Abstract
Background and Objective
Prior molecular modelling analysis identified several medicines as potential inhibitors of glutathione peroxidase 1 (GPx1) which may contribute to development or progression of chronic obstructive pulmonary disease (COPD). This study investigates 40 medicines (index medicines) for signals of COPD development or progression in a real-world dataset.
Methods
Sequence symmetry analysis (SSA) was conducted using a 10% extract of Australian Pharmaceutical Benefits Scheme (PBS) claims data between January 2013 and September 2019. Patients must have been initiated on an index medicine and a medicine for COPD development or progression within 12 months of each other. Sequence ratios were calculated as the number of patients who initiated an index medicine followed by a medicine for COPD development or progression divided by the number who initiated the index medicine second. An adjusted sequence ratio (aSR) was calculated which accounted for changes in prescribing trends. Adverse drug event signals (ADEs) were identified where the aSR lower 95% confidence interval (CI) was greater than 1.
Results
Twenty-one of 40 (53%) index medicines had at least one ADE signal of COPD development or progression. Signals of COPD development, as identified using initiation of tiotropium, were observed for atenolol (aSR 1.32, 95% CI 1.23–1.42) and naproxen (aSR 1.14, 95% CI 1.06–1.23). Several signals of COPD progression were observed, including initiation of fluticasone propionate/salmeterol following initiation of atenolol (aSR 1.44, 95% CI 1.30–1.60) and initiation of aclidinium/formoterol following initiation of naproxen (aSR 2.21, 95% CI 1.34–3.65).
Conclusion
ADE signals were generated for several potential GPx1 inhibitors; however, further validation of signals is required in large well-controlled observational studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Twenty-one of 40 (53%) medicines with potential to inhibit GPx1 as identified by our prior molecular modelling analysis were associated with adverse drug event signals of COPD development or progression in real-world data. |
Atenolol, naproxen, cefuroxime, ibuprofen and nicotine were associated with multiple COPD adverse drug event signals. |
The SSA design may be useful for screening real-world data to identify safety signals of medicines identified in molecular modelling as medicines that may cause ADEs. |
1 Introduction
Chronic obstructive pulmonary disease (COPD) is an insidious and incurable lung disease characterised by airflow limitation that is not fully reversible and symptoms such as difficulty breathing, cough and sputum production [1]. The prevalence of COPD is estimated to be 13% worldwide, with approximately 1 in 20 Australians over the age of 45 years having COPD [2, 3]. COPD is the fifth leading cause of death in Australia and the third leading cause of death worldwide [2, 4]. Commonly prescribed medications may affect lung function and contribute to the development or progression of COPD [5]. Whilst this is known for some medications, such as opioids which can cause respiratory depression, beta-blockers that can cause bronchospasm, abatacept may worsen respiratory disease and ticagrelor can cause dyspnoea, it is less well known whether other commonly prescribed medications may contribute to development or progression of COPD because of undetermined mechanisms of these effects and limited studies in large populations [6,7,8,9,10].
Inhaled environmental pollutants such as dust and tobacco smoke can increase oxidative stress, resulting in the development and progression of lung conditions such as COPD [11, 12]. Moreover, COPD is also characterised by low activity of an antioxidant enzyme glutathione peroxidase 1 (GPx1) [13,14,15]. GPx1 usually protects the lungs from damage caused by free radicals; however, people with COPD are more susceptible to the effects of oxidative stress due to low enzyme activity. Medications have the potential to inhibit GPx1 activity, further lowering enzyme activity, worsening COPD symptoms and contributing to disease progression [16]. Our previous analysis, which used computational molecular modelling analyses, highlighted several commonly prescribed medications that could inhibit GPx1 and worsen COPD [17].
Currently, it is not clear whether use of medicines that may inhibit GPx1 can lead to development or progression of COPD. However, administrative claims data can be used to investigate and detect adverse events associated with COPD development or progression and the use of the medicines identified as potential inhibitors in our prior analysis. One method that can be used to analyse administrative claims data is sequence symmetry analysis (SSA). SSA uses the dispensing of medicines as a surrogate measure of an adverse drug event (ADE) occurring [18]. Previously, sequence symmetry analysis (SSA) has been validated for medication safety signal detection and showed moderate sensitivity and high specificity for detecting ADE signals [18]. SSA is powered to detect rare adverse events and those that occur after long-term exposure, which is beneficial when analysing an insidious condition such as COPD [18]. This method has been shown to have comparable signal detection properties to common ADE signal detection techniques such as disproportionality analyses [19]. SSA has previously been utilised to confirm ADE signals such as amiodarone causing hypothyroidism, the risk of Clostridium difficile infection following prescription of proton pump inhibitors and also highlighted new signals between common medicines and heart failure [18, 20, 21].
This study aimed to evaluate whether initiation of 40 common prescription medications, previously identified in the literature as potential GPx1 inhibitors, were associated with signals of an increased risk of (1) development or (2) progression of COPD.
