Abstract
Background
Spinal cord lesions in multiple sclerosis (MS) have considerable impact on disability. High-efficacy disease-modifying treatments (hDMTs) are associated with greater reduction of relapses and new brain lesions compared to low-efficacy treatments (lDMTs). Knowledge on the impact of DMTs on cord lesion formation is limited as these outcome measures were not included in MS treatment trials. This study aims to investigate whether hDMTs reduce the formation of cord lesions more effectively than lDMTs.
Methods
Patients with relapse-onset MS, a cord magnetic resonance imaging (MRI) within 6 months before/after initiation of their first DMT and ≥1 cord MRI at follow-up (interval > 6 months) were extracted from the MSBase registry (ACTRN12605000455662). Patients treated with hDMTs ≥90% or lDMTs ≥90% of follow-up duration were considered the hDMT and lDMT groups, respectively. Matching was performed using propensity scores. Cox proportional hazards models were used to estimate the hazards of new cord lesions, brain lesions and relapses.
Results
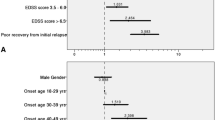
Ninety-four and 783 satisfied hDMT and lDMT group criteria, respectively. Seventy-seven hDMT patients were matched to 184 lDMT patients. In the hDMT group there was no evidence of reduction of new cord lesions (hazard ratio [HR] 0.99 [95% CI 0.51, 1.92], p = 0.97), while there were fewer new brain lesions (HR 0.22 [95% CI 0.10, 0.49], p < 0.001) and fewer relapses (HR 0.45 [95% CI 0.28, 0.72], p = 0.004).
Conclusion
A potential discrepancy exists in the effect of hDMTs over lDMTs in preventing spinal cord lesions versus brain lesions and relapses. While hDMTs provided a significant reduction for the latter when compared to lDMTs, there was no significant reduction in new spinal cord lesions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
While high-efficacy disease-modifying treatments for MS provided a reduction in new brains lesions and relapses when compared to low-efficacy disease-modifying treatments, there was no evidence of a reduction in new spinal cord lesions. |
This study should encourage further research by including spinal cord outcome measures in MS drug trials and in prospective observational cohorts, to show whether there is indeed a regional difference in the effect of DMTs. |
1 Introduction
Multiple sclerosis (MS) is an immune-mediated inflammatory disease of the central nervous system involving both the brain and spinal cord. In addition to brain lesions, approximately 80% of people with MS develop lesions within the spinal cord [1, 2], which are an important contributor to disability [3]. Spinal cord lesions, symptomatic as well as asymptomatic, are associated with more disability accrual in the long term and give an increased risk of secondary progression [2, 4]. Hence, the presence of spinal cord lesions generally warrants a more aggressive treatment strategy [5].
Disease-modifying treatments (DMTs) aim at reducing disease activity by targeting neuroinflammation, where a distinction is made between low- and high-efficacy DMTs, usually defined based on the degree of relapse reduction [6]. Of the DMTs currently used in clinical practice, no trials exist that report spinal cord lesions as an outcome. Consequently, little is known about whether DMTs do inhibit lesion formation in the cord as is the case for brain lesions. One single-center retrospective study of relapse-onset MS patients compared a group on intermediate- and high-efficacy DMTs to a matched group treated with no DMT and/or low-efficacy DMTs. There were significantly fewer new spinal cord lesions in the group with intermediate- and high-efficacy DMTs. However, when only patients with low-efficacy DMTs during follow-up were considered controls, the study was underpowered to show whether high-efficacy DMTs give a larger reduction in formation of new cord lesions than low-efficacy DMTs [7].
Important differences exist between the brain and spinal cord in MS. This argues that brain imaging outcomes in DMT studies should not just be extrapolated to the cord: First, anatomical differences exist, for example in white/grey matter organization, volume and venous anatomy [8, 9]. Second, the blood-brain (BBB) and blood-spinal cord barrier (BSCB) are different with regard to composition, function and, subsequently, their permeability for various cytokines [10, 11]. Last, immunological differences seem to be at play as well. For example, there are indications that the balance between Th1 and Th17 helper cells (through interferon [IFN]γ and interleukin [IL]-17) influence the degree of brain versus spinal cord involvement [12, 13]. These differences underline the importance to evaluate spinal cord separately from brain outcome measures.
