Abstract
Continuous professional development among stakeholders involved in drug safety monitoring and surveillance is imperative in strengthening pharmacovigilance (PV) systems. The “Pharmacovigilance infrastructure and post-marketing surveillance system capacity building for regional medicine regulatory harmonization in East Africa” (PROFORMA) project aims to enhance the national PV infrastructure, post-marketing surveillance systems and clinical trial regulatory capabilities in Ethiopia, Tanzania, Kenya and Rwanda. To achieve this, training, including short-term training (STT) activities, at various levels is required. This article aims to describe the experiences of the authors during the development and implementation of STT in an attempt to improve the PV training landscape of these countries. To identify gaps, a baseline assessment of PV teaching and practices at the national medicines regulatory authorities (NMRAs) and medical universities was conducted. Five successive training sessions, tailored to each country's specific needs and regulatory environments, were conducted; three focusing on fundamental concepts in PV and two dedicated to training-of-trainers courses. The training targeted staff from PV units of the NMRAs and medical universities. Enabling participation from all four countries in the same training fostered cross-country learning and collaboration. The contribution of STT to university education and the operational methodologies within NMRAs are explored, showcasing the impact on knowledge transfer and skill development in each country. In conclusion, by investing strategically in STT activities and fostering partnerships with academic institutions and NMRAs, we demonstrated a sustainable approach to PV capacity strengthening in resource-limited settings. The success of this model underscores its potential for adoption and replication across the African continent, offering a valuable framework for strengthening drug safety regulation and ultimately protecting public health.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Short-term training activities offer a useful way to allow pharmacovigilance capacity strengthening in resource-limited settings. |
Enabling participation with academic institutions and national medicines regulatory authorities from multiple countries to participate in the same training fosters efficient cross-country learning. |
The achievements of this model demonstrate its potential for adoption and replication throughout the African continent. |
1 Introduction
Over the past decades, initiatives to increase access to safe medicines and vaccines in low- and middle income countries have been deployed [1, 2]. To ensure the monitoring of medicinal product safety after approval for marketing, pharmacovigilance (PV) infrastructures need to be in place [3]. However, every country is unique, the characteristics of their systems may vary and not all healthcare professionals and consumers are familiar with the objectives of monitoring drug safety and the procedures involved [2]. The capacity strengthening project entitled “Pharmacovigilance infrastructure and post-marketing surveillance system capacity building for regional medicine regulatory harmonization in East Africa (PROFORMA)” aims at strengthening the national PV infrastructures, post-marketing surveillance systems and clinical trial regulatory capacity in Ethiopia, Tanzania, Kenya and Rwanda to promote regional medicine regulatory harmonisation [4]. This facilitates introduction of new and safe products for the treatment of poverty-related diseases and enhances PV for mass drug administration and immunisation programmes at the national level.
To support the optimisation of PV systems, competence development and training were required. For sustainable capability building, this training was given to all stakeholders, including the staff working at medical universities and regulatory authorities. Although the participating countries had PV systems at different levels of maturity, the basic healthcare infrastructure was sufficiently similar to learn from each other [5]. This involved several strategies that included both short- and long-term training methods aimed at enhancing capacity in understanding, identifying, evaluating, preventing and managing adverse drug reactions (ADRs) for the various stakeholders.
Short-term training (STT) played a crucial role in strengthening the national PV systems by providing opportunities for healthcare professionals and regulatory staff to enhance their knowledge and skills in PV and improve the quality of ADR reporting and data collection, enabling regulatory authorities to make informed decisions about drug safety. Reflecting on our experiences of this, STT may be helpful in the development of courses for (future) healthcare professionals in similar settings and to show the advantage of close collaboration between regulatory authorities and academia. The aim of this article is to describe the development, and our experiences, of the PROFORMA STT activities over the past 5 years and to illustrate how it changed the PV training landscape in the Eastern African region.
