Abstract
Severe Cushing’s syndrome presents an acute emergency and is defined by massively elevated random serum cortisol [more than 36 μg/dL (1000 nmol/L)] at any time or a 24-h urinary free cortisol more than fourfold the upper limit of normal and/or severe hypokalaemia (<3.0 mmol/L), along with the recent onset of one or more of the following: sepsis, opportunistic infection, intractable hypokalaemia, uncontrolled hypertension, heart failure, gastrointestinal haemorrhage, glucocorticoid-induced acute psychosis, progressive debilitating myopathy, thromboembolism or uncontrolled hyperglycaemia and ketocacidosis. Treatment focuses on the management of the severe metabolic disturbances followed by rapid resolution of the hypercortisolaemia, and subsequent confirmation of the cause. Emergency lowering of the elevated serum cortisol is most rapidly achieved with oral metyrapone and/or ketoconazole; if parenteral therapy is required then intravenous etomidate is rapidly effective in almost all cases, but all measures require careful supervision. The optimal order and combination of drugs to treat severe hypercortisolaemia—mostly in the context of ectopic ACTH-secreting syndrome, adrenocortical carcinoma or an ACTH-secreting pituitary adenoma (mainly macroadenomas)—is not yet established. Combination therapy may be useful not only to rapidly control cortisol excess but also to lower individual drug dosages and consequently the possibility of adverse effects. If medical treatments fail, bilateral adrenalectomy should be performed in the shortest possible time span to prevent the debilitating complications of uncontrolled hypercortisolaemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Cushing’s syndrome (CS) is defined by long-standing exposure to supraphysiological concentrations of circulating glucocorticoids [1]. Severe CS (SCS) is defined by massively elevated random serum cortisol [more than 41 μg/dL (1100 nmol/L)] at any time or a 24-h urinary free cortisol (UFC) more than fourfold the upper limit of normal (ULN) and/or severe hypokalaemia (<3.0 mmol/L), along with the recent onset of one or more of the following: sepsis, opportunistic infection, intractable hypokalaemia, uncontrolled hypertension, oedema, heart failure, gastrointestinal haemorrhage, glucocorticoid-induced acute psychosis, progressive debilitating myopathy, thromboembolism or uncontrolled hyperglycaemia and ketocacidosis. The patients will generally show clear clinical features of CS with the exception of CS as a paraneoplastic syndrome accompanying a neuroendocrine neoplasm (NEN) such as small cell lung carcinoma (SCLC) [2–4].
This definition of SCS clearly emphasises the importance of immediate intervention since CS per se carries increased mortality and morbidity rates [5] with an increased rate of health impairment even after cure [6]. Indeed, uncontrolled CS results in very high morbidity and mortality, mainly because of its cardio-metabolic abnormalities and the risk of overwhelming infection [5]. Overall, SCS can be accompanied by acute cardiovascular, metabolic and infectious complications, and is considered an emergency situation dictating immediate diagnosis together with supportive and hypocortisolaemic therapy [1, 2, 7, 8]; this treatment has to take precedence over investigations into the cause and localisation [9, 10]. The need for urgent treatment (within 24–72 h) of hypercortisolism to prevent life-threatening complications of CS has been also recently acknowledged in the Endocrine Society Clinical Practice Guideline for the Treatment of Cushing’s Syndrome [7].
2 Diagnosis
The first step in the diagnosis of CS is clinical suspicion followed by a detailed medical and drug history, whenever possible. The diagnosis is usually straightforward when CS is florid, with the exception of the paraneoplastic-wasting syndrome due to an ectopic adrenocorticotropic hormone (ACTH) syndrome (EAS) which may have a rapid onset with severe features masking the hypercortisolism; systemic features of CS may be minimal, but in this scenario the lung lesion should be obvious [11].
Signs that can be seen in CS include central obesity, buffalo hump, purplish skin striae or skin pigmentation, limb wasting and muscle weakness, a plethoric red face with hirsutism and frontal balding, and spontaneous bruising [11]. Co-morbidities in CS include carbohydrate metabolism abnormalities (prediabetes or diabetes), cardiovascular abnormalities [hypertension, cardiovascular failure, venous thromboembolism, prolonged QTc dispersion on the electrocardiogram (ECG), left ventricular hypertrophy and hyperhomocysteinaemia], hepatic steatosis, calcium metabolism abnormalities (osteoporotic fractures, renal stones), reproductive abnormalities (hypogonadotrophic hypogonadism and polycystic ovaries), cognitive and memory impairment, recurrent infections and growth retardation in children [11]. Oedema, hypertension and hypokalemia are due to a functional mineralocorticoid excess state when severe hypercortisolaemia overwhelms the 11β-HSD2 enzyme because of substrate saturation leading to spillover of cortisol to the mineralocorticoid receptor [12]. Psychiatric features, such as severe psychosis, may be the presenting features with the need for acute intervention or an increased suicidal risk [7]. In severe hypercortisolaemia, all cardio-metabolic and catabolic consequences as well as susceptibility to infection are exacerbated [3, 7, 13].
If we consider severely ill patients as the ones admitted to an intensive care unit (ICU), such patients display increased cortisol levels along with the ACTH-cortisol dissociation usually seen immediately after the very acute phase of a critical illness; this relative hypercortisolaemia seems not to be driven by ACTH but by alternative mechanisms (such as immunological/inflammatory stimulators) and suppressed cortisol clearance [14, 15]. It is difficult to define cutoff values to differentiate increased baseline cortisol levels due to a critical illness as opposed to true CS, since few studies have been performed and no thresholds have been properly validated. In this situation, a clinical suspicion of CS is critically important [16].
When CS is suspected, usually a step-by-step work-up has to be followed for investigation of the aetiology and source of hypercortisolaemia; however, when hypercortisolaemia is severe, this systematic process can be postponed until after the patient is stabilised [7].
Severe CS has been mostly seen in the context of EAS, adrenocortical carcinoma (ACC) or occasionally with ACTH-secreting pituitary adenomas (mainly macroadenomas), i.e. Cushing’ disease (CD). However, it has recently been suggested that mutations of the armadillo repeat-containing-5 (ARMC5) gene, a probable tumour suppressor gene, may be implicated in clinically SCS associated with macronodular adrenal hyperplasia (MAH), and SCS may be seen in MAH where exogenous agents may precipitate cortisol excess (Table 1) [3, 4, 9, 17, 18].
3 Management of Severe Cushing’s Syndrome
Having established the diagnosis of SCS, establishing the cause is less important than treatment of the acute problems. Medical therapy targets the patient’s condition to correct the metabolic derangements urgently, and then measures are taken to lower the cortisol levels. If medical therapy fails to reverse the clinical emergency as well as to reduce hypercortisolaemia, bilateral adrenalectomy (BA) provides immediate control of the hypercortisolism and can be lifesaving, but the risk of surgery must be balanced against the likelihood of medical control failure.
3.1 Αcute Intervention of Severe Cushing’s Syndrome (SCS) Targeting Patient Haemodynamic Stabilisation
Different systems can be affected during an episode of SCS, but all of them have to be well controlled to avoid further complications.
Diabetes needs to be controlled, often requiring insulin administration even in patients on no previous anti-diabetic therapy.
Hypertension will require urgent control but no specific agents are recommended. The combination of fluid retention and hypertension may be associated with cardiac failure, especially in the older patient. Hypokalaemia is present in almost all patients with EAS and around 10 % of patients with other aetiologies; spironolactone 50 or 100 mg/day should be started, with triamterene or amiloride as alternatives.
