patients; no serious drug-related AEs occurred in the elbasvir/grazoprevir without ribavirin or placebo groups [6]. The findings of this pooled analysis are supported by an integrated analysis of the same three trials plus five phase II studies, in which patients had received elbasvir/grazoprevir with or without ribavirin (n = 657 and 1033) or placebo (n = 105) for 8–18 weeks (available as an abstract plus conference report) [29]. There were no treatment-related deaths and no association between the frequency of AEs and sex, age, HIV co-infection or presence of cirrhosis [29].
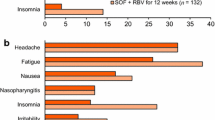
The most common (≥10%) drug-related AEs that occurred in any treatment group of the pooled analysis included fatigue, headache, nausea and anaemia, all of which occurred in numerically more patients receiving elbasvir/grazoprevir plus ribavirin than in other treatment groups (Fig. 1) [6]. Other common drug-related AEs (incidence ≥5 to <10% in any treatment group), including asthenia, decreased appetite, dizziness, insomnia, cough, dyspnoea and pruritus, also occurred in numerically more recipients of elbasvir/grazoprevir plus ribavirin than elbasvir/grazoprevir or placebo recipients (5.8–9.6 vs. 0.3–2.7 and 0–6.7% of patients) [6]. Overall, numerically higher rates of drug-related AEs (particularly asthenia, fatigue, pruritus) occurred in cirrhotic than non-cirrhotic patients in the elbasvir/grazoprevir plus ribavirin treatment arm; numerically higher rates of anaemia, fatigue, dyspnoea, gastrointestinal complaints and pruritus occurred in cirrhotic patients receiving elbasvir/grazoprevir plus ribavirin than without ribavirin [6]. No further details were reported.
Adverse events with ≥10% incidence in any treatment arm in a pooled analysis of C-EDGE trials: TN, TE and CO-INFECTION [6]. EBR elbasvir, GZR grazoprevir, PL placebo, RBV ribavirin, SPP safety population pool, θ indicates that anaemia was not observed in EBR/GZR (no RBV) or PL recipients
The tolerability profile of elbasvir/grazoprevir regimens in individual phase II/III trials (Sect. 4) was generally consistent with that of the pooled analysis [6]. Moreover, in treatment-experienced patients in C-EDGE TE, elbasvir/grazoprevir, with or without ribavirin, was generally well tolerated regardless of duration of treatment (i.e. 12 or 16 weeks), although haemoglobin levels <10 g/dL occurred in twice as many patients who received elbasvir/grazoprevir plus ribavirin for 16 weeks than for 12 weeks (21 vs. 9%) [8]. No patients receiving elbasvir/grazoprevir without ribavirin had decreased haemoglobin levels. In addition, elbasvir/grazoprevir did not affect haematological or clotting measures or the treatment of the underlying blood disorder in patients with IBLDs in C-EDGE IBLD [14] and did not differ from placebo to any statistically meaningful extent with regard to renal function AEs (e.g. increased CKD stage, worsening of proteinuria or initiation of maintenance dialysis) in patients with advanced CKD in C-SURFER [18]. Notably, neither treatment group in the latter trial had consistent mean changes in creatinine or eGFR [18].
In the phase III part of the Japanese trial [15], drug-related AEs occurred in 25.6 and 18.9% of non-cirrhotic patients receiving elbasvir plus grazoprevir or placebo, and in 37.1% of cirrhotic patients receiving elbasvir/grazoprevir, but were serious in < 1% of patients in any group. The most commonly reported drug-related AE (incidence ≥5%) with elbasvir/grazoprevir was increased ALT levels, both in non-cirrhotic patients (5.3 vs. 1.4% with placebo) and cirrhotic patients (14.3%); other commonly reported drug-related AEs in cirrhotic patients included increased aspartate aminotransferase levels (14.3%), diarrhoea (8.6%), constipation (5.7%) and malaise (5.7%) [15].
