Abstract
Oral rifaximin 550 mg (Refero®; Targaxan®; Tixteller®; Xifaxan®) twice daily, either alone or more commonly with medicines containing lactulose, is approved in several countries, including the UK, EU and USA, for use in adults with liver disease to reduce the recurrence of episodes of overt hepatic encephalopathy (HE). Rifaximin is a broad-spectrum antibacterial that acts locally in the gut to reduce intestinal flora, including ammonia-producing species, with hyperammonaemia considered to play a central role in the pathogenesis of HE. In a 6-month, multinational trial in patients with liver disease, rifaximin 550 mg twice daily (± lactulose) was an effective and well tolerated treatment for reducing the recurrence of HE episodes. At study end, rifaximin therapy significantly prolonged the time to the first breakthrough HE episode compared with placebo (± lactulose), irrespective of geographical region or baseline patient and disease characteristics. Rifaximin treatment also significantly reduced HE-related hospitalizations and improved health-related quality of life compared with placebo. Furthermore, the efficacy of rifaximin with or without lactulose in reducing the recurrence of overt HE episodes was maintained after up to 2.5 years of treatment, with no new safety signals arising during this period. This article reviews the pharmacology and therapeutic efficacy of rifaximin 550 mg twice daily in reducing the recurrence of overt HE episodes in adults with liver disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Minimally absorbable, broad-spectrum antibacterial with activity against most Gram-positive and Gram-negative aerobic and anaerobic enteric bacteria, including ammonia-producing species |
Prolongs the time to first breakthrough HE episode compared with placebo (both typically taken with lactulose) |
Reduces hospitalization involving HE compared with placebo |
Sustained efficacy with long-term therapy |
Similar tolerability profile to that of placebo |
1 Introduction
Hepatic encephalopathy (HE) is a common, serious neuropsychiatric syndrome occurring in patients with acute and chronic liver disease, has significant impacts on patient’s morbidity and mortality and poses a significant economic burden on healthcare systems [1–6]. The syndrome may have subclinical manifestations (i.e. minimal HE, which occurs in up to 80 % of patients with cirrhotic liver disease [1, 3] and is predictive for the development of overt HE [3]) or clinical manifestations [i.e. overt HE, which occurs in ≈30–45 % of patients with cirrhotic liver disease [1, 3] and 10–50 % of patients with transjugular intrahepatic portosystemic shunt (TIPS) [1, 6]]. Overt HE requires frequent hospitalization, with severe cases potentially resulting in coma or death, and is an independent predictor of mortality in patients with cirrhotic liver disease, with respective 1- and 3-year survival rates of approximately 50 and 25 % [2, 3]. Clinical manifestations of overt HE include mental and personality changes, asterixis, motor-sensory abnormalities, decreased energy, impaired cognition, impaired sleep-wake cycle and decreased hand-eye co-ordination. Patients with minimal HE have normal mental and neurological status upon clinical examination, but have abnormal results in specific psychometric tests [1–3].
Although the pathogenesis of HE remains to be fully elucidated, hyperammonaemia is considered to play a central role, with decreased hepatic function or portal-systemic shunts resulting in increased systemic circulation of ammonia produced by enteric bacteria [1–3, 5]. The ammonia crosses the blood-brain barrier and enters the CNS, resulting in morphological changes to astrocytes and direct effects on excitatory and inhibitory neurotransmitters. Hence, a key strategy in the treatment of HE is to target the hyperammonaemia by reducing production and absorption of ammonia from the gastrointestinal tract through empirical therapy. Non-absorbable disaccharides such as lactulose have a cathartic effect and act to reduce ammonia synthesis and absorption in the gut by reducing the colonic pH and interfering with mucosal uptake of glutamine. Although lactulose is considered a component of the current standard of care, lactulose treatment regimens are complex and over-treatment may result in serious adverse effects such as severe dehydration, hyponatraemia and worsening of HE. Treatment with oral rifaximin (Refero®; Targaxan®; Tixteller®; Xifaxan®), a broad-spectrum antibacterial that is minimally absorbed and generally well tolerated and, like lactulose, is considered standard care, provides another strategy to reduce the ammonia load by reducing enteric bacterial flora, including ammonia-producing bacteria. Antibacterials utilized as empirical therapy in patients with HE include metronidazole and neomycin, albeit their use is limited by potential serious adverse effects (peripheral neuropathy with metronidazole, and ototoxicity and nephrotoxicity with neomycin) [1–3, 5]. Other potential options under investigation for treatment of HE include glycerol phenylbutyrate (a metabolic ammonia scavenger), branched-chain amino acid-enriched formulations and probiotics [6]. Once the current episode of HE has resolved, the goals of therapy are prevention of the recurrence of HE episodes through ongoing therapy for an indefinite period with lactulose and rifaximin [5].