A significant pro-thrombotic tendency is present in CS, dictating the use of anticoagulant treatment. We therefore recommend that subcutaneous heparin at prophylactic doses (low-molecular-weight heparins) should be considered in all hospitalised patients admitted with SCS; when pulmonary embolism and/or deep vein thrombosis has been confirmed, heparin should be used at therapeutic doses [19], in particular when patients are bedridden or have low mobility [7].
Mental changes may be severe, such as untreatable psychosis, causing problems in management; haloperidol may be necessary to calm the patient, although there is also some experience with olanzapine.
When osteoporotic fractures have been confirmed, then adequate pain relief is necessary.
However, sepsis is the most feared complication of SCS since this may be life-threatening and lack some of the usual indicators and signs. In patients with severe infection, the serum cortisol should be lowered to a level compatible with that seen in other patients with a similar infection, which we consider to be 22–36 μg/dL (600–1000 nmol/L) [7, 10]. Hence, any bacterial, fungal or viral infection must be vigorously treated as soon as possible when recognised, as seen in other immune-suppressed patients. Prophylaxis with trimethoprim-sulfamethoxazole (or dapsone in allergic patients) is highly effective for pneumocystis pneumonia (PCP) in patients receiving a glucocorticoid dose equivalent to ≥20 mg of prednisone daily for 1 month or longer, especially if they have an additional cause for immunocompromise, such as chemotherapy in a patient with NEN-associated EAS [7, 10]. However, PCP has been described in a hypercortisolaemic patient who developed PCP despite the administration of prophylactic treatment, implying the necessity of curative doses of trimethoprim-sulfamethoxazole [20]. The immune reconstitution inflammatory syndrome characterised by an altered function of the immune system immediately after hypercortisolaemia control may play a role [20].
Peritonitis may be present with minimal evidence when caused by perforation of a viscus in a patient with SCS, especially in the elderly with underlying diverticular disease; vigorous resuscitation should be undertaken with broad-spectrum antibiotics, and surgery deferred (if possible) until control of the hypercortisolaemia. Typical signs of bowel perforation, such as rebound, guarding, loss of bowel sounds, fever and elevated white blood cell count may be lacking due to hypercortisolism [7, 21]. Some patients need ICU management with a multidisciplinary approach that includes experienced endocrinologists [7].
In conclusion, it is very important to note that many of these aberrations are acute effects of the hypercortisolaemic state; hypercortisolaemia control may rapidly reverse these complications, so constant careful monitoring is mandatory to avoid further complications such as hypoglycaemia due to insulin therapy [10].
3.2 Αcute Intervention of SCS Targeting Hypercortisolaemia Control
In a large retrospective cohort study compared to treatment-naïve patients, patients who were treated with cortisol-lowering therapy before surgery had a reduced risk for developing venous thromboembolism postoperatively, although this difference was not statistically significant [22, 23]. There is therefore some evidence regarding the importance of an acute effort to lower serum cortisol levels as soon as the urgent measures for patient stabilisation have been initiated.
3.2.1 Management of Drug Interactions
When drug interactions are involved in the aetiology of CS, it is worth considering alternative therapeutic options that are not interacting with cortisol metabolism. This type of SCS has been described recently as a severe form of iatrogenic CS concerning the drug interaction of antiretroviral drugs (ritonavir-containing antiretroviral therapy) given for human immunodeficiency virus (HIV) together with the local administration of steroids [10, 18, 24]. Changing ritonavir-containing antiretroviral therapy to a non-interacting compound, such as an integrase inhibitor, may be considered [7, 10, 18, 24]. Moreover, one might substitute the corticosteroid used, such as switching to beclomethasone as an inhaled glucocorticoid since it is not metabolised by CYP3A4.
3.2.2 Medical Therapy of Hypercortisolaemia
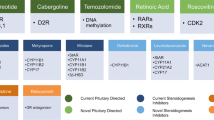
Regarding endogenous CS, hypercortisolaemia control demands adrenal-specific therapy with the use of drugs that are predominantly directed at controlling adrenal secretion. We will first describe the established therapeutic approaches of SCS, and later other therapies which have been tried or that may eventually be useful.
These compounds decrease cortisol levels by direct inhibition of steroidogenesis at one or more enzymatic steps, being highly effective in treating hypercortisolism, although they do not restore normal hypothalamo-pituitary-adrenal (HPA) secretory dynamics. All these drugs require escalation after an initial low dose to minimise their adverse effects (AEs); frequent monitoring is required to achieve an acceptable clinical and biochemical profile. The inhibition can be partial or complete; a ‘block-and-replace’ scheme is an option, particularly in SCS [25]. Even in this case it is important to undertake careful monitoring to avoid hypocortisolaemia since hypoadrenalism can often be mistaken as gastrointestinal side effects of the agents used to control SCS [10].
Metyrapone blocks 11β-hydroxylase (CYP11B1), and represents an optimal initial choice as it is rapid in onset and highly effective. Additionally, it inhibits 17α-(CYP17A1), 18- (CYP11B2) and 19-hydroxylase [25, 26] with good control of cortisol levels frequently obtained in both short- and long-term studies [27–30]. Biochemical control was achieved in 83 % of patients with monotherapy and 76 % of those with combination treatment in the largest and recent series of 195 patients with CS [29]. In this latter retrospective multicentre study, 84 % of patients received metyrapone monotherapy with a duration of therapy of 8 months (range 3 days to 11.6 years). From the first evaluation to the last review, statistically significant improvements were reported in: the cortisol day curve (CDC) [from 722.9 nmol/L (26.2 μg/dL) to 348.6 nmol/L (12.6 μg/dL)], UFC [from 1483 nmol/24 h (537 μg/24 h) to 452.6 nmol/24 h (164 μg/24 h)] [29]. The effect is usually seen within hours, and we would generally start with an initial daily dose of 0.5–1 g, in 3–4 divided doses daily, and this may be increased every few days to a maximal daily dose of 6 g daily [25, 26]. The median final dose as described in the most recent study of metyrapone was 1375 mg for CD, 1500 mg for EAS, 750 mg for benign adrenal disease and 1250 mg for ACC [29]. The strong cortisol-lowering effect of metyrapone results in a loss of its negative feedback on ACTH levels and consequently in a rise of ACTH, but this is not relevant in an emergency situation; however, acne and hirsutism driven by a rise of androgenic precursors are a longer-term problem [28, 30]. Adverse effects include hypertension, hypokalaemia and oedema due to an increase in mineralocorticoid precursors (although this is rarely problematic) [30], or dizziness and gastrointestinal upset (minimised when metyrapone is taken with food or milk) [7, 26]. It is important to note that 11-deoxycortisol may cross-react with many cortisol assays, other than those employing gas chromatography-mass spectrometry (GC-MS), and blood levels of apparent ‘cortisol’ may over-read by around 25 % or more [31].