In the present study we compared the occurrence of new spinal cord lesions in patients who started with a high-efficacy DMT as initial treatment to matched patients starting a low-efficacy DMT using observational data from the international MSBase registry. The aim is to improve our understanding on the effect of DMTs on spinal cord pathology in MS.
2 Methods
Observational patient-level data were collected from the MSBase registry (WHO International Clinical Trials Registry Platform identifier: ACTRN12605000455662). The MSBase Registry is an observational international MS database established in July 2004. Data are entered into the registry in a standardized manner, using the iMed or the MSBase online data entry systems. The entered MRI data are based upon local radiology reports. All code for data preparation and analysis can be found on https://github.com/danielkreiter/spinalcord-msbase. Data for this study were extracted on the 1st of July, 2022 (i.e., patients included between the start of the registry, July 2004, and data extraction, July 2022, could be included). Ethical approval for the MSBase registry was granted by the Melbourne Health Human Research Ethics Committee and institutional review boards at each site (or exemptions were granted according to local regulations). All patients provided informed consent as per local institutional regulations for inclusion of their data in the registry for clinical and research purposes.
2.1 Study Population
Selected relapse-onset MS patients had at least (i) a spinal cord MRI (at minimum cervical cord coverage) within 6 months before or after initiation of a first DMT, (ii) brain MRI and an EDSS score within 3 months of baseline spinal cord MRI, (iii) another spinal cord MRI at minimum 6 months later, (iv) availability of a minimal baseline dataset (date of birth, sex, treating center, dates of disease onset, clinical definite diagnosis and relapses, treatment start/stop dates). Patients who received placebos, blinded trial medication or treatment not in the list of eligible treatments (see below) were excluded. For the procedures applied to identify any invalid or inconsistent entries, see supplement S1. For a visual overview of baseline and follow-up time window definitions, see Fig. 1.
Baseline and follow-up time window definitions [34].* Censor on last follow-up spinal cord MRI within timeframe where treatment group cut-offs remained satisfied DMT disease modifying treatment; EDSS Expanded Disability Status Scale
Alemtuzumab, cladribine, mitoxantrone, natalizumab, ocrelizumab, ofatumumab, rituximab were classified as hDMTs [14, 15]. Interferons (beta-1a, beta-1b, peginteferon), glatiramer acetate, teriflunomide, methotrexate, azathioprine and immunoglobulins were considered lDMTs. For a clear distinction between the hDMT and lDMT groups, the S1P receptor modulators (S1Ps; fingolimod, ponesimod, ozanimod, siponimod) and dimethyl fumarate (DMF) were excluded from the primary analysis. In the secondary analyses DMF and the S1P receptor modulators were included as hDMTs. Patients treated with either lDMTs or hDMTs for ≥90% of the spinal cord MRI follow-up duration were included, respectively, in the lDMT and hDMT group. Follow-up time was defined as the longest possible spinal cord MRI follow-up in which treatment-group cut-offs remained satisfied. Patients receiving treatment from either class <90% of follow-up were excluded from the primary and secondary analyses. Since in most cases a time interval exists between the baseline spinal cord MRI and initiating the DMT, a 90% of follow-up cut-off was chosen instead of 100%. To assess the impact of the chosen cut-off, sensitivity analyses with ≥95% and ≥80% cut-off were also performed.
To account for the differences in duration of the treatment effect between therapies, the assumed duration of treatment effect after the last dose was based on data on the duration of biological effectiveness and values used in earlier studies: 2 months for natalizumab [15]; 6 months for mitoxantrone, ocrelizumab, rituximab and ofatumumab [15,16,17]; 5 years for alemtuzumab [15]; 96 weeks for cladribine [18]. For the other therapies, the treatment effect was assumed to last until the last dose.
2.2 Outcome
The primary outcome event was new spinal cord lesions during follow-up (new T2 or T1-Gd+ lesions), where the first spinal cord MRI (within 6 months before or after DMT initiation) is considered the baseline. Relapses and new brain MRI lesions were secondary outcomes included as validation, given that for these outcome measures there is a known stronger protective effect of hDMTs over lDMTs. Patients could have had repeated events during follow-up.