2 Methods
2.1 Dataset
A 10% extract of the Pharmaceutical Benefits Scheme (PBS) claims data was provided by Services Australia which included data from 1 January 2013 to 30 September 2019. To maintain the privacy of patients and health professionals, all dates in the data were offset by 0–14 days plus or minus the actual date. Medicines in the database were coded using Anatomic and Therapeutic Chemical (ATC) classification codes and PBS item codes [22, 23].
The analysis included people 45 years or older to minimise inclusion of patients with asthma which is often diagnosed earlier in life. COPD is usually only diagnosed once airway obstructive becomes prominent and begins to significantly impact daily activities [2, 24, 25]. Limiting the analysis to patients over 45 years of age also provided more confidence that people were dispensed these medications for COPD rather than other respiratory conditions. Each unique patient served as their own control, therefore age, sex and other medical conditions were accounted for and were not explicitly required for the analysis [19].
2.2 Statistical Methods
The SSA methodology was implemented as previously described by Lai et al. [18] and Janetzki et al. [26] for adverse event signal detection. Briefly, SSA aims to detect asymmetry between the initiation of two medicines. If a medicine is commonly initiated after another, this could be a sign that the first medicine is causing an adverse effect which is treated by the subsequent medication. In SSA, one of the medicines is designated as the index medicine and another as the outcome medicine. The index medicine is the medicine under investigation for causing an adverse event and the outcome medicine is a surrogate marker for the outcome of interest.
2.3 Implementation of Methodology
SSA was utilized to investigate the association between the initiation of 40 prescription medications and (1) the initiation of a medication for treatment of COPD (as a surrogate measure for COPD development) or (2) the initiation of a medication that indicates progression of COPD.
2.3.1 Index Medicines
The index medicines of interest were 40 medications that were selected from our previous molecular modelling analysis. These medicines were selected based on their potential ability to inhibit GPx1, as demonstrated in either ligand and/or structure-based in silico modelling by ranking within the top 150 molecules in either analysis in the prior study [17]. They were also selected based on their availability on prescription in Australia and clinical interest (that is, if a signal is detected, would there be potential for clinical implications). Medicines without at least one oral formulation available on the PBS were not considered for analysis to minimise misclassification of prevalent and incident users of index medicines. Medicines which were available primarily over the counter were also excluded (such as acetylsalicylic acid, also known as aspirin). Moreover, medicines used infrequently or as necessary were also excluded, as the dispensing date may not be an appropriate indicator of when the patient used the medication. Candidate index medicines of interest were then mapped to their relevant ATC and PBS item codes using the PBS Item Drug Map version October 2019 [22, 23]. A full list of included medicines and their respective ATC codes and PBS item codes is listed in Online Resource 1.
2.3.2 Outcome Medicines
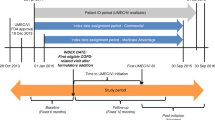
COPD is managed in Australia in a stepwise manner, as described in Fig. 1, and is guided by medicine subsidy [27]. Development and progression of COPD in this study were considered as separate outcomes as defined below.
COPD management begins with patients being initiated on a short-acting reliever to be used when required for symptoms of dyspnoea. At the same time, or if still symptomatic, patients will be initiated on a long-acting bronchodilator (LABD), either a long-acting muscarinic antagonist (LAMA) or a long-acting beta2 agonist (LABA) (this denotes the second step of management). As short-acting relievers are subsidised via the PBS for any indication and use is sporadic, it is it difficult to determine whether treatment is being initiated or continued. Here, initiation of a LABD has been used as a surrogate marker for (1) COPD development as these medications are used daily for symptom and disease control in the second step of COPD management.
Escalation in therapy by prescription of subsequent inhaled medication beyond the second step of COPD management marks (2) progression of COPD. If the patient is still symptomatic and escalation of therapy is required, usually a patient would be switched to dual combination therapy of LAMA/LABA (this denotes the third step of management). If the patient remains symptomatic and shows signs of clinical progression, the patient is usually switched to an inhaled corticosteroid (ICS) and LABA combination with concomitant LAMA therapy (this denotes the fourth step of management). Note, some medicines on the PBS are available as ‘authority required (streamlined)’. Prescribers can provide access to these medications by selecting the correct item and corresponding streamline authority number without requiring further approval from Services Australia. Streamline authority codes for ICS/LABAs provide access to these medicines for specific conditions such as COPD or asthma. Streamline authority codes were implemented in the third quarter of 2018 for ICS/LABA combination therapies. Prior to this date, it could not be determined whether the patient was prescribed the therapy for COPD or asthma. Consequently, in this analysis a history of tiotropium (PBS item code 10509D or 08626B) was used to identify patients with COPD in the study period.
If further escalation of therapy is required or simplification of therapy is desirable, patients can be switched to triple therapy combinations of ICS/LAMA/LABA in one formulation.
Table 1 lists each medicine or multiple ingredient inhaler therapy utilized as the ‘outcome medicine’ in this analysis.
