Abstract
Zoledronic acid (Reclast®, Aclasta®) is an intravenous, highly potent aminobisphosphonate approved worldwide, including in the USA, EU and Japan for use in patients with primary or secondary osteoporosis or low bone mass (approved indications vary between countries). Its high affinity to and long half-life in bone, and long duration of action, allow for once-yearly administration, which has the potential to improve adherence to therapy. Zoledronic acid once yearly for up to 3 years improved bone mineral density (BMD) at several skeletal sites, reduced fracture risk and bone turnover, and/or preserved bone structure and mass relative to placebo in clinical studies in patients with primary or secondary osteoporosis. While additional benefits were seen when treatment was continued for up to 6 years, as evidenced by a reduced risk of vertebral fractures and higher BMD relative to 3 years’ therapy, there was minimal advantage of treatment beyond 6 years. Therefore, in patients with low fracture risk, treatment discontinuation should be considered after approximately 5 years’ therapy. Zoledronic acid administered annually or once in 2 years was also effective in preventing bone loss in patients with low bone mass. Zoledronic acid was generally well tolerated, with the most common adverse events (AEs) being transient, mild-to-moderate post-infusion symptoms, which decreased with subsequent infusions. To conclude, zoledronic acid once yearly is an effective and generally well tolerated treatment option for patients with osteoporosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Improves BMD at several skeletal sites, reduces fracture risk and bone turnover and preserves bone structure and mass |
Most common AEs are transient, mild-to-moderate post-infusion symptoms, which decrease with subsequent infusions |
Once-yearly administration has the potential to improve treatment adherence |
1 Introduction
Osteoporosis is sometimes referred to as a silent disease, as it develops painlessly, often with no symptoms until a fracture occurs [1]. Both men and women are at risk of osteoporotic fractures, most commonly spinal, hip and wrist fractures [1]. Several pharmacological options are available for the prevention and treatment of primary and secondary osteoporosis, which can be broadly categorized into antiresorptive agents (e.g. bisphosphonates, estrogen) that preserve bone mineral density (BMD) by reducing bone resorption, and anabolic agents (e.g. teriparatide) that increase BMD by stimulating bone formation. Antiresorptive agents are a cornerstone for the treatment of osteoporosis [2], with several drug classes currently available, of which bisphosphonates are often recommended as first-line options for men and women at risk of osteoporotic fractures [3–7]. Zoledronic acid (Reclast®, Aclasta®), an intravenous, highly potent aminobisphosphonate, is one such antiresorptive agent approved worldwide (including in the USA [8], EU [9] and Japan [10]) for use in patients with primary or secondary osteoporosis or low bone mass (Sect. 5). This narrative review focuses on the therapeutic efficacy and tolerability of zoledronic acid 5 mg once yearly in these patients and summarizes relevant pharmacological data. Zoledronic acid is also approved for use in other indications, the discussion of which is beyond the scope of this review.
2 Pharmacological Properties of Zoledronic Acid
The pharmacological properties of intravenous zoledronic acid are well established and reviewed previously [11, 12]; therefore, a brief overview focussing on data relevant to osteoporosis, wherever possible, is provided.
2.1 Mechanism of Action
Zoledronic acid has high affinity for mineralized bone [8, 9, 13], accumulating rapidly after intravenous administration and localizing preferentially at sites of high bone turnover [8]. It is thought to be internalized during bone resorption via the endocytic activity of osteoclasts [14] and inhibits bone resorption by inhibiting farnesyl pyrophosphate synthase (FPPS) and preventing protein prenylation [15, 16]. The high binding affinity of zoledronic acid for mineralized bone [13] and for the FPPS active site [17] is thought to account for its long duration of action [9]. In vitro, the binding affinity of zoledronic acid for hydroxyapatite was higher than that of other bisphosphonates (binding affinity constants of 3.47 × 10−6 mol/L vs. 2.94, 2.36, 2.19, 1.19 and 0.72 × 10−6 mol/L for alendronic acid, ibandronic acid, risedronic acid, etidronic acid and clodronic acid, respectively) [13]. Inhibition of FPPS also results in the monocyte-mediated activation and expansion of γδ-T cells and subsequent release of proinflammatory cytokines (e.g. tumour necrosis factor-α, interleukin-6, interferon-γ), which are thought to cause the influenza-like symptoms (also referred to as acute-phase response (APR)] associated with aminobisphosphonates such as zoledronic acid (Sect. 4) [18, 19]. More recently, it has been suggested that the lower incidence of APR in patients with prior exposure to aminobisphosphonates may be because of a sustained decrease in circulating γδ-T cell levels after aminobisphosphonate treatment, probably due to the activation and extravasation of these cells into peripheral lymphoid tissues [20].
2.2 Pharmacokinetic Profile
The pharmacokinetic properties of intravenous zoledronic acid are based on data from 12 Japanese patients with primary osteoporosis who received a single ≥15-min infusion of zoledronic acid 5 mg [10] and 64 patients with cancer and bone metastases who received single or multiple 5- or 15-min infusions of zoledronic acid 2–16 mg every 28 days [8, 9]. Plasma concentrations of zoledronic acid increased rapidly after intravenous administration in cancer patients, with peak concentrations (Cmax) reached at the end of the infusion [8, 9]. Drug concentrations declined rapidly thereafter to <10% of Cmax after 4 h and <1% of Cmax after 24 h and remained at ≤0.1% of Cmax for a prolonged period [8, 9]. Similar results were seen in patients with osteoporosis; after reaching Cmax at the end of the infusion, plasma concentrations of zoledronic acid decreased rapidly to <1% of Cmax within 24 h and gradually thereafter to less than the lower limit of quantification after 336 h [10]. Zoledronic acid did not accumulate in plasma after repeat administration every 28 days in cancer patients [9].
Zoledronic acid is not metabolized and does not inhibit CYP enzymes [8, 9]; it is excreted unchanged renally, with 39% of a dose (in cancer patients) [8, 9] and 45% of a dose (in osteoporosis patients) [10] eliminated in the urine within 24 h. The remainder of the dose is largely bound to bone and released back into the systemic circulation very slowly and excreted renally [8, 9]. Zoledronic acid was eliminated in a triphasic manner in cancer patients, disappearing rapidly from the systemic circulation during the first two phases [half-life (t½) α and t½β of 0.24 and 1.87 h, respectively], presumably because of uptake into bone and renal excretion, followed by a prolonged terminal elimination phase (t½γ 146 h) [8, 9]. Renal clearance of zoledronic acid over 0–24 h in these patients was 3.7 L/h [8]; the total body clearance was 5.04 L/h, regardless of dose, age, gender, race or bodyweight [9].
No dosage adjustment of zoledronic acid is required in the elderly [9], in patients with hepatic impairment [9] and in patients with mild or moderate renal impairment [creatinine clearance (CLCR) ≥35 mL/min] (see also Sect 4.1) [8, 9]. As zoledronic acid is excreted renally, caution is advised when coadministering it with drugs that affect renal function (e.g. aminoglycosides or diuretics, because of a risk of dehydration [9]) [8, 9] or nephrotoxic drugs (e.g. NSAIDs) [8, 21]. Exposure to drugs that are largely excreted by the kidneys may increase when coadministered with zoledronic acid in renally impaired patients; consideration should be given to monitoring serum creatinine levels in at-risk patients [9]. No drug interaction studies have been undertaken with zoledronic acid; however, as zoledronic acid does not inhibit CYP enzymes, it is unlikely to affect the metabolic clearance of drugs metabolized by these enzymes [8, 9]. Due to its low plasma protein binding (approximately 43–55% [9]), zoledronic acid is unlikely to interact via displacement of highly plasma protein bound drugs [8, 9].
3 Therapeutic Efficacy of Zoledronic Acid
This section focuses on large (n > 200 patients) clinical trials assessing the efficacy of intravenous zoledronic acid 5 mg administered once yearly. Patients in all studies also received supplemental oral calcium and vitamin D and in one study (HORIZON-RFT) [22], the majority of patients were given an oral or intramuscular loading dose of ergocalciferol or colecalciferol 2 weeks prior to the first zoledronic acid infusion. Baseline values (where reported) are means, unless specified otherwise.
3.1 In Women with Postmenopausal Osteoporosis
3.1.1 HORIZON-PFT and Its Extensions
The efficacy of zoledronic acid in postmenopausal women with osteoporosis was assessed in a large, randomized, double-blind, placebo-controlled, multicentre, phase III study, HORIZON-PFT, and its extensions [23]. Eligible patients were aged 65–89 years, had a BMD T-score ≤−2.5 at the femoral neck with or without existing vertebral fracture, or a T-score of ≤−1.5 with radiological evidence of at least two mild or one moderate vertebral fracture(s). Hormone therapy or treatment with raloxifene, tamoxifen or calcitonin was permitted at baseline and during follow-up, and patients receiving prior bisphosphonate therapy could enter the study after a washout period. Patients were stratified into those who were not taking any osteoporosis medications at baseline (stratum 1) and those taking a permitted medication (stratum 2), and were randomized within each stratum to receive zoledronic acid or placebo for 3 years; 81% of patients received all three infusions in the core study [23]. Patients who had received 3 years’ treatment with zoledronic acid in the core study were randomized in the first extension to receive zoledronic acid or placebo for an additional 3 years (i.e. a total of 6 or 3 years’ zoledronic acid therapy) [24], and patients who had received at least the first and second zoledronic acid infusions in the first extension and completed the study were randomized in the second extension to receive a further 3 years of zoledronic acid or placebo (i.e. a total of 9 or 6 years’ zoledronic acid therapy) [25]. Coprimary endpoints in the core study were new vertebral fractures in stratum 1 and hip fractures in both strata over a median duration of 3 years [8, 23]. The primary endpoint in the first extension was the change in femoral neck BMD at 6 versus 3 years [24] and in the second extension was the change in total hip BMD at 9 versus 6 years [25].
