Abstract
Introduction
Gastric acid-related symptoms are highly prevalent in the general population (21–40%), and more than 11% of individuals use medication for the treatment of these symptoms. The uptake of micronutrients is dependent on the gastrointestinal potential of hydrogen (pH).
Objective
We hypothesized that medication affecting gastrointestinal pH reduces the availability of B vitamins, thereby deranging one-carbon metabolism and detrimentally affecting spermatogenesis.
Methods
This explorative nested case–control study in men of subfertile couples investigated associations between medication used for gastric acid-related symptoms and semen parameters. We included 40 men using medication for gastric acid-related symptoms and 843 men not using medication. Semen analyses were performed between 70 days before and 21 days after the visit.
Results
The use of medication was associated with a twofold higher risk of a low total motile sperm count [TMSC <1 × 106, odds ratio (OR) 2.090, p = 0.049] and negatively with sperm concentration (β −0.320, p = 0.028). Red blood cell folate was positively associated with TMSC (β 0.257, p = 0.026), sperm count (β 1.679, p = 0.013) and ejaculate volume (β 0.120, p = 0.023), and total homocysteine (tHcy) was negatively associated with sperm count (β −0.077, p = 0.021).
Conclusion
Here we delineate associations between the use of medication for gastric acid-related symptoms and poor semen quality in men of subfertile couples. The use of medication for gastric acid-related symptoms is associated with a twofold higher risk of a low TMSC and a decreased sperm concentration. Although these findings warrant further research on causality, the associations between folate, tHcy and semen quality emphasize the importance of preconception counselling in male subfertility.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Medication used for gastric acid-related symptoms is associated with low total motile sperm count and decreased sperm concentration. |
More studies are needed to test drug safety of medication on fertility parameters in men. |
1 Introduction
Around 15% of couples are subfertile—pregnancy not achieved after 1 year of unprotected intercourse—of which half remain involuntarily childless [1]. In 45%, the cause can be attributed to a male factor [2]. To contribute to future treatment and prevention of male subfertility, it is of great importance to investigate causes and the underlying pathophysiology.
In 20–40% of the general population, gastric acid-related symptoms are present, and in about 11%, medication is used [3, 4]. However, its impact on semen parameters has scarcely been studied. Antacids, proton-pump inhibitors (PPIs) and histamine receptor antagonists (H2RAs) induce a prolonged increase in gastric pH, impairing the gastrointestinal absorption of nutrients, including folate and cobalamin, these being essential for spermatogenesis [5–7]. B vitamin shortages derange one-carbon metabolism and induce hyper-homocysteinaemia, which causes excessive oxidative stress and interferes with biological processes and DNA structures [8].
Seminal plasma folate, cobalamin and total homocysteine (tHcy) are associated with the sperm DNA fragmentation index and sperm concentration [9, 10]. This is supported by the detrimental effects of poor nutrition and beneficial effects of a healthy diet on sperm parameters [9, 11, 12]. In addition, folic acid and zinc supplements increase sperm count, concentration and seminal plasma folate concentration [9, 13, 14].
Therefore this explorative study aims to investigate whether the use of medication for gastric acid-related symptoms is associated with semen parameters and biomarkers of one-carbon metabolism in men of subfertile couples.
2 Materials and Methods
2.1 Study Design
Between 2007 and 2012, couples contemplating pregnancy and visiting the outpatient clinic of the Department of Obstetrics and Gynaecology at the Erasmus MC, University Medical Centre in Rotterdam, the Netherlands, were offered preconception counselling. These couples were referred because of subfertility, i.e. when pregnancy is not achieved after 1 year of unprotected intercourse [1]. Men were invited to participate in the study and completed a self-administered questionnaire to obtain data on medication use (type, dosage and frequency), smoking (yes/no), use of alcohol (yes/no), recreational drugs (yes/no) and folic acid supplements (yes/no) (see Electronic Supplementary Material 1). At the visit, the questionnaires were verified by a trained counsellor, and height and weight were measured to calculate body mass index (BMI) (kg/m2). The information on nutrition and lifestyle was screened for risk factors, and individual advice on inadequacies was given during the visit. Men who provided written informed consent and a semen analysis between 70 days before and 21 days after the visit were included in the study. This window was defined because it covers 3 months of spermatogenesis during which medication use was assessed and reduces confounding by counselling. We excluded men with semen samples provided by microsurgical epididymal sperm aspiration (MESA), percutaneous epididymal sperm aspiration (PESA) or retrograde ejaculation. Men with incomplete data and men using other medication for gastric acid-related symptoms were excluded as well.
