Abstract
The long-acting anticholinergic agent tiotropium bromide (Spiriva®) is available as a solution for inhalation via Respimat® Soft Mist™ Inhaler in the EU and various other countries for the treatment of chronic obstructive pulmonary disease (COPD). With the Respimat® Soft Mist™ Inhaler there is improved lung deposition of drug (allowing a reduced dosage compared with tiotropium HandiHaler®), the delivered drug dose is independent of inspiratory effort and the prolonged duration of the aerosol cloud should make the co-ordination of actuation and inhalation easier. In patients with COPD, tiotropium Respimat® improved lung function, COPD exacerbations, health-related quality of life and dyspnoea and was at least as effective as tiotropium HandiHaler®. Tiotropium Respimat® was generally well tolerated in patients with COPD, with anticholinergic adverse events among the most commonly reported adverse events. In the TIOSPIR trial, tiotropium Respimat® was noninferior to tiotropium HandiHaler® in terms of all-cause mortality, and the risk of cardiovascular mortality or major adverse cardiovascular events did not significantly differ between the two treatment groups. In conclusion, tiotropium Respimat® Soft Mist™ Inhaler is a useful option for the treatment of patients with COPD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Long-acting anticholinergic agent available as a solution for inhalation administered by Respimat® Soft Mist™ Inhaler |
With Respimat® Soft Mist™ Inhaler there is improved lung deposition of drug, the delivered drug dose is independent of inspiratory effort and the prolonged duration of the aerosol cloud should make the co-ordination of actuation and inhalation easier |
Improves lung function, COPD exacerbations, health-related quality of life and dyspnoea, and is at least as effective as tiotropium HandiHaler® |
Generally well tolerated in patients with COPD |
In the TIOSPIR trial, tiotropium Respimat® was noninferior to tiotropium HandiHaler® in terms of all-cause mortality, and the risk of cardiovascular mortality and major adverse cardiovascular events did not significantly differ between tiotropium Respimat® and tiotropium HandiHaler® |
1 Introduction
Globally, chronic obstructive pulmonary disease (COPD) is a major cause of morbidity and mortality [1]. The burden posed by COPD is expected to increase as the population ages and with continued exposure to COPD risk factors [1].
COPD is characterized by chronic airflow limitation [1]. Muscarinic M1, M2 and M3 receptors are found in the human airways, with M3 receptors mediating bronchoconstriction and mucus secretion [2]. Thus, anticholinergic agents represent a rational approach to the management of COPD.
The anticholinergic agent tiotropium bromide (Spiriva®) is available in the EU and various other countries as a solution for inhalation administered via the Respimat® Soft Mist™ Inhaler [3] and as an inhalation powder administered via HandiHaler® [4] for the treatment of COPD. The use of tiotropium bromide inhalation powder administered via HandiHaler® in COPD has been reviewed previously [5]. This article reviews the clinical efficacy, tolerability and safety of tiotropium bromide solution for inhalation administered via the Respimat® Soft Mist™ Inhaler (hereafter referred to as tiotropium Respimat®) in patients with COPD, as well as summarizing the pharmacological properties of tiotropium bromide.
2 Device Characteristics and Drug Delivery
The Respimat® Soft Mist™ Inhaler is a propellant-free, multi-dose inhaler that uses mechanical power from a spring to generate a fine aerosol cloud suitable for inhalation [6, 7]. The aerosol cloud is generated from a solution, rather than a powder [6]. The majority of the aerosol particle mass is 1–5 μm in diameter, with a high proportion of the droplets in the aerosol cloud falling into the fine particle fraction (i.e. <5.8 μm in diameter) [6, 7]. The particle size and the delivered drug dose is not dependent on the patient’s inspiratory effort [7].
The aerosol cloud produced by the Respimat® Soft Mist™ Inhaler moved more slowly and had a prolonged duration compared with aerosols generated by pressurized metered-dose inhalers (pMDIs) [8]. This has the potential to reduce the extent of oropharyngeal deposition and facilitate the co-ordination of actuation and inhalation [8].
The Respimat® Soft Mist™ Inhaler deposited drug in the lungs more efficiently than a dry powder inhaler (DPI) or pMDI [9, 10]. For example, in patients with asthma, mean whole lung deposition of budesonide was significantly (p < 0.001) greater with Respimat® Soft Mist™ Inhaler than with a DPI with a fast inhaled flow rate, a DPI with a slow inhaled flow rate or a pMDI (51.6 vs. 28.5, 17.8 and 8.9 % of the metered dose); the mean percentage of the metered dose deposited in the oropharynx was 19.3 % versus 49.3, 40.5 and 82.2 %, respectively (p < 0.001 for Respimat® Soft Mist™ Inhaler vs. the other devices) [9].
Low drug deposition on the face and in the eyes is anticipated when Respimat® Soft Mist™ Inhaler is fired externally to the body [11]. Firing of Respimat® Soft Mist™ Inhaler in three positions external to the body resulted in a mean total face deposition of 7.3–9.1 % of the ex-valve dose, and mean eye deposition of 0.1–0.6 % of the ex-valve dose [11].
Although three versions of the Respimat® Soft Mist™ Inhaler were used in the tiotropium Respimat® development programme, all of the inhalers had the same nozzle type, meaning that the aerodynamic performance of the emitted aerosol was identical [12]. With the Respimat® Soft Mist™ Inhaler, ≈40 % of the inhaled tiotropium bromide dose is deposited in the lungs, with the remainder of the dose deposited in the gastrointestinal tract [3].
3 Pharmacodynamic Properties
The pharmacodynamic properties of tiotropium bromide have been reviewed previously [5]. This section provides a brief overview, with a focus on data relevant to tiotropium Respimat®.
3.1 Mechanism of Action
Tiotropium bromide is an anticholinergic agent with a quaternary ammonium structure, and is a potent, specific, long-acting muscarinic receptor antagonist [2, 13]. Tiotropium bromide binds with high affinity to muscarinic M1, M2 and M3 receptors in the human airways [2, 13, 14]. The competitive and reversible inhibition of M3 receptors by tiotropium bromide results in relaxation of the bronchial smooth muscle [15, 16].
Tiotropium bromide showed kinetic selectivity for M1 and M3 receptors over M2 receptors, with dissociation half-lives from M1 and M3 receptors of 14.6 and 34.7 h, respectively, versus a dissociation half-life of 3.6 h from M2 receptors [13, 15]. The long duration of action of tiotropium bromide was attributed to its slow dissociation from the M3 receptor [14–17], although there may be other factors that also contribute to its long duration of action [18].
Inhaled tiotropium bromide is topically selective, with bronchodilation mainly resulting from local airway effects, rather than systemic effects [3, 5].
3.2 Effects on Lung Function
Rapid improvement in lung function was seen with tiotropium Respimat® in patients with COPD [19–21]. Significant (p < 0.0001 vs. placebo) improvement in forced expiratory volume in 1 s (FEV1) was seen within 30 min of the first dose of tiotropium Respimat® in patients with COPD [3]. In addition, on day 1 of treatment, a therapeutic response (defined as an increase from baseline of ≥15 % in FEV1 within 2 h of the first dose) was seen in 64 % of tiotropium Respimat® 5 μg recipients, 72 % of tiotropium Respimat® 10 μg recipients, 57 % of tiotropium HandiHaler® 18 μg recipients and 22 % of placebo recipients [19].
Once-daily tiotropium Respimat® achieved prolonged (i.e. 24 h) bronchodilation in patients with COPD, as shown by trough FEV1 and forced vital capacity (FVC) responses [19–24]. In terms of the increase in trough FEV1, steady state was achieved during the first week of treatment in patients with COPD who received tiotropium Respimat® 5 μg once daily [20].
No correlation was seen between FEV1 responses and tiotropium bromide plasma concentrations in patients with COPD who received tiotropium Respimat® 1.25, 2.5 or 5 μg once daily [22].
Additional information regarding the short- and long-term effects of tiotropium Respimat® on lung function in patients with COPD is presented in Sect. 5.
3.3 Other Effects
It appears unlikely that inadvertent ocular exposure to tiotropium bromide would be associated with ocular adverse effects [25]. Administration of a single ocular dose of tiotropium bromide 0.02, 0.04, 0.08, 0.16, 0.28 or 0.40 μg or placebo (instilled as two drops to one eye) to 48 healthy men did not affect pupil diameter or the pupillary reflex, and was not associated with changes in intraocular pressure or accommodation [25].
It has been suggested that anti-inflammatory activity may also contribute to the beneficial effects of tiotropium bromide in COPD [26, 27]. Administration of tiotropium HandiHaler® 18 μg once daily for 1 year did not reduce markers of airway or systemic inflammation in patients with COPD in one study [28]. However, anti-inflammatory effects were observed in another study, with increased peroxisome proliferator-activated receptor-γ protein and decreased cAMP response element binding protein signalling seen ex vivo in induced sputum cells from patients with COPD following the addition of tiotropium HandiHaler® 18 μg once daily to long-acting β2-agonist therapy [29].
4 Pharmacokinetic Properties
This section reviews the pharmacokinetic properties of tiotropium bromide administered by the Respimat® Soft Mist™ Inhaler, and includes a comparison with tiotropium bromide administered by HandiHaler® [22]. The recommended tiotropium bromide dosages are 5 μg once daily via Respimat® [3] (Sect. 7), and 18 μg once daily via HandiHaler® [4].
