Abstract
Introduction
A risk factor for a potentially fatal ventricular arrhythmia Torsade de Pointes is a prolongation in the heart rate-corrected QT interval (QTc) ≥ 500 milliseconds (ms) or an increase of ≥ 60 ms from a patient’s baseline value, which can cause sudden cardiac death. The Tisdale risk score calculator uses clinical variables to predict which hospitalized patients are at the highest risk for QTc prolongation.
Objective
To determine the rate of overridden QTc drug–drug interaction (DDI)-related clinical decision support (CDS) alerts per patient admission and the prevalence by Tisdale risk score category of these overridden alerts. Secondary outcome was to determine the rate of drug-induced QTc prolongation (diQTP) associated with overrides.
Methods
Our organization’s enterprise data warehouse was used to retrospectively access QTc DDI alerts presented for patients aged ≥ 18 years who were admitted to Brigham and Women’s Hospital during 2022. The QTc DDI CDS alerts were included if shown to a physician, fellow, resident, physician assistant, or nurse practitioner when entering the order in inpatient areas for patients with a length of stay of at least 2 days. Variables collected for the Tisdale calculator included age, sex, whether patient was on a loop diuretic, potassium level, admission QTc value, admitting diagnosis of acute myocardial infarction, sepsis, or heart failure, and number of QTc-prolonging drugs given to the patient.
Results
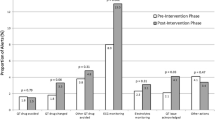
A total of 2649 patients with 3033 patient admissions had 18,432 QTc DDI alerts presented that were overridden. An average of 3 unique QTc DDI alerts were presented per patient admission and the alerts were overridden an average of 6 times per patient admission. Overall, 6% of patient admissions were low risk (score ≤ 6), 64% moderate risk (score 7–10), and 30% high risk (score ≥ 11) of QTc prolongation. The most common QTc DDI alerts overridden resulting in an diQTP were quetiapine and propofol (11%) and amiodarone and haloperidol (7%). The diQTP occurred in 883 of patient admissions (29%) and was more frequent in those with higher risk score, with 46% of patient admissions with diQTP in high risk, 23% in moderate risk, and 8% in low risk.
Conclusion
Use of the Tisdale calculator to assess patient-specific risk of QT prolongation combined with CDS may improve overall alert quality and acceptance rate, which may decrease the diQTP rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Drug-induced QTc prolongation (diQTP) was more frequent in patients who had a higher Tisdale risk score. |
Using the Tisdale calculator to assess risk of QTc prolongation combined with clinical decision support may improve alert acceptance rate, decrease diQTP rates, and improve patient safety. |
1 Introduction
The QT interval on the electrocardiogram (ECG) has gained clinical importance because a prolongation in the heart rate-corrected QT interval (QTc) ≥ 500 milliseconds (ms) or an increase of ≥ 60 ms from a patient’s baseline value is a risk factor for a potentially fatal ventricular arrhythmia known as Torsade de Pointes (TdP), which can cause sudden cardiac death [1, 2]. However, the QTc alone is a relatively poor predictor of TdP, and other clinical context such as types of medications ordered and patient-specific factors including laboratory results have been associated with QTc prolongation including female gender, age ≥ 65 years, cardiovascular history, and electrolyte imbalances [3,4,5].
Minimizing the risk for QT prolongation is important for patient safety. The American Heart Association and the American College of Cardiology Foundation published a statement about how to prevent TdP in the hospital setting by having appropriate ECG monitoring and managing QTc prolongation through minimization of QTc prolonging drugs and electrolyte replacements [6]. Most institutions utilize clinical decision support (CDS) alerts within the patient’s electronic health record (EHR), which alert providers on potential harm of QTc prolonging drug–drug interactions (DDIs) of medications being ordered for a patient [7]. The current CDS DDI alerts in the EHR are provided by medication knowledge vendors, which have a medication-related warning alert that appears from a standardized list of one medication co-ordered with another interacting medication. However, these vendor alerts generally exclude patient-specific factors and the low specificity of DDI alerts has caused alert fatigue for health care providers [8].