Ketoconazole, an imidazole blocking cytochrome P450 enzymes, acts at a number of sites, the strongest effect being on 17,20-lyase, and side-chain cleavage complex (P450scc, CYP11A1, 20,22 desmolase), 11β-hydroxylase and 17α-hydroxylase [25, 26, 32]. It is probably slower in onset than metyrapone, occurring over several days or possibly weeks. Treatment with ketoconazole is usually started at 400 mg/day (divided in two doses) and increased every 3 or more days to a maximum of 1.2–1.6 g/day in 3–4 divided doses. Gastric acidity is necessary to metabolise ketoconazole into the active compound, rendering this drug not an option in achlorhydric patients or those treated with proton pump antagonists, unless it is formulated locally in an acidic vehicle [25, 26]. Its multitarget inhibition results in a drop of androgen synthesis with favourable effects on hirsutism. Extra-adrenal actions have been reported since an acute in vitro decrease in basal and corticotropin-releasing hormone (CRH)-stimulated ACTH secretion by corticotroph tumour cells obtained from two patients with Nelson’s syndrome (NS) was reported [33]. The fact that ACTH concentrations increase during long-term treatment with ketoconazole suggests that its major effect is on the adrenal cortex rather than the corticotroph cells. Interestingly, at high concentrations, it has been shown in vitro to be an antagonist of the glucocorticoid receptor (GR) [34]. Ketoconazole has a relatively benign spectrum of AEs, including gastrointestinal symptoms, gynaecomastia (affecting male patients), irregular menses (affecting female patients), decreased libido and impotence (cause of treatment discontinuation in men), teratogenicity (contraindicated in pregnancy) and its interactions with other medications because of the potent inhibitory effects on cytochrome P450 enzymes (CYP3A4, CYP2C9, CYP1A2) [7, 25, 26, 35]. An idiosyncratic hepatic dyscrasia occurs in about 1 in 15,000 cases, and this may very rarely be fatal [7, 25, 35, 36]. Mild asymptomatic elevation in serum transaminases occurs in approximately 10 –15 % of cases, usually when therapy starts or when doses increase; values generally return to normal within 2–4 weeks after stopping therapy or reducing doses [7, 37]. Monitoring liver enzyme elevation is advised when remaining less than threefold the ULN, and most clinicians continue therapy, while when this is higher, discontinuation or dose reduction is advised [7]. Recently, its efficacy and safety profile have been confirmed in a French retrospective multicentre study reviewing data from 200 patients treated with ketoconazole monotherapy for CD [37]. In this French retrospective multicentre study of patients with CD, 49 % had UFC normalisation, and 26 % a 50 % decrease of UFC levels; 21 % stopped the treatment due to poor tolerance. Mild (less than fivefold the ULN) and major (more than fivefold the ULN) increases in liver enzymes were observed in 13.5 and 2.5 % of patients, respectively, but no fatal hepatitis was observed [36]. The US Food and Drug Administration (FDA) issued a ‘Black Box’ warning in 2013, and the European Medicines Agency has restricted access to the agent to physicians specialised in treating CS [7]. Levo-ketoconazole is the single 2S,4R enantiomer of ketoconazole, purified from racemic ketoconazole, an investigational new drug for the treatment of CS hypothesised to provide better safety and efficacy than the currently used racemic ketoconazole. A single-arm, open-label, dose titration study is currently assessing its efficacy, safety, tolerability and pharmacokinetics, identifying the minimally effective and maximally tolerated doses of levo-ketoconazole in patients with CS [38].
A combination of these two a drugs is another option for SCS. In 14 patients with EAS and 8 with ACC with SCS, combination therapy with metyrapone and ketoconazole was well tolerated and provided rapid control of life-threatening hypercortisolism [3]. The starting dosages were variable (median: metyrapone 2125 mg/day and ketoconazole 900 mg/day) and were subsequently adjusted. After 1 week of treatment, the median UFC fell from 40.0 to 3.2 ULN and from 16.0 to 1.0 ULN in patients with EAS and ACC respectively. After 1 month UFC was 0.5 and 1.0 ULN in patients with EAS and ACC, respectively, and UFC values were normal in 73 and 86 % of patients, respectively. One confounding factor for the analysis of the results was the introduction of mitotane simultaneously or later in 6/14 patients with EAS and 6/8 patients with ACC [3].
If all the above measures fail, the intravenous imidazole derivative etomidate can be extremely useful; compared to ketoconazole, it inhibits 11β-hydroxylase more potently, showing a similar inhibition of 17α-hydroxylase but a lesser effect on 17,20 lyase; at higher concentrations it has an effect on the cholesterol side-chain cleavage complex but also aldosterone synthase (CYP11B2) [25, 39]. It may be life-saving since it acts within hours and is almost always highly effective. Blunting of the cortisol response to ACTH has been reported in vivo [40], confirming a direct effect on the adrenal cortex. This drug may be used as first-line treatment in severely ill patients, or in cases in which oral medications are ineffective or oral therapy is impossible, such as in cases of glucocorticoid-induced psychosis or respiratory failure [7, 41–43]. Recent guidelines suggest a loading dose of 3–5 mg is followed by a continuous infusion of 0.03–0.10 mg/kg/h (2.5–3.0 mg/h), effectively reducing serum cortisol within 12 h [7], with dose titration according to serum cortisol if cortisol levels are not falling within 12–24 h and a maximum dose of up to 5 mg/h in selected cases [4, 44]. Studies have not reported sedation at these doses. Monitoring of serum cortisol levels (every 4–6 h) is necessary to achieve the desired blockade and to prevent hypoadrenalism. If complete rather than partial blockade is desired, a hydrocortisone infusion may be added to prevent hypoadrenalism after 24 h of etomidate infusion. It is recommended that the infusion rate is titrated to achieve a stable serum cortisol level in the range 150–300 nmol/L in an unstressed patient, or a block-and-replace strategy can be used [7, 44]. In the ICU, dosages of 0.1–0.3 mg/kg/h can be used to rapidly suppress cortisol production in complicated EAS [45]. The recent guidelines recommend that management takes place in an ICU setting in units not thoroughly experienced since the drug needs to be very carefully monitored [7]. Care should be taken to prevent possible sedation, and adjustments should be made with regard to renal failure and stressed situations such as sepsis [44]. It may be prudent to administer etomidate preparations containing propylene glycol (which may cause thrombophlebitis and pain on injection) through a central venous line considering the increased thrombotic risk of such patients [7].
3.2.3 Urgent Surgical Treatment: Bilateral Adrenalectomy
Bilateral adrenalectomy induces rapid resolution of uncontrolled hypercortisolaemia in an emergency department when all else fails, and the clinical situation of the patient is deteriorating. Nevertheless, even with a good laparoscopic technique, surgery in the presence of SCS is far from ideal; every attempt should be made to lower the cortisol levels preoperatively with medical therapy. However, as the recent guidelines underline, if aggressive medical management does not control hypercortisolism, clinicians should consider BA even in high-surgical-risk patients [7]. In a recently published review along with a case series presentation of 58 patients [4], BA was a highly effective treatment providing adequate control of long-term co-morbidities associated with hypercortisolism, while in EAS it was mostly performed as an emergency procedure because of life-threatening complications caused by SCS. However, BA was also a relatively safe treatment (median surgical morbidity 15 %, median surgical mortality 3 %), providing excellent control of hypercortisolism with Cushing-associated features rapidly corrected, and co-morbidities stabilised. In CD, the quality of life (QOL) following BA rapidly improved and long-term mortality was low, while specific long-term complications included hypoadrenalism and NS. On the other hand, in EAS, long-term mortality is high but mostly dependent on the prognosis of the underlying malignant NEN. Malignant or catastrophic CS characterises the emergency scenario where BA had to be performed in the shortest possible time span in the context of SCS as confirmed by massive ACTH and cortisol excess, mostly patients with EAS, who present life-threatening complications [2, 46, 47]. The timing of BA is important since the outcome is generally fatal if hypercortisolism cannot be controlled, and if BA is delayed or postponed [7, 47]. However, a medical approach is always needed for the patient with catastrophic CS scheduled for BA in a pre-surgical phase aiming at stabilising the patient with parenteral adrenostatic treatment [4, 9]. There are also challenging cases where SCS is instituted after a long natural history of CS, and BA seems the only means for controlling co-morbidities due to SCS such as severe hypertension, hypokalaemia and hyperglycaemia, along with bilateral pneumonia complicated by sepsis [48].