2.3 Statistical Analysis
Patients from both treatment groups were matched using propensity scores based on clinical (age, sex, time since first clinical event, EDSS, number of relapses in the preceding 12 months, number of relapses in the preceding 24 months, country) and radiological parameters (baseline number of brain and cord MRI lesions) [19]. The covariates chosen for matching are based upon factors influencing the choice of treatment class in clinical practice and which are used in earlier MS registry studies [15, 19]. Nearest-neighbor matching with a 1:3 variable ratio, without replacement and caliper of 0.1 was performed using the MatchIt R-package [20]. The balance of baseline covariates was assessed using the standardized mean difference (SMD). An SMD of < 0.1 was considered a negligible difference in the mean of a covariate between groups. All subsequent analyses using matched data were weighted to take the variable matching ratio into account. The common follow-up for each matched pair was determined as the shorter of the pairs follow-up periods (pairwise censoring) in order to mitigate attrition bias.
Cox proportional hazards models were applied on matched data to estimate the risk ratio of new spinal lesions, new brain lesions and relapses between treatment groups. In case of repeated events (i.e., multiple relapses, new brain or cord lesions during follow-up) these were all included in the time-to-event analyses. Cumulative hazard plots were used to visualize time-to-event data. All statistical analyses were performed in R version 4.2.1.
A secondary analysis was carried out including S1Ps and one with both S1Ps and DMF as hDMT. To evaluate the robustness of the results and the influence of methodological choices, four sensitivity analyses were performed: (i) changing the group cut-off of ≥90% lDMT/hDMT treatment of follow-up duration to 95%; or (ii) 80% to assess the impact of the chosen cut-off. Additionally, to assess the influence of matching procedure parameters, sensitivity analyses (iii) using a broad caliper in the matching procedure (1:10 match, with broad caliper of 0.4) were performed. In the final sensitivity analysis, (iv) the broad caliper was combined with an 80% cut-off to assess the effect of using a parameter set that maximizes the included sample size.
All analyses were corrected for multiple testing using the Benjamini–Hochberg procedure. Adjusted p-values are reported unless stated otherwise. Where in the primary analysis no evidence of a significant difference was found between the compared groups, the minimum detectable effect (MDE) was calculated within the available cohort at 1 − β = 0.80 and α = 0.05 with 200 simulations per outcome [21].
3 Results
In total, 1842 patients were identified with a relapse-onset MS who underwent spinal cord MRI within a time window of 6 months around initiation of their first DMT and had at least one more spinal cord MRI at follow-up (minimal interval 6 months after baseline spinal cord MRI). Where 68.7% of spinal cord MRIs covered the whole cord, the rest covered only the cervical cord. In 82.5% of cord investigations post-gadolinium sequences were acquired. Figure 2 shows the flowchart of patient selection and exclusion. Ninety-four and 783 satisfied hDMT and lDMT group criteria, respectively. Seventy-seven hDMT patients were matched to 184 lDMT patients. Patient characteristics before and after matching are shown in Table 1. The two matched groups were well balanced on the measured characteristics at baseline (SMD < 0.1). For additional figures on the matching procedure, see Supplement S2. The list of countries of where patients were treated can be found in Supplement S3. Treatments used during follow-up in both treatment groups (total groups and the subgroups that developed new cord lesions) as proportion of the total follow-up time are shown in Fig. 3.
