Abstract
3-Hydroxy-3-methylglutaryl-coenzyme A reductase inhibitors (statins) are currently among the most commonly prescribed pharmaceutical agents worldwide. Apart from their well-established therapeutic value in cardiovascular disease, there is a long-standing debate on their potential association with cancer. To obtain and discuss the existing clinical evidence, an overview of meta-analysis articles addressing this issue was carried out. As of today, the accumulated evidence does not support the hypothesis that statins affect the risk of developing cancer, when they are taken at low doses for managing hypercholesterolaemia. However, current data cannot exclude an increased cancer risk in elderly patients associated with hydrophilic statin use, or decreases in the risks of certain cancers, such as gastric, oesophageal, liver, colorectal and advanced/aggressive prostate cancer. On the other hand, some recent observational studies have provided evidence that statins might be useful in modifying the prognosis of patients diagnosed with malignancy. Until a definitive benefit is demonstrated in randomized controlled trials, statins cannot be recommended either for cancer prevention or for modifying cancer-related outcomes. Further research is warranted to clarify the potential role(s) of statins in the prevention and treatment of cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The accumulated clinical evidence shows that statins are not a ‘magic bullet’ for cancer. However, it is still possible that statins may have a role to play in cancer prevention or treatment. |
Statins cannot be recommended for primary cancer prevention or for modification of cancer-related outcomes, until and unless a definitive benefit is demonstrated in prospective randomized trials. |
1 Introduction
3-Hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase inhibitors (statins) are currently among the most commonly prescribed pharmaceutical agents worldwide [1, 2] as a result of their well-established efficacy in primary and secondary prevention of cardiovascular disease in a variety of populations [3–8]. The release of the 2013 American College of Cardiology/American Heart Association (ACC/AHA) guidelines on the assessment of cardiovascular risk [9] and on the treatment of blood cholesterol, which included recommendations for primary prevention with statins [10], are expected to lead to a further increase in their use [11].
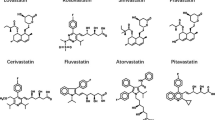
There are currently seven statins on the market: atorvastatin, fluvastatin, lovastatin, pitavastatin, pravastatin, rosuvastatin and simvastatin. Their main mechanism of action is the reduction of serum cholesterol levels by means of competitive inhibition of hepatic HMG-CoA reductase, which is the rate-limiting enzyme in the mevalonate synthesis pathway [12]. This leads to reduced endogenous cholesterol biosynthesis and, thus, to decreased levels of low-density lipoprotein, which is a major risk factor for atherosclerosis [13]. In addition, statins have been shown to improve endothelial function, stabilize plaques, reduce free radical formation and inhibit endothelial inflammatory reactions, thereby yielding other potential benefits for patients, regardless of cholesterol level reduction [14–16].
Apart from their well-documented therapeutic value in cardiovascular disease, there is a long-standing debate on the potential association between statins and cancer. In recent years, a growing body of studies has suggested that statins may have a potential role in the field of cancer chemoprevention [17–20] (also termed ‘cancer-preventive therapy’). A number of mechanisms have been proposed regarding the potential antitumour effects of statins, through inhibition of proliferation, migration and invasion, and through induction of apoptosis [21]. On the other hand, concerns have also been raised regarding their safety [22]. An early review of rodent carcinogenicity data reported that lipid-lowering drugs, including statins, initiate or promote cancer (liver, forestomach, lung and thyroid tumours, and lymphoma) in rats and mice [23]. However, in most of the reviewed studies, the doses used were substantially higher than the doses recommended for humans, and the employed bioassays were criticized for being inadequate to predict carcinogenicity in humans [24].
There is already a large number of randomized trials and observational studies examining the association between statins and cancer, and even several meta-analyses thereof. Given that meta-analysis is high up in the proposed hierarchies of evidence [25–27], an overview of meta-analysis articles addressing this association was performed in order to obtain and discuss the existing clinical data on the subject.