Interestingly, the combination of mitotane, metyrapone and ketoconazole introduced concomitantly (metyrapone: 2.25 g/24 h, ketoconazole: 800 mg/24 h, mitotane: 3.0 g/24 h, dosages adjusted to clinical severity, UFC excretion, tolerance) was proven to be an effective alternative to BA in 11 patients with severe ACTH-dependent CS (four pituitary microadenomas, two occult possibly EAS, one occult EAS and four metastatic EAS). Median UFC excretion dropped sharply, from 2737 μg/24 h (range 853–22,605) at baseline to 50 μg/24 h (range 18–298) after 24–48 h of combination treatment [9].
Mitotane (O,p′DDD: 1-(o-chlorophenyl)-1-(p-chlorophenyl)-2,2-dichloroethane), an insecticide analogue of dichlorodiphenyltrichloroethane, inhibits steroidogenesis in the steps of the cytochrome P450 enzymes CYP11A1, 11β-hydroxylase and 18-hydroxylase, and non-P450 enzymes (3β-hydroxysteroid dehydrogenase) [25, 26]. It has a specific adrenolytic action and for this reason is considered to be an effective alternative to BA in severe ACTH-dependent CS [7]; this action was initially described in animal studies as lipid accumulation and atrophy of the zona fasciculata and reticularis regions of the adrenal cortex with effects on the zona glomerulosa only after prolonged therapy [49], displaying a slow onset of action (weeks or months) [25, 26]. Hence, as in BA, patients treated with mitotane long term generally receive replacement doses of hydrocortisone (generally higher than usual) because of the typical suppressive and adrenolytic effects of long-term mitotane therapy. Other disadvantages of its use include a long half-life, significant gastrointestinal and neurological adverse effects, hypercholesterolaemia, and less common problems such as gynaecomastia [25]. Numerous drug interactions have been described [7, 50]. Μitotane induces a large rise in corticosteroid binding globulin (CBG) such that measurement of total cortisol is unreliable, and it is necessary to rely on plasma ACTH measurement, and urinary, serum or salivary free cortisol to avoid an adrenocortical crisis [51].
3.2.4 Other Drugs That Have Been Used or That Could Eventually be Useful to Control Adrenal Secretion in Cases of Severe Hypercortisolaemia
3.2.4.1 Glucocorticoid Receptor Antagonists
The first potent glucocorticoid antagonist available for clinical use is mifepristone, 11β-[p-(dimethylamino)phenyl]-17β-hydroxy-17-(1-propynyl)estra-4,9-dien-3-one, a competitive antagonist of androgen, progesterone and GRs, displaying very little agonist effect on GR [26, 52]. Mifepristone binds to GR with an 18-fold higher affinity than cortisol [53], resulting in a loss of negative feedback effects at the HPA by cortisol, leading to an increase in ACTH secretion in CD with a concomitantly increased cortisol production [23]. Mifepristone should be started at 300 mg/day, and be titrated slowly, since 400–800 mg/day may rapidly reduce the symptoms and signs of CS; dose adjustment must be based on clinical parameters, primarily glucose, and weight reduction, since cortisol levels cannot be used as a marker of efficacy and the patient can become Addisonian unless care is taken [7]. Following mifepristone treatment, two patients with EAS caused by bronchial NEN converted the negative octreotide scintiscan to positive, allowing the identification and consequently the resection of the tumour [54]. Mifepristone showed improvement of clinical signs in 15/20 patients with CS of different aetiologies [55], while in a recent study improved hypertension and/or diabetes in 40 and 60 %, respectively, was seen as an improvement of 87 % in other features of CS (weight, depression, cognition, clinical appearance or QOL), gaining approval for the control of carbohydrate metabolism abnormalities secondary to hypercortisolism in patients who failed surgery or were not surgical candidates [53]. In this latter 24-week multicentre open-label trial, 50 adults with endogenous CS associated with carbohydrate metabolism abnormalities (type 2 diabetes or impaired glucose tolerance), or a diagnosis of hypertension after failed multimodality therapy, received mifepristone at 300–1200 mg/day: 60 % improved their carbohydrate metabolism with glycated haemoglobin (HbA1c) decreasing from 7.43 ± 1.52 to 6.29 ± 0.99 % and a diastolic blood pressure (BP) response in 38 % of patients, along with loss of weight of −5.7 ± 7.4 % and drop in waist circumference −6.78 ± 5.8 cm in women and −8.44 ± 5.9 cm in men [53]. One patient with an ACTH-secreting pituitary macroadenoma responded extremely well to high doses (up to 25 mg/kg/day) after radiotherapy with remission of life-threatening clinical symptomatology [56].
An advantage of mifepristone is its rapid onset of action that makes it a good candidate for emergency treatment such that psychiatric symptoms were improved within 1 week in 4/5 patients, while revision of earlier published case reports revealed clinical improvement in 9/9 patients with EAS after mifepristone treatment [57]. As opposed to its rapid onset and its use as emergency treatment in some described cases of patients with CS [20, 57], high doses of mifepristone expose patients to frequent and/or severe AEs, with hypokalaemia and adrenal insufficiency making this choice not safe in critically ill patients since it is not possible to readily monitor clinical signs. Dosages more than 1000 mg/day and for long periods seem to be associated with more AEs, in particular increased mineralocorticoid action (hypertension, hypokalaemia and oedema) which needed treatment with spironolactone [56], hypoadrenalism (fatigue, nausea, vomiting, arthralgias and headache) with difficulty in biochemical confirmation [26, 52, 57], and endometrial thickening [7]. Mifepristone should not be administered with drugs that are metabolised by CYP3A or CYP2C because of an increased toxicity risk [26]. Further evaluation of its safety and of follow-up methodology might render this agent a more attractive option for acute short-term use. Moreover, at present, it is also extremely expensive in most regions.
3.2.4.2 Adrenal-Specific Therapy
Osilodrostat (LCI699) is an investigational oral agent which is a potent inhibitor of human 11β-hydroxylase and aldosterone synthase, enzymes which are responsible for catalysing the final steps of cortisol and aldosterone biosynthesis, respectively, in the adrenal cortex [58]. It may be considered to be broadly similar to metyrapone and it has shown encouraging efficacy and safety in one proof-of-concept study of 12 patients with moderate-to-severe CD [59]. In this proof-of-concept study, it was initiated at 4 mg/day in two equal doses; the dose was escalated every 14 days to 10, 20, 40 and 100 mg/day until UFC normalised, whereupon the dose was maintained until treatment ended (10 weeks). All 12 patients achieved UFC within the ULN or a ≥50 % decrease from baseline while 92 % normalised UFC. Mean 11-deoxycortisol, 11-deoxycorticosterone and ACTH levels increased during treatment and declined after discontinuation. Mean systolic and diastolic BP decreased from baseline by 10.0 and 6.0 mmHg, respectively. Osilodrostat was generally well tolerated; most AEs were mild or moderate (fatigue: 7/12; nausea: 5/12; headache: 3/12) [59]. Other AEs reported were hypernatraemia, gastrointestinal effects (nausea and diarrhoea), headache, oedema and hypokalaemia (the latter as for metyrapone caused by mineralocorticoid precursor accumulation) [60]. In due course it will be interesting to compare its efficacy, ease of use and AE profile with metyrapone. It is also of interest to investigate whether osilodrostat therapy in CD is characterised by an escape phenomenon caused by up-regulation of ACTH secretion as seen with other steroidogenesis inhibitors that are not adrenolytic, although experience with metyrapone suggests that this is unlikely to be a major problem.