Disease-modifying treatment usage during follow-up as proportion of follow-up time. ALE alemtuzumab, CLA cladribine, GLA glatiramer acetate, IFN interferons, IVIG immunoglobulins, MIT mitoxantrone, NAT natalizumab, OCR ocrelizumab, OFA ofatumumab, ONA ozanimod, SIP siponimod, TER teriflunomide. * Fingolimod (0.06%), glatiramer acetate (0.17%) for the hDMT group. In the control group: methotrexate (0.21%), dimethylfumarate (0.03%), natalizumab (0.13%), fingolimod (0.12%), siponimod (0.44%). In the subgroup with new cord lesions in the control group: methotrexate (0.67%), natalizumab (0.10%)
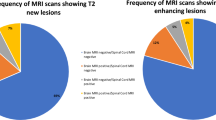
At baseline, 81.2% of matched patients had at least one spinal cord lesion (60.5% in unmatched cohort). In the hDMT group there were 12 (15.6%) patients who developed 12 new cord lesions (mean follow-up 2.6 years [SD 1.5 years]; 0.06 lesions per patient year; 55.6% gadolinium-enhancing). In the lDMT group, 51 (27.7%) patients developed 65 new cord lesions (mean follow-up 4.2 years [SD 3.0 years]; 0.08 lesions per patient year; 41.3% gadolinium-enhancing). After pairwise censoring, mean follow-up time was 2.1 years (SD 1.2, range 0.5–8.3 years). There was no statistically or clinically significant difference in the risk of new cord lesions between groups (HR 0.99, [95% CI 0.51, 1.92], p = 0.97), as can also been seen the survival curves in Fig. 4. This while there were fewer new brain lesions (HR 0.22, [95% CI 0.10, 0.49], p < 0.001) on MRI and relapses (HR 0.45, [95% CI 0.28, 0.72], p = 0.004) in the hDMT compared to the lDMT group. When S1Ps and DMF were included as hDMT, there was a similar pattern (see Table 2).
Sensitivity analyses showed similar results, an overview of which is shown in Table 2. Here the differences in the occurrence of spinal cord lesions were somewhat larger (HRs between 0.58 and 0.70 across the different sensitivity analyses) but not statistically significant. Analysis of the minimum detectable effect size was performed for the primary analyses. This did not show statistically significant differences, which was only the case for the occurrence of new cord lesions. This analysis was sufficiently powered to detect a minimum difference of 55% in cumulative hazard for new spinal cord lesions.
4 Discussion
This observational propensity score-matched study of patients with relapse-onset MS aimed to show whether treatment with hDMTs results in a larger reduction of new spinal cord lesions when compared to lDMTs. The study found no evidence of a difference for the occurrence of new cord lesions between the hDMT and lDMT groups. In contrast, the study found a reduction of new brain lesions and relapses in the hDMT when compared with lDMT. Therefore, while earlier literature suggests that using a DMT in general reduces the formation of new spinal cord lesions [7], currently there is no evidence for a larger reduction of spinal cord disease activity when using hDMTs compared to lDMTs, as is the case for brain lesions and clinical relapses.
While the primary analysis convincingly shows no difference in new cord lesions between groups, the sensitivity analysis using a broad caliper combined with a loosened cut-off for the proportion of follow-up duration used for the definition of treatment groups (≥80% instead of ≥90%) showed some difference between groups for new cord lesions (HR 0.58, p = 0.05). While these liberal parameters led to a larger included sample, with still small differences in baseline group characteristics (SMD < 0.1, see Supplement S4), this result needs to be interpreted with caution, since 20% of time not on the group-defining medication could be of influence.
A possible reason for the discrepancy in the effect of hDMTs in preventing new cord lesions versus brain lesions lies in the differences between brain and spinal cord with regard to anatomical organization, BBB/BSCB composition and function [10], regional immunological differences [12, 22, 23] and maybe also in repair capabilities [24,25,26].
Exploratively comparing the medications being used in the group of patients that developed new cord lesions while under a hDMT to the group that did not (see Fig. 3), there are no striking differences with regard to which treatments were used. Therefore, currently, there are no indications that one subgroup of hDMTs would have a more potent effect on the spinal cord compartment of the CNS. This contrasts with a smaller recent local cohort study, where cord lesions were less common in patients being treated with B-cell–depleting therapies [7].
With the use of conventional MRI, as in the present study, we can only address focal inflammatory demyelinating activity for which focal lesions on MRI are a marker [27]. However, diffuse inflammation and axonal loss in the cord are other important components of cord pathology resulting in disability worsening [28, 29]. Therefore, we do not know whether these different groups of DMTs have a different effect on the relevant pathological processes other than focal demyelination. Currently, quantification of diffuse inflammation and demyelination in the CNS in vivo, and even more in the spinal cord, is still challenging and requires advanced imaging techniques, which currently are not easily applied in clinical practice [30, 31].