3.1.1.1 Effect on Fractures
Zoledronic acid was effective in reducing the risk of osteoporotic fractures in women with postmenopausal osteoporosis [23]. In stratum 1, patients receiving zoledronic acid had significantly lower incidences of morphometric vertebral fractures after 1 year’s [1.5 vs. 3.7%; relative risk (RR) 0.40], 2 years’ (2.2 vs. 7.7%; RR 0.29) and 3 years’ (coprimary endpoint; 70% reduction; Table 1) treatment (all p < 0.001) than patients receiving placebo. The risk of hip fractures in strata 1 and 2 was also significantly reduced by 41% after 3 years’ therapy (Table 1; coprimary endpoint). In addition, patients receiving zoledronic acid had significantly (p < 0.001) lower incidences of nonvertebral fractures (Table 1), any clinical fractures (Table 1), clinical vertebral fractures [cumulative incidence 0.5 vs. 2.6%; hazard ratio (HR) 0.23; 95% CI 0.14–0.37] and multiple morphometric fractures (0.2 vs. 2.3%; HR 0.11; 95% CI 0.05–0.23) than patients receiving placebo for 3 years. Patients in the zoledronic acid group also had significantly less height loss than those in the placebo group (−4.2 vs. −7.0 mm; p < 0.001) [23].
Preplanned subgroup analyses showed that zoledronic acid reduced the risk of fractures across a broad range of patient subgroups based on demographics and baseline risk factors, such as the presence of vertebral fractures, the femoral neck T-score and prior bisphosphonate treatment [26]. With the exception of significant (p < 0.05) interactions between treatment and body mass index (BMI) and between treatment and CLCR for vertebral fractures, there were no significant treatment-by-subgroup interactions for vertebral, hip and nonvertebral fractures over 3 years [26].
During longer-term therapy in the first extension, the risk of morphometric vertebral fractures after 6 years’ treatment was significantly reduced by 49% in patients who received 6 versus 3 years’ zoledronic acid therapy, but no significant between-group differences were seen for nonvertebral, clinical vertebral, hip or all clinical fractures (Table 1) [24]. These results suggest benefit of longer-term treatment with zoledronic acid in patients at high risk of fractures, particularly vertebral fractures [24]. In the second extension study, fractures were too few for a meaningful comparison and no significant differences were seen for morphometric vertebral fractures (3 vs. 5 patients) or all clinical fractures (10 vs. 9 patients) between patients receiving 9 years (n = 95) versus 6 years (n = 95) of zoledronic acid therapy, suggesting little additional benefit of continuing treatment after 6 years [25].
3.1.1.2 Effect on Bone Mineral Density
Three years’ treatment with zoledronic acid significantly increased BMD [assessed by dual-energy X-ray absorptiometry (DXA)] at the lumbar spine (6.71% increase), total hip (6.02% increase) and femoral neck (5.06% increase) relative to placebo (Table 2) [23]. A subsequent analysis found that the 3-year change in total hip BMD explained 40% of the treatment effect in reducing vertebral fractures and 61% of the treatment effect in reducing nonvertebral fractures [27]. In addition, subgroup analyses showed that zoledronic acid increased femoral neck BMD across a broad range of patient subgroups, with no significant treatment-by-subgroup interactions for the percentage and/or absolute changes in BMD [26]
During longer-term therapy in the first extension study, femoral neck BMD from year 3 to 6 (primary endpoint) was maintained in patients receiving zoledronic acid for 6 years and reduced slightly in those receiving the drug for 3 years (mean change +0.24 vs. −0.80%), with a significant between-group difference of 1.04% (p = 0.0009); BMD in both groups remained above pretreatment levels [24]. Significant benefits with longer-term therapy were also seen at the total hip (mean change −0.36 with 6 years’ vs. −1.58% with 3 years’ zoledronic acid therapy) and lumbar spine (3.20 vs. 1.18%) during this period (both p ≤ 0.0002) [24]. In the second extension study, there were no significant differences between patients receiving 9 versus 6 years of zoledronic acid in terms of the total hip BMD (mean change −0.54 years vs. −1.31%; primary endpoint) and femoral neck BMD (−1.11 vs. −1.17%) [25].
3.1.1.3 Effect on Bone Turnover Markers
Bone turnover marker (BTM) levels were significantly decreased after the first infusion of zoledronic acid, with the low levels sustained over the 3-year study duration and no progressive decrease after the second and third infusions [28]. β-C-terminal telopeptide of type I collagen (CTX) and bone-specific alkaline phosphatase (BALP) levels were assessed in 604 patients and procollagen type 1 amino-terminal propeptide (P1NP) levels were assessed in 1245 patients [28]. At 1 year, CTX, BALP and P1NP levels in patients receiving zoledronic acid decreased by a mean of 59, 30 and 58%, respectively (all p < 0.001) [23], and at 3 years by a median of 51, 30 and 56% (p value not reported) [28]. By contrast, BTM levels in patients receiving placebo were maintained at baseline levels over this period [23, 28]. Although substantially decreased, BTM levels in the majority (>57%) of patients receiving zoledronic acid remained within the premenopausal reference range (established in 637 healthy premenopausal women from the OFELY study) [23, 28]. CTX levels after the third infusion of zoledronic acid sharply decreased (by 60%) within 9–11 days (indicating a rapid inhibition of osteoclastic activity) and then increased gradually, with levels at 3 years similar to those before the third infusion (median 0.17 vs. 0.16 ng/mL), suggesting that bone turnover is still reactive after the third infusion [28]. A subsequent analysis of the study found that the 1-year change in log P1NP levels explained 58% of the reduction in risk of new vertebral fractures with zoledronic acid relative to placebo [27].
During longer-term treatment with zoledronic acid in the first extension study, P1NP levels increased at 6 versus 3 years both in patients who continued treatment throughout and in those who switched to placebo after initial 3 years’ therapy, with a significantly greater increase seen in patients receiving placebo (+19 vs. +33%; p = 0.0001); CTX and BALP levels were also increased in both groups, but results were limited by small sample sizes [24]. In the second extension study, at 9 years, there were no meaningful differences in BTM levels between patients who continued treatment for 9 years and in those who discontinued therapy after 6 years [25]. BTM levels in the two extensions and in all treatment groups remained below pretreatment levels throughout and were within the premenopausal reference range at all but one assessment [24, 25]. Taken together with the effects on BMD (Sect. 3.1.1.2), these results suggest residual effects of zoledronic acid and the potential for most patients to discontinue therapy for up to 3 years after three annual infusions, and almost all patients could discontinue therapy after six annual infusions and expect to maintain treatment benefits for up to 3 years [25]. Based on this, it is recommended in the USA and EU that treatment discontinuation should be considered after approximately 5 years’ therapy in patients who are at low fracture risk (Sect. 5).
3.1.1.4 Effect on Bone Histology
Microcomputer tomography of iliac crest bone biopsies from 50 and 49 patients in the zoledronic acid and placebo groups, respectively, showed that trabecular bone structure and mass were preserved following three annual infusions of zoledronic acid, as indicated by significantly higher trabecular bone volume (median 16.6 vs. 12.8%) and trabecular number (1.36 vs. 1.22/mm), and significantly decreased trabecular separation (0.72 vs. 0.80 mm) with zoledronic acid than placebo (all p < 0.05) [29]. Zoledronic acid also significantly (p < 0.05) reduced bone turnover (median 63% reduction in activation frequency) and improved osteoblast function relative to placebo, as indicated by several quantitative parameters of bone remodelling assessed in up to 59 biopsies from patients receiving zoledronic acid and 52 biopsies from patients receiving placebo. Evidence of ongoing bone remodelling was seen in 81 of the 82 biopsies from patients receiving zoledronic acid [29].
3.1.1.5 Health-Related Quality of Life (HR-QOL)
HR-QOL was assessed using the mini-Osteoporosis Quality of Life Questionnaire in a subset of patients from HORIZON-PFT (n = 712 and 710 in zoledronic acid and placebo groups) [30]. While the overall summary score did not differ significantly between the zoledronic acid and placebo groups at any timepoint, significant benefits with zoledronic acid were seen in some of the domains over the course of the study [30]. For example, zoledronic acid significantly (p < 0.05) improved the ‘overall symptom’ domain and the item ‘pain’ at 1 and 3 years and the item ‘standing pain’ at 1 year [30]. According to a prespecified analysis of HORIZON-PFT, although the incidence of back pain over 3 years was high in women with postmenopausal osteoporosis (56.6% with zoledronic acid vs. 59.5% with placebo; p = 0.014), patients receiving zoledronic acid had 18 fewer days of back pain (mean 264 vs. 282 days), 11 fewer days of limited activity (mean 61 vs. 72 days) and were less likely to experience ≥7 days of bed rest due to a fracture (RR 0.58; 95% CI 0.47–0.72) or ≥7 days of limited activity due to a fracture (0.67; 95% CI 0.58–0.78) than patients receiving placebo (all p < 0.05; self-reported parameters) [31].