To identify potential COPD adverse drug event (ADE) signals, causal and non-causal groups were generated to reflect the sequence in dispensings of the index medicine or COPD outcome medicine. The index medicine or COPD outcome medicine were required to be initiated within 12 months of each other to be included in the analysis. The causal group included patients who initiated on an index medicine (Online Resource1) and were subsequently initiated on a COPD outcome medicine indicating either COPD development or progression depending on the outcome medicine (Table 1). The index date of a medicine was defined as the date that the medicine was first ever dispensed to the patient. At least 12 months of observation period was required (within the designated study period) prior to the first ever dispensing of the medication. Once initiation index dates were determined, we restricted our analyses to those index events that occurred within 12 months of each other [28]. Then, the sequence of those events were determined, that is the number of patients with a potential GPx1 inhibitor occurring before a COPD medicine (causal events) and the number with a COPD medicine before a potential GPx1 inhibitor (non-causal sequences). SSA allows for estimation of risk by comparing the ratio of causal to non-causal patient groups by calculation of crude sequence ratios. Crude sequence ratios (cSRs) were calculated as the causal group divided by the non-casual group as outlined in the equation below.
where initiation of COPD outcome medicines increases after the initiation of an index medicine, this is indicative of a positive ADE association and increased risk of developing COPD or experiencing progression after the initiation of the index medicine.
Changes in prescribing trends over time were accounted for by calculating the null-effect sequence ratio (nSR) and subsequent calculation of adjusted sequence ratios (aSRs) with 95% confidence intervals (CIs) as previously described elsewhere [18, 28]. An aSR with lower 95% confidence interval (CI) greater than 1 indicated a potential COPD ADE signal as the outcome medicine was more commonly initiated, subsequent to the index medicine compared with the outcome medicine being initiated prior to the index medicine.
All statistical analyses in this study utilized SAS software version 9.4.
3 Results
Twenty-one of 40 (53%) medicines of interest had at least one ADE signal (Table 2).
The highest aSR was observed for acetazolamide and tiotropium/olodaterol; however, the study population (n = 26) was small (aSR 4.83, 95% CI 2.31–10.1, Online resource 8). Sixteen of 40 (40%) of medicines had at least one ADE signal for development of COPD as indicated by initiation of a long-acting bronchodilator. During the study period, most patients (54,844) were initiated on tiotropium. Less patients were initiated on any other LAMA (4996 for glycopyrronium, 4614 for umeclidinium and 4590 for aclidinium) or LABA (7282 for indacaterol).
Figure 2 shows a single SSA analysis for the association between commencing atenolol and tiotropium (aSR 1.32, 95% CI 1.23–1.42). The results for index medicines with five or more ADE signals (aSR 95% lower CI > 1) are shown in Figs. 3, 4 and 5. The results for each index medicine are available in the Online Resources.
Initiation of atenolol was associated with 32% increased risk of initiation of tiotropium (study population = 1604, aSR 1.32 95% CI 1.23–1.42, Fig. 3). Figure 2 shows that commencing tiotropium was more common after commencing atenolol rather than commencing tiotropium then atenolol. Moreover, the sequence of tiotropium after initiating atenolol appears to be sustained over the subsequent weeks (Fig. 3). ADE signals were observed for atenolol and each long-acting bronchodilator except umeclidinium, demonstrating a possible association between atenolol and the development of COPD (Fig. 3).
ADE signals of COPD progression were also observed for atenolol and glycopyrronium/indacaterol (aSR 1.74, 95% CI 1.16–2.63) and fluticasone propionate/salmeterol (aSR 1.44, 95% CI 1.30–1.60), demonstrating a possible increased risk of both development and progression of COPD with use of atenolol at the population level.
Five COPD ADE signals were observed for naproxen (Fig. 4). Two signals were observed for development of COPD between the most commonly dispensed long-acting muscarinic antagonist tiotropium (aSR 1.14, 95% CI 1.06–1.23) and the long-acting beta2 agonist indacaterol (aSR 1.27, 95% CI 1.05–1.55). Three signals were observed for progression of COPD. The greatest COPD progression ADE signal for naproxen was observed with aclidinium/formoterol (aSR 2.21, 95% CI 1.34–3.65).
Five COPD ADE signals were also observed with initiation of nicotine (Fig. 5). Two ADE signals for the development of COPD were observed with initiation of the long-acting muscarinic antagonist umeclidinium (aSR 1.26, 95% CI 1.00–1.57) and the long-acting beta2 agonist indacaterol (aSR 1.31, 95% CI 1.13–1.52). Three COPD ADE signals were identified between nicotine and COPD progression. Two signals were observed for initiation of LAMA/LABA combinations, glycopyrronium/indacaterol (aSR 1.32, 95% CI 1.11–1.57) and tiotropium/olodaterol (aSR 1.29, 95% CI 1.10–1.53). Another ADE signal was observed with the triple therapy combination of fluticasone furoate/umeclidinium/vilanterol (aSR 1.48, 95% CI 1.18–1.85).