4.1 Absorption and Distribution
Tiotropium bromide was rapidly absorbed following administration via the Respimat® Soft Mist™ Inhaler to healthy volunteers [25] and patients with COPD [22]. At steady state, the median time to the maximum plasma concentration (Cmax,ss) was 7 min in patients with COPD who received tiotropium Respimat® 5 μg once daily for 26 days [22]. A rapid decline in plasma tiotropium bromide concentrations was seen for 30 min after Cmax,ss; plasma tiotropium bromide concentrations then declined more gradually until 6 h postdose [22]. Systemic exposure to tiotropium bromide increased in a dose-proportional manner following administration of tiotropium Respimat® 1.25, 2.5 and 5.0 μg once daily for 26 days to patients with COPD [22].
In patients with COPD, systemic exposure to tiotropium bromide after administration of a 5 μg dose via Respimat® Soft Mist™ Inhaler was lower than that seen after administration of an 18 μg dose via HandiHaler® [22]. In patients receiving tiotropium Respimat® 5 μg once daily for 26 days, the geometric mean Cmax,ss was 10.5 pg/mL and the geometric mean area under the plasma concentration-time curve from time zero to 6 h at steady state (AUC6,ss) was 22.1 pg·h/mL. In patients receiving tiotropium HandiHaler® 18 μg once daily for 26 days, the geometric mean Cmax,ss was 12.9 pg/mL and the geometric mean AUC6,ss was 28.4 pg·h/mL. Thus, the geometric mean ratio for tiotropium Respimat® 5 μg versus tiotropium HandiHaler® 18 μg was 81 % (90 % CI 73–89 %) for Cmax,ss and 76 % (90 % CI 70–82 %) for AUC6,ss, meaning that bioequivalence was not established [22].
Absorption of tiotropium bromide from the gastrointestinal tract was poor and was not expected to be altered by food [3].
Tiotropium bromide was 72 % plasma protein bound, with a volume of distribution of 32 L/kg [3]. Tiotropium bromide did not penetrate the blood-brain barrier to a clinically relevant extent, according to the results of studies in rats [3].
4.2 Metabolism and Excretion
Tiotropium bromide undergoes minimal biotransformation, with 74 % of the dose excreted in the urine as unchanged drug following intravenous administration to healthy volunteers [3]. Nonenzymatic cleavage converted tiotropium bromide to inactive alcohol (N-methylscopine) and acid (dithienylglycolic acid) compounds [3]. In addition, <20 % of an intravenous dose underwent further metabolism by cytochrome P450 (CYP) 2D6 and CYP3A4 to a variety of phase II metabolites [3].
Following administration of tiotropium Respimat® to healthy volunteers, 20–29 % of the dose underwent urinary excretion, with most of the remainder of the dose being non-absorbed drug that was deposited in the gastrointestinal tract and eliminated in the faeces [3]. At steady-state, the urinary excretion of tiotropium bromide was dose-dependent in patients with COPD receiving tiotropium Respimat® 1.25–20 μg [30].
At steady state, the geometric mean amount of drug excreted in the urine from 0 to 6 h (Ae6,ss) was 387 ng following administration of tiotropium Respimat® 5 μg once daily for 26 days to patients with COPD, which was 26 % lower than the geometric mean Ae6,ss value seen following administration of tiotropium HandiHaler® 18 μg once daily for 26 days (522 ng) [22].
Total clearance of tiotropium bromide was 880 mL/min following intravenous administration to healthy volunteers [3]. Tiotropium bromide is actively secreted by the kidneys [31]. Tiotropium bromide had a terminal elimination half-life of 5–6 days following inhalation [3].
4.3 Special Patient Populations
In keeping with the renal excretion of tiotropium bromide, Cmax,ss and AUC6,ss values were slightly increased in patients with COPD and mild or moderate renal impairment, compared with patients with COPD and normal renal function, following administration of tiotropium Respimat® 5 μg once daily or tiotropium HandiHaler® 18 μg once daily, with no differences seen between the devices (analysis available as a slide presentation) [32]. The EU summary of product characteristics (SPC) states that tiotropium bromide should only be used in patients with moderate to severe renal impairment if the expected benefit outweighs the potential risk [3].
No adjustment of the tiotropium Respimat® dosage is required in the elderly or in patients with hepatic impairment [3].
4.4 Potential Drug Interactions
In vitro, tiotropium bromide did not inhibit CYP1A1, CYP1A2, CYP2B6, CYP2C9, CYP2C19, CYP2D6, CYP2E1 or CYP3A [3]. Although formal drug interaction studies have not been performed, there was no evidence of drug interactions when tiotropium bromide was coadministered with sympathomimetic bronchodilators, methylxanthines or oral or inhaled corticosteroids [3]. Coadministration of tiotropium bromide with other anticholinergic agents has not been studied and is not recommended [3].
5 Therapeutic Efficacy
5.1 Short-Term Trials
Several short-term, randomized, double-blind, multicentre trials examined the efficacy of tiotropium Respimat® in patients with COPD [19–22, 30].
Inclusion criteria included age ≥40 years; a diagnosis of COPD; a prebronchodilator FEV1 of ≤60 % predicted [19, 20], ≤70 % predicted [21], or ≥30 % and ≤65 % predicted [30]; a postbronchodilator FEV1 of <80 % predicted [22]; a FEV1:FVC ratio of ≤0.70; and a smoking history of ≥10 pack-years [19–22, 30].
A crossover, dose-ranging trial compared once-daily tiotropium Respimat® 1.25, 2.5 or 5 μg and once-daily tiotropium HandiHaler® 18 μg with placebo; each treatment period was of 4 weeks’ duration and tiotropium HandiHaler® was administered in an open-label manner [22]. In addition, a 3-week, parallel-group dose-ranging trial compared once-daily tiotropium Respimat® 1.25, 2.5, 5, 10 or 20 μg and once-daily tiotropium HandiHaler® 18 μg with placebo [30]. Two other trials of identical crossover design were reported as a prespecified pooled analysis [19]. These trials compared once-daily tiotropium Respimat® 5 or 10 μg with once-daily tiotropium HandiHaler® 18 μg or placebo; each treatment period was of 4 weeks’ duration [19]. Another trial of crossover design compared once-daily tiotropium Respimat® 5 μg with once-daily tiotropium HandiHaler® 18 μg; each treatment period was of 4 weeks’ duration [21]. Finally, two 12-week, parallel-group trials of identical design were reported as a prespecified pooled analysis; these trials compared tiotropium Respimat® 5 or 10 μg once daily with ipratropium bromide 36 μg four times daily via pMDI or placebo [20].
Stable dosages of oral or inhaled corticosteroids [19–22, 30], theophylline [20, 21, 30], mucolytics [19–22] and/or inhaled short-acting β2-agonists [21, 30] were permitted during the studies, with the use of inhaled short-acting β2-agonists [21, 30] or salbutamol (albuterol) [19, 20, 22] as rescue medication also allowed.
Across trials, the mean duration of COPD ranged from 5.8 to 10.5 years [19–22, 30], patients had a mean smoking history of 44.7–60.4 pack-years [19–22, 30] and 36–77 % of patients were ex-smokers [19, 21, 22, 30].
In most trials, the primary endpoint was the trough FEV1 response [19–21, 30]. One trial was primarily designed to examine pharmacokinetic endpoints (see Sect. 4), with lung function parameters assessed as secondary endpoints [22].
5.1.1 Comparisons with Placebo
Tiotropium Respimat® improved lung function in patients with COPD [19, 20, 22, 30].
In the crossover dose-ranging study (which included 154 patients with a mean prebronchodilator FEV1 at baseline of 1.44 L), mean trough FEV1 was significantly (p < 0.0001) greater with tiotropium Respimat® 1.25, 2.5 or 5 μg and with tiotropium HandiHaler® 18 μg than with placebo (1.432, 1.446, 1.466 and 1.473 vs. 1.345 L at week 4) [superiority testing for tiotropium Respimat® 1.25 μg vs. placebo was not predefined] [22]. The adjusted mean difference seen between tiotropium Respimat® 5 μg and tiotropium HandiHaler® 18 μg in the trough FEV1 response (−0.007 L) was not significant [22, 33].
In the parallel-group dose-ranging study (which included 202 patients with a mean prebronchodilator FEV1 at baseline of 1.31 L), mean trough FEV1 improved to a significantly (p < 0.05) greater extent with tiotropium Respimat® 5 and 20 μg than with placebo (0.15 and 0.15 vs. 0.02 L at day 21) [30]. The mean trough FEV1 response in patients receiving tiotropium Respimat® 1.25, 2.5 and 10 μg was 0.10, 0.05 and 0.13 L, respectively. Mean trough FEV1 was also improved to a significantly greater extent with tiotropium HandiHaler® 18 μg than with placebo at day 21 (0.23 vs. −0.09 L; p ≤ 0.001). Based on these results, tiotropium Respimat® doses of 5 and 10 μg were selected for further study [30].
In other trials, mean trough FEV1, area under the FEV1 time-response curve (FEV1 AUC) and peak FEV1 improved to a significantly greater extent with tiotropium Respimat® 5 and 10 μg than with placebo at day 29 [19] or week 12 [20] (Table 1). Tiotropium HandiHaler® 18 μg was also significantly more effective than placebo at day 29 (Table 1) [19].