2 Literature Review
2.1 Methods
Articles of interest for this overview were meta-analyses that examined the association between statins and cancer, having incorporated the evidence from randomized controlled trials of statins against placebo (or no treatment) and/or data from observational studies. The Medline database was searched from inception to 15 April 2014. Search terms included {HMG-CoA reductase inhibitor(s) or statin(s)} combined with {cancer(s), carcinoma(s), malignancy(ies), neoplasm(s) or tumor(s)}. The database search was limited to meta-analysis articles (publication type) and was also limited to the English language, human subjects and having an abstract available.
The titles and abstracts of identified published articles were scanned to exclude irrelevant publications. The full text of the selected articles was carefully read. Meta-analyses were considered regardless of whether they had included randomized trials, observational studies or both study designs; however, the meta-analyses of randomized trials was the preferred source of evidence for this overview, because the randomized controlled trial is the study design that is least likely to be biased. Cancer was the outcome of interest—either all malignancies combined or site- and type-specific cancers. The following information was collected from each meta-analysis article: the first author’s last name, journal, year of publication, type of meta-analysis (i.e. individual participant data-based or literature-based), statin medications, cancer sites/types, number and design of included studies, and main and secondary results.
2.2 Search Results
Forty meta-analyses examining the association between statin use and cancer were identified (Table 1) [28–67]. Thirteen of those (32.5 %) included only large-scale randomized controlled trials of statins for cardiovascular outcomes, which reported cancer outcomes as secondary/safety endpoints [29, 30, 45, 49, 50, 52, 59, 61–64, 66, 67]. Eight of the meta-analyses (20 %) included only observational studies [34, 36, 38, 40, 44, 46, 48, 56], while the remaining 19 (47.5 %) included both study designs [28, 31–33, 35, 37, 39, 41–43, 47, 51, 53–55, 57, 58, 60, 65].
The majority of the meta-analyses were literature based [28–44, 46–48, 52–62, 64–67], while five analyzed individual participant data [45, 49–51, 63]. Their publication dates ranged between 2001 and 2014. Of note, these meta-analyses are chronologically built on an ever-expanding array of studies, and so there are inherent correlations from an earlier meta-analysis to a later one.
2.3 Limitations
This overview of meta-analysis articles suffers some limitations; only one database was searched, a single author selected studies for inclusion and quality assessment of the meta-analyses was not performed. Further limitations reflect the nature of the primary data included in the 40 meta-analyses identified. By design, the participants enrolled in the randomized controlled trials of statins for cardiovascular outcomes were at low risk of developing cancer. Given the small numbers of cancer cases, these studies may have not been adequately powered to detect potentially small differences in cancer risk. Moreover, because cancer occurrence was not the primary outcome of these trials, patients were not routinely screened for cancer—a fact that may have affected the cancer detection rate. On the other hand, the observational data may have suffered some common limitations of pharmacoepidemiological studies, such as lack of control for drug dose and duration, short follow-up periods, recall bias from self-reported data, detection bias and confounding by indication, as well as selective reporting and other biases.
3 Do Statins Have a Potential Role in Cancer Prevention?
The evidence from meta-analyses of randomized and observational studies does not support the hypothesis that statin treatment affects cancer risk when taken at low doses for managing hypercholesterolaemia. The null findings are consistent for total cancer (i.e. the aggregate of all malignancies) and for most of the site-specific cancers (e.g. respiratory, breast, pancreatic, haematological, kidney or bladder cancer, or melanoma) [28, 29, 32, 39, 42, 43, 45–47, 49–54, 57, 60–67]. Moreover, a recent meta-analysis of large randomized trials with extended follow-up confirmed that statin treatment did not affect cancer incidence or mortality in the long term (up to 10 years and beyond), having included data for 47,296 individuals with total follow-up ranging from 6.7 to 14.7 years [30].
On the other hand, current evidence cannot exclude a modest decrease in the risk of developing colorectal cancer [31, 56, 58], a lower risk of advanced/aggressive prostate cancer [48, 55] or even larger risk reductions for certain cancer types (i.e. gastric, oesophageal or hepatocellular) [33–35, 37, 38, 41] associated with statin use. These hypotheses are mainly driven by observational studies, while the randomized evidence is scarce. However, observational studies lack the experimental random allocation of the intervention, which is necessary to optimally test exposure–outcome hypotheses. In any event, these findings should be regarded with caution because the possibility of residual confounding cannot be excluded, either from unknown or unmeasured factors, or from imperfectly adjusted real confounders [68, 69].