Cefuroxime and ibuprofen were both associated with four COPD ADE signals. Three ADE signals were observed for development of COPD with initiation of cefuroxime as indicated by the initiation of tiotropium, glycopyrronium or indacaterol (see Online Resources). Cefuroxime was also associated with increased risk of COPD progression as indicated by initiation of the LAMA/LABA combination glycopyrronium/indacaterol (aSR 1.21, 95% CI 1.02–1.44).
Ibuprofen was associated with risk of both COPD development and progression. Two ADE signals were observed for the development of COPD as indicated by initiation of either tiotropium or glycopyrronium (see Online Resources). Two ADE signals were also observed for progression of COPD as indicated by the initiation of either the ICS/LABA combination of budesonide/formoterol or fluticasone propionate/salmeterol.
Strong positive ADE signals (aSR lower 95% CI > 1) were also identified for COPD development (as indicated by initiation of the most commonly dispensed LAMA, tiotropium) following initiation of acamprosate, mycophenolate, rizatriptan, gemfibrozil and methyldopa. Moreover, strong positive ADE signals (aSR lower 95% CI > 1) were identified for COPD progression (as defined by the initiation of a combination inhaler) following initiation of acamprosate, baclofen, rizatriptan, mesalazine, sodium valproate, acetazolamide, captopril, furosemide, labetalol and mefenamic acid.
4 Discussion
Initiation of atenolol, a cardioselective beta blocker, was associated with an increased risk of starting four of the long-acting bronchodilators (tiotropium, glycopyrronium, aclidinium or indacaterol, risk 32%, 51%, 62% and 32%, respectively) which may indicate that atenolol is associated with development of COPD. A temporal association between atenolol and tiotropium could be explained by beta-blocker-induced bronchospasm or bronchoconstriction [29]. However, Fig. 2 demonstrates that the sequence of initiating tiotropium after initiating atenolol is sustained over several weeks subsequent to initiating atenolol, rather than demonstrating a temporal association with first prescription of atenolol.
Atenolol may increase airways resistance and precipitate bronchospasm and wheezing due to beta-adrenergic blockade, and the product information indicates that atenolol is contraindicated in patients with a history of airway obstruction or bronchospasm [30]. However, in practice, prescription of cardioselective beta blockers, such as atenolol, is preferred in patients with respiratory conditions compared with non-selective beta blockers due to their antagonistic effects on beta2 adrenergic receptors in the bronchi [31, 32]. Despite this, atenolol may impair lung function and induce bronchoconstriction, particularly in patients with chronic bronchitis or asthma, but also suggested by positive ADE signals in this study [33, 34]. This may in part be due to beta-adrenergic receptor blockade or it could also be due to pharmacological mechanisms such GPx1 inhibition [17].
Non-steroidal anti-inflammatory drugs (NSAIDs) including naproxen and ibuprofen are associated with an increased risk of bronchospasm which may be a symptom of COPD [9]. Use of NSAIDs has previously been associated with prolonged and complicated cases of pneumonia which is a complication and sign of progression of COPD [35]. In this study, naproxen was associated with increased risk of initiating tiotropium or indacaterol, indicating possible development of COPD, and aclidinium/formoterol and fluticasone proportionate/salmeterol, indicating progression of COPD (Fig. 4). Whilst the product information for naproxen lists dyspnoea, pulmonary oedema, asthma and bronchospasm as adverse reactions for this medication in patients with a history of asthma, allergic disease or aspirin sensitivity, another possible pharmacological explanation for the ADE signal here is that naproxen has been shown to inhibit glutathione peroxidase (GPx), an antioxidant enzyme involved in the regulation of oxidative stress, which may further impair lung function [30, 36]. The positive ADE signals in this study provide evidence that an ADE could be occurring at the population level.
Initiation of ibuprofen was also associated with increased risk of initiating tiotropium or glycopyrronium, indicating COPD development, and budesonide/formoterol or fluticasone propionate/salmeterol, indicating COPD progression. Previous research has highlighted that administration of ibuprofen may benefit patients with lung conditions due to its anti-inflammatory properties [37]. Conversely, treatment with ibuprofen has also been associated with increased concentrations of LTB4 a leukotriene, indicating airway inflammation [38]. Similar to naproxen, the product information for ibuprofen also lists asthma, bronchospasm, dyspnoea and wheezing as adverse reactions to ibuprofen [30]. In this study, initiation of ibuprofen was associated with initiation of COPD medicines for both development and progression of COPD. This study provides further evidence, in addition to the product information, of the adverse effect on lung function associated with use of NSAIDs. Further studies are required to confirm whether inhibition of GPx is a contributing pharmacological mechanism to this ADE and symptoms rather than allergic or immunologic reactions to NSAIDs.