Trough FVC [19, 20], FVC AUC [19] and peak FVC [19] also improved to a significantly (p < 0.01) greater extent with tiotropium Respimat® 5 and 10 μg than with placebo at day 29 [19] or week 12 [20]. At day 29, the mean difference between tiotropium Respimat® 5 or 10 μg and placebo in trough FVC was 0.232 and 0.263 L, respectively, in FVC AUC from 0 to 12 h (FVC AUC12) was 0.359 and 0.369 L, respectively, and in peak FVC was 0.405 and 0.410 L, respectively [19]. At week 12, the mean difference between tiotropium Respimat® 5 or 10 μg and placebo in trough FVC was 0.132 and 0.180 L, respectively [20].
In addition, morning and evening peak expiratory flow rate (PEFR) increased to a significantly (p < 0.0001) greater extent with tiotropium Respimat® 5 or 10 μg than with placebo at day 29 [19] or week 12 [20]. At day 29, the mean difference between tiotropium Respimat® 5 or 10 μg recipients and placebo recipients in weekly morning PEFR was 19.8 and 21.5 L/min, respectively, and in weekly evening PEFR was 23.7 and 24.1 L/min, respectively [19]. At week 12, the mean difference between tiotropium Respimat® 5 or 10 μg recipients and placebo recipients in morning PEFR was 25 and 23 L/min, respectively, and in evening PEFR was 32 and 29 L/min, respectively [20].
Rescue medication use was significantly (p < 0.01) reduced with tiotropium Respimat® 5 and 10 μg versus placebo [19, 20]. For example, at day 29, the mean difference between tiotropium Respimat® 5 or 10 μg recipients and placebo recipients in the number of occasions in a 24-h period in which rescue medication was used was −1.1 and −1.1, respectively [19]. There was no evidence of a rebound effect following the cessation of treatment with tiotropium Respimat® 5 or 10 μg [20].
5.1.2 Comparisons with Tiotropium HandiHaler®
In terms of the improvement in mean trough FEV1, tiotropium Respimat® 5 μg [19, 21] and 10 μg [19] was noninferior to tiotropium HandiHaler® 18 μg (Table 1).
Compared with patients receiving tiotropium HandiHaler® 18 μg, patients receiving tiotropium Respimat® 5 or 10 μg had significantly greater improvements in mean FEV1 AUC12 (between-group differences of 0.031 and 0.028 L) and peak FEV1 (between-group differences of 0.030 and 0.034 L) at day 29 in a pooled analysis [19] (Table 1). No significant difference was seen between tiotropium Respimat® 5 μg and tiotropium HandiHaler® 18 μg in terms of the improvement in mean FEV1 AUC from 0 to 3 h (FEV AUC3) and peak FEV1 in another study [21] (Table 1).
Improvements in mean trough FVC, FVC AUC and peak FVC did not significantly differ between tiotropium Respimat® 5 or 10 μg and tiotropium HandiHaler® 18 μg recipients at day 29 [19, 21]. In the pooled analysis, the mean difference between tiotropium Respimat® 5 or 10 μg and tiotropium HandiHaler® in trough FVC was 0.022 and 0.053 L, respectively, in FVC AUC12 was 0.021 and 0.031 L, respectively, and in peak FVC was 0.010 and 0.016 L, respectively [19]. In the other study, the mean difference between tiotropium Respimat® 5 μg and tiotropium HandiHaler® in trough FVC, FVC AUC3 and peak FVC was −0.004, 0.013 and 0.010 L, respectively [21].
The mean difference between tiotropium Respimat® 10 μg and tiotropium HandiHaler® 18 μg in the improvement in weekly morning PEFR (4.7 L/min) and evening PEFR (4.5 L/min) was significant (p < 0.05), with no significant difference seen between tiotropium Respimat® 5 μg and tiotropium HandiHaler® 18 μg in either endpoint [19].
Changes in 24-h rescue medication use did not significantly differ between tiotropium Respimat® 5 or 10 μg recipients and tiotropium HandiHaler® recipients [19].
5.1.3 Comparison with Ipratropium Bromide
Mean trough FEV1 improved to a significantly greater extent with tiotropium Respimat® 5 or 10 μg than with ipratropium bromide pMDI at week 12 (Table 1) [20]. Changes in mean FEV1 AUC from 0 to 6 h and peak FEV1 did not significantly differ between patients receiving tiotropium Respimat® 5 or 10 μg and those receiving ipratropium bromide pMDI (Table 1) [20].
At week 12, the mean difference between tiotropium Respimat® 10 μg recipients and ipratropium bromide pMDI recipients in the improvement in trough FVC was significant (0.125 L; p < 0.01), with no significant difference between tiotropium Respimat® 5 μg and ipratropium bromide pMDI (mean 0.077 L) [20].
Morning and evening PEFR increased to a significantly (p < 0.001) greater extent with tiotropium Respimat® 5 and 10 μg than with ipratropium bromide pMDI [20]. At week 12, the mean difference between tiotropium Respimat® 5 or 10 μg recipients and ipratropium bromide pMDI recipients in morning PEFR was 24 and 21 L/min, respectively, and in evening PEFR was 22 and 19 L/min, respectively [20].
5.2 Longer-Term Trials
5.2.1 Comparisons with Placebo
Three randomized, double-blind, multinational, 1-year trials compared once-daily tiotropium Respimat® 5 μg [23, 24] or 10 μg [23] with placebo in patients with COPD. Two of these trials, which were of identical design, were reported as a prespecified pooled analysis [23]. Inclusion criteria included age ≥40 years, a diagnosis of COPD, a prebronchodilator FEV1 of ≤60 % predicted, a FEV1:FVC ratio of ≤0.70 and a smoking history of ≥10 pack-years [23, 24].
During the studies, stable dosages of oral or inhaled corticosteroids, theophylline, mucolytics or antileukotrienes [23] or all respiratory medications other than inhaled anticholinergics [24] were permitted, with salbutamol used as a rescue medication [23, 24]. In terms of patient characteristics at baseline, the mean duration of COPD was ≈9 years [23] and ≈8 years [24], patients had a mean smoking history of ≈46 pack-years [24] and ≈36 % of patients were current smokers [23, 24].
Primary endpoints included trough FEV1 response [23, 24], time to first COPD exacerbation [24], the number of COPD exacerbations per patient-year [23], the change in the St George’s Respiratory Questionnaire (SGRQ) total score [23] and the change in the Mahler Transition Dyspnoea Index (TDI) focal score [23].
Tiotropium Respimat® improved lung function, COPD exacerbations, health-related quality of life (HR-QOL) and dyspnoea, according to the results of the 1-year trials [23, 24].
At week 48, the improvement from baseline in trough FEV1 was significantly greater with tiotropium Respimat® 5 or 10 μg than with placebo (Table 2) [23, 24]. There was no evidence of tachyphylaxis, in that the improvement in trough FEV1 seen at week 48 was similar to that seen on day 1 [23].
Mean trough FVC also improved from baseline to a significantly (p < 0.0001) greater extent with tiotropium Respimat® 5 or 10 μg than with placebo [23, 24]. At week 48, the mean difference between tiotropium Respimat® 5 μg and placebo was 0.168 L in one study [24], and the mean difference between tiotropium Respimat® 5 or 10 μg and placebo was 0.209 and 0.286 L, respectively, in the pooled analysis [23].
The time to the first COPD exacerbation was significantly longer in patients receiving tiotropium Respimat® 5 or 10 μg than in those receiving placebo (Table 2) [23, 24]. In addition, the number of COPD exacerbations per patient-year was significantly smaller with tiotropium Respimat® 5 or 10 μg than with placebo (Table 2). At least one COPD exacerbation was experienced by significantly fewer recipients of tiotropium Respimat® 5 or 10 μg than placebo (Table 2) [23, 24].
The mean number of COPD exacerbations requiring hospitalization was significantly lower with tiotropium Respimat® 5 μg than placebo in one study (0.12 vs. 0.15 per patient-year; p < 0.005) [24], with no significant difference seen between tiotropium Respimat® 5 or 10 μg and placebo in the pooled analysis (0.12 and 0.16 vs. 0.20 per patient-year) [23].
In terms of HR-QOL, the SGRQ total score improved from baseline to week 48 to a significantly greater extent with tiotropium Respimat® 5 or 10 μg than with placebo (Table 2) [23, 24]. In addition, an improvement in the SGRQ total score exceeding the minimal clinically important difference (i.e. ≥4 units) was seen in significantly (p < 0.0001) more tiotropium Respimat® 5 μg than placebo recipients in one study (49.5 vs. 41.4 %) [24] and in significantly (p < 0.05) more tiotropium Respimat® 5 or 10 μg than placebo recipients in the pooled analysis (50.5 and 51.4 vs. 40.7 %) [23].
The Mahler TDI focal score improved from baseline to week 48 to a significantly greater extent with tiotropium Respimat® 5 or 10 μg than with placebo (Table 2) [23]. Significantly (p < 0.0001) more recipients of tiotropium Respimat® 5 or 10 μg than placebo had an improvement in the Mahler TDI focal score exceeding the minimal clinically important difference (i.e. ≥1 unit) [56 and 56 vs. 44 %] [23].
The mean number of occasions per day on which rescue medication was used was reduced to a significantly (p < 0.0001) greater extent with tiotropium Respimat® 5 or 10 μg than with placebo (−0.6 and −0.7 vs. −0.1) [23].