3.1.2 Versus Comparators
Two 1-year, randomized, double-blind, multicentre studies assessed the efficacy of a single dose of intravenous zoledronic acid versus oral alendronic acid 70 mg once weekly in women with postmenopausal osteoporosis previously treated with alendronic acid [intent-to-treat (ITT) n = 113 and 112)] [32], or versus subcutaneous denosumab 60 mg every 6 months (a fully human monoclonal antibody against RANKL) in postmenopausal women with osteoporosis previously treated with oral bisphosphonates (ITT n = 322 and 321) [33].
3.1.2.1 Compared with Alendronic Acid
Postmenopausal women aged 45–79 years who had been treated with alendronic acid for ≥1 year immediately prior to randomization and had a T-score of ≤−2.0 at the lumbar spine or femoral neck prior to starting alendronic acid were eligible [32]. The mean duration of prior alendronic acid therapy was approximately 4 years.
Postmenopausal women with low bone mass can be switched from oral alendronic acid once weekly to zoledronic acid once yearly, with therapeutic benefits maintained for at least 1 year after a single dose of zoledronic acid [32]. At 1 year, the mean change from baseline in BMD at the lumbar spine (primary endpoint) with zoledronic acid was noninferior to that with alendronic acid both in the ITT (0.167 vs. 0.813%; baseline 0.86 and 0.88 g/cm2, respectively) and modified-ITT (0.120 vs. 0.828%) populations. Unlike in patients receiving alendronic acid, in whom BTMs [CTX, BALP, P1NP and urine N-telopeptide of type 1 collagen (NTX)] remained at or close to baseline levels throughout the study (albeit significantly lower than baseline at some timepoints), by 3 months, BTM levels with zoledronic acid were decreased significantly (p < 0.05) from baseline, returning close to baseline by 6 months and then increasing gradually to levels significantly (p < 0.05) higher than baseline (but within the range for premenopausal women) by 1 year. This suggests that in patients previously exposed to long-term oral alendronic acid and then switched to zoledronic acid, bone turnover does not remain maximally suppressed and recovers from the acute effects of the potent intravenous bisphosphonate zoledronic acid. Transilial biopsies at study end from 10 patients in the zoledronic acid group and 13 patients in the alendronic acid group also showed evidence of bone turnover in both treatment groups [32].
3.1.2.2 Compared with Denosumab
Eligible patients were ambulatory postmenopausal women aged ≥55 years who were receiving oral bisphosphonate therapy for ≥2 years immediately prior to screening, had a T-score of ≤−2.5 at the lumbar spine, total hip or femoral neck, ≥2 lumbar vertebrae and one hip evaluable by DXA, and baseline CTX levels of ≤500 pg/mL [33].
At 1 year, denosumab was noninferior to zoledronic acid in terms of the mean change from baseline in BMD at the lumbar spine (primary endpoint; 3.2 vs. 1.1%; baseline T-score approximately −2.7), with a subsequent analysis demonstrating its superiority over zoledronic acid (p < 0.0001 for noninferiority and superiority) [33]. Denosumab was also noninferior (and superior) to zoledronic acid in terms of the mean change from baseline in BMD at the total hip (1.9 vs. 0.6%; baseline T-score −1.93; p < 0.0001 for noninferiority and superiority), and superior to zoledronic acid for the mean changes from baseline in BMD at the femoral neck (1.2 vs. −0.1%; p < 0.0001) and 1/3 radius (0.6 vs. 0%; p = 0.018). CTX and P1NP levels (assessed in 61 and 56 patients in the denosumab and zoledronic acid groups, respectively) decreased from baseline in both treatment groups, with the median decrease significantly (all p < 0.05) greater with denosumab than with zoledronic acid at all timepoints from day 10 for CTX and month 1 for P1NP. While the decrease in BTM levels with denosumab persisted over the 6-month dosing interval, BTM levels with zoledronic acid increased gradually after an initial decline within 3 months of therapy, which may explain the smaller gains in BMD with zoledronic acid relative to denosumab. Osteoporosis-related fractures, assessed as adverse events (AEs), were reported in 15 patients receiving zoledronic acid and seven patients receiving denosumab [33].
3.1.3 Other Studies/Analyses
3.1.3.1 In Chinese Patients
The efficacy of zoledronic acid in Chinese women was assessed in a post hoc subgroup analysis of patients from Hong Kong and Taiwan who were participating in HORIZON-PFT [34] and in a randomized, placebo-controlled, single-centre trial in women from China who had postmenopausal osteoporosis [35]. The HORIZON-PFT subgroup analysis showed that as in the overall population (Sect. 3.1.1.1), Chinese patients receiving zoledronic acid (n = 163) had significantly lower risks of morphometric vertebral fractures (8 vs. 16.5% in stratum 1; RR 0.48; 95% 0.24–1.00) and clinical vertebral fractures (0 vs. 2.7%) than patients receiving placebo (n = 160) at 3 years (both p < 0.05) [34]. No significant between-group differences were seen in the incidences of hip (0 vs. 1.9%), any clinical (5.7 vs. 9.4%) and nonvertebral (5.7 vs. 6.7%) fractures with zoledronic acid relative to placebo [34]. Patients in the zoledronic acid group had significant (p < 0.001) increases in BMD at the total hip (mean 4.9% increase), femoral neck (4.3%) and femoral trochanter (7.0%) relative to patients in the placebo group [34].
Benefits of zoledronic acid therapy were also seen in the single-centre study, which enrolled Chinese women (mean age approximately 57 years) with a BMD T-score of ≤−2.5 at the femoral neck and no evidence of vertebral fractures, or a T-score of ≤1.5 and ≥2 vertebral fractures [35]. At 2 years, patients receiving zoledronic acid (ITT n = 242) had a significantly lower overall risk of fractures (OR 0.54; 95% CI 0.29–0.98) and significantly lower mean incidence of fractures at the trochanter (7.9 vs. 13.3%; p < 0.05) than patients receiving placebo (n = 241), but no significant between-group differences were seen in the mean incidences of fractures at the hip (5 vs. 8.7%), femoral neck (2.1 vs. 3.7%) and at the L1–L4 vertebrae (2.5 vs. 4.2%). BMD was significantly (p < 0.05) increased with zoledronic acid relative to placebo at these sites [35].
3.1.3.2 In Combination with Teriparatide
The efficacy of zoledronic acid in combination with subcutaneous teriparatide 20 μg/day was assessed in a 1-year, randomized, partial double-blind, multicentre study in postmenopausal women with osteoporosis [36]. Patients aged 45–89 years with a BMD T-score of ≤−2.5 at the femoral neck, total hip or lumbar spine, or a BMD T-score of ≤−2.0 at any site plus ≥1 vertebral or nonvertebral fractures were eligible. Treatment-naïve patients were randomized to receive zoledronic acid plus teriparatide (ITT n = 137), placebo plus teriparatide (n = 138) or zoledronic acid alone (n = 137); zoledronic acid and placebo were administered in a blinded manner, while teriparatide administration was open-label [36]. Discussion focuses on the comparison of combination therapy versus teriparatide or zoledronic acid alone.
At 1 year, zoledronic acid plus teriparatide was noninferior to teriparatide alone in increasing BMD at the lumbar spine (primary endpoint) both in the ITT population [least-squares (LS) mean change from baseline 7.5% with the combination, 7.0% with teriparatide and 4.4% with zoledronic acid] and in the per-protocol population (7.3, 7.3 and 4.3%, respectively) (BMD at baseline 0.73 g/cm2) [36]. Subsequent superiority testing did not show a significant difference between combination therapy and teriparatide. At all timepoints during the study, BMD was significantly (p < 0.05) increased with the combination versus teriparatide at the total hip, femoral neck and trochanter. Significantly greater increases in BMD were also seen with the combination versus zoledronic acid at the lumbar spine at all timepoints and at the total hip at week 13 (all p < 0.05). The incidence of clinical fractures (assessed as AEs) did not differ significantly between patients receiving combination therapy and those receiving teriparatide (4 vs. 8 patients), but was significantly lower with the combination than with zoledronic acid alone (4 vs. 13 patients; risk ratio 0.31; 95% CI 0.10–0.92; p = 0.04) [36].
Concomitant teriparatide reduced the duration of zoledronic acid-induced reduction of bone resorption, possibly because zoledronic acid was removed more rapidly from the bone surface in the presence of teriparatide [36]. After an initial decline, CTX and PINP levels with combination therapy increased gradually from 1 and 2 months, respectively, to levels higher than baseline levels over the last 6 months of therapy; by contrast, CTX and P1NP levels with zoledronic acid reduced within 1 and 2 months, respectively, of the infusion, and remained below baseline levels throughout the 1-year study period [36].