Nicotine was associated with development and progression of COPD. Umeclidinium, indacaterol, glycopyronnium/indacaterol, tiotropium/olodaterol and fluticasone furoate/umeclidinium/vilanterol were more often prescribed after initiation of nicotine. Tobacco smoking is a prominent modifiable risk factor for COPD [25]. More than 25% of people with COPD smoke daily and 47% are ex-smokers [39]. It is therefore not surprising that SSA has identified a positive signal between initiating nicotine replacement therapy and initiation of COPD medicines. Rather, the results presented here confirm the substantial risk smoking has on COPD progression, and initiation of nicotine is simply a surrogate marker for current or previous smoking history. Indeed, the SSA of nicotine to tiotropium or fluticasone propionate/salmeterol (which had the largest study populations for this initiation medicine) both demonstrated a reduction in risk of initiating either of these COPD treatments (Fig. 5).
In Australia, cefuroxime is used to treat community- and hospital-acquired pneumonia, community- and hospital-acquired lung abscess due to aspiration of oral bacteria, acute epiglottitis and acute bacterial rhinosinusitis [40]. Exacerbations of COPD are known to be caused by viral and bacterial infections [13, 40, 41]. Additionally, infections are common complications of COPD and cefuroxime may be prescribed to treat the underlying infection [42]. The results in this study for cefuroxime may indicate protopathic bias [18]. Whilst medications for COPD are commonly initiated subsequent to the initiation of cefuroxime, SSA is unable to account for confounding by indication. The results here for cefuroxime suggest that either COPD is diagnosed shortly after initiating cefuroxime or that escalation in therapy is required, indicating that an exacerbation or complication of COPD has occurred and the condition may have progressed.
Additional signals worthy of further investigation include the signals of COPD development for acamprosate, mycophenolate, rizatriptan, gemfibrozil and methyldopa, as indicated by their positive aSRs and subsequent initiation of tiotropium. The Australian product information for acamprosate, rizatriptan, gemfibrozil and methyldopa does not provide any information on risk of COPD development and therefore mechanisms for this association should be investigated [30]. Mycophenolate is an immunosuppressant and therefore risk of respiratory infection is anticipated and may provide an explanation of the mechanism for the signals observed in initiation of medicines for COPD in this study. Infective exacerbations are important events in COPD and require acute management to prevent deterioration of lung function. Importantly, the treatment sequences observed here are not necessarily reflective of clinical practice and the management of infective exacerbations of COPD. Some treatment sequences may reflect continual deterioration of the condition as opposed to acute events. Despite this, prior murine models have demonstrated that mycophenolate reduces GPx1 activity, indicating a possible alternative mechanistic explanation of the COPD signals in this study [43]. Future case-control studies should investigate the association of these medicines with COPD development, especially given that an alternative explanation for these signals is unlikely. Similarly, the strong positive ADE signals for COPD progression associated with initiation of acamprosate, baclofen, rizatriptan, mesalazine, sodium valproate, acetazolamide, captopril, furosemide, labetalol and mefenamic acid should be investigated. To our knowledge, and based on the product information, there is limited explanation why any of these medicines with at least one positive ADE signal for COPD progression would be associated with COPD, despite perhaps acetazolamide, captopril, furosemide, labetalol and mefenamic acid, where signals may be explained by confounding by indication, protopathic bias or alternative pharmacological mechanisms. Caution should however be used when interpreting and investigating SSA signals where the causal or non-causal groups contain less than five pairs.
To the best of our knowledge, this is the first study to utilize SSA to determine whether common prescription medicines are associated with COPD development or progression in the real world, based on pharmacological mechanistic findings from computational molecular modelling techniques. SSA is a validated, moderately sensitive and highly specific tool for detecting ADE signals [18]. The use of SSA in this study was advantageous over other more common ADE signal detection methods, such as disproportionality methods, because it has sufficient power to detect rare adverse events and those that occur after long-term exposure, which is important given the slow progressive nature of COPD [18, 19, 44]. The within-person study design of SSA is also valuable as it controls for confounders that are stable over time such as concomitant medical conditions, regular medications, age and sex [45].
Whilst 53% (21 of 40) of the index medicines had at least one positive ADE signal associated with initiation of a COPD outcome medication, the number of patients dispensed certain COPD outcome medications was limited, which may affect the interpretability of results and lead to a low number of observed pairs in initiation of medicines. Any sequences with small numbers should be interpreted with caution. SSA requires that administrative databases include sufficient data for it to be applied effectively. For the long-acting bronchodilators which indicated COPD development, most people were initiated on tiotropium (54,884), compared with any other LAMA or LABA (umeclidinium 4614, glycopyrronium 4996, aclidinium 4590, indacaterol 7282) which reflects current prescribing preferences and familiarity with tiotropium.