Fluconazole, an antifungal agent, a triazole, inhibits 11β-hydroxylase and 17-hydroxylase, and is less toxic than ketoconazole, and it can be administered in either intravenous or oral forms. Fluconazole at a dose of 100 mg twice daily successfully controlled UFC levels in two patients [61]. Its efficacy in SCS has not been tried, but in a case report in an elderly female patient with EAS the dose was started at 200 mg daily, after 2 days increased to 400 mg, then gradually increased up to 1200 mg, and 1 week later doses were tapered again to 400 mg [62] (Table 2).
3.2.4.3 Medical Therapy Targeting ACTH-Secreting Tissues
Somatostatin (SST) analogue (SA) use is based on inhibition of the somatostatin receptor(s) (sstr) [63]. In the central nervous system, SST plays a key inhibitory role in the secretion of growth hormone, prolactin, thyrotrophin and ACTH from the anterior pituitary gland [26]. The majority of corticotroph adenomas (>85 %) express sstr5 mRNA, and to a lesser extent sstr1 and sstr2 (63 %) [64]. The membrane density of sstr, particularly sstr2, is affected by hypercortisolism [65, 66]. In contrast, sstr5 expression appears to be relatively unaffected by high cortisol levels. Therefore, in patients with active CD, sstr5 is predominantly expressed compared with sstr2. Ιt is predicted that after restoration of eucortisolaemia, sstr2 expression recovers, becoming as abundant as sstr5, improving treatment responsiveness by agents targeting this receptor as well [66–68].
Indeed, pasireotide, a newer multi-ligand SA, which has high binding affinity to sstr5 and 1, 2 and 3 subtypes [69], was recently approved (in the USA and Europe) for the treatment of patients with CD for whom surgery has failed or is not possible. In the first published phase II, open-label, single-arm, multicentre pilot study of pasireotide in 29 patients with CD, normalisation of UFC was demonstrated in 17.2 % along with a reduction in serum cortisol and plasma ACTH levels, implying that pasireotide may have dual anti-secretory and anti-proliferative properties [70]. A subsequent double-blind, randomised, multicentre phase III trial with pasireotide 600–900 µg twice daily revealed UFC reduction in most of 162 patients with CD and normalisation in approximately 25 % of them [71]. In eight patients with CD taking pasireotide 600–1200 µg twice daily for at least 6 months (up to 24 months), marked tumour shrinkage was observed after 12 months of treatment, while in one patient disappearance of the tumour was also documented [72]. The absence of expression of sstr5 mRNA in 40 % of ACTH-secreting pituitary adenomas might explain the different responses to pasireotide [73]. A higher degree and frequency of hyperglycaemia was documented in 73 % of patients and 6 % of patients discontinued the study, while the other AEs were similar to those of other SSTs (gastrointestinal, including biliary sludge and gallstones) [7, 72, 73]. Clinicians should correct hypokalaemia and hypomagnesaemia before initiating pasireotide and test for baseline liver function tests, thyroid function (including free thyroid hormone), IGF-1, fasting glucose/HbA1c, as well as gallbladder ultrasounds and ECGs for corrected QT interval prolongation or bradycardia; the drug is better taken after meals [7]. It is of interest that pasireotide was shown to have some role in SCS (four- to sixfold the ULN) in CD since the UFC level decreased by 25–50 % from baseline in 4/5 patients with severe hypercortisolism in the first 4 weeks of monotherapy with pasireotide [74]. However, available data come mostly from retrospective case series or clinical trials using just two doses of the drug, while clinical trials with active comparator agents are lacking. At present, it is not a drug to be recommended early in the treatment of SCS.
Use of dopamine agonists (DAs) is based on the presence of dopamine receptor-2 (D2R) in the anterior and intermediate lobe of the pituitary gland [25, 75] showing variable and heterogeneous expression in 89 % of all types of pituitary tumours [76]. D2R has also been detected in 69 % of silent or functioning ACTH-secreting pituitary tumours in one study, or in more than 75 % of such tumours in another [76, 77]. However, no specific binding of a DA was demonstrated in some corticotroph pituitary tumours [78], and the D2R was not demonstrated by 123I-epidepride and SPECT imaging in CD or NS [79].
Cabergoline, an ergot-derived DA [23] with a particularly high affinity for D2R, has been investigated as a potential therapy in patients with CD who have failed surgery [73], since it inhibits ACTH secretion in vitro in cases with D2R-positive cells; a direct effect on peripheral cortisol secretion has not been identified [77]. After 3 months of therapy at doses of 2.5–3.5 mg/week, a decrease of >50 % in UFC level and a normalisation of cortisol production were observed in 60 and 40 % of the patients, respectively [77]. In a more recent study, 75 % of 20 patients treated with cabergoline had an initial response [80]; 40 % of these patients still had a sustained response over a 2-year period with a median cabergoline dosage of 3.5 mg/week [80, 81]. In a retrospective study of 30 patients with CD a complete response to cabergoline therapy was reported in 37 % using an initial dose of 0.5–1 mg/week with a further increment of up to 6 mg/week. At a mean dose of 2.1 mg/week, 30 % still had sustained control after 3 years. However, in the group of non-responders, the mean cabergoline dose was only 2 mg/week (range 1–4.5 mg/week) for an average period of 4 months (range 1–9 months). The relatively low dose of cabergoline that was used in most patients might have underestimated the maximal inhibitory effect. Tumour volume decreased or remained stable in the small number of reported patients with visible adenomas [82]. Approximately 25 % of patients show an escape phenomenon at 2–5 years. Nausea, dizziness and asthenia are typical AEs for DA [7, 80]. Doses ranging from 0.5 to 7.0 mg/week (median 3.5 mg) raise potential concerns about long-term safety by activating valvular fibroblasts through serotonin receptor 2B, since the dose of cabergoline as well as the period of exposure to the drug seems to mostly affect the occurrence of this AE [83, 84]. However, this has not so far proven to be a problem [85]. D2R can also be expressed by ACTH-producing NENs, and in a small case series, complete responses were observed after treatment with cabergoline, even when used as monotherapy [86].
Nevertheless, based on available data, pasireotide and cabergoline do not appear to have a rapid onset of action, while no pertinent data have been published in critically ill patients with hypercortisolism. Despite the fact that it would be prudent not to recommend them as monotherapy in critically ill patients based on available data, there are few reports of their use as combination therapy in SCS.
Combination treatment with ketoconazole and cabergoline was studied in patients with CD, and effective control was seen only with their combination [87]. Fourteen patients with CD were divided into two groups: six patients initially treated with cabergoline for 4–6 months (increasing from 0.5–1 mg/week up to 3.0 mg/week), after which ketoconazole was added and eight patients first took ketoconazole alone for 4–6 months (increasing from 200 mg/day to 600 mg/day), then cabergoline was added; they were compared with 14 age-matched patients in prolonged remission after effective neurosurgery for CD. The combination therapy led to UFC normalisation in 79 % of patients with no differences between the groups, but with a persistent subclinical hypercortisolism; only one patient failed to respond at all. Neither drug succeeded in controlling the disease when taken alone [87].