This article reviews the pharmacology and therapeutic use of the oral rifaximin 550 mg (Refero®; Targaxan®; Tixteller®; Xifaxan®) in reducing the recurrence of overt episodes of HE in adult patients with liver cirrhosis. Discussion of its use in the treatment of HE episodes per se and the use of other formulations and dosages of rifaximin in reducing the recurrence of HE episodes are beyond the scope of this review.
2 Pharmacodynamic Properties
Rifaximin α-polymorph (the formulation used in branded rifaximin [7]) is a poorly absorbed (Sect. 3), non-aminoglycoside, semisynthetic antibacterial derived from rifamycin [8–10]. In contrast to the poor absorption of rifaximin-α, the amorphous formulations of rifaximin commonly found in some generic formulations showed high absorbability that was similar to that of a systemically absorbed agent [11, 12].
Rifaximin acts locally in the gut to inhibit bacterial RNA synthesis by binding irreversibly to the β-subunit of the DNA-dependent RNA polymerase. Rifaximin has a broad spectrum of in vitro activity against aerobic and anaerobic Gram-positive and Gram-negative enteric bacteria, including ammonia-producing species [8–10]. By reducing the division of deaminating enteric bacteria, rifaximin decreases production of nitrogenous and other neurotoxic compounds that are believed to be important in the pathogenesis of HE [10, 13]. In addition, the mechanism action of rifaximin in the clinical setting may, at least in part, relate to its ability to modify microbiota-associated metabolic function [7].
Development of resistance to rifaximin primarily involves a reversible chromosomal one-step alteration in the rpoB gene encoding bacterial RNA polymerase [10]. Based on clinical studies in patients with traveller’s diarrhoea, rifaximin did not appear to select for resistance among Gram-positive and -negative intestinal flora during a 3-day course of rifaximin [8, 10]. Following multiple high doses of rifaximin, strains resistant to rifaximin did develop in normal intestinal bacterial flora in healthy volunteers and in patients with inflammatory bowel disease; however, these strains were unstable and did not colonize the gastrointestinal tract or replace rifaximin-sensitive strains [10]. Rifaximin treatment in patients harbouring Mycobacterium tuberculosis or Neisseria meningitides will not select for rifampicin resistance, based on experimental and clinical data [10].
3 Pharmacokinetic Properties
Rifaximin exhibits non-linear, dose-dependent absorption, which is consistent with the possibility of dissolution-rate-limited absorption of the drug [10]. The drug undergoes minimal systemic absorption (<1%) in humans, with negligible plasma levels (<10 ng/mL) after multiple therapeutic doses of rifaximin in patients with inflammatory bowel disease and in healthy volunteers [10, 14]. In patients with HE receiving rifaximin 550 mg twice daily, mean systemic exposure to rifaximin was approximately 12-fold higher than that in healthy volunteers [10, 15]. Rifaximin is moderately bound to human plasma proteins in vivo, with a mean protein binding ratio of 67.5 % in healthy volunteers and 62 % in patients with hepatic impairment receiving rifaximin 550 mg [10].
Analyses of faeces indicated that rifaximin was excreted as the unchanged drug, implying that it is not degraded or metabolized during passage through the gastrointestinal tract [10]. Less than 0.01 % of a radio-labelled dose of rifaximin was recovered as 25-desacetylrifaximin, which is the only metabolite of rifaximin that has been identified in humans. In a radiolabelled study, 96.9 % of the rifaximin dose was eliminated in the faeces, with ≤0.4 % of the dose recovered in the urine [10].
Based on in vitro studies, rifaximin does not inhibit the major cytochrome P450 (CYP) drug metabolizing enzymes (CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP2E1 and CYP3A4) or induce CYP1A2 and CYP2B6, although it was a weak inducer of CYP3A4 [10]. In a study in healthy volunteers, rifaximin did not appear to induce intestinal or hepatic CYP3A activity [16].
Coadministration of rifaximin with the oral contraceptive ethinylestradiol/norgestimate did not alter the pharmacokinetics of ethinylestradiol/norgestimate in healthy women [17].