3.2 In Patients with Low-Trauma Hip Fracture
The efficacy of zoledronic acid in the prevention of new clinical fractures in women and men who have undergone recent hip fracture was assessed in the randomized, double-blind, placebo-controlled, multicentre HORIZON-RFT [22]. Eligible patients (aged ≥50 years) were required to have undergone surgery to repair a hip fracture sustained with minimal trauma and were unwilling or unable to take oral bisphosphonates; patients with prior bisphosphonate or parathyroid hormone therapy were permitted entry after a washout period. Patients were monitored for ≤5 years; the median duration of follow-up was 1.9 years and 71.3% of patients completed the study [22].
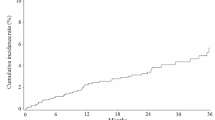
Zoledronic acid administered within 90 days after repair of a low-trauma hip fracture was effective in reducing the risk of new clinical fractures (i.e. fractures other than facial and digital fractures and fractures of abnormal bone), with a significant (p = 0.001) 35% reduction in risk with zoledronic acid relative to placebo at 2 years (primary endpoint; Table 1) [22]. Significant (p = 0.02) separation between the Kaplan-Meier curves for the cumulative incidence of clinical fractures in the zoledronic acid and placebo groups was seen after as early as 1 year of therapy (post hoc analysis). The mean time to clinical fracture in patients who had a fracture was 39.8 months with zoledronic acid and 36.4 months with placebo. The rates of new clinical vertebral and new clinical nonvertebral fractures were also significantly lower with zoledronic acid than with placebo, but there was no significant between-group difference for hip fractures (Table 1) [22].
Zoledronic acid significantly (p < 0.001) improved BMD at the total hip and femoral neck at 1, 2 and 3 years in patients receiving treatment after repair of low-trauma hip fracture (Table 2) [22]. The improvements in BMD at the total hip and femoral neck at 1 and 2 years with zoledronic acid relative to placebo were consistent across a broad range of subgroups (e.g. based on age, fracture history, time to first infusion) [37]. For example, for total hip BMD, there were no significant treatment-by-subgroup interactions for all subgroups, except for those based on gender, BMI and baseline T-score [37]. Greater improvements in total hip BMD at 1 year were seen in females [37, 38], patients with BMI ≤22.6 kg/m2 and baseline femoral neck BMD T-score of ≤−2.5 [37] (nominal p < 0.05 for interaction). There were no significant treatment-by-subgroup interactions for total hip BMD in any subgroup at 2 years [37, 38].
When patients were stratified based on the timing of first infusion at 2-week intervals from surgical repair, with the exception of the subgroup of patients who received the first infusion ≤2 weeks after surgery, a consistent reduction in the risk of overall clinical fractures (HRs of <1) was seen at 2 years in all subgroups, regardless of the timing of infusion (post hoc analysis) [39]. However, a statistically significant (p < 0.05) reduction in the risk of clinical fractures was seen only in the largest group, i.e. patients who received the first infusion 4–6 weeks after surgical repair (24% of the population). For total hip BMD, a significant (p < 0.05) increase relative to placebo was seen in all subgroups that received zoledronic acid >2 weeks (but not in those who received treatment ≤2 weeks) after surgical repair. By 2 years, all subgroups, regardless of the timing of infusion, had significant (p < 0.05) improvement in total hip BMD with zoledronic acid relative to placebo [39]. Based on these results, in the EU, it is recommended that zoledronic acid be administered ≥2 weeks after hip fracture repair (Sect. 5).
Some HR-QOL benefits were seen with zoledronic acid in a secondary predefined exploratory analysis [40]. Significantly (p < 0.005) greater increases from baseline in Euro QOL five dimensions questionnaire (EQ-5D) visual analogue scale (VAS) scores were seen with zoledronic acid relative to placebo at 2 years and at study end (5 years), but not at 1 and 3 years [40]. EQ-5D utility scores did not differ significantly between the zoledronic acid and placebo groups at any timepoint [40].
3.3 In Japanese Patients with Primary Osteoporosis
The 2-year, randomized, double-blind, placebo-controlled, multicentre, ZONE study assessed the efficacy of zoledronic acid in 665 male or female Japanese patients (aged 65–89 years) with primary osteoporosis (according to the Japanese Society for Bone and Mineral Research criteria [41]) and 1–4 vertebral fractures from the fourth thoracic to the fourth lumbar vertebra [21]. Patients with prior bisphosphonate therapy within 2 years of the study were excluded. As in the pivotal study HORIZON-PFT, zoledronic acid significantly (p < 0.05) reduced the incidence of new vertebral fractures (primary endpoint; Table 1), nonvertebral fractures (Table 1), any clinical fractures (Table 1) and clinical vertebral fractures (1.7 vs. 5.6%) at 2 years in Japanese patients with primary osteoporosis. BMD at the total hip, femoral neck and lumbar spine was also significantly (p < 0.0001) improved with zoledronic acid relative to placebo (Table 2). CTX levels in the zoledronic acid group decreased in the first week after both the first and the second infusion and increased slightly thereafter, but were significantly (p < 0.0001) less than in the placebo group throughout the study. BALP levels in the zoledronic acid group decreased gradually over 3 months and then remained generally stable and were significantly (p < 0.01) less than in the placebo group over the 2-year period [21].
3.4 In Men with Primary or Secondary Osteoporosis
A 2-year, randomized, double-blind, placebo-controlled, multicentre study assessed the efficacy of zoledronic acid in men (aged 50–85 years) with primary osteoporosis or osteoporosis associated with low testosterone levels (modified ITT n = 553 and 574 in the zoledronic acid and placebo groups) [42]. Patients included were required to have: a BMD T-score of ≤−1.5 at the total hip or femoral neck and 1–3 vertebral fractures of mild or moderate grade; men without fractures could be included if they had a BMD T-score of ≤−2.5 at the total hip, femoral neck or lumbar spine. Patients with prior osteoporotic therapies, including bisphosphonates, could be included after a washout period. Zoledronic acid was effective in reducing the risk of new vertebral fractures in men with osteoporosis, as indicated by significantly (p = 0.002) fewer patients in the zoledronic acid group than in the placebo group having new morphometric vertebral fractures over 2 years (primary endpoint; 1.6 vs. 4.9%; RR 0.33; 95% CI 0.16–0.70). Zoledronic acid also significantly (p < 0.05) reduced the risk of new morphometric vertebral fractures at 1 year (0.9 vs. 2.8%; RR 0.32; 95% CI 0.12–0.88), new moderate-to-severe morphometric vertebral fractures at 1 year (81% reduction) and 2 years (63% reduction), and new or worsening vertebral fractures at 2 years (59% reduction), relative to placebo. BMD at the lumbar spine, total hip and femoral neck was significantly (p < 0.05) improved with zoledronic acid relative to placebo over the 2-year study period. In addition, height was reduced to a significantly (p < 0.01) lesser extent with zoledronic acid both at 1 year (LS mean change from baseline −0.8 vs. −2.5 mm) and 2 years (−2.2 vs. −4.5 mm) [42].
Another 2-year, randomized, double-blind, multicentre study compared the efficacy of zoledronic acid versus alendronic acid 70 mg once weekly in men with primary osteoporosis or osteoporosis associated with hypogonadism (ITT n = 154 and 148 in the respective groups) [43]. The study included patients (aged 25–85 years) with a BMD T-score of −2 at the femoral neck and −1 at the lumbar spine, or those with a score of −1 at the femoral neck and a prior low-trauma vertebral or nonvertebral fracture or with a radiographic vertebral fracture identified during screening. All but three patients included were naïve to bisphosphonate treatment. Zoledronic acid was noninferior to alendronic acid in increasing BMD at the lumbar spine (primary endpoint; LS mean change from baseline 6.1 vs. 6.2%; baseline 0.85 g/cm2), total hip and femoral neck at 2 years. Superiority of zoledronic acid over alendronic acid for BMD at these sites was not demonstrated in a subsequent analysis. While CTX, NTX, P1NP and BALP levels decreased from baseline in both treatment groups over the first 18 months, at most assessments, patients receiving zoledronic acid had significantly (p < 0.05) lower levels of CTX, NTX and P1NP than patients receiving alendronic acid; BALP levels were generally similar between the two treatment groups. At study end, BTM levels did not differ significantly between the two groups. Of the 275 patients who completed a questionnaire, 59–75% of patients preferred zoledronic acid, found the drug more convenient and satisfying, and were willing to take it over a long period (versus 12–15% for alendronic acid; all p < 0.0001) [43].