2 Methods
The development of the STT programme is detailed, with an emphasis on the content of various training sessions and the process involved in designing the curriculum and implementation within the PROFORMA project. Achievements in the participating countries are highlighted, focusing on the contribution of the STT to PV education at universities and the operational methods within national medicines regulatory authorities (NMRAs). Additionally, the barriers and facilitators for implementing various aspects learned in the STT are discussed.
3 Short-Term Training
The STT was aimed at improving knowledge on PV in general for staff of PV units of the NMRAs and healthcare professionals who play a key role in providing information on the safety of drugs after approval for marketing. The STT was organised in collaboration with the NMRAs, universities and Pharmacovigilance Centre Lareb—the national centre for ADR reporting in the Netherlands. Staff members of the national regulatory centres and academic personnel in the participating countries received education and training, enabling them to operate and maintain all essential functions of a national PV system up to international standards in a sustainable way. Because of staff turnover, this STT by itself is not sufficient to achieve sustainability. To ensure a long-lasting effect, academic institutions were engaged, ensuring that curricula were developed for continuous training of PV methods for local healthcare professionals. The major focus of the STT was empowering participants in terms of knowledge, attitude and skills on various aspects of PV. Moreover, training-of-trainers (ToT) activities were implemented within the STT, enabling both the development of dedicated country-specific courses as well as ensuring that an adequate number of teachers are trained to deliver sustainable training to stakeholders in the future.
The training was organised and run in such a way that staff working in all four countries could participate in the same training, which also enabled cross-country learning. Such training ensures that healthcare professionals across different regions or institutions receive standardised education on PV practices and procedures. This helps in promoting consistency and coherence in reporting and monitoring ADRs and promotes regional medicine regulatory harmonisation and PV practices.
A total number of five trainings sessions were organised, comprising three that focused on basic concepts in PV and the operation of a PV unit and two involving a ToT course. The three STT sessions focussed on various topics, such as assessment of Individual Case Safety Reports, signal detection, management, regulatory decision-making and good safety communication practices. One of the ToT courses focussed on developing a country-specific course for training healthcare professionals in PV. The other focused on developing a training programme for qualified persons responsible for pharmacovigilance (QPPVs), who are responsible for supervising the PV system within a marketing authorisation holder (MAH) company and the safety of its pharmaceutical products [6]. As such, the QPPV serves as a crucial intermediary for the NMRAs. In many geographical areas (e.g. the European Union [EU], Ghana, Kenya, South Africa), the presence of a QPPV within an MAH company is mandatory [6,7,8,9]. However, this is not yet the case for every country.
The topics of the STT were defined at the start of the PROFORMA project, based on local needs and priorities of the NMRAs, and their content was decided upon in the various annual consortium meetings. Achievements were evaluated through post-training discussions during the training sessions and participant feedback and learning goals established for focusing on skill acquisition and practical application. Bloom’s taxonomy was used to develop learning objectives that describe both skills and abilities [10]. A distinction was made between learning objectives primarily focused on imparting knowledge, which were covered in the lectures, and those requiring higher levels of cognitive skills and involving a wide variety of tasks and contexts. The latter were addressed through various workshops. The following course modules were organised:
-
(A)
General aspects of PV: This comprehensive training discussed the general aspects of PV, like data-collection, assessment of reports, basic concepts of signal detection and management, communication to the general public and teaching of PV.
-
(B)
ToT for PV training: This aimed at the development of country-specific PV courses to teach methods and skills and engage stakeholders. Various approaches for delivering training were discussed, and assignments and workshops were developed. Attention was also paid to the implementation and evaluation of the courses to ensure their effectiveness in enhancing PV practices within each country. The training evaluation included a pre-test and post-test to evaluate if the knowledge and skills were sufficiently gained by participants.
-
(C)
Signal detection and management: This training focussed on various ways to detect and manage safety signals. Amongst others, differences between case-by-case and statistical signal detection and case-series analysis were discussed as well as deciding on regulatory actions. Workshops focussed on both qualitative and quantitative signal detection, causality assessment and the use of VigiLyze, the data analysis tool of the World Health Organization (WHO) collaborating centre of international drug monitoring, the Uppsala Monitoring Centre (UMC) [11].