The Tisdale risk score calculator was designed as a new risk advisory tool to help guide decision making when managing patients at risk of TdP. It calculates a score through easily obtainable clinical variables to predict the hospitalized patients who are at the highest risk for QTc prolongation. The Tisdale risk score was validated in 2013 from a prospective observational study used to predict QTc prolongation in hospitalized patients as a potential tool to guide patient monitoring and treatment decisions [9, 10]. Variables collected for the Tisdale risk score calculator include age, sex, if a patient was on a loop diuretic medication, potassium level, admission QTc level, admitted to hospital for acute myocardial infarction, sepsis, or heart failure and the number of QTc-prolonging drugs given to the patient. A patient has a high risk for QT prolongation with a score of ≥ 11, intermediate with 7–10 and a low risk with a score of ≤ 6. The Tisdale risk score calculator can help providers estimate the risk of QT prolongation when managing patients in the inpatient setting [10,11,12,13].
Although several published research studies are available regarding methods to mitigate the risk of QTc prolongation, few studies have analyzed the use of the Tisdale calculator within the inpatient setting, and most studies utilized a modified version of the original Tisdale risk score calculator [8,9,10,11]. For example, Tan et al conducted a multicenter retrospective observational study to assess the association between a modified Tisdale QTc-risk score and inpatient mortality and length of stay in a diverse inpatient population who were prescribed medications with known risk of TdP. Findings of the study suggested that there was a strong relationship between mortality as well as longer duration of hospitalization with an increased QTc risk score [14]. Gallo et al implemented an inpatient TdP risk advisory system in 30 hospitals with CDS programed to appear when prescribers attempted to order medications with known risk of TdP in a patient with a QT risk score of ≥ 12. The investigators found that clinicians most often monitored patients by taking action to order ECGs (20%) or canceled a medication order due to the risk advisory (18%) [15].
The goal of this study was to determine if there is a need to improve QTc DDI alerts by utilizing the Tisdale risk score calculator to provide another level of support for health care providers in treatment decisions. The objective of the study was to determine the rate of overridden QTc DDI-related CDS alerts per patient admission and the prevalence by Tisdale risk score category of these overridden alerts. A secondary outcome was to determine the rate of drug-induced QTc prolongation (diQTP) associated with overrides as well as to calculate the risk score using a modified Tisdale calculator with patient information at the time the alert presented.
2 Methods
The Mass General Brigham’s Enterprise Data Warehouse (EDW) was used to retrospectively access QTc DDI alerts presented for patients aged ≥ 18 years admitted to Brigham and Women’s Hospital (BWH) during 01/01/2022–12/31/2022. Patients were included in the cohort if the QTc DDI CDS alerts were shown to a physician, fellow, resident, physician assistant, or nurse practitioner when entering the order in inpatient areas for patients with a length of stay of at least two days. This study was deemed exempt by the Mass General Brigham Institutional Review Board (2023P000243). Descriptive statistics were calculated to summarize the data.
The medication knowledge vendor integrated into BWH’s EHR responsible for providing medication-related alert warnings including drug-dose, drug-allergy, DDI and drug-disease interactions, geriatrics-based alerts, and duplicate therapy is First DataBank (FDB) (San Bruno, California, USA). The DDI medication warning alerts appear on the screen when a provider orders a new medication and there is an interaction with an active medication in the patient’s profile or an interaction with another new medication within the order entry. For example, a DDI warning between amiodarone and levofloxacin will appear on the screen stating, “The concurrent use of amiodarone with other agents that prolong the QTc may result in potentially life-threatening cardiac arrythmias, including TdP.” The provider has the option to override the warning to continue placing the order of the desired medication or can discontinue, cancel, or change the order to another medication, which is all recorded in the EDW.
Data were collected for the total number of QTc DDI alerts and override frequency. Variables collected retrospectively for the Tisdale risk score calculator included age, sex, whether a patient was on a loop diuretic, potassium level, admission QTc level, admitting diagnosis of acute myocardial infarction, sepsis, or heart failure, and number of QTc-prolonging drugs given to the patient (see Fig. 1) [11]. We used the variables that were available from the EHR. For example, the calculator does not require a patient to have an ECG on admission and can be calculated if the patient did not have an ECG on admission. If the QTc value was unknown/not documented, or was a value of less than 450 ms, the patient received a score of zero for that variable. If the patient had an ECG of ≥450 ms, the patient received 2 points for that variable. We modified the Tisdale QTc risk score calculator to also compute specifically at the time of the alert presented instead of at the time when the patient was admitted to the hospital, which affected three variables: the QTc level, potassium level, and whether a patient was on a loop diuretic. For the variable of the number of QTc-prolonging drugs given, all patients received the maximum of 6 points as patients needed to be on at least two QTc-prolonging drugs to be part of the inclusion criteria.