2.2 Semen Sample Collection and Analysis
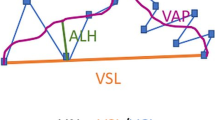
Semen analyses were performed on the clinical indication of subfertility, and these data were obtained from medical records. The examination and processing were performed before 2010 according to the fourth edition of the World Health Organization (WHO) laboratory manual and afterwards according to the fifth edition [15, 16]. Men received a leaflet with instructions on how to provide a semen sample. The obligatory abstinence period for producing a semen sample was 3–5 days. The sample had to be collected in a non-toxic plastic container provided by the laboratory and had to be delivered within 1 h of production at the outpatient clinic of the Division of Reproductive Medicine at the Erasmus MC, University Medical Centre, Rotterdam, The Netherlands. To avoid large changes in temperature, the semen sample had to be kept at ambient temperature during transport [17]. After liquefaction the following sperm parameters were assessed using a Zeiss microscope (Carl Zeiss, Oberkochen, Germany): ejaculate volume (normal range >2.0 mL); sperm concentration (normal range >20 × 106 sperm/mL); and percentage of motile and immotile spermatozoa (normal range >50% with grade A + B motility). Sperm concentration was determined with an improved Neubauer Hemocytometer counting chamber. Total sperm count was calculated as the product of ejaculate volume and sperm concentration. Sperm motility parameters type A (rapid progressive motility), type B (slow or sluggish progressive motility), type C (local motility) and type D (immotility) were assessed at 37 °C. Total motile sperm count (TMSC) was calculated as the product of ejaculate volume, sperm concentration and grade A + B motility. A TMSC <1 × 106 was defined as low because it represents severe oligoasthenoteratozoospermia [18, 19]. All semen analyses were performed in one centre and laboratory, which participates in the external quality control scheme of the Dutch Foundation for Quality Assessment in Clinical Laboratories (SKML). The staff performing these analyses are trained and tested annually according to the certified ESHRE (European Society of Human Reproduction and Embryology) course for performing semen analyses.
The laboratory of the Erasmus MC received the certification of the International Organization for Standardization (ISO9001), the international standard for quality measurement. The between-technician variation for sperm concentration was 1.6% [intraclass correlation coefficient (ICC) 0.992, 95% confidence interval (CI) 0.978–0.997]. The between-technician variation for sperm motility was 2.4% (ICC 0.988, 95% CI 0.972–0.996).
2.3 Biomarkers
At the preconception visit, venous blood samples were drawn in a Vacutainer ethylenediaminetetraacetate (EDTA) tube for the determination of red blood cell (RBC) folate and plasma tHcy; for serum folate and cobalamin, a dry Vacutainer tube (BD diagnostics, Plymouth, UK) was used. EDTA blood was kept on ice, and plasma was separated by centrifugation within 1 h for determination of tHcy. Immediately after blood sampling, 0.1 mL of EDTA blood was haemolysed with 0.9 mL freshly prepared 1.0% ascorbic acid. The haematocrit in EDTA blood was determined on an ADVIA 120 Hematology Analyzer (Bayer Diagnostics, Leverkusen, Germany). The haemolysate was centrifuged for 5 min at 1000×g, after which folate was measured in the haemolysate. RBC folate was calculated with the following formula: (nM haemolysate folate × 10/haematocrit) − [nM serum folate × (1 − haematocrit)/haematocrit] = nM RBC folate. tHcy was determined using a sensitive liquid chromatography tandem mass spectrum method (HPLC-Tandem MS, Waters Micromass Quattro Premier XE Mass Spectrometer with Acquity UPLC system, Milford, Massachusetts, USA). Blood obtained in dry Vacutainer tubes was centrifuged at 2000×g; serum was collected and, during routine laboratory procedures, analysed using an immunoelectrochemiluminescence assay (E170; Roche Diagnostics GmbH, Mannheim, Germany). Inter-assay coefficients of variation for serum folate were 4.5% at 13 nmol/L and 5.7% at 23 nmol/L; for serum cobalamin, they were 3.6% at 258 pmol/L and 2.2% at 832 pmol/L; and for plasma tHcy, they were 4.8% at 14.6 μmol/L and 3.3% at 34.2 μmol/L.