-
(D)
Risk management and communication: Information on risk management and good safety communication practices for feedback and risk minimisation measures was provided and how these concepts can be applied. Hands-on training was provided on preparation and dissemination of safety communication, including Direct Healthcare Professional Communications (DHPCs). Finally, the strengths, weaknesses, opportunities and threats of the national risk communication strategies were discussed.
-
(E)
ToT for QPPV training: This training focussed on the development of national training for QPPVs of MAHs and PV audits. This training discussed the role and responsibilities of a QPPV, the nature and purpose of the Periodic Safety Update Report (PSUR), Periodic Benefit/Risk Evaluation Report (PBER) and risk management plans, inspections and audits. In the various workshops, country-specific QPPV training and implementation plans were developed. This training was carried out in collaboration with the Ghana Food and Drugs Authority.
Although the intention was to organise all meetings on site, due to the coronavirus disease 2019 (COVID-19) pandemic, the course modules on signal detection and management as well as the ToT QPPV training modules were organised as a teleconference. The training session on risk management and communication was partially online and partially onsite.
4 Country-Specific Achievements
A baseline assessment of PV teaching practices in the four countries uncovered distinct approaches to PV education and training. These distinctions reflected the different educational environments and institutional frameworks specific to each country. The assessment underscored the necessity for customised strategies to improve PV training and education. Details regarding the baseline assessment can be found in the electronic supplementary material for this article (see online resource 1).
Within this section, we elucidate the progress and advancements made in PV training and education in the four countries over recent years. The involvement of NMRAs and universities in the STT is outlined, and the contribution of the STT to PV education at universities and the operational methods within NMRAs is discussed more comprehensively. A summary of diverse accomplishments and contributions is presented in Table 1.
4.1 Ethiopia
In Ethiopia, the teaching methodology at baseline primarily relied on traditional approaches such as lectures and independent and collaborative learning. The School of Pharmacy at Addis Ababa University (AAU) offered clinical internships with hands-on experience. No stand-alone PV course for undergraduate pharmacy students existed, but an elective pharmacoepidemiology course included limited hours dedicated to PV. In the School of Medicine, including the Department of Dentistry, some aspects of PV and managing ADRs in clinical practice were taught.
The STT was attended by staff of AAU involved in the safety monitoring committee and the Ethiopian Food and Drug Authority (EFDA). This contributed to the inclusion of PV topics in the clinical trial Master of Science (MSc) programme of AAU, the newly approved Clinical Pharmacy PhD programme and teaching about PV in the 10-week clinical trial operation online training programme.
At the start of the PROFORMA project, the EFDA, the former Ethiopian Food, Medicine and Healthcare Administration and Control Authority (EFMHACA), was being restructured, leading to an increase in staff size and number of reports and signals to be processed. Twenty-one standard operating procedures for guiding the PV activities were developed, and training was provided for better understanding and proper implementation. Under the new PV directive, a requirement for MAHs to assign a QPPV was added. Training for QPPVs is planned to be conducted in the coming years by the national PV experts who participated in the ToT course on QPPV through the STT.
4.2 Kenya
At the start of the project, stand-alone PV courses were not yet integrated in the undergraduate programmes in the schools of Medicine, Dental Science, Pharmacy and Nursing, but a postgraduate course and a masters’ programme in PV and pharmacoepidemiology at the University of Nairobi (UON) were offered at the School of Pharmacy. Also, the Pharmacy and Poisons Board (PPB) offered an in-service module on PV, which adopted a diverse array of teaching methods, including lectures, assignments and practical work.
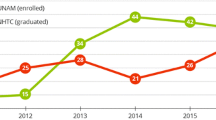
Faculty from the four schools of the College of Health Sciences (CHS) joined the PROFROMA STT, with participants being drawn from the schools of Dental Science, Nursing and Pharmacy, along with members from the Kenyatta National Hospital (KNH) and the PPB.