However, in a small cohort of patients with CD displaying mild, moderate or severe hypercortisolaemia, the combination of pasireotide, cabergoline and ketoconazole controlled hypercortisolaemia in 88 % of patients, while this rate was only 29 % with pasireotide monotherapy and 47 % when the latter was combined with cabergoline, emphasising that patients with more severe hypercortisolism at baseline needed more drugs to normalise UFC excretion [74]. In vitro studies showed that sst2 mRNA expression levels of adenomas from patients after pasireotide mono- or combination therapy submitted in resection of pituitary adenoma, who were all in remission, were significantly higher than those of adenomas from patients with elevated preoperative UFC excretion. This fact confirmed that glucocorticoid-induced sst2 down-regulation is a dynamic process that might be reversed by cortisol-lowering therapy [23].
Temozolomide is an orally administrated second-generation alkylating chemotherapeutic drug leading to cell apoptosis [26]. Temozolomide has been used in cases of aggressive corticotroph pituitary adenomas or carcinomas refractory to surgery or pituitary irradiation with some promising results [23, 88–91], implying a role in SCS when these neoplasms are accompanied by uncontrolled hypercortisolaemia.
Other combination treatments may succeed in reducing cortisol levels in the short term. In one case, a 43-year-old woman with EAS associated with a typical bronchial NEN was on medical therapy with high doses of ketoconazole in addition to supportive therapies (intravenous potassium chloride, furosemide, potassium canrenoate, insulin, enoxaparin and antidepressants), but her clinical condition continued to worsen, with the onset of a psychotic crisis and suicidal ideations implying a high surgical risk. Thus, ketoconazole along with radiofrequency ablation with computerised tomography (CT) guidance was performed in the primary lung cancer and hypercortisolaemia was improved along with her clinical condition; surgical resection of the primary ACTH-producing tumour was performed later as a definitive procedure [92].
4 Conclusions
In an acute situation in a patient with clinically obvious CS, this can be confirmed in most instances with a single grossly elevated serum cortisol level taken at any time of the day. The most urgent priority is to treat the metabolic complications such as diabetes, hypokalaemia and hypertension, cardiac failure and thromboembolism, stabilise any psychotic state, and vigorously treat any suspected sepsis or perforated viscus. Emergency lowering of the elevated serum cortisol is most rapidly achieved with oral metyrapone and/or ketoconazole; if parenteral therapy is required then intravenous etomidate is rapidly effective in almost all cases. Combination therapy seems useful to allow the use of lower individual drug dosages. All measures require careful supervision to avoid hypoadrenalism when hypercortisolism is controlled. If medical treatment fails, BA has to be performed in the shortest possible time span to prevent the debilitating complications of uncontrolled hypercortisolaemia.
References
Newell-Price J, Bertagna X, Grossman AB, et al. Cushing’s syndrome. Lancet. 2006;367:1605–17.
Sarlis NJ, Chanock SJ, Nieman LK. Cortisolemic indices predict severe infections in Cushing syndrome due to ectopic production of adrenocorticotropin. J Clin Endocrinol Metab. 2000;85:42–7.
Corcuff JB, Young J, Masquefa-Giraud P, et al. Rapid control of severe neoplastic hypercortisolism with metyrapone and ketoconazole. Eur J Endocrinol. 2015;172:473–8.
Reincke M, Ritzel K, Osswald A, et al. A critical re-appraisal of bilateral adrenalectomy for ACTH-dependent Cushing’s syndrome. Eur J Endocrinol. 2015;173:M23–32.
Lindholm J, Juul S, Jørgensen JO, et al. Incidence and late prognosis of Cushing’s syndrome: a population-based study. J Clin Endocrinol Metab. 2001;86:117–23.
van Haalen FM, Broersen LH, Jorgensen JO, et al. Management of endocrine disease: mortality remains increased in Cushing’s disease despite biochemical remission: a systematic review and meta-analysis. Eur J Endocrinol. 2015;172:R143–9.
Nieman LK, Biller BM, Findling JW, et al. Treatment of Cushing’s syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2015;100:2807–31.
Van Zaane B, Nur E, Squizzato A, et al. Hypercoagulable state in Cushing’s syndrome: a systematic review. J Clin Endocrinol Metab. 2009;94:2743–50.
Kamenický P, Droumaguet C, Salenave S, et al. Mitotane, metyrapone, and ketoconazole combination therapy as an alternative to rescue adrenalectomy for severe ACTH-dependent Cushing’s syndrome. J Clin Endocrinol Metab. 2011;96:2796–804.
Alexandraki KI, Grossman AB. Emergency treatment of florid Cushing’s Syndrome in endocrine and metabolic medical emergencies: a clinician’s guide. Endocrine Press. 2014. doi:10.1210/EME.9781936704811.ch16.
Alexandraki KI, Grossman AB. Cushing’s syndrome. In: Bandeira F, Gharib H, Golbert A, Griz L, Faria M, editors. Endocrinology and diabetes: a problem oriented approach. New York: Springer Science + Business Media; 2014. p. 99–111.
Singh Y, Kotwal N, Menon AS. Endocrine hypertension—Cushing’s syndrome. Indian J Endocrinol Metab. 2011;15(Suppl 4):S313–6.
Arlt A, Harbeck B, Anlauf M, et al. Fatal pneumocystis jirovecii pneumonia in a case of ectopic Cushing’s syndrome due to neuroendocrine carcinoma of the kidney. Exp Clin Endocrinol Diabetes. 2008;116:515–9.
Christ-Crain M, Jutla S, Widmer I, et al. Measurement of serum free cortisol shows discordant responsivity to stress and dynamic evaluation. J Clin Endocrinol Metab. 2007;92:1729–35.
Boonen E, Bornstein SR, Van den Berghe G. New insights into the controversy of adrenal function during critical illness. Lancet Diabetes Endocrinol. 2015;3:805–15.
Moraes RB, Czepielewski MA, Friedman G, et al. Diagnosis of adrenal failure in critically ill patients. Arq Bras Endocrinol Metabol. 2011;55:295–302.
Faucz FR1, Zilbermint M, Lodish MB, et al. Macronodular adrenal hyperplasia due to mutations in an armadillo repeat containing 5 (ARMC5) gene: a clinical and genetic investigation. J Clin Endocrinol Metab. 2014;99:E1113–9.
Epperla N, McKiernan F. Iatrogenic Cushing syndrome and adrenal insufficiency during concomitant therapy with ritonavir and fluticasone. Springerplus. 2015;4:455.
Pai M, Douketis JD, section editors, Lawrence LK Leung, Jess Mandel, Deputy Editor Geraldine Finlay. Prevention of venous thromboembolic disease in medical patients. Topic 1346 version 40.0. Literature review current through: Mar 2013. This topic last updated: Feb 12, 2013.
Oosterhuis JK, van den Berg G, Monteban-Kooistra WE, et al. Life-threatening Pneumocystis jiroveci pneumonia following treatment of severe Cushing’s syndrome. Neth J Med. 2007;65:215–7.
Drake WM, Perry LA, Hinds CJ, et al. Emergency and prolonged use of intravenous etomidate to control hypercortisolemia in a patient with Cushing’s syndrome and peritonitis. J Clin Endocrinol Metab. 1998;83:3542–4.
Stuijver DJ, van Zaane B, Feelders RA, et al. Incidence of venous thromboembolism in patients with Cushing’s syndrome: a multicenter cohort study. J Clin Endocrinol Metab. 2011;96:3525–32.
van der Pas R, de Herder WW, Hofland LJ, et al. New developments in the medical treatment of Cushing’s syndrome. Endocr Relat Cancer. 2012;19:R205–23.
Hall JJ, Hughes CA, Foisy MM, et al. Iatrogenic Cushing syndrome after intra-articular triamcinolone in a patient receiving ritonavir-boosted darunavir. Int J STD AIDS. 2013;24:748–52.