A yet uncertain issue refers to the hypothesis that the different chemical structures and pharmacokinetic properties of statins may imply different effects on cancer risk [70]. Statins are subclassified as either hydrophilic (such as pravastatin and rosuvastatin) or lipophilic (such as atorvastatin, fluvastatin, lovastatin and simvastatin). It has been suggested that lipophilic statins may be more effective for cancer chemoprevention [71, 72]. Most meta-analyses have pooled hydrophilic and lipophilic statins, ignoring any potential differential effect on cancer risk. However, even those meta-analyses that analyzed by statin class failed to show any difference in cancer risk with hydrophilic versus lipophilic statins [60, 64].
The potential relationship between pravastatin use and the risk of cancer in elderly patients is another issue that remains unclear [59]. The PROSPER (Prospective Study of Pravastatin in the Elderly at Risk) trial [73] showed a higher cancer risk in elderly patients treated with pravastatin, compared with those on placebo (p = 0.02). The authors suggested that the increased cancer rate was most likely due to chance [73, 74]. However, a significant increase in cancer rates among elderly patients assigned to pravastatin therapy was also reported in a subgroup analysis of the LIPID (Long-Term Intervention with Pravastatin in Ischaemic Disease) trial [75]. Moreover, in the CARE (Cholesterol and Recurrent Events) trial [6], breast cancer occurred in a greater number of women treated with pravastatin (p = 0.002). Similarly, WOSCOPS (the West of Scotland Coronary Prevention Study) [76] showed an increase in prostate cancer risk in the pravastatin group (p = 0.03). A meta-regression analysis of all available pravastatin trials [59] suggested the hypothesis that pravastatin therapy may be associated with an increasing risk of cancer as age increases.
Though a causal relationship cannot be established, it has been hypothesized [22] that hydrophilic pravastatin may promote cancer by causing an induction of HMG-CoA reductase and, hence, mevalonate synthesis in extrahepatic tissues. Mevalonate can promote the growth of occult neoplastic or preneoplastic cells [77]. Because of the absence of uptake of pravastatin by most extrahepatic cells, this statin will be unable to mitigate the increase in mevalonate synthesis in extrahepatic tissues that accompanies the decrease in circulating cholesterol caused by its inhibition of hepatic HMG-CoA reductase. Thus, increased mevalonate synthesis in extrahepatic tissues might explain an increased cancer risk in elderly patients, who are expected to harbour a large number of preneoplastic and occult neoplastic lesions [22]. Conversely, the uptake of the lipophilic statins in extrahepatic tissues mitigates the increase in mevalonate synthesis that accompanies the decrease in serum cholesterol that they induce [78]. Thus, lipophilic statins should be expected not to promote cancer [22]. However, the epidemiological evidence on those issues remains unclear. Further research and detailed individual patient data-based meta-analyses, following appropriate methods of analysis, are warranted [79, 80].
4 Do Statins Have a Potential Role in Modifying Cancer-Related Outcomes?
Unlike the plethora of randomized controlled trials and observational studies providing data for the evaluation of statins for the primary prevention of cancer (and adequate meta-analytic evidence thereof), data are lacking for any effects of statin treatment on cancer prognosis and secondary/tertiary prevention, with the exception of weak evidence from a limited number of large observational studies. Recently, a population-based registry study [81] assessed mortality among over 295,000 Danish patients who had received a diagnosis of cancer between 1995 and 2007. The study reported that statin use (begun before the cancer diagnosis) was associated with a 15 % reduction in cancer-related mortality across a broad range of malignancies. Though this study suffered from some inherent limitations [82] stemming from its observational nature, the results have captured much attention, and further prospective randomized research is urgently warranted to confirm or refute the hypothesis that statin administration prolongs the survival of patients with cancer. Given that numerous experimental studies have also demonstrated that statins, especially the lipophilic ones, exert strong antiproliferative and proapoptotic effects on various tumour cell lines of differing origins [83–86], a role of statins in modifying cancer-related outcomes is still quite possible.