2.1 Definition of diQTP
The diQTP was defined as a QTc value increased ≥ 60 points from baseline or if the post-QTc value was ≥ 500 ms [16]. The diQTP was also counted if there was no baseline QTc value available, but the post-QTc value was ≥ 500 ms. The Tisdale risk score calculator used the variable of QTc value at admission. To determine if an diQTP occurred with the Tisdale risk score calculator, we defined baseline QTc as a QTc value on the day of or the day after admission. The post-QTc value was defined as any QTc value recorded ≥ 2 days since patient admission. No diQTP was defined if the post-QTc value was < 500, if the post-QTc value was < 60 points increase from baseline, if the QTc value decreased, or if the Qc value remained the same. The diQTP was considered unknown if no post-QTc value was done. For our modified risk score calculator, we used the QTc value at the time the alert presented, which may have differed from the value at admission. To determine if diQTP occurred, we defined baseline QTc value at the time of the alert presented (either the QTc value on the day the alert presented or the day before the alert presented). The post-QTc value was defined as any QTc value recorded ≥ 1 day since the date the alert presented.
3 Results
During the study period, a total of 2766 patients with 3172 admissions had 20,024 QTc DDI alerts presented. Of these, 1592 alerts were accepted (8%). The QTc DDI alerts presented and overridden totaled 18,432 alerts (92%), which consisted of 2649 patients with 3033 patient admissions. An average of 3 unique QTc DDI alerts presented and overridden per patient admission (standard deviation [SD] of 3, range of 1–44) and the alerts were overridden on average 6 times (SD of 14, range of 1–432) per patient admission. Patient sociodemographic characteristics are provided in Table 1. A total of 44% of patients were aged within the 65–84 age group, 50% male, 78% White, and 90% non-Hispanic.
When retrospectively entering the variables of each patient admission through the Tisdale risk score calculator, 6% of patient admissions were categorized as low risk (score ≤ 6, n = 182), 64% moderate risk (score 7–10, n = 1938), and 30% at high risk (score ≥ 11, n = 913) of QTc prolongation. The breakdown of each variable of the Tisdale risk score calculator is provided in Table 2. If a patient had an unknown value for a variable in the calculator, we assigned the patient zero points. For instance, on admission, 10% of patients did not have a QTc value documented (n = 289) and 1% of patients did not have a potassium value documented (n = 39).
3.1 Adverse Drug Events
A total of 883 patient admissions experienced a diQTP of a QTc value increased ≥ 60 points from baseline or if the post-QTc value ≥ 500 ms (29%) (Table 3), with 47% of diQTP in all patient admissions in the high-risk category, 51% in the moderate-risk category, and 2% in the low-risk category. Of the 883 patients, the QTc value increased ≥ 60 points from baseline or post-QTc value increased to ≥ 500 ms for 39% patients who experienced diQTP and for 61% patients who had diQTP where there was no baseline QTc value available but the post-QTc value was ≥ 500 ms.
The most common QTc DDI medication combination alerts overridden that resulted in diQTP (Table 4) were quetiapine and propofol (11%), amiodarone and haloperidol (7%), propofol and haloperidol (6%), methadone and quetiapine (5%), and amiodarone and fluconazole (4%).
3.2 Modified QTc Risk Score at the Time of Alert
A modified QTc risk score was also calculated specifically at the time of the alert, compared to the traditional Tisdale risk score, which is primarily based on patient admission information. The only variables modified included the QTc value, potassium value, and whether a patient was on a loop diuretic at the time the alert presented. There were a total of 18,432 QTc DDI alerts presented that were overridden for the 2649 patients with 7462 dates at which the alerts were presented in the patient encounters (see Fig. 2). When entering the variables through the modified QTc risk score calculator, 14% of patient admissions were categorized as low risk (score ≤ 6, n = 1005), 65% moderate risk (score 7–10, n = 4873), and 21% high risk (score ≥ 11, n = 1584) of QTc prolongation. In the modified QTc risk score calculator at the time the alert generated, 5% of patients did not have a QTc value documented (n = 339) and 1% did not have a potassium value documented (n = 41).