2.4 Statistical Analyses
Chi-squared tests and Mann–Whitney U tests were performed to evaluate differences between the groups. To perform linear and logistic regression analyses, a normal distribution of the sperm parameters was achieved with root transformation of ejaculate volume and sperm count, and fourth root transformation of TMSC and sperm concentration. Univariable and multivariable linear and logistic regression models were applied to study associations between medication use and sperm parameters. For the univariable linear regression analyses of sperm parameters, RBC folate was assessed in pmol/L for better interpretation of the estimate (pmol/L = nmol/L × 103). Age, ethnicity, smoking and alcohol use were selected as potential confounders based on associations with semen parameters. The cut-off concentration for serum folate of ≥22.5 nmol/L was used to confirm folic acid supplement use [20]. Statistical analyses were performed using SPSS software for Windows (version 21.0, IBM SPSS, Statistics for Windows, Armonk, NY, USA; IBM Corp.) with a level of significance of 0.05.
3 Results
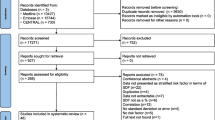
A total of 2255 men visiting the preconception outpatient clinic were eligible for participation, from whom we excluded 137 who did not provide written informed consent and 846 who did not provide a semen analysis between 70 days before and 21 days after the visit. From the remaining 1272 men, we excluded 23 with MESA, PESA or retrograde ejaculation samples, ten with incomplete data, 329 using any other medication and 27 without information on medication use. This resulted in the analysis of 883 men, of whom 40 used medication for gastric acid-related symptoms (PPIs n = 34, antacids n = 3, and H2RAs n = 3), and 843 controls not using any medication. Of the 40 medication users, the use was daily in 29 men, weekly in two men and when needed in seven men. This data was missing in two men. General characteristics of included (n = 883) and excluded (n = 1235) men of subfertile couples are presented in Electronic Supplementary Material 2. All characteristics were comparable between the groups except a slightly lower age (34 vs. 35 years, p = 0.003) and higher percentage of no medication use in the study population (95.5 and 52.6% non-users, p < 0.001) inherent to the selection. Table 1 shows the general characteristics of medication users (n = 40) and controls (n = 843). In medication users, age was significantly higher (38 and 34 years, p = 0.002) and alcohol and drug use was lower than in controls (55 and 71%, p = 0.031, and 0.0 and 7.7%, p = 0.029, respectively). Serum and RBC folate tended to be higher and cobalamin and tHcy tended to be lower in medication users, albeit not significantly. The abstinence period and time to semen analysis were comparable between the groups. All sperm parameter values were slightly but not significantly lower in medication users, except for a higher ejaculate volume (3.4 and 2.8 mL, p = 0.036). Figure 1 depicts the median values and interquartile ranges of sperm concentration, TMSC and sperm motility.
a Sperm concentration (p = 0.090), b total motile sperm count (p = 0.209) and c motility (A + B%) (p = 0.095) in men using medication for gastric acid-related symptoms (n = 40) and controls (n = 843). The box plots display the 25th and 75th percentile, the horizontal line marks the median value, and the whiskers extend to the minimum and maximum observations that are within 1.5 times the interquartile range
Being a Dutch native was associated with a lower sperm concentration (β −0.128, 95% CI −0.23 to −0.02, p = 0.016) and a higher ejaculate volume (β 0.126, 95% CI 0.07–0.18, p < 0.001). Smoking was negatively associated with TMSC (β −0.173, 95% CI −0.30 to −0.05, p = 0.008), sperm count (β −1.138, 95% CI −1.88 to −0.40, p = 0.003) and ejaculate volume (β −0.093, 95% CI −0.15 to −0.04, p = 0.001). Alcohol use was positively associated with sperm motility (β 2.506, 95% CI 0.26–4.75, p = 0.029), TMSC (β 0.130, 95% CI 0.001–0.26, p = 0.048) and ejaculate volume (β 0.069, 95% CI 0.01–0.13, p = 0.020). Age, BMI, folic acid supplement use and drug use were not significantly associated with sperm parameters.