A subgroup analysis of one of these trials [24] was conducted in Chinese patients who received tiotropium Respimat® 5 μg (n = 167) or placebo (n = 171) [34]. In this subgroup analysis, mean trough FEV1 improved to a significantly (p < 0.0001) greater extent with tiotropium Respimat® 5 μg than with placebo (adjusted mean between-group difference of 0.109, 0.119 and 0.134 at weeks 4, 24 and 48, respectively). Mean trough FVC also improved to a significantly (p < 0.0001) greater extent with tiotropium Respimat® 5 μg than with placebo (adjusted mean between-group difference of 0.207, 0.222 and 0.236 at weeks 4, 24 and 48, respectively) [34].
Compared with placebo, tiotropium Respimat® 5 μg significantly (p = 0.0004) delayed the time to first exacerbation [hazard ratio (HR) 0.54; 95 % CI 0.38–0.76] and tiotropium Respimat® 5 μg recipients were significantly (p = 0.0076) less likely than placebo recipients to experience a COPD exacerbation (34.7 vs. 48.5 %) [odds ratio (OR) 0.55; 95 % CI 0.35–0.85] [34].
5.2.2 Comparison with Tiotropium HandiHaler®: the TIOSPIR Trial
TIOSPIR (Tiotropium Safety and Performance in Respimat) was a large (n = 17,135), randomized, double-blind, multinational trial designed to compare the safety and efficacy of tiotropium Respimat® with that of tiotropium HandiHaler® in patients with COPD [35]. Baseline patient characteristics and key inclusion and exclusion criteria are shown in Table 3 [35].
In TIOSPIR, patients were randomized to receive once-daily tiotropium Respimat® 2.5 or 5 μg or tiotropium HandiHaler® 18 μg [35]. All other COPD medications apart from other inhaled anticholinergics were permitted. The mean duration of follow-up was 2.3 years, with a median treatment duration of 835 days [35].
The primary safety outcome (time to death from any cause) is discussed in Sect. 6.2.2 and the primary efficacy outcome was the risk of the first COPD exacerbation [35]. Primary endpoints were tested using a hierarchical analysis plan (Table 3) [35].
The risk of the first COPD exacerbation did not significantly differ between patients receiving tiotropium Respimat® 5 μg and those receiving tiotropium HandiHaler® 18 μg (Table 4), with a median time to first COPD exacerbation of 756 and 719 days in the corresponding treatment groups [35]. In addition, no significant difference was seen between tiotropium Respimat® 2.5 μg recipients and tiotropium HandiHaler® 18 μg recipients in the risk of the first COPD exacerbation (Table 4) [35].
The incidence of moderate or severe COPD exacerbations did not significantly differ between tiotropium Respimat® 5 μg recipients and tiotropium HandiHaler® 18 μg recipients (47.2 vs. 48.0 % of patients) [HR 0.98; 95 % CI 0.93–1.04], or between tiotropium Respimat® 2.5 μg recipients and tiotropium HandiHaler® 18 μg recipients (48.4 vs. 48.0 %) [HR 1.01; 95 % CI 0.96–1.07], with an adjusted event rate of 0.58 per patient-year in all three treatment groups [35].
In addition, the incidence of severe COPD exacerbations did not significantly differ between tiotropium Respimat® 5 μg recipients and tiotropium HandiHaler® 18 μg recipients (14.5 vs. 14.3 %) [HR 1.02; 95 % CI 0.93–1.13], or between tiotropium Respimat® 2.5 μg recipients and tiotropium HandiHaler® 18 μg recipients (15.2 vs. 14.3 %) [HR 1.07; 95 % CI 0.97–1.18] [35]. The adjusted event rate was 0.12 per patient-year in tiotropium Respimat® 2.5 or 5 μg recipients and 0.11 per patient-year in tiotropium HandiHaler® recipients [35].
Lung function was examined in a spirometry substudy including 1,370 patients [33, 35]. The adjusted mean trough FEV1 (average for weeks 24–120) was 1.258 L in tiotropium Respimat® 2.5 μg recipients, 1.285 L in tiotropium Respimat® 5 μg recipients and 1.295 L in tiotropium HandiHaler® 18 μg recipients. Tiotropium Respimat® 5 μg was noninferior to tiotropium HandiHaler® (between-group difference of −0.01 L; 95 % CI −0.038 to 0.018) [noninferiority margin of −0.05 L], but noninferiority was not shown between tiotropium Respimat® 2.5 μg and tiotropium HandiHaler® (between-group difference of −0.037 L; 95 % CI −0.065 to −0.009) [33, 35].
5.3 Clinical Practice Study
A German, multicentre, observational study examined the efficacy of tiotropium Respimat® in 1,230 patients with COPD in a real-life setting [36]. Patients received tiotropium Respimat® 5 μg once daily for 6 weeks. The mean duration of COPD was 7.5 years and 35 % of patients were current smokers. In terms of co-morbidities, 44 % of patients had cardiac disease, 22 % had vascular disorders, 19 % had metabolic or endocrine disorders and 12 % had additional pulmonary disorders [36]. The primary endpoint was ‘therapeutic success’, defined as an improvement in the physical function domain (PF-10) of the Short Form-36 questionnaire of ≥10 points from baseline to week 6; PF-10 scores ranged from 0 to 100 [36].
The therapeutic success rate was 61.5 %, and the mean PF-10 score significantly (p < 0.001) improved from 49.0 points at baseline to 62.3 points at week 6. At week 6, 76.9 % of patients were ‘satisfied’ or ‘very satisfied’ with tiotropium Respimat® Soft Mist™ Inhaler [36].
6 Tolerability and Safety
6.1 General Tolerability Profile
Tiotropium Respimat® was generally well tolerated in patients with COPD. The tolerability profile of tiotropium bromide administered via Respimat® Soft Mist™ Inhaler was generally similar to that of tiotropium bromide administered via HandiHaler® [19, 21, 30].
As expected, anticholinergic adverse events were among the most commonly reported adverse events in patients receiving inhaled tiotropium bromide [19–21, 23, 24, 30]. For example, the dry mouth incidence rate was 3.41 per 100 patient-years with tiotropium Respimat® 5 μg and 1.54 per 100 patient-years with placebo in a 1-year trial [rate ratio (RR) 2.21; 95 % CI 1.41–3.49] [24]. In addition, among patients receiving tiotropium Respimat® 5 or 10 μg or placebo in a pooled analysis of two 1-year trials, dry mouth was reported in 7.2, 14.5 and 2.1 % of patients, respectively, constipation was reported in 2.1, 2.2 and 1.5 %, respectively, and urinary tract infection was reported in 2.5, 4.2 and 1.1 %, respectively [23]. Dry mouth was also reported in 8.3 % of tiotropium Respimat® 5 μg recipients, 10.0 % of tiotropium Respimat® 10 μg recipients, 3.9 % of ipratropium bromide pMDI recipients and 2.2 % of placebo recipients in a pooled analysis of two 12-week trials [20].
Other commonly reported adverse events in patients receiving tiotropium Respimat®, tiotropium HandiHaler®, ipratropium bromide pMDI or placebo include COPD exacerbations [19–21, 23, 24, 30], nasopharyngitis [19, 21, 24] and dyspnoea [19, 20, 24]. COPD exacerbations (incidence rate 44.1 vs. 56.8 per 100 patient-years) [RR 0.78; 95 % CI 0.70–0.86] and bronchitis (incidence rate 3.79 vs. 5.52 per 100 patient-years) [RR 0.69; 95 % CI 0.50–0.94] occurred in significantly fewer tiotropium Respimat® 5 μg than placebo recipients in the 1-year trial [24].
There were no reports of paradoxical bronchospasm occurring after inhalation among patients receiving tiotropium Respimat® 5 or 10 μg or placebo, according to a retrospective analysis [37] of the pooled 1-year trials [23]. The incidence of paradoxical bronchoconstriction appeared low, with at least two events suggestive of bronchoconstriction (rescue medication use, administration-related bronchoconstriction indicators, asymptomatic fall in FEV1 of ≥15 % from test-day prebronchodilator value) occurring in 0.3 % of tiotropium Respimat® 5 μg recipients, 0.4 % of tiotropium Respimat® 10 μg recipients and 0.2 % of placebo recipients, with either rescue medication use or administration-related bronchoconstriction indicators (but not both) occurring in 1.2, 0.7 and 1.2 % of patients in the corresponding treatment groups [37].
In 1-year trials, discontinuation because of adverse events occurred in 10, 11.8 and 18.7 % of patients receiving tiotropium Respimat® 5 or 10 μg and placebo, respectively [23], and in 7.2 and 7.8 % of patients receiving tiotropium Respimat® 5 μg and placebo, respectively [24].
The risk of adverse events, serious adverse events or fatal adverse events was not increased in patients with mild renal impairment (n = 3,018) or moderate renal impairment (n = 1,322) who received tiotropium Respimat® 5 μg versus placebo, according to a pooled analysis (available as an abstract and poster) of seven trials [38].
In shorter-term trials, no clinically relevant changes in vital signs [19–21, 30], ECG recordings [20, 21, 30], physical examination findings [20] or laboratory values [19, 21, 30] were seen in tiotropium Respimat® recipients. In addition, no clinically relevant differences were seen between tiotropium Respimat® and placebo recipients in terms of vital signs [24], ECG recordings [23, 24], Holter monitoring [23] or physical examination findings [24] in 1-year trials. A combined analysis (available as an abstract and poster) of four trials in which patients with COPD (n = 727) underwent Holter ECG monitoring found that maintenance therapy with tiotropium Respimat® 1.25–10 μg or tiotropium HandiHaler® 18 μg was not associated with changes in heart rate, pauses (i.e. absence of a heart beat for >3 s), supraventricular premature beats or ventricular premature beats, when compared with placebo or the pretreatment baseline period [39].