Since rifaximin acts locally, no dosage adjustments of rifaximin are required in patients with hepatic impairment, despite a 10-, 13- and 20-fold increase in systemic exposure in patients with mild (Child-Pugh A), moderate (Child-Pugh B) and severe hepatic impairment (Child-Pugh C), respectively, compared with healthy volunteers [10].
4 Therapeutic Efficacy
4.1 Short-Term Pivotal Trial
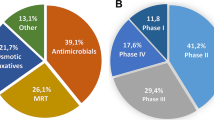
The efficacy of oral rifaximin 550 mg twice daily in reducing recurrent episodes of HE in adult patients (aged ≥18 years) who were in remission from recurrent HE episodes associated with chronic liver disease was investigated in a 6-month, double-blind, multinational phase III trial [18, 19]. The majority of patients (91 % in both groups) received concomitant lactulose [mean lactulose dosage in the rifaximin (n = 140) and placebo (n = 159) groups was 3.14 and 3.51 cups/day; each cup = 10 g lactulose/15 mL] [18].
Participants had experienced ≥2 episodes of overt HE (Conn score ≥2) associated with hepatic cirrhosis during the previous 6 months, were in remission at enrolment (Conn score 0–1) and had a score of ≤25 on the Model for End-Stage Liver Disease (MELD) scale (higher scores indicate more severe disease) [18]. Key exclusion criteria included the expectation of liver transplantation within 1 month after the screening visit, the presence of conditions that are known precipitants of HE within 3 months prior to the screening visit, and the presence of chronic renal or respiratory insufficiency or specified laboratory abnormalities. There were no significant differences between treatment groups in baseline characteristics [18].
The primary endpoint was the time to first breakthrough episode of HE, defined as the time from the first dose of study drug to an increase from baseline Conn score to a Conn score of ≥2 or a Conn score of 1 plus a 1-unit increase in asterixis grade [18]. The key secondary endpoint was the time to the first hospitalization involving HE. Analyses were conducted in the intent-to-treat population (i.e. all patients who received ≥1 dose of study drug), with primary and key secondary endpoint analyses assessed using Kaplan–Meier methods [18].
Rifaximin plus lactulose significantly prolonged the time to the first breakthrough HE episode compared with placebo plus lactulose, with a 58 % relative reduction in the risk of a breakthrough HE episode in the rifaximin group [hazard ratio (HR) 0.42; 95 % CI 0.28–0.64; p < 0.001] [18]. This correlated to a number needed-to-treat (NNT) with rifaximin for 6 months of four to prevent one overt episode of HE. By study end, 22.1 % of rifaximin recipients had experienced breakthrough episodes of HE compared with 45.9 % of placebo recipients. In pre-specified subgroup analyses in which patients were stratified according to baseline characteristics, the risk of breakthrough HE episode was significantly (p < 0.05) lower in rifaximin than in placebo recipients, irrespective of geographical region or the patient’s sex, age, ethnic group, MELD score (in those with a score of ≤10 or 11–18) or Conn score (0 or 1), the presence or absence of comorbid diabetes, duration of remission of HE episodes (≤90 or >90 days), number of HE episodes in the previous 6 months (2 or >2) and the presence or absence of TIPS. There was no statistically significant between-group difference in the risk of a breakthrough HE episode in patients who were not using lactulose at baseline and those with more severe disease (MELD score 19–24) at baseline [18].
In the rifaximin and placebo groups, 13.6 and 22.6 % of patients had hospitalizations involving HE, reflecting a 50 % relative reduction in the risk of these hospitalizations in rifaximin recipients (HR 0.50; 95 % CI 0.29–0.87; p = 0.01) [18]. This correlated to an NNT of nine to prevent one hospitalization involving HE.
During the 6-months study, rifaximin recipients experienced significant improvements in health-related quality of life (HR-QOL) compared with placebo recipients, based on a longitudinal analysis using time-weighted averages (Twa) of Chronic Liver Disease Questionnaire (CLDQ) scores normalized by days on study therapy [19]. In the overall population, mean Twa scores for the CLDQ total score and for each of the six individual domains (fatigue, abdominal symptoms, systemic symptoms, activity, emotional function and worry) were significantly (p < 0.0001) higher (i.e. better HR-QOL) in patients who maintained remission (n = 134) than in those who experienced a breakthrough HE episode (n = 85). In addition, least-square mean differences in the Twa CLDQ total and individual domain scores all favoured rifaximin over placebo (p < 0.05) [19]. The validity of utilizing the CLDQ to estimate HR-QOL in this patient population was demonstrated in an analysis of the relationship between patient scores for the CLDQ and health-related utility, as measured by the estimated European quality of life-5D (EQ-5D) index in patients with HE (poster presentation) [20].