At the level of site-specific cancers, there is also some weak evidence suggesting that statins might be effective to prevent recurrence and/or improve survival in patients suffering from colorectal, breast, prostate or hepatocellular malignancies. In a large population-based cohort study of newly diagnosed colorectal cancer patients [87], statin use after the diagnosis was associated with reduced colorectal cancer-specific mortality. A number of cohort studies have also reported a reduced risk of recurrence in breast cancer patients using statins [88–93], but others have not [94]. Similarly, a recent cohort study [95] demonstrated that statin administration was associated with a decreased risk of prostate cancer mortality. An earlier well-conducted meta-analysis of 13 cohort studies [36] examined the association between statin use and recurrence-free survival following treatment of localized prostate cancer, and suggested a potentially beneficial effect of statins in prostate cancer patients treated with radiotherapy, but not among those patients treated with radical prostatectomy. Nevertheless, this meta-analysis was limited by the observational nature of the primary studies that were included, and the statistically significant between-studies heterogeneity that was identified [36]. On the other hand, a small randomized clinical trial performed in a population of patients with hepatocellular cancer [96] has demonstrated that pravastatin use significantly increased their survival. In contrast, other recently published observational studies have failed to show any beneficial effect of statins on the recurrence and progression of renal [97] and gastric [98] malignancies.
5 Conclusions
A large number of clinical studies have analyzed the cancer risk in statin users. As of today, the accumulated data do not support the hypothesis that statins affect the risk of developing cancer when taken at low doses for managing hypercholesterolaemia. However, current evidence cannot exclude an increased cancer risk in elderly patients associated with hydrophilic statin use, or important decreases in the risk of certain cancers, such as gastric, oesophageal, liver, colorectal and advanced/aggressive prostate cancer. On the other hand, some recently published observational studies provide weak evidence that statins might be useful in modifying cancer-related outcomes in patients who are already suffering from malignancies.
Statins cannot be recommended either for primary cancer prevention or for modification of cancer-related outcomes, until and unless a definitive benefit is demonstrated in prospective randomized trials. However, large-scale clinical trials of statins for cancer prevention are difficult to conduct [99]. Because of statins’ widespread use, it would be very difficult to recruit suitable patient populations, and the long duration of such trials would pose many challenges in terms of probable contamination [100]. It is encouraging, however, that several relatively small clinical trials are ongoing. There are currently over 100 studies on the ClinicalTrials.gov website [101], in various stages of recruitment and data collection, which are investigating different aspects of the relationship between statins and cancer. This effort should continue to help clinicians determine the potential role of statin therapy in the prevention and treatment of cancer.
References
Mann D, Reynolds K, Smith D, et al. Trends in statin use and low-density lipoprotein cholesterol levels among US adults: impact of the 2001 National Cholesterol Education Program guidelines. Ann Pharmacother. 2008;42:1208–15.
Walley T, Folino-Gallo P, Schwabe U, et al. Variations and increase in use of statins across Europe: data from administrative databases. BMJ. 2004;328:385–6.
Ridker PM, Danielson E, Fonseca FA, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359:2195–207.
The Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med. 1998;339:1349–57.
Downs JR, Clearfield M, Weis S, et al. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA. 1998;279:1615–22.
Sacks FM, Pfeffer MA, Moye LA, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial Investigators. N Engl J Med. 1996;335:1001–9.
Shepherd J, Cobbe SM, Ford I, et al. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N Engl J Med. 1995;333:1301–7.
The Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet. 1994;344:1383–9.
Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2935–59.
Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2889–934.
Ioannidis JP. More than a billion people taking statins? Potential implications of the new cardiovascular guidelines. JAMA. 2014;311:463–4.
Goldstein JL, Brown MS. Regulation of the mevalonate pathway. Nature. 1990;343:425–30.