Medicines such as umeclidinium, glycopyrronium and aclidinium were only listed on the PBS during the study period [46]. Similarly, for COPD medications indicating COPD progression, the LAMA/LABAs glycopyrronium/indacaterol and umeclidinium/vilanterol were first listed on the PBS in November and December 2014, respectively, and aclidinium/formoterol and tiotropium/olodaterol were initially made available on the PBS a year later in December 2015 [46]. For the ICS/LABAs which also indicate COPD progression, the dry powder inhaler formulation of budesonide/formoterol was available on the PBS prior to the study period commencing; however, the metered dose inhaler was only made available on the PBS in July 2013 and fluticasone furoate/vilanterol was only listed in July 2014. The most commonly initiated ICS/LABA fluticasone propionate/salmeterol (26,646), however, was PBS listed prior to the study period commencing [46]. The last step of inhaled therapy, ICS/LABA/LAMA of fluticasone/umeclidinium/vilanterol, was only PBS listed in June 2018, which explains the relatively low number of people (4752) initiated on this therapy [47]. Listing of a medicine on the PBS during the study period rather than beforehand limited the data pool from which pairs of initiation and outcome medicines could be extracted. Additionally, as COPD therapy increases in a stepwise manner, the number of patients initiated on each COPD treatments declines as severity of COPD increases. Because of this, it is inherently difficult to determine the impact that medicines have in more severe forms of COPD and when therapies are very new to market. To account for this, and to stratify by development or progression of COPD, outcome medicines initiated at each stage of therapy were selected [18].
Given that we have performed a large number of comparisons, there is a chance of identifying false positive signals due to chance alone. The use of active controls is also currently recommended in sequence symmetry analyses to assist in adjusting for protopathic bias [48, 49]. This study was the first step in a screening approach to validate the findings from our prior molecular modelling analyses. Active controls were not used in the present study as their use has not been validated in large-scale hypothesis generating processes and it is unclear as to what the active controls would be given there is minimal information on the in vitro GPx1 inhibitory activity of registered medicines; however, use of active controls should be the focus of future research and analyses.
In this analysis, signals generated by SSA for medicines available over the counter such as ibuprofen, mefenamic acid, naproxen and nicotine may be underestimated as sale or dispensing of over these medicines are not captured in the PBS dataset and the sequence of initiation medicine to outcome medicine will not be included in the analysis which dampens the signal [18].
Implementation of SSA was important in this study because the association between initiation of these common medicines and subsequent development or progression of COPD is largely unknown [18]. Moreover, if a clinician were to know that a medicine causes an adverse event then they would cease the offending medicine and an ADE signal would be dampened [18]. Due diligence must still be exercised when interpreting the SSA results presented here as COPD medicines have been used as a proxy for adverse events rather than hospitalization codes that indicate outcomes associated with COPD. However, our previous findings that these medicines may inhibit GPx1 improve the strength of these COPD ADE signals and prompt for further investigations [17].
5 Conclusion and Future Directions
Sequence symmetry analysis has identified associations between initiation of 21 prescription medicines that potentially inhibit GPx1 such as acetazolamide, atenolol, naproxen, nicotine and cefuroxime, and subsequent initiation of medications for COPD development or progression. The results for cefuroxime and nicotine may be indicative of protopathic bias; however, the results achieved for atenolol, ibuprofen, naproxen and other medicines warrant further investigation via in vitro analyses and well-controlled observational studies. The ADE signals achieved in this study could be due to bronchospasm or may be part of a more complex mechanism such as inhibition of antioxidant enzymes, such as GPx1, which could further contribute to development and progression of COPD in the long term.
References
Lung Foundation Australia. Overview chronic obstructive pulmonary disease. 2022 [cited 16 February 2022]. Available from: https://lungfoundation.com.au/patients-carers/living-with-a-lung-disease/copd/overview/.
Australian Institute of Health and Welfare. Chronic obstructive pulmonary disease (COPD). [Cited16 February 2022]. Available from: https://www.aihw.gov.au/reports/chronic-respiratory-conditions/copd/contents/copd.
Blanco I, Diego I, Bueno P, Casas-Maldonado F, Miravitlles M. Geographic distribution of COPD prevalence in the world displayed by Geographic Information System maps. Eur Respir J. 2019;54(1):1900610.
World Health Organization. Chronic obstructive pulmonary disease (COPD)
Diez-Manglano J, Barquero-Romero J, Mena PA, Recio-Iglesias J, Cabrera-Aguilar J, Lopez-Garcia F, et al. Polypharmacy in patients hospitalised for acute exacerbation of COPD. Eur Respir J. 2014;44(3):791–4.
Boom M, Niesters M, Sarton E, Aarts L, Smith TW, Dahan A. Non-analgesic effects of opioids: opioid-induced respiratory depression. Curr Pharm Des. 2012;18(37):5994–6004.
Prosser AE, Dawson JL, Koo K, O’Kane KM, Ward MB, Woodman RJ, et al. Real-world incidence of patient-reported dyspnoea with ticagrelor. Ther Adv Drug Saf. 2018;9(10):577–84.
Miller KL, Sawitzke AD, Doane J. Abatacept and serious respiratory infections in patients with previous lung disease. Clin Rheumatol. 2008;27(12):1569–71.