Alexandraki KI, Grossman AB. Medical therapy for Cushing’s disease: past and future modes of treatment. Eur Endocrinol. 2009;4:74–80.
Cuevas-Ramos D, Fleseriu M. Treatment of Cushing’s disease: a mechanistic update. J Endocrinol. 2014;223:R19–39.
Jeffcoate WJ, Rees LH, Tomlin S, et al. Metyrapone in long-term management of Cushing’s disease. Br J Med. 1977;2:215–7.
Donckier J, Burrin JM, Ramsay ID, et al. Successful control of Cushing’s disease in the elderly with long term metyrapone. Postgrad Med J. 1986;62:727–30.
Daniel E, Aylwin S, Mustafa O, et al. Effectiveness of metyrapone in the treatment of Cushing’s Syndrome: a retrospective multicenter study in 195 patients. J Clin Endocrinol Metab. 2015;100:4146–54.
Verhelst JA, Trainer PJ, Howlett TA, et al. Short- and long-term responses to metyrapone in the medical management of 91 patients with Cushing’s syndrome. Clin Endocrinol. 1991;35:169–78.
Monaghan PJ, Owen LJ, Trainer PJ, et al. Comparison of serum cortisol measurement by immunoassay and liquid chromatography-tandem mass spectrometry in patients receiving the 11β-hydroxylase inhibitor metyrapone. Ann Clin Biochem. 2011;48:441–6.
Loose DS, Kan PB, Hirst MA, et al. Ketoconazole blocks adrenal steroidogenesis by inhibiting cytochrome P450-dependent enzymes. J Clin Invest. 1983;71:1495–9.
Jimenez Reina L, Leal-Cerro A, Garcia J, et al. In vitro effects of ketoconazole on corticotrope cell morphology and ACTH secretion of two pituitary adenomas removed from patients with Nelson’s syndrome. Acta Endocrinol (Copenh), 1989;121:185–90.
Loose DS, Stover EP, Feldman D. Ketoconazole binds to glucocorticoid receptors and exhibits glucocorticoid antagonist activity in cultured cells. J Clin Invest. 1983;72:404–8.
Castinetti F, Morange I, Jaquet P, et al. Ketoconazole revisited: a preoperative or postoperative treatment in Cushing’s disease. Eur J Endocrinol. 2008;158:91–9.
Duarte PA, Chow CC, Simmons F, et al. Fatal hepatitis associated with ketoconazole therapy. Arch Intern Med. 1984;144:1069–70.
Castinetti F, Guignat L, Giraud P, et al. Ketoconazole in Cushing’s disease: is it worth a try? J Clin Endocrinol Metab. 2014;99:1623–30.
Salvatori R, DelConte A, Geer EB, et al. An open-label study to assess the safety and efficacy of levoketoconazole (COR-003) in the treatment of endogenous Cushing’s syndrome. In: Program of the 97th annual meeting of The Endocrine Society, March 5–8, 2015; San Diego, CA. Abstract endocrine reviews. 2015;36:376.
Lamberts SW, Bons EG, Bruining HA, et al. Differential effects of the imidazole derivatives etomidate, ketoconazole and miconazole and of metyrapone on the secretion of cortisol and its precursors by human adrenocortical cells. J Pharmacol Exp Ther. 1987;240:259–64.
Klausen NO, Moelgaard J, Ferguson AH, et al. Negative synacthen test during etomidate infusion. Lancet. 1983;2:848.
Krakoff J, Koch CA, Calis KA, et al. Use of a parenteral propylene glycol-containing etomidate preparation for the long-term management of ectopic Cushing’s syndrome. J Clin Endocrinol Metab. 2001;86:4104–8.
Johnson TN, Canada TW. Etomidate use for Cushing’s syndrome caused by an ectopic adrenocorticotropic hormone-producing tumor. Ann Pharmacother. 2007;41:350–3.
Greening JE, Brain CE, Perry LA, et al. Efficient short-term control of hypercortisolaemia by low-dose etomidate in severe paediatric Cushing’s disease. Horm Res. 2005;64:140–3.
Preda VA, Sen J, Karavitaki N, Ab Grossman, et al. Etomidate in the management or hypercortisolaemia in Cushing’s syndrome: a review. Eur J Endocrinol. 2012;167:137–43.
Schulte HM, Benker G, Reinwein D, et al. Infusion of low dose etomidate: correction of hypercortislemia in patients with Cushing’s syndrome and dose–response relationship in normal subjects. J Clin Endocrinol Metab. 1990;70:1426–30.
Ntali G, Asimakopoulou A, Siamatras T, et al. Mortality in Cushing’s syndrome: systematic analysis of a large series with prolonged follow-up. Eur J Endocrinol. 2013;8(169):715–23.
Morris LF, Harris RS, Milton DR, et al. Impact and timing of bilateral adrenalectomy for refractory adrenocorticotropic hormone-dependent Cushing’s syndrome. Surgery. 2013;154:1174–83.
Farage M, Costa MA, Godoy-Matos AF. A rare case of Cushing syndrome by cyclic ectopic-ACTH. Arq Bras Endocrinol Metabol. 2012;56:324–30.
Cueto C, Brown JHU. Biological studies on an adrenocorticolytic agent and the isolation of the active components. Endocrinology. 1958;62:326–33.
Kroiss M, Quinkler M, Lutz WK, et al. Drug interactions with mitotane by induction of CYP3A4 metabolism in the clinical management of adrenocortical carcinoma. Clin Endocrinol (Oxf). 2011;75:585–91.
Alexandraki KI, Kaltsas GA, le Roux CW, et al. Assessment of serum-free cortisol levels in patients with adrenocortical carcinoma treated with mitotane: a pilot study. Clin Endocrinol (Oxf). 2010;72:305–11.
Bertagna X, Bertagna C, Laudat MH, et al. Pituitary-adrenal response to the antiglucocorticoid action of RU 486 in Cushing’s syndrome. J Clin Endocrinol Metab. 1986;63:639–43.
Fleseriu M, Biller BM, Findling JW, et al. Mifepristone, a glucocorticoid receptor antagonist, produces clinical and metabolic benefits in patients with Cushing’s syndrome. J Clin Endocrinol Metab. 2012;97:2039–49.
de Bruin C, Hofland LJ, Nieman LK, et al. Mifepristone effects on tumor somatostatin receptor expression in two patients with Cushing’s syndrome due to ectopic adrenocorticotropin secretion. J Clin Endocrinol Metab. 2012;97:455–62.
Castinetti F, Fassnacht M, Johanssen S, et al. Merits and pitfalls of mifepristone in Cushing’s syndrome. Eur J Endocrinol. 2009;160:1003–10.
Chu JW, Matthias DF, Belanoff J, et al. Successful long-term treatment of refractory Cushing’s disease with high-dose mifepristone (RU 486). J Clin Endocrinol Metab. 2001;86:3568–73.
Fleseriu M, Findling JW, Koch CA, et al. Changes in plasma ACTH levels and corticotroph tumor size in patients with Cushing’s disease during long-term treatment with the glucocorticoid receptor antagonist mifepristone. J Clin Endocrinol Metab. 2014;99:3718–27.
Calhoun DA, White WB, Krum H, et al. Effects of a novel aldosterone synthase inhibitor for treatment of primary hypertension: results of a randomized, double-blind, placebo- and active-controlled phase 2 trial. Circulation. 2011;124:1945–55.
Bertagna X, Pivonello R, Fleseriu M, et al. LCI699, a potent 11β-hydroxylase inhibitor, normalizes urinary cortisol in patients with Cushing’s disease: results from a multicenter, proof-of-concept study. J Clin Endocrinol Metab. 2014;99:1375–83.