After the launch of the PROFORMA undergraduate PV curriculum, the School of Pharmacy introduced a module covering principles of PV in the Bachelor of Pharmacy programme offered in collaboration with the PBB. With support from the Medicines, Technologies, and Pharmaceutical Services (MTaPS) programme, the PPB in collaboration with the UON reviewed the in-service curriculum and has so far trained 4025 healthcare workers on the different modules. The PPB collaborated with the National Vaccines Immunisation programme for COVID-19 vaccine rollout, conducting webinars and training for healthcare workers, and continues such collaboration.
Members of the Pharmacovigilance Expert Review and Advisory Committee, having attended the PROFORMA STT, gained further skills that have optimised their case assessments during their quarterly meetings. While Kenya did not have a QPPV training programme at the time of the baseline assessment, the module ToT for QPPV training created a good basis for implementing this training. After additional training by the Ghana FDA in collaboration with the African Collaborating Centre, the PPB and UON developed a 2-week QPPV curriculum, which has the first cohort trained.
4.3 Rwanda
At the start of the PROFORMA project in Rwanda, PV was already integrated in the curriculum of the pharmacy department of the University of Rwanda (UR). The PROFORMA project developed an online in-service professional PV training curriculum that was integrated into the UR e-learning platform under the College of Medicine and Health Sciences. Through the collaboration of the Rwanda FDA and UR, different seminars and conferences on PV were conducted, especially targeting students in the final year of pharmacy and medicine and other health-related sciences.
Following the completion of the first STT in 2019, a series of country-specific training courses, seminars and workshops were developed to equip stakeholders involved in PV at various levels, primarily public and private health facilities (hospitals, health centres, clinics), public health programmes, academia and the national medicine regulatory authority. The training coincided with the establishment of a newly regulatory agency with a dedicated division of PV. More than 2000 health professionals were trained, and different PV structures, like the National Adverse Events Following Immunization Committee and Drugs and Therapeutics Committee, were reactivated based on the skills and competency acquired during the trainings.
The developed training activities improved vaccine safety surveillance systems also in the context of the COVID-19 pandemic. The training improved the signal detection and management processes, risk management and communication for both medicines and vaccines. The STT contributed to reactivating some PV structures, raising awareness and sustaining the PV system and increased adverse event reporting. An overview of the training activities is shown in Table 1. In addition, the national agency developed different regulations and guidelines related to PV activities, and Rwanda FDA improved and strengthened the PV processes.
4.4 Tanzania
At baseline, Tanzania utilised various theoretical and practical forms of teaching methods. The School of Pharmacy demonstrated comprehensive coverage of PV topics in its curriculum, but the schools of Dentistry, Nursing and Medicine lacked some relevant topics. The PV roadmap that provided guidance on the implementation of national PV activities at the Tanzania Medicines and Medical Device Authority (TMDA) was developed based on the gaps and challenges identified during the baseline situational analysis [5, 12]. At that time, there was no systematic pre-service training on PV.
Following the initial STT, the TMDA and Muhimbili University of Health and Allied Sciences (MUHAS) developed their own country-specific short and long training courses. For the short courses, trainers were academics from MUHAS, PV staff from the TMDA and clinicians. ToT courses enabled the creation of a pool of trainers. Short courses on PV were developed for regulatory staff, academia, healthcare workers, MAHs and QPPVs. All these training courses were conducted in collaboration between the TMDA and MUHAS. The skills, knowledge and capacity gained have contributed to several PV activities, and also enabled the TMDA to attain and maintain WHO maturity level 3.
A training curriculum was also developed for undergraduate studies, and PV modules were incorporated in the undergraduate course at MUHAS. A total of 367 students have been trained since its inception (2018–2022), and a 2-year Master of Science course for PV and pharmacoepidemiology was developed. The collaboration with experienced TMDA staff has enabled the students to have real-life knowledge and skills, and the TMDA is now one of the training sites for fieldwork.