Witztum JL, Steinberg D. Role of oxidized low density lipoprotein in atherogenesis. J Clin Invest. 1991;88:1785–92.
LaRosa JC. Pleiotropic effects of statins and their clinical significance. Am J Cardiol. 2001;88:291–3.
Davignon J. Beneficial cardiovascular pleiotropic effects of statins. Circulation. 2004;109:III39–43.
Bonetti PO, Lerman LO, Napoli C, et al. Statin effects beyond lipid lowering: are they clinically relevant? Eur Heart J. 2003;24:225–48.
Gazzerro P, Proto MC, Gangemi G, et al. Pharmacological actions of statins: a critical appraisal in the management of cancer. Pharmacol Rev. 2012;64:102–46.
Bonovas S, Tsantes A, Drosos T, et al. Cancer chemoprevention: a summary of the current evidence. Anticancer Res. 2008;28:1857–66.
Demierre MF, Higgins PD, Gruber SB, et al. Statins and cancer prevention. Nat Rev Cancer. 2005;5:930–42.
Katz MS. Therapy insight: potential of statins for cancer chemoprevention and therapy. Nat Clin Pract Oncol. 2005;2:82–9.
Pisanti S, Picardi P, Ciaglia E, et al. Novel prospects of statins as therapeutic agents in cancer. Pharmacol Res. 2014;88C:84–98.
Duncan RE, El-Sohemy A, Archer MC. Statins and cancer development. Cancer Epidemiol Biomarkers Prev. 2005;14:1897–8.
Newman TB, Hulley SB. Carcinogenicity of lipid-lowering drugs. JAMA. 1996;275:55–60.
Dalen JE, Dalton WS. Does lowering cholesterol cause cancer? JAMA. 1996;275:67–9.
Harbour R, Miller J. A new system for grading recommendations in evidence based guidelines. BMJ. 2001;323:334–6.
Harris RP, Helfand M, Woolf SH, et al. Methods Work Group, Third US Preventive Services Task Force. Current methods of the US Preventive Services Task Force: a review of the process. Am J Prev Med. 2001;20:21–35.
Nikolopoulos GK, Bagos PG, Bonovas S. Developing the evidence base for cancer chemoprevention: use of meta-analysis. Curr Drug Targets. 2011;12:1989–97.
Zhang XL, Liu M, Qian J, et al. Statin use and risk of kidney cancer: a meta-analysis of observational studies and randomized trials. Br J Clin Pharmacol. 2014;77:458–65.
Bonovas S, Lytras T, Sitaras NM. Statin use and breast cancer: do we need more evidence and what should this be? Expert Opin Drug Saf. 2014;13:271–5.
Lv HL, Jin DM, Liu M, et al. Long-term efficacy and safety of statin treatment beyond six years: a meta-analysis of randomized controlled trials with extended follow-up. Pharmacol Res. 2014;81:64–73.
Lytras T, Nikolopoulos G, Bonovas S. Statins and the risk of colorectal cancer: an updated systematic review and meta-analysis of 40 studies. World J Gastroenterol. 2014;20:1858–70.
Li X, Wu XB, Chen Q. Statin use is not associated with reduced risk of skin cancer: a meta-analysis. Br J Cancer. 2014;110:802–7.
Wu XD, Zeng K, Xue FQ, et al. Statins are associated with reduced risk of gastric cancer: a meta-analysis. Eur J Clin Pharmacol. 2013;69:1855–60.
Beales IL, Hensley A, Loke Y. Reduced esophageal cancer incidence in statin users, particularly with cyclo-oxygenase inhibition. World J Gastrointest Pharmacol Ther. 2013;4:69–79.
Singh PP, Singh S. Statins are associated with reduced risk of gastric cancer: a systematic review and meta-analysis. Ann Oncol. 2013;24:1721–30.
Park HS, Schoenfeld JD, Mailhot RB, et al. Statins and prostate cancer recurrence following radical prostatectomy or radiotherapy: a systematic review and meta-analysis. Ann Oncol. 2013;24:1427–34.