Rifaximin treatment (n = 61) was more effective than placebo (n = 67) in reducing the occurrence of breakthrough HE episodes in patients in whom hepatitis C virus infection was the etiology of advanced liver disease, based on a post hoc subgroup analysis (abstract presentation) [21]. Over the 6-month study, breakthrough HE episodes occurred in 26.2 % of rifaximin recipients versus 47.8 % of placebo recipients, resulting in a 52.2 % relative reduction in the risk of a breakthrough HE episode (HR 0.478; 95 % CI 0.262–0.871; p = 0.0136). These results were similar to those observed in patients with other etiologies of advanced liver disease, in whom breakthrough HE episodes occurred in 19.0 % of patients in the rifaximin group (n = 79) versus 44.6 % in the placebo group (n = 92) (HR 0.367; 95 % CI 0.203–0.663; p = 0.0005) [21].
4.2 Maintenance Trial
A 24-month, open-label maintenance study evaluated safety (n = 392 in integrated safety analysis; see Sect. 5) and hospitalization rates with long-term use of rifaximin 550 mg twice daily in patients who had participated in the pivotal 6-month trial (n = 70 from the rifaximin group and 82 from the placebo group; see Sect. Error! Reference source not found.) and in newly enrolled patients with cirrhosis and recurrent HE (n = 170) [22]. Concomitant treatment with lactulose was optional during the maintenance study. There were generally no significant differences between the all-rifaximin (n = 392; all patients from the pivotal trial and maintenance study), new–rifaximin (n = 252; all patients who initiated rifaximin in the maintenance study), and historical-rifaximin and historical-placebo populations (i.e. participants in the pivotal trial) with regard to baseline demographics, liver disease history and HE severity. The median exposure to rifaximin in the all-rifaximin population was 427.0 days [510.5 patient-years’ exposure (PYE)] and in the new-rifaximin population was 475.5 days (342.3 PYE). Hospitalization rates reported were normalized for exposure [22].
Rates of HE-related hospitalization remained low during rifaximin treatment in the maintenance study, with respective rates in the all-rifaximin (109 HE-related hospitalizations/510.5 PYE), new-rifaximin (79 HE-related hospitalizations/342.3 PYE), historical-rifaximin (15 HE-related hospitalizations/50.0 PYE) and historical-placebo (33 HE-related hospitalizations/46.0 PYE) populations of 0.21, 0.23, 0.30 and 0.72 events/PYE [22]. The rate of HE-related hospitalizations was significantly (p < 0.001) lower in the historical-rifaximin group than in the historical-placebo group (0.30 vs. 0.72 events/PYE). Rates of all-cause hospitalizations in the all-rifaximin, new-rifaximin, historical-rifaximin and historical-placebo populations were 0.45, 0.44, 0.92 and 1.30 events/PYE, respectively [22].
A prior history of more than two HE episodes was predicted to increase the risk of death [23] and the risk of an HE episode as the number of prior episodes increases) [24], based on Kaplan–Meier estimates in post hoc analyses of data from patients participating in the extension study (median follow-up of 17 months) [abstract presentations]. In patients who had experienced one, two or at least three prior HE episodes (n = 321), 1-year survival rates were 0.947 (95 % CI 0.891–1.000), 0.898 (95 % CI 0.845–0.953) and 0.793 (95 % CI 0.735–0.856), respectively, with corresponding 2-year survival rates of 0.910 (95 % CI 0.822–1.000), 0.808 (95 % CI 0.719–0.909) and 0.783 (95 % CI 0.677–0.828). For both 1- and 2-year survival curves, there were significant (p < 0.001 log rank test) differences in survival curves in patients who had experienced one or two prior HE episodes compared with those who had experienced more than two prior HE episodes, with no significant difference between those who had one prior and those who had two prior HE episodes [23]. In patients who had experienced one, two, three or ≥4 HE episodes (n = 319), the probability of being event free at 1 year was 0.644 (95 % CI 0.543–0.763), 0.615 (95 % CI 0.541–0.700), 0.396 (95 % CI 0.303–0.518) and 0.302 (95 % CI 0.246–0.371), respectively; corresponding probabilities of being event free at 2 years were 0.579 (95 % CI 0.469–0.713), 0.539 (95 % CI 0.455–0.638), 0.292 (95 % CI 0.199–0.428) and 0.218 (95 % CI 0.163–0.290). There was a significant difference in curves between those who had experienced one or two HE episodes and those who had experienced more than two HE episodes (p < 0.001 log rank test) [24].