5 Facilitators and Barriers
Within the programme, focused knowledge was imparted on a multitude of topics about PV in a short period of time. Based on the information offered in the STT, it was up to the countries themselves to determine which information could be implemented in education or the way of working within the NMRAs. For this step, different facilitators and barriers were mentioned by the countries. As an example, Tanzania mentioned that a collaborative working and planning approach had been established between the TMDA and the relevant departments responsible for teaching various PV modules at MUHAS. Additionally, the cooperation and support from the heads of various health facilities was instrumental, as they granted permission for their employees to attend the training sessions at designated centres. Lastly, the programme benefited from the involvement of experienced PV experts from the TMDA, who contributed significantly to the hands-on training, thereby enhancing the overall quality of the educational experience. Rwanda also mentioned the involvement of FDA staff, clinical staff from referral hospitals and university lecturers trained by the PROFORMA project. Another facilitator for this country was the need to fulfil the WHO key requirements for a functional PV system, which led the Rwanda FDA to establish a national PV advisory committee to support the agency in the analysis of PV reports and proper safety regulatory actions.
One of the barriers encountered in Tanzania was the lack of a well-coordinated training programme, resulting in the participation of only one department at MUHAS. Secondly, the absence of senior staff from MUHAS might have diminished the sense of confidence and seriousness among adult trainees during the training process as the participating department predominantly utilised tutorial assistants and assistant lecturers. Lastly, the proposed use of VigiMobile as a new tool for reporting adverse drug events [13] during the STT faced a hurdle, as it had not undergone testing and approval at the time the training sessions were conducted. Finally, the need for financial support was mentioned.
6 Discussion
For all the four countries participating in the PROFORMA project, STT has played a crucial role in advancing PV training. It has been instrumental in the formulation of procedures and guidelines for signal detection and management. Additionally, STT has directly or indirectly contributed to the continuous professional development of healthcare providers in the field of PV and has played a role in QPPV training in several countries. It should be noted that various training and education initiatives were already ongoing in the participating countries, among which were comprehensive ToT courses focussing on principles of PV and cohort event monitoring, specifically within the context of mass drug administration and immunisation initiatives. In addition, a short e-learning module targeting pre-service (internship students) and in-service (healthcare professionals) individuals to enhance their knowledge and skills in PV has been developed to raise awareness among healthcare professionals about the importance of PV in ensuring drug safety. Determining the specific contribution of the various short courses and ToT courses of the STT themselves is challenging and cannot always be expressed quantitatively. Nonetheless, the courses may have served as a catalyst for the organisation of subsequent courses, as shown by the activities in Tanzania, for example.
Earlier studies showed that providing targeted PV training to stakeholders was an efficient way to reach a large number of healthcare professionals and other stakeholders to disseminate knowledge about PV. Delivery of 18-month PV training and mentoring in three sub-Saharan countries (Côte d’Ivoire, Malawi and the Democratic Republic of Congo) resulted in an increase in the number and quality of reports to PV centres. In Côte d’Ivore, 80% of the reports came from trained healthcare professionals, showing the strength of this approach [14]. A more detailed analysis of the reports submitted in Malawi confirmed the impact of the training and showed a high increase in reporting after the training, as well as an improvement in the quality of the information provided [15]. Like in the PROFORMA STT, there was a strong collaboration in these countries between the regulatory authorities and universities.
For the PROFORMA STT, it was decided to provide both a theoretical background, practical exercises and workshops. This helped ensure that the information was closely aligned with practices and policies of the healthcare professionals and NMRAs, and that the knowledge transferred is directly applicable as much as possible. Education on PV for healthcare professionals in drug prescription, dispensing and administration is essential in improving the safe use of drugs. According to Herrera Comoglio, training should focus on awareness, knowledge and reporting. This holds for the training in undergraduate curricula, but also for postgraduate training as part of continuing education [16]. The finding of a low reporting rate in the neglected tropical diseases programmes in the four countries in this PROFORMA project, despite the presence of PV aspects in the programmes, seems to support this statement [17].