4.1 Limitations and Strengths
Inherent to the use of registry-based data in this study, there are some important limitations. A main limitation is the absence of systematic and comparable acquisition of radiological outcomes and the lack of information in the registry on acquisition methods. Since spinal cord MRI imaging is challenging in acquisition as well as the assessment, and artifact-prone, detection of lesions is very dependent on the quality of the investigation. Also, information on the field strength on which the investigations were performed was not available. But, in contrast to brain imaging, the difference in lesion sensitivity between 1.5 T and 3 T seems limited for spinal cord MRI [32]. Still, with regard to acquisition, it is not expected that there would be a structural difference between the two groups. One has to recognize that the incidence of new spinal cord lesions in this study is probably not representative of the true occurrence of new cord lesions. Spinal cord MRI is currently not an investigation performed routinely at follow-up [33] and is mostly performed at the discretion of the clinician. This means that the included patients (with >1 spinal cord MRI) were probably patients with either new cord-related symptoms, unexplained disability progression, who possibly switched therapies during follow-up or were followed-up with cord MRI due to earlier cord lesions. This could have resulted in patients with good therapy response to be underrepresented in both groups. Finally, given the minimum detectable difference of 55%, a small-to-moderate reduction of the risk of spinal cord activity when using hDMTs compared to lDMTs for new cord lesions cannot be fully ruled out.
With regard to the propensity scores, ideally, gadolinium-enhancing lesions on MRI and CSF markers (number of oligoclonal bands, IgG index) would also be part of the covariates used in the matching procedure, since these are also considered in treatment decisions in clinical practice. However, due to the degree of incomplete cases that this would lead to, these were not included.
Furthermore, a large number of patients from the registry could not be included because there was no spinal cord MRI close enough to treatment initiation (see Fig. 2). For a large part, this could be due to more limited registration of spinal cord MRIs in the registry compared to brain MRIs, while in reality these were probably performed since spinal-cord MRI is a routine part of the diagnostic workup in international guidelines. However, when patients initiate treatment—not after diagnosis but later at follow-up—it is likely that there are a certain number of cases where there was no rebaseline spinal cord MRI causing their exclusion from this study. However, this is unlikely to have caused a structural difference between groups since this applies to both groups. Also, there were differences in the median follow-up time, where the median follow-up time in the lDMT group was longer than in the hDMT group. A possible reason is that in the lDMT group relapses or progression occurred more often until longer after baseline leading to more spinal-cord MRIs being performed until later after baseline. To avoid attrition bias, this has been accounted for in the analyses by adapting pairwise censoring.
A strength of this study is the application of matching to address confounding by severity and the matching resulted in similar groups across the important determinants. But it is still possible that differences exist between the groups on unmeasured variables. Another strength of this registry-based study is that it is a multicentric study including patients from all over the world. Although, it is important to note that the main part of the sample consisted of patients from Italy followed by Turkey and Australia.
5 Conclusion
In conclusion, there is currently no evidence that hDMT usage results in a larger reduction of new cord lesions than lDMTs, as is the case for new brain lesions and relapses. Whilst, this is an interesting and important finding, results need to be interpreted with caution as the present registry study has important limitations as discussed in the limitations section. The current findings should be considered a plea to work towards more, and a higher level, of evidence to either confirm or reject the presently suggested discrepancy of the hDMT effect on brain lesions and relapses versus spinal cord lesions. In order to gain further insight into the effect of DMTs on spinal cord pathology in MS, it is necessary to (i) more often include spinal cord outcome measures in MS drug trials and prospective observational cohorts, (ii) encourage registration of spinal cord data in MS registries and (iii) study the interplay between therapies and the different MS pathological processes in the cord using advanced imaging techniques, which have increasingly become part of the research toolbox.
References
Bot JC, Barkhof F, Polman CH, Lycklama a Nijeholt GJ, de Groot V, Bergers E, et al. Spinal cord abnormalities in recently diagnosed MS patients: added value of spinal MRI examination. Neurology. 2004;62:226–33.
Lukas C, Sombekke MH, Bellenberg B, Hahn HK, Popescu V, Bendfeldt K, et al. Relevance of spinal cord abnormalities to clinical disability in multiple sclerosis: MR imaging findings in a large cohort of patients. Radiology. 2013;269:542–52.