Table 2 presents associations between medication for gastric acid-related symptoms and a decreased sperm concentration [β −0.311, standard error (SE) 0.144]. Backwards transformation to the original scale resulted in a decrease in sperm concentration of 10.5 × 106/mL in medication users. Moreover, a twofold higher risk of low TMSC was observed in medication users [unadjusted odds ratio (OR) 2.158, 95% CI 1.05–4.43, p = 0.036]. After adjustment for smoking, this risk slightly increased (OR 2.161, 95% CI 1.05–4.44, p = 0.036). Additional adjustment for alcohol use, age and ethnicity slightly attenuated the risk estimate (OR 2.090, 95% CI 1.00–4.35, p = 0.049). Adjustment of the latter model for the WHO manual edition did not affect the results (OR 2.148, 95% CI 1.02–4.48, p = 0.042). The multivariable linear regression analysis showed the same (β −0.323, SE 0.146, p = 0.027).
Univariable linear regression analyses revealed positive associations between RBC folate (pmol/L) and TMSC (β 0.257, 95% CI 0.03–0.48, p = 0.026), sperm count (β 1.679, 95% CI 0.35–3.01, p = 0.013) and ejaculate volume (β 0.120, 95% CI 0.02–0.22, p = 0.023). tHcy was negatively associated with sperm count (β −0.077, 95% CI −0.14 to −0.01, p = 0.021). Serum folate and cobalamin were not associated with any sperm parameter.
4 Discussion
This explorative study shows that use of antacids, PPIs and H2RAs is associated with impaired semen parameters in men of subfertile couples visiting a tertiary hospital in the Netherlands. These medication users showed a decreased sperm concentration and a twofold higher risk of low TMSC.
The strengths of the study are the standardized semen sample collection and semen analyses in a single and qualified laboratory centre, thereby limiting risks of methodological and measurements errors. Protocols were used by trained counsellors for data collection, verification of medication use in a defined window, and measurements. To exclude selection bias, we also showed that general characteristics were largely comparable in included and excluded men. Weaknesses are, firstly, that due to the small sample sizes, the individual medicines (PPIs, H2RAs and antacids) could not be evaluated, and, secondly, confounding by indication, because in all medication users, gastrointestinal symptoms were present. Although no abnormal semen parameters were shown in men with digestive diseases, these issues have to be addressed in future research [21]. Under-reporting of medication use is an issue to be considered, because previous research reported that 11% of Dutch men and women used medication for gastric acid-related symptoms, which is much higher than the 5% in our study [3]. Because these medicines are also available over the counter, a validation through pharmacy databases was not possible.
In addition, frequency of medication use, but not duration of use, was taken into account, which is a limitation but compensates the reliability of current use. Therefore this study can also not assess the—although very unlikely—harmful pharmacological effects of a single dose on semen quality. One semen sample of each man was available, which does not account for intra-individual variation of semen parameters. Residual confounding by a sedentary lifestyle, sauna visits, nutritional behaviour or incompleteness of the sample collection cannot be excluded as well and has to be addressed in future [22, 23]. Confounding, however, was reduced by selecting semen samples only in a strictly defined window that was independent of exposures and bias due to the exclusion of conditions affecting semen parameters, i.e. varicoceles or cryptorchidism.