Singh S, Singh AG, Singh PP, et al. Statins are associated with reduced risk of esophageal cancer, particularly in patients with Barrett’s esophagus: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2013;11:620–9.
Pradelli D, Soranna D, Scotti L, et al. Statins and primary liver cancer: a meta-analysis of observational studies. Eur J Cancer Prev. 2013;22:229–34.
Zhang XL, Geng J, Zhang XP, et al. Statin use and risk of bladder cancer: a meta-analysis. Cancer Causes Control. 2013;24:769–76.
Scosyrev E, Tobis S, Donsky H, et al. Statin use and the risk of biochemical recurrence of prostate cancer after definitive local therapy: a meta-analysis of eight cohort studies. BJU Int. 2013;111:E71–7.
Singh S, Singh PP, Singh AG, et al. Statins are associated with a reduced risk of hepatocellular cancer: a systematic review and meta-analysis. Gastroenterology. 2013;144:323–32.
Wang J, Li C, Tao H, et al. Statin use and risk of lung cancer: a meta-analysis of observational studies and randomized controlled trials. PLoS One. 2013;8:e77950.
Tan M, Song X, Zhang G, et al. Statins and the risk of lung cancer: a meta-analysis. PLoS One. 2013;8:e57349.
Mass AY, Agalliu I, Laze J, et al. Preoperative statin therapy is not associated with biochemical recurrence after radical prostatectomy: our experience and meta-analysis. J Urol. 2012;188:786–91.
Cholesterol Treatment Trialists’ (CTT) Collaborators, Mihaylova B, Emberson J, Blackwell L, et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380:581–590.
Undela K, Srikanth V, Bansal D. Statin use and risk of breast cancer: a meta-analysis of observational studies. Breast Cancer Res Treat. 2012;135:261–9.
Cui X, Xie Y, Chen M, et al. Statin use and risk of pancreatic cancer: a meta-analysis. Cancer Causes Control. 2012;23:1099–111.
Bansal D, Undela K, D’Cruz S, et al. Statin use and risk of prostate cancer: a meta-analysis of observational studies. PLoS One. 2012;7:e46691.
Cholesterol Treatment Trialists’ (CTT) Collaboration, Emberson JR, Kearney PM, Blackwell L, et al. Lack of effect of lowering LDL cholesterol on cancer: meta-analysis of individual data from 175,000 people in 27 randomised trials of statin therapy. PLoS One. 2012;7:e29849.
Cholesterol Treatment Trialists’ (CTT) Collaboration, Baigent C, Blackwell L, Emberson J, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376:1670–81.
Matsushita Y, Sugihara M, Kaburagi J, et al. Pravastatin use and cancer risk: a meta-analysis of individual patient data from long-term prospective controlled trials in Japan. Pharmacoepidemiol Drug Saf. 2010;19:196–202.
Bonovas S, Nikolopoulos G, Filioussi K, et al. Can statin therapy reduce the risk of melanoma? A meta-analysis of randomized controlled trials. Eur J Epidemiol. 2010;25:29–35.
Bonovas S, Filioussi K, Sitaras NM. Statins are not associated with a reduced risk of pancreatic cancer at the population level, when taken at low doses for managing hypercholesterolemia: evidence from a meta-analysis of 12 studies. Am J Gastroenterol. 2008;103:2646–51.
Kuoppala J, Lamminpää A, Pukkala E. Statins and cancer: a systematic review and meta-analysis. Eur J Cancer. 2008;44:2122–32.
Bonovas S, Filioussi K, Sitaras NM. Statin use and the risk of prostate cancer: a metaanalysis of 6 randomized clinical trials and 13 observational studies. Int J Cancer. 2008;123:899–904.
Taylor ML, Wells BJ, Smolak MJ. Statins and cancer: a meta-analysis of case-control studies. Eur J Cancer Prev. 2008;17:259–68.
Bonovas S, Filioussi K, Tsantes A, et al. Use of statins and risk of haematological malignancies: a meta-analysis of six randomized clinical trials and eight observational studies. Br J Clin Pharmacol. 2007;64:255–62.