Brownlee WJ, Altmann DR, Prados F, Miszkiel KA, Eshaghi A, Gandini Wheeler-Kingshott CAM, et al. Early imaging predictors of long-term outcomes in relapse-onset multiple sclerosis. Brain. 2019;142:2276–87.
Lauerer M, McGinnis J, Bussas M, El Husseini M, Pongratz V, Engl C, et al. Prognostic value of spinal cord lesion measures in early relapsing-remitting multiple sclerosis. J Neurol Neurosurg Psychiatry. 2023. https://doi.org/10.1136/jnnp-2023-331799.
Rotstein D, Montalban X. Reaching an evidence-based prognosis for personalized treatment of multiple sclerosis. Nat Rev Neurol. 2019;15:287–300.
Li H, Hu F, Zhang Y, Li K. Comparative efficacy and acceptability of disease-modifying therapies in patients with relapsing-remitting multiple sclerosis: a systematic review and network meta-analysis. J Neurol. 2020;267:3489–98.
Kreiter D, Spee R, Merry A, Hupperts R, Gerlach O. Effect of disease-modifying treatment on spinal cord lesion formation in multiple sclerosis: a retrospective observational study. Mult Scler Relat Disord. 2023;79: 104994.
Henmar S, Simonsen EB, Berg RW. What are the gray and white matter volumes of the human spinal cord? J Neurophysiol. 2020;124:1792–7.
Thron AK. Vascular anatomy of the spinal cord: radioanatomy as the key to diagnosis and treatment. Berlin: Springer; 2016.
Bartanusz V, Jezova D, Alajajian B, Digicaylioglu M. The blood-spinal cord barrier: morphology and clinical implications. Ann Neurol. 2011;70:194–206.
Pan W, Banks WA, Kastin AJ. Permeability of the blood-brain and blood-spinal cord barriers to interferons. J Neuroimmunol. 1997;76:105–11.
Goverman J. Autoimmune t cell responses in the central nervous system. Nat Rev Immunol. 2009;9:393–407.
Johnson MC, Pierson ER, Spieker AJ, Nielsen AS, Posso S, Kita M, et al. Distinct t cell signatures define subsets of patients with multiple sclerosis. Neurol Neuroimmunol Neuroinflamm. 2016;3: e278.
Filippi M, Amato MP, Centonze D, Gallo P, Gasperini C, Inglese M, et al. Early use of high-efficacy disease-modifying therapies makes the difference in people with multiple sclerosis: An expert opinion. J Neurol. 2022;269:5382–94.
He A, Merkel B, Brown JWL, Zhovits Ryerson L, Kister I, Malpas CB, et al. Timing of high-efficacy therapy for multiple sclerosis: a retrospective observational cohort study. Lancet Neurol. 2020;19:307–16.
Bar-Or A, Grove RA, Austin DJ, Tolson JM, VanMeter SA, Lewis EW, et al. Subcutaneous ofatumumab in patients with relapsing-remitting multiple sclerosis: the MIRROR study. Neurology. 2018;90:e1805–14.
Hauser S, Bar-Or A, Cohen JA, Comi G, Correale J, Coyle PK, et al. B-cell depletion and efficacy outcomes with ofatumumab: subgroup analysis from the pooled phase 3 ASCLEPIOS I and II trials (2356). Neurology. 2020;94(15 Supplement):2356.
Comi G, Cook S, Giovannoni G, Rieckmann P, Sorensen PS, Vermersch P, et al. Effect of cladribine tablets on lymphocyte reduction and repopulation dynamics in patients with relapsing multiple sclerosis. Multiple Scler Relat Disord. 2019;29:168–74.
Roos I, Leray E, Casey R, Horakova D, Havrdova E, Izquierdo G, et al. Effects of high- and low-efficacy therapy in secondary progressive multiple sclerosis. Neurology. 2021;97:e869–80.
Stuart EA, King G, Imai K, Ho D. MatchIt: nonparametric preprocessing for parametric causal inference. J Stat Softw. 2011;42(8):1–28.
Kalincik T, Brown JWL, Robertson N, Willis M, Scolding N, Rice CM, et al. Treatment effectiveness of alemtuzumab compared with natalizumab, fingolimod, and interferon beta in relapsing-remitting multiple sclerosis: a cohort study. Lancet Neurol. 2017;16:271–81.