Australian Medicines H. Australian medicines handbook: AMH. AMH; 2022.
Garcia Rodriguez LA, Wallander MA, Tolosa LB, Johansson S. Chronic obstructive pulmonary disease in UK primary care: incidence and risk factors. COPD. 2009;6(5):369–79.
Jacobson GA, Yee KC, Ng CH. Elevated plasma glutathione peroxidase concentration in acute severe asthma: comparison with plasma glutathione peroxidase activity, selenium and malondialdehyde. Scand J Clin Lab Investig. 2007;67(4):423–30.
Nadeem A, Chhabra SK, Masood A, Raj HG. Increased oxidative stress and altered levels of antioxidants in asthma. J Allergy Clin Immunol. 2003;111(1):72–8.
Vlahos R, Bozinovski S. Glutathione peroxidase-1 as a novel therapeutic target for COPD. Redox Rep. 2013;18(4):142–9.
Rahman I. Pharmacological antioxidant strategies as therapeutic interventions for COPD. Biochim Biophys Acta. 2012;1822(5):714–28.
Calzetta L, Rogliani P, Facciolo F, Rinaldi B, Cazzola M, Matera MG. N-Acetylcysteine protects human bronchi by modulating the release of neurokinin A in an ex vivo model of COPD exacerbation. Biomed Pharmacother. 2018;103:1–8.
Zinellu E, Zinellu A, Pau MC, Piras B, Fois AG, Mellino S, et al. Glutathione peroxidase in stable chronic obstructive pulmonary disease: a systematic review and meta-analysis. Antioxidants (Basel). 2021;10(11):1745.
Janetzki JL, Pratt NL, Ward MB, Sykes MJ. Application of an integrative drug safety model for detection of adverse drug events associated with inhibition of glutathione peroxidase 1 in chronic obstructive pulmonary disease. Pharm Res. 2023;40:1553–68.
Lai EC, Pratt N, Hsieh CY, Lin SJ, Pottegard A, Roughead EE, et al. Sequence symmetry analysis in pharmacovigilance and pharmacoepidemiologic studies. Eur J Epidemiol. 2017;32(7):567–82.
Pratt NL, Ilomaki J, Raymond C, Roughead EE. The performance of sequence symmetry analysis as a tool for post-market surveillance of newly marketed medicines: a simulation study. BMC Med Res Methodol. 2014;14(1):66.
King CE, Pratt NL, Craig N, Thai L, Wilson M, Nandapalan N, et al. Detecting medicine safety signals using prescription sequence symmetry analysis of a national prescribing data set. Drug Saf. 2020;43(8):787–95.
Roughead EE, Chan EW, Choi NK, Griffiths J, Jin XM, Lee J, et al. Proton pump inhibitors and risk of Clostridium difficile infection: a multi-country study using sequence symmetry analysis. Expert Opin Drug Saf. 2016;15(12):1589–95.
World Health Organization Collaborating Centre for Drug Statistics Methodology. Anatomical therapeutic chemical code classification index with defined daily doses.
Australian Government Department of Health. Pharmaceutical benefits scheme. 2022 [cited 7 April 2022]. Available from: https://www.pbs.gov.au/pbs/home.
Toelle BG, Xuan W, Bird TE, Abramson MJ, Atkinson DN, Burton DL, et al. Respiratory symptoms and illness in older Australians: the Burden of Obstructive Lung Disease (BOLD) study. Med J Aust. 2013;198(3):144–8.
Liu Y, Pleasants RA, Croft JB, Wheaton AG, Heidari K, Malarcher AM, et al. Smoking duration, respiratory symptoms, and COPD in adults aged >/=45 years with a smoking history. Int J Chron Obstr Pulm Dis. 2015;10:1409–16.
Janetzki JL, Sykes MJ, Ward MB, Pratt NL. Proton pump inhibitors may contribute to progression or development of chronic obstructive pulmonary disease—a sequence symmetry analysis approach. J Clin Pharm Ther. 2021;46(6):1687–94.
Lung Foundation Australia. Stepwise Management of Stable COPD. 2020.
Preiss AK, Roughead EE, Pratt NL. Sequence symmetry analysis graphic adjustment for prescribing trends. BMC Med Res Methodol. 2019;19(1):143.
Baker JG, Wilcox RG. Beta-Blockers, heart disease and COPD: current controversies and uncertainties. Thorax. 2017;72(3):271–6.
MIMS Australia. MIMS Online. Monthly index of medical specialities. St Leonards, N.S.W.: MIMS Australia; 1996.
Gulea C, Zakeri R, Alderman V, Morgan A, Ross J, Quint JK. Beta-blocker therapy in patients with COPD: a systematic literature review and meta-analysis with multiple treatment comparison. Respir Res. 2021;22(1):64.
Salpeter SR, Ormiston TM, Salpeter EE. Cardiovascular effects of beta-agonists in patients with asthma and COPD: a meta-analysis. Chest. 2004;125(6):2309–21.