A post hoc analysis based on pooled data from the pivotal trial (Sect. 4.1) and maintenance study (Sect. 4.2) indicated that rifaximin monotherapy (n = 40) was more effective than rifaximin plus lactulose therapy (n = 352) in maintaining HE remission (abstract presentation) [25]. Breakthrough HE episodes occurred in 10 % of patients receiving rifaximin monotherapy compared with 44.6 % of those receiving rifaximin plus lactulose, representing an 82.2 % reduction in the relative risk of a breakthrough HE episode with rifaximin monotherapy (HR 0.178; 95 % CI 0.066–0.480; p = 0.0001).
4.3 Pharmacoeconomic Considerations
In a cost-effectiveness analysis conducted from the UK health payer perspective and utilizing a Markov model, rifaximin was estimated to be cost effective compared with standard care over 5-year, 10-year and lifetime (i.e. 42 years = death of last patient) horizons, assuming a willingness-to-pay (WTP) threshold of £30,000 per quality-adjusted life-year (QALY) gained (poster presentations) [26]. The time to first observed HE event was based on the pivotal trial (Sect. 4.1), with the time to all subsequent events and time to death determined from the maintenance study (Sect. 4.2). The year of costing was 2012, with an annual discount rate of 3.5 % for costs and benefits. Drug acquisition costs per calendar month were £289.95 for rifaximin and £9.09 for lactulose. Based on this model, rifaximin was likely to be associated with reduced progression of HE events and improved survival due to a reduction in HE episodes compared with standard care. Discounted costs for rifaximin over a 5-year, 10-year and lifetime horizon were £15,559, £22,358 and £28,874, respectively, with corresponding discounted rates for the standard care group of £4,574, £5,887 and £6,925. QALYs gained were not reported. Incremental cost-effective ratios over a 5-year, 10-year and lifetime horizon, respectively, were £20,829, £19,207 and £17,681 per QALY gained. At a WTP of £30,000/QALY, rifaximin treatment had an 84, 89 and 95 % likelihood of being cost effective over a 5-year, 10-year and lifetime horizon, respectively. These results were robust across a broad range of clinically plausible scenarios [26].
This pharmacoeconomic analysis, as with all such modelled analyses, is subject to limitations, with a potential for input data from clinical trials to differ from real-life situations. Furthermore, results obtained in one country may not be applicable to other geographical regions because of differences such as those in healthcare systems, medical practice and costs. In addition to these inherent limitations of pharmacoeconomic studies, specific limitations of this study [26] included the lack of placebo data in the long-term maintenance trial, which meant that assumptions were validated using real world data, and the model was based on a combination of clinical trial and epidemiological sources along with expert opinion.
5 Tolerability
Rifaximin treatment for up to 2.5 years was generally well tolerated in patients with hepatic cirrhosis participating in trials [18, 22] discussed in Sect. 4. The nature and incidence of treatment-emergent adverse events occurring in rifaximin recipients was generally similar to that in placebo recipients in the pivotal 6-month trial [18], with no new safety signals arising during the subsequent maintenance study [22]. Most adverse events were of mild to moderate intensity [18]. At the end of the maintenance study, the rate of any adverse events (0.69 vs. 0.71 events/PYE), serious adverse events (0.46 vs. 0.48 events/PYE) and discontinuation because of an adverse event (0.22 vs. 0.25 events/PYE) were generally similar in the new-rifaximin (2 years’ exposure) and all-rifaximin populations (≤2.5 years’ exposure; see Sect. 4.2 for further design details) [22].
In the pivotal trial, 80 % of patients in the rifaximin and placebo groups experienced at least one treatment-emergent adverse event, with those occurring with an incidence of ≥5 % and a ≥2 % higher frequency in the rifaximin than in the placebo group summarized in Fig. 1 [18]. There were no significant between-group differences in the incidence of any treatment-emergent adverse events. All serious treatment-emergent adverse events were reported with an incidence of ≤2.9 % in rifaximin or placebo recipients, except for hepatic cirrhosis (2.1 vs. 3.8 %), with these events appearing to occur with a similar incidence in both treatment groups [18].