DeLuca GC, Alterman R, Martin JL, Mittal A, Blundell S, Bird S, et al. Casting light on multiple sclerosis heterogeneity: the role of HLA-DRB1 on spinal cord pathology. Brain. 2013;136(Pt 4):1025–34.
Qiu W, Raven S, James I, Luo Y, Wu J, Castley A, et al. Spinal cord involvement in multiple sclerosis: a correlative MRI and high-resolution HLA-DRB1 genotyping study. J Neurol Sci. 2011;300:114–9.
Hampton DW, Anderson J, Pryce G, Irvine KA, Giovannoni G, Fawcett JW, et al. An experimental model of secondary progressive multiple sclerosis that shows regional variation in gliosis, remyelination, axonal and neuronal loss. J Neuroimmunol. 2008;201–202:200–11.
Wolswijk G. Oligodendrocyte precursor cells in the demyelinated multiple sclerosis spinal cord. Brain. 2002;125(Pt 2):338–49.
Frischer JM, Weigand SD, Guo Y, Kale N, Parisi JE, Pirko I, et al. Clinical and pathological insights into the dynamic nature of the white matter multiple sclerosis plaque. Ann Neurol. 2015;78:710–21.
Filippi M, Brück W, Chard D, Fazekas F, Geurts JJG, Enzinger C, et al. Association between pathological and MRI findings in multiple sclerosis. Lancet Neurol. 2019;18:198–210.
Petrova N, Carassiti D, Altmann DR, Baker D, Schmierer K. Axonal loss in the multiple sclerosis spinal cord revisited. Brain Pathol. 2018;28:334–48.
DeLuca GC, Ebers GC, Esiri MM. Axonal loss in multiple sclerosis: a pathological survey of the corticospinal and sensory tracts. Brain. 2004;127(Pt 5):1009–18.
Combes AJE, Clarke MA, O’Grady KP, Schilling KG, Smith SA. Advanced spinal cord MRI in multiple sclerosis: current techniques and future directions. NeuroImage Clin. 2022. https://doi.org/10.1016/j.nicl.2022.103244.
Rissanen E, Tuisku J, Rokka J, Paavilainen T, Parkkola R, Rinne JO, et al. In vivo detection of diffuse inflammation in secondary progressive multiple sclerosis using PET imaging and the radioligand (1)(1)c-PK11195. J Nucl Med. 2014;55:939–44.
Stankiewicz JM, Neema M, Alsop DC, Healy BC, Arora A, Buckle GJ, et al. Spinal cord lesions and clinical status in multiple sclerosis: a 1.5 T and 3 T MRI study. J Neurol Sci. 2009;279:99–105.
Wattjes MP, Ciccarelli O, Reich DS, Banwell B, de Stefano N, Enzinger C, et al. 2021 MAGNIMS-CMSC-NAIMS consensus recommendations on the use of MRI in patients with multiple sclerosis. Lancet Neurol. 2021;20:653–70.
Wang SV, Schneeweiss S. A framework for visualizing study designs and data observability in electronic health record data. Clin Epidemiol. 2022;14:601–8.
Acknowledgments
The authors thank all patients and their caregivers who have participated in this study and who have contributed data to the MSBase cohort. The MSBase Study co-investigators and contributors are listed in the supplementary appendix S5. Collaborators of the MSBase Study Group: Barnett MH, Shaw C, John NA, Buzzard KA, Skibina OG, Garber JY, McCombe PA, Taylor BV, Van der Walt A, Butzkueven H, Grammond P, Grand’Maison F, Lapointe E, Sanchez-Menoyo JL, Besora S, Lugaresi A, Onofrj M, Amato MP, Alkhaboori J, Al-Asmi A, Boz C, Soysal A, Turkoglu R.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Funding
The MSBase Foundation is a not-for-profit organization that receives support from Biogen, Novartis, Merck, Roche, Teva, and Sanofi Genzyme. This specific study did not receive any specific grant from funding agencies in the public, commercial, or non-profit sectors.