When comparing the standard Tisdale risk score calculator and the modified calculator, there was no change in the risk category of low, moderate, and high for the majority of alerts (67%). Furthermore, there was no change in diQTP findings for the majority of alerts (77%) when comparing the Tisdale risk calculator and the modified version. While the risk category did change for 2447 alerts presented for patient encounters (33%) when using the modified risk calculator (increasing risk for 23% of alerts and decreasing risk for 10%), nevertheless for 1848 alerts presented for patient encounters, the diQTP status did not change even though their risk changed (75%).
4 Discussion
We evaluated the potential improvement of QTc risk prediction with the Tisdale calculator in a population of patients admitted to the hospital over a one-year period with one or more QTc alerts. We found, as have others, that patient-specific risk factors are more predictive of QTc prolongation and TdP than using medication lists or ECG QTc values alone [16,17,18]. However, the typical CDS DDI alerts in the EHR provided by medication knowledge vendors focus only on medication lists and result in alert fatigue, leading to alerts being overridden for most of the time. The Tisdale calculator enabled risk scores of QTc prolongation to be computed for patients using clinical variables and can be used to provide another level of support for health care providers in treatment decisions and to decrease alert fatigue. A QTc risk score could be automated and built into CDS to continuously update the patient’s risk throughout their hospital encounter. While there was not much difference associated with modifying the Tisdale risk score calculator to use the data at the time of the alert, this is technically easy to do and should probably be implemented in this way.
Previous studies, such as one conducted by Van der Sijs et al, evaluated whether physicians who overrode QTc-related DDI alerts subsequently requested ECGs and if those ECGs had clinically significant QTc prolongation [19]. That study found that 33% of patients with overridden alerts had an ECG recorded within the past month and among the cases of patients with ECGs before and after the override, 31% showed clinically relevant QTc prolongation and were thus at increased risk of cardiac arrythmias [19]. Our study similarly found 29% of patient encounters had diQTP suggested by the Tisdale risk score calculator and 32% through the modified risk score calculator. Furthermore, Stettner et al performed a retrospective quasi-experimental study with a customized QTc interval CDS alert based on the Tisdale risk score calculator implemented in the EHR for hospitalized patients [2]. While 19% of patients each in the pre- and post-implementation group developed QTc prolongation, the odds of an action taken post-implementation were significantly higher. There was also a decrease in total orders for QTc prolonging medications, indicating the effectiveness of the customized CDS approach instead of the current standardized vendor approach [2]. Similar to our findings, by using the Tisdale risk score calculator, patient exposure to QTc prolonging medications may be reduced without increasing the rate of QTc prolongation, emphasizing the benefits of a validated risk score with CDS strategy over a traditional vendor-based approach. Further research would be helpful to confirm the effectiveness of this approach as well as focus on long-term outcomes and integration of such tools in routine clinical practice.
In the future, another approach would be to leverage artificial intelligence to make predictions regarding which patients are likely to have issues. This could allow consideration of large numbers of factors. It might also be possible to specifically predict development of torsade itself, which would require very large datasets. For example, Simon et al studied machine learning techniques in EHR data to identify an integrated risk-prediction model to predict risk of diQTP [20].
4.1 Limitations
The study was retrospective so the Tisdale risk score calculator and modified risk score calculator could not be used in real time. Another issue is that it is difficult to fully understand why a provider may have overridden an alert. It may be that the provider had information not available to the reviewer. We evaluated alerts that were documented during an inpatient hospitalization but not every patient had both a pre- and post-pharmacotherapy ECG available from the EHR. Specifically, 447 patients (15%) did not have an ECG either before and/or after the patient was admitted so it was unknown if those patients experienced diQTP. The timing of the ECG or repeat ECGs may have been based on when the provider was rounding on the patient or when the nurse was available to check the ECG, and not necessarily at the drug’s peak concentration of when QTc may be most prolonged. The study focused on diQTP and did not evaluate clinical outcomes of patients. We also only used the patient’s QTc values from the ECG and did not look at baseline QRS complex data. We did not follow up on patients once discharged where it was likely that the patient continued to take the medication and could have developed diQTP post-discharge. The study was conducted at a single academic medical center so the results may not be generalizable to other settings. We did not assess if the medications presented in the alert were chronic versus new medications. The Tisdale calculator has been validated in the cardiac critical care setting, but other QTc risk score calculators exist such as RISQ-PATH score, which incorporates other variables not in the Tisdale calculator such as smoking status, body mass index, hypertension, hypocalcemia, arrythmia, existing prolonged QTc, thyroid disturbances and more [21, 22]. Finally, we did not exclude DDI QTc alerts for patients for which calculation of accurate QTc may be challenging; for example, those with ventricular pacemakers, as has been done in some other studies [4, 12].