6.2 Mortality and Cardiovascular Adverse Events
6.2.1 One-Year Trials
In 1-year trials, all-cause mortality did not significantly differ between tiotropium Respimat® 5 μg and placebo recipients, with an incidence rate of 2.94 versus 2.13 events per 100 patient-years (RR 1.38; 95 % CI 0.91–2.10) in one trial [24] and a frequency during treatment plus the 30-day observation period of 1.79 versus 0.77 % in the pooled analysis of two other trials [23]. However, in the pooled analysis, all-cause mortality during treatment plus the 30-day observation period was significantly higher with tiotropium Respimat® 10 μg than with placebo (2.55 vs. 0.77 %; p = 0.0161) [23]. When the 409 patients who discontinued treatment prematurely were included in the pooled analysis, the between-group difference in all-cause mortality between tiotropium Respimat® 10 μg and placebo recipients was no longer significant; all-cause mortality was 2.39 % in tiotropium Respimat® 5 μg recipients, 2.70 % in tiotropium Respimat® 10 μg recipients and 1.53 % in placebo recipients. Mean exposure to treatment was 304.7, 297.2 and 265.6 days in the corresponding treatment groups [23].
In the pooled analysis, angina pectoris occurred in 0.4 % of tiotropium Respimat® 5 μg recipients, 1.0 % of tiotropium Respimat® 10 μg recipients and 0.2 % of placebo recipients, with myocardial infarction (MI) occurring in 0.3, 0.1 and 0.9 % of patients in the corresponding treatment groups [23].
In the other trial, fatal cardiac disorders occurred in tiotropium Respimat® 5 μg and placebo recipients with an incidence rate of 0.51 and 0.22 per 100 patient-years (RR 2.27; 95 % CI 0.70–7.37) [24]. Post hoc analysis found no significant difference between tiotropium Respimat® 5 μg and placebo recipients in terms of a composite cardiovascular endpoint (incidence rate 1.77 vs. 1.58 per 100 patient-years) [RR 1.12; 95 % CI 0.67–1.86]; the composite cardiovascular endpoint comprised fatal and nonfatal MI and stroke, fatal events in the organ classes cardiac disorders and vascular disorders, and the terms sudden death, cardiac death and sudden cardiac death [24].
6.2.2 The TIOSPIR Trial
In the TIOSPIR trial, tiotropium Respimat® 5 and 2.5 μg were noninferior to tiotropium HandiHaler® 18 μg in terms of the risk of death from any cause (Table 4) [35].
The risk of death from a cardiovascular cause did not significantly differ between patients receiving tiotropium Respimat® 5 μg and those receiving tiotropium HandiHaler® 18 μg (2.0 vs. 1.8 %) [HR 1.11; 95 % CI 0.85–1.45] or between patients receiving tiotropium Respimat® 2.5 μg and those receiving tiotropium HandiHaler® 18 μg (2.1 vs. 1.8 %) [HR 1.17; 95 % CI 0.90–1.53] [35].
In patients receiving tiotropium Respimat® 2.5 μg, tiotropium Respimat® 5 μg and tiotropium HandiHaler® 18 μg, death from MI occurred in 0.2, 0.2 and 0.1 % of patients, respectively, sudden death occurred in 1.4, 1.2 and 1.2 %, respectively, death from stroke occurred in 0.2, 0.2 and 0.2 %, respectively, and death from other cardiovascular causes occurred in 0.3, 0.4 and 0.3 %, respectively [35].
Among the 1,825 patients with a history of cardiac arrhythmias, mortality did not significantly differ between patients receiving tiotropium Respimat® 5 μg and those receiving tiotropium HandiHaler® 18 μg (10.6 vs. 12.9 %) [HR 0.81; 95 % CI 0.58–1.12] or between patients receiving tiotropium Respimat® 2.5 μg and those receiving tiotropium HandiHaler® 18 μg (13.1 vs. 12.9 %) [HR 1.02; 95 % CI 0.74–1.39] [35]. Subgroup analysis in patients with a history of cardiac disorders indicated that mortality did not significantly differ between patients receiving tiotropium Respimat® 5 μg and those receiving tiotropium HandiHaler® 18 μg (10.6 vs. 11.2 %) [HR 0.94; 95 % CI 0.76–1.17] or between patients receiving tiotropium Respimat® 2.5 μg and those receiving tiotropium HandiHaler® 18 μg (11.2 vs. 11.2 %) [HR 1.00; 95 % CI 0.81–1.24]. It should be noted that patients with unstable cardiovascular conditions were excluded from TIOSPIR (see also Sect. 8) [35].
There was no significant difference between patients receiving tiotropium Respimat® 5 μg and those receiving tiotropium HandiHaler® 18 μg in the incidence of major adverse cardiovascular events (3.9 vs. 3.6 %) [HR 1.10; 95 % CI 0.91–1.33], stroke (0.9 vs. 1.0 %) [HR 0.91; 95 % CI 0.63–1.33], transient ischaemic attack (0.5 vs. 0.4 %) [HR 1.50; 95 % CI 0.85–2.65] or MI (1.3 vs. 0.9 %) [HR 1.41; 95 % CI 0.98–2.00] [35]. Similarly, there was no significant difference between patients receiving tiotropium Respimat® 2.5 μg and those receiving tiotropium HandiHaler® 18 μg in the incidence of major adverse cardiovascular events (3.9 vs. 3.6 %) [HR 1.11; 95 % CI 0.91–1.34], stroke (1.0 vs. 1.0 %) [HR 0.98; 95 % CI 0.68–1.41], transient ischaemic attack (0.4 vs. 0.4 %) [HR 1.24; 95 % CI 0.69–2.24] or MI (1.2 vs. 0.9 %) [HR 1.34; 95 % CI 0.94–1.92] [35].
In patients receiving tiotropium Respimat® 2.5 μg, tiotropium Respimat® 5 μg or tiotropium HandiHaler® 18 μg, serious adverse events were reported in 33.8, 32.4 and 32.4 % of patients, respectively; serious respiratory, thoracic or mediastinal disorders were reported in 17.8, 16.8 and 17.0 %, respectively; serious infections or infestations were reported in 8.7, 8.8 and 8.7 %, respectively; and serious cardiac disorders were reported in 5.1, 4.8 and 4.7 %, respectively [35]. Cardiac arrhythmia was reported in 2.3 % of tiotropium Respimat® 2.5 μg recipients, 2.1 % of tiotropium Respimat® 5 μg recipients and 2.1 % of tiotropium HandiHaler® 18 μg recipients [35].
7 Dosage and Administration
Tiotropium Respimat® is approved in the EU as a maintenance bronchodilator treatment to relieve symptoms in patients with COPD [3]. The recommended dosage of tiotropium Respimat® is 5 μg, administered as two puffs once daily, at the same time each day [3].
Local prescribing information should be consulted for contraindications, special warnings and precautions for use relating to tiotropium Respimat®, as well as for instructions relating to the use and handling of the tiotropium Respimat® inhaler and cartridge.
8 Place of Tiotropium Respimat® Soft Mist™ Inhaler in the Management of Chronic Obstructive Pulmonary Disease
Bronchodilators are central to the symptomatic management of COPD, with long-acting bronchodilators generally preferred over short-acting bronchodilators and inhaled therapy generally preferred over oral therapy [1]. Inhaled long-acting bronchodilators include the anticholinergics tiotropium bromide, aclidinium bromide and glycopyrrolate and the β2-agonists salmeterol, formoterol, arformoterol and indacaterol [1].
Long-acting anticholinergics or long-acting β2-agonists are recommended first-line options in Global Initiative for Chronic Obstructive Lung Disease (GOLD) group B patients, with long-acting anticholinergics or combination therapy with an inhaled corticosteroid plus a long-acting β2-agonist recommended as first-line options in GOLD group C patients, and an inhaled corticosteroid plus a long-acting β2-agonist and/or a long-acting anticholinergic recommended as first-line options in GOLD group D patients [1].
There is a large body of data supporting the efficacy of tiotropium bromide administered via HandiHaler® in patients with COPD [5]. Clinical trials have also demonstrated the efficacy of tiotropium bromide administered via Respimat® Soft Mist™ Inhaler in patients with COPD, with improvements seen in lung function, COPD exacerbations, HR-QOL and dyspnoea (Sect. 5). In these trials, tiotropium Respimat® was shown to be at least as effective as tiotropium HandiHaler®. Tiotropium Respimat® 10 μg did not offer an efficacy advantage over tiotropium Respimat® 5 μg (Sect. 5) and was associated with a numerically higher incidence of anticholinergic adverse events (Sect. 6.1), leading to tiotropium Respimat® 5 μg once daily being the recommended dosage (Sect. 7). Tiotropium Respimat® Soft Mist™ Inhaler is available in the EU and various other countries, and the FDA recently approved tiotropium Respimat® in the US for use in the maintenance treatment of COPD [40]. In clinical practice, inhaled tiotropium bromide has an estimated 40,049 million patient-years of use, with 37,543 million patient-years of use attributable to tiotropium HandiHaler® and 2,506 million patient-years of use attributable to tiotropium Respimat® [41].