Knowledge of PV is important for medical practitioners, pharmacists and NMRA personnel. Established educational structures offer a foundation for incorporating PV components into educational programmes. However, it should be noted that, depending on the target audience, the level of complexity addressed in these structures may differ. The ToT modules offer the opportunity to develop tailor-made courses taking into consideration the target audience and country-specific aspects like the educational landscape and infrastructure of their respective healthcare professional programmes.
In 2016, a stakeholders’ meeting was initiated on behalf of the WHO to define the PV competencies undergraduate students need to develop and which should therefore be part of the curriculum. It stressed the importance that students should be competent in recognising, managing and preventing ADRs to improve the safe use of drugs. Five key aspects were defined, i.e. understanding the importance of PV in the context of pharmacotherapy and recognising, managing, preventing and reporting ADRs [18]. It was suggested to add these key aspects into the existing courses for medical, pharmacy, dentistry and nursing education programmes as it was expected that integration of these elements required limited time investment. These key aspects were also part of the STT organised within the PROFORMA project. In this stakeholder meeting, the collaboration between national centres of the NMRAs, universities and others to optimise the development of PV training was also stressed.
The PROFORMA project exhibits several commendable strengths of using STT. Notably, the collaboration between the participating countries in the development of teaching materials and exchanging ideas on PV enriched the diversity of educational content. Moreover, the alliance between academia and NMRAs in the development of teaching and education materials ensures a broad all-encompassing approach, incorporating both theoretical knowledge and practical insights. The use of the ToT approach in two of the modules facilitated the creation of tailor-made solutions for the specific needs of the participating countries. Aligning the content with the ideas of the WHO's stakeholder meeting reflected international standards, and incorporating Bloom's taxonomy enhances the effectiveness of the teaching methods, fostering a comprehensive understanding of the subject matter [18]. Using STT as a catalyst for developing additional studies has been shown to be a time-efficient, sustainable and cost-effective way of conveying PV knowledge. The experience of Tanzania shows that the concept of using short- and long-term courses can be extended to a national level, while the creation of a pool of potential teachers enables a large number to be reached within a relatively short timeframe. These strengths collectively contribute to the potential of STT to make a meaningful and scalable impact on education.
While the STT approach presents notable strengths, it is essential to acknowledge its inherent limitations. While the concept proves to be time effective, the requirement for both time and financial resources remains a limiting factor. Additionally, the inherent constraint of the amount of information that can be conveyed in an STT poses challenges to comprehensive knowledge transfer.
7 Conclusion
Training is a paramount factor in improving PV systems. STT sessions for NMRA staff and universities are useful for knowledge transfer and developing skills on PV activities and establishing bespoke national PV training. Collaboration between countries from similar regions allows for exchanging experiences and knowledge. Strengthening of PV systems can be done by joining efforts of all stakeholders at a national and regional level, fostering collaboration and promoting regional medicine regulatory harmonisation in Africa. By strategically investing in STT and nurturing collaborative partnerships with academic institutions and NMRAs, we have demonstrated a sustainable approach to strengthening PV capacity in the four east African countries. The success of this model highlights its potential for adoption and replication across the African continent, providing a valuable framework for enhancing drug safety regulation and safeguarding public health in sub-Saharan Africa
References
Kiguba R, Olsson S, Waitt C. Pharmacovigilance in low- and middle-income countries: a review with particular focus on Africa. Br J Clin Pharmacol. 2023;89(2):491–509.
Olsson S, Pal SN, Dodoo A. Pharmacovigilance in resource-limited countries. Expert Rev Clin Pharmacol. 2015;8(4):449–60.
Roadmap for access to medicines, vaccines and health product 2019-2023: comprehensive support for access to medicines, vaccines and other health products. World Health Organization; 2019.
Website PROFORMA. Pharmacovigilance infrastructure and post-marketing surveillance system capacity building for regional medicine regulatory harmonization in East Africa. Available from https://proforma.ki.se/#.
Barry A, Olsson S, Minzi O, Bienvenu E, Makonnen E, Kamuhabwa A, et al. Comparative assessment of the national pharmacovigilance systems in East Africa: Ethiopia, Kenya, Rwanda and Tanzania. Drug Saf. 2020;43(4):339–50.