3.5 In Patients with Glucocorticoid-Induced Osteoporosis
The 1-year, randomized, double-blind, multicentre HORIZON study compared the efficacy of zoledronic acid versus risedronic acid 5 mg/day for the treatment (ITT n = 272 and 273 in the respective groups) and prevention (n = 144 in each treatment group) of glucocorticoid-induced osteoporosis (GIO) [44]. Patients (men or women aged 18–85 years) included were required to be receiving oral prednisolone ≥7.5 mg/day (or equivalent) and were expected to continue glucocorticoid therapy for ≥1 year; patients with prior bisphosphonate therapy were excluded [44]. At 1 year, zoledronic acid was noninferior to risedronic acid in terms of the increase from baseline in lumbar spine BMD (primary endpoint) both in the treatment cohort (LS mean change 4.1 vs. 2.7%) and the prevention cohort (2.6 vs. 0.64%), with a subsequent superiority analysis showing significant (p ≤ 0.005) benefit with zoledronic acid over risedronic acid in both cohorts (baseline BMD 0.90 and 0.96 g/cm2, respectively) [44]. Significant (p ≤ 0.0005) improvements in BMD with zoledronic acid relative to risedronic acid were also seen at the trochanter and total hip in both cohorts [44]. Zoledronic acid also preserved or improved BMD to a greater extent than risedronic acid in the subgroup of men, as indicated by significantly (p < 0.05) greater increases in BMD at the lumbar spine and total hip at 1 year in the treatment and prevention cohorts [45].
CTX and P1NP levels in both cohorts were reduced from baseline in both treatment groups, with significantly (p < 0.05) greater reductions seen with zoledronic acid than with risedronic acid at all timepoints from 9–11 days onwards, with the exception of P1NP levels in the prevention cohort at the 9–11 day assessment [44]. It has been suggested that the faster and greater inhibition of bone resorption with zoledronic acid may help in preventing GIO, as a glucocorticoid therapy-associated decrease in BMD and resulting increase in the risk of fracture may occur soon after initiation of glucocorticoid therapy. HR-QOL (assessed by the EQ-5D VAS and utility scores) was generally similar between the two groups over the 1-year study period [44].
3.6 In Postmenopausal Women with Low Bone Mass
A 2-year, randomized, double-blind, placebo-controlled, multicentre study assessed the efficacy of zoledronic acid in postmenopausal women (aged ≥45 years) with low bone mass. Women with a BMD T-score of <−1 and >−2.5 at the lumbar spine and a BMD T-score of >−2.5 at the femoral neck were included [46]. Patients received zoledronic acid at randomization and at 1 year (i.e. two infusions of zoledronic acid; ITT n = 198), zoledronic acid at randomization and placebo at 1 year (i.e. one infusion of zoledronic acid; n = 181) or placebo at randomization and 1 year (n = 202). Once-yearly zoledronic acid or a single dose of the agent prevented bone loss at the lumbar spine and proximal femur sites in postmenopausal women with low bone mass. At 2 years, significant (p < 0.001) improvements from baseline in lumbar spine BMD were seen in patients receiving two infusions or one infusion of zoledronic acid relative to placebo (LS mean change 5.18 and 4.42 vs. −1.32%; BMD at baseline 0.86 g/cm2). Significant (p < 0.001) increases in BMD were also seen at 1 year at the lumbar spine and at 1 and 2 years at proximal femoral sites (total hip, trochanter and femoral neck). CTX, P1NP and BALP levels were significantly (p < 0.001) reduced with both regimens of zoledronic acid relative to placebo at all timepoints during the study [46].
4 Tolerability of Zoledronic Acid
Zoledronic acid was generally well tolerated in clinical studies in patients with primary or secondary osteoporosis or low bone mass (Sect. 3), with the most common AEs being mild-to-moderate post-infusion symptoms, which generally resolved within 3 days and decreased with subsequent infusions. Discussion in this section is based largely on the two large, placebo-controlled studies, HORIZON-PFT and HORIZON-RFT, and supplemented with relevant data from other studies and the US [8] and EU [9] prescribing information.
In HORIZON-PFT in women with postmenopausal osteoporosis, significantly more patients in the zoledronic acid group than in the placebo group experienced AEs over 3 years’ treatment (95.5 vs. 93.9%; p = 0.002), largely because of post-infusion symptoms occurring most frequently after the first infusion (incidence of the five most common symptoms was 31.6 vs. 6.2% with placebo) compared with subsequent infusions (6.6 vs. 2.1% with placebo after the second infusion and 2.8 vs. 1.1% after the third infusion) (all p < 0.001 vs. placebo) [23]. The most common post-infusion symptoms were pyrexia (16.1 vs. 2.1%), myalgia (9.5 vs. 1.7%), influenza-like symptoms (7.8 vs. 1.6%), headache (7.1 vs. 2.3%) and arthralgia (6.3 vs. 2.0%) (all p < 0.001) [23]. A subsequent analysis of HORIZON-PFT found that post-infusion symptoms associated with zoledronic acid included >30 AEs, which were grouped into five clusters for convenience: fever, musculoskeletal events (e.g. pain, stiffness), gastrointestinal (GI) events (e.g. nausea, vomiting, diarrhoea), eye inflammation and general events (e.g. influenza-like symptoms, headache, fatigue) (all p < 0.05 vs. placebo) [47]. In this analysis, after the first infusion, the overall incidence of post-infusion symptoms was almost four times higher with zoledronic acid than with placebo (42.4 vs. 11.7%; p < 0.0001), with most (90%) AEs being of mild or moderate severity [47]. The peak onset of post-infusion symptoms was within 1 day of dose administration and the median duration of symptoms was 3 days [47]. Non-Japanese Asians and Pacific Islanders, younger patients and those taking NSAIDs were at significantly higher risk of post-infusion symptoms, while Latin Americans, patients with prior bisphosphonate therapy or calcitonin therapy, smokers and patients with diabetes were at significantly lower risk (all p < 0.05) [47].
In HORIZON-RFT in patients with low-trauma hip fracture, AEs occurred in 82.3% of patients in the zoledronic acid group and 80.6% of patients in the placebo group over 3 years’ treatment, with the most common post-infusion symptoms being pyrexia (6.9 vs. 0.9%; p < 0.001), myalgia (3.1 vs. 0.9%; p < 0.001), arthralgia (3.1 vs. 2.2%), headache (1.5 vs. 0.9%) and influenza-like symptoms (0.6 vs. 0.3%) [22]. Overall, the incidence of post-infusion symptoms was lower in HORIZON-RFT than in HORIZON-PFT, which was thought to be because of standard oral paracetamol (acetaminophen) provided at the time of infusion and, as needed, over the next 72 h in patients without a contraindication for paracetamol [8, 22]. Indeed, a randomized double-blind multicentre study in postmenopausal osteopenic women showed that significantly (p < 0.0001) fewer patients receiving zoledronic acid plus ibuprofen (ITT n = 137) or zoledronic acid plus paracetamol (n = 135) had increased oral temperature (≥1 °C above 37.5 °C) within 3 days of the infusion compared with patients receiving zoledronic acid plus placebo (n = 137) (36.8 and 37.3 vs. 63.5%); in the placebo plus placebo group (n = 72), 11.1% of patients had increased oral temperature [48].
In HORIZON-PFT and HORZON-RFT, there were no significant differences between the zoledronic acid and placebo groups for the incidence of serious AEs (29.2 vs. 30.1% [23]; 38.3 vs. 41.2% [22]) and the rate of discontinuation of follow-up due to AEs (2.1 vs. 1.8% [23]; 2.0 vs. 1.7% [22]). The incidence of death in the zoledronic acid and placebo groups in HORIZON-PFT was 3.4 and 2.9% [23], and in HORIZON-RFT was 9.6 and 13.3% [p < 0.01; 1.0 vs. 1.7% because of cardiovascular disease (CV) and 0.7 vs. 0.7% because of cerebrovascular disease] [22].
4.1 Other Adverse Events
Renal impairment (i.e. increased levels of serum creatinine) and rare cases of acute renal failure have been reported in patients receiving intravenous bisphosphonates [8]. In HORIZON-PFT, renal safety of zoledronic acid was assessed in a subgroup of 5035 patients 9–11 days after the infusion [23]. In these patients, a transient increase from baseline of >0.5 mg/dL in serum creatinine levels was seen in significantly more patients in the zoledronic acid group than in the placebo group (1.2 vs. 0.4%; p = 0.001), with levels returning to ≤0.5 mg/dL of preinfusion levels in >85% of patients within 30 days, and in the remaining patients by the next infusion [23]. Longer-term (3 years) assessment of renal safety in the total safety population (n = 7714) found that these transient, short-term increases in serum creatinine levels with zoledronic acid, particularly in patients with an estimated CLCR of 30–35 mL/min, were not associated with long-term deterioration of renal function [49]. In HORIZON-RFT, there was no significant difference between the zoledronic acid and placebo groups for the proportion of patients with a >0.5 mg/dL increase in serum creatinine levels (6.2 vs. 5.6%) [22]. Zoledronic acid has been associated with acute renal impairment and, rarely, with renal failure requiring dialysis or with fatal outcomes, particularly in patients with pre-existing renal dysfunction or other risk factors (e.g. advanced age, concomitant use of nephrotoxic drugs or diuretics). Therefore, caution is advised when using zoledronic acid in patients with chronic renal impairment [8] or moderate renal impairment [21] and its use is contraindicated in patients with severe renal impairment (CLCR <35 mL/min) [8–10], acute renal failure [8] or in dehydrated patients (due to a risk of acute renal failure) [10].