Treatment-emergent adverse events occurring in ≥5 % of patients and with a ≥2% higher incidence in the rifaximin than placebo group in a 6-month, multinational trial in adult patients in remission from recurrent hepatic encephalopathy episodes [18]
In the pivotal 6-month trial, adverse events possibly related to infection that were of special interest because of known potential side effects of systemic antibiotics, as a drug class, and known effects of rifaximin occurring with an incidence of ≥1 % were pneumonia (2.9 % in the rifaximin group vs. 0.6 % in the placebo group), bacterial peritonitis (1.4 vs. 2.5 %), haematochezia (1.4 vs. 0.6 %), gastritis (1.4 vs. 0 %) and Clostridium difficile infection (1.4 vs. 0 %) [18]. Both of the rifaximin-treated patients who had C. difficile infections had several concurrent risk factors for such infections, with both patients making a full recovery following concomitant treatment for the infection [18]. The rates of C. difficile infection remained stable during the 2-year extension study [22] of this trial [18]; overall during both studies, six patients treated with rifaximin had C. difficile infections (event rate 0.012 events/PYE). All of these patients had several concurrent risk factors for C. difficile infection [22]. In a US retrospective analysis of medical charts of 211 patients with cirrhosis who received rifaximin at a university practice or community practices, 18 patients had diarrhoea during rifaximin treatment, with all cases resolving with appropriate therapy and none testing positive for C. difficile [27].
During postmarketing experience, cases of C. difficile-associated diarrhoea (CDAD) have been reported during rifaximin treatment [9]. Hypersensitivity reactions such as exfoliative dermatitis, rash, angioneurotic oedema, urticaria, flushing, pruritus and anaphylaxis have also been reported. Hypersensitivity reactions occurred as early as within 15 min of drug administration [9].
6 Dosage and Administration
Oral rifaximin, either alone or more commonly with medicines containing lactulose, is approved in several European countries under the Decentralised Procedure, with the UK as the Reference Member State, for use in adults with liver disease to reduce the recurrence of episodes of overt HE (featured indication) [28]. It is also approved in the USA for this indication [9]. In the UK [10], the recommended dosage of rifaximin in this patient population is 550 mg twice daily, with no dosage adjustments required in elderly patients. The drug may be taken without regard to food [10].
In the UK, rifaximin is contraindicated in patients with intestinal obstruction and in those with hypersensitivity to the drug, rifamycin derivatives or any of the excipients of the tablet formulation [10]. The potential association of rifaximin with CDAD and pseudomembranous colitis cannot be ruled out; CDAD has been reported with nearly all antibacterial agents, including rifaximin. Concomitant use of rifaximin with other rifamycins is not recommended, since there is a lack of data and a potential for severe disruption of gut flora with unknown consequences. As is the case with all rifamycins, patients should be warned of the potential for a reddish discolouration of the urine with rifaximin use, despite minimal absorption of the drug. Caution is advised in patients with severe (Child-Pugh C) hepatic impairment and in those with an MELD score of >25; since the drug acts locally, no dosage adjustments are required in patients with hepatic impairment. Caution is advised in patients with renal impairment, with no clinical data available on the use of rifaximin in this patient population [10].
Local prescribing information should be consulted for detailed information regarding the use of rifaximin in specific patient populations, contraindications, warnings and precautions.
7 Current Status of Rifaximin in Reducing Recurrence of Overt Hepatic Encephalopathy Episodes
Oral rifaximin, typically in combination with lactulose, was an effective and well tolerated treatment for reducing the recurrence of HE episodes in patients with liver disease participating in a 6-month, placebo-controlled, multinational trial. At 6 months, rifaximin treatment significantly prolonged the time to the first breakthrough HE episode compared with placebo with or without lactulose (primary endpoint), irrespective of geographical region or baseline patient characteristics. Relative to placebo, rifaximin treatment also significantly reduced hospitalizations involving HE and improved HR-QOL. Furthermore, the efficacy of rifaximin with or without lactulose in reducing the recurrence of overt HE episodes was maintained after up to 2.5 years of treatment, with no new safety signals arising during long-term rifaximin treatment.
HE episodes impose significant costs from a societal and healthpayer perspective, with these costs being an important consideration in determining the choice of treatment. Given the recent approval of rifaximin for reducing the recurrence of overt HE episodes, it is not unexpected that robust pharmacoeconomic data are limited. A recent cost-effectiveness analysis conducted from the UK healthpayer perspective and utilizing a Markov model estimated that rifaximin was cost effective compared with standard care over 5-year, 10-year and lifetime horizons, based on acceptable WTP thresholds. This pharmacoeconomic analysis, as with all such modelled analyses, is subject to limitations, with a potential for input data from clinical trials to differ from real-life situations and data from one country not necessarily applicable to other geographical regions.