Daniel E, Newell-Price JD. Therapy of endocrine disease: steroidogenesis enzyme inhibitors in Cushing’s syndrome. Eur J Endocrinol. 2015;172:R263–80.
Riedl M, Maier C, Zettinig G, et al. Long term control of hypercortisolism with fluconazole: case report and in vitro studies. Eur J Endocrinol. 2006;154:519–24.
Schwetz V, Aberer F, Stiegler C, et al. Fluconazole and acetazolamide in the treatment of ectopic Cushing’s syndrome with severe metabolic alkalosis. Endocrinol Diabetes Metab Case Rep. 2015;2015:150027.
Patel YC. Somatostatin and its receptor family. Front Neuroendocrinol. 1999;20:157–98.
Miller GM, Alexander JM, Bikkal HA, et al. Somatostatin receptor subtype gene expression in pituitary adenomas. J Clin Endocrinol Metab. 1995;80:1386–92.
Schonbrunn A. Glucocorticoids down-regulate somatostatin receptors on pituitary cells in culture. Endocrinology. 1982;110:1147–54.
Stalla GK, Brockmeier SJ, Renner U, et al. Octreotide exerts different effects in vivo and in vitro in Cushing’s disease. Eur J Endocrinol. 1994;130:125–31.
van der Pas R, Feelders RA, Gatto F, et al. Preoperative normalization of cortisol levels in Cushing’s disease after medical treatment: consequences for somatostatin and dopamine receptor subtype expression and in vitro response to somatostatin analogs and dopamine agonists. J Clin Endocrinol Metab. 2013;98:E1880–90.
Park S, Kamegai J, Kineman RD. Role of glucocorticoids in the regulation of pituitary somatostatin receptor subtype (sst1-sst5) mRNA levels: evidence for direct and somatostatin-mediated effects. Neuroendocrinology. 2003;78:163–75.
van der Hoek J, Waaijers M, van Koetsveld PM, et al. Distinct functional properties of native somatostatin receptor subtype 5 compared with subtype 2 in the regulation of ACTH release by corticotroph tumor cells. Am J Physiol Endocrinol Metab. 2005;289:E278–87.
Boscaro M, Ludlam WH, Atkinson B, et al. Treatment of pituitary-dependent Cushing’s disease with the multireceptor ligand somatostatin analog pasireotide (SOM230): a multicenter, phase II trial. J Clin Endocrinol Metab. 2009;94:115–22.
Colao A, Petersenn S, Newell-Price J, et al. A 12-month phase 3 study of pasireotide in Cushing’s disease. N Engl J Med. 2012;366:914–24.
Simeoli C, Auriemma RS, Tortora F, et al. The treatment with pasireotide in Cushing’s disease: effects of long-term treatment on tumor mass in the experience of a single center. Endocrine. 2015;50:725–40.
de Bruin C, Feelders RA, Lamberts SW, et al. Somatostatin and dopamine receptors as targets for medical treatment of Cushing’s syndrome. Rev Endocr Metab Disord. 2009;10:91–102.
Feelders RA, de Bruin C, Pereira AM, et al. Pasireotide alone or with cabergoline and ketoconazole in Cushing’s disease. N Engl J Med. 2010;362:1846–8.
Caron MG, Beaulieu M, Raymond V, et al. Dopaminergic receptors in the anterior pituitary gland. Correlation of [3H]dihydroergocryptine binding with the dopaminergic control of prolactin release. J Biol Chem. 1978;253:2244–53.
Stefaneanu L, Kovacs K, Horvath E, et al. Dopamine D2 receptor gene expression in human adenohypophysial adenomas. Endocrine. 2001;14:329–36.
Pivonello R, Ferone D, de Herder WW, et al. Dopamine receptor expression and function in corticotroph pituitary tumors. J Clin Endocrinol Metab. 2004;89:2452–62.
Cronin MJ, Cheung CY, Wilson CB, et al. [3H]Spiperone binding to human anterior pituitaries and pituitary adenomas secreting prolactin, growth hormone, and adrenocorticotropic hormone. J Clin Endocrinol Metab. 1980;50:387–91.
Pirker W, Riedl M, Luger A, et al. Dopamine D2 receptor imaging in pituitary adenomas using iodine-123-epidepride and SPECT. J Nucl Med. 1996;37:1931–7.
Pivonello R, De Martino MC, Cappabianca P, et al. The medical treatment of Cushing’s disease: effectiveness of chronic treatment with the dopamine agonist cabergoline in patients unsuccessfully treated by surgery. J Clin Endocrinol Metab. 2009;94:223–30.
Lila AR, Gopal RA, Acharya SV, et al. 2010 efficacy of cabergoline in uncured (persistent or recurrent) Cushing disease after pituitary surgical treatment with or without radiotherapy. Endocr Pract. 2010;16:968–76.
Godbout A, Manavela M, Danilowicz K, et al. Cabergoline monotherapy in the long-term treatment of Cushing’s disease. Eur J Endocrinol. 2010;163:709–16.
Zanettini R, Antonini A, Gatto G, et al. Valvular heart disease and the use of dopamine agonists for Parkinson’s disease. N Engl J Med. 2007;356:39–46.
Schade R, Andersohn F, Suissa S, et al. Dopamine agonists and the risk of cardiac-valve regurgitation. N Engl J Med. 2007;356:29–38.
Delgado V, Biermasz NR, van Thiel SW, et al. Changes in heart valve structure and function in patients treated with dopamine agonists for prolactinomas, a 2-year follow-up study. Clin Endocrinol (Oxf). 2012;77:99–105.
Pivonello R, Ferone D, de Herder WW, et al. Dopamine receptor expression and function in corticotroph ectopic tumors. J Clin Endocrinol Metab. 2007;92:65–9.
Barbot M, Albiger N, Ceccato F, et al. Combination therapy for Cushing’s disease: effectiveness of two schedules of treatment: should we start with cabergoline or ketoconazole? Pituitary. 2014;17:109–17.
McCormack AI, Wass JA, Grossman AB. Aggressive pituitary tumours: the role of temozolomide and the assessment of MGMT status. Eur J Clin Invest. 2011;41:1133–48.
Dillard TH, Gultekin SH, Delashaw JB Jr, et al. Temozolomide for corticotroph pituitary adenomas refractory to standard therapy. Pituitary. 2011;14:80–91.
Curtò L, Torre ML, Ferraù F, et al. Temozolomide-induced shrinkage of a pituitary carcinoma causing Cushing’s disease—report of a case and literature review. ScientificWorldJournal. 2010;10:2132–8.
Alexandraki K, Boutzios G, Nikolopoulos G, et al. Optic neuropathy following radiotherapy for Cushing’s disease followed by the diagnosis of pituitary carcinoma. Endocrine Abstracts. 2015;37(EP75):4.
Corsello SM, Senes P, Iezzi R, Rufini, et al. Cushing’s syndrome due to a bronchial ACTH-secreting carcinoid successfully treated with radiofrequency ablation (RFA). J Clin Endocrinol Metab. 2014;99:E862–5.
Acknowledgments
ABG has received consulting and lecture fees from Novartis, Ipsen and HRA Pharma. KIA has nothing to declare. No funding was used in the preparation of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alexandraki, K.I., Grossman, A.B. Therapeutic Strategies for the Treatment of Severe Cushing’s Syndrome. Drugs 76, 447–458 (2016). https://doi.org/10.1007/s40265-016-0539-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-016-0539-6