Bonovas S, Filioussi K, Flordellis CS, et al. Statins and the risk of colorectal cancer: a meta-analysis of 18 studies involving more than 1.5 million patients. J Clin Oncol. 2007;25:3462–8.
Bonovas S, Sitaras NM. Does pravastatin promote cancer in elderly patients? A meta-analysis. CMAJ. 2007;176:649–54.
Browning DR, Martin RM. Statins and risk of cancer: a systematic review and metaanalysis. Int J Cancer. 2007;120:833–43.
Freeman SR, Drake AL, Heilig LF, et al. Statins, fibrates, and melanoma risk: a systematic review and meta-analysis. J Natl Cancer Inst. 2006;98:1538–46.
Bonovas S, Filioussi K, Tsavaris N, et al. Statins and cancer risk: a literature-based meta-analysis and meta-regression analysis of 35 randomized controlled trials. J Clin Oncol. 2006;24:4808–17.
Stein EA, Corsini A, Gimpelewicz CR, et al. Fluvastatin treatment is not associated with an increased incidence of cancer. Int J Clin Pract. 2006;60:1028–34.
Dale KM, Coleman CI, Henyan NN, et al. Statins and cancer risk: a meta-analysis. JAMA. 2006;295:74–80.
Bonovas S, Filioussi K, Tsavaris N, et al. Use of statins and breast cancer: a meta-analysis of seven randomized clinical trials and nine observational studies. J Clin Oncol. 2005;23:8606–12.
Dellavalle RP, Drake A, Graber M, et al. Statins and fibrates for preventing melanoma. Cochrane Database Syst Rev. 2005;(4):CD003697.
Bjerre LM, LeLorier J. Do statins cause cancer? A meta-analysis of large randomized clinical trials. Am J Med. 2001;110:716–23.
Bonovas S, Nikolopoulos G, Sitaras NM. Statins and reduced risk of hepatocellular carcinoma in patients with hepatitis C virus infection: further evidence is warranted. J Clin Oncol. 2013;31:4160.
Bonovas S, Sitaras NM. Statins and cancer risk: a confounded association. Gastroenterology 2009;137:740.
Boudreau DM, Yu O, Johnson J. Statin use and cancer risk: a comprehensive review. Expert Opin Drug Saf. 2010;9:603–21.
Kumar AS, Campbell M, Benz CC, et al. A call for clinical trials: lipophilic statins may prove effective in treatment and prevention of particular breast cancer subtypes. J Clin Oncol. 2006;24:2127.
Prowell TM, Stearns V, Trock B. Lipophilic statins merit additional study for breast cancer chemoprevention. J Clin Oncol. 2006;24:2128–9.
Shepherd J, Blauw GJ, Murphy MB, et al. PROSPER Study Group. Prospective Study of Pravastatin in the Elderly at Risk. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet. 2002;360:1623–30.
Shepherd J, Blauw GJ, Murphy MB. The PROSPER trial. Authors’ reply. Lancet. 2003;361:428.
Hunt D, Young P, Simes J, et al. Benefits of pravastatin on cardiovascular events and mortality in older patients with coronary heart disease are equal to or exceed those seen in younger patients: results from the LIPID trial. Ann Intern Med. 2001;134:931–40.
Ford I, Murray H, Packard CJ, et al. West of Scotland Coronary Prevention Study Group. Long-term follow-up of the West of Scotland Coronary Prevention Study. N Engl J Med. 2007;357:1477–86.
Duncan RE, El-Sohemy A, Archer MC. Mevalonate promotes the growth of tumors derived from human cancer cells in vivo and stimulates proliferation in vitro with enhanced cyclin-dependent kinase-2 activity. J Biol Chem. 2004;279:33079–84.
Stone BG, Evans CD, Prigge WF, et al. Lovastatin treatment inhibits sterol synthesis and induces HMG-CoA reductase activity in mononuclear leukocytes of normal subjects. J Lipid Res. 1989;30:1943–52.
Bonovas S, Nikolopoulos G, Sitaras NM. Efficacy and safety of more intensive lowering of LDL cholesterol. Lancet. 2011;377:715.