Recent 2014 international guidelines indicate that lactulose is the usual initial treatment for overt HE based on current evidence and cost factors, albeit there are concerns regarding side effects that may arise with overuse of lactulose [6]. Rifaximin is considered an effective add-on therapy to lactulose for the prevention of overt HE recurrence, with no strong evidence supporting the use of rifaximin monotherapy for preventing recurrence of overt HE episodes [6]. Rifaximin appears to have a more favourable tolerability profile and a more convenient dosage regimen than lactulose and, as a consequence, may potentially become the preferred choice in the future for reducing the recurrence of overt HE episodes [5]. Direct head-to-head randomized trials comparing rifaximin monotherapy with lactulose monotherapy would help to more definitely establish the relative position of these two agents. In the meantime, rifaximin 550 mg twice daily, either as monotherapy or more commonly in combination with lactulose, is a valuable emerging option for the reducing the recurrence of overt HE episodes in patients with liver disease.
Data selection sources:
Relevant medical literature (including published and unpublished data) on rifaximin was identified by searching databases including MEDLINE (from 1946) and EMBASE (from 1996) [searches last updated 17 September 2014], bibliographies from published literature, clinical trial registries/databases and websites. Additional information was also requested from the company developing the drug.
Search terms: Rifaximin, Targaxan, Xifaxin, hepatic encephalopathy.
Study selection: Studies in patients in remission from recurrent hepatic encephalopathy episodes who received rifaximin. When available, large, well designed, comparative trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
References
Iadevaia MD, Prete AD, Cesaro C, et al. Rifaximin in the treatment of hepatic encephalopathy. Hepat Med Evid Res. 2011;3:109–17.
Poh Z, Chang PEJ. A current review of the diagnostic and treatment strategies of hepatic encephalopathy. Int J Hepatol. 2012. doi:10.1155/2012/480309.
Schiano TD. Clinical management of hepatic encephalopathy. Pharmacotherapy. 2010;30(5 Pt 2):10S–5S.
Orr JG, et al. Resource use associated with hepatic encephalopathy in patients with liver disease [abstract no. P478]. J Hepatol. 2014;60(Supp):S228–9.
Prakash R, Mullen K. Mechanisms, diagnosis and mangement of hepatic encephalopathy. Nat Rev Gastroenterol Hepatol. 2010;7:515–25.
Vilstrup H, Amodio P, Bajaj J, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014;60(2):715–35.
Bajaj JS, Heuman DM, Sanyal AJ, et al. Modulation of the metabiome by rifaximin in patients with cirrhosis and minimal hepatic encephalopathy. PLoS One. 2013;8(4):e60042.
Robins GW, Wellington K. Rifaximin: a review of its use in the management of traveller’s diarrhoea. Drugs. 2005;65:1697–713.
Salix Pharmacetuicals Inc. Xifaxan® (rifaximin): US prescribing information. 2011. http://www.salix.com/assets/pdf/prescribe_info/xifaxan-pi.pdf. Accessed 30 June 2014.
Norgine Ltd. Targaxan 550 mg film-coated tablets: summary of product characteristics. 2013. http://www.medicines.org.uk/emc/medicine/27427/SPC/TARGAXAN+550+mg+film-coated+tablets/. Accessed 30 June 2014.
Blandizzi C, Viscomi GC, Marzo A, et al. Is generic rifaximin still a poorly absorbed antibiotic? A comparison of branded and generic formulations in healthy volunteers. Pharmacol Res. 2014;85:39–44.
Viscomi GC, Campana M, Barbanti M, et al. Crystal forms of rifaximin and their effect on pharmaceutical properties. CrystEngComm. 2008;10(8):1074–81.
Flamm SL. Rifaximin treatment for reduction of risk of overt hepatic encephalopathy recurrence. Ther Adv Gastroenterol. 2011;4(3):199–206.
Descombe JJ, Dubourg D, Picard M. Pharmacokinetic study of rifaximin after oral administration in healthy volunteers. Int J Clin Pharmacol Res. 1994;14:51–6.
Golden PL, Pieniaszek HJ, Forbes WP. Steady-state rifaximin pharmacokinetics in patients with chronic liver disease and hepatic encephalopathy [abstract no. 1932]. Hepatology. 2011;54:1270A–1A.
Pentikis HS, Connolly M, Trapnell CB, et al. The effect of multiple-dose, oral rifaximin on the pharmacokinetics of intravenous and oral midazolam in healthy volunteers. Pharmacotherapy. 2007;27(10):1361–9.