Our findings are supported by Hayashi et al., who reported that quitting or switching H2RAs improved semen quality [24]. Others have shown a reduction in sperm viability in a dose- and time-dependent manner when liquefied semen samples were exposed to H2RAs [25]. Both ranitidine and cimetidine were considered to be acting as anti-androgens, but only the use of cimetidine impaired hypothalamic–pituitary–gonadal function [26]. Ranitidine, the only H2RA reported in our study, did not bind to androgen receptors or influence basal serum concentrations of testosterone, luteinizing hormone, follicle stimulating hormone or prolactin in fertile men. The mean sperm count decreased during ranitidine treatment, although this difference was not significant [27]. The higher ejaculate volume in medication users is new and so far cannot be explained by a pharmacological mechanism of action. Our previous study investigating the effect of the duration of PPIs only on semen quality substantiates the potential harmful effects observed in this study. A threefold higher risk of a low TMSC was observed in men visiting the general practitioner when PPIs were used between 12 and 6 months preceding semen analysis, suggesting that a long-term increase in gastric pH results in a decline of sperm quality [28].
Detrimental effects of BMI, age or alcohol consumption on semen quality were not observed. This may be due to the small variation of these conditions and effect estimates relative to the large variations in sperm parameters. Our studies and those of others reported that obesity or central adiposity are associated with impaired sperm motility, ejaculate volume, sperm concentration, TMSC [29, 30] and azoospermia or oligozoospermia [31]. The latter study also reported no differences in sperm concentration across BMI categories. Age above 60 has been associated with a raised sperm DNA fragmentation index, but similar to our results, was not significantly associated with other sperm parameters [32]. The association between alcohol use and semen parameters is not substantiated by the rather conflicting literature and is complicated because the majority of men in this study used alcohol [33–37]. In addition, smoking negatively influenced TMSC, ejaculate volume and sperm count, which is in line with the studies of others [38, 39]. From these data, we conclude that differences in general characteristics of the study populations, sample sizes, precision of exposure assessment, and the effects at the extremes of conditions only (BMI >30, excessive alcohol consumption) might explain the differences in associations between BMI, age, alcohol use and sperm parameters.
Associations between the biomarkers of one-carbon metabolism, RBC folate, tHcy and semen quality are in line with our studies and those of others [9, 10, 40]. Moreover, these observations are supported by studies demonstrating associations between folate intake by supplements or food and semen quality [12, 41]. A traditional Dutch diet is positively associated with RBC folate and with sperm concentration, and a diet rich in fruits and vegetables is negatively associated with seminal plasma tHcy and sperm DNA fragmentation index [9, 11]. In our study, the slightly lower cobalamin level in medication users did not differ significantly from non-users. This may be explained by a higher percentage of vitamin supplement users in medication users, resulting in higher serum and RBC folate, albeit not significantly, and the small sample size. The use of folic acid supplements was not associated with semen quality and therefore not included in the multivariable analyses [9, 12–14]. This is very likely due to the limited folic acid supplement use in our study.
5 Conclusion
The use of medication for gastric acid-related symptoms is associated with impaired semen parameters in men of subfertile couples contemplating pregnancy. These first findings have to be interpreted with caution and emphasize the need for further research on causality and awareness of potential detrimental effects of medication for gastric acid-related symptoms on semen quality.
Authors’ contribution
All authors contributed to the writing of the manuscript and approved the final version. NAH contributed to the data collection, analysis and interpretation; she wrote the first draft and revised all versions of the manuscript. HJG was involved in data collection and analysis and contributed to the first draft of the manuscript. JMT was involved in data collection and analysis. AM contributed to the interpretation of the results and to the revision of the manuscript. JL and GD both contributed to the revision of the manuscript, and JL was responsible for the determination of the biomarkers. JSEL was clinically responsible for the patients visiting the outpatient clinic and contributed to the interpretation of the data. RPMS-T designed and supervised all aspects of the study and contributed to all revisions of the manuscript.
References
Evers JL. Female subfertility. Lancet. 2002;360(9327):151–9. doi:10.1016/S0140-6736(02)09417-5.
van der Steeg JW, Steures P, Eijkemans MJ, Hompes PG, Kremer JA, et al. Role of semen analysis in subfertile couples. Fertil Steril. 2011;95(3):1013–9. doi:10.1016/j.fertnstert.2010.02.024.