Serious atrial fibrillation was reported in significantly more patients in the zoledronic acid group than in the placebo group in HORIZON-PFT (1.3 vs. 0.5%; p < 0.001), but there were no significant between-group differences for any atrial fibrillation event (2.4 vs. 1.9%), stroke (2.3 vs. 2.3%), death from stroke (0.5 vs. 0.3%), myocardial infarction (1.0 vs. 1.2%) or death from CV causes (1.0 vs. 0.9%) [23]. In HORIZON-RFT, CV AEs occurred in <5% of patients in the zoledronic acid and placebo groups, with no significant between-group differences for any of the events [22]. A subsequent US FDA review of safety data on the risk of serious atrial fibrillation with bisphosphonates did not find a clear association between the use of these agents and the rate of serious or any atrial fibrillation [50].
The use of bisphosphonates, including zoledronic acid, has been associated with osteonecrosis of the jaw (ONJ), with most cases occurring in cancer patients undergoing dental procedures during bisphosphonate therapy [8]. In HORIZON-PFT, there was one case each of potential ONJ in the zoledronic acid and placebo groups [23] and no reports in either group in HORIZON-RFT [22]. Pooled data from five clinical trials [22, 23, 43, 44, 46] showed that ONJ occurred very rarely (<1 in 14,200 patient-treatment years) in patients with primary or secondary osteoporosis who had received zoledronic acid therapy [51]. It is recommended that a routine oral exam and any appropriate preventative dentistry be performed prior to initiating treatment with zoledronic acid [8, 9]. There have been reports of atypical, low energy or low-trauma fractures of the femoral shaft in patients receiving bisphosphonates, usually during long-term therapy for osteoporosis [8, 9]; however, causality has not been established [8]. Signs and symptoms of fracture should be assessed and interruption of zoledronic acid therapy should be considered in any patient presenting with an atypical femur fracture, pending an evaluation of the patient [8, 9].
Transient and asymptomatic hypocalcaemia (serum levels of <2.075 mmol/L) was reported in 49 zoledronic acid and one placebo recipient(s) 9–11 days after the first infusion in HORIZON-PFT [23]. There were three reports of hypocalcaemia in patients receiving zoledronic acid and none in patients receiving placebo in HORIZON-RFT, with the overall low incidence in this study probably because of a vitamin D loading dose administered to the majority of patients [22]. It is recommended that pre-existing hypocalcaemia and disturbances of mineral metabolism be treated prior to initiating zoledronic acid therapy, and calcium and mineral levels in these patients monitored during therapy. Adequate calcium and vitamin D should be taken during zoledronic acid treatment; zoledronic acid is contraindicated in patients with hypocalcaemia [8–10].
Zoledronic acid should not be used [8] or is contraindicated [9] in pregnant women (as reproductive toxicological effects were seen in animals) or in breast-feeding women (as not known if secreted in milk) [8, 9].
4.2 In Japanese Patients
The tolerability profile of zoledronic acid in the ZONE study [21] in Japanese patients with primary osteoporosis was generally similar to that seen in the pivotal studies, HORIZON-PFT and HORIZON- RFT. In ZONE, the overall incidence of AEs at 2 years did not differ significantly between the zoledronic acid and placebo groups (94.6 vs. 92.2%) [21]. However, the incidence of treatment-related AEs was significantly higher in the zoledronic acid group than in the placebo group (59.2 vs. 12%; p < 0.0001), largely because of post-infusion symptoms, of which the most common (incidence >5%) were pyrexia (39.3 vs. 3.3%), arthralgia (16.2 vs. 7.2%), myalgia (10.8 vs. 1.8%), malaise (9.0 vs. 3.0%), headache (7.5 vs. 3.9%) and influenza-like illness (6.9 vs. 0%). Most post-infusion symptoms resolved within 3 days of the infusion. The incidence of serious AEs was 17.4% in the zoledronic acid group and 13.3% in the placebo group, with one serious treatment-related AE reported in each group (pneumonia and atrial fibrillation, respectively). There were no reports of ONJ or atypical femoral fractures in either group and there was no mention of treatment-related acute kidney failure events in the study [21].
4.3 Versus Active Comparators
The tolerability profile of intravenous zoledronic acid was generally similar to that of the oral bisphosphonates alendronic acid [32, 43] and risedronic acid [44], with the exception of a higher incidence of AEs within 3 days of treatment. This is largely because of post-infusion symptoms with zoledronic acid relative to alendronic acid (e.g. myalgia, pyrexia and arthralgia; all p < 0.0001) [43] and risedronic acid (e.g. pyrexia, influenza-like illness and vomiting; all p < 0.05) [44] in bisphosphonate-naïve patients. Post-infusion symptoms were also more frequent with subcutaneous teriparatide plus zoledronic acid and zoledronic acid alone compared with teriparatide alone, resulting in more than twofold higher AE rates within 3 days of the zoledronic acid infusion (68.6, 58.4 and 27.0%, respectively); AE rates after 3 days were 84.7, 87.6 and 84.7% [36]. Compared with subcutaneous denosumab, while the overall incidence of AEs with intravenous zoledronic acid was similar to that with denosumab (62.2% in each group), significantly more patients in the zoledronic acid group than in the denosumab group had musculoskeletal pain (19.7 vs. 13.4%; p < 0.05) [33] and at least twice as many patients in the denosumab as in the zoledronic acid group had AEs potentially related to hypersensitivity (3.8 vs. 1.9%), cardiac disorders (3.4 vs. 1.3%) and eczema (1.6 vs. 0.3%). The incidence of infections was 20.9% in the denosumab group and 16.9% in the zoledronic acid group [33].
5 Dosage and Administration of Zoledronic Acid
In the USA, intravenous zoledronic acid is indicated for the treatment and prevention of postmenopausal osteoporosis and GIO, and as treatment for increasing bone mass in men with osteoporosis [8]. In the EU, zoledronic acid is indicated for the treatment of osteoporosis in men and postmenopausal women at increased risk of fracture (including recent low-trauma hip fracture) and for the treatment of osteoporosis associated with long-term systemic glucocorticoid therapy in men and postmenopausal women at increased risk of fracture [9]. In Japan, zoledronic acid is indicated for the treatment of osteoporosis (as defined by the diagnostic criteria of the Japanese Society for Bone and Mineral Research [52]) [10].
The recommended dosage of zoledronic acid for the treatment of postmenopausal osteoporosis, treatment of osteoporosis in men and the treatment and prevention of GIO in the USA and EU, and for the treatment of osteoporosis in Japan, is a 5 mg infusion administered once yearly, intravenously over ≥15 min [8–10]. In the USA, the recommended dosage for the prevention of osteoporosis in postmenopausal women is a 5 mg infusion administered once every 2 years intravenously over ≥15 min [8]. In the EU, it is recommended that in patients with low-trauma hip fracture, zoledronic acid infusion be given ≥2 weeks after hip fracture repair and a loading dose of oral or intramuscular vitamin D be administered prior to the first infusion [9]. The need for continued therapy should be re-evaluated periodically, and in patients at low fracture risk, treatment discontinuation should be considered after 3–5 years’ [8] or ≥5 years’ [9] therapy. Patients receiving zoledronic acid should also take supplemental calcium if their dietary intake is inadequate; paracetamol taken after a zoledronic acid infusion may reduce the incidence of post-infusion symptoms (Sect. 4) [8, 9]. There are several contraindications to the use of zoledronic acid (see Sect. 4.1).
Local prescribing information should be consulted for further information, including dosage and administration details, contraindications, warnings and precautions.
6 Place of Zoledronic Acid in the Management of Osteoporosis
The aim of osteoporosis therapy is to reduce the risk of fracture and associated morbidity and mortality by prescribing treatment to at-risk patients and ensuring adherence to the treatment plan [7, 53]. Management strategies include nonpharmacological options (e.g. adequate intake of calcium and vitamin D, engaging in regular weight-bearing and muscle-strengthening exercises, implementation of fall-prevention strategies) and pharmacological options (e.g. antiresorptive and anabolic agents), with treatment individualized according to patients’ needs and preferences [3, 4]. While basic bone health using nonpharmacological options is recommended for all individuals, pharmacotherapy is initiated based on a patient’s fracture risk, categorized on the basis of established clinical risk factors such as age, sex, previous fragility fracture and glucocorticoid therapy, with or without assessment of BMD [4, 7, 54, 55]. Although the exact guidance for identifying patients requiring pharmacotherapy varies between international guidelines, in general, treatment is recommended for individuals with a prior fragility fracture, in patients at high fracture risk (as assessed by risk calculators such as FRAX®) [3, 4, 54], and in those with a femoral neck, total hip or lumbar spine T-score of ≤−2.5 [54].