5 Conclusion
We evaluated QTc DDI alerts and found that over 90% were overridden. The constant over-alerting emphasizes the need to improve the design of medication-related CDS alerts associated with DDIs to improve upon medication safety. The use of the Tisdale risk score calculator to assess risk of QTc prolongation combined with CDS may improve overall alert quality and acceptance rate, which may decrease patient diQTP rates and improve patient safety.
References
Al-Khatib SM, LaPointe NMA, Kramer JM, et al. What clinicians should know about the QT interval. JAMA. 2003;289(16):2120–7. https://doi.org/10.1001/jama.289.16.2120.
Stettner S, Adie S, Hanigan S, et al. Effect of replacing vendor QTc alerts with a custom QTc risk alert in inpatients. Appl Clin Inform. 2022;13(1):19–29. https://doi.org/10.1055/s-0041-1740483.
Grindrod KA, Nagge J. Simplifying QT prolongation for busy clinicians. Can Fam Physician. 2019;65(4):268–70.
Noel ZR, See VY, Flannery AH. Walk the line-the importance of well-informed interpretation of QT prolongation. Ann Pharmacother. 2021;55(1):123–6. https://doi.org/10.1177/1060028020934718.
Khatib R, Sabir FRN, Omari C, Pepper C, Tayebjee MH. Managing drug-induced QT prolongation in clinical practice. Postgrad Med J. 2021;97(1149):452–8. https://doi.org/10.1136/postgradmedj-2020-138661. (Epub 2020 Oct 29).
American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology; Council on Cardiovascular Nursing; American College of Cardiology Foundation. Drew B J, Ackerman M J, Funk M. Prevention of Torsade de Pointes in hospital settings: a scientific statement from the American Heart Association and the American College of Cardiology Foundation. J Am Coll Cardiol. 2010;55(09):934–947.
Schwartz PJ, Woosley RL. Predicting the unpredictable: drug-induced QT prolongation and Torsades de Pointes. J Am Coll Cardiol. 2016;67(13):1639–50. https://doi.org/10.1016/j.jacc.2015.12.063.
Muylle KM, van Laere S, Pannone L, et al. Added value of patient- and drug-related factors to stratify drug–drug interaction alerts for risk of QT prolongation: development and validation of a risk prediction model. Br J Clin Pharmacol. 2023;89(4):1374–85. https://doi.org/10.1111/bcp.15580.
Su K, McGloin R, Gellatly RM. Predictive validity of a QTc interval prolongation risk score in the intensive care unit. Pharmacotherapy. 2020;40(6):492–9. https://doi.org/10.1002/phar.2400.
Tisdale JE, Jaynes HA, Kingery JR, et al. Clinician responses to a clinical decision support advisory for high-risk torsade’s de pointes. JAMA. 2013;6(4):479–87.
Tisdale JE, Jaynes HA, Kingery JR, et al. Development and validation of a risk score to predict QT interval prolongation in hospitalized patients [published correction appears in Circ Cardiovasc Qual Outcomes. 2013 Nov;6(6):e57]. Circ Cardiovasc Qual Outcomes. 2013;6(4):479–487. https://doi.org/10.1161/CIRCOUTCOMES.113.000152
Tisdale JE, Jaynes HA, Kingery JR, et al. Effectiveness of a clinical decision support system for reducing the risk of QT interval prolongation in hospitalized patients [published correction appears in Circ Cardiovasc Qual Outcomes. 2014 Nov;7(6):981]. Circ Cardiovasc Qual Outcomes. 2014;7(3):381–390. https://doi.org/10.1161/CIRCOUTCOMES.113.000651
Tisdale JE. Drug-induced QT interval prolongation and torsades de pointes: Role of the pharmacist in risk assessment, prevention and management. Can Pharm J (Ott). 2016;149(3):139–52. https://doi.org/10.1177/1715163516641136.