Tielemans MM, Jaspers Focks J, van Rossum LG, Eikendal T, Jansen JB, Laheij RJ, et al. Gastrointestinal symptoms are still prevalent and negatively impact health-related quality of life: a large cross-sectional population based study in The Netherlands. PLoS One. 2013;8(7):e69876. doi:10.1371/journal.pone.0069876.
Ronkainen J, Aro P, Storskrubb T, Johansson SE, Lind T, Bolling-Sternevald E, et al. Prevalence of Barrett’s esophagus in the general population: an endoscopic study. Gastroenterology. 2005;129(6):1825–31. doi:10.1053/j.gastro.2005.08.053.
Laine L, Ahnen D, McClain C, Solcia E, Walsh JH. Review article: potential gastrointestinal effects of long-term acid suppression with proton pump inhibitors. Aliment Pharmacol Ther. 2000;14(6):651–68 (pii: apt768).
Lam JR, Schneider JL, Zhao W, Corley DA. Proton pump inhibitor and histamine 2 receptor antagonist use and vitamin B12 deficiency. JAMA. 2013;310(22):2435–42. doi:10.1001/jama.2013.280490.
Marcuard SP, Albernaz L, Khazanie PG. Omeprazole therapy causes malabsorption of cyanocobalamin (vitamin B12). Ann Intern Med. 1994;120(3):211–5.
Steegers-Theunissen RP, Twigt J, Pestinger V, Sinclair KD. The periconceptional period, reproduction and long-term health of offspring: the importance of one-carbon metabolism. Hum Reprod Update. 2013;19(6):640–55. doi:10.1093/humupd/dmt041.
Boxmeer JC, Smit M, Utomo E, Romijn JC, Eijkemans MJ, Lindemans J, et al. Low folate in seminal plasma is associated with increased sperm DNA damage. Fertil Steril. 2009;92(2):548–56. doi:10.1016/j.fertnstert.2008.06.010.
Boxmeer JC, Smit M, Weber RF, Lindemans J, Romijn JC, Eijkemans MJ, et al. Seminal plasma cobalamin significantly correlates with sperm concentration in men undergoing IVF or ICSI procedures. J Androl. 2007;28(4):521–7. doi:10.2164/jandrol.106.001982.
Vujkovic M, de Vries JH, Dohle GR, Bonsel GJ, Lindemans J, Macklon NS, et al. Associations between dietary patterns and semen quality in men undergoing IVF/ICSI treatment. Hum Reprod. 2009;24(6):1304–12. doi:10.1093/humrep/dep024.
Wong WY, Thomas CM, Merkus JM, Zielhuis GA, Steegers-Theunissen RP. Male factor subfertility: possible causes and the impact of nutritional factors. Fertil Steril. 2000;73(3):435–42 (pii: S0015-0282(99)00551-8).
Ebisch IM, Pierik FH, de Jong FH, Thomas CM, Steegers-Theunissen RP. Does folic acid and zinc sulphate intervention affect endocrine parameters and sperm characteristics in men? Int J Androl. 2006;29(2):339–45. doi:10.1111/j.1365-2605.2005.00598.x.
Wong WY, Merkus HM, Thomas CM, Menkveld R, Zielhuis GA, Steegers-Theunissen RP. Effects of folic acid and zinc sulfate on male factor subfertility: a double-blind, randomized, placebo-controlled trial. Fertil Steril. 2002;77(3):491–8 (pii: S0015028201032290).
World Health Organization DoRHaR. WHO laboratory manual for the examination and processing of human semen. Geneva: World Health Organization; 2010.
World Health Organization DoRHaR. WHO laboratory manual for the examination of human semen and sperm–cervical mucus interaction. 4th ed. Cambridge: World Health Organization; 1999.