In the pooled analysis, 0.3 and 0.8% of patients treated with elbasvir/grazoprevir (without ribavirin) had elevations in ALT levels of >2.5–5 and >5 × baseline; the majority of ALT elevations were grade 1 and <1% of patients had either grade 3 [5.1–10 × the upper limit of normal (ULN)] or grade 4 (>10 × ULN) ALT elevations [6]. ALT elevations with an increase of >2.5–5 × baseline occurred in 1.0 and 1.9% of elbasvir/grazoprevir plus ribavirin and placebo recipients; ALT elevations from baseline occurred in 57.1% of placebo recipients [6]. Generally, ALT elevations (>5 × ULN) were observed at or after week 8, were asymptomatic and resolved with ongoing therapy or after completion of therapy[2, 3]. The risk of late ALT elevations increased with increasing grazoprevir plasma concentrations but was not impacted by cirrhosis or treatment duration.
In the EU [2] and the USA [3], hepatic laboratory testing should be performed at baseline and at week 8 of treatment with additional testing at week 12 for patients receiving 16 weeks of therapy; discontinuation of elbasvir/grazoprevir is recommended if ALT elevations are accompanied by signs and symptoms of liver inflammation or increasing conjugated bilirubin, alkaline phosphatase or international normalized ratio; discontinuation of elbasvir/grazoprevir should be considered in cases of persistently elevated ALT levels of >10 × ULN [2, 3].
Bilirubin elevations occurred more frequently in recipients of elbasvir/grazoprevir plus ribavirin than in patients receiving elbasvir/grazoprevir without ribavirin, with worsening grade from baseline occurring in 25 and 2.2% of these patients, respectively, in the pooled analysis; bilirubin elevations typically occurred in the first 2 weeks of therapy and resolved spontaneously [6]. In elbasvir/grazoprevir plus ribavirin recipients, the time course of bilirubin elevations was consistent with ribavirin-induced haemolysis leading to saturation of the hepatic bilirubin transporter.
6 Dosage and Administration of Elbasvir/Grazoprevir
Fixed-dose elbasvir/grazoprevir 50/100 mg tablets are indicated for use, with or without ribavirin, for the treatment of adults with chronic HCV genotype 1 or 4 infection in the EU [2] and the USA [3]. The recommended dosage is one tablet taken once daily, with or without food [2, 3]. Prior to initiation of therapy, testing patients with HCV genotype 1a infection for the presence of NS5A resistance-associated polymorphisms at amino acid positions 28, 30, 31 or 93 is recommended [3]; hepatic laboratory testing should also be performed (Sect. 5).
Elbasvir/grazoprevir is recommended for use alone or in combination with ribavirin for a duration of 12 or 16 weeks, depending on various factors, including the infecting HCV genotype [2, 3], the presence of NS5A polymorphisms (for some genotype subtypes) [2, 3] and HCV RNA levels [2] (see supplementary information for specific details). The most appropriate elbasvir/grazoprevir regimen and treatment duration has not yet been established for patients infected with HCV GT 1a with baseline NS5A resistance-associated polymorphisms who have previously received pegIFNα-ribavirin plus an HCV NS3/4A protease inhibitor. Local prescribing information should be consulted for further information regarding specific regimen recommendations, drug interactions, contraindications, warnings and precautions related to elbasvir/grazoprevir treatment, and for further information regarding dosage modifications, warnings and precautions pertaining to concomitant ribavirin.
7 Place of Elbasvir/Grazoprevir in the Management of Chronic Hepatitis C
The goals of HCV therapy are to cure the HCV infection and prevent HCV-related complications (e.g. hepatic fibrosis or severe extrahepatic complications) [22]. The advent of IFN-free DAA regimens has demonstrated marked improvements in efficacy and tolerability compared with IFN-based regimens [30], with several combinations of DAA agents associated with high SVR12 rates (>90%) and reduced treatment duration [31]. Effective use of these agents requires consideration of patient-specific factors including HCV genotype, comorbidities (e.g. cirrhosis), presence of baseline RAVs and drug interactions with commonly used medications (e.g. lipid-lowering drugs) [21]. One of the most recent of these DAA combinations to be introduced is fixed-dose elbasvir/grazoprevir.