The safety of inhaled tiotropium bromide has been a matter of debate in recent times [42]. Concerns over its safety were initially prompted by results of a pooled analysis [43] and a meta-analysis [44] that signalled possible increases in the risk of stroke and/or cardiovascular risk in patients receiving inhaled tiotropium bromide [43] or inhaled anticholinergics [44]. These analyses were conducted prior to the publication of the large, well-designed, 4-year UPLIFT (Understanding Potential Long-Term Impacts on Function with Tiotropium) trial, which revealed no increase in stroke and a reduced risk of on-treatment mortality and serious cardiac adverse events in patients receiving tiotropium HandiHaler® versus placebo [45]. Thus, concerns regarding tiotropium HandiHaler® were allayed by the findings of UPLIFT [46], and subsequent results of a meta-analysis [47] and pooled analyses [48, 49] that included the UPLIFT trial did not show an increased risk of mortality, cardiovascular mortality and/or major cardiovascular events.
However, concerns persisted over the safety of tiotropium bromide solution for inhalation administered via Respimat® Soft Mist™ Inhaler. Numerical mortality imbalances between tiotropium Respimat® and placebo were seen in 1-year trials (Sect. 6.2.1); these imbalances appeared to occur in patients with cardiovascular disease, particularly a history of arrhythmias [50]. Prior to the publication of the TIOSPIR trial, results of meta-analyses [51, 52], a systematic review [53] and a database study [54] also suggested an increased risk of mortality with tiotropium Respimat®. However, these meta-analyses have been the subject of various criticisms [50, 55–57], including the way in which data was selected and used [50, 55, 56]. Similarly, the methodology of the database study has been criticized [57].
The results of the TIOSPIR trial can be considered more robust than results of meta-analyses or database studies [57]. TIOSPIR demonstrated that tiotropium Respimat® was noninferior to tiotropium HandiHaler® in terms of all-cause mortality and that the risk of cardiovascular mortality or major adverse cardiovascular events did not significantly differ between the two treatment groups (Sect. 6.2.2). A numerical imbalance was seen in TIOSPIR between tiotropium Respimat® and tiotropium HandiHaler® recipients in terms of the number of fatal MIs (Sect. 6.2.2), although the numbers were small [35]. The European Medicines Agency requested additional analysis of the TIOSPIR data in patients with cardiac disorders at baseline to explore if the risk of fatal MI is particularly increased in these subgroups [58]. Further analysis revealed no increased risk of all-cause mortality or fatal cardiac events in the subgroup of patients with cardiac disorders at baseline, and it was concluded that the apparent higher risk of fatal MI seen with tiotropium Respimat® in TIOSPIR most likely reflected variability of rare events [59].
Approximately 10 % of patients in TIOSPIR had prior cardiac arrhythmias and approximately 20 % had prior MI, ischaemic heart disease or coronary artery disease (Table 3) [35]. In TIOSPIR, subgroup analysis in patients with a history of stable cardiac disorders, including stable cardiac arrhythmias, demonstrated no significant difference between tiotropium Respimat® recipients and tiotropium HandiHaler® recipients in the risk of all-cause mortality (Sect. 6.2.2). The current EU SPC recommends that tiotropium Respimat® be used with caution in patients with known cardiac rhythm disorders [3].
It should be noted that TIOSPIR excluded patients with unstable cardiovascular conditions (e.g. MI within the previous 6 months, hospitalization for New York Heart Association class III or IV heart failure in the previous year, or any unstable or life-threatening cardiac arrhythmia requiring new treatment in the previous year) [Table 3], meaning that its findings cannot be extended to these patient groups [35].
TIOSPIR also excluded patients with moderate to severe renal impairment [35]. Tiotropium is excreted renally (Sect. 4.2) and the EU SPC for both tiotropium HandiHaler® [4] and tiotropium Respimat® [3] recommends administration in patients with moderate to severe renal impairment only if the expected benefit outweighs the potential risk. A recent pooled analysis indicated that the risk of adverse events, serious adverse events or fatal adverse events was not increased in patients with mild or moderate renal impairment who received tiotropium Respimat® (Sect. 6.1). Further studies regarding the safety of tiotropium Respimat® in patients with renal impairment would be of interest [60].
A recent pooled analysis (available as an abstract) of randomized, double-blind, placebo-controlled trials did not indicate an increased risk of fatal adverse events or fatal or nonfatal major adverse cardiovascular events with tiotropium HandiHaler® or Respimat® versus placebo [61]. In addition, survival and the risk of exacerbation did not significantly differ between patients with COPD receiving tiotropium Respimat® 5 μg and those receiving tiotropium HandiHaler® 18 μg, according to a post hoc, mixed treatment analysis of clinical trial data (available as an abstract and poster) [62]. Survival did not significantly differ between tiotropium Respimat® 5 μg recipients and placebo recipients or between tiotropium HandiHaler® 18 μg and placebo recipients, although the risk of exacerbation was significantly lower with tiotropium Respimat® 5 μg than with placebo (OR 0.79; 95 % CI 0.70–0.88) and with tiotropium HandiHaler® 18 μg than with placebo (OR 0.87; 95 % CI 0.78–0.98) [62].
An important consideration when selecting a treatment option in COPD is that the response to treatment may be affected by factors such as inhaler technique and patient adherence [20, 63]. The dose of tiotropium bromide delivered via Respimat® Soft Mist™ Inhaler is independent of inspiratory effort (Sect. 2). In addition, the prolonged duration of the aerosol cloud (Sect. 2) should make it easier for patients to co-ordinate actuation and inhalation [64, 65].
The improved lung deposition of drug seen with the Respimat® Soft Mist™ Inhaler (Sect. 2) allows a lower nominal tiotropium bromide dose with this inhaler than with HandiHaler®. Previously, it has been suggested that systemic exposure to tiotropium bromide may be greater with Respimat® Soft Mist™ Inhaler than with HandiHaler®, and that this may result in differential toxicity with Respimat® versus HandiHaler® [51, 66]. However, results of a recent bioequivalence study demonstrated lower systemic exposure with tiotropium Respimat® 5 μg than with tiotropium HandiHaler® 18 μg (Sect. 4) and, as previously discussed, tiotropium Respimat® 5 μg and tiotropium HandiHaler® 18 μg had similar safety profiles in TIOSPIR. A study in 34 patients with COPD examined the ease of switching from tiotropium HandiHaler® 18 μg to tiotropium Respimat® 5 μg [67]. Both devices were considered easy to use, although 21 patients reported that tiotropium Respimat® was easier or much easier than tiotropium HandiHaler® in terms of usability [67].
Case reports [68–70] have suggested that ocular adverse effects may occur after the inadvertent administration of inhaled anticholinergics to the eyes. However, no ocular adverse effects were seen when tiotropium bromide drops were instilled into the eyes of healthy volunteers (Sect. 3.3); the tiotropium bromide doses used in this study were much higher than the dose that could potentially enter the eye after misuse of Respimat® Soft Mist™ Inhaler [25]. Moreover, low facial/ocular deposition was seen after misuse of Respimat® Soft Mist™ Inhaler (Sect. 2).
A fixed-dose combination of tiotropium bromide and the novel long-acting β2-agonist olodaterol administered via Respimat® Soft Mist™ Inhaler is currently under development for use in COPD [71, 72]. In the randomized, double-blind, phase III, VIVACITO trial (available as a poster) in patients with COPD (n = 219), the adjusted mean FEV1 AUC from 0 to 24 h, FEV1 AUC12 and FEV1 AUC from 12 to 24 h significantly (p < 0.0001) favoured tiotropium Respimat®/olodaterol Respimat® 2.5/5 μg or 5/5 μg versus tiotropium Respimat® alone or olodaterol Respimat® alone after 6 weeks’ therapy [73]. In addition, results of the two randomized, double-blind, multinational, 52-week, TONADO 1 and 2 trials (available as an abstract and poster) in patients with COPD (n = 5,162) found that lung function was improved to significantly (p < 0.001) greater extent with tiotropium Respimat®/olodaterol Respimat® than with tiotropium Respimat® or olodaterol Respimat® alone [74, 75].
Studies examining the use of tiotropium Respimat® in combination with other novel long-acting β2-agonists (e.g. vilanterol and indacaterol) and comparing tiotropium Respimat® with other long-acting anticholinergics such as aclidinium bromide and glycopyrrolate would also be of interest [76].
In conclusion, the long-acting anticholinergic agent tiotropium bromide is available as a solution for inhalation administered by Respimat® Soft Mist™ Inhaler for the treatment of COPD. With the Respimat® Soft Mist™ Inhaler, there is improved lung deposition of drug, the delivered drug dose is independent of inspiratory effort and the prolonged duration of the aerosol cloud should make the co-ordination of actuation and inhalation easier. In patients with COPD, tiotropium Respimat® improved lung function, COPD exacerbations, HR-QOL and dyspnoea and was at least as effective as tiotropium HandiHaler®. Tiotropium Respimat® was generally well tolerated in patients with COPD, with anticholinergic adverse events among the most commonly reported adverse events. In the TIOSPIR trial, tiotropium Respimat® was noninferior to tiotropium HandiHaler® in terms of all-cause mortality, and the risk of cardiovascular mortality or major adverse cardiovascular events did not significantly differ between the two devices. Thus, tiotropium Respimat® Soft Mist™ Inhaler is a useful option for the treatment of patients with COPD.
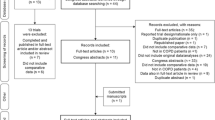
Data selection sources:
Relevant medical literature (including published and unpublished data) on tiotropium bromide was identified by searching databases including MEDLINE (from 1946) and EMBASE (from 1996) [searches last updated 22 September 2014], bibliographies from published literature, clinical trial registries/databases and websites. Additional information was also requested from the company developing the drug.