Beijer C, Kooij van R, Repping S, Rhemrev JP, Breejen EME. Multidisciplinaire richtlijn Semenanalyse: Nederlandse Vereniging voor Obstetrie en Gynaecologie; 2011 [in Ducth, updated 2011; cited 2012 9 november]. Available from: http://nvog-documenten.nl/uploaded/docs/Multidisciplinaire%20richtlijn%20Semenanalyse%20def.pdf
Repping S, van Weert JM, Mol BW, de Vries JW, van der Veen F. Use of the total motile sperm count to predict total fertilization failure in in vitro fertilization. Fertil Steril. 2002;78(1):22–8 (pii: S0015028202031783).
Rhemrev JP, Lens JW, McDonnell J, Schoemaker J, Vermeiden JP. The postwash total progressively motile sperm cell count is a reliable predictor of total fertilization failure during in vitro fertilization treatment. Fertil Steril. 2001;76(5):884–91 (pii: S0015-0282(01)02826-6).
Brouwer IA, van Dusseldorp M, Thomas CM, Duran M, Hautvast JG, Eskes TK, et al. Low-dose folic acid supplementation decreases plasma homocysteine concentrations: a randomized trial. Am J Clin Nutr. 1999;69(1):99–104.
Eisenberg ML, Li S, Behr B, Pera RR, Cullen MR. Relationship between semen production and medical comorbidity. Fertil Steril. 2015;103(1):66–71. doi:10.1016/j.fertnstert.2014.10.017.
Sanchez-Pozo MC, Mendiola J, Serrano M, Mozas J, Bjorndahl L, Menkveld R, et al. Proposal of guidelines for the appraisal of SEMen QUAlity studies (SEMQUA). Hum Reprod. 2013;28(1):10–21. doi:10.1093/humrep/des355.
Magnusdottir EV, Thorsteinsson T, Thorsteinsdottir S, Heimisdottir M, Olafsdottir K. Persistent organochlorines, sedentary occupation, obesity and human male subfertility. Hum Reprod. 2005;20(1):208–15. doi:10.1093/humrep/deh569.
Hayashi T, Miyata A, Yamada T. The impact of commonly prescribed drugs on male fertility. Hum Fertil (Camb). 2008;11(3):191–6. doi:10.1080/14647270701739566.
Gupta A, Gupta S, Tiwary AK. Spermicidal efficacy of H2-receptor antagonists and potentiation with 2’, 4’-dichlorobenzamil hydrochloride: role of intrasperm Ca2+. Contraception. 2003;68(1):61–4 (pii: S0010782403001021).
Van Thiel DH, Gavaler JS, Smith WI Jr, Paul G. Hypothalamic–pituitary–gonadal dysfunction in men using cimetidine. N Engl J Med. 1979;300(18):1012–5. doi:10.1056/NEJM197905033001803.
Wang C, Wong KL, Lam KC, Lai CL. Ranitidine does not affect gonadal function in man. Br J Clin Pharmacol. 1983;16(4):430–2.
Huijgen N, De Ridder M, Verhamme K, Dohle GR, Vanrolleghem A, Sturkenboom MC et al. Are proton-pump inhibitors harmful for semen quality in men of couples planning pregnancy? Fertil Steril. 2016;0015-0282. doi:10.1016/j.fertnstert.2016.09.010.
Hammiche F, Laven JS, Twigt JM, Boellaard WP, Steegers EA, Steegers-Theunissen RP. Body mass index and central adiposity are associated with sperm quality in men of subfertile couples. Hum Reprod. 2012;27(8):2365–72. doi:10.1093/humrep/des177.
Eisenberg ML, Kim S, Chen Z, Sundaram R, Schisterman EF, Buck Louis GM. The relationship between male BMI and waist circumference on semen quality: data from the LIFE study. Hum Reprod. 2014;29(2):193–200. doi:10.1093/humrep/det428.
Sermondade N, Faure C, Fezeu L, Shayeb AG, Bonde JP, Jensen TK, et al. BMI in relation to sperm count: an updated systematic review and collaborative meta-analysis. Hum Reprod Update. 2013;19(3):221–31. doi:10.1093/humupd/dms050.
Hammiche F, Laven JS, Boxmeer JC, Dohle GR, Steegers EA, Steegers-Theunissen RP. Sperm quality decline among men below 60 years of age undergoing IVF or ICSI treatment. J Androl. 2011;32(1):70–6. doi:10.2164/jandrol.109.009647.