Trapnell CB, Connolly M, Pentikis H. Absence of effect of oral rifaximin on the pharmacokinetics of ethinyl estradiol/norgestimate in healthy females. Ann Pharmacother. 2007;41:222–8.
Bass NM, Mullen KD, Sanyal A, et al. Rifaximin treatment in hepatic encephalopathy. N Engl J Med. 2010;362(12):1071–81.
Sanyal A, Younossi ZM, Bass NM, et al. Randomised clinical trial: rifaximin improves health-related quality of life in cirrhotic patients with hepatic encephalopathy: a double-blind placebo-controlled study. Aliment Pharmacol Ther. 2011;34(8):853–61.
Berni E, Bannister C, Poole C, et al. The first evaluation of the relationship between the Chronic Liver Disease Questionnaire and the EQ-5D Index in hepatic encephalopathy patients treated with rifaximin-α [poster no. PWE-154]. Meeting of the British Society of Gastroenterologists; 16–19 Jun 2014; Manchester.
Neff GW, Barrett AC, Bortey E, et al. Efficacy and tolerability of rifaximin in hepatitis C patients with recurrent hepatic encephalopathy [abstract no. Su1300]. Gastroenterology. 2013;144(5 Suppl):S451–2.
Mullen KD, Sanyal AJ, Bass NM, et al. Rifaximin is safe and well tolerated for long-term maintenance of remission from overt hepatic encephalopathy. Clin Gastroenterol Hepatol. 2014;12(8):1390–7.
Bannister CA, Conway P, Radwan A, et al. Patients experiencing repeated episodes of hepatic encephalopathy have increasing risk of death: a post hoc analysis of rifaximin-α open label study [abstract]. British Association for the Study of the Liver Annual Meeting; 15–17 Sep 2014; Newcastle.
Bannister CA, Conway P, Radwan A, et al. Patients experiencing repeated episodes of hepatic encephalopathy have increasing risk of subsequent episodes: a post hoc analysis of rifaximin-α open label study [abstract]. United European Gastroenterology Week; 18–24 Oct 2014; Vienna.
Neff GW, Flamm SL, Mullen KD, et al. Improved outcomes in hepatic encephalopathy using rifaximin monotherapy compared to rifaximin and lactulose combination therapy [abstract no. Su1298]. Gastroenterology. 2013;144(5 Suppl):S451.
Poole CD, Conway P, Nanuwa K, et al. Cost effectiveness of rifaximin-α in the reduction of recurrence of overt hepatic encephalopathy [poster no. P451]. International Liver Congress, 49th Annual Meeting of the European Association for the Study of the Liver; 9–13 Apr 2014; London.
Neff GW, Jones M, Jonas M, et al. Lack of Clostridium difficile infection in patients treated with rifaximin for hepatic encephalopathy: a retrospective analysis. J Clin Gastroenterol. 2013;47(2):188–92.
Medicines and Healthcare products Regulatory Agency. Public Assessment Report Decentralised Procedure. Refero 550 mg film-coated tablets: procedure no. UK/H/5075/001/DC. 2012. http://www.mhra.gov.uk/SearchHelp/GoogleSearch/index.htm?q=rifaximin. Accessed 30 June 2014.
Disclosure
The preparation of this review was not supported by any external funding. During the peer review process, the manufacturer of the agent under review was offered an opportunity to comment on this article. Changes resulting from comments received were made by the authors on the basis of scientific and editorial merit. Lesley Scott is a salaried employee of Adis/Springer.
Author information
Authors and Affiliations
Corresponding author
Additional information
The manuscript was reviewed by: N. Bass, Department of Medicine, UCSF, San Francisco, CA, USA; G. Bertino, University of Catania, Hepatology Unit, Regional Reference Centre for the Treatment of Hepatitis C, Department of Medical and Paediatric Science, Catania, Italy; F. Bessone, Department of Gastroenterology and Hepatology, University of Rosario School of Medicine, Urquiza, Rosario, Argentina; J. Chang, Department of Gastroenterology and Hepatology, Singapore General Hospital, Singapore; E. Giangreco, School of Specialization of Gastroenterology, University of Catania, Catania, Italy; K. J. Simpson, Hepatology, University of Edinburgh, Edinburgh, UK.
Rights and permissions
About this article
Cite this article
Scott, L.J. Rifaximin: A Review of Its Use in Reducing Recurrence of Overt Hepatic Encephalopathy Episodes. Drugs 74, 2153–2160 (2014). https://doi.org/10.1007/s40265-014-0300-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-014-0300-y