In phase III trials (Sect. 4), treatment with elbasvir/grazoprevir, with or without ribavirin, for 12 or 16 weeks achieved high SVR12 rates in treatment-naive (Sect. 4.1) and -experienced (Sect. 4.2) patients with chronic HCV genotype 1a, 1b or 4 infection, including patients with HIV co-infection (Sect. 4.1.2), IBLDs (Sect. 4.3), CKD (Sect. 4.4), patients receiving OAT (Sect. 4.1.3) or of Japanese origin (Sect. 4.5). The efficacy of elbasvir/grazoprevir was seen regardless of compensated cirrhosis status. Pooled analyses were used to support the approval of elbasvir/grazoprevir for genotype 4 infection, as this is a much rarer genotype and patient numbers in individual trials were relatively small [32]. Improvements or no marked worsening of general or disease-specific HR-QOL were observed in treatment-naive patients (Sect. 4.1.4); to date, HR-QOL data in treatment-experienced patients have not been reported. The presence of baseline NS5A polymorphisms appeared to impact SVR12 rates particularly in patients with HCV genotype 1a infection (Sect. 2.1); baseline testing of patients with HCV genotype 1a infection for NS5A resistance-associated polymorphisms is recommended in the USA (Sect. 6).
Elbasvir/grazoprevir was generally well tolerated in clinical trials, with the most common AE being fatigue (Fig. 1); however, when coadministered with ribavirin, the tolerability profile appeared to be less favourable with regard to most AEs, including anaemia and elevated bilirubin (Sect. 5). Besides hepatic laboratory monitoring, the American Association for the Study of Liver Diseases (AASLD) and the Infectious Diseases Society of America (IDSA) recommend various laboratory tests before and during treatment (e.g. complete blood counts, GFR), with particular attention given to patients receiving concomitant ribavirin (monitoring for anaemia) [21]. Local guidelines should be consulted for further information on additional monitoring for individual regimens and patient populations.
Current European Association for the Study of the Liver (EASL) guidelines [22] recommend 12 weeks of elbasvir/grazoprevir as an option for treatment-naive and -experienced patients with chronic HCV genotype 1a, 1b and 4 infection, with or without cirrhosis or HIV co-infection. If HCV RNA is >800,000 IU/mL, the addition of ribavirin to elbasvir/grazoprevir and prolonging therapy to 16 weeks is recommended; where resistance-associated substitution testing is available, substitutions that confer resistance to elbasvir at baseline should also be considered when prolonging therapy and adding ribavirin in patients with HCV genotype 1a infection [22].
Similarly, current AASLD/IDSA guidelines recommend 12 weeks of elbasvir/grazoprevir as an option for patients with chronic HCV genotype 1a, 1b or 4 infection, with or without compensated cirrhosis, who are treatment-naive or -experienced [21]. The addition of ribavirin with or without extending the duration of treatment to 16 weeks may be necessary in some patients (e.g. patients with baseline substitutions that confer resistance); local guidelines should be consulted for further details.
Other DAA-based combination regimens recommended by EASL [22] and AASLD/IDSA [21] include sofosbuvir/ledipasvir [21, 22] and sofosbuvir/velpatasvir [21, 22] for HCV genotype 1a, 1b or 4 infection; sofosbuvir plus daclatasvir is also recommended for patients with HCV genotype 1a, 1b [21, 22] and 4 infections [22]. Other recommendations include ombitasvir/paritaprevir/ritonavir plus dasabuvir [21, 22] for HCV genotype 1a and 1b infection, and ombitasvir/paritaprevir /ritonavir for HCV genotype 4 infection [21, 22].
The choice of treatment in some hard-to-treat patient populations can be influenced by additional factors. For example, the EASL guidelines indicate that coadministration of elbasvir/grazoprevir and antiretrovirals is particularly limited, which could limit the use of elbasvir/grazoprevir in patients who are co-infected with HIV [22]. However, for drug users, elbasvir/grazoprevir, like sofosbuvir/ledipasvir and sofosbuvir/velpatasvir, has no clinically significant interactions with illicit recreational drugs, making these combinations more prudent choices in this setting than ombitasvir/paritaprevir/ritonavir plus dasabuvir (which may potentially interact with illicit drugs) [22].