Hansen ML, Thulstrup AM, Bonde JP, Olsen J, Hakonsen LB, Ramlau-Hansen CH. Does last week’s alcohol intake affect semen quality or reproductive hormones? A cross-sectional study among healthy young Danish men. Reprod Toxicol. 2012;34(3):457–62. doi:10.1016/j.reprotox.2012.06.004.
Lopez Teijon M, Garcia F, Serra O, Moragas M, Rabanal A, Olivares R, et al. Semen quality in a population of volunteers from the province of Barcelona. Reprod Biomed Online. 2007;15(4):434–44.
Martini AC, Molina RI, Estofan D, Senestrari D, Fiol de Cuneo M, Ruiz RD. Effects of alcohol and cigarette consumption on human seminal quality. Fertil Steril. 2004;82(2):374–7. doi:10.1016/j.fertnstert.2004.03.022.
Povey AC, Clyma JA, McNamee R, Moore HD, Baillie H, Pacey AA, et al. Modifiable and non-modifiable risk factors for poor semen quality: a case-referent study. Hum Reprod. 2012;27(9):2799–806. doi:10.1093/humrep/des183.
Jensen TK, Swan S, Jorgensen N, Toppari J, Redmon B, Punab M, et al. Alcohol and male reproductive health: a cross-sectional study of 8344 healthy men from Europe and the USA. Hum Reprod. 2014;29(8):1801–9. doi:10.1093/humrep/deu118.
Joo KJ, Kwon YW, Myung SC, Kim TH. The effects of smoking and alcohol intake on sperm quality: light and transmission electron microscopy findings. J Int Med Res. 2012;40(6):2327–35.
Kunzle R, Mueller MD, Hanggi W, Birkhauser MH, Drescher H, Bersinger NA. Semen quality of male smokers and nonsmokers in infertile couples. Fertil Steril. 2003;79(2):287–91 (pii: S0015028202046642).
Wallock LM, Tamura T, Mayr CA, Johnston KE, Ames BN, Jacob RA. Low seminal plasma folate concentrations are associated with low sperm density and count in male smokers and nonsmokers. Fertil Steril. 2001;75(2):252–9 (S0015-0282(00)01697-6).
Young SS, Eskenazi B, Marchetti FM, Block G, Wyrobek AJ. The association of folate, zinc and antioxidant intake with sperm aneuploidy in healthy non-smoking men. Hum Reprod. 2008;23(5):1014–22. doi:10.1093/humrep/den036.
Acknowledgements
We thank the preconception counselling team of the outpatient clinic of the Division of Reproductive Medicine and Obstetrics and Prenatal Medicine of the Department of Obstetrics and Gynaecology at the Erasmus MC, University Medical Centre in Rotterdam, the Netherlands, for their significant clinical and research contributions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research received no grants from any funding agency in the public, commercial or not-for-profit sectors.
Conflicts of interest
Nicole Huijgen, Hedwig Goijen, John Twigt, Annemarie Mulders, Jan Lindemans, Gert Dohle, Joop Laven and Régine Steegers-Theunissen have no conflicts of interest that are directly relevant to the content of this study. Joop Laven has received research grants from the following companies: Ferring, Organon, Merck Sharpe and Dome, Merck Serono, Serono, Shering Plough, and Schering.
Ethical approval
All questionnaires and materials were processed anonymously. This study was conducted according to the guidelines of the Declaration of Helsinki, and all procedures involving patients were approved by the Medical Ethical and Institutional Review Board at the Erasmus MC, University Medical Centre in Rotterdam, The Netherlands.
Patient consent
Written informed consent was obtained from all patients.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Huijgen, N.A., Goijen, H.J., Twigt, J.M. et al. Effect of Medications for Gastric Acid-Related Symptoms on Total Motile Sperm Count and Concentration: A Case–Control Study in Men of Subfertile Couples from the Netherlands. Drug Saf 40, 241–248 (2017). https://doi.org/10.1007/s40264-016-0488-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-016-0488-8