Tan MS, Heise CW, Gallo T, et al. Relationship between a risk score for QT interval prolongation and mortality across rural and urban inpatient facilities. J Electrocardiol. 2023;77:4–9. https://doi.org/10.1016/j.jelectrocard.2022.11.008.
Gallo T, Heise CW, Woosley RL, et al. Clinician responses to a clinical decision support advisory for high risk of Torsades de Pointes. J Am Heart Assoc. 2022;11(11): e024338. https://doi.org/10.1161/JAHA.122.024338.
Vandael E, Vandenberk B, Vandenberghe J, et al. Risk factors for QTc-prolongation: systematic review of the evidence. Int J Clin Pharm. 2017;39(1):16–25.
Woosley RL, Heise CW, Gallo T, Tate J, Woosley D, Romero KA. QTdrugs List. Oro Valley, AZ: AZCERT, Inc. http://www.CredibleMeds.org. Accessed 28 Nov 2023.
Riad FS, Andrew M, Davis AM, et al. Drug-induced QTc prolongation. Am J Cardiol. 2017;119(2):280–3.
van der Sijs H, Kowlesar R, Klootwijk AP, Nelwan SP, Vulto AG, van Gelder T. Clinically relevant QTc prolongation due to overridden drug–drug interaction alerts: a retrospective cohort study. Br J Clin Pharmacol. 2009;67(3):347–54. https://doi.org/10.1111/j.1365-2125.2008.03357.x.
Simon ST, Mandair D, Tiwari P, Rosenberg MA. Prediction of drug-induced long QT syndrome using machine learning applied to harmonized electronic health record data. J Cardiovasc Pharmacol Ther. 2021;26(4):335–40. https://doi.org/10.1177/1074248421995348.
Newell B, Wirick N, Rigelsky F, Migal K. Implementation of a pharmacist monitoring process for patients on QTc prolonging antibiotics: a pilot study. Hosp Pharm. 2021;56(6):772–6. https://doi.org/10.1177/0018578720965429.
Vandael E, Vandenberk B, Vandenberghe J, Van den Bosch B, Willems R, Foulon V. A smart algorithm for the prevention and risk management of QTc prolongation based on the optimized RISQ-PATH model. Br J Clin Pharmacol. 2018;84(12):2824–35. https://doi.org/10.1111/bcp.13740.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of interest
Dr. Bates reports grants and personal fees from EarlySense, personal fees from CDI Negev, equity from ValeraHealth, equity from Clew, equity from MDClone, personal fees and equity from AESOP, personal fees and equity from Feelbetter, equity from Guided Clinical Solutions, and grants from IBM Watson Health, outside the submitted work. Dr. Bates has a patent pending (PHC-028564 US PCT), on intraoperative clinical decision support. Dr. Bates is the Editor-in-Chief of the Journal of Patient Safety. Dr. Bates was not involved in the selection of peer reviewers for the manuscript nor any of the subsequent editorial decisions. Other authors have no conflict of interest that are relevant to the content of this study.
Ethics approval
This study was deemed exempt by the Mass General Brigham Institutional Review Board (2023P000243) as the study involved only information collection and analysis of identifiable health information for the purposes of secondary research for which consent is not required.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Data of the study is restricted and cannot be shared openly due to the sensitive protected health information which cannot be anonymized including patient identifiers such as birth dates, admission dates and discharge dates.
Code availability
Not applicable.
Authors contributions
All authors contributed to the study conception; design; and acquisition, analysis, or interpretation of the data. RLW, DLS, MGA, and DWB were responsible for study conception or design. RLW, DLS, and JF did the data cleanup and analysis. RLW, MGA, DLS, AYH, and DWB were responsible for the first draft of the manuscript with all authors reviewing the draft and providing critical feedback. All authors contributed to and approved the final manuscript.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wasserman, R.L., Seger, D.L., Amato, M.G. et al. A Calculated Risk: Evaluation of QTc Drug–Drug Interaction (DDI) Clinical Decision Support (CDS) Alerts and Performance of the Tisdale Risk Score Calculator. Drug Saf (2024). https://doi.org/10.1007/s40264-024-01466-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s40264-024-01466-w