Furthermore, elbasvir/grazoprevir is the first IFN-free regimen to be supported by robust data in CKD patients receiving haemodialysis (a previously unmet need) [22]; confirmatory data for CKD patients with genotype 4 infection would be beneficial (as C-SURFER was conducted solely in patients with genotype 1 infection). Elbasvir/grazoprevir is recommended for genotype 1 and 4 infections in patients with severe renal impairment; ombitasvir/paritaprevir/ritonavir with/without dasabuvir is also a recommended option [21, 22]. However, ombitasvir/paritaprevir/ritonavir plus dasabuvir requires twice-daily administration of dasabuvir [21, 22], which complicates the dosing regimen (relative to once-daily elbasvir/grazoprevir) and may impact treatment adherence. Data for sofosbuvir-based regimens in patients with severe renal dysfunction are lacking (as sofosbuvir is mainly eliminated by renal clearance) and sofosbuvir-free regimens are preferred, wherever possible [22].
Unlike sofosbuvir/ledipasvir, sofosbuvir/velpatasvir and sofosbuvir plus daclatasvir (with or without ribavirin), elbasvir/grazoprevir cannot be used in patients with decompensated cirrhosis [21, 22]; patients with decompensated cirrhosis were excluded from clinical trials (Sect. 4) and remain one of the last truly difficult-to-treat populations.
Although the emergence of DAA-based regimens has revolutionised HCV treatment, access to new agents remains limited by extremely high costs [33, 34]. Pharmacoeconomic analyses of the cost-effectiveness of elbasvir/grazoprevir, with or without ribavirin, would be of interest. Given the paucity of direct comparative studies in the HCV field, additional active comparator-controlled head-to-head trials for elbasvir/grazoprevir versus other recommended DAA-based regimens would be beneficial.
In conclusion, elbasvir/grazoprevir, with or without ribavirin, is an effective new option for the treatment of adults with chronic HCV genotype 1 and 4 infection, including the difficult-to-treat patient populations with compensated cirrhosis, previous treatment experience, HIV co-infection, IBLDs, CKD or receiving OAT.
Data Selection Elbasvir/Grazoprevir: 486 records identified
Duplicates removed | 27 |
Excluded at initial screening (e.g. press releases; news reports; not relevant drug/indication) | 39 |
Excluded during initial selection (e.g. preclinical study; review; case report; not randomized trial) | 9 |
Excluded during writing (e.g. reviews; duplicate data; small patient number; nonrandomized/phase I/II trials) | 379 |
Cited efficacy/tolerability articles | 14 |
Cited articles not efficacy/tolerability | 18 |
Search Strategy: EMBASE, MEDLINE and PubMed from1946 to present. Clinical trial registries/databases and websites were also searched for relevant data. Key words were Zepatier, elbasvir, MK-8742, grazoprevir, MK-5172. Records were limited to those in English language. Searches last updated 4 April 2017 | |
References
Myers RP, Shah H, Burak KW, et al. An update on the management of chronic hepatitis C: 2015 consensus guidelines from the Canadian Association for the Study of the Liver. Can J Gastroenterol Hepatol. 2015;29(1):19–34.
European Medicines Agency. Zepatier (elbasvir/grazoprevir) film-coated tablets: EU summary of product characteristics. 2016. http://www.ema.europa.eu/. Accessed 4 Apr 2017.
Merck & Co., Inc. Zepatier™ (elbasvir and grazoprevir) tablets, for oral use: US prescribing information 2016. http://www.merck.com/. Accessed 4 Apr 2017.
Merck & Co., Inc. Merck to present new data on Zepatier™ (elbasvir/grazoprevir) and chronic hepatitis C clinical development programs at The Liver Meeting® [media release]. 3 October 2016. http://www.businesswire.com/. Accessed 4 Apr 2017.
Coburn CA, Meinke PT, Chang W, et al. Discovery of MK-8742: an HCV NS5A inhibitor with broad genotype activity. Chemmedchem. 2013;8(12):1930–40.
European Medicines Agency. Assessment report: Zepatier (elbasvir/grazoprevir). 2016. http://www.ema.europa.eu/. Accessed 4 Apr 2017.