Various therapeutic options are available for the treatment of osteoporosis, with the choice of therapy determined by antifracture efficacy at skeletal sites, adverse events and cost considerations [3]. Bisphosphonates are generally first-choice options for the treatment of osteoporosis [3–7], with zoledronic acid recommended by several guidelines either as a first-line bisphosphonate [3–5] or as an option if other bisphosphonates (often generic alendronic acid because of its low cost) are contraindicated or not tolerated by patients with postmenopausal osteoporosis [3, 4] or GIO [3, 5], or men with osteoporosis [3, 4]. Zoledronic acid is approved in several countries worldwide (including in the USA, EU and Japan) for the treatment of patients with primary or secondary osteoporosis and for the prevention of osteoporosis in patients with low bone mass (indication varies between countries; see Sect. 5).
Zoledronic acid is a highly potent, intravenous aminobisphosphonate, with high binding affinity for mineralized bone and the FPPS active site, which is thought to account for its long half-life in bone (Sect. 2.2) and its long duration of action (Sect. 3), allowing for once-yearly administration (Sect. 5). Annual and intravenous administration of zoledronic acid circumvents some of the issues associated with oral bisphosphonates, such as low bioavailability, complicated and more frequent dosing regimens (daily to monthly) and potential GI irritation and mucosal ulceration [56], which may contribute to poor adherence [56, 57].
In clinical studies of ≤3 years’ duration, intravenous zoledronic acid once yearly improved BMD at several skeletal sites, reduced fracture risk and bone turnover, and/or preserved bone structure and mass in patients with primary or secondary osteoporosis (Sect. 3). During continued therapy in the extensions of one of the pivotal studies (HORIZON-PFT), additional benefits were seen with 6 versus 3 years’ treatment with zoledronic acid, as evidenced by a reduced risk of vertebral fractures and a higher BMD. However, no meaningful differences in BMD and BTM levels were seen in patients receiving treatment for 9 versus 6 years (Sect. 3.1.1), suggesting residual benefits after treatment discontinuation and minimal advantage of treatment beyond 6 years [25], and the potential to discontinue therapy in patients at low fracture risk (Sect. 5). Zoledronic acid administered annually or once in 2 years was also effective in preventing bone loss (as assessed by BMD and BTM levels) in patients with low bone mass (Sect. 3.6). Zoledronic acid was generally well tolerated in these studies, with the most common AEs being mild-to-moderate post-infusion symptoms (Sect. 4), probably because of proinflammatory cytokines released by activated γδ-T cells (Sect. 2.1).
Because of its intravenous route of administration, zoledronic acid is expected to be associated with fewer GI AEs than oral bisphosphonate. However, a recent large, network meta-analysis (n = 44,270) found a higher probability of GI AEs with zoledronic acid than with oral bisphosphonates, largely because of a higher incidence of nausea [58]. Since this analysis was limited by its indirect nature, heterogeneity among the studies and as nausea was only assessed in a limited number of small studies with oral bisphosphonates [58], further direct, head-to-head comparative studies are needed to confirm this observation [58]. In addition, few studies have compared the efficacy of zoledronic acid with that of other osteoporotic agents (Sect. 3), none of which were designed to compare their antifracture efficacy; additional comparative studies assessing this outcome would be helpful.
Adherence to treatment with bisphosphonates is associated with reduced fracture rates in patients with osteoporosis [59] and because of its once-yearly dosing regimen, zoledronic acid has the potential to improve adherence relative to more frequently administered bisphosphonates. However, few real-world studies have assessed adherence to zoledronic acid in patients with osteoporosis. The largest of these studies (n = 1621), based on US Medicare data from 2005 to 2009, found that although adherence to zoledronic acid once yearly was significantly higher than with intravenous ibandronic acid every 3 months (82 vs. approximately 60%; p < 0.0001), approximately 30% of patients receiving zoledronic acid did not receive a second infusion [60]. Older patients (≥85 vs. 65–69 years) and those with no osteoporosis therapy in the preceding year (relative to recent therapy) were more likely to be nonadherent, while patients receiving the first infusion at an internist’s, rheumatologist’s or endocrinologist’s office (relative to the outpatient setting) were more likely to be adherent to zoledronic acid [60]. Additional large studies are needed to assess the impact of the once-yearly dosing regimen on adherence to osteoporosis therapy.
To conclude, zoledronic acid 5 mg once yearly is an effective and generally well tolerated treatment option for patients with osteoporosis, which has the potential to improve adherence in some patients.
Data selection sources:
Relevant medical literature (including published and unpublished data) on zoledronic acid was identified by searching databases including MEDLINE (from 1946), PubMed (from 1946) and EMBASE (from 1996) [searches last updated 4 November 2016], bibliographies from published literature, clinical trial registries/databases and websites. Additional information was also requested from the company developing the drug.
Search terms: Zoledronic acid, Aclasta®, Reclast®, osteoporosis.
Study selection: Studies in patients with primary or secondary osteoporosis or low bone mass who received zoledronic acid. When available, large, well designed, comparative trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
References
International Osteoporosis Foundation. Osteoporosis and musculoskeletal disorders. 2015. https://www.iofbonehealth.org. Accessed 4 Nov 2016.
Chen JS, Sambrook PN. Antiresorptive therapies for osteoporosis: a clinical overview. Nat Rev Endocrinol. 2012;8(2):81–91.
National Osteoporosis Guideline Group. Osteoporosis: clinical guideline for prevention and treatment. 2016. https://www.shef.ac.uk/NOGG/NOGG_Executive_Summary.pdf. Accessed 4 Nov 2016.
Papaioannou A, Morin S, Cheung AM, et al. 2010 Clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ. 2010;182(17):1864–73.
Lekamwasam S, Adachi JD, Agnusdei D, et al. A framework for the development of guidelines for the management of glucocorticoid-induced osteoporosis. Osteoporos Int. 2012;23(9):2257–76.
Suzuki Y, Nawata H, Soen S, et al. Guidelines on the management and treatment of glucocorticoid-induced osteoporosis of the Japanese Society for Bone and Mineral Research: 2014 update. J Bone Miner Metab. 2014;32(4):337–50.
Kanis JA, McCloskey EV, Johansson H, et al. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2013;24(1):23–57.
Novartis Pharmaceuticals Corporation. Reclast® (zoledronic acid): US prescribing information. 2016. https://www.pharma.us.novartis.com. Accessed 4 Nov 2016.
European Medicines Agency. Aclasta (zoledronic acid): summary of product characteristics. 2016. http://www.ema.europa.eu. Accessed 4 Nov 2016.
Asahi Kasei Pharma Corporation. Reclast® (zoledronic acid): Japanese prescribing information. Tokyo: Asahi Kasei Pharma Corporation; 2016.
Deeks ED, Perry CM. Zoledronic acid: a review of its use in the treatment of osteoporosis. Drugs Aging. 2008;25(11):963–86.
Li EC, Davis LE. Zoledronic acid: a new parenteral bisphosphonate. Clin Ther. 2003;25(11):2669–708.
Nancollas GH, Tang R, Phipps RJ, et al. Novel insights into actions of bisphosphonates on bone: differences in interactions with hydroxyapatite. Bone. 2006;38(5):617–27.
Russell RG. Bisphosphonates: from bench to bedside. Ann NY Acad Sci. 2006;1068:367–401.
Coxon FP, Helfrich MH, Van’t Hof R, et al. Protein geranylgeranylation is required for osteoclast formation, function, and survival: inhibition by bisphosphonates and GGTI-298. J Bone Miner Res. 2000;15(8):1467–76.
Dunford JE, Thompson K, Coxon FP, et al. Structure-activity relationships for inhibition of farnesyl diphosphate synthase in vitro and inhibition of bone resorption in vivo by nitrogen-containing bisphosphonates. J Pharmacol Exp Ther. 2001;296(2):235–42.
Rondeau JM, Bitsch F, Bourgier E, et al. Structural basis for the exceptional in vivo efficacy of bisphosphonate drugs. ChemMedChem. 2006;1(2):267–73.
Kunzmann V, Bauer E, Wilhelm M. Gamma/delta T-cell stimulation by pamidronate. N Engl J Med. 1999;340(9):737–8.
Roelofs AJ, Jauhiainen M, Monkkonen H, et al. Peripheral blood monocytes are responsible for γδ T cell activation induced by zoledronic acid through accumulation of IPP/DMAPP. Br J Haematol. 2009;144(2):245–50.
Rossini M, Adami S, Viapiana O, et al. Long-term effects of amino-bisphosphonates on circulating γδ T cells. Calcif Tissue Int. 2012;91(6):395–9.
Nakamura T, Fukunaga M, Nakano T, et al. Efficacy and safety of once-yearly zoledronic acid in Japanese patients with primary osteoporosis: two-year results from a randomized placebo-controlled double-blind study (ZOledroNate treatment in Efficacy to osteoporosis; ZONE study). Osteoporos Int. 2016. doi:10.1007/s00198-016-3736-y.
Lyles KW, Colon-Emeric CS, Magaziner JS, et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007;357(18):1799–809.
Black DM, Delmas PD, Eastell R, et al. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007;356(18):1809–22.
Black DM, Reid IR, Boonen S, et al. The effect of 3 versus 6 years of zoledronic acid treatment of osteoporosis: a randomized extension to the HORIZON-Pivotal Fracture Trial (PFT). J Bone Miner Res. 2012;27(2):243–54.