Dorow P, Thalhofer S, Bethge H, Disselhoff G, Wagner G. Long-term treatment of angina pectoris with bisoprolol or atenolol in patients with chronic obstructive bronchitis: a randomized, double-blind crossover study. J Cardiovasc Pharmacol. 1990;16(Suppl 5):S36-44.
van Zyl AI, Jennings AA, Bateman ED, Opie LH. Comparison of respiratory effects of two cardioselective beta-blockers, celiprolol and atenolol, in asthmatics with mild to moderate hypertension. Chest. 1989;95(1):209–13.
Voiriot G, Philippot Q, Elabbadi A, Elbim C, Chalumeau M, Fartoukh M. Risks related to the use of non-steroidal anti-inflammatory drugs in community-acquired pneumonia in adult and pediatric patients. J Clin Med. 2019;8(6):786.
Orhan H, Sahin G. In vitro effects of NSAIDS and paracetamol on oxidative stress-related parameters of human erythrocytes. Exp Toxicol Pathol. 2001;53(2–3):133–40.
McKeever TM, Lewis SA, Smit HA, Burney P, Britton JR, Cassano PA. The association of acetaminophen, aspirin, and ibuprofen with respiratory disease and lung function. Am J Respir Crit Care Med. 2005;171(9):966–71.
Montuschi P, Macagno F, Parente P, Valente S, Lauriola L, Ciappi G, et al. Effects of cyclo-oxygenase inhibition on exhaled eicosanoids in patients with COPD. Thorax. 2005;60(10):827–33.
Health AIo, Welfare. Chronic obstructive pulmonary disease (COPD), associated comorbidities and risk factors. Canberra: AIHW; 2020.
Therapeutic Guidelines. Therapeutic Guidelines. eTG complete. West Melbourne: Therapeutic Guidelines Ltd.; 2003.
Geraghty P, Baumlin N, Salathe MA, Foronjy RF, D’Armiento JM. Glutathione peroxidase-1 suppresses the unfolded protein response upon cigarette smoke exposure. Mediat Inflamm. 2016;2016:9461289.
Sethi S. Infection as a comorbidity of COPD. Eur Respir J. 2010;35(6):1209–15.
Dalmarco EM, Budni P, Parisotto EB, Wilhelm Filho D, Frode TS. Antioxidant effects of mycophenolate mofetil in a murine pleurisy model. Transpl Immunol. 2009;22(1–2):12–7.
Faillie JL. Case-non-case studies: principle, methods, bias and interpretation. Therapie. 2019;74(2):225–32.
Hersom K, Neary MP, Levaux HP, Klaskala W, Strauss JS. Isotretinoin and antidepressant pharmacotherapy: a prescription sequence symmetry analysis. J Am Acad Dermatol. 2003;49(3):424–32.
Pharmaceutical Benefits Scheme. Post-market review of chronic obstructive pulmonary disease medicines background and tor 1 final report. 2017.
Australian Government Department of Health. PBS publications archive: schedule of pharmaceutical benefits (Summary of Changes) 1 June 2021. 2022 [cited 24 February 2022]. Available from: https://www.pbs.gov.au/publication/schedule/2018/06/2018-06-01-general-soc.pdf.
Hallas J, Whitaker H, Delaney JA, Cadarette SM, Pratt N, Maclure M. The use of active comparators in self-controlled designs. Am J Epidemiol. 2021;190(10):2181–7.
Vouri SM, Jiang X, Morris EJ, Brumback BA, Winterstein AG. Use of negative controls in a prescription sequence symmetry analysis to reduce time-varying bias. Pharmacoepidemiol Drug Saf. 2021;30(9):1192–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
JLJ received the Australian Government Research Training Program (RTP) fee offset scholarship to conduct this study.
Conflict of interest
All authors have no conflicts of interest to declare.
Ethics approval
This study was approved by the External Request Evaluation Committee (EREC) Australian Government Department of Human Services (approval reference number RMS0862).
Consent to participate
Not applicable.
Consent for publication
Consent for publication was obtained from External Request Evaluation Committee (EREC) Australian Government Department of Human Services (approval reference number RMS0862).
Availability of data and materials
Data from Services Australia are available however restrictions apply so are not readily available to the public. A request for data can be submitted to Services Australia.
Code availability
SAS code is available upon request from the corresponding author.
Author contribution
JJ, MW, MS and NP developed and designed the study. NP developed the code and statistical methods to conduct this research. JJ adjusted and utilised the code as necessary to conduct the analysis. JJ wrote the primary manuscript. All authors reviewed and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Janetzki, J.L., Sykes, M.J., Ward, M.B. et al. Chronic Obstructive Pulmonary Disease Adverse Event Signals Associated with Potential Inhibitors of Glutathione Peroxidase 1: A Sequence Symmetry Analysis. Drug Saf 47, 59–70 (2024). https://doi.org/10.1007/s40264-023-01374-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-023-01374-5