Conflict of Interest
Serkan Ozakbas has nothing to disclose. Daniel Kreiter and Oliver Gerlach received institutional research grants. Tomas Kalincik served on scientific advisory boards for MS International Federation and World Health Organization, BMS, Roche, Janssen, Sanofi Genzyme, Novartis, Merck and Biogen, steering committee for Brain Atrophy Initiative by Sanofi Genzyme, received conference travel support and/or speaker honoraria from WebMD Global, Eisai, Novartis, Biogen, Roche, Sanofi-Genzyme, Teva, BioCSL and Merck and received research or educational event support from Biogen, Novartis, Genzyme, Roche, Celgene and Merck. Tomas Kalincik is also an Editorial Board member of CNS Drugs. He was not involved in the selection of peer reviewers for the manuscript nor any of the subsequent editorial decisions. Raymond Hupperts received institutional research grants and fees for lectures and advisory boards from Biogen, Merck and Genzyme-Sanofi. Francesco Patti received personal compensation for serving on advisory board for Almirall, Alexion, Biogen, Bristol, Berck, Novartis and Roche. He further received research grants by Biogen, Merck and Roche and by FISM, Reload Association (Onlus), Italian Health Minister, University of Catania. Daniele Spitaleri received honoraria as a consultant on scientific advisory boards by Bayer-Schering, Novartis and Sanofi-Aventis and compensation for travel from Novartis, Biogen, Sanofi Aventis, Teva and Merck. Matteo Foschi received travel and meeting attendance support from Novartis, Biogen, Roche, Sanofi-Genzyme and Merck. Davide Maimone received speaker honoraria for Advisory Board and travel grants from Almirall, Biogen, Merck, Novartis, Roche, Sanofi-Genzyme, and Teva. Bassem Yamout received honoraria as a speaker and member of scientific advisory boards from Sanofi, Bayer, Biogen, Merck, Janssen, Novartis, Roche and Aspen. Samia J. Khoury received compensation for scientific advisory board activity from Merck and Roche and received compensation for serving on the IDMC for Biogen. Jeannette Lechner-Scott travel compensation from Novartis, Biogen, Roche and Merck. Her institution receives the honoraria for talks and advisory board commitment as well as research grants from Biogen, Merck, Roche, TEVA and Novartis.
Ethics Approval
Ethical approval for the MSBase registry was granted by the Melbourne Health Human Research Ethics Committee and institutional review boards at each site (or exemptions were granted according to local regulations).
Consent to Participate
All patients provided informed consent as per local institutional regulations for inclusion of their data in the registry for clinical and research purposes.
Consent to Publication
Not applicable
Availability of Data and Material
Data were obtained from the international MSBase registry. Information on data access and availability can be found on the https://www.msbase.org/.
Code Availability
All code for data preparation and analysis can be found on https://github.com/danielkreiter/spinalcord-msbase.
Authors’ Contributions
Daniel Kreiter: Conceptualization, Methodology, Formal analysis, Visualization, Writing—Original Draft; Tomas Kalincik: Conceptualization, Methodology, Writing—Review & Editing; Raymond Hupperts: Supervision, Conceptualization, Writing—Review & Editing; Francesco Patti: Writing—Review & Editing, Data Curation; Daniele Spitaleri: Writing—Review & Editing, Data Curation, Matteo Foschi: Writing—Review & Editing, Data Curation; Andrea Surcinelli: Writing—Review & Editing, Data Curation; Davide Maimone: Writing—Review & Editing, Data Curation; Bassem Yamout: Writing—Review & Editing, Data Curation; Samia J. Khoury: Writing—Review & Editing, Data Curation; Jeannette Lechner-Scott: Writing—Review & Editing, Data Curation; Serkan Ozakbas: Writing—Review & Editing, Data Curation; Oliver Gerlach: Supervision, Conceptualization, Writing—Review & Editing, Data Curation. All authors had authority over manuscript preparation and the decision to submit this manuscript for publication.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kreiter, D., Kalincik, T., Hupperts, R. et al. Effectiveness of Disease-Modifying Treatment on Spinal Cord Lesion Formation in Relapse-Onset Multiple Sclerosis: An MSBase Registry Study. CNS Drugs (2024). https://doi.org/10.1007/s40263-024-01115-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s40263-024-01115-x