Black DM, Reid IR, Cauley JA, et al. The effect of 6 versus 9 years of zoledronic acid treatment in osteoporosis: a randomized second extension to the HORIZON-Pivotal Fracture Trial (PFT). J Bone Miner Res. 2015;30(5):934–44.
Eastell R, Black DM, Boonen S, et al. Effect of once-yearly zoledronic acid five milligrams on fracture risk and change in femoral neck bone mineral density. J Clin Endocrinol Metab. 2009;94(9):3215–25.
Jacques RM, Boonen S, Cosman F, et al. Relationship of changes in total hip bone mineral density to vertebral and nonvertebral fracture risk in women with postmenopausal osteoporosis treated with once-yearly zoledronic acid 5 mg: the HORIZON-Pivotal Fracture Trial (PFT). J Bone Miner Res. 2012;27(8):1627–34.
Delmas PD, Munoz F, Black DM, et al. Effects of yearly zoledronic acid 5 mg on bone turnover markers and relation of PINP with fracture reduction in postmenopausal women with osteoporosis. J Bone Miner Res. 2009;24(9):1544–51.
Recker RR, Delmas PD, Halse J, et al. Effects of intravenous zoledronic acid once yearly on bone remodeling and bone structure. J Bone Miner Res. 2008;23(1):6–16.
Sambrook PN, Silverman SL, Cauley JA, et al. Health-related quality of life and treatment of postmenopausal osteoporosis: results from the HORIZON-PFT. Bone. 2011;48(6):1298–304.
Cauley JA, Black D, Boonen S, et al. Once-yearly zoledronic acid and days of disability, bed rest, and back pain: randomized, controlled HORIZON Pivotal Fracture Trial. J Bone Miner Res. 2011;26(5):984–92.
McClung M, Recker R, Miller P, et al. Intravenous zoledronic acid 5 mg in the treatment of postmenopausal women with low bone density previously treated with alendronate. Bone. 2007;41(1):122–8.
Miller PD, Pannacciulli N, Brown JP, et al. Denosumab or zoledronic acid in postmenopausal women with osteoporosis previously treated with oral bisphosphonates. J Clin Endocrinol Metab. 2016;101(8):3163–70.
Hwang JS, Chin LS, Chen JF, et al. The effects of intravenous zoledronic acid in Chinese women with postmenopausal osteoporosis. J Bone Miner Metab. 2011;29(3):328–33.
Bai H, Jing D, Guo A, et al. Randomized controlled trial of zoledronic acid for treatment of osteoporosis in women. J Int Med Res. 2013;41(3):697–704.
Cosman F, Eriksen EF, Recknor C, et al. Effects of intravenous zoledronic acid plus subcutaneous teriparatide [rhPTH(1-34)] in postmenopausal osteoporosis. J Bone Miner Res. 2011;26(3):503–11.
Magaziner JS, Orwig DL, Lyles KW, et al. Subgroup variations in bone mineral density response to zoledronic acid after hip fracture. J Bone Miner Res. 2014;29(12):2545–51.
Boonen S, Orwoll E, Magaziner J, et al. Once-yearly zoledronic acid in older men compared with women with recent hip fracture. J Am Geriatr Soc. 2011;59(11):2084–90.
Eriksen EF, Lyles KW, Colon-Emeric CS, et al. Antifracture efficacy and reduction of mortality in relation to timing of the first dose of zoledronic acid after hip fracture. J Bone Miner Res. 2009;24(7):1308–13.
Adachi JD, Lyles KW, Colon-Emeric CS, et al. Zoledronic acid results in better health-related quality of life following hip fracture: the HORIZON-Recurrent Fracture Trial. Osteoporos Int. 2011;22(9):2539–49.
Orimo H, Hayashi Y, Fukunaga M, et al. Diagnostic criteria for primary osteoporosis: year 2000 revision. J Bone Miner Metab. 2001;19(6):331–7.
Boonen S, Reginster JY, Kaufman JM, et al. Fracture risk and zoledronic acid therapy in men with osteoporosis. N Engl J Med. 2012;367(18):1714–23.
Orwoll ES, Miller PD, Adachi JD, et al. Efficacy and safety of a once-yearly i.v. infusion of zoledronic acid 5 mg versus a once-weekly 70-mg oral alendronate in the treatment of male osteoporosis: a randomized, multicenter, double-blind, active-controlled study. J Bone Miner Res. 2010;25(10):2239–50.
Reid DM, Devogelaer J-P, Saag K, et al. Zoledronic acid and risedronate in the prevention and treatment of glucocorticoid-induced osteoporosis (HORIZON): a multicentre, double-blind, double-dummy, randomised controlled trial. Lancet. 2009;373(9671):1253–63.
Sambrook PN, Roux C, Devogelaer JP, et al. Bisphosphonates and glucocorticoid osteoporosis in men: results of a randomized controlled trial comparing zoledronic acid with risedronate. Bone. 2012;50(1):289–95.
McClung M, Miller P, Recknor C, et al. Zoledronic acid for the prevention of bone loss in postmenopausal women with low bone mass: a randomized controlled trial. Obstet Gynecol. 2009;114(5):999–1007.
Reid IR, Gamble GD, Mesenbrink P, et al. Characterization of and risk factors for the acute-phase response after zoledronic acid. J Clin Endocrinol Metab. 2010;95(9):4380–7.
Wark JD, Bensen W, Recknor C, et al. Treatment with acetaminophen/paracetamol or ibuprofen alleviates post-dose symptoms related to intravenous infusion with zoledronic acid 5 mg. Osteoporos Int. 2012;23(2):503–12.
Boonen S, Sellmeyer DE, Lippuner K, et al. Renal safety of annual zoledronic acid infusions in osteoporotic postmenopausal women. Kidney Int. 2008;74(5):641–8.
US FDA. Update of safety review follow-up to the October 1, 2007 early communication about the ongoing safety review of bisphosphonates. 2008. http://www.fda.gov/drugs/drugsafety. Accessed 4 Nov 2016.
Grbic JT, Black DM, Lyles KW, et al. The incidence of osteonecrosis of the jaw in patients receiving 5 milligrams of zoledronic acid: data from the Health Outcomes and Reduced Incidence with Zoledronic acid Once Yearly clinical trials program. J Am Dent Assoc. 2010;141(11):1365–70.
Soen S, Fukunaga M, Sugimoto T, et al. Diagnostic criteria for primary osteoporosis: year 2012 revision. J Bone Miner Metab. 2013;31(3):247–57.
Kanis JA, McCloskey E, Branco J, et al. Goal-directed treatment of osteoporosis in Europe. Osteoporos Int. 2014;25(11):2533–43.
Cosman F, de Beur SJ, LeBoff MS, et al. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25(10):2359–81.
National Institute of Health and Care Excellence. Osteoporosis: assessing the risk of fragility fracture. 2012. https://www.nice.org.uk/guidance/cg146. Accessed 4 Nov 2016.
Grey A, Reid IR. Differences between the bisphosphonates for the prevention and treatment of osteoporosis. Ther Clin Risk Manag. 2006;2(1):77–86.
Rampakakis E, Sampalis JS. What can be done to maximize adherence of bisphosphonates in patients with osteoporosis? Int J Clin Rheumtol. 2012;7(4):361–4.
Tadrous M, Wong L, Mamdani MM, et al. Comparative gastrointestinal safety of bisphosphonates in primary osteoporosis: a network meta-analysis. Osteoporos Int. 2014;25(4):1225–35.
Siris ES, Harris ST, Rosen CJ, et al. Adherence to bisphosphonate therapy and fracture rates in osteoporotic women: relationship to vertebral and nonvertebral fractures from 2 US claims databases. Mayo Clin Proc. 2006;81(8):1013–22.
Curtis JR, Yun H, Matthews R, et al. Adherence with intravenous zoledronate and intravenous ibandronate in the United States Medicare population. Arthritis Care Res (Hoboken). 2012;64(7):1054–60.
Center for Drug Evaluation and Research. Reclast (zoledronic acid): Medical review(s) (Pt 2). 2006. http://www.accessdata.fda.gov. Accessed 4 Nov 2016.
Acknowledgements
During the peer review process, the manufacturer of zoledronic acid (Reclast®, Aclasta®) was also offered an opportunity to review this article. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Conflict of interest
Sohita Dhillon is a salaried employee of Adis/Springer, is responsible for the article content and declares no relevant conflicts of interest.
Additional information
The manuscript was reviewed by: J. Iwamoto, Institute for Integrated Sports Medicine, Keio University School of Medicine, Tokyo, Japan; H. Kaji, Department of Physiology and Regenerative Medicine, Kinki University Faculty of Medicine, Osaka, Japan; J. M. Kaufman, Department of Internal Medicine, Ghent University, Ghent, Belgium; I. Reid, Faculty of Medical and Health Sciences, The University of Auckland, Auckland, New Zealand; J. Takada, Department of Orthopedic Surgery, Sapporo Medical University, Sapporo, Japan.
Rights and permissions
About this article
Cite this article
Dhillon, S. Zoledronic Acid (Reclast®, Aclasta®): A Review in Osteoporosis. Drugs 76, 1683–1697 (2016). https://doi.org/10.1007/s40265-016-0662-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-016-0662-4