Search terms: Tiotropium, tiotropium bromide, Respimat®, chronic obstructive pulmonary disease, chronic obstructive lung disease, COPD.
Study selection: Studies in patients with chronic obstructive pulmonary disease who received tiotropium bromide via Respimat®. When available, large, well-designed, comparative trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
References
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: updated 2014. http://www.goldcopd.org/guidelines-global-strategy-for-diagnosis-management.html (2014). Accessed 22 Sep 2014.
Barnes PJ. The pharmacological properties of tiotropium. Chest. 2000;117(2 Suppl):63S–6S.
Boehringer Ingelheim Limited. Spiriva (tiotropium) Respimat 2.5 micrograms, solution for inhalation: UK summary of product characteristics. 2014. http://www.medicines.org.uk/emc/medicine/20134/SPC/Spiriva+Respimat+2.5+micrograms+solution+for+inhalation/. Accessed 22 Sep 2014.
Boehringer Ingelheim Limited. Spiriva (tiotropium) 18 microgram inhalation powder, hard capsule: UK summary of product characteristics. 2013. http://www.medicines.org.uk/emc/medicine/10039. Accessed 22 Sep 2014.
Keating GM. Tiotropium bromide inhalation powder: a review of its use in the management of chronic obstructive pulmonary disease. Drugs. 2012;72(2):273–300.
Dalby R, Spallek M, Voshaar T. A review of the development of Respimat® Soft Mist™ Inhaler. Int J Pharm. 2004;283(1–2):1–9.
Zierenberg B. Optimizing the in vitro performance of Respimat. J Aerosol Med. 1999;12(Suppl 1):S19–24.
Hochrainer D, Hölz H, Kreher C, et al. Comparison of the aerosol velocity and spray duration of Respimat® Soft Mist™ inhaler and pressurized metered dose inhalers. J Aerosol Med. 2005;18(3):273–82.
Pitcairn G, Reader S, Pavia D, et al. Deposition of corticosteroid aerosol in the human lung by Respimat® Soft Mist™ inhaler compared to deposition by metered dose inhaler or by Turbuhaler® dry powder inhaler. J Aerosol Med. 2005;18(3):264–72.
Newman SP, Steed KP, Reader SJ, et al. Efficient delivery to the lungs of flunisolide aerosol from a new portable hand-held multidose nebulizer. J Pharm Sci. 1996;85(9):960–4.
Newman SP, Steed KP, Reader SJ, et al. An in vitro study to assess facial and ocular deposition from Respimat® Soft Mist™ inhaler. J Aerosol Med. 2007;20(1):7–12.
Medicines Evaluation Board. Public assessment report of the Medicines Evaluation Board in the Netherlands: Spiriva (tiotropium) Respimat 2.5 microgram, solution for inhalation. 2011. http://www.cbg-meb.nl/CBG/en/human-medicines/geneesmiddeleninformatiebank/default.htm. Accessed 22 Sep 2014.
Disse B, Speck GA, Rominger KL, et al. Tiotropium (Spiriva™): mechanistical considerations and clinical profile in obstructive lung disease. Life Sci. 1999;64(6–7):457–64.
Haddad E-B, Mak JCW, Barnes PJ. Characterization of [3H]Ba 679 BR, a slowly dissociating muscarinic antagonist, in human lung: radioligand binding and autoradiographic mapping. Mol Pharmacol. 1994;45(5):899–907.
Disse B, Reichl R, Speck G, et al. BA 679 BR, a novel long-acting anticholinergic bronchodilator. Life Sci. 1993;52(5–6):537–44.
Tautermann CS, Kiechle T, Seeliger D, et al. Molecular basis for the long duration of action and kinetic selectivity of tiotropium for the muscarinic M3 receptor. J Med Chem. 2013;56(21):8746–56.
Takahashi T, Belvisi MG, Patel H, et al. Effect of BA 679 BR, a novel long-acting anticholinergic agent, on cholinergic neurotransmission in guinea pig and human airways. Am J Respir Crit Care Med. 1994;150(6 Pt 1):1640–5.
Sykes DA, Dowling MR, Leighton-Davies J, et al. The influence of receptor kinetics on the onset and duration of action and the therapeutic index of NVA237 and tiotropium. J Pharmacol Exp Ther. 2012;343(2):520–8.
van Noord JA, Cornelissen PJG, Aumann J-L, et al. The efficacy of tiotropium administered via Respimat® Soft Mist Inhaler™ or HandiHaler® in COPD patients. Respir Med. 2009;103(1):22–9.
Voshaar T, Lapidus R, Maleki-Yazdi R, et al. A randomized study of tiotropium Respimat® Soft Mist™ Inhaler vs. ipratropium pMDI in COPD. Respir Med. 2008;102(1):32–41.
Ichinose M, Fujimoto T, Fukuchi Y. Tiotropium 5 μg via Respimat and 18 μg via HandiHaler; efficacy and safety in Japanese COPD patients. Respir Med. 2010;104(2):228–36.
Hohlfeld JM, Sharma A, van Noord JA, et al. Pharmacokinetics and pharmacodynamics of tiotropium solution and tiotropium powder in chronic obstructive pulmonary disease. J Clin Pharmacol. 2014;54(4):405–14.
Bateman E, Singh D, Smith D, et al. Efficacy and safety of tiotropium Respimat® SMI in COPD in two 1-year randomized studies. Int J Chron Obstruct Pulmon Dis. 2010;5:197–208.
Bateman ED, Tashkin D, Siafakas N, et al. A one-year trial of tiotropium Respimat® plus usual therapy in COPD patients. Respir Med. 2010;104(10):1460–72.
Feifel U, Wallenstein G, Rominger K-L, et al. Pharmacokinetics and tolerability (study 1) with particular reference to ocular safety (study 2) of tiotropium Respimat® Soft Mist Inhaler™: findings from two dose-ranging studies in healthy men. Int J Chron Obstruct Pulmon Dis. 2008;3(3):397–403.
Asano K, Shikama Y, Shibuya Y, et al. Suppressive activity of tiotropium bromide on matrix metalloproteinase production from lung fibroblasts in vitro. Int J Chron Obstruct Pulmon Dis. 2008;3(4):781–9.
Asano K, Shikama Y, Shoji N, et al. Tiotropium bromide inhibits TGF-β-induced MMP production from lung fibroblasts by interfering with Smad and MAPK pathways in vitro. Int J Chron Obstruct Pulmon Dis. 2010;5:277–86.
Powrie DJ, Wilkinson TMA, Donaldson GC, et al. Effect of tiotropium on sputum and serum inflammatory markers and exacerbations in COPD. Eur Respir J. 2007;30(3):472–8.
Holownia A, Mroz RM, Skopinski T, et al. Tiotropium increases PPARγ and decreases CREB in cells isolated from induced sputum of COPD patients. Adv Exp Med Biol. 2013;756:9–14.
Caillaud D, Le Merre C, Martinat Y, et al. A dose-ranging study of tiotropium delivered via Respimat® Soft Mist Inhaler™ or HandiHaler® in COPD patients. Int J Chron Obstruct Pulmon Dis. 2007;2(4):559–65.
Nakanishi T, Haruta T, Shirasaka Y, et al. Organic cation transporter-mediated renal secretion of ipratropium and tiotropium in rats and humans. Drug Metab Dispos. 2011;39(1):117–22.
Sharma A, Hohlfeld J, Cornelissen PJG, et al. Comparison of the pharmacokinetics and pharmacodynamics of once daily tiotropium Respimat® and tiotropium HandiHaler® in COPD patients [slide presentation]. In: European Respiratory Society Annual Congress 2013; 7–11 Sep 2013; Barcelona.
Calverley P, Könen-Bergmann M, Metzdorf N, et al. Tiotropium Respimat®: comparison of bronchodilator efficacy of 5- and 2.5-μg doses [abstract no. P924 plus poster]. In: European Respiratory Society International Congress 2014; 6–10 Sep 2014; Munich.
Tang Y, Massey D, Zhong N-S. Evaluation of the efficacy and safety of tiotropium bromide (5 μg) inhaled via Respimat in Chinese patients with chronic obstructive pulmonary disease. Chin Med J. 2013;126(19):3603–7.
Wise RA, Anzueto A, Cotton D, et al. Tiotropium respimat inhaler and the risk of death in COPD. N Engl J Med. 2013;369(16):1491–501.
Rau-Berger H, Mitfessel H, Glaab T. Tiotropium Respimat® improves physical functioning in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2010;5:367–73.
Hodder R, Pavia D, Lee A, et al. Lack of paradoxical bronchoconstriction after administration of tiotropium via Respimat® Soft Mist™ Inhaler in COPD. Int J Chron Obstruct Pulmon Dis. 2011;6:245–51.
Tashkin D, Metzdorf N, Hallmann C, et al. Safety of tiotropium in renally impaired patients [abstract no. P923 plus poster]. In: European Respiratory Society International Congress 2014; 6–10 Sep 2014; Munich.
Hohlfeld JM, Furtwaengler A, Könen-Bergmann M, et al. Cardiac safety of tiotropium in patients with COPD: combined analysis of Holter-ECG data from four randomized clinical trials [abstract no. P284 plus poster]. In: European Respiratory Society International Congress 2014; 6–10 Sep 2014; Munich.