ICH guideline Q9 on quality risk management. European Medicines Agency.
Guidelines for Qualified Person for Pharmacovigilance [press release]. Ghana Food and Drugs Authority; 2013.
Alshammari TM, Alshakka M, Aljadhey H. Pharmacovigilance system in Saudi Arabia. Saudi Pharm J. 2017;25(3):299–305.
Ampadu HH, Hoekman J, Arhinful D, Amoama-Dapaah M, Leufkens HGM, Dodoo ANO. Organizational capacities of national pharmacovigilance centres in Africa: assessment of resource elements associated with successful and unsuccessful pharmacovigilance experiences. Glob Health. 2018;14(1):109.
Adams NE. Bloom’s taxonomy of cognitive learning objectives. J Med Libr Assoc. 2015;103(3):152–3.
Lindquist M. VigiBase, the WHO global ICSR database system. Drug Inf J. 2008;42(5):10.
The National Pharmcovigilance Roadmap 2019–2023. Tanzania Medicines and Medical Devices Authority; 2021.
Adverse event reporting in the palm of your hand: Uppsala Monitoring Centre; 2024. Available from https://who-umc.org/pv-products/vigiflow/vigimobile/.
Stegmann JU, Jusot V, Menang O, Gardiner G, Vesce S, Volpe S, et al. Challenges and lessons learned from four years of planning and implementing pharmacovigilance enhancement in sub-Saharan Africa. BMC Public Health. 2022;22(1):1568.
Jusot V, Chimimba F, Dzabala N, Menang O, Cole J, Gardiner G, et al. Enhancing pharmacovigilance in sub-Saharan Africa through training and mentoring: a GSK pilot initiative in Malawi. Drug Saf. 2020;43(6):583–93.
Herrera CR. Undergraduate and postgraduate pharmacovigilance education: a proposal for appropriate curriculum content. Br J Clin Pharmacol. 2020;86(4):779–90.
Barry A, Olsson S, Khaemba C, Kabatende J, Dires T, Fimbo A, et al. Comparative assessment of the pharmacovigilance systems within the neglected tropical diseases programs in East Africa-Ethiopia, Kenya, Rwanda, and Tanzania. Int J Environ Res Public Health. 2021;18(4):1941.
van Eekeren R, Rolfes L, Koster AS, Magro L, Parthasarathi G, Al Ramimmy H, et al. What future healthcare professionals need to know about pharmacovigilance: introduction of the WHO PV core curriculum for university teaching with focus on clinical aspects. Drug Saf. 2018;41(11):1003–11.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This short-term training was part of the “Pharmacovigilance infrastructure and post-marketing surveillance system capacity building for regional medicine regulatory harmonization in East Africa” (PROFORMA) project supported by the European and Developing Countries Clinical Trials Partnership (EDCTP) 2 programme supported by the European Union (grant number CSA2016S-1618).
Conflict of Interest
Eugène van Puijenbroek is an Editorial Board member of Drug Safety. Eugène van Puijenbroek was not involved in the selection of peer reviewers for the manuscript nor any of the subsequent editorial decisions. All other authors declare no relevant conflicts of interest relevant to this article.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Code Availability
The code of the e-learning modules developed is not available.
Availability of Data and Material
Not Applicable.
Author Contributions
The design of the manuscript was determined by EvP. The baseline assessment was conducted by AB. Views from academic institutions and national medicines regulatory authorities were provided by AB, CK, LN, TDG, AF, OM, EM, MO, AG and EL. All authors contributed to manuscript drafting and revision. All authors approved the final version to be published and agreed to be accountable for all aspects of the work.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
van Puijenbroek, E., Barry, A., Khaemba, C. et al. Short-Term Training, a Useful Approach for Sustainable Pharmacovigilance Knowledge Development in Tanzania, Kenya, Ethiopia and Rwanda. Drug Saf (2024). https://doi.org/10.1007/s40264-024-01469-7
Accepted:
Published:
DOI: https://doi.org/10.1007/s40264-024-01469-7