Bonovas S, Nikolopoulos G, Sitaras NM. Commentary on pravastatin and cancer: need for individual patient data meta-analyses. Pharmacoepidemiol Drug Saf. 2010;19:203–4.
Nielsen SF, Nordestgaard BG, Bojesen SE. Statin use and reduced cancer-related mortality. N Engl J Med. 2012;367:1792–802.
Caporaso NE. Statins and cancer-related mortality—let’s work together. N Engl J Med. 2012;367:1848–50.
Osmak M. Statins and cancer: current and future prospects. Cancer Lett. 2012;324:1–12.
Jakobisiak M, Golab J. Potential antitumor effects of statins. Int J Oncol. 2003;23:1055–69.
Chan KKW, Oza AM, Siu LL. The statins as anticancer agents. Clin Cancer Res. 2003;9:10–9.
Gauthaman K, Fong CY, Bongso A. Statins, stem cells, and cancer. J Cell Biochem. 2009;106:975–83.
Cardwell CR, Hicks BM, Hughes C, et al. Statin use after colorectal cancer diagnosis and survival: a population-based cohort study. J Clin Oncol. 2014;32(28):3177–3183.
Ahern TP, Pedersen L, Tarp M, et al. Statin prescriptions and breast cancer recurrence risk: a Danish nationwide prospective cohort study. J Natl Cancer Inst. 2011;103:1461–8.
Chae YK, Valsecchi ME, Kim J, et al. Reduced risk of breast cancer recurrence in patients using ACE inhibitors, ARBs, and/or statins. Cancer Invest. 2011;29:585–93.
Kwan ML, Habel LA, Flick ED, et al. Post-diagnosis statin use and breast cancer recurrence in a prospective cohort study of early stage breast cancer survivors. Breast Cancer Res Treat. 2008;109:573–9.
Brewer TM, Masuda H, Liu DD, et al. Statin use in primary inflammatory breast cancer: a cohort study. Br J Cancer. 2013;109:318–24.
Sendur MA, Aksoy S, Yazici O, et al. Statin use may improve clinicopathological characteristics and recurrence risk of invasive breast cancer. Med Oncol. 2014;31:835.
Ahern TP, Lash TL, Damkier P, et al. Statins and breast cancer prognosis: evidence and opportunities. Lancet Oncol. 2014;15:e461–8.
Nickels S, Vrieling A, Seibold P, et al. Mortality and recurrence risk in relation to the use of lipid-lowering drugs in a prospective breast cancer patient cohort. PLoS One. 2013;8:e75088.
Yu O, Eberg M, Benayoun S, et al. Use of statins and the risk of death in patients with prostate cancer. J Clin Oncol. 2014;32:5–11.
Kawata S, Yamasaki E, Nagase T, et al. Effect of pravastatin on survival in patients with advanced hepatocellular carcinoma: a randomized controlled trial. Br J Cancer. 2001;84:886–91.
Choi SK, Min GE, Jeon SH, et al. Effects of statins on the prognosis of local and locally advanced renal cell carcinoma following nephrectomy. Mol Clin Oncol. 2013;1:365–8.
Nam DH, Lee H, Park JC, et al. Long-term statin therapy improves oncological outcome after radical gastrectomy for stage II and III gastric cancer. Anticancer Res. 2014;34:355–61.
Hawk E, Viner JL. Statins and cancer—beyond the “one drug, one disease” model. N Engl J Med. 2005;352:2238–9.
Kim K. Statin and cancer risks: from tasseomancy of epidemiologic studies to meta-analyses. J Clin Oncol. 2006;24:4796–7.
US National Institutes of Health. ClinicalTrials.gov [online]. http://www.clinicaltrials.gov. Accessed 20 Sep 2014.
Acknowledgments
No sources of funding were used in the preparation of this manuscript.
Dr. Stefanos Bonovas has no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bonovas, S. Statins: Do They Have a Potential Role in Cancer Prevention and Modifying Cancer-Related Outcomes?. Drugs 74, 1841–1848 (2014). https://doi.org/10.1007/s40265-014-0309-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-014-0309-2