Boehringer Ingelheim. Boehringer Ingelheim announces FDA approval of Spiriva® Respimat® (tiotropium bromide) inhalation spray for the maintenance treatment of COPD [media release]. 25 Sep 2014. http://us.boehringer-ingelheim.com/news_events/press_releases/press_release_archive/2014/09-25-14-boehringer-ingelheim-announces-fda-approval-spiriva-respimat-tiotropium-bromide-inhalation-spray-maintenance-treatment-copd.html.
Data on file, Boehringer Ingelheim: 2014.
Mathioudakis AG, Chatzimavridou-Grigoriadou V, Evangelopoulou E, et al. Comparative mortality risk of tiotropium administered via handihaler or respimat in COPD patients: are they equivalent? Pulm Pharmacol Ther. 2014;28(2):91–7.
US Food and Drug Administration. Early communication about an ongoing safety review of tiotropium (marketed as Spiriva HandiHaler). 2008. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/DrugSafetyInformationforHeathcareProfessionals/ucm070651.htm. Accessed 22 Sep 2014.
Singh S, Loke YK, Furberg CD. Inhaled anticholinergics and risk of major adverse cardiovascular events in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. JAMA. 2008;300(12):1439–50.
Tashkin DP, Celli B, Senn S, et al. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med. 2008;359(15):1543–54.
US Food and Drug Administration. Follow-up to the October 2008 updated early communication about an ongoing safety review of tiotropium (marketed as Spiriva HandiHaler). 2010. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/DrugSafetyInformationforHeathcareProfessionals/ucm197429.htm. Accessed 22 Sep 2014.
Rodrigo GJ, Castro-Rodriguez JA, Nannini LJ, et al. Tiotropium and risk for fatal and nonfatal cardiovascular events in patients with chronic obstructive pulmonary disease: systematic review with meta-analysis. Respir Med. 2009;103(10):1421–9.
Celli B, Decramer M, Leimer I, et al. Cardiovascular safety of tiotropium in patients with COPD. Chest. 2010;137(1):20–30.
Kesten S, Celli B, Decramer M, et al. Tiotropium HandiHaler® in the treatment of COPD: a safety review. Int J Chron Obstruct Pulmon Dis. 2009;4:397–409.
Bateman ED. Tiotropium Respimat increases the risk of mortality: con. Eur Respir J. 2013;42(3):590–3.
Singh S, Loke YK, Enright PL, et al. Mortality associated with tiotropium mist inhaler in patients with chronic obstructive pulmonary disease: systematic review and meta-analysis of randomised controlled trials. BMJ. 2011;342:d3215.
Dong Y-H, Lin H-H, Shau W-Y, et al. Comparative safety of inhaled medications in patients with chronic obstructive pulmonary disease: systematic review and mixed treatment comparison meta-analysis of randomised controlled trials. Thorax. 2013;68(1):48–56.
Karner C, Chong J, Poole P. Tiotropium versus placebo for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012;7: CD009285.
Verhamme KMC, Afonso A, Romio S, et al. Use of tiotropium Respimat Soft Mist Inhaler versus HandiHaler and mortality in patients with COPD. Eur Respir J. 2013;42(3):606–15.
Disse B, Metzdorf N, Martin A, et al. Mortality associated with tiotropium mist inhaler? A critical appraisal of the authors’ selection and use of previously communicated tiotropium Respimat data [letter]. 2011. http://www.bmj.com/content/342/bmj.d3215?tab=responses. Accessed 22 Sep 2014.
Metzdorf N, Hallmann C, Disse B. Thorax editorial by Jenkins and Beasley related to tiotropium respimat [letter]. Thorax. 2013;68(8):782.
Barnes NC, Jones PW, Davis KJ. Safety of tiotropium through the Handihaler: why did meta-analyses and database studies appear to give a false alarm? Thorax. 2014;69(6):598–9.
European Medicines Agency. Pharmacovigilance Risk Assessment Committee (PRAC): PRAC minutes of the meeting on 2-5 December 2013. 2013. www.ema.europa.eu/docs/en_GB/document_library/Minutes/2014/01/WC500159614.pdf. Accessed 22 Sep 2014.
European Medicines Agency. Pharmacovigilance Risk Assessment Committee (PRAC): minutes of the meeting on 5-8 May 2014. 2014. www.ema.europa.eu/docs/en_GB/document_library/Minutes/2014/06/WC500169468.pdf. Accessed 22 Sep 2014.
Verhamme KMC, Van Blijderveen N, Sturkenboom MCJM. Tiotropium and the risk of death in COPD [letter]. N Engl J Med. 2014;370(5):481–2.
Halpin D, Dahl R, Hallmann C, et al. Tiotropium Handihaler® and Respimat® in COPD: a safety analysis on pooled data [abstract]. In: American Thoracic Society 2014 International Conference; 16–21 May 2014; San Diego (CA).
Dahl R, Schmidt H, Könen-Bergmann M, et al. Mixed treatment analysis comparing tiotropium HandiHaler® and Respimat® [abstract no. P925 plus poster]. In: European Respiratory Society International Congress 2014; 6–10 Sep 2014; Munich.
Bateman ED. Improving inhaler use in COPD and the role of patient preference. Eur Respir Rev. 2005;14(96):85–8.
Anderson P. Use of Respimat® Soft Mist™ Inhaler in COPD patients. Int J Chron Obstruct Pulmon Dis. 2006;1(3):251–9.
Fink JB, Colice GL, Hodder R. Inhaler devices for patients with COPD. COPD. 2013;10(4):523–35.
Beasley R. Tiotropium Respimat increases the risk of mortality: pro. Eur Respir J. 2013;42(3):584–9.
Asakura Y, Nishimura N, Maezawa K, et al. Effect of switching tiotropium HandiHaler® to Respimat® Soft Mist™ Inhaler in patients with COPD: the difference of adverse events and usability between inhaler devices. J Aerosol Med Pulm Drug Deliv. 2013;26(1):41–5.
Shah P, Dhurjon L, Metcalfe T, et al. Acute angle closure glaucoma associated with nebulised ipratropium bromide and salbutamol. BMJ. 1992;304(6818):40–1.
Oksuz H, Tamer C, Akoglu S, et al. Acute angle-closure glaucoma precipitated by local tiotropium absorption. Pulm Pharmacol Ther. 2007;20(6):627–8.
Hall SK. Acute angle-closure glaucoma as a complication of combined beta-agonist and ipratropium bromide therapy in the emergency department. Ann Emerg Med. 1994;23(4):884–7.
Boehringer Ingelheim. Tiotropium + olodaterol fixed dose combination (FDC) in chronic obstructive pulmonary disease (OTEMTO 2) [ClinicalTrials.gov identifier NCT02006732] US National Institutes of Health, ClinicalTrials.gov. 2014. http://www.clinicaltrials.gov/ct2/show/NCT02006732. Accessed 22 Sep 2014.
Boehringer Ingelheim. Tiotropium + olodaterol fixed dose combination (FDC) in chronic obstructive pulmonary disease (OTEMTO 1) [ClinicalTrials.gov identifier NCT01964352] US National Institutes of Health, ClinicalTrials.gov. 2014. http://www.clinicaltrials.gov/ct2/show/NCT01964352. Accessed 22 Sep 2014.
Derom E, Westerman J, Grönke L, et al. The 24-hour lung function profile of once-daily tiotropium and olodaterol fixed-dose combination compared with placebo and monotherapies in chronic obstructive pulmonary disease (VIVACITO) [poster]. In: American Thoracic Society International Conference; 16–21 May 2014; San Diego (CA).
Buhl R, Derom E, Ferguson G, et al. Once-daily tiotropium and olodaterol fixed-dose combination via the Respimat improves ouctomes vs monocomponents in COPD in two 1-year studies [abstract no. 1895]. In: European Respiratory Society International Congress 2014; 6–10 Sep 2014; Munich.
Buhl R, Abrahams R, Bjermer L, et al. Safety of once-daily tiotropium and olodaterol fixed-dose combination via the Respimat® in chronic obstructive pulmonary disease in two 1-year studies [poster]. In: European Respiratory Society International Congress 2014; 6–10 Sep 2014; Munich.
Yohannes AM, Connolly MJ, Hanania NA. Ten years of tiotropium: clinical impact and patient perspectives. Int J Chron Obstruct Pulmon Dis. 2013;8:117–25.
Disclosure
The preparation of this review was not supported by any external funding. Gillian Keating is a salaried employee of Adis/Springer. During the peer review process, the manufacturer of the agent under review was offered an opportunity to comment on this article. Changes resulting from comments received were made by the author on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Additional information
The manuscript was reviewed by: S.A. Antoniu, University of Medicine and Pharmacy Grigore T Popa Iasi, Department of Interdisciplinarity-Palliative Care Nursing, Iasi, Romania; M. Confalonieri, Department of Pneumology & Respiratory Intensive Care Unit, University Hospital of Cattinara, Trieste, Italy; F. García-Río, Servicio de Neumología, Hospital Universitario La Paz, Facultad de Medicina, Universidad Autónoma de Madrid, IdiPAZ, Madrid, Spain; C. Incorvaia, Pulmonary Rehabilitation Unit, Istituti Clinici di Perfezionamento, Presidio Ospedaliero CTO, Milan, Italy.
Rights and permissions
About this article
Cite this article
Keating, G.M. Tiotropium Respimat® Soft Mist™ Inhaler: A Review of Its Use in Chronic Obstructive Pulmonary Disease. Drugs 74, 1801–1816 (2014). https://doi.org/10.1007/s40265-014-0307-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-014-0307-4