Summa V, Ludmerer SW, McCauley JA, et al. MK-5172, a selective inhibitor of hepatitis C virus NS3/4a protease with broad activity across genotypes and resistant variants. Antimicrob Agents Chemother. 2012;56(8):4161–7.
Kwo PY, Gane E, Peng C-Y, et al. Effectiveness of elbasvir and grazoprevir combination, with or without ribavirin, for treatment-experienced patients with chronic hepatitis C infection. Gastroenterology. 2017;152(1):164–75.
Rockstroh JK, Nelson M, Katlama C, et al. Efficacy and safety of grazoprevir (MK-5172) and elbasvir (MK-8742) in patients with hepatitis C virus and HIV co-infection (C-EDGE CO-INFECTION): a non-randomised, open-label trial. Lancet HIV. 2015;2(8):e319–27.
Dore GJ, Altice F, Litwin AH, et al. Elbasvir–grazoprevir to treat hepatitis C virus infection in persons receiving opioid agonist therapy: a randomized trial. Ann Intern Med. 2016;165(9):625–34.
Zeuzem S, Ghalib R, Reddy KR, et al. Grazoprevir-elbasvir combination therapy for treatment-naive cirrhotic and noncirrhotic patients with chronic hepatitis C virus genotype 1, 4, or 6 Infection: a randomized trial. Ann Intern Med. 2015;163(1):1–13.
Forns X, Gordon SC, Zuckerman E, et al. Grazoprevir and elbasvir plus ribavirin for chronic HCV genotype-1 infection after failure of combination therapy containing a direct-acting antiviral agent. J Hepatol. 2015;63(3):564–72.
George J, Burnevich E, Sheen I, et al. Efficacy and safety of elbasvir/grazoprevir in treatment-naive subjects with chronic HCV GT 1, GT 4 and GT 6 infection (C-CORAL): a phase III randomized multinational clinical trial [abstract no. 76 plus conference report]. Hepatology. 2016;64(Suppl 1):41A.
Hezode C, Colombo M, Bourliere M, et al. Elbasvir/grazoprevir for patients with hepatitis C virus infection and inherited blood disorders: a phase III study. Hepatology. 2017. doi:10.1002/hep.29139.
Kumada H, Suzuki F, Karino Y, et al. The combination of elbasvir and grazoprevir for the treatment of chronic HCV infection in Japanese patients: a randomized phase II/III study. J Gastroenterol. 2017;52(4):520–33.
Lahser FC, Bystol K, Curry S, et al. The combination of grazoprevir, a hepatitis C virus (HCV) NS3/4A protease inhibitor, and elbasvir, an HCV NS5A inhibitor, demonstrates a high genetic barrier to resistance in HCV genotype 1a replicons. Antimicrob Agents Chemother. 2016;60(5):2954–64.
US FDA. Application number: 208261Orig1s000 clinical pharmacology and biopharmaceutics review(s). 2015. http://www.accessdata.fda.gov/. Accessed 4 Apr 2017.
Roth D, Nelson DR, Bruchfeld A, et al. Grazoprevir plus elbasvir in treatment-naive and treatment-experienced patients with hepatitis C virus genotype 1 infection and stage 4-5 chronic kidney disease (the C-SURFER study): a combination phase 3 study. Lancet. 2015;386(10003):1537–45.
US National Institutes of Health. ClinicalTrials.gov identifier NCT02252016. 2017. https://clinicaltrials.gov. Accessed 4 Apr 2017.
Sperl J, Horvath G, Halota W, et al. Efficacy and safety of elbasvir/grazoprevir and sofosbuvir/pegylated interferon/ribavirin; a phase III randomized controlled trial. J Hepatol. 2016;65(6):1112–9.
American Association for the Study of Liver Diseases and Infectious Diseases Society of America. Recommendations for testing, managing and treating hepatitis C. 2016. http://hcvguidelines.org/. Accessed 4 Apr 2017.
European Association for the Study of the Liver. EASL recommendations on treatment of hepatitis C 2016. J Hepatol. 2017;66(1):153–94.
Data on file, Merck & Co., Inc. 2017.
Buti M, Gordon SC, Zuckerman E, et al. Grazoprevir, elbasvir, and ribavirin for chronic hepatitis C virus genotype 1 infection after failure of pegylated interferon and ribavirin with an earlier-generation protease inhibitor: Final 24-week results from C-SALVAGE. Clin Infect Dis. 2016;62(1):32–6.
Arduino JM, Jiang Z, Shaughnessy M, et al. C-EDGE Co-Infection: impact of 12-week oral regimen of grazoprevir (GZR, MK-5172)/elbasvir (EBR, MK-8742) on patient-reported outcomes (PROs) in treatment-naive patients with HCV/HIV co-infection [abstract no. 729 plus conference report]. Hepatology. 2015;62(Suppl 1):572-3A.
Arduino JM, Shibolet O, Litwin AH, et al. C-EDGE CO-STAR: favorable impact of elbasvir and grazoprevir on health-related quality of life in treatment-naive HCV-infected persons who inject drugs receiving opioid agonist therapy [abstract no. THU-225 plus conference report]. J Hepatol. 2016;64(Suppl 2):S403–4.
Arduino JM, Wang Y, Brown DD, et al. C-EDGE TN: impact of 12-week oral regimen of grazoprevir (GZR, MK-5172)/elbasvir (EBR, MK-8742) on patient-reported outcomes (PROs) in treatment-naive patients with chronic hepatitis C virus (HCV) genotype (GT) 1, 4, or 6 infection [abstract no. 717 plus conference report]. Hepatology. 2015;62(Suppl 1):565-6A.
Zeuzem S, Ghalib R, Reddy KR, et al. Final SVR24 data from the phase 3 C-EDGE treatment-naive study of elbasvir/grazoprevir in patients with chronic HCV genotype 1, 4 or 6 infection [abstract no. SAT-266 plus conference report]. J Hepatol. 2016;64(Suppl 2):S821.
Dusheiko GM, Manns MP, Vierling JM, et al. Safety and tolerability of grazoprevir/elbasvir in patients with chronic hepatitis C (HCV) infection: integrated analysis of phase 2–3 trials [abstract no. 712 plus conference report]. Hepatology. 2015;62(Suppl 1):562A.
Zhang J, Nguyen D, Hu KQ. Chronic hepatitis C virus infection: a review of current direct-acting antiviral treatment strategies. N Am J Med Sci (Boston). 2016;9(2):47–54.
Asselah T, Boyer N, Saadoun D, et al. Direct-acting antivirals for the treatment of hepatitis C virus infection: optimizing current IFN-free treatment and future perspectives. Liver Int. 2016;36(Suppl 1):47–57.
US FDA. Clinical review appendum. 2016. http://www.accessdata.fda.gov/. Accessed 4 Apr 2017.
Woolston SL, Kim N. Cost and access to direct-acting antiviral agents. 2016. http://www.hepatitisc.uw.edu/. Accessed 4 Apr 2017.
Rosenthal ES, Graham CS. Price and affordability of direct-acting antiviral regimens for hepatitis C virus in the United States. Infect Agent Cancer. 2016;11:24.
Acknowledgements
During the peer review process, the manufacturer of elbasvir/grazoprevir was also offered an opportunity to review this article. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Conflict of interest
Zaina T. Al-Salama and Emma D. Deeks are salaried employees of Adis/Springer, are responsible for the article content and declare no relevant conflicts of interest
Additional information
The manuscript was reviewed by: A. Ascione, Department of Internal Medicine, Centre for Liver Disease, Fatebenefratelli Hospital, Naples, Italy; N. Izumi, Department of Gastroenterology and Hepatology, Musashino Red-Cross Hospital, Tokyo, Japan; S. Karatapanis, First Department of Internal Medicine, General Hospital of Rhodes, Rhodes, Greece.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Al-Salama, Z.T., Deeks, E.D. Elbasvir/Grazoprevir: A Review in Chronic HCV Genotypes 1 and 4. Drugs 77, 911–921 (2017). https://doi.org/10.1007/s40265-017-0